Sat, Oct 18, 2025
[Archive]
Volume 3, Issue 1 (Winter 2017 -- 2017)
JCCNC 2017, 3(1): 45-50 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rafii F, Haghani H, Heidari Beni F. Health-Related Quality of Life and Related Factors in Patients With Chronic Obstructive Pulmonary Disease . JCCNC 2017; 3 (1) :45-50
URL: http://jccnc.iums.ac.ir/article-1-120-en.html
URL: http://jccnc.iums.ac.ir/article-1-120-en.html
1- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Biostatics, School of Health, Iran University of Medical Sciences,Tehran, Iran.
3- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,heidarifarshad70@yahoo.com
2- Department of Biostatics, School of Health, Iran University of Medical Sciences,Tehran, Iran.
3- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
Keywords: Health-related quality of life, Chronic Obstructive Pulmonary Disease (COPD), Related factors
Full-Text [PDF 553 kb]
(1555 Downloads)
| Abstract (HTML) (4979 Views)
Full-Text: (1105 Views)
1. Background
Chronic Obstructive Pulmonary Disease (COPD) is a common illness that affects millions of people around the world (Yang et al. 2017). As one of the most serious public health problems, COPD is in the fourth place and among the top 10 causes of death worldwide. In 2015, about 3.17 million people died around the world due to COPD (Wang et al. 2017). The deaths from this disease is on the rise, and it is expected to be the third leading cause of death worldwide by 2020 (Sarioglu et al. 2016). The prevalence of this disease in Iran and among people over 40 years old worldwide is estimated at 10% (Mirbagher-Ajorpaz & Rezaei 2011; Hagstad et al. 2015). The individual, social, and economic costs of this disease are huge, for instance, it is about 50 $ billion a year in the United States (Nguyen et al. 2016).
COPD is an irreversible disease characterized by permanent and progressive airway obstruction (Clari et al. 2017). The chronic airway obstruction in COPD is caused by the inflammation of small airways (bronchitis) or degeneration of the lung parenchyma (emphysema) (Vogelmeier et al. 2017). The symptoms of COPD, including shortness of breath, cough and sputum/secretion have a negative effect on the health status of the patient and may lead to disability. Although COPD is initially a lung disease, it is considered as a systemic disorder due to non-pulmonary manifestations that affects other organs of the body and the health status of patients (Divo 2013). This disease has no definitive treatment (Norrie et al. 2016) and the existing treatments only delay the progression of the disease. Patients should therefore suffer from the disease for many years which has a negative impact on the physical, mental, and social aspects of their lives (Yu, Guo & Zhang 2014); most patients with COPD, despite the best medical treatments, suffer from reduced physical activity, poor general health, social isolation and depression, which all have a profound effect on the patients’ life (Nguyen et al. 2016). As a result, patients with COPD have lower level of health-related quality of life (Brandl et al. 2016).
Health-related quality of life refers to those aspects of health perceived by individuals which are affected by the disease or treatment (Karimi & Brazier 2016). Because of the chronic, untreatable, and usually progressive nature of COPD, assessment of health-related quality of life is an important tool for evaluating and managing this disease (Ryynänen et al. 2013). Measuring health-related quality of life is important for examining the limitations and progression of the disease over time, as well as the effect of medical procedure (Wacker et al. 2016a). On the other hand, health-related quality of life is a relevant concept in nursing. Due to the impact of this disease on all aspects of patient’s life, nurses should evaluate the patients’ quality of life to provide proper care based on the patients’ health status (Masroor et al. 2012).
Theoretical models have identified factors such as age, sex, severity of disease, lung function, body mass index, smoking status, symptoms, level of activity, comorbidity, depression, anxiety and exacerbation of the disease among the most important factors affecting the health status of patients with COPD. The identification of factors associated with the health-related quality of life in patients with COPD helps healthcare personnel, and in particular nurses, organize their activities through an adjustment of these factors and thereby take an important step to improve the patients’ health-related quality of life. However, no study has been carried out in our country to determine the factors associated with health-related quality of life. Therefore, the researchers decided to conduct a study aimed at determining the health-related quality of life and related factors in patients with COPD.
2. Materials & Methods
Study design and participants
The present study is a cross-sectional descriptive research that was performed in 2016 on patients with COPD who referred to selected hospitals of Shahrekord University of Medical Sciences (Hajar Hospital and Ayatollah Kashani Hospital). A total of 141 patients were selected and entered the study through consecutive sampling method. Inclusion criteria were being 40-75 years old, having COPD diagnosed by a physician, being in the stage 2 or 3 of disease, the patient’s ability to understand and speak Persian, the ability of patients or their companion to read or write in Persian, having ability to interview and complete the questionnaire, not attending at a previous self-management programs of COPD, lacking mental illness, pulmonary tuberculosis, active cancer and severe neurological problems, and lack of communicative problems. The exclusion criteria also included having any signs, symptoms or diagnosis of asthma, bronchiectasis, pulmonary tuberculosis, pneumoconiosis and acute congestive heart failure. After obtaining informed consent from patients and explaining the objectives of the study, the required data were collected. (Ethics Code: IR.IUMS.REC.1394.9211196.203)
Data collection
The research tools included a demographic questionnaire, assessing age, sex, marital status, educational level, income adequacy, body mass index, stage of disease, history of disease, comorbidity, and smoking status, as well as St. George’s Respiratory Questionnaire (SGRQ) for health-related quality of life. SGRQ is one of the most commonly used tools for measuring the health-related quality of life in patients with respiratory problems. The questionnaire has 50 questions and consists of three sections: 1) signs and symptoms of lung complaints in terms of severity and intensity, 2) activity section, including activities that the patient is unable to do because of the disease, and 3) the disease impact on social and psychosocial performance of individuals. The mean score of these three sections makes the total score of health-related quality of life. The score of each section in this questionnaire ranges from 0 to 100, where 0 indicates complete health and the health-related quality of life health is reduced with increasing scores. This questionnaire has been widely used by Iranian and foreign researchers and its validity and reliability for patients with COPD have been confirmed. In Iran, the Cronbach α was 0.74 for the signs and symptoms section and 0.93 for the sections of activity, impact and total score of health-related quality of life (Fallah Tafti et al. 2007).
Data analysis
Statistical tests of Independent t test, one-way ANOVA, and linear regression were used for data analysis which was done by SPSS V. 24. The significance level was considered less than 0.05.
3. Results
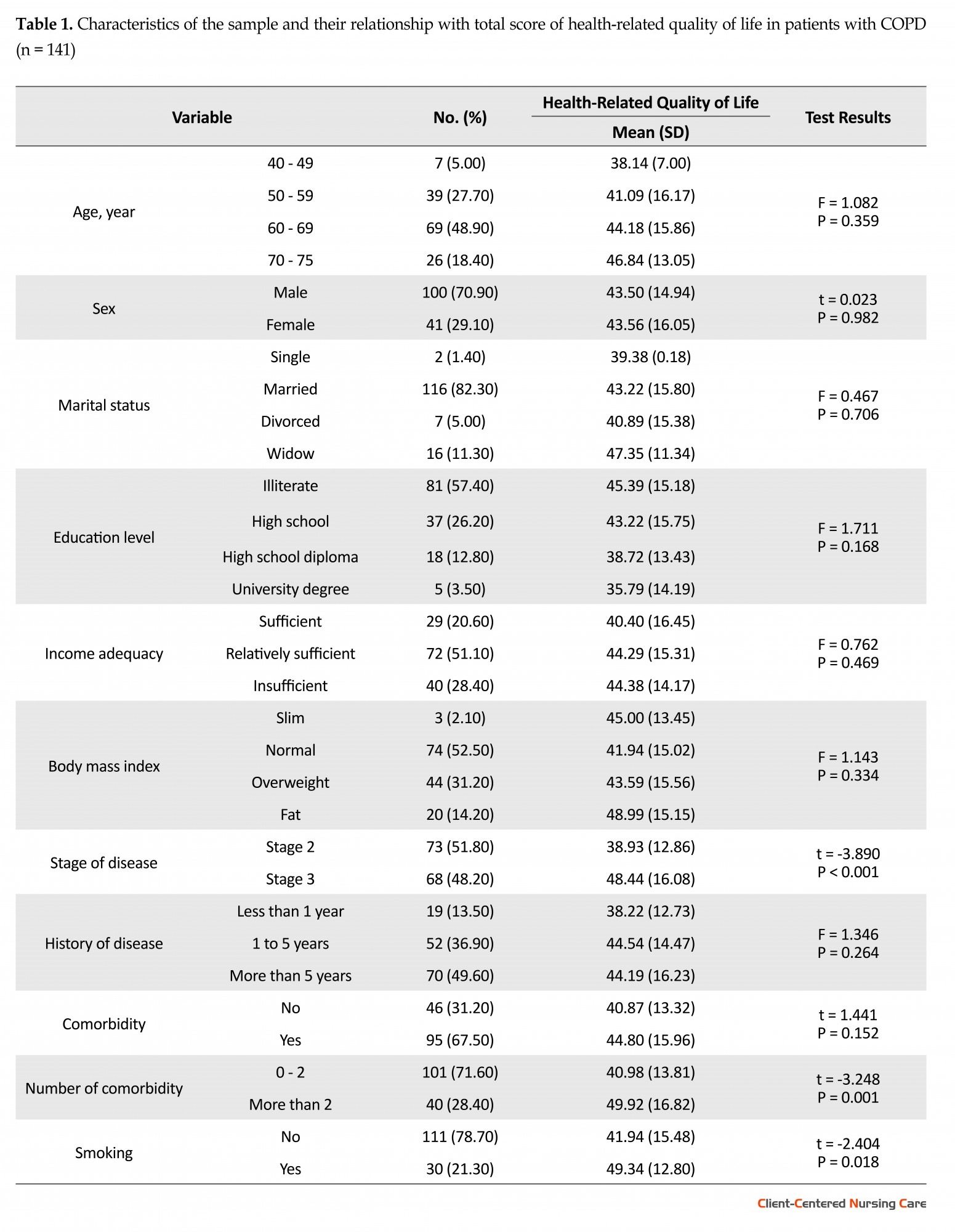
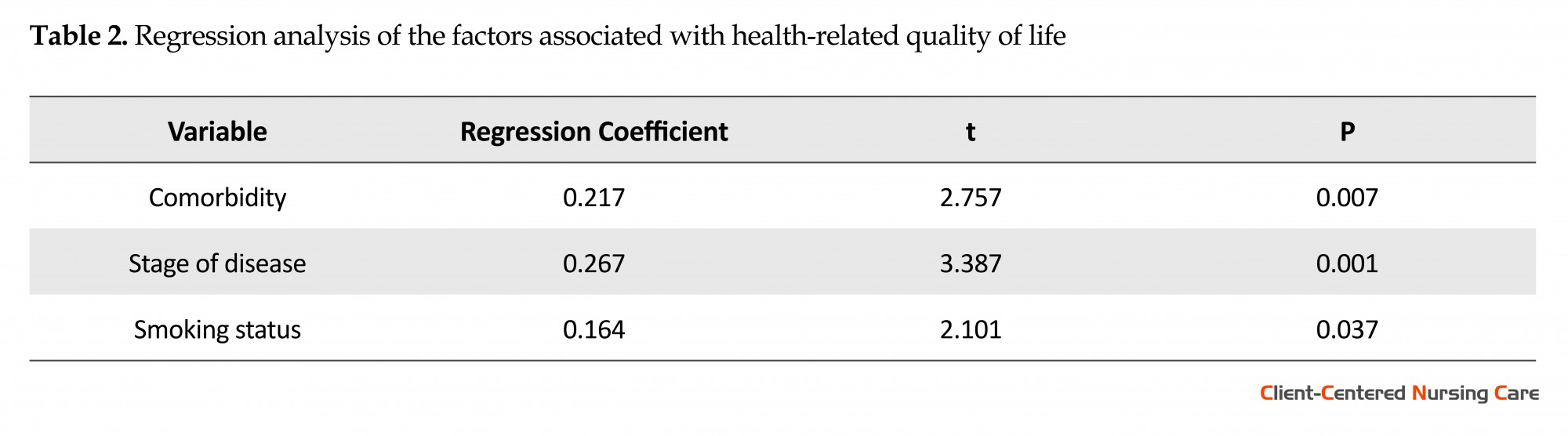
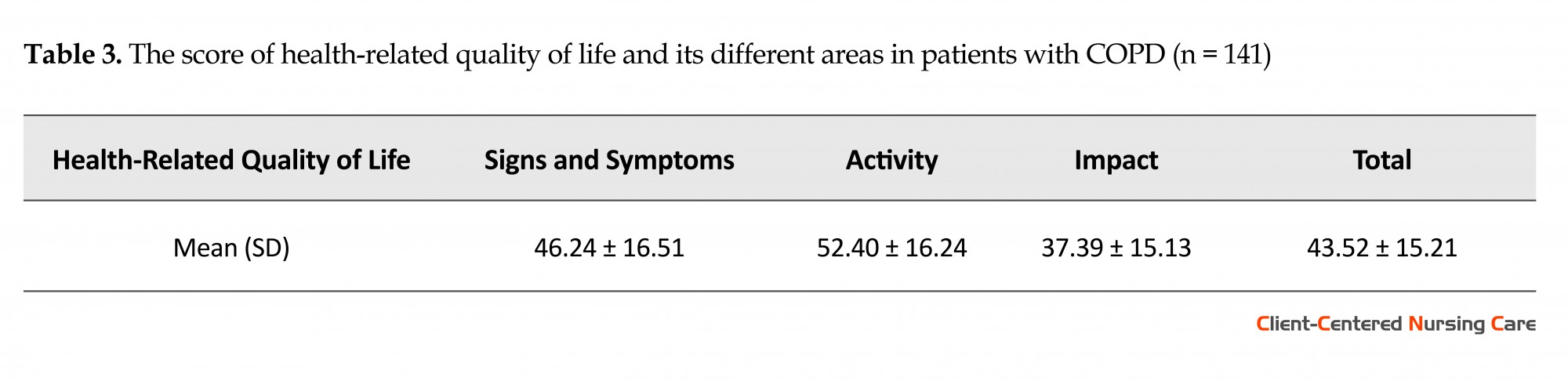
Most study participants (70.9%) were male. The Mean (SD) age of participants was 62.75 (7.39) years. According to Table 1, there was no relationship between the level of health-related quality of life and the variables of age, sex, marital status, comorbidity, education level, income adequacy, body mass index, and history of COPD. However according to Table 2, there was a statistically significant relationship between health-related quality of life with the variables of disease stage, number of comorbidity (0-2 and more than 2 diseases), and smoking status (P = 0.001, P = 0.007, P = 0.037, respectively). As shown in Table 3, the average (SD) total score of health-related quality of life in study patients with COPD was 43.52 (15.21); also the average (SD) score of symptoms, activity, and impact sections were 46.24 (16.51), 52.40 (16.24), and 37.39 (15.14), respectively.
Chronic Obstructive Pulmonary Disease (COPD) is a common illness that affects millions of people around the world (Yang et al. 2017). As one of the most serious public health problems, COPD is in the fourth place and among the top 10 causes of death worldwide. In 2015, about 3.17 million people died around the world due to COPD (Wang et al. 2017). The deaths from this disease is on the rise, and it is expected to be the third leading cause of death worldwide by 2020 (Sarioglu et al. 2016). The prevalence of this disease in Iran and among people over 40 years old worldwide is estimated at 10% (Mirbagher-Ajorpaz & Rezaei 2011; Hagstad et al. 2015). The individual, social, and economic costs of this disease are huge, for instance, it is about 50 $ billion a year in the United States (Nguyen et al. 2016).
COPD is an irreversible disease characterized by permanent and progressive airway obstruction (Clari et al. 2017). The chronic airway obstruction in COPD is caused by the inflammation of small airways (bronchitis) or degeneration of the lung parenchyma (emphysema) (Vogelmeier et al. 2017). The symptoms of COPD, including shortness of breath, cough and sputum/secretion have a negative effect on the health status of the patient and may lead to disability. Although COPD is initially a lung disease, it is considered as a systemic disorder due to non-pulmonary manifestations that affects other organs of the body and the health status of patients (Divo 2013). This disease has no definitive treatment (Norrie et al. 2016) and the existing treatments only delay the progression of the disease. Patients should therefore suffer from the disease for many years which has a negative impact on the physical, mental, and social aspects of their lives (Yu, Guo & Zhang 2014); most patients with COPD, despite the best medical treatments, suffer from reduced physical activity, poor general health, social isolation and depression, which all have a profound effect on the patients’ life (Nguyen et al. 2016). As a result, patients with COPD have lower level of health-related quality of life (Brandl et al. 2016).
Health-related quality of life refers to those aspects of health perceived by individuals which are affected by the disease or treatment (Karimi & Brazier 2016). Because of the chronic, untreatable, and usually progressive nature of COPD, assessment of health-related quality of life is an important tool for evaluating and managing this disease (Ryynänen et al. 2013). Measuring health-related quality of life is important for examining the limitations and progression of the disease over time, as well as the effect of medical procedure (Wacker et al. 2016a). On the other hand, health-related quality of life is a relevant concept in nursing. Due to the impact of this disease on all aspects of patient’s life, nurses should evaluate the patients’ quality of life to provide proper care based on the patients’ health status (Masroor et al. 2012).
Theoretical models have identified factors such as age, sex, severity of disease, lung function, body mass index, smoking status, symptoms, level of activity, comorbidity, depression, anxiety and exacerbation of the disease among the most important factors affecting the health status of patients with COPD. The identification of factors associated with the health-related quality of life in patients with COPD helps healthcare personnel, and in particular nurses, organize their activities through an adjustment of these factors and thereby take an important step to improve the patients’ health-related quality of life. However, no study has been carried out in our country to determine the factors associated with health-related quality of life. Therefore, the researchers decided to conduct a study aimed at determining the health-related quality of life and related factors in patients with COPD.
2. Materials & Methods
Study design and participants
The present study is a cross-sectional descriptive research that was performed in 2016 on patients with COPD who referred to selected hospitals of Shahrekord University of Medical Sciences (Hajar Hospital and Ayatollah Kashani Hospital). A total of 141 patients were selected and entered the study through consecutive sampling method. Inclusion criteria were being 40-75 years old, having COPD diagnosed by a physician, being in the stage 2 or 3 of disease, the patient’s ability to understand and speak Persian, the ability of patients or their companion to read or write in Persian, having ability to interview and complete the questionnaire, not attending at a previous self-management programs of COPD, lacking mental illness, pulmonary tuberculosis, active cancer and severe neurological problems, and lack of communicative problems. The exclusion criteria also included having any signs, symptoms or diagnosis of asthma, bronchiectasis, pulmonary tuberculosis, pneumoconiosis and acute congestive heart failure. After obtaining informed consent from patients and explaining the objectives of the study, the required data were collected. (Ethics Code: IR.IUMS.REC.1394.9211196.203)
Data collection
The research tools included a demographic questionnaire, assessing age, sex, marital status, educational level, income adequacy, body mass index, stage of disease, history of disease, comorbidity, and smoking status, as well as St. George’s Respiratory Questionnaire (SGRQ) for health-related quality of life. SGRQ is one of the most commonly used tools for measuring the health-related quality of life in patients with respiratory problems. The questionnaire has 50 questions and consists of three sections: 1) signs and symptoms of lung complaints in terms of severity and intensity, 2) activity section, including activities that the patient is unable to do because of the disease, and 3) the disease impact on social and psychosocial performance of individuals. The mean score of these three sections makes the total score of health-related quality of life. The score of each section in this questionnaire ranges from 0 to 100, where 0 indicates complete health and the health-related quality of life health is reduced with increasing scores. This questionnaire has been widely used by Iranian and foreign researchers and its validity and reliability for patients with COPD have been confirmed. In Iran, the Cronbach α was 0.74 for the signs and symptoms section and 0.93 for the sections of activity, impact and total score of health-related quality of life (Fallah Tafti et al. 2007).
Data analysis
Statistical tests of Independent t test, one-way ANOVA, and linear regression were used for data analysis which was done by SPSS V. 24. The significance level was considered less than 0.05.
3. Results
Most study participants (70.9%) were male. The Mean (SD) age of participants was 62.75 (7.39) years. According to Table 1, there was no relationship between the level of health-related quality of life and the variables of age, sex, marital status, comorbidity, education level, income adequacy, body mass index, and history of COPD. However according to Table 2, there was a statistically significant relationship between health-related quality of life with the variables of disease stage, number of comorbidity (0-2 and more than 2 diseases), and smoking status (P = 0.001, P = 0.007, P = 0.037, respectively). As shown in Table 3, the average (SD) total score of health-related quality of life in study patients with COPD was 43.52 (15.21); also the average (SD) score of symptoms, activity, and impact sections were 46.24 (16.51), 52.40 (16.24), and 37.39 (15.14), respectively.
4. Discussion
The present study showed that the average level of health-related quality of life in patients with COPD was 43.52; as well, the score of symptoms, activity, and impact area were 46.24 (16.51), 52.40 (16.24) and 37.39 (15.14), respectively, indicating a significant reduction in the level of their health-related quality of life.
Miravitlles et al. (2009) reported that the score of health-related quality of life is 8.8 in normal people without COPD, as well the score of symptoms, activity, and impact areas were 11.11, 12.6, and 5.6, respectively. The average total score of health-related quality of life in people with COPD in seven European countries (Belgium, France, Spain, Italy, Netherlands, United Kingdom, and Germany) is close to the results of the present study, ranging from 39.2 to 50.1. It indicates a decrease in the level of health-related quality of life among patients with COPD (Jones et al. 2011). Some other studies have also reported a significant reduction in the health-related quality of life in patients with COPD (De Sousa Pinto et al. 2010; Marin et al. 2011).
The present study approved the relationship between health-related quality of life and disease stage, smoking status and number of comorbidity (0 to 2 and more than 2 diseases). Several studies similar to the present study have reported the relationship between health-related quality of life and stage of the disease (Medinas Amorós et al. 2009; Ståhl et al. 2005; Wacker et al., 2016b).
The results of a research aimed at assessing the health status of patients with COPD were similar to the present study results, and reported a significant difference between the scores of health-related quality of life in patients with 0-2 comorbidities compared to patients with 3 and more comorbidities (Jones et al. 2011). However, the results of another study showed a statistically significant difference between health-related quality of life in patients with 3 comorbidities compared to patients with more than 3 (Wacker et al., 2016b).
Other studies published by Jones et al. in 2012 also found a statistically significant difference between health-related quality of life and the number of comorbidities (Jones et al. 2012). The study by Balcells et al. (2010) revealed a link between the reduction in the level of health-related quality of life and two or more comorbidities measured by the Charlson Index. Since the type of comorbidity has been shown to affect the health-related quality of life in patients with COPD (Burgel et al. 2013), different results may be due to the difference in the type of comorbidity of the subjects. Another study similar to the present study did not report a significant relationship between age, sex, and BMI with health-related quality of life. However, the results of this study, contrary to the present study results, did not show a significant relationship between smoking status and the total score of health-related quality of life (Deslee et al. 2016).
The most important limitation of this study was the old age and thus, low education level of patients with COPD. To overcome this limitation, it was tried to get help from the families and companions of patients who did not have enough education to complete the questionnaire.
Based on the research findings, the level of health-related quality of life in patients with COPD is significantly low and the variables of disease stage, number of comorbidity, and smoking status are inversely related with health-related quality of life. Therefore, it is better for healthcare personnel, especially nurses, to assess the health-related quality of life in patients with COPD, and thus plan for appropriate measures to improve the quality level and related factors.
Acknowledgments
This study has been extracted from a research project approved by Vice Chancellor of Research in Iran University of Medical Sciences (approval code: 95-01-28-27738). The authors are very thankful to all the patients participated in this research.
Conflict of Interest
The authors declared no conflicts of interest.
References
Balcells, E., et al., 2010. Factors affecting the relationship between psychological status and quality of life in COPD pa-tients. Health and Quality of Life Outcomes, 8(1), p. 108. doi: 10.1186/1477-7525-8-108
Brandl, M., et al., 2016. Factors associated with health-related quality of life (HRQOL) in adults with chronic obstructive pulmonary disease (COPD). Das Gesundheitswesen, 78(8-9). doi: 10.1055/s-0036-1586635
Burgel, P. R., et al., 2013. Impact of comorbidities on COPD-specific health-related quality of life. Respiratory Medicine, 107(2), pp. 233–41. doi: 10.1016/j.rmed.2012.10.002
Clari, M., et al., 2017. Self-care of people with chronic obstructive pulmonary disease: A meta-synthesis. The Patient - Patient-Centered Outcomes Research, 10(4), pp. 407–27. doi: 10.1007/s40271-017-0218-z
Das, A., et al., 2015. Evaluation of correlation of BODE index with health-related quality of life among patients with sta-ble COPD attending a tertiary care hospital. Lung India, 32(1), p. 24. doi: 10.4103/0970-2113.148434
De Sousa Pinto, J. M. et al., 2010. The health-related quality of life of patients with chronic obstructive pulmonary disease and asthma evaluated by the SGRQ. Revista Portuguesa de Pneumologia (English Edition), 16(4), pp. 543–58. doi: 10.1016/s2173-5115(10)70058-0
Deslee, G., et al., 2016. Impact of current cough on health-related quality of life in patients with COPD. International Journal of Chronic Obstructive Pulmonary Disease, 11, pp. 2091–7. doi: 10.2147/copd.s106883
Divo, M., 2013. COPD, co-morbidities and health-related quality of Life (HRQOL): More is less. Journal of Chronic Obstructive Pulmonary Disease, 10(3), pp. 275–6. doi: 10.3109/15412555.2013.795409
Fallah Tafti, S., Marashian, S. M., Cheraghvandi, A. & Emami, H., 2007. Investigation of validity and reliability of Per-sian version of the" St. George Respiratory Questionaire". Pejouhandeh: Bimonthly Research Journal, pp. 43-50.
Hagstad, S. et al., 2015. Prevalence and risk factors of COPD among never-smokers in two areas of Sweden – occupa-tional exposure to gas, dust or fumes is an important risk factor. Respiratory Medicine, 109(11), pp. 1439–45. doi: 10.1016/j.rmed.2015.09.012
Ioanna, T., et al., 2011. Factors that influence disease-specific quality of life or health status in patients with COPD: A systematic review and meta-analysis of Pearson correlations. Primary Care Respiratory Journal, 20(3), pp. 257–68. doi: 10.4104/pcrj.2011.00029
Jones, P. W., et al., 2011. Health-related quality of life in patients by COPD severity within primary care in Europe. Res-piratory Medicine, 105(1), pp. 57–66. doi: 10.1016/j.rmed.2010.09.004
Jones, P. W., et al., 2012. Patient-centred assessment of COPD in primary care: Experience from a cross-sectional study of health-related quality of life in Europe. Primary Care Respiratory Journal, 21(3), pp. 329–36. doi: 10.4104/pcrj.2012.00065
Karimi, M. & Brazier, J., 2016. Health, health-related quality of life, and quality of life: What is the difference. Phar-macoEconomics, 34(7), pp. 645–9. doi: 10.1007/s40273-016-0389-9
Marin, J. M., et al., 2011. Prognostic assessment in COPD: Health related quality of life and the BODE index. Respiratory Medicine, 105(6), pp. 916–21. doi: 10.1016/j.rmed.2011.01.007
Masroor, D. D., et al., 2012. Health-related quality of life in patients with chronic obstructive pulmonary disease. Iran Journal of Nursing, 25(76), pp. 19-27.
Medinas Amorós, M., et al., 2009. Health-related quality of life is associated with COPD severity: A comparison between the GOLD staging and the BODE index. Chronic Respiratory Disease, 6(2), pp. 75–80. doi: 10.1177/1479972308101551
Miravitlles, M., et al., 2009. Prevalence of COPD in Spain: Impact of undiagnosed COPD on quality of life and daily life activities. Thorax, 64(10), pp. 863–868. doi: 10.1136/thx.2009.115725
Mirbagher-Ajorpaz, N. & Rezaei, M., 2011. The effect of pulmonary rehabilitation program on quality of life of elderly patients with chronic obstructive pulmonary disease. Zahedan Journal of Research in Medical Sciences, 13(1), pp. 30-5.
Nguyen, H. Q., et al., 2016. Patient-centered physical activity coaching in COPD (Walk On!): A study protocol for a prag-matic randomized controlled trial. Contemporary Clinical Trials, 46, pp. 18–29. doi: 10.1016/j.cct.2015.10.010
Norrie, O. S., et al., 2016. Chronic obstructive pulmonary disease (COPD) in-tegrated care pathway project: Evaluation of patient outcomes and system efficiencies. Journal of Population Thera-peutics and Clinical Pharmacology, 23(3), pp. 169-82.
Ryynänen, O. P., et al., 2013. Bayesian predictors of very poor health related quality of life and mortality in patients with COPD. BMC Medical Informatics and Decision Making, 13, p. 34. doi: 10.1186/1472-6947-13-34
Sarioglu, N., et al., 2016. Is the COPD assessment test (CAT) effective in demonstrating the systemic inflammation and other components in COPD. Revista Portuguesa de Pneumologia (English Edition), 22(1), pp. 11–7. doi: 10.1016/j.rppnen.2015.08.007
Ståhl, E., et al., 2005. Health-related quality of life is related to COPD disease severity. Health and Quality of Life Outcomes, 3(1), p. 56. doi: 10.1186/1477-7525-3-56
Vogelmeier, C. F., et al., 2017. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report. Respirology, 22(3), pp. 575–601. doi: 10.1111/resp. 13012
Wacker, M. E., et al., 2016a. Assessing health-related quality of life in COPD: Comparing generic and disease-specific in-struments with focus on comorbidities. BMC Pulmonary Medicine, 16, pp. 70. doi: 10.1186/s12890-016-0238-9
Wacker, M. E., et al., 2016b. Relative impact of COPD and comorbidities on generic health-related quality of life: A pooled analysis of the COSYCONET patient cohort and control subjects from the KORA and SHIP studies. Respiratory Re-search, 17, pp. 81. doi: 10.1186/s12931-016-0401-0
Wang, T., et al., 2017. Effectiveness of disease-specific self-management education on health outcomes in patients with chronic obstructive pulmonary disease: An updated systematic review and meta-analysis. Patient Education and Counseling, 100(8), pp. 1432–46. doi: 10.1016/j.pec.2017.02.026
Yang, F., et al., 2017. Continuity of care to prevent readmissions for patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Journal of Chronic Obstructive Pulmonary Disease, 14(2), pp. 251–61. doi: 10.1080/15412555.2016.1256384
Yu, S. H., Guo, A. M. & Zhang, X. J., 2014. Effects of self-management education on quality of life of patients with chronic obstructive pulmonary disease. International Journal of Nursing Sciences, 1(1), pp. 53–7. doi: 10.1016/j.ijnss.2014.02.014
The present study showed that the average level of health-related quality of life in patients with COPD was 43.52; as well, the score of symptoms, activity, and impact area were 46.24 (16.51), 52.40 (16.24) and 37.39 (15.14), respectively, indicating a significant reduction in the level of their health-related quality of life.
Miravitlles et al. (2009) reported that the score of health-related quality of life is 8.8 in normal people without COPD, as well the score of symptoms, activity, and impact areas were 11.11, 12.6, and 5.6, respectively. The average total score of health-related quality of life in people with COPD in seven European countries (Belgium, France, Spain, Italy, Netherlands, United Kingdom, and Germany) is close to the results of the present study, ranging from 39.2 to 50.1. It indicates a decrease in the level of health-related quality of life among patients with COPD (Jones et al. 2011). Some other studies have also reported a significant reduction in the health-related quality of life in patients with COPD (De Sousa Pinto et al. 2010; Marin et al. 2011).
The present study approved the relationship between health-related quality of life and disease stage, smoking status and number of comorbidity (0 to 2 and more than 2 diseases). Several studies similar to the present study have reported the relationship between health-related quality of life and stage of the disease (Medinas Amorós et al. 2009; Ståhl et al. 2005; Wacker et al., 2016b).
The results of a research aimed at assessing the health status of patients with COPD were similar to the present study results, and reported a significant difference between the scores of health-related quality of life in patients with 0-2 comorbidities compared to patients with 3 and more comorbidities (Jones et al. 2011). However, the results of another study showed a statistically significant difference between health-related quality of life in patients with 3 comorbidities compared to patients with more than 3 (Wacker et al., 2016b).
Other studies published by Jones et al. in 2012 also found a statistically significant difference between health-related quality of life and the number of comorbidities (Jones et al. 2012). The study by Balcells et al. (2010) revealed a link between the reduction in the level of health-related quality of life and two or more comorbidities measured by the Charlson Index. Since the type of comorbidity has been shown to affect the health-related quality of life in patients with COPD (Burgel et al. 2013), different results may be due to the difference in the type of comorbidity of the subjects. Another study similar to the present study did not report a significant relationship between age, sex, and BMI with health-related quality of life. However, the results of this study, contrary to the present study results, did not show a significant relationship between smoking status and the total score of health-related quality of life (Deslee et al. 2016).
The most important limitation of this study was the old age and thus, low education level of patients with COPD. To overcome this limitation, it was tried to get help from the families and companions of patients who did not have enough education to complete the questionnaire.
Based on the research findings, the level of health-related quality of life in patients with COPD is significantly low and the variables of disease stage, number of comorbidity, and smoking status are inversely related with health-related quality of life. Therefore, it is better for healthcare personnel, especially nurses, to assess the health-related quality of life in patients with COPD, and thus plan for appropriate measures to improve the quality level and related factors.
Acknowledgments
This study has been extracted from a research project approved by Vice Chancellor of Research in Iran University of Medical Sciences (approval code: 95-01-28-27738). The authors are very thankful to all the patients participated in this research.
Conflict of Interest
The authors declared no conflicts of interest.
References
Balcells, E., et al., 2010. Factors affecting the relationship between psychological status and quality of life in COPD pa-tients. Health and Quality of Life Outcomes, 8(1), p. 108. doi: 10.1186/1477-7525-8-108
Brandl, M., et al., 2016. Factors associated with health-related quality of life (HRQOL) in adults with chronic obstructive pulmonary disease (COPD). Das Gesundheitswesen, 78(8-9). doi: 10.1055/s-0036-1586635
Burgel, P. R., et al., 2013. Impact of comorbidities on COPD-specific health-related quality of life. Respiratory Medicine, 107(2), pp. 233–41. doi: 10.1016/j.rmed.2012.10.002
Clari, M., et al., 2017. Self-care of people with chronic obstructive pulmonary disease: A meta-synthesis. The Patient - Patient-Centered Outcomes Research, 10(4), pp. 407–27. doi: 10.1007/s40271-017-0218-z
Das, A., et al., 2015. Evaluation of correlation of BODE index with health-related quality of life among patients with sta-ble COPD attending a tertiary care hospital. Lung India, 32(1), p. 24. doi: 10.4103/0970-2113.148434
De Sousa Pinto, J. M. et al., 2010. The health-related quality of life of patients with chronic obstructive pulmonary disease and asthma evaluated by the SGRQ. Revista Portuguesa de Pneumologia (English Edition), 16(4), pp. 543–58. doi: 10.1016/s2173-5115(10)70058-0
Deslee, G., et al., 2016. Impact of current cough on health-related quality of life in patients with COPD. International Journal of Chronic Obstructive Pulmonary Disease, 11, pp. 2091–7. doi: 10.2147/copd.s106883
Divo, M., 2013. COPD, co-morbidities and health-related quality of Life (HRQOL): More is less. Journal of Chronic Obstructive Pulmonary Disease, 10(3), pp. 275–6. doi: 10.3109/15412555.2013.795409
Fallah Tafti, S., Marashian, S. M., Cheraghvandi, A. & Emami, H., 2007. Investigation of validity and reliability of Per-sian version of the" St. George Respiratory Questionaire". Pejouhandeh: Bimonthly Research Journal, pp. 43-50.
Hagstad, S. et al., 2015. Prevalence and risk factors of COPD among never-smokers in two areas of Sweden – occupa-tional exposure to gas, dust or fumes is an important risk factor. Respiratory Medicine, 109(11), pp. 1439–45. doi: 10.1016/j.rmed.2015.09.012
Ioanna, T., et al., 2011. Factors that influence disease-specific quality of life or health status in patients with COPD: A systematic review and meta-analysis of Pearson correlations. Primary Care Respiratory Journal, 20(3), pp. 257–68. doi: 10.4104/pcrj.2011.00029
Jones, P. W., et al., 2011. Health-related quality of life in patients by COPD severity within primary care in Europe. Res-piratory Medicine, 105(1), pp. 57–66. doi: 10.1016/j.rmed.2010.09.004
Jones, P. W., et al., 2012. Patient-centred assessment of COPD in primary care: Experience from a cross-sectional study of health-related quality of life in Europe. Primary Care Respiratory Journal, 21(3), pp. 329–36. doi: 10.4104/pcrj.2012.00065
Karimi, M. & Brazier, J., 2016. Health, health-related quality of life, and quality of life: What is the difference. Phar-macoEconomics, 34(7), pp. 645–9. doi: 10.1007/s40273-016-0389-9
Marin, J. M., et al., 2011. Prognostic assessment in COPD: Health related quality of life and the BODE index. Respiratory Medicine, 105(6), pp. 916–21. doi: 10.1016/j.rmed.2011.01.007
Masroor, D. D., et al., 2012. Health-related quality of life in patients with chronic obstructive pulmonary disease. Iran Journal of Nursing, 25(76), pp. 19-27.
Medinas Amorós, M., et al., 2009. Health-related quality of life is associated with COPD severity: A comparison between the GOLD staging and the BODE index. Chronic Respiratory Disease, 6(2), pp. 75–80. doi: 10.1177/1479972308101551
Miravitlles, M., et al., 2009. Prevalence of COPD in Spain: Impact of undiagnosed COPD on quality of life and daily life activities. Thorax, 64(10), pp. 863–868. doi: 10.1136/thx.2009.115725
Mirbagher-Ajorpaz, N. & Rezaei, M., 2011. The effect of pulmonary rehabilitation program on quality of life of elderly patients with chronic obstructive pulmonary disease. Zahedan Journal of Research in Medical Sciences, 13(1), pp. 30-5.
Nguyen, H. Q., et al., 2016. Patient-centered physical activity coaching in COPD (Walk On!): A study protocol for a prag-matic randomized controlled trial. Contemporary Clinical Trials, 46, pp. 18–29. doi: 10.1016/j.cct.2015.10.010
Norrie, O. S., et al., 2016. Chronic obstructive pulmonary disease (COPD) in-tegrated care pathway project: Evaluation of patient outcomes and system efficiencies. Journal of Population Thera-peutics and Clinical Pharmacology, 23(3), pp. 169-82.
Ryynänen, O. P., et al., 2013. Bayesian predictors of very poor health related quality of life and mortality in patients with COPD. BMC Medical Informatics and Decision Making, 13, p. 34. doi: 10.1186/1472-6947-13-34
Sarioglu, N., et al., 2016. Is the COPD assessment test (CAT) effective in demonstrating the systemic inflammation and other components in COPD. Revista Portuguesa de Pneumologia (English Edition), 22(1), pp. 11–7. doi: 10.1016/j.rppnen.2015.08.007
Ståhl, E., et al., 2005. Health-related quality of life is related to COPD disease severity. Health and Quality of Life Outcomes, 3(1), p. 56. doi: 10.1186/1477-7525-3-56
Vogelmeier, C. F., et al., 2017. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report. Respirology, 22(3), pp. 575–601. doi: 10.1111/resp. 13012
Wacker, M. E., et al., 2016a. Assessing health-related quality of life in COPD: Comparing generic and disease-specific in-struments with focus on comorbidities. BMC Pulmonary Medicine, 16, pp. 70. doi: 10.1186/s12890-016-0238-9
Wacker, M. E., et al., 2016b. Relative impact of COPD and comorbidities on generic health-related quality of life: A pooled analysis of the COSYCONET patient cohort and control subjects from the KORA and SHIP studies. Respiratory Re-search, 17, pp. 81. doi: 10.1186/s12931-016-0401-0
Wang, T., et al., 2017. Effectiveness of disease-specific self-management education on health outcomes in patients with chronic obstructive pulmonary disease: An updated systematic review and meta-analysis. Patient Education and Counseling, 100(8), pp. 1432–46. doi: 10.1016/j.pec.2017.02.026
Yang, F., et al., 2017. Continuity of care to prevent readmissions for patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Journal of Chronic Obstructive Pulmonary Disease, 14(2), pp. 251–61. doi: 10.1080/15412555.2016.1256384
Yu, S. H., Guo, A. M. & Zhang, X. J., 2014. Effects of self-management education on quality of life of patients with chronic obstructive pulmonary disease. International Journal of Nursing Sciences, 1(1), pp. 53–7. doi: 10.1016/j.ijnss.2014.02.014
Type of Study: Research |
Subject:
General
Received: 2016/07/21 | Accepted: 2016/10/28 | Published: 2017/08/20
Received: 2016/07/21 | Accepted: 2016/10/28 | Published: 2017/08/20
References
1. Balcells, E., et al., 2010. Factors affecting the relationship between psychological status and quality of life in COPD pa-tients. Health and Quality of Life Outcomes, 8(1), p. 108. doi: 10.1186/1477-7525-8-108 [DOI:10.1186/1477-7525-8-108]
2. Brandl, M., et al., 2016. Factors associated with health-related quality of life (HRQOL) in adults with chronic obstructive pulmonary disease (COPD). Das Gesundheitswesen, 78(8-9). doi: 10.1055/s-0036-1586635 [DOI:10.1055/s-0036-1586635]
3. Burgel, P. R., et al., 2013. Impact of comorbidities on COPD-specific health-related quality of life. Respiratory Medicine, 107(2), pp. 233–41. doi: 10.1016/j.rmed.2012.10.002 [DOI:10.1016/j.rmed.2012.10.002]
4. Clari, M., et al., 2017. Self-care of people with chronic obstructive pulmonary disease: A meta-synthesis. The Patient - Patient-Centered Outcomes Research, 10(4), pp. 407–27. doi: 10.1007/s40271-017-0218-z [DOI:10.1007/s40271-017-0218-z]
5. Das, A., et al., 2015. Evaluation of correlation of BODE index with health-related quality of life among patients with sta-ble COPD attending a tertiary care hospital. Lung India, 32(1), p. 24. doi: 10.4103/0970-2113.148434 [DOI:10.4103/0970-2113.148434]
6. De Sousa Pinto, J. M. et al., 2010. The health-related quality of life of patients with chronic obstructive pulmonary disease and asthma evaluated by the SGRQ. Revista Portuguesa de Pneumologia (English Edition), 16(4), pp. 543–58. doi: 10.1016/s2173-5115(10)70058-0 [DOI:10.1016/S2173-5115(10)70058-0]
7. Deslee, G., et al., 2016. Impact of current cough on health-related quality of life in patients with COPD. International Journal of Chronic Obstructive Pulmonary Disease, 11, pp. 2091–7. doi: 10.2147/copd.s106883 [DOI:10.2147/COPD.S106883]
8. Divo, M., 2013. COPD, co-morbidities and health-related quality of Life (HRQOL): More is less. Journal of Chronic Obstructive Pulmonary Disease, 10(3), pp. 275–6. doi: 10.3109/15412555.2013.795409 [DOI:10.3109/15412555.2013.795409]
9. Fallah Tafti, S., Marashian, S. M., Cheraghvandi, A. & Emami, H., 2007. Investigation of validity and reliability of Per-sian version of the" St. George Respiratory Questionaire". Pejouhandeh: Bimonthly Research Journal, pp. 43-50.
10. Hagstad, S. et al., 2015. Prevalence and risk factors of COPD among never-smokers in two areas of Sweden – occupa-tional exposure to gas, dust or fumes is an important risk factor. Respiratory Medicine, 109(11), pp. 1439–45. doi: 10.1016/j.rmed.2015.09.012 [DOI:10.1016/j.rmed.2015.09.012]
11. Ioanna, T., et al., 2011. Factors that influence disease-specific quality of life or health status in patients with COPD: A systematic review and meta-analysis of Pearson correlations. Primary Care Respiratory Journal, 20(3), pp. 257–68. doi: 10.4104/pcrj.2011.00029 [DOI:10.4104/pcrj.2011.00029]
12. Jones, P. W., et al., 2011. Health-related quality of life in patients by COPD severity within primary care in Europe. Res-piratory Medicine, 105(1), pp. 57–66. doi: 10.1016/j.rmed.2010.09.004 [DOI:10.1016/j.rmed.2010.09.004]
13. Jones, P. W., et al., 2012. Patient-centred assessment of COPD in primary care: Experience from a cross-sectional study of health-related quality of life in Europe. Primary Care Respiratory Journal, 21(3), pp. 329–36. doi: 10.4104/pcrj.2012.00065 [DOI:10.4104/pcrj.2012.00065]
14. Karimi, M. & Brazier, J., 2016. Health, health-related quality of life, and quality of life: What is the difference. Phar-macoEconomics, 34(7), pp. 645–9. doi: 10.1007/s40273-016-0389-9 [DOI:10.1007/s40273-016-0389-9]
15. Marin, J. M., et al., 2011. Prognostic assessment in COPD: Health related quality of life and the BODE index. Respiratory Medicine, 105(6), pp. 916–21. doi: 10.1016/j.rmed.2011.01.007 [DOI:10.1016/j.rmed.2011.01.007]
16. Masroor, D. D., et al., 2012. Health-related quality of life in patients with chronic obstructive pulmonary disease. Iran Journal of Nursing, 25(76), pp. 19-27.
17. Medinas Amorós, M., et al., 2009. Health-related quality of life is associated with COPD severity: A comparison between the GOLD staging and the BODE index. Chronic Respiratory Disease, 6(2), pp. 75–80. doi: 10.1177/1479972308101551 [DOI:10.1177/1479972308101551]
18. Miravitlles, M., et al., 2009. Prevalence of COPD in Spain: Impact of undiagnosed COPD on quality of life and daily life activities. Thorax, 64(10), pp. 863–868. doi: 10.1136/thx.2009.115725 [DOI:10.1136/thx.2009.115725]
19. Mirbagher-Ajorpaz, N. & Rezaei, M., 2011. The effect of pulmonary rehabilitation program on quality of life of elderly patients with chronic obstructive pulmonary disease. Zahedan Journal of Research in Medical Sciences, 13(1), pp. 30-5.
20. Nguyen, H. Q., et al., 2016. Patient-centered physical activity coaching in COPD (Walk On!): A study protocol for a prag-matic randomized controlled trial. Contemporary Clinical Trials, 46, pp. 18–29. doi: 10.1016/j.cct.2015.10.010 [DOI:10.1016/j.cct.2015.10.010]
21. Norrie, O. S., et al., 2016. Chronic obstructive pulmonary disease (COPD) in-tegrated care pathway project: Evaluation of patient outcomes and system efficiencies. Journal of Population Thera-peutics and Clinical Pharmacology, 23(3), pp. 169-82.
22. Ryynänen, O. P., et al., 2013. Bayesian predictors of very poor health related quality of life and mortality in patients with COPD. BMC Medical Informatics and Decision Making, 13, p. 34. doi: 10.1186/1472-6947-13-34 [DOI:10.1186/1472-6947-13-34]
23. Sarioglu, N., et al., 2016. Is the COPD assessment test (CAT) effective in demonstrating the systemic inflammation and other components in COPD. Revista Portuguesa de Pneumologia (English Edition), 22(1), pp. 11–7. doi: 10.1016/j.rppnen.2015.08.007 [DOI:10.1016/j.rppnen.2015.08.007]
24. Ståhl, E., et al., 2005. Health-related quality of life is related to COPD disease severity. Health and Quality of Life Outcomes, 3(1), p. 56. doi: 10.1186/1477-7525-3-56 [DOI:10.1186/1477-7525-3-56]
25. Vogelmeier, C. F., et al., 2017. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report. Respirology, 22(3), pp. 575–601. doi: 10.1111/resp. 13012
26. Wacker, M. E., et al., 2016a. Assessing health-related quality of life in COPD: Comparing generic and disease-specific in-struments with focus on comorbidities. BMC Pulmonary Medicine, 16, pp. 70. doi: 10.1186/s12890-016-0238-9 [DOI:10.1186/s12890-016-0238-9]
27. Wacker, M. E., et al., 2016b. Relative impact of COPD and comorbidities on generic health-related quality of life: A pooled analysis of the COSYCONET patient cohort and control subjects from the KORA and SHIP studies. Respiratory Re-search, 17, pp. 81. doi: 10.1186/s12931-016-0401-0 [DOI:10.1186/s12931-016-0401-0]
28. Wang, T., et al., 2017. Effectiveness of disease-specific self-management education on health outcomes in patients with chronic obstructive pulmonary disease: An updated systematic review and meta-analysis. Patient Education and Counseling, 100(8), pp. 1432–46. doi: 10.1016/j.pec.2017.02.026 [DOI:10.1016/j.pec.2017.02.026]
29. Yang, F., et al., 2017. Continuity of care to prevent readmissions for patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Journal of Chronic Obstructive Pulmonary Disease, 14(2), pp. 251–61. doi: 10.1080/15412555.2016.1256384 [DOI:10.1080/15412555.2016.1256384]
30. Yu, S. H., Guo, A. M. & Zhang, X. J., 2014. Effects of self-management education on quality of life of patients with chronic obstructive pulmonary disease. International Journal of Nursing Sciences, 1(1), pp. 53–7. doi: 10.1016/j.ijnss.2014.02.014 [DOI:10.1016/j.ijnss.2014.02.014]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |