Sun, Aug 10, 2025
[Archive]
Volume 3, Issue 2 (Spring 2017 -- 2017)
JCCNC 2017, 3(2): 147-152 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khachian A, Seyedoshohadaee M, Hosseini A F, Shamsi M, Bahiraei N. Self-Management and Its Related Factors Among People With Epilepsy Referring to Iranian Epilepsy Association. JCCNC 2017; 3 (2) :147-152
URL: http://jccnc.iums.ac.ir/article-1-126-en.html
URL: http://jccnc.iums.ac.ir/article-1-126-en.html
Alice Khachian1 
 , Mahnaz Seyedoshohadaee2
, Mahnaz Seyedoshohadaee2 
 , Agha Fatemeh Hosseini1
, Agha Fatemeh Hosseini1 
 , Marzieh Shamsi3
, Marzieh Shamsi3 
 , Narges Bahiraei *4
, Narges Bahiraei *4 


 , Mahnaz Seyedoshohadaee2
, Mahnaz Seyedoshohadaee2 
 , Agha Fatemeh Hosseini1
, Agha Fatemeh Hosseini1 
 , Marzieh Shamsi3
, Marzieh Shamsi3 
 , Narges Bahiraei *4
, Narges Bahiraei *4 

1- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Rehabilitation Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,narges_bahiraei@yahoo.com
2- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Rehabilitation Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 559 kb]
(1150 Downloads)
| Abstract (HTML) (3977 Views)
Full-Text: (848 Views)
1. Background
Epilepsy is a chronic neurological disorder that imposes many costs on individuals and society. In Iran, epilepsy is prevalent in 1.2 to 4 individuals per 1,000 people (Akbarbegloo et al. 2015). People with epilepsy have limited information on their disease and thus, are poorly adapted to their conditions (Edward et al. 2015). Since epilepsy has a devastating effect on the lives of the affected people, these people may feel like a burden on their family and community (Sawangchareon et al. 2013). The lack of awareness of the disease and its social stigma often result in an increased risk of personal injury premature death (Mameniskiene, Sakalauskaite Juodeikiene & Budrys 2015). The treatment and control of chronic diseases, including epilepsy, involve learning how to live with symptoms or disability and being accustomed to the resultant identity change.
Another part of the treatment includes lifestyle changes and implementation of necessary treatments to control symptoms and prevent complications (Hinkle & Cheever 2014). Also, individuals with epilepsy should take preventive care to improve disease control and reduce the risk of complications (Pascual et al. 2015). The lack of adherence to treatment may result in further symptoms, more functional disability, increased use of healthcare services, and increased related costs (Fitzsimons et al. 2012). People with epilepsy should be educated so as to identify and manage hysteria stimuli in their surroundings, employ strategies to remember the use of antiepileptic drugs, and take some measures to minimize the risks of hysteria (Merianos et al. 2014). However, people with epilepsy often receive little support from healthcare services regarding self-management behaviors, which results in such people, especially those with low education levels, having limited information about their illness (Noble et al. 2015).
Over the past few decades, there has been a steady change in the provision of services to people with mental disorders. Accordingly, the system-based approach of service provision has been gradually replaced by the individual-based approach. Individual support has been widely welcomed and has become a major issue in providing services to people with mental disorders (Ratti et al. 2016). On the other hand, the importance of self-management among people with epilepsy has recently drawn much attention (Clark et al. 2010). Self-management in epilepsy includes taking medication according to prescriptions, regulating the individual’s lifestyle to prevent hysteria, tracking hysteria and its side effects, timely meeting your doctor, getting information about hysteria, and treating and managing the disease (Walker et al. 2014). The process of self-management can help the patients to control and better adapt to the disease and increase their self-care capabilities (Miller et al. 2015).
Educational interactions and self-management education in people with epilepsy are not necessarily consistent with standard practices (Edward et al. 2015). This has been substantiated by a previous study that showed the methods currently used in self-management education to be ineffective for people with epilepsy, as it causes people to be independent of others, including their family (Fraser et al. 2011). Therefore, the present study aims to determine the self-management behaviors of people with epilepsy.
2. Materials & Methods
This descriptive-correlational study consisted of all patients with epilepsy admitted to the Iranian Epilepsy Association in 2016. From among them, 100 patients were selected using available sampling method. The average age of the participants in the study was about 35, and the majority of participants in the study were single and male. The inclusion criteria in this study were 18-60 years of age, having epilepsy for at least one year, taking antiepileptic drugs, having at least one attack in the recent year, and having read and write literacy. The research ethics were observed by getting permission from the Ethics Committee of Iran University of Medical Sciences to the Code of Ethics IR.IUMS.REC1395.9311686005 and the Iranian Epilepsy Association as well as obtaining written consent from the included patients.
Self-reporting questionnaires such as the demographic information questionnaire, the disease profile form, and the self-management questionnaire for epilepsy were used for collecting the data. The self-management questionnaire for epilepsy, developed by Delirio et al. in 2010, included 38 questions about self-management behaviors on five areas of drug self-management, safety and lifestyle management, hysteria management, and information. The questionnaire was rated on a Likert scale from 1 (never) to 5 (always). For this questionnaire, scores less than 50%, i.e. 38-114, indicated low self-management level, between 50 and 75%, i.e. 115-150, indicated moderate self-management, and above 75%, i.e. 150-190, indicated high self-management.
In the study of Aliasgharpour et al. (2014), the Cronbach’s Alpha coefficient of the questionnaire was determined to be 0.838. The content validity method was used to determine the scientific validity of the data gathering tool. For this purpose, the tools used in the research were provided to ten faculty members of the Faculty of Nursing and Midwifery of Iran Medical Sciences University. The Cronbach’s alpha coefficient was 0.79 in this study. For data collection, the researcher invited the participants to the Epilepsy Association and gave them the questionnaires to complete. The statistical calculations for the information
Epilepsy is a chronic neurological disorder that imposes many costs on individuals and society. In Iran, epilepsy is prevalent in 1.2 to 4 individuals per 1,000 people (Akbarbegloo et al. 2015). People with epilepsy have limited information on their disease and thus, are poorly adapted to their conditions (Edward et al. 2015). Since epilepsy has a devastating effect on the lives of the affected people, these people may feel like a burden on their family and community (Sawangchareon et al. 2013). The lack of awareness of the disease and its social stigma often result in an increased risk of personal injury premature death (Mameniskiene, Sakalauskaite Juodeikiene & Budrys 2015). The treatment and control of chronic diseases, including epilepsy, involve learning how to live with symptoms or disability and being accustomed to the resultant identity change.
Another part of the treatment includes lifestyle changes and implementation of necessary treatments to control symptoms and prevent complications (Hinkle & Cheever 2014). Also, individuals with epilepsy should take preventive care to improve disease control and reduce the risk of complications (Pascual et al. 2015). The lack of adherence to treatment may result in further symptoms, more functional disability, increased use of healthcare services, and increased related costs (Fitzsimons et al. 2012). People with epilepsy should be educated so as to identify and manage hysteria stimuli in their surroundings, employ strategies to remember the use of antiepileptic drugs, and take some measures to minimize the risks of hysteria (Merianos et al. 2014). However, people with epilepsy often receive little support from healthcare services regarding self-management behaviors, which results in such people, especially those with low education levels, having limited information about their illness (Noble et al. 2015).
Over the past few decades, there has been a steady change in the provision of services to people with mental disorders. Accordingly, the system-based approach of service provision has been gradually replaced by the individual-based approach. Individual support has been widely welcomed and has become a major issue in providing services to people with mental disorders (Ratti et al. 2016). On the other hand, the importance of self-management among people with epilepsy has recently drawn much attention (Clark et al. 2010). Self-management in epilepsy includes taking medication according to prescriptions, regulating the individual’s lifestyle to prevent hysteria, tracking hysteria and its side effects, timely meeting your doctor, getting information about hysteria, and treating and managing the disease (Walker et al. 2014). The process of self-management can help the patients to control and better adapt to the disease and increase their self-care capabilities (Miller et al. 2015).
Educational interactions and self-management education in people with epilepsy are not necessarily consistent with standard practices (Edward et al. 2015). This has been substantiated by a previous study that showed the methods currently used in self-management education to be ineffective for people with epilepsy, as it causes people to be independent of others, including their family (Fraser et al. 2011). Therefore, the present study aims to determine the self-management behaviors of people with epilepsy.
2. Materials & Methods
This descriptive-correlational study consisted of all patients with epilepsy admitted to the Iranian Epilepsy Association in 2016. From among them, 100 patients were selected using available sampling method. The average age of the participants in the study was about 35, and the majority of participants in the study were single and male. The inclusion criteria in this study were 18-60 years of age, having epilepsy for at least one year, taking antiepileptic drugs, having at least one attack in the recent year, and having read and write literacy. The research ethics were observed by getting permission from the Ethics Committee of Iran University of Medical Sciences to the Code of Ethics IR.IUMS.REC1395.9311686005 and the Iranian Epilepsy Association as well as obtaining written consent from the included patients.
Self-reporting questionnaires such as the demographic information questionnaire, the disease profile form, and the self-management questionnaire for epilepsy were used for collecting the data. The self-management questionnaire for epilepsy, developed by Delirio et al. in 2010, included 38 questions about self-management behaviors on five areas of drug self-management, safety and lifestyle management, hysteria management, and information. The questionnaire was rated on a Likert scale from 1 (never) to 5 (always). For this questionnaire, scores less than 50%, i.e. 38-114, indicated low self-management level, between 50 and 75%, i.e. 115-150, indicated moderate self-management, and above 75%, i.e. 150-190, indicated high self-management.
In the study of Aliasgharpour et al. (2014), the Cronbach’s Alpha coefficient of the questionnaire was determined to be 0.838. The content validity method was used to determine the scientific validity of the data gathering tool. For this purpose, the tools used in the research were provided to ten faculty members of the Faculty of Nursing and Midwifery of Iran Medical Sciences University. The Cronbach’s alpha coefficient was 0.79 in this study. For data collection, the researcher invited the participants to the Epilepsy Association and gave them the questionnaires to complete. The statistical calculations for the information
obtained in this study were performed using SPSS software version 22.
3. Results
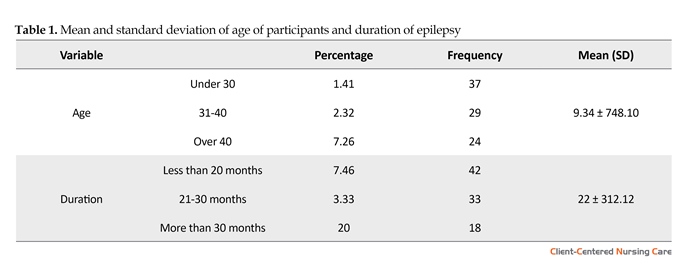
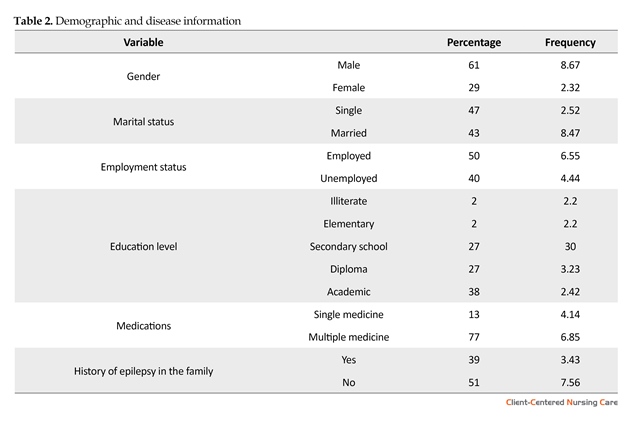
Cognitive and disease information is detailed in Tables 1 and 2. Table 3 shows the results of the difference between the means in the cognitive characteristics of self-management using the independent t-test. According to the results of the independent t-test, there is a significant difference between marital status and total self-management (P < 0.05). Accordingly, married patients have higher self-management than unmarried patients. There is no significant difference between total self-management score and other cognitive characteristics (P > 0.05).
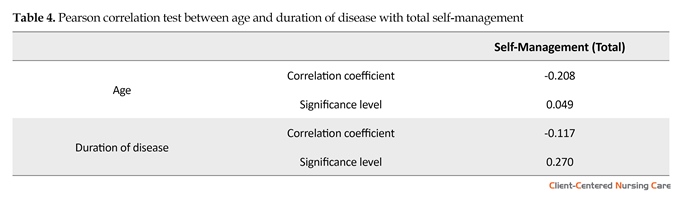
Table 4 shows the results of Pearson correlation test between age and duration of disease with total self-management. According to the Table 4, there is a significant and inverse relationship between age and self-management (P < 0.05). This means that with increasing age, total self-management is reduced. Also, no significant relationship could be established between duration of disease and self-management (P > 0.05).
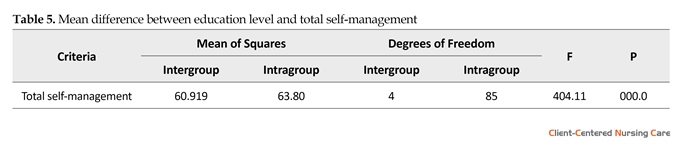
Table 5 shows the results of the mean difference between education level and total self-management using one-way ANOVA. According to the results, there is a significant difference between education level and total self-management (P < 0.01). Table 6 shows the total self-management classification of patients in two low and high classes. Accordingly, 79% of the subjects had low self-management, and 21% had high self-management level.
3. Results
Cognitive and disease information is detailed in Tables 1 and 2. Table 3 shows the results of the difference between the means in the cognitive characteristics of self-management using the independent t-test. According to the results of the independent t-test, there is a significant difference between marital status and total self-management (P < 0.05). Accordingly, married patients have higher self-management than unmarried patients. There is no significant difference between total self-management score and other cognitive characteristics (P > 0.05).
Table 4 shows the results of Pearson correlation test between age and duration of disease with total self-management. According to the Table 4, there is a significant and inverse relationship between age and self-management (P < 0.05). This means that with increasing age, total self-management is reduced. Also, no significant relationship could be established between duration of disease and self-management (P > 0.05).
Table 5 shows the results of the mean difference between education level and total self-management using one-way ANOVA. According to the results, there is a significant difference between education level and total self-management (P < 0.01). Table 6 shows the total self-management classification of patients in two low and high classes. Accordingly, 79% of the subjects had low self-management, and 21% had high self-management level.
4. Discussion
In the present study, the independent t-test showed a significant difference between marital status and total self-management (P < 0.05), indicating that married patients have higher self-management than single ones. This finding was also supported by Tol et al. (2012) study, which showed a significant relationship between marital status and self-management (P < 0.04). Similarly, Rahimian Booger et al. (2010) showed a significant relationship between marital status and self-management of diabetes. Given these results, marital status can have an impact on self-management behaviors, considering the supporting role of the spouse in changing lifestyles. In fact, married people have a relatively stable source of social support in contrast to single people who provide self-care. Also, the results of study by Walker et al. (2012) showed that
In the present study, the independent t-test showed a significant difference between marital status and total self-management (P < 0.05), indicating that married patients have higher self-management than single ones. This finding was also supported by Tol et al. (2012) study, which showed a significant relationship between marital status and self-management (P < 0.04). Similarly, Rahimian Booger et al. (2010) showed a significant relationship between marital status and self-management of diabetes. Given these results, marital status can have an impact on self-management behaviors, considering the supporting role of the spouse in changing lifestyles. In fact, married people have a relatively stable source of social support in contrast to single people who provide self-care. Also, the results of study by Walker et al. (2012) showed that
married people control their illness better. However, the study by Yadollahi et al. (2015) reported that patients who live alone have a higher score in self-management behaviors than those who live with others.
The Pearson test results indicated a significant inverse relationship between age and self-management (P < 0.05). This means that total self-management reduces with increasing age. The study results also showed that age had a significant and negative relationship with the self-management of participants. This may be due to the fact that people’s self-management is affected by age, complications, and treatment. Based on Yadollahi et al. (2015) study, there was no significant relationship between epileptic people's self-management score with epilepsy and age, while in McAuley et al. (2008) study, older people had higher self-management scores.
In the study by Yadollahi et al. (2015), there was a significant relationship between safety self-management and the level of education. Having more information, more educated individuals are more capable of controlling and managing their diseases than those with lower levels of education.
The results of the study by Aliasgharpour et al. (2013) also showed that before the educational intervention, the majority of participants in the study had an average level of self-management. The research results confirmed that due to the low level of self-management behaviors in most of the participants in the study, appropriate training regarding cognitive variables should be done in future studies. There was no specific limitation in this research. It is suggested to examine the impact of self-management education programs regarding the demographic variables in future programs.
Acknowledgments
This paper was extracted from the MSc. thesis of the fourth author in Department of Medical Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences of Tehran. I acknowledge the staffs of Iran University of Medical Sciences, Iranian Epilepsy Association, Chancellor and the faculty members of Nursing and Midwifery, Iran University of Medical Sciences, and all the patients who participated in this study.
Conflict of Interest
The authors declared no conflicts of interest.
References
Aliasgharpour, M. et al., 2013. Effects of an educational program on self-management in patients with epilepsy. Seizure, 22(1), pp. 48–52. doi: 10.1016/j.seizure.2012.10.005
Akbarbegloo, M. et al., 2015. The Relationship between Self-Efficacy and Psychosocial Care in Adolescents with Epilepsy. Epilepsy Research and Treatment, 2015, pp. 1–7. doi: 10.1155/2015/756849
Clark, N. M. et al., 2010. Fostering epilepsy self management: The perspectives of professionals. Epilepsy & Behavior, 19(3), pp. 255–63. doi: 10.1016/j.yebeh.2010.08.033
Edward, K., Cook, M. & Giandinoto, J. A., 2015. An integrative review of the benefits of self-management interventions for adults with epilepsy. Epilepsy & Behavior, 45, pp. 195–204. doi: 10.1016/j.yebeh.2015.01.026
Fitzsimons, M. et al., 2012. Evidence-based models of care for people with epilepsy. Epilepsy & Behavior, 23(1), pp. 1–6. doi: 10.1016/j.yebeh.2011.10.019
Fraser, R.T. et al., 2011. Managing epilepsy well: Self-management needs assessment. Epilepsy & Behavior, 20(2), pp. 291–298. doi: 10.1016/j.yebeh.2010.10.010
Hinkle J. L., & Cheever K. H., 2014. Biophysical and psychosocial concepts in nursing practice. In: JL Hinkle & KH Cheever (ed), Brunner & Suddarth's Textbook of Medical-Surgical Nursing [J Abed Saeidi & H Esmaeili Persian trans]. Tehran: Jame'e Negar.
Mameniskiene, R., Sakalauskaite Juodeikiene, E. & Budrys, V., 2015. People with epilepsy lack knowledge about their disease. Epilepsy & Behavior, 46, pp. 192–7. doi: 10.1016/j.yebeh.2015.03.002
McAuley, J. W. et al., 2008. An evaluation of self-management behaviors and medication adherence in patients with epilepsy. Epilepsy & Behavior, 13(4), pp. 637–641. doi: 10.1016/j.yebeh.2008.07.005
Merianos, A. L. et al., 2014. Hospital, school, and community-based strategies to enhance the quality of life of youth with chronic illness-es. Applied Research in Quality of Life, 10(2), pp. 329–42. doi: 10.1007/s11482-014-9311-9
Miller, W. R. et al., 2015. Chronic disease self-management: A hybrid concept analysis. Nursing Outlook, 63(2), pp. 154–61. doi: 10.1016/j.outlook.2014.07.005
Noble, A. et al., 2015. “Seizure first aid training” for people with epilepsy who attend emergency departments, and their family and friends: study protocol for intervention development and a pilot randomised controlled trial. BMJ Open, 5(7), p. e009040. doi: 10.1136/bmjopen-2015-009040
Pascual, F. T. et al., 2015. Outpatient education reduces emergency room use by patients with epilepsy. Epilepsy & Behavior, 42, pp. 3–6. doi: 10.1016/j.yebeh.2014.10.024
Rahimian Boogar, E., et al., 2010. [Diabetes self management: Social, demographical and disease factors (Persian)]. Journal of Clinical Psychology, 1(4), pp. 43-57.
Ratti, V. et al., 2016. The effectiveness of person-centred planning for people with intellectual disabilities: A systematic review. Research in Developmental Disabilities, 57, pp. 63–84. doi: 10.1016/j.ridd.2016.06.015
Sawangchareon, K., et al., 2013. Moving the self-esteem of people with epilepsy by supportive group: A clinical trial. Journal of Caring Sciences, 2(4), pp. 329-35. doi: 10.5681/jcs.2013.039
Tol, A., et al., 2012. [Relation between empowerment of diabetes control and adoption of self-management behaviors and its related fac-tors among type 2 diabetic patients (Persian)]. Razi Journal of Medical Sciences, 19(98), pp. 11-8.
Walker, E. R. et al., 2012. Social support for self-management behaviors among people with epilepsy: A content analysis of the WebEase program. Epilepsy & Behavior, 23(3), pp. 285–90. doi: 10.1016/j.yebeh.2012.01.006
Yadollahi, S. et al., 2015. [Correlation between Epilepsy Self-Management Behaviors and Seizure Frequency among Patients with Epilepsy in Iran Epilepsy Association (Persian)]. Preventive Care in Nursing & Midwifery Journal, 5(1), pp. 59-70.
The Pearson test results indicated a significant inverse relationship between age and self-management (P < 0.05). This means that total self-management reduces with increasing age. The study results also showed that age had a significant and negative relationship with the self-management of participants. This may be due to the fact that people’s self-management is affected by age, complications, and treatment. Based on Yadollahi et al. (2015) study, there was no significant relationship between epileptic people's self-management score with epilepsy and age, while in McAuley et al. (2008) study, older people had higher self-management scores.
In the study by Yadollahi et al. (2015), there was a significant relationship between safety self-management and the level of education. Having more information, more educated individuals are more capable of controlling and managing their diseases than those with lower levels of education.
The results of the study by Aliasgharpour et al. (2013) also showed that before the educational intervention, the majority of participants in the study had an average level of self-management. The research results confirmed that due to the low level of self-management behaviors in most of the participants in the study, appropriate training regarding cognitive variables should be done in future studies. There was no specific limitation in this research. It is suggested to examine the impact of self-management education programs regarding the demographic variables in future programs.
Acknowledgments
This paper was extracted from the MSc. thesis of the fourth author in Department of Medical Surgical Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences of Tehran. I acknowledge the staffs of Iran University of Medical Sciences, Iranian Epilepsy Association, Chancellor and the faculty members of Nursing and Midwifery, Iran University of Medical Sciences, and all the patients who participated in this study.
Conflict of Interest
The authors declared no conflicts of interest.
References
Aliasgharpour, M. et al., 2013. Effects of an educational program on self-management in patients with epilepsy. Seizure, 22(1), pp. 48–52. doi: 10.1016/j.seizure.2012.10.005
Akbarbegloo, M. et al., 2015. The Relationship between Self-Efficacy and Psychosocial Care in Adolescents with Epilepsy. Epilepsy Research and Treatment, 2015, pp. 1–7. doi: 10.1155/2015/756849
Clark, N. M. et al., 2010. Fostering epilepsy self management: The perspectives of professionals. Epilepsy & Behavior, 19(3), pp. 255–63. doi: 10.1016/j.yebeh.2010.08.033
Edward, K., Cook, M. & Giandinoto, J. A., 2015. An integrative review of the benefits of self-management interventions for adults with epilepsy. Epilepsy & Behavior, 45, pp. 195–204. doi: 10.1016/j.yebeh.2015.01.026
Fitzsimons, M. et al., 2012. Evidence-based models of care for people with epilepsy. Epilepsy & Behavior, 23(1), pp. 1–6. doi: 10.1016/j.yebeh.2011.10.019
Fraser, R.T. et al., 2011. Managing epilepsy well: Self-management needs assessment. Epilepsy & Behavior, 20(2), pp. 291–298. doi: 10.1016/j.yebeh.2010.10.010
Hinkle J. L., & Cheever K. H., 2014. Biophysical and psychosocial concepts in nursing practice. In: JL Hinkle & KH Cheever (ed), Brunner & Suddarth's Textbook of Medical-Surgical Nursing [J Abed Saeidi & H Esmaeili Persian trans]. Tehran: Jame'e Negar.
Mameniskiene, R., Sakalauskaite Juodeikiene, E. & Budrys, V., 2015. People with epilepsy lack knowledge about their disease. Epilepsy & Behavior, 46, pp. 192–7. doi: 10.1016/j.yebeh.2015.03.002
McAuley, J. W. et al., 2008. An evaluation of self-management behaviors and medication adherence in patients with epilepsy. Epilepsy & Behavior, 13(4), pp. 637–641. doi: 10.1016/j.yebeh.2008.07.005
Merianos, A. L. et al., 2014. Hospital, school, and community-based strategies to enhance the quality of life of youth with chronic illness-es. Applied Research in Quality of Life, 10(2), pp. 329–42. doi: 10.1007/s11482-014-9311-9
Miller, W. R. et al., 2015. Chronic disease self-management: A hybrid concept analysis. Nursing Outlook, 63(2), pp. 154–61. doi: 10.1016/j.outlook.2014.07.005
Noble, A. et al., 2015. “Seizure first aid training” for people with epilepsy who attend emergency departments, and their family and friends: study protocol for intervention development and a pilot randomised controlled trial. BMJ Open, 5(7), p. e009040. doi: 10.1136/bmjopen-2015-009040
Pascual, F. T. et al., 2015. Outpatient education reduces emergency room use by patients with epilepsy. Epilepsy & Behavior, 42, pp. 3–6. doi: 10.1016/j.yebeh.2014.10.024
Rahimian Boogar, E., et al., 2010. [Diabetes self management: Social, demographical and disease factors (Persian)]. Journal of Clinical Psychology, 1(4), pp. 43-57.
Ratti, V. et al., 2016. The effectiveness of person-centred planning for people with intellectual disabilities: A systematic review. Research in Developmental Disabilities, 57, pp. 63–84. doi: 10.1016/j.ridd.2016.06.015
Sawangchareon, K., et al., 2013. Moving the self-esteem of people with epilepsy by supportive group: A clinical trial. Journal of Caring Sciences, 2(4), pp. 329-35. doi: 10.5681/jcs.2013.039
Tol, A., et al., 2012. [Relation between empowerment of diabetes control and adoption of self-management behaviors and its related fac-tors among type 2 diabetic patients (Persian)]. Razi Journal of Medical Sciences, 19(98), pp. 11-8.
Walker, E. R. et al., 2012. Social support for self-management behaviors among people with epilepsy: A content analysis of the WebEase program. Epilepsy & Behavior, 23(3), pp. 285–90. doi: 10.1016/j.yebeh.2012.01.006
Yadollahi, S. et al., 2015. [Correlation between Epilepsy Self-Management Behaviors and Seizure Frequency among Patients with Epilepsy in Iran Epilepsy Association (Persian)]. Preventive Care in Nursing & Midwifery Journal, 5(1), pp. 59-70.
Type of Study: Research |
Subject:
Special
Received: 2016/11/15 | Accepted: 2017/02/27 | Published: 2017/05/1
Received: 2016/11/15 | Accepted: 2017/02/27 | Published: 2017/05/1
References
1. Aliasgharpour, M. et al., 2013. Effects of an educational program on self-management in patients with epilepsy. Seizure, 22(1), pp. 48–52. doi: 10.1016/j.seizure.2012.10.005 [DOI:10.1016/j.seizure.2012.10.005]
2. Akbarbegloo, M. et al., 2015. The Relationship between Self-Efficacy and Psychosocial Care in Adolescents with Epilepsy. Epilepsy Research and Treatment, 2015, pp. 1–7. doi: 10.1155/2015/756849 [DOI:10.1155/2015/756849]
3. Clark, N. M. et al., 2010. Fostering epilepsy self management: The perspectives of professionals. Epilepsy & Behavior, 19(3), pp. 255–63. doi: 10.1016/j.yebeh.2010.08.033 [DOI:10.1016/j.yebeh.2010.08.033]
4. Edward, K., Cook, M. & Giandinoto, J. A., 2015. An integrative review of the benefits of self-management interventions for adults with epilepsy. Epilepsy & Behavior, 45, pp. 195–204. doi: 10.1016/j.yebeh.2015.01.026 [DOI:10.1016/j.yebeh.2015.01.026]
5. Fitzsimons, M. et al., 2012. Evidence-based models of care for people with epilepsy. Epilepsy & Behavior, 23(1), pp. 1–6. doi: 10.1016/j.yebeh.2011.10.019 [DOI:10.1016/j.yebeh.2011.10.019]
6. Fraser, R.T. et al., 2011. Managing epilepsy well: Self-management needs assessment. Epilepsy & Behavior, 20(2), pp. 291–298. doi: 10.1016/j.yebeh.2010.10.010 [DOI:10.1016/j.yebeh.2010.10.010]
7. Hinkle J. L., & Cheever K. H., 2014. Biophysical and psychosocial concepts in nursing practice. In: JL Hinkle & KH Cheever (ed), Brunner & Suddarth's Textbook of Medical-Surgical Nursing [J Abed Saeidi & H Esmaeili Persian trans]. Tehran: Jame'e Negar.
8. Mameniskiene, R., Sakalauskaite Juodeikiene, E. & Budrys, V., 2015. People with epilepsy lack knowledge about their disease. Epi-lepsy & Behavior, 46, pp. 192–7. doi: 10.1016/j.yebeh.2015.03.002 [DOI:10.1016/j.yebeh.2015.03.002]
9. McAuley, J. W. et al., 2008. An evaluation of self-management behaviors and medication adherence in patients with epilepsy. Epi-lepsy & Behavior, 13(4), pp. 637–641. doi: 10.1016/j.yebeh.2008.07.005 [DOI:10.1016/j.yebeh.2008.07.005]
10. Merianos, A. L. et al., 2014. Hospital, school, and community-based strategies to enhance the quality of life of youth with chronic illness-es. Applied Research in Quality of Life, 10(2), pp. 329–42. doi: 10.1007/s11482-014-9311-9 [DOI:10.1007/s11482-014-9311-9]
11. Miller, W. R. et al., 2015. Chronic disease self-management: A hybrid concept analysis. Nursing Outlook, 63(2), pp. 154–61. doi: 10.1016/j.outlook.2014.07.005 [DOI:10.1016/j.outlook.2014.07.005]
12. Noble, A. et al., 2015. "Seizure first aid training" for people with epilepsy who attend emergency departments, and their family and friends: study protocol for intervention development and a pilot randomised controlled trial. BMJ Open, 5(7), p. e009040. doi: 10.1136/bmjopen-2015-009040 [DOI:10.1136/bmjopen-2015-009040]
13. Pascual, F. T. et al., 2015. Outpatient education reduces emergency room use by patients with epilepsy. Epilepsy & Behavior, 42, pp. 3–6. doi: 10.1016/j.yebeh.2014.10.024 [DOI:10.1016/j.yebeh.2014.10.024]
14. Rahimian Boogar, E., et al., 2010. [Diabetes self management: Social, demographical and disease factors (Persian)]. Journal of Clini-cal Psychology, 1(4), pp. 43-57.
15. Ratti, V. et al., 2016. The effectiveness of person-centred planning for people with intellectual disabilities: A systematic review. Re-search in Developmental Disabilities, 57, pp. 63–84. doi: 10.1016/j.ridd.2016.06.015 [DOI:10.1016/j.ridd.2016.06.015]
16. Sawangchareon, K., et al., 2013. Moving the self-esteem of people with epilepsy by supportive group: A clinical trial. Journal of Car-ing Sciences, 2(4), pp. 329-35. doi: 10.5681/jcs.2013.039
17. Tol, A., et al., 2012. [Relation between empowerment of diabetes control and adoption of self-management behaviors and its related fac-tors among type 2 diabetic patients (Persian)]. Razi Journal of Medical Sciences, 19(98), pp. 11-8.
18. Walker, E. R. et al., 2012. Social support for self-management behaviors among people with epilepsy: A content analysis of the We-bEase program. Epilepsy & Behavior, 23(3), pp. 285–90. doi: 10.1016/j.yebeh.2012.01.006 [DOI:10.1016/j.yebeh.2012.01.006]
19. Yadollahi, S. et al., 2015. [Correlation between Epilepsy Self-Management Behaviors and Seizure Frequency among Patients with Epilepsy in Iran Epilepsy Association (Persian)]. Preventive Care in Nursing & Midwifery Journal, 5(1), pp. 59-70.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |