Sun, Jul 6, 2025
[Archive]
Volume 3, Issue 2 (Spring 2017 -- 2017)
JCCNC 2017, 3(2): 119-124 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azimi Jahed N, Borimnejad L, Haghani H. Effect of Body Position on Physiological Alteration While Feeding Infants: A Systematic Review. JCCNC 2017; 3 (2) :119-124
URL: http://jccnc.iums.ac.ir/article-1-103-en.html
URL: http://jccnc.iums.ac.ir/article-1-103-en.html
1- Department of Neonatal Intensive Care Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Nursing Care Research Center, Iran University of Medical Sciences, Tehran, Iran. ,l.borimnejad@gmail.com
3- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
2- Nursing Care Research Center, Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 563 kb]
(3985 Downloads)
| Abstract (HTML) (4669 Views)
Full-Text: (1536 Views)
1. Background
According to WHO, one in every ten infants are born prematurely all over the world with a gradual increase in the number nowadays (World Health Organization 2012; World Health Organization 2014). Of all, low birth weight infants are at greater risk. It is, therefore, necessary to pay more attention to their feeding position to monitor their growth in a better way (World Health Organization 2016).Generally, an infant should be able to coordinate sucking, swallowing, and breathing to have a safe and effective feeding, which is developed with the increasing gestational age. Any problem in each of these functions can lead to the risk of aspiration, pneumonia, decreased oxygenation saturation, apnea, and bradycardia (Sabrina Lopes et al. 2014; Clark et al. 2007). Coordination of sucking and swallowing occurs when the infant shows no symptoms of aspiration, decreased oxygenation saturation, apnea, or bradycardia in the proportion of 1:1:1 or 2:2:1 for sucking: swallowing: breathing, respectively (Barlow 2009). According to Gewolb and Vice, there are 9 patterns of breathing and swallowing. The pattern 5 (apnea-swallow-apnea) is a dominant pattern for premature infants of 32-34 weeks post-menstrual age, which changes to pattern 7 (inhale-swallow-exhale) after maturation (Park 2012).
A termed infant is capable of sucking and breathing simultaneously. While sucking, breathing is interrupted for a short while oxygen saturation (SpO2) is still high. But, it is less in bottle feeding compared to breast feeding because milk comes in variable flow from breast and compressibility is less (Sakalidis et al. 2012). Feeding problems of preterm infants have been reported in lots of studies including those with increased physiological instability, weak sucking pattern, low coordination between sucking and swallowing, insufficient absorption, and increased duration to complete the oral intake (Park et al. 2014).
Nutritional support, which includes even the tracing of the minimum drop in oxygen during feeding, is one of the major aspects of care for those who take care of the preterm infants. It is also believed that sufficient oxygenation helps in maintaining the body tune; oral - move control; coordination of sucking, swallowing, and breathing during feeding. Infants with more oxygen drop during their feeding, make a less effort for sucking as a result of which it takes a long time to attain the complete oral feeding (Thoyre & Carlson 2003a). In response to the increased impact of breathing, cardiac output of supplying blood, oxygen, and adequate food increases during feeding. In the heart of a mature person, cardiac contractility increases to enhance cardiac output, but in the preterm heart it causes more impulses. Therefore, the heart rate can be a good indication of physiological function to maintain an infant’s stability (Park 2012).
Following the improvements in the care of infants, it resulted in the promotion of the survival of premature infants with more attention towards the importance of feeding strategies (Clark et al. 2007). Positioning is a simple strategy that is applicable while taking care of the infants. There are no definite guidelines for health care providers, according to the prior clinical evidences, about the infant’s position during feeding (Park 2012). There is, therefore, a review of the impact of positioning during bottle feeding infants over their physiological stability in order to determine a better position in feeding infants to help in their growth in a non-invasive manner.
2. Materials and Methods
All published articles based on randomized and quasi-randomized clinical trial, and also crossover studies with proper conditions were included in this study through an electronic search. Databases such as Scopus, Ovid, Science Direct, ProQuest, Pub Med, Wiley Cochrane Library, Magiran, Medlib, SID, and Google Scholar were referred. English keywords, i.e., position nutrition newborn from 1997 to 2016, and Persian keywords including Vaz’iyat-e qarar-giri (position) Taqzia (nutrition) Nowzad (newborn) from 2010 to 2016 were searched. At the first step, each article was scanned and then selected for analysis after meeting all the required criteria. The quality of previous studies was decided by using the Cochran bias search tool.
3. Results
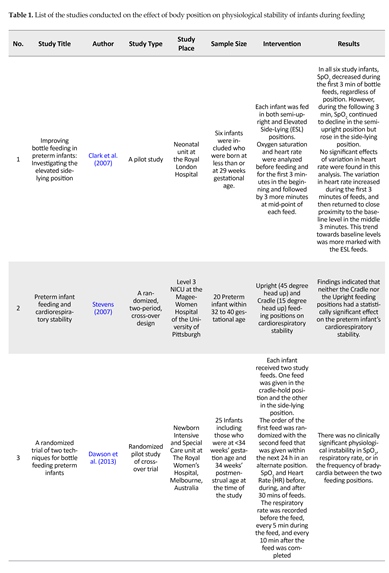
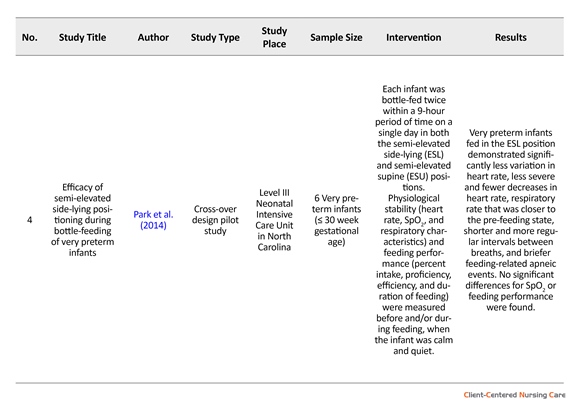
Total 4 clinical trials with crossover eligible criteria were selected to study the impact of the positioning of preterm infants while bottle feeding (N = 57) (Clark et al. 2007) (N = 6); Stevens (2007) (N = 20); Dawson et al. (2013) (N = 25); and Park et al. 2014(N = 6). There was no Persian study in this concern. All four crossover studies reviewed the impact of different positions on physiological parameters during bottle feeding, as mentioned in Table 1.
Clark et al. 2007 in their review of elevated side-lying vs. semi-upright showed that there is no significant statistical difference between two positions, but the heart rate increased in the first 3 minutes of feeding and returned to the normal state in the mid 3 minutes, and thus, the elevated side-lying position was more preferred. There was a significant interaction between nutrition and feeding positions, with the decreased rate of SpO2 during the first 3 minutes of feeding in both the positions, which later increased to mid 3 minutes in the elevated side-lying position while decreased in the semi-upright position.
Stevens (2007) indicated there is no significant difference in feeding in an upright position (head and body in
According to WHO, one in every ten infants are born prematurely all over the world with a gradual increase in the number nowadays (World Health Organization 2012; World Health Organization 2014). Of all, low birth weight infants are at greater risk. It is, therefore, necessary to pay more attention to their feeding position to monitor their growth in a better way (World Health Organization 2016).Generally, an infant should be able to coordinate sucking, swallowing, and breathing to have a safe and effective feeding, which is developed with the increasing gestational age. Any problem in each of these functions can lead to the risk of aspiration, pneumonia, decreased oxygenation saturation, apnea, and bradycardia (Sabrina Lopes et al. 2014; Clark et al. 2007). Coordination of sucking and swallowing occurs when the infant shows no symptoms of aspiration, decreased oxygenation saturation, apnea, or bradycardia in the proportion of 1:1:1 or 2:2:1 for sucking: swallowing: breathing, respectively (Barlow 2009). According to Gewolb and Vice, there are 9 patterns of breathing and swallowing. The pattern 5 (apnea-swallow-apnea) is a dominant pattern for premature infants of 32-34 weeks post-menstrual age, which changes to pattern 7 (inhale-swallow-exhale) after maturation (Park 2012).
A termed infant is capable of sucking and breathing simultaneously. While sucking, breathing is interrupted for a short while oxygen saturation (SpO2) is still high. But, it is less in bottle feeding compared to breast feeding because milk comes in variable flow from breast and compressibility is less (Sakalidis et al. 2012). Feeding problems of preterm infants have been reported in lots of studies including those with increased physiological instability, weak sucking pattern, low coordination between sucking and swallowing, insufficient absorption, and increased duration to complete the oral intake (Park et al. 2014).
Nutritional support, which includes even the tracing of the minimum drop in oxygen during feeding, is one of the major aspects of care for those who take care of the preterm infants. It is also believed that sufficient oxygenation helps in maintaining the body tune; oral - move control; coordination of sucking, swallowing, and breathing during feeding. Infants with more oxygen drop during their feeding, make a less effort for sucking as a result of which it takes a long time to attain the complete oral feeding (Thoyre & Carlson 2003a). In response to the increased impact of breathing, cardiac output of supplying blood, oxygen, and adequate food increases during feeding. In the heart of a mature person, cardiac contractility increases to enhance cardiac output, but in the preterm heart it causes more impulses. Therefore, the heart rate can be a good indication of physiological function to maintain an infant’s stability (Park 2012).
Following the improvements in the care of infants, it resulted in the promotion of the survival of premature infants with more attention towards the importance of feeding strategies (Clark et al. 2007). Positioning is a simple strategy that is applicable while taking care of the infants. There are no definite guidelines for health care providers, according to the prior clinical evidences, about the infant’s position during feeding (Park 2012). There is, therefore, a review of the impact of positioning during bottle feeding infants over their physiological stability in order to determine a better position in feeding infants to help in their growth in a non-invasive manner.
2. Materials and Methods
All published articles based on randomized and quasi-randomized clinical trial, and also crossover studies with proper conditions were included in this study through an electronic search. Databases such as Scopus, Ovid, Science Direct, ProQuest, Pub Med, Wiley Cochrane Library, Magiran, Medlib, SID, and Google Scholar were referred. English keywords, i.e., position nutrition newborn from 1997 to 2016, and Persian keywords including Vaz’iyat-e qarar-giri (position) Taqzia (nutrition) Nowzad (newborn) from 2010 to 2016 were searched. At the first step, each article was scanned and then selected for analysis after meeting all the required criteria. The quality of previous studies was decided by using the Cochran bias search tool.
3. Results
Total 4 clinical trials with crossover eligible criteria were selected to study the impact of the positioning of preterm infants while bottle feeding (N = 57) (Clark et al. 2007) (N = 6); Stevens (2007) (N = 20); Dawson et al. (2013) (N = 25); and Park et al. 2014(N = 6). There was no Persian study in this concern. All four crossover studies reviewed the impact of different positions on physiological parameters during bottle feeding, as mentioned in Table 1.
Clark et al. 2007 in their review of elevated side-lying vs. semi-upright showed that there is no significant statistical difference between two positions, but the heart rate increased in the first 3 minutes of feeding and returned to the normal state in the mid 3 minutes, and thus, the elevated side-lying position was more preferred. There was a significant interaction between nutrition and feeding positions, with the decreased rate of SpO2 during the first 3 minutes of feeding in both the positions, which later increased to mid 3 minutes in the elevated side-lying position while decreased in the semi-upright position.
Stevens (2007) indicated there is no significant difference in feeding in an upright position (head and body in
45o) vs. cradle position (head and body in 15o). However, the results showed that heart rate was slightly lower, and SpO2 and the feeding time were shorter in semi-upright position vs. cradle position.
Dawson et al. (2013) tried feeding each infant twice in 24 hours gaps in both side-lying and cradle positions; and measured their heart rate, SpO2, and respiratory rate prior to, during, and after 30 minutes of being fed. There was a small difference in oxygen saturation between the cradle position (94%) and side-lying (95%). The drop in oxygen saturation was recorded in 68% of infants in the cradle position, and 56% in the side-lying position. There was a very small difference in the heart rate prior to, during, and 30 minutes of being fed between two positions, whereas the infants fed in cradle position experienced a less number of symptomatic bradycardia (100 beat/min). There was no significant difference between two positions for respiratory rate. The resulted time to complete feeding was found to be 27 minutes for cradle position, and 23 minutes for side-lying. It was also found that the milk consumed in cradle position was comparatively less.
Park et al. (2014) tried feeding each infant twice in 9 hours gaps in both semi-elevated side-lying and semi-elevated supine positions; and measured their heart rate, SpO2, and respiratory rate prior to and during being fed. There was a small difference in oxygen saturation for cradle position (94%) and side-lying (95%), whereas the drop in the oxygen saturation was recorded in 68% of infants in the cradle position, and 56% in the side-lying position. There was a very small difference in heart rate prior to, during, and after 30 minutes of being fed between two positions. The infants fed in cradle position experienced a less number of symptomatic bradycardia (100 beat/min). There was no significant difference between two positions for respiratory rate.
4. Discussion
These two cases, among all the selected studies, tended to obtain a better stability in side-lying during feeding (Clark et al. 2007; Park et al. 2014); where two other studied deduced that there is no significant difference between two positions (Stevens (2007); Dawson et al. (2013)). It was further observed in two studies that milk consuming was more when the infants were in side-lying position, but their head angles were different in these cases (Dawson et al. (2013); Park et al. 2014). It was also shown that semi-elevated supine position was more efficient and needed less skill compared to the side-lying position (Park et al. 2014). In a systematic review studied by Gillies, Wells, and Bhandari (2012), there was no significant difference in arterial oxygen saturation for both side-lying and supine positions. They also observed that the direction of infant’s placement, either in right or left, had no impact on the physiologic stability of the infants.
Findings of this study are in accordance with the results obtained by Balaguer et al., (2013). They reviewed seven studies, which were conducted on the impact of the infants’ positioning on physiological stability under mechanical ventilation, and found that there was no significant difference. They suggested about the prone position, whose effects on infants’ physiological parameters during feeding are not yet studied. However, this position is also suggested by Kallet (2015) to facilitate infants’ tolerance of enteral nutrition. Raiten et al., (2016) evaluated the evidence for feeding premature infants and indicated that none of these evidences suffice for preparing of the infants’ clinical guidelines.
Regarding the quality of the studies, it can be said that there is not enough evidence for the importance of the role of preterm infants’ positioning on their physiological parameters while being fed. In all cases, the infants were placed in a selected position for a short period of time resulting in the inappropriate blinding and randomization of the small sample size. The lack of considering the long-term effects of positioning is also another constrain for such a study. It is evident that there is not enough evidence and sample to define the role of an infant’s positioning on its physiological stability while feeding. It is, therefore, necessary to study such impacts and the related angle more deeply by implementing better methodologies in future studies.
Acknowledgments
This paper is based on the MSc. thesis of the first Author in the Department of Neonatal Intensive Care Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences of Tehran. The Authors are thankful to International Campus of Iran University of Medical Sciences, Nursing and Midwifery School for financial support. This work has registered by IR.IUMS.REC.1394.9213387201 in Iran Center for Clinical Trials.
Conflict of Interest
The authors declared no conflicts of interest.
References
Abdeyazdan, Z., et al., 2015. [Investigation of oxygenation in premature infants under mechanical ventilation in supine position compare to side lying (Persian)]. Journal of Holistic Nursing and Midwifery, 25(1), pp. 18-25.
Balaguer, A., et al., 2013. Infant position in neonates receiving mechanical ventilation A. Cochrane Database of Systematic Reviews, 11. doi: 10.1002/14651858.cd003668.pub3
Barlow, S. M., 2009. Oral and respiratory control for preterm feeding. Current Opinion in Otolaryngology & Head and Neck Surgery, 17(3), pp. 179-86. doi: 10.1097/moo.0b013e32832b36fe
Chan, S. H. T., et al., 2016. Nutrition and neurodevelopmental outcomes in preterm infants: A systematic review. Acta Paediatrica, 105(6), pp. 587-99. doi: 10.1111/apa.13344
Clark, L., et al., 2007. Improving bottle feeding in preterm infants: Investigating the elevated side lying position. Infant, 3(4), pp. 154-158.
Dawson, J. A., et al., 2013. A randomised trial of two techniques for bottle feeding preterm infants. Journal of Paediatrics and Child Health, 49(6), pp. 462-6. doi: 10.1111/jpc.12208
Elser, H. E., 2012. Positioning after feedings. Advances in Neonatal Care, 12(3), pp. 172-5. doi: 10.1097/anc.0b013e318256b7c1
Gillies, D., Wells, D. & Bhandari, A. P., 2012. Positioning for acute respiratory distress in hospitalised infants and children. Cochrane Database of Systematic Reviews. doi: 10.1002/14651858.cd003645.pub3
Gouna, G., et al., 2013. Positioning effects on lung function and breathing pattern in premature newborns. The Journal of Pediatrics, 162(6), pp. 1133-7.e1. doi: 10.1016/j.jpeds.2012.11.036
Kallet, R. H., 2015. A comprehensive review of prone position in ARDS. Respiratory Care, 60(11), pp. 1660–87. doi: 10.4187/respcare.04271
Park, J., 2012. Feeding outcomes in very preterm infants: Preliminary effects of positioning (PhD dissertation). Chapel Hill, North Carolina: The University of North Carolina at Chapel Hill.
Park, J. et al., 2014. Efficacy of semielevated side lying positioning during bottle feeding of very preterm infants. The Journal of Perinatal & Neonatal Nursing, 28(1), pp. 69-79. doi: 10.1097/jpn.0000000000000004
Picheansathian, W., Woragidpoonpol, P. & Baosoung, C., 2009. Positioning of preterm infants for optimal physiological development: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 7(7), pp. 224-59. doi: 10.11124/01938924-200907070-00001
Raiten, D. J., et al., 2016. Working group reports: Evaluation of the evidence to support practice guidelines for nutritional care of preterm infants—the Pre-B Project. The American Journal of Clinical Nutrition, 103(2), pp. 648S-78S. doi: 10.3945/ajcn.115.117309
Sabrina Lopes, L., et al., 2014. A non invasive technique for evaluation of respiratory efforts in preterm infants during feeding. Journal of Neonatal Nursing, 20(4), pp. 171-7. doi: 10.1016/j.jnn.2013.10.006
Sakalidis, V. S., et al., 2012. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. International Journal of Pediatrics, 2012, pp. 1-10. doi: 10.1155/2012/130769
Stevens, E. E., 2007. Preterm infant feeding and cardiorespiratory stability (PhD dissertation). Pennsylvania: University of Pittsburgh.
Thoyre, S. M. & Carlson, J., 2003a. Occurrence of oxygen desaturation events during preterm infant bottle feeding near discharge. Early Human Development, 72(1), pp. 25-36. doi: 10.1016/s0378-3782(03)00008-2
Thoyre, S. M. & Carlson, J. R., 2003b. Preterm infants’ behavioural indicators of oxygen decline during bottle feeding. Journal of Advanced Nursing, 43(6), pp. 631-41. doi: 10.1046/j.1365-2648.2003.02762.x
World Health Organization, 2012. Born too soon: The global action report on preterm birth. Geneva: World Health Organization.
World Health Organization, 2014. World prematurity day. Geneva: World Health Organization.
World Health Organization, 2016. Newborns: Reducing mortality. Geneva: World Health Organization.
Dawson et al. (2013) tried feeding each infant twice in 24 hours gaps in both side-lying and cradle positions; and measured their heart rate, SpO2, and respiratory rate prior to, during, and after 30 minutes of being fed. There was a small difference in oxygen saturation between the cradle position (94%) and side-lying (95%). The drop in oxygen saturation was recorded in 68% of infants in the cradle position, and 56% in the side-lying position. There was a very small difference in the heart rate prior to, during, and 30 minutes of being fed between two positions, whereas the infants fed in cradle position experienced a less number of symptomatic bradycardia (100 beat/min). There was no significant difference between two positions for respiratory rate. The resulted time to complete feeding was found to be 27 minutes for cradle position, and 23 minutes for side-lying. It was also found that the milk consumed in cradle position was comparatively less.
Park et al. (2014) tried feeding each infant twice in 9 hours gaps in both semi-elevated side-lying and semi-elevated supine positions; and measured their heart rate, SpO2, and respiratory rate prior to and during being fed. There was a small difference in oxygen saturation for cradle position (94%) and side-lying (95%), whereas the drop in the oxygen saturation was recorded in 68% of infants in the cradle position, and 56% in the side-lying position. There was a very small difference in heart rate prior to, during, and after 30 minutes of being fed between two positions. The infants fed in cradle position experienced a less number of symptomatic bradycardia (100 beat/min). There was no significant difference between two positions for respiratory rate.
4. Discussion
These two cases, among all the selected studies, tended to obtain a better stability in side-lying during feeding (Clark et al. 2007; Park et al. 2014); where two other studied deduced that there is no significant difference between two positions (Stevens (2007); Dawson et al. (2013)). It was further observed in two studies that milk consuming was more when the infants were in side-lying position, but their head angles were different in these cases (Dawson et al. (2013); Park et al. 2014). It was also shown that semi-elevated supine position was more efficient and needed less skill compared to the side-lying position (Park et al. 2014). In a systematic review studied by Gillies, Wells, and Bhandari (2012), there was no significant difference in arterial oxygen saturation for both side-lying and supine positions. They also observed that the direction of infant’s placement, either in right or left, had no impact on the physiologic stability of the infants.
Findings of this study are in accordance with the results obtained by Balaguer et al., (2013). They reviewed seven studies, which were conducted on the impact of the infants’ positioning on physiological stability under mechanical ventilation, and found that there was no significant difference. They suggested about the prone position, whose effects on infants’ physiological parameters during feeding are not yet studied. However, this position is also suggested by Kallet (2015) to facilitate infants’ tolerance of enteral nutrition. Raiten et al., (2016) evaluated the evidence for feeding premature infants and indicated that none of these evidences suffice for preparing of the infants’ clinical guidelines.
Regarding the quality of the studies, it can be said that there is not enough evidence for the importance of the role of preterm infants’ positioning on their physiological parameters while being fed. In all cases, the infants were placed in a selected position for a short period of time resulting in the inappropriate blinding and randomization of the small sample size. The lack of considering the long-term effects of positioning is also another constrain for such a study. It is evident that there is not enough evidence and sample to define the role of an infant’s positioning on its physiological stability while feeding. It is, therefore, necessary to study such impacts and the related angle more deeply by implementing better methodologies in future studies.
Acknowledgments
This paper is based on the MSc. thesis of the first Author in the Department of Neonatal Intensive Care Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences of Tehran. The Authors are thankful to International Campus of Iran University of Medical Sciences, Nursing and Midwifery School for financial support. This work has registered by IR.IUMS.REC.1394.9213387201 in Iran Center for Clinical Trials.
Conflict of Interest
The authors declared no conflicts of interest.
References
Abdeyazdan, Z., et al., 2015. [Investigation of oxygenation in premature infants under mechanical ventilation in supine position compare to side lying (Persian)]. Journal of Holistic Nursing and Midwifery, 25(1), pp. 18-25.
Balaguer, A., et al., 2013. Infant position in neonates receiving mechanical ventilation A. Cochrane Database of Systematic Reviews, 11. doi: 10.1002/14651858.cd003668.pub3
Barlow, S. M., 2009. Oral and respiratory control for preterm feeding. Current Opinion in Otolaryngology & Head and Neck Surgery, 17(3), pp. 179-86. doi: 10.1097/moo.0b013e32832b36fe
Chan, S. H. T., et al., 2016. Nutrition and neurodevelopmental outcomes in preterm infants: A systematic review. Acta Paediatrica, 105(6), pp. 587-99. doi: 10.1111/apa.13344
Clark, L., et al., 2007. Improving bottle feeding in preterm infants: Investigating the elevated side lying position. Infant, 3(4), pp. 154-158.
Dawson, J. A., et al., 2013. A randomised trial of two techniques for bottle feeding preterm infants. Journal of Paediatrics and Child Health, 49(6), pp. 462-6. doi: 10.1111/jpc.12208
Elser, H. E., 2012. Positioning after feedings. Advances in Neonatal Care, 12(3), pp. 172-5. doi: 10.1097/anc.0b013e318256b7c1
Gillies, D., Wells, D. & Bhandari, A. P., 2012. Positioning for acute respiratory distress in hospitalised infants and children. Cochrane Database of Systematic Reviews. doi: 10.1002/14651858.cd003645.pub3
Gouna, G., et al., 2013. Positioning effects on lung function and breathing pattern in premature newborns. The Journal of Pediatrics, 162(6), pp. 1133-7.e1. doi: 10.1016/j.jpeds.2012.11.036
Kallet, R. H., 2015. A comprehensive review of prone position in ARDS. Respiratory Care, 60(11), pp. 1660–87. doi: 10.4187/respcare.04271
Park, J., 2012. Feeding outcomes in very preterm infants: Preliminary effects of positioning (PhD dissertation). Chapel Hill, North Carolina: The University of North Carolina at Chapel Hill.
Park, J. et al., 2014. Efficacy of semielevated side lying positioning during bottle feeding of very preterm infants. The Journal of Perinatal & Neonatal Nursing, 28(1), pp. 69-79. doi: 10.1097/jpn.0000000000000004
Picheansathian, W., Woragidpoonpol, P. & Baosoung, C., 2009. Positioning of preterm infants for optimal physiological development: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 7(7), pp. 224-59. doi: 10.11124/01938924-200907070-00001
Raiten, D. J., et al., 2016. Working group reports: Evaluation of the evidence to support practice guidelines for nutritional care of preterm infants—the Pre-B Project. The American Journal of Clinical Nutrition, 103(2), pp. 648S-78S. doi: 10.3945/ajcn.115.117309
Sabrina Lopes, L., et al., 2014. A non invasive technique for evaluation of respiratory efforts in preterm infants during feeding. Journal of Neonatal Nursing, 20(4), pp. 171-7. doi: 10.1016/j.jnn.2013.10.006
Sakalidis, V. S., et al., 2012. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. International Journal of Pediatrics, 2012, pp. 1-10. doi: 10.1155/2012/130769
Stevens, E. E., 2007. Preterm infant feeding and cardiorespiratory stability (PhD dissertation). Pennsylvania: University of Pittsburgh.
Thoyre, S. M. & Carlson, J., 2003a. Occurrence of oxygen desaturation events during preterm infant bottle feeding near discharge. Early Human Development, 72(1), pp. 25-36. doi: 10.1016/s0378-3782(03)00008-2
Thoyre, S. M. & Carlson, J. R., 2003b. Preterm infants’ behavioural indicators of oxygen decline during bottle feeding. Journal of Advanced Nursing, 43(6), pp. 631-41. doi: 10.1046/j.1365-2648.2003.02762.x
World Health Organization, 2012. Born too soon: The global action report on preterm birth. Geneva: World Health Organization.
World Health Organization, 2014. World prematurity day. Geneva: World Health Organization.
World Health Organization, 2016. Newborns: Reducing mortality. Geneva: World Health Organization.
Type of Study: Research |
Subject:
Special
Received: 2016/10/23 | Accepted: 2017/02/10 | Published: 2017/05/1
Received: 2016/10/23 | Accepted: 2017/02/10 | Published: 2017/05/1
References
1. Abdeyazdan, Z., et al., 2015. [Investigation of oxygenation in premature infants under mechanical ventilation in supine position compare to side lying (Persian)]. Journal of Holistic Nursing and Midwifery, 25(1), pp. 18-25.
2. Balaguer, A., et al., 2013. Infant position in neonates receiving mechanical ventilation A. Cochrane Database of Systematic Reviews, 11. doi: 10.1002/14651858.cd003668.pub3 [DOI:10.1002/14651858.CD003668.pub3]
3. Barlow, S. M., 2009. Oral and respiratory control for preterm feeding. Current Opinion in Otolaryngology & Head and Neck Surgery, 17(3), pp. 179-86. doi: 10.1097/moo.0b013e32832b36fe [DOI:10.1097/MOO.0b013e32832b36fe]
4. Chan, S. H. T., et al., 2016. Nutrition and neurodevelopmental outcomes in preterm infants: A systematic review. Acta Paediatrica, 105(6), pp. 587-99. doi: 10.1111/apa.13344 [DOI:10.1111/apa.13344]
5. Clark, L., et al., 2007. Improving bottle feeding in preterm infants: Investigating the elevated side lying position. Infant, 3(4), pp. 154-158.
6. Dawson, J. A., et al., 2013. A randomised trial of two techniques for bottle feeding preterm infants. Journal of Paediatrics and Child Health, 49(6), pp. 462-6. doi: 10.1111/jpc.12208 [DOI:10.1111/jpc.12208]
7. Elser, H. E., 2012. Positioning after feedings. Advances in Neonatal Care, 12(3), pp. 172-5. doi: 10.1097/anc.0b013e318256b7c1 [DOI:10.1097/ANC.0b013e318256b7c1]
8. Gillies, D., Wells, D. & Bhandari, A. P., 2012. Positioning for acute respiratory distress in hospitalised infants and children. Cochrane Database of Systemat-ic Reviews. doi: 10.1002/14651858.cd003645.pub3 [DOI:10.1002/14651858.CD003645.pub3]
9. Gouna, G., et al., 2013. Positioning effects on lung function and breathing pattern in premature newborns. The Journal of Pediatrics, 162(6), pp. 1133-7.e1. doi: 10.1016/j.jpeds.2012.11.036 [DOI:10.1016/j.jpeds.2012.11.036]
10. Kallet, R. H., 2015. A comprehensive review of prone position in ARDS. Respiratory Care, 60(11), pp. 1660–87. doi: 10.4187/respcare.04271 [DOI:10.4187/respcare.04271]
11. Park, J., 2012. Feeding outcomes in very preterm infants: Preliminary effects of positioning (PhD dissertation). Chapel Hill, North Carolina: The University of North Carolina at Chapel Hill.
12. Park, J. et al., 2014. Efficacy of semielevated side lying positioning during bottle feeding of very preterm infants. The Journal of Perinatal & Neonatal Nursing, 28(1), pp. 69-79. doi: 10.1097/jpn.0000000000000004 [DOI:10.1097/JPN.0000000000000004]
13. Picheansathian, W., Woragidpoonpol, P. & Baosoung, C., 2009. Positioning of preterm infants for optimal physiological development: A systematic re-view. JBI Database of Systematic Reviews and Implementation Reports, 7(7), pp. 224-59. doi: 10.11124/01938924-200907070-00001 [DOI:10.11124/01938924-200907070-00001]
14. Raiten, D. J., et al., 2016. Working group reports: Evaluation of the evidence to support practice guidelines for nutritional care of preterm infants—the Pre-B Project. The American Journal of Clinical Nutrition, 103(2), pp. 648S-78S. doi: 10.3945/ajcn.115.117309 [DOI:10.3945/ajcn.115.117309]
15. Sabrina Lopes, L., et al., 2014. A non invasive technique for evaluation of respiratory efforts in preterm infants during feeding. Journal of Neonatal Nursing, 20(4), pp. 171-7. doi: 10.1016/j.jnn.2013.10.006 [DOI:10.1016/j.jnn.2013.10.006]
16. Sakalidis, V. S., et al., 2012. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releas-ing milk only with vacuum. International Journal of Pediatrics, 2012, pp. 1-10. doi: 10.1155/2012/130769 [DOI:10.1155/2012/130769]
17. Stevens, E. E., 2007. Preterm infant feeding and cardiorespiratory stability (PhD dissertation). Pennsylvania: University of Pittsburgh.
18. Thoyre, S. M. & Carlson, J., 2003a. Occurrence of oxygen desaturation events during preterm infant bottle feeding near discharge. Early Human Develop-ment, 72(1), pp. 25-36. doi: 10.1016/s0378-3782(03)00008-2 [DOI:10.1016/S0378-3782(03)00008-2]
19. Thoyre, S. M. & Carlson, J. R., 2003b. Preterm infants' behavioural indicators of oxygen decline during bottle feeding. Journal of Advanced Nursing, 43(6), pp. 631-41. doi: 10.1046/j.1365-2648.2003.02762.x [DOI:10.1046/j.1365-2648.2003.02762.x]
20. World Health Organization, 2012. Born too soon: The global action report on preterm birth. Geneva: World Health Organization.
21. World Health Organization, 2014. World prematurity day. Geneva: World Health Organization.
22. World Health Organization, 2016. Newborns: Reducing mortality. Geneva: World Health Organization.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |