Wed, Apr 17, 2024
[Archive]
Volume 2, Issue 3 (Summer 2016 -- 2016)
JCCNC 2016, 2(3): 135-144 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bastani F, Birjandi M, Haghani H, Sobhan M R. Factors Associated With Fear of Falling and Functional Independence in Older Adult Living in an Iranian Nursing Home: A Cross-Sectional Study. JCCNC 2016; 2 (3) :135-144
URL: http://jccnc.iums.ac.ir/article-1-75-en.html
URL: http://jccnc.iums.ac.ir/article-1-75-en.html
1- Department of Geriatric Nursing, School of Nursing & Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Community Health Nursing, School of Nursing & Midwifery, Iran University of Medical Sciences, Tehran, Iran. , m.birjandi155@gmail.com
3- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedics, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Department of Community Health Nursing, School of Nursing & Midwifery, Iran University of Medical Sciences, Tehran, Iran. , m.birjandi155@gmail.com
3- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedics, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Full-Text [PDF 1660 kb]
(2405 Downloads)
| Abstract (HTML) (7585 Views)
Full-Text: (975 Views)
1. Background
Falls are a major health concern in older population and require effective prevention. Falls are the second leading cause of accidental death worldwide with an annual rate of 424000 deaths (Vavilala, Curry, & Ramaiah, 2011). Fear of falling is a complex construct, thought to predominantly affect older adults. However, not everyone who falls develops a fear of falling and people who have not fallen may be fearful even though it is commonly assumed that falls and fear of falling are conflated (Yardley et al. 2002; Painter et al. 2012). Additionally, fall-related injuries are 5 times more likely to occur in older adults aged over 65 years (Orces 2014). Both the incidence of falls and the severity of fall-related complications rise steadily after the age of 60 (Kalula et al. 2016). About a third of community-dwelling people aged 65 years and older fall each year; the rate of falls rises with age (Bertera et al. 2007).
Fear of falling has been suggested to be an important factor in predicting future falls with the major consequence of avoiding activities (Bertera et al. 2007; Soriano et al. 2007). With regard to consequences of falling, it is crucial that at risk individuals understand possible causes of falling. Providing fall prevention education for older adults can help them understand falling risk factors (Soriano et al. 2007). Educational level was identified as an independent risk factor for any and multiple falls (Gill, Taylor & Pengelly 2005); higher education and income were both associated with lower falling risk (Tao & McRoy 2015).
Falling risk factors could be categorized as intrinsic or extrinsic (Guthrie et al. 2012). The intrinsic risk factors included health history and biological factors. These factors extend beyond age, health and medical conditions, physical fitness, mobility, function, history of falls, gender, race/ethnicity, and cognitive and psychological issues (Guthrie et al. 2012). According to the annual rates of nonfatal injuries, the health impact from falls may be greater for female older adults than males (Self-Reported Falls, 2006). Similarly, white women also showed significantly higher rates of fall-related fractures such as hip than women of other ethnicities (Hanlon et al. 2002).
Functional disability is common in older adults, which is associated with high risk of subsequent health decline (Soriano et al. 2007). Traditionally functional status is defined as the ability to perform activities such as bathing, dressing, feeding, toileting, having continence, housekeeping, transferring, using telephone, cooking, managing money, and so on. It is a strong predictor of survival, a determinant of caregiving needs and health care costs, and a factor in decisions about medical procedures (Kurella et al., 2009; Tao & McRoy 2015). It is reported that fear of falling may only indirectly influence activity restriction through its impact on balance and functional mobility (Allison et al. 2013). However, there is an association between functional mobility and recurrent falls for community-dwelling older adults (Shumway-Cook, Brauer & Woollacott 2000).
A major goal for societies with elderly population is to create conditions for them to stay healthy and remain active at their homes as long as possible (Kurella et al. 2009). Therefore, studying correlates of fear of falling is an important research avenue as it can provide guidance for identifying elderly people who are at risk of falls, loss of functional independence and quality of life. Therefore, the purpose of this study was to determinate association between demographic characteristics of elderly living in nursing homes and fear of falling and functional independence.
2. Materials and Methods
This was a cross-sectional study, with a sample of older adults recruited in 25 nursing homes in Tehran, Iran between September 2015 and November 2015. To conduct the research study, the researchers obtained approval from the Iran Medical Science University, Tehran Review Board (IR.IUMS.REC:1394.921180202) for the protection of human subjects. All participants provided written informed consents which were approved by the institutional review board before participation.
Sample size
Calculation of the sample size was based on the data collected from previous studies and the following formula:

, where n stands for "sample size", σ2 for "standard deviation", Zβ for "0.84 for 80% power", Zα/2 for "level of statistical difference as 1.96", and r for "according to the previous studies". Using the above formula and similar studies conducted previously, we calculated the sample size as 200.
Two hundred nursing home living older adults, were recruited with convenience sampling method, and participated in this study. Eligibility requirements included aged 65 years or older, able to walk three meters comfortably (with or without aid), and stand for a few minutes unsupported (two to three minutes to administer the Functional Reach test). Exclusion criteria included having cognitive impairment confirmed by abbreviated mental states test (AMTs) score < 6, psychiatric disorders, acute conditions such as arthritis, cardiac disease, and stroke, severe hearing and vision deficits, and language impairment.
Assessment tools
Falls-related self-efficacy (FES-1) was designed to assess the degree of perceived efficacy at avoiding fall during each of 10 relatively non-hazardous activities of daily living, including taking a bath or shower, reaching into cabinets or closets, preparing meals that do not require carrying heavy or hot objects, walking around the house, getting in and out of bed, answering the door or telephone, getting in and out of a chair, getting dressed and undressed, light housekeeping, and simple shopping (Mahoney et al. 1965; Tinetti et al. 1990).
The Persian version of FES-I questionnaire was used to evaluate the worry associated with the possibility of falling when performing 16 activities inside and outside home, with scores from 1 to 4 points per each activity (Dadgari et al. 2015). The total score is obtained by the sum of the scores in all activities, ranging from 16 to 64 points, in which the higher value indicates lower self-efficacy. Both reliability and validity of the Persian FES-I were found to be acceptable (Cronbach α = 0.75, interclass correlation coefficients = 0.99, P < 0.001 and standard errors of measurements = 1.82) (Mosallanezhad et al., 2011).
Activities of daily living were based on the Barthel Index (BI) (Morris et al., 2004). BI is a scale that measures disability or dependence in activities of the elderly. It measures the capacity to perform 10 basic activities of daily living. In particular, items are divided into groups that relate to self-care such as feeding, grooming, bathing, dressing, bowel and bladder care, and toilet use and mobility such as ambulation, transfers, and stairs climbing. In this scale, higher scores reflect greater independence in the participants. In BI original version, a patient with 100 score is continent; independent in feeding, dressing, getting in and out of bed, and bathing; can walk at least one block; and can climb up and down stairs without help. According to the Shah et al., a score of 0–20 suggests total dependence, 21–60, severe dependence; 61–90, moderate dependence; and 91–99 slight, dependence (Shah, Vanclay & Cooper 1989).
In this study, the inter-rater reliability coefficient (Kappa) for every item was more than 0.6; Inter-rater reliability of total BI was 0.998. In addition, the questionnaire reliability coefficient (internal consistency) was measured as 0.96-0.99 and item-total correlation confirmed its reliability, too. In Tagharrobi et al. study, its concurrent validity with Persian original BI was confirmed (r = 0.993, P < 0.0001) and the known-groups approach revealed its validity (P < 0.0001) (Tagharrobi, Sharifi & Sooky 2011).
Statistical Analyses
Statistical analyses were performed by IBM SPSS version 20.0 (IBM Corporation, Armonk, NY, USA). In this study, variables were analyzed using Student t test and ANOVA. Pearson coefficient correlation was used to examine the relationship between FES and BBS. A 2-tailed P < 0.05 was considered statistically significant.
3. Results
Demographic characteristics of the participants are presented in Table 1. A total of 200 elderly living in nursing homes with the mean (SD) age of 76.89(8.50) years (age range 60-93) were included in the study and remained until the end of the study. One hundred and three females and 97 male participated in the study. Fifty-nine participants were 70 years of age and 65 participants were 71-80 years of age. Nine percent of the participants were illiterate (84%) and 32% of them were living for more than 2 years in the nursing homes. As for marital status, 50.3% were widowed, 32.7% married, and 14.5% had no children. About 36% had good economic status. The most frequently reported medical condition among participants was cardiovascular (70 %) problems, followed by Type 2 diabetes mellitus (31.5%), and pulmonary diseases (11.5%). Twenty (39.2%) participants reported one fall in the previous 12 months (Table 1).
Falls are a major health concern in older population and require effective prevention. Falls are the second leading cause of accidental death worldwide with an annual rate of 424000 deaths (Vavilala, Curry, & Ramaiah, 2011). Fear of falling is a complex construct, thought to predominantly affect older adults. However, not everyone who falls develops a fear of falling and people who have not fallen may be fearful even though it is commonly assumed that falls and fear of falling are conflated (Yardley et al. 2002; Painter et al. 2012). Additionally, fall-related injuries are 5 times more likely to occur in older adults aged over 65 years (Orces 2014). Both the incidence of falls and the severity of fall-related complications rise steadily after the age of 60 (Kalula et al. 2016). About a third of community-dwelling people aged 65 years and older fall each year; the rate of falls rises with age (Bertera et al. 2007).
Fear of falling has been suggested to be an important factor in predicting future falls with the major consequence of avoiding activities (Bertera et al. 2007; Soriano et al. 2007). With regard to consequences of falling, it is crucial that at risk individuals understand possible causes of falling. Providing fall prevention education for older adults can help them understand falling risk factors (Soriano et al. 2007). Educational level was identified as an independent risk factor for any and multiple falls (Gill, Taylor & Pengelly 2005); higher education and income were both associated with lower falling risk (Tao & McRoy 2015).
Falling risk factors could be categorized as intrinsic or extrinsic (Guthrie et al. 2012). The intrinsic risk factors included health history and biological factors. These factors extend beyond age, health and medical conditions, physical fitness, mobility, function, history of falls, gender, race/ethnicity, and cognitive and psychological issues (Guthrie et al. 2012). According to the annual rates of nonfatal injuries, the health impact from falls may be greater for female older adults than males (Self-Reported Falls, 2006). Similarly, white women also showed significantly higher rates of fall-related fractures such as hip than women of other ethnicities (Hanlon et al. 2002).
Functional disability is common in older adults, which is associated with high risk of subsequent health decline (Soriano et al. 2007). Traditionally functional status is defined as the ability to perform activities such as bathing, dressing, feeding, toileting, having continence, housekeeping, transferring, using telephone, cooking, managing money, and so on. It is a strong predictor of survival, a determinant of caregiving needs and health care costs, and a factor in decisions about medical procedures (Kurella et al., 2009; Tao & McRoy 2015). It is reported that fear of falling may only indirectly influence activity restriction through its impact on balance and functional mobility (Allison et al. 2013). However, there is an association between functional mobility and recurrent falls for community-dwelling older adults (Shumway-Cook, Brauer & Woollacott 2000).
A major goal for societies with elderly population is to create conditions for them to stay healthy and remain active at their homes as long as possible (Kurella et al. 2009). Therefore, studying correlates of fear of falling is an important research avenue as it can provide guidance for identifying elderly people who are at risk of falls, loss of functional independence and quality of life. Therefore, the purpose of this study was to determinate association between demographic characteristics of elderly living in nursing homes and fear of falling and functional independence.
2. Materials and Methods
This was a cross-sectional study, with a sample of older adults recruited in 25 nursing homes in Tehran, Iran between September 2015 and November 2015. To conduct the research study, the researchers obtained approval from the Iran Medical Science University, Tehran Review Board (IR.IUMS.REC:1394.921180202) for the protection of human subjects. All participants provided written informed consents which were approved by the institutional review board before participation.
Sample size
Calculation of the sample size was based on the data collected from previous studies and the following formula:

, where n stands for "sample size", σ2 for "standard deviation", Zβ for "0.84 for 80% power", Zα/2 for "level of statistical difference as 1.96", and r for "according to the previous studies". Using the above formula and similar studies conducted previously, we calculated the sample size as 200.
Two hundred nursing home living older adults, were recruited with convenience sampling method, and participated in this study. Eligibility requirements included aged 65 years or older, able to walk three meters comfortably (with or without aid), and stand for a few minutes unsupported (two to three minutes to administer the Functional Reach test). Exclusion criteria included having cognitive impairment confirmed by abbreviated mental states test (AMTs) score < 6, psychiatric disorders, acute conditions such as arthritis, cardiac disease, and stroke, severe hearing and vision deficits, and language impairment.
Assessment tools
Falls-related self-efficacy (FES-1) was designed to assess the degree of perceived efficacy at avoiding fall during each of 10 relatively non-hazardous activities of daily living, including taking a bath or shower, reaching into cabinets or closets, preparing meals that do not require carrying heavy or hot objects, walking around the house, getting in and out of bed, answering the door or telephone, getting in and out of a chair, getting dressed and undressed, light housekeeping, and simple shopping (Mahoney et al. 1965; Tinetti et al. 1990).
The Persian version of FES-I questionnaire was used to evaluate the worry associated with the possibility of falling when performing 16 activities inside and outside home, with scores from 1 to 4 points per each activity (Dadgari et al. 2015). The total score is obtained by the sum of the scores in all activities, ranging from 16 to 64 points, in which the higher value indicates lower self-efficacy. Both reliability and validity of the Persian FES-I were found to be acceptable (Cronbach α = 0.75, interclass correlation coefficients = 0.99, P < 0.001 and standard errors of measurements = 1.82) (Mosallanezhad et al., 2011).
Activities of daily living were based on the Barthel Index (BI) (Morris et al., 2004). BI is a scale that measures disability or dependence in activities of the elderly. It measures the capacity to perform 10 basic activities of daily living. In particular, items are divided into groups that relate to self-care such as feeding, grooming, bathing, dressing, bowel and bladder care, and toilet use and mobility such as ambulation, transfers, and stairs climbing. In this scale, higher scores reflect greater independence in the participants. In BI original version, a patient with 100 score is continent; independent in feeding, dressing, getting in and out of bed, and bathing; can walk at least one block; and can climb up and down stairs without help. According to the Shah et al., a score of 0–20 suggests total dependence, 21–60, severe dependence; 61–90, moderate dependence; and 91–99 slight, dependence (Shah, Vanclay & Cooper 1989).
In this study, the inter-rater reliability coefficient (Kappa) for every item was more than 0.6; Inter-rater reliability of total BI was 0.998. In addition, the questionnaire reliability coefficient (internal consistency) was measured as 0.96-0.99 and item-total correlation confirmed its reliability, too. In Tagharrobi et al. study, its concurrent validity with Persian original BI was confirmed (r = 0.993, P < 0.0001) and the known-groups approach revealed its validity (P < 0.0001) (Tagharrobi, Sharifi & Sooky 2011).
Statistical Analyses
Statistical analyses were performed by IBM SPSS version 20.0 (IBM Corporation, Armonk, NY, USA). In this study, variables were analyzed using Student t test and ANOVA. Pearson coefficient correlation was used to examine the relationship between FES and BBS. A 2-tailed P < 0.05 was considered statistically significant.
3. Results
Demographic characteristics of the participants are presented in Table 1. A total of 200 elderly living in nursing homes with the mean (SD) age of 76.89(8.50) years (age range 60-93) were included in the study and remained until the end of the study. One hundred and three females and 97 male participated in the study. Fifty-nine participants were 70 years of age and 65 participants were 71-80 years of age. Nine percent of the participants were illiterate (84%) and 32% of them were living for more than 2 years in the nursing homes. As for marital status, 50.3% were widowed, 32.7% married, and 14.5% had no children. About 36% had good economic status. The most frequently reported medical condition among participants was cardiovascular (70 %) problems, followed by Type 2 diabetes mellitus (31.5%), and pulmonary diseases (11.5%). Twenty (39.2%) participants reported one fall in the previous 12 months (Table 1).
Sixty-nine percent reported high level of fear of falling. Only 3% were fully independent functionally (Table 2). The Pearson correlation coefficient between the fear of falling and the functional independence were -0.524, which showed a high correlation between them with the significance of P < 0.001 (Table 3).
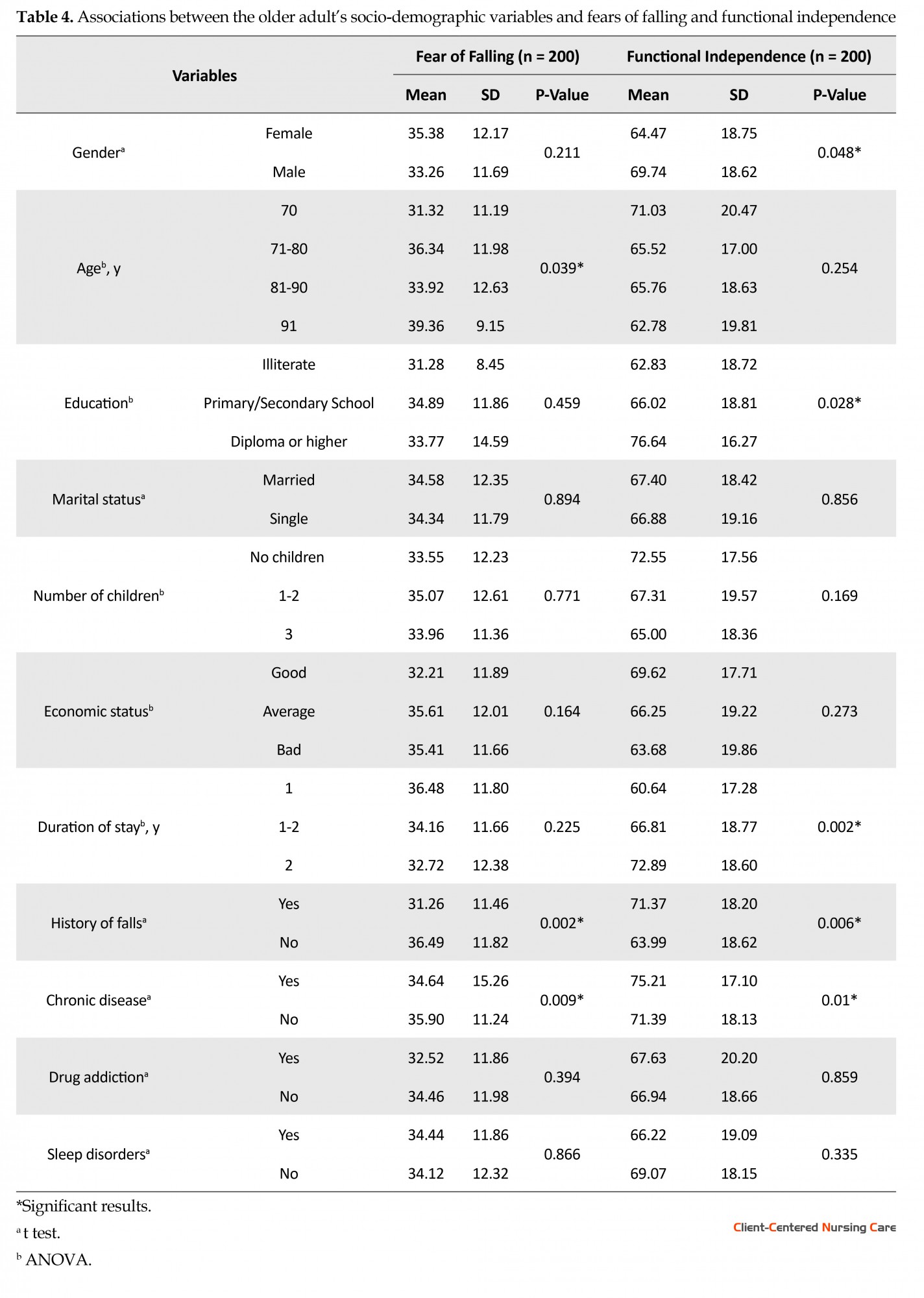
Factors associated with the fear of falling are shown in Table 4. In this study, fear of falling in the elderly living in nursing homes increased significantly with age (P = 0.039), history of falls (P = 0.002) and chronic diseases (P = 0.009). There was a significant association between functional independence and gender (P = 0.048), education (P = 0.028), duration of stay (P = 0.002), and chronic diseases (P = 0.01).
4. Discussion
Our objective was to study the impact of socio-demographic and health-related variables on fear of falling and functional independence in older persons. We identified two socio-demographic and one health-related factors which were significant correlates of fear of falling.
To date, only one group of risk factors such as gender, age, demographic status, and cognitive status were reported to be robustly associated with fear of falling (Guthrie et al., 2012). However, some new factors such as depression and anxiety, multiple drugs, and psychotropic drugs have been reported in different cohorts (Denkinger et al., 2015). Compared to previous studies, Kumar et al. reported that a wider range of factors are associated with fear of falling among community-dwelling elders. According to them, these variables are relatively easy to assess clinically and could be used to identify older people at a higher risk of fear of falling (Kumar et al., 2013). Choi et al. found characteristics which were independently associated with fear-induced activity restriction such as low socioeconomic status, cognitive impairment, difficulty with activities of daily living, and history of injurious falls (Choi & Ko 2015). Hanlon et al. in a study aimed to identify more socio-demographic falls risk factors. They found that educational level as an independent risk factor for any and multiple falls, and higher education and income were both associated with lower risk of falling (Hanlon et al., 2002). They have suggested that falls risk may be influenced more by a social determinant such as educational or income level than a biological determinant such as race (Tao & McRoy 2015).
Being a female is a risk factor for fear of falling among adults (Mahoney et al. 1965). The absence of association, in our study between gender and the fear of falling is inconsistent with other studies that have found links between gender and the fear of falling (Friedman et al., 2002; Lach 2005; Mann 200; Austin et al., 2007; Zijlstra et al., 2007), and in two longitudinal studies, in which women developed this fear more frequently than male adults (Mann 2006; Austin et al., 2007). The association between the history of falling and fear of falling is in agreement with the literature (Murphy, Williams & Gill 2002). However, Filiatrault et al. did not find a significant association between the fall history and the fear of falling (Filiatrault Desrosiers, & Trottier 2009). The association found in our study (after Pearson’s correlation coefficient analysis) between age and the fear of falling is inconsistent with other studies (Austin et al., 2007; Scheffer et al., 2008; Da Costa et al. 2012). However, Zijlstra et al., in a study among 504 adults aged 70 and older who reported fear of falling and fear-induced activity avoidance, observed an association between the increase in age and the fear of falling (Zijlstra et al., 2007).
In the literature, different instruments were used to measure fear of falling in the elderly. Firstly, some instruments measure fear of falling directly; these are mostly one-item instruments with a single question, such as how much fear of falling do you have? Secondly, they used instruments focusing on balance and fall-related self-efficacy, such as the falls-efficacy scales, of which several modifications have been developed. Other scales, such as the Activity-specific Balance Confidence (ABC) scale, are used but are less sensitive to change than the FES (Visschedijk et al., 2010; Mattos et al., 2014). Furthermore, FES is more suitable for use in vulnerable older persons than the ABC scale, which includes several more complex activities. Nowadays, the FES-I, which has been validated in Iran, is regarded as the most suitable instrument for community-dwelling older people. In conclusion, our study supports the use of the FES-I as an easy to apply instrument to measure fear of falling in nursing home living people.
In this study, we found that 41% of the nursing home living adults had high level of independence and 41% had moderate dependence. There were different reports about distribution of functional capacity in the older adults. For example, in a study conducted on 760 institutionalized Brazilian elders, Mattos et al., found Activities of Daily Living (ADL) dependence of 50.3% and ADL dependence of 81.2% using the Katz and Lawton scales (Araújo & Ceolim 2007). In another study, Araújo and Ceolim evaluated ADL dependence of elderly residents in long-term care institutions in Taubate, São Paulo, using the Katz and Lawton scales, and found that 63% of elderly people were dependent (Binkin et al. 2007). In addition, it was reported that France would be the European country with 28% dependence in the ADL in contrast to Ireland, with only 8% (Millán-Calenti J et al. 2010). In the United States, 34% of the older adults (≥65 y) were dependent on carrying out activities of daily living. This difference among studies for functional capacity in adults seems to be due to the socio-economic and cultural differences, as well as to the methodology used. Therefore, homogeneous criteria should be established to compare different populations.
With respect to functional independence, we identified 4 socio-demographic factors (gender, education, history of falling, and duration of stay) and one health-related factor (chronic disease), which were significant univariate correlates. This pattern is consistent with fear of falling in history of falling and chronic disease. Comparing with a study performed in the Brazil, which has used different study instruments (Araújo & Ceolim 2007), a high prevalence of functionally dependence was seen among elderly who had stayed at the institution for less than one year. With regard to the age, we did not find any association between age of elderly persons and functional capacity.
However, inconsistence with this result, several studies (Binkin et al. 2007; Millán-Calenti J et al. 2010), mostly Brazilian studies, have pointed out the association between higher dependence with older age among community-residing elderly population (Freitas et al., 2012). The results of this study showed that the probability of dependence was higher in female elderly. Similarly, an American study reported the percentage of independence of 56.1% for women and 77.7% for men.
Our research survey had some limitations, too. First, its cross-sectional nature does not allow conclusions of causality on the observed associations (e.g. between avoidance of activity and limitations in activity of daily living). Second, we included nursing home living older persons and excluded cognitive impaired persons, which can be considered as a heterogeneous and limited sample. Finally, in this study all measures were self-reported and none were performance-based measures. Therefore, future studies should measures other variables to enrich our understanding of the complex construct of fear of falling such as balance, gait, muscle strength, vision, etc.
In conclusion, there was a high association between fear of falling and functional independency in older adults. The fear of falling in the nursing home living older adults is associated with age, history of falling, and chronic disease. Moreover, there was a significant association between functional independence and variables of gender, education level, length of living in nursing home, history of falling, and chronic disease. The evaluation of this data contributes to establishing indicators and development of preventive strategies and specific interventions for the elderly with fear of falling.
Acknowledgments
This research was supported by Iran Medical Science University. The authors wish to thank the elderly who participated in this study. We would like to thank the staff members of the 25 nursing homes for providing the opportunity and impetus to perform this study.
Conflict of interest
The authors declared no Conflict of interests.
References
Allison, L. K., Painter, J. A., Emory, A., Whitehurst, P., & Raby, A. 2013. Participation restriction, not fear of falling, predicts actual balance and mobility abilities in rural community-dwelling older adults. Journal of Geriatric Physical Therapy, 36(1), pp. 13–23. doi: 10.1519/jpt.0b013e3182493d20
Anon. 2008. Self-reported falls and fall-related injuries among persons aged≥65 years—United States, 2006. JAMA, 299(14), pp. 1658. doi: 10.1001/jama.299.14.1658
Araújo, M. O. P. H., & Ceolim, M. F. 2007. Avaliação do grau de independência de idosos residentes em instituições de longa permanência. Revista da Escola de Enfermagem da USP, 41(3), pp. 378–85. doi: 10.1590/s0080-62342007000300006
Austin, N., Devine, A., Dick, I., Prince, R., & Bruce, D. 2007. Fear of falling in older women: A longitudinal study of incidence, persistence, and predictors. Journal of the American Geriatrics Society, 55(10), pp. 1598–603. doi: 10.1111/j.1532-5415.2007.01317.x
Bertera, E. M., & Bertera, R. L. 2008. Fear of falling and activity avoidance in a national sample of older adults in the United States. Health & Social Work, 33(1), pp. 54–62. doi: 10.1093/hsw/33.1.54
Binkin, N., Bertozzi, N., Bakken, E., & Vitali, P. 2007. Prevalence of and risk factors for functional dependence in the non-institutionalised elderly population of 11 Italian regions: Results of the Argento study, 2002. Ig Sanita Pubbl, 63(3):263-72. PMID: 17805352
Choi, K., & Ko, Y. 2015. Characteristics associated with fear of falling and activity restriction in South Korean older adults. Journal of Aging and Health, 27(6), pp. 1066–83. doi: 10.1177/0898264315573519
Dadgari, A., Hamid, T. A., Mousavi, S. A., Hakim, N., Hin, L. P. & Dadvar, L. 2016. Internal consistency of Persian version of falls efficacy scale and activity-specific balance scale. International Journal of Health Studies, 1(3), pp. 29-32.
Da Costa, E. M., Pepersack, T., Godin, I., Bantuelle, M., Petit, B., & Levêque, A. 2012. Fear of falling and associated activity restriction in older people: Results of a cross-sectional study conducted in a Belgian town. Archives of Public Health, 70(1). doi: 10.1186/0778-7367-70-1
Denkinger, M. D., Lukas, A., Nikolaus, T., & Hauer, K. 2015. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: A systematic review. The American Journal of Geriatric Psychiatry, 23(1), pp. 72–86. doi: 10.1016/j.jagp.2014.03.002
Filiatrault, J., Desrosiers, J., & Trottier, L. 2009. An exploratory study of individual and environmental correlates of fear of falling among community-dwelling seniors. Journal of Aging and Health, 21(6), pp. 881–94. doi: 10.1177/0898264309340694
Freitas, R. S., Fernandes, M. H., Coqueiro, R. Da, S., Reis Júnior, W. M., Rocha, S. V., & et al. 2012. Capacidade funcional e fatores associados em idosos: Estudo populacional. Acta Paulista de Enfermagem, 25(6), pp. 933–9. doi: 10.1590/s0103-21002012000600017
Friedman, S. M., Munoz, B., West, S. K., Rubin, G. S., & Fried, L. P. 2002. Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. Journal of the American Geriatrics Society, 50(8), pp. 1329–35. doi: 10.1046/j.1532-5415.2002.50352.x
Gill, T., Taylor, A. W., & Pengelly, A. 2005. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology, 51(5), pp. 340–5. doi: 10.1159/000086372
Guthrie, D. M., Fletcher, P. C., Berg, K., Williams, E., Boumans, N., & Hirdes, J. P. 2011. The role of medications in predicting activity restriction due to a fear of falling. Journal of Aging & Health, 24(2), pp. 269–86. doi: 10.1177/0898264311422598
Hanlon, J. T., Landerman, L. R., Fillenbaum, G. G., & Studenski, S. 2002. Falls in African American and white community-dwelling elderly residents. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 57(7), pp. 473–8. doi: 10.1093/gerona/57.7.m473
Kalula, S. Z, Ferreira, M., Swingler, G. H., & Badri, M. 2016. Risk factors for falls in older adults in a South African urban community. BMC Geriatrics, 16:51. doi: 10.1186/s12877-016-0212-7
Kumar, A., Carpenter, H., Morris, R., Iliffe, S., & Kendrick, D. 2013. Which factors are associated with fear of falling in community-dwelling older people. Age & Ageing, 43(1), pp. 76–84. doi: 10.1093/ageing/aft154
Kurella Tamura, M., Covinsky, K., Chertow, G., Yaffe, K., Landefeld, C., & Mc Culloch, C. 2009. Functional status of elderly adults before and after initiation of dialysis. New England Journal of Medicine, 361(16), pp. 1539–47. doi: 10.1056/nejmoa090465
Lach, H. W. 2005. Incidence and risk factors for developing fear of falling in older adults. Public Health Nursing, 22(1), pp. 45–52. doi: 10.1111/j.0737-1209.2005.22107.x
Mahoney, F. I., Barthel, D. W. 1965. Functional evaluation: The Barthel index. Maryland State Medical Journal, 14, pp. 61-65. PMID: 14258950
Mattos, I. E., Do Carmo, C. N., Santiago, L. M., & Luz, L. L. 2014. Factors associated with functional incapacity in elders living in long stay institutions in Brazil: A cross-sectional study. BMC Geriatrics, 14(1), pp. 47. doi: 10.1186/1471-2318-14-47
Mann, R. 2006. Exploring the relationship between fear of falling and neuroticism: A cross-sectional study in community-dwelling women over 70. Age & Ageing, 35(2), pp. 143–7. doi: 10.1093/ageing/afj013
Millán-Calenti, J. C., Tubío, J., Pita-Fernández, S., González-Abraldes, I., Lorenzo, T., Fernández-Arruty, T., et al. 2010. Prevalence of functional disability in activities of daily living, instrumental activities of daily living and associated factors, as predictors of morbidity and mortality. Archives of Gerontology and Geriatrics, 50(3), pp. 306–10. doi: 10.1016/j.archger.2009.04.017
Morris, M., Osborne, D., Hill, K., Kendig, H., Lundgren-Lindquist, B., Browning, C., et al. 2004. Predisposing factors for occasional and multiple falls in older Australians who live at home. Australian Journal of Physiotherapy, 50(3), pp. 153–9. doi: 10.1016/s0004-9514(14)60153-7
Mosallanezhad, Z., Salavati, M., Hellström, K., Reza Sotoudeh, G., Nilsson Wikmar, L., & Frändin, K. 2011. Cross-cultural adaptation, reliability and validity of the Persian version of the modified falls efficacy scale. Disability & Rehabilitation, 33(25-26), pp. 2446–53. doi: 10.3109/09638288.2011.574774
Murphy, S. L., Williams, C. S. & Gill, T. M. 2002. Characteristics associated with fear of falling and activity restriction in community-living older persons. Journal of the American Geriatrics Society, 50(3), pp. 516–20. doi: 10.1046/j.1532-5415.2002.50119.x
Orces, C. H. 2014. Prevalence and determinants of fall-related injuries among oder adults in Ecuador. Current Gerontology & Geriatrics Research, 2014, pp. 1–7. doi: 10.1155/2014/863473
Painter, J. A., Allison, L., Dhingra, P., Daughtery, J., Cogdill, K., & Trujillo, L. G. 2012. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. American Journal of Occupational Therapy, 66(2), pp. 169–76. doi: 10.5014/ajot.2012.002535
Shah, S., Vanclay, F., & Cooper, B. 1989. Improving the sensitivity of the barthel index for stroke rehabilitation. Journal of Clinical Epidemiology, 42(8), pp. 703–9. doi: 10.1016/0895-4356(89)90065-6
Scheffer, A. C., Schuurmans, M. J., Van Dijk, N., Vander Hooft, T., & De Rooij, S. E. 2007. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age & Ageing, 37(1), pp. 19–24. doi: 10.1093/ageing/afm169
Soriano, T. 2008. Falls in the community-dwelling older adult: A review for primary-care providers. Clinical Interventions in Aging, 2(4), pp. 545–53. doi: 10.2147/cia.s1080
Shumway-Cook, A., Brauer, S., & Woollacott, M. 2000. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical therapy, 80(9), pp. 896-903.
Tagharrobi, Z., Sharifi, K., & Sooky, Z. 2011. [Psychometric evaluation of Shah version of modified Barthel index in elderly people residing in Kashan Golabchi nursing home (Persian)]. Feyz Journals of Kashan University of Medical Sciences, 15(3).pp: 213-224.
Tao, H., & McRoy, S. 2015. Caring for and keeping the elderly in their homes. Chinese Nursing Research, 2(2-3), pp. 31–4. doi: 10.1016/j.cnre.2015.08.002
Tinetti, M. E., Richman, D., & Powell, L. 1990. Falls efficacy as a measure of fear of falling. Journal of Gerontology, 45(6), pp. 239–43. doi: 10.1093/geronj/45.6.p239
Vavilala, M., Curry, P., & Ramaiah, R. 2011. Current trends and update on injury prevention. International Journal of Critical Illness & Injury Science, 1(1), pp. 57-65. doi: 10.4103/2229-5151.79283
Visschedijk, J., Achterberg, W., Van Balen, R., & Hertogh, C. 2010. Fear of falling after hip fracture: A systematic review of measurement instruments, prevalence, interventions, and related factors. Journal of the American Geriatrics Society, 58(9), pp. 1739–48. doi: 10.1111/j.1532-5415.2010.03036.x
Yardley, L., & Smith, H. 2002. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. The Gerontologist, 42(1), pp. 17–23. doi: 10.1093/geront/42.1.17
Zijlstra, G. A. R., Van Haastregt, J. C. M., Van Eijk, J. T. M., Van Rossum, E., Stalenhoef, P. A., & Kempen, G. I. J. M. 2007. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age and Ageing, 36(3), pp. 304–9. doi: 10.1093/ageing/afm021
Our objective was to study the impact of socio-demographic and health-related variables on fear of falling and functional independence in older persons. We identified two socio-demographic and one health-related factors which were significant correlates of fear of falling.
To date, only one group of risk factors such as gender, age, demographic status, and cognitive status were reported to be robustly associated with fear of falling (Guthrie et al., 2012). However, some new factors such as depression and anxiety, multiple drugs, and psychotropic drugs have been reported in different cohorts (Denkinger et al., 2015). Compared to previous studies, Kumar et al. reported that a wider range of factors are associated with fear of falling among community-dwelling elders. According to them, these variables are relatively easy to assess clinically and could be used to identify older people at a higher risk of fear of falling (Kumar et al., 2013). Choi et al. found characteristics which were independently associated with fear-induced activity restriction such as low socioeconomic status, cognitive impairment, difficulty with activities of daily living, and history of injurious falls (Choi & Ko 2015). Hanlon et al. in a study aimed to identify more socio-demographic falls risk factors. They found that educational level as an independent risk factor for any and multiple falls, and higher education and income were both associated with lower risk of falling (Hanlon et al., 2002). They have suggested that falls risk may be influenced more by a social determinant such as educational or income level than a biological determinant such as race (Tao & McRoy 2015).
Being a female is a risk factor for fear of falling among adults (Mahoney et al. 1965). The absence of association, in our study between gender and the fear of falling is inconsistent with other studies that have found links between gender and the fear of falling (Friedman et al., 2002; Lach 2005; Mann 200; Austin et al., 2007; Zijlstra et al., 2007), and in two longitudinal studies, in which women developed this fear more frequently than male adults (Mann 2006; Austin et al., 2007). The association between the history of falling and fear of falling is in agreement with the literature (Murphy, Williams & Gill 2002). However, Filiatrault et al. did not find a significant association between the fall history and the fear of falling (Filiatrault Desrosiers, & Trottier 2009). The association found in our study (after Pearson’s correlation coefficient analysis) between age and the fear of falling is inconsistent with other studies (Austin et al., 2007; Scheffer et al., 2008; Da Costa et al. 2012). However, Zijlstra et al., in a study among 504 adults aged 70 and older who reported fear of falling and fear-induced activity avoidance, observed an association between the increase in age and the fear of falling (Zijlstra et al., 2007).
In the literature, different instruments were used to measure fear of falling in the elderly. Firstly, some instruments measure fear of falling directly; these are mostly one-item instruments with a single question, such as how much fear of falling do you have? Secondly, they used instruments focusing on balance and fall-related self-efficacy, such as the falls-efficacy scales, of which several modifications have been developed. Other scales, such as the Activity-specific Balance Confidence (ABC) scale, are used but are less sensitive to change than the FES (Visschedijk et al., 2010; Mattos et al., 2014). Furthermore, FES is more suitable for use in vulnerable older persons than the ABC scale, which includes several more complex activities. Nowadays, the FES-I, which has been validated in Iran, is regarded as the most suitable instrument for community-dwelling older people. In conclusion, our study supports the use of the FES-I as an easy to apply instrument to measure fear of falling in nursing home living people.
In this study, we found that 41% of the nursing home living adults had high level of independence and 41% had moderate dependence. There were different reports about distribution of functional capacity in the older adults. For example, in a study conducted on 760 institutionalized Brazilian elders, Mattos et al., found Activities of Daily Living (ADL) dependence of 50.3% and ADL dependence of 81.2% using the Katz and Lawton scales (Araújo & Ceolim 2007). In another study, Araújo and Ceolim evaluated ADL dependence of elderly residents in long-term care institutions in Taubate, São Paulo, using the Katz and Lawton scales, and found that 63% of elderly people were dependent (Binkin et al. 2007). In addition, it was reported that France would be the European country with 28% dependence in the ADL in contrast to Ireland, with only 8% (Millán-Calenti J et al. 2010). In the United States, 34% of the older adults (≥65 y) were dependent on carrying out activities of daily living. This difference among studies for functional capacity in adults seems to be due to the socio-economic and cultural differences, as well as to the methodology used. Therefore, homogeneous criteria should be established to compare different populations.
With respect to functional independence, we identified 4 socio-demographic factors (gender, education, history of falling, and duration of stay) and one health-related factor (chronic disease), which were significant univariate correlates. This pattern is consistent with fear of falling in history of falling and chronic disease. Comparing with a study performed in the Brazil, which has used different study instruments (Araújo & Ceolim 2007), a high prevalence of functionally dependence was seen among elderly who had stayed at the institution for less than one year. With regard to the age, we did not find any association between age of elderly persons and functional capacity.
However, inconsistence with this result, several studies (Binkin et al. 2007; Millán-Calenti J et al. 2010), mostly Brazilian studies, have pointed out the association between higher dependence with older age among community-residing elderly population (Freitas et al., 2012). The results of this study showed that the probability of dependence was higher in female elderly. Similarly, an American study reported the percentage of independence of 56.1% for women and 77.7% for men.
Our research survey had some limitations, too. First, its cross-sectional nature does not allow conclusions of causality on the observed associations (e.g. between avoidance of activity and limitations in activity of daily living). Second, we included nursing home living older persons and excluded cognitive impaired persons, which can be considered as a heterogeneous and limited sample. Finally, in this study all measures were self-reported and none were performance-based measures. Therefore, future studies should measures other variables to enrich our understanding of the complex construct of fear of falling such as balance, gait, muscle strength, vision, etc.
In conclusion, there was a high association between fear of falling and functional independency in older adults. The fear of falling in the nursing home living older adults is associated with age, history of falling, and chronic disease. Moreover, there was a significant association between functional independence and variables of gender, education level, length of living in nursing home, history of falling, and chronic disease. The evaluation of this data contributes to establishing indicators and development of preventive strategies and specific interventions for the elderly with fear of falling.
Acknowledgments
This research was supported by Iran Medical Science University. The authors wish to thank the elderly who participated in this study. We would like to thank the staff members of the 25 nursing homes for providing the opportunity and impetus to perform this study.
Conflict of interest
The authors declared no Conflict of interests.
References
Allison, L. K., Painter, J. A., Emory, A., Whitehurst, P., & Raby, A. 2013. Participation restriction, not fear of falling, predicts actual balance and mobility abilities in rural community-dwelling older adults. Journal of Geriatric Physical Therapy, 36(1), pp. 13–23. doi: 10.1519/jpt.0b013e3182493d20
Anon. 2008. Self-reported falls and fall-related injuries among persons aged≥65 years—United States, 2006. JAMA, 299(14), pp. 1658. doi: 10.1001/jama.299.14.1658
Araújo, M. O. P. H., & Ceolim, M. F. 2007. Avaliação do grau de independência de idosos residentes em instituições de longa permanência. Revista da Escola de Enfermagem da USP, 41(3), pp. 378–85. doi: 10.1590/s0080-62342007000300006
Austin, N., Devine, A., Dick, I., Prince, R., & Bruce, D. 2007. Fear of falling in older women: A longitudinal study of incidence, persistence, and predictors. Journal of the American Geriatrics Society, 55(10), pp. 1598–603. doi: 10.1111/j.1532-5415.2007.01317.x
Bertera, E. M., & Bertera, R. L. 2008. Fear of falling and activity avoidance in a national sample of older adults in the United States. Health & Social Work, 33(1), pp. 54–62. doi: 10.1093/hsw/33.1.54
Binkin, N., Bertozzi, N., Bakken, E., & Vitali, P. 2007. Prevalence of and risk factors for functional dependence in the non-institutionalised elderly population of 11 Italian regions: Results of the Argento study, 2002. Ig Sanita Pubbl, 63(3):263-72. PMID: 17805352
Choi, K., & Ko, Y. 2015. Characteristics associated with fear of falling and activity restriction in South Korean older adults. Journal of Aging and Health, 27(6), pp. 1066–83. doi: 10.1177/0898264315573519
Dadgari, A., Hamid, T. A., Mousavi, S. A., Hakim, N., Hin, L. P. & Dadvar, L. 2016. Internal consistency of Persian version of falls efficacy scale and activity-specific balance scale. International Journal of Health Studies, 1(3), pp. 29-32.
Da Costa, E. M., Pepersack, T., Godin, I., Bantuelle, M., Petit, B., & Levêque, A. 2012. Fear of falling and associated activity restriction in older people: Results of a cross-sectional study conducted in a Belgian town. Archives of Public Health, 70(1). doi: 10.1186/0778-7367-70-1
Denkinger, M. D., Lukas, A., Nikolaus, T., & Hauer, K. 2015. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: A systematic review. The American Journal of Geriatric Psychiatry, 23(1), pp. 72–86. doi: 10.1016/j.jagp.2014.03.002
Filiatrault, J., Desrosiers, J., & Trottier, L. 2009. An exploratory study of individual and environmental correlates of fear of falling among community-dwelling seniors. Journal of Aging and Health, 21(6), pp. 881–94. doi: 10.1177/0898264309340694
Freitas, R. S., Fernandes, M. H., Coqueiro, R. Da, S., Reis Júnior, W. M., Rocha, S. V., & et al. 2012. Capacidade funcional e fatores associados em idosos: Estudo populacional. Acta Paulista de Enfermagem, 25(6), pp. 933–9. doi: 10.1590/s0103-21002012000600017
Friedman, S. M., Munoz, B., West, S. K., Rubin, G. S., & Fried, L. P. 2002. Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. Journal of the American Geriatrics Society, 50(8), pp. 1329–35. doi: 10.1046/j.1532-5415.2002.50352.x
Gill, T., Taylor, A. W., & Pengelly, A. 2005. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology, 51(5), pp. 340–5. doi: 10.1159/000086372
Guthrie, D. M., Fletcher, P. C., Berg, K., Williams, E., Boumans, N., & Hirdes, J. P. 2011. The role of medications in predicting activity restriction due to a fear of falling. Journal of Aging & Health, 24(2), pp. 269–86. doi: 10.1177/0898264311422598
Hanlon, J. T., Landerman, L. R., Fillenbaum, G. G., & Studenski, S. 2002. Falls in African American and white community-dwelling elderly residents. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 57(7), pp. 473–8. doi: 10.1093/gerona/57.7.m473
Kalula, S. Z, Ferreira, M., Swingler, G. H., & Badri, M. 2016. Risk factors for falls in older adults in a South African urban community. BMC Geriatrics, 16:51. doi: 10.1186/s12877-016-0212-7
Kumar, A., Carpenter, H., Morris, R., Iliffe, S., & Kendrick, D. 2013. Which factors are associated with fear of falling in community-dwelling older people. Age & Ageing, 43(1), pp. 76–84. doi: 10.1093/ageing/aft154
Kurella Tamura, M., Covinsky, K., Chertow, G., Yaffe, K., Landefeld, C., & Mc Culloch, C. 2009. Functional status of elderly adults before and after initiation of dialysis. New England Journal of Medicine, 361(16), pp. 1539–47. doi: 10.1056/nejmoa090465
Lach, H. W. 2005. Incidence and risk factors for developing fear of falling in older adults. Public Health Nursing, 22(1), pp. 45–52. doi: 10.1111/j.0737-1209.2005.22107.x
Mahoney, F. I., Barthel, D. W. 1965. Functional evaluation: The Barthel index. Maryland State Medical Journal, 14, pp. 61-65. PMID: 14258950
Mattos, I. E., Do Carmo, C. N., Santiago, L. M., & Luz, L. L. 2014. Factors associated with functional incapacity in elders living in long stay institutions in Brazil: A cross-sectional study. BMC Geriatrics, 14(1), pp. 47. doi: 10.1186/1471-2318-14-47
Mann, R. 2006. Exploring the relationship between fear of falling and neuroticism: A cross-sectional study in community-dwelling women over 70. Age & Ageing, 35(2), pp. 143–7. doi: 10.1093/ageing/afj013
Millán-Calenti, J. C., Tubío, J., Pita-Fernández, S., González-Abraldes, I., Lorenzo, T., Fernández-Arruty, T., et al. 2010. Prevalence of functional disability in activities of daily living, instrumental activities of daily living and associated factors, as predictors of morbidity and mortality. Archives of Gerontology and Geriatrics, 50(3), pp. 306–10. doi: 10.1016/j.archger.2009.04.017
Morris, M., Osborne, D., Hill, K., Kendig, H., Lundgren-Lindquist, B., Browning, C., et al. 2004. Predisposing factors for occasional and multiple falls in older Australians who live at home. Australian Journal of Physiotherapy, 50(3), pp. 153–9. doi: 10.1016/s0004-9514(14)60153-7
Mosallanezhad, Z., Salavati, M., Hellström, K., Reza Sotoudeh, G., Nilsson Wikmar, L., & Frändin, K. 2011. Cross-cultural adaptation, reliability and validity of the Persian version of the modified falls efficacy scale. Disability & Rehabilitation, 33(25-26), pp. 2446–53. doi: 10.3109/09638288.2011.574774
Murphy, S. L., Williams, C. S. & Gill, T. M. 2002. Characteristics associated with fear of falling and activity restriction in community-living older persons. Journal of the American Geriatrics Society, 50(3), pp. 516–20. doi: 10.1046/j.1532-5415.2002.50119.x
Orces, C. H. 2014. Prevalence and determinants of fall-related injuries among oder adults in Ecuador. Current Gerontology & Geriatrics Research, 2014, pp. 1–7. doi: 10.1155/2014/863473
Painter, J. A., Allison, L., Dhingra, P., Daughtery, J., Cogdill, K., & Trujillo, L. G. 2012. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. American Journal of Occupational Therapy, 66(2), pp. 169–76. doi: 10.5014/ajot.2012.002535
Shah, S., Vanclay, F., & Cooper, B. 1989. Improving the sensitivity of the barthel index for stroke rehabilitation. Journal of Clinical Epidemiology, 42(8), pp. 703–9. doi: 10.1016/0895-4356(89)90065-6
Scheffer, A. C., Schuurmans, M. J., Van Dijk, N., Vander Hooft, T., & De Rooij, S. E. 2007. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age & Ageing, 37(1), pp. 19–24. doi: 10.1093/ageing/afm169
Soriano, T. 2008. Falls in the community-dwelling older adult: A review for primary-care providers. Clinical Interventions in Aging, 2(4), pp. 545–53. doi: 10.2147/cia.s1080
Shumway-Cook, A., Brauer, S., & Woollacott, M. 2000. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical therapy, 80(9), pp. 896-903.
Tagharrobi, Z., Sharifi, K., & Sooky, Z. 2011. [Psychometric evaluation of Shah version of modified Barthel index in elderly people residing in Kashan Golabchi nursing home (Persian)]. Feyz Journals of Kashan University of Medical Sciences, 15(3).pp: 213-224.
Tao, H., & McRoy, S. 2015. Caring for and keeping the elderly in their homes. Chinese Nursing Research, 2(2-3), pp. 31–4. doi: 10.1016/j.cnre.2015.08.002
Tinetti, M. E., Richman, D., & Powell, L. 1990. Falls efficacy as a measure of fear of falling. Journal of Gerontology, 45(6), pp. 239–43. doi: 10.1093/geronj/45.6.p239
Vavilala, M., Curry, P., & Ramaiah, R. 2011. Current trends and update on injury prevention. International Journal of Critical Illness & Injury Science, 1(1), pp. 57-65. doi: 10.4103/2229-5151.79283
Visschedijk, J., Achterberg, W., Van Balen, R., & Hertogh, C. 2010. Fear of falling after hip fracture: A systematic review of measurement instruments, prevalence, interventions, and related factors. Journal of the American Geriatrics Society, 58(9), pp. 1739–48. doi: 10.1111/j.1532-5415.2010.03036.x
Yardley, L., & Smith, H. 2002. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. The Gerontologist, 42(1), pp. 17–23. doi: 10.1093/geront/42.1.17
Zijlstra, G. A. R., Van Haastregt, J. C. M., Van Eijk, J. T. M., Van Rossum, E., Stalenhoef, P. A., & Kempen, G. I. J. M. 2007. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age and Ageing, 36(3), pp. 304–9. doi: 10.1093/ageing/afm021
Type of Study: Research |
Subject:
General
Received: 2016/07/17 | Accepted: 2016/09/19 | Published: 2016/12/25
Received: 2016/07/17 | Accepted: 2016/09/19 | Published: 2016/12/25
References
1. Allison, L. K., Painter, J. A., Emory, A., Whitehurst, P., & Raby, A. 2013. Participation restriction, not fear of falling, predicts actual balance and mobility abilities in rural community-dwelling older adults. Journal of Geriatric Physical Therapy, 36(1), pp. 13–23. doi: 10.1519/jpt.0b013e3182493d20 [DOI:10.1519/JPT.0b013e3182493d20]
2. Anon. 2008. Self-reported falls and fall-related injuries among persons aged≥65 years—United States, 2006. JAMA, 299(14), pp. 1658. doi: 10.1001/jama.299.14.1658 [DOI:10.1001/jama.299.14.1658]
3. Araújo, M. O. P. H., & Ceolim, M. F. 2007. Avaliação do grau de independência de idosos residentes em instituições de longa permanência. Revista da Escola de Enfermagem da USP, 41(3), pp. 378–85. doi: 10.1590/s0080-62342007000300006 [DOI:10.1590/S0080-62342007000300006]
4. Austin, N., Devine, A., Dick, I., Prince, R., & Bruce, D. 2007. Fear of falling in older women: A longitudinal study of incidence, persistence, and predictors. Journal of the American Geriatrics Society, 55(10), pp. 1598–603. doi: 10.1111/j.1532-5415.2007.01317.x [DOI:10.1111/j.1532-5415.2007.01317.x]
5. Bertera, E. M., & Bertera, R. L. 2008. Fear of falling and activity avoidance in a national sample of older adults in the United States. Health & Social Work, 33(1), pp. 54–62. doi: 10.1093/hsw/33.1.54 [DOI:10.1093/hsw/33.1.54]
6. Binkin, N., Bertozzi, N., Bakken, E., & Vitali, P. 2007. Prevalence of and risk factors for functional dependence in the non-institutionalised elderly population of 11 Italian regions: Results of the Argento study, 2002. Ig Sanita Pubbl, 63(3):263-72. PMID: 17805352 [PMID]
7. Choi, K., & Ko, Y. 2015. Characteristics associated with fear of falling and activity restriction in South Korean older adults. Journal of Aging and Health, 27(6), pp. 1066–83. doi: 10.1177/0898264315573519 [DOI:10.1177/0898264315573519]
8. Dadgari, A., Hamid, T. A., Mousavi, S. A., Hakim, N., Hin, L. P. & Dadvar, L. 2016. Internal consistency of Persian version of falls efficacy scale and activity-specific balance scale. International Journal of Health Studies, 1(3), pp. 29-32.
9. Da Costa, E. M., Pepersack, T., Godin, I., Bantuelle, M., Petit, B., & Levêque, A. 2012. Fear of falling and associated activity restriction in older people: Results of a cross-sectional study conducted in a Belgian town. Archives of Public Health, 70(1). doi: 10.1186/0778-7367-70-1 [DOI:10.1186/0778-7367-70-1]
10. Denkinger, M. D., Lukas, A., Nikolaus, T., & Hauer, K. 2015. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: A systematic review. The American Journal of Geriatric Psychiatry, 23(1), pp. 72–86. doi: 10.1016/j.jagp.2014.03.002 [DOI:10.1016/j.jagp.2014.03.002]
11. Filiatrault, J., Desrosiers, J., & Trottier, L. 2009. An exploratory study of individual and environmental correlates of fear of falling among community-dwelling seniors. Journal of Aging and Health, 21(6), pp. 881–94. doi: 10.1177/0898264309340694 [DOI:10.1177/0898264309340694]
12. Freitas, R. S., Fernandes, M. H., Coqueiro, R. Da, S., Reis Júnior, W. M., Rocha, S. V., & et al. 2012. Capacidade funcional e fatores associados em idosos: Estudo populacional. Acta Paulista de Enfermagem, 25(6), pp. 933–9. doi: 10.1590/s0103-21002012000600017 [DOI:10.1590/S0103-21002012000600017]
13. Friedman, S. M., Munoz, B., West, S. K., Rubin, G. S., & Fried, L. P. 2002. Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. Journal of the American Geriatrics Society, 50(8), pp. 1329–35. doi: 10.1046/j.1532-5415.2002.50352.x [DOI:10.1046/j.1532-5415.2002.50352.x]
14. Gill, T., Taylor, A. W., & Pengelly, A. 2005. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology, 51(5), pp. 340–5. doi: 10.1159/000086372 [DOI:10.1159/000086372]
15. Guthrie, D. M., Fletcher, P. C., Berg, K., Williams, E., Boumans, N., & Hirdes, J. P. 2011. The role of medications in predicting activity restriction due to a fear of falling. Journal of Aging & Health, 24(2), pp. 269–86. doi: 10.1177/0898264311422598 [DOI:10.1177/0898264311422598]
16. Hanlon, J. T., Landerman, L. R., Fillenbaum, G. G., & Studenski, S. 2002. Falls in African American and white community-dwelling elderly residents. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 57(7), pp. 473–8. doi: 10.1093/gerona/57.7.m473 [DOI:10.1093/gerona/57.7.M473]
17. Kalula, S. Z, Ferreira, M., Swingler, G. H., & Badri, M. 2016. Risk factors for falls in older adults in a South African urban community. BMC Geriatrics, 16:51. doi: 10.1186/s12877-016-0212-7 [DOI:10.1186/s12877-016-0212-7]
18. Kumar, A., Carpenter, H., Morris, R., Iliffe, S., & Kendrick, D. 2013. Which factors are associated with fear of falling in community-dwelling older people. Age & Ageing, 43(1), pp. 76–84. doi: 10.1093/ageing/aft154 [DOI:10.1093/ageing/aft154]
19. Kurella Tamura, M., Covinsky, K., Chertow, G., Yaffe, K., Landefeld, C., & Mc Culloch, C. 2009. Functional status of elderly adults before and after initiation of dialysis. New England Journal of Medicine, 361(16), pp. 1539–47. doi: 10.1056/nejmoa090465
20. Lach, H. W. 2005. Incidence and risk factors for developing fear of falling in older adults. Public Health Nursing, 22(1), pp. 45–52. doi: 10.1111/j.0737-1209.2005.22107.x [DOI:10.1111/j.0737-1209.2005.22107.x]
21. Mahoney, F. I., Barthel, D. W. 1965. Functional evaluation: The Barthel index. Maryland State Medical Journal, 14, pp. 61-65. PMID: 14258950 [PMID]
22. Mattos, I. E., Do Carmo, C. N., Santiago, L. M., & Luz, L. L. 2014. Factors associated with functional incapacity in elders living in long stay institutions in Brazil: A cross-sectional study. BMC Geriatrics, 14(1), pp. 47. doi: 10.1186/1471-2318-14-47 [DOI:10.1186/1471-2318-14-47]
23. Mann, R. 2006. Exploring the relationship between fear of falling and neuroticism: A cross-sectional study in community-dwelling women over 70. Age & Ageing, 35(2), pp. 143–7. doi: 10.1093/ageing/afj013 [DOI:10.1093/ageing/afj013]
24. Millán-Calenti, J. C., Tubío, J., Pita-Fernández, S., González-Abraldes, I., Lorenzo, T., Fernández-Arruty, T., et al. 2010. Prevalence of functional disability in activities of daily living, instrumental activities of daily living and associated factors, as predictors of morbidity and mortality. Archives of Gerontology and Geriatrics, 50(3), pp. 306–10. doi: 10.1016/j.archger.2009.04.017 [DOI:10.1016/j.archger.2009.04.017]
25. Morris, M., Osborne, D., Hill, K., Kendig, H., Lundgren-Lindquist, B., Browning, C., et al. 2004. Predisposing factors for occasional and multiple falls in older Australians who live at home. Australian Journal of Physiotherapy, 50(3), pp. 153–9. doi: 10.1016/s0004-9514(14)60153-7 [DOI:10.1016/S0004-9514(14)60153-7]
26. Mosallanezhad, Z., Salavati, M., Hellström, K., Reza Sotoudeh, G., Nilsson Wikmar, L., & Frändin, K. 2011. Cross-cultural adaptation, reliability and validity of the Persian version of the modified falls efficacy scale. Disability & Rehabilitation, 33(25-26), pp. 2446–53. doi: 10.3109/09638288.2011.574774 [DOI:10.3109/09638288.2011.574774]
27. Murphy, S. L., Williams, C. S. & Gill, T. M. 2002. Characteristics associated with fear of falling and activity restriction in community-living older persons. Journal of the American Geriatrics Society, 50(3), pp. 516–20. doi: 10.1046/j.1532-5415.2002.50119.x [DOI:10.1046/j.1532-5415.2002.50119.x]
28. Orces, C. H. 2014. Prevalence and determinants of fall-related injuries among oder adults in Ecuador. Current Gerontology & Geriatrics Research, 2014, pp. 1–7. doi: 10.1155/2014/863473 [DOI:10.1155/2014/863473]
29. Painter, J. A., Allison, L., Dhingra, P., Daughtery, J., Cogdill, K., & Trujillo, L. G. 2012. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. American Journal of Occupational Therapy, 66(2), pp. 169–76. doi: 10.5014/ajot.2012.002535 [DOI:10.5014/ajot.2012.002535]
30. Shah, S., Vanclay, F., & Cooper, B. 1989. Improving the sensitivity of the barthel index for stroke rehabilitation. Journal of Clinical Epidemiology, 42(8), pp. 703–9. doi: 10.1016/0895-4356(89)90065-6 [DOI:10.1016/0895-4356(89)90065-6]
31. Scheffer, A. C., Schuurmans, M. J., Van Dijk, N., Vander Hooft, T., & De Rooij, S. E. 2007. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age & Ageing, 37(1), pp. 19–24. doi: 10.1093/ageing/afm169 [DOI:10.1093/ageing/afm169]
32. Soriano, T. 2008. Falls in the community-dwelling older adult: A review for primary-care providers. Clinical Interventions in Aging, 2(4), pp. 545–53. doi: 10.2147/cia.s1080 [DOI:10.2147/CIA.S1080]
33. Shumway-Cook, A., Brauer, S., & Woollacott, M. 2000. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical therapy, 80(9), pp. 896-903. [PMID]
34. Tagharrobi, Z., Sharifi, K., & Sooky, Z. 2011. [Psychometric evaluation of Shah version of modified Barthel index in elderly people residing in Kashan Golabchi nursing home (Persian)]. Feyz Journals of Kashan University of Medical Sciences, 15(3).pp: 213-224.
35. Tao, H., & McRoy, S. 2015. Caring for and keeping the elderly in their homes. Chinese Nursing Research, 2(2-3), pp. 31–4. doi: 10.1016/j.cnre.2015.08.002 [DOI:10.1016/j.cnre.2015.08.002]
36. Tinetti, M. E., Richman, D., & Powell, L. 1990. Falls efficacy as a measure of fear of falling. Journal of Gerontology, 45(6), pp. 239–43. doi: 10.1093/geronj/45.6.p239 [DOI:10.1093/geronj/45.6.P239]
37. Vavilala, M., Curry, P., & Ramaiah, R. 2011. Current trends and update on injury prevention. International Journal of Critical Illness & Injury Science, 1(1), pp. 57-65. doi: 10.4103/2229-5151.79283 [DOI:10.4103/2229-5151.79283]
38. Visschedijk, J., Achterberg, W., Van Balen, R., & Hertogh, C. 2010. Fear of falling after hip fracture: A systematic review of measurement instruments, prevalence, interventions, and related factors. Journal of the American Geriatrics Society, 58(9), pp. 1739–48. doi: 10.1111/j.1532-5415.2010.03036.x [DOI:10.1111/j.1532-5415.2010.03036.x]
39. Yardley, L., & Smith, H. 2002. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. The Gerontologist, 42(1), pp. 17–23. doi: 10.1093/geront/42.1.17 [DOI:10.1093/geront/42.1.17]
40. Zijlstra, G. A. R., Van Haastregt, J. C. M., Van Eijk, J. T. M., Van Rossum, E., Stalenhoef, P. A., & Kempen, G. I. J. M. 2007. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age and Ageing, 36(3), pp. 304–9. doi: 10.1093/ageing/afm021 [DOI:10.1093/ageing/afm021]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |