Fri, Apr 4, 2025
[Archive]
Volume 4, Issue 2 (Spring 2018 -- 2018)
JCCNC 2018, 4(2): 104-111 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mansoori M, Shegarf-Nakhaie M, Rakhshani M H, Koushan M. Reduction of the Incidence of Delirium in CCU: A Controlled Clinical Trial. JCCNC 2018; 4 (2) :104-111
URL: http://jccnc.iums.ac.ir/article-1-170-en.html
URL: http://jccnc.iums.ac.ir/article-1-170-en.html
1- Department of Nursing, Vasei Hospital, Sabzevar University of Medical Sciences, Sabzevar, Iran. , a.dehnabi95@gmail.com
2- Department of Psychiatry, Faculty of Medicine, Sabzevar University of Medical Sciences, Sabzevar, Iran.
3- Department of Statistics and Epidemiology, School of Public Health, Sabzevar University of Medical Sciences, Sabzevar, Iran.
4- Department of Nursing, Faculty of Nursing and Midwifery, Sabzevar University of Medical Sciences, Sabzevar, Iran.
2- Department of Psychiatry, Faculty of Medicine, Sabzevar University of Medical Sciences, Sabzevar, Iran.
3- Department of Statistics and Epidemiology, School of Public Health, Sabzevar University of Medical Sciences, Sabzevar, Iran.
4- Department of Nursing, Faculty of Nursing and Midwifery, Sabzevar University of Medical Sciences, Sabzevar, Iran.
Full-Text [PDF 564 kb]
(1355 Downloads)
| Abstract (HTML) (3448 Views)
4. Discussion
Based on the study results the occurrence rate of delirium has reduced due to the environmental modifications in CCU. These modifications included providing suitable lighting, eliminating noise, encouraging medical staff to promote favorable conditions for the patient’s sleep, describing the equipment alarms to the patient, allowing relatives to visit the patient outside the regular visiting hours. In addition, the patient’s relatives were allowed to bring patient’s glasses, hearing aids and cane so that the patient can have a normal and full life like outside the hospital. Finally the hospital provided a telephone number to the family so that they can talk to the patient in the presence of the researcher at the ward.
A clinical trial by Zolfaghari et al. (2012) Investigated the effect of a multifactorial intervention program on the prevention of delirium among 90 patients who underwent an elective open heart surgery during their stay at Cardiac Surgical Wards of Imam Khomeini Hospital. They showed that the prevalence rate of delirium was 35.6% in the control group. However, the multifactorial intervention was associated with 11.1% reduction in the delirium occurrence rate. Their study also confirmed that the modification of the sensory stimulations can lead to a significant reduction of the delirium rate among the patients hospitalized at CCUs.
In another randomized clinical trial study, Marcontonio et al. (2002) studied the reduction of delirium among the patients with hip fracture. The study was performed on 126 patients (62 in the experimental group, 64 in the control group) who suffered from hip fracture and were taken to the emergency room of Boston Hospital in the United States. The intervention consisted of a large array of measures including environmental modifications such as putting a clock and a calendar at the patient’s sight, allowing controlled visits, reducing noises and alarms in the ward, using moderate lighting, providing a radio, glasses, and hearing aids if needed, and allowing the patients to get out of the bed early.
The obtained results suggested that these interventions have led to a significant reduction of delirium occurrence rate in the experimental group. More specifically, out of 64 patients in the control group, 32 (50%) suffered from delirium, while, out of 62 patients in the experimental group, only 20 (32%) suffered from delirium (P=0.04) (Marcantonio et al. 2002). Their results are consistent with the present study results and confirm the impact of adjusted environment on the reduction of delirium in patients in the special hospital wards.
A study by Naughton et al. (2005) on internal patients, showed that the incidence of delirium in the first stage and before the intervention was 40.9%, and 22.7% at 4 months after intervention, and 19%, at 9 months after the intervention. Also, the study of Vidan et al. Conducted on patients admitted to the elderly and the public health sector, showed that the incidence of delirium reduced in the test group, compared to the control group (7.11% vs. 18.5%) (Tabet et al. 2005). In a study by Modabernia, Khalkhali and Najafi (2002) On patients admitted to the special department of heart, the incidence of delirium was reported as 13.13%. Interventions in the above studies mainly aimed at modifying the risk factors for delirium and informing the care staff in the early detection of delirium, which are consistent with the present study results.
Kalani, Tavangar and Rahimi (2013) Examined the effect of nursing measures on the occurrence rate of delirium among the patients hospitalized at CCUs of Shiraz hospitals. This randomized clinical trial was performed on 120 patients (60 in the control group, 60 in the experimental group) hospitalized at the CCUs of the state hospitals in Shiraz. Their results showed no statistically significant differences between the 2 groups, with one case of delirium observed in the control group and no delirium cases occurring in the experimental group. It seems that the inappropriate exclusion criteria used in that study could have partly accounted for the low rate of delirium occurrence in both study groups. These results were inconsistent with the results of the present study, which is probably due to the differences in the exclusion criteria.
Martinez et al. (2012) studied the effectiveness of a non-pharmacological intervention in preventing delirium among hospitalized patients. It was a single-blind randomized clinical trial and performed on 287 patients (144 in the experimental group, 143 in the control group) hospitalized at the internal ward of Naval Hospital at Elmirant, USA. In total, 27 cases of delirium, 6 (22%) hyperactive cases, 10 (37%) hypoactive cases, and 11 (41%) mixed cases, were observed. Of the 27 cases of delirium, 8 (5.6%) occurred in the experimental group, while the remaining 19 cases were observed in the control group. The results showed a statistically significant difference (P=0.027). A logarithmic test was performed on the collected data to control the potential effect of other variables (P=0.008). Their study also emphasized the use of non-pharmacological methods to reduce the incidence of delirium.
Van Rompaey et al. (2012) Examined the effect of wearing earplugs at night on the onset of delirium and sleep perception. Their randomized clinical trial included adult intensive care patients in an intervention group of 69 patients sleeping with earplugs at night and a control group of 67 patients sleeping without earplugs. The researchers were blinded during data collection. Eligible patients had an expected length of stay in the ICU for more than 24 hours, were Dutch- or English-speaking and scored a minimum Glasgow Coma Scale of 10. Delirium was assessed using the validated Neecham Scale, sleep perception was reported by the patients in response to 5 questions.
The use of earplugs during the night lowered the incidence of confusion in the studied intensive care patients. A vast improvement was shown by a hazard ratio of 0.47 (95% CI: 0.27 to 0.82). Also, patients sleeping with earplugs developed confusion later than the patients sleeping without earplugs. After the first night in the ICU, patients sleeping with earplugs reported a better sleep perception (Van Rompaey et al. 2012). This study also highlights non-pharmacological methods to reduce the incidence of delirium which is in line with the results of the current study.
The present study results indicate that the modification of sensory stimulations had a statistically positive and significant effect on preventing the occurrence of delirium among the participating patients. These modifications included the presence of the nurse researcher and interacting with the patient, explaining the reason for the patient’s transfer to CCU and the advantages of staying here, familiarizing the patient with the personnel and the atmosphere of the ward, providing a telephone number to the patient’s family members and friends to talk to him/her twice a day, asking them to bring the patient’s necessary items such as, glasses, hearing aids and, cane, so that the patient can continue his/her routines like reading and listening to the radio, and taking into account the patient’s sleep habits, too. Therefore, these measures could be safe methods to reduce the side effects of illnesses and the treatment costs imposed on the medical staff and the patients’ families.
Some factors prolonged the data collection phase of the present study, including not meeting the inclusion criteria, transferring some patients to other hospitals, some patients’ leaving the hospital, patient’s death, and transferring of the patients to other wards (within the first 24 hours of their stay at the ward). Moreover, the limitations set by the hospital for the families to visit their patients were another limitation of this study. There was also no possibility for randomized allocation of the subjects, due to the presence of only one CCU in the hospital.
Implications for practice
The evidence-based results of the present study can help ICU nurses to prevent delirium in the patients by taking measures and modify sensory inputs.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (code: IR.MEDSAB.REC.1394.81) and was registered at the Iranian Registry of Clinical Trials (IRCT2015101424536N1). All the participants meeting the inclusion criteria provided written consent forms before conducting the study.
Funding
This article was the result of MSc. thesis of Moslem Mansoori in Department of Nursing, Sabzevar University of Medical Sciences.
Authors contributions
Authors contribution is as follows: Investigation: Moslem Mansoori and Mohsen Koushan; Writing original draft: Moslem Mansoori, Mohsen Koushan, Mohammad Hasan Rakhshani, and Mohammadreza Shegarf-Nakhaie; Writing, review and editing: Moslem Mansoori and Mohsen Koushan; Funding Acquisition: Mohsen Koushan and Moslem Mansoori; Resources: Moslem Mansoori and Mohsen Koushan; Supervision: Mohammadreza Shegarf-Nakhaie, Mohsen Koushan, and Mohammad Hasan Rakhshani.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
We would like to express our sincere gratitude to the Research Department of Sabzevar Medical University, the Dean of the Nursing Faculty, and the Manager of Vasei Hospital, the medical staff and the head nurse of the hospital, also the patients and their families for their cooperation in conducting this research.
References
● Delirium in patients hospitalized in coronary care units are common.
● Delirium can be decreased in these patients by providing suitable environmental modifications.
● These modification include more cooperation of the medical staff, describing the environmental conditions, and allowing relatives to see the patient.
Plain Language Summary
Delirium is one of the oldest known medical disorders, characterized by acute and swirling start (several hours to several days) disturbances in consciousness, orientation, memory, thinking, perception, and behavior. The patients hospitalized at coronary care units are susceptible to delirium which is responsible for an increased death rate among these patients. The results obtained in the present study confirmed that the modification of the sensory stimulations can significantly reduce the delirium rate among the patients hospitalized at coronary care units.
● Delirium can be decreased in these patients by providing suitable environmental modifications.
● These modification include more cooperation of the medical staff, describing the environmental conditions, and allowing relatives to see the patient.
Plain Language Summary
Delirium is one of the oldest known medical disorders, characterized by acute and swirling start (several hours to several days) disturbances in consciousness, orientation, memory, thinking, perception, and behavior. The patients hospitalized at coronary care units are susceptible to delirium which is responsible for an increased death rate among these patients. The results obtained in the present study confirmed that the modification of the sensory stimulations can significantly reduce the delirium rate among the patients hospitalized at coronary care units.
Full-Text: (974 Views)
1. Background
Delirium is a syndrome resulting from impairments in the central nervous system. It is associated with an array of neuropsychiatric, and bio-behavioral symptoms (Inouye 2006). It initiates with impairments in cognitive functioning, disturbance in consciousness, adverse physiological and psychomotor changes, along with instability in the central autonomic nervous system (Inouye 2006; Clary & Krishnan 2001).
Delirium is associated with adverse consequences like death (Kiely et al. 2007). Old age and dementia are among important predisposing factors which make individuals susceptible to delirium. In addition, infection, hypoxia, sleep disturbances, and severe illnesses are considered important precipitating factors for this disease (Yamaguchi, Tsukioka & Kishi 2014). Delirium has a prevalence rate of 10% to 80% among the severely and terminally ill hospitalized patients (Uguz et al. 2010). In different countries, delirium has a prevalence of 10% to 40% among the patients in Coronary Care Units (CCUs) (Kalani, Tavangar & Rahimi 2013).
Patients suffering from delirium during hospitalization have a 62% higher chance of death, compared to those without delirium (Leslie et al. 2005). McPherson et al. Reported a prevalence rate of 29% among the patients at CCU with a death rate of 9%, while the prevalence rate for the patients at Intensive Care Units (ICUs) was 24% with a death rate of 0. Similarly, in another study, the prevalence rate of delirium among the patients at ICUs was reported 27.8 % in Japan (McPherson et al. 2013). A study in Iran showed that delirium had a prevalence rate of 13.4% among the patients at CCUs (Modabernia, Khalkhali & Najafi 2002).
Studies show that the prevalence rate of delirium at ICU is 89%, which causes a marked increase of 39% in the treatment costs (Zolfaghari et al. 2012). Delirium imposed an annual cost of 4 to 19 billion dollars in the United States (Barr et al. 2013). Moreover, in the long run, delirium can lead to permanent cognitive disorders like dementia (Pisani et al. 2009).
Patients become more susceptible and vulnerable to delirium by a number of factors such as bed rest, fewer visitors, less agitation, lower cardiac output, electrolyte imbalance, infections, treatment with sedatives and opiates, fear of death and illness, and sensory deprivation (separation from the family, limited oral communication, and reduced orientation) (Tsios & Alichanidou 2008). Thus, it seems that providing an appropriate level of sensory stimulation at CCU can reduce the risk for delirium.
A number of studies have investigated the potential effects of various nursing interventions including reducing noise, providing moderate lighting and suitable conditions at night (for the patients to have sufficient sleep) on delirium occurrence. Zolfaghari et al. Reported that providing instructions to the clinical staff could reduce the incidence of delirium up to 25% among the patients who underwent open heart surgery (Zolfaghari et al. 2012). Moreover, Marcantonio et al. (2002) concluded that putting a clock or calendar at the patient’s bedside, controlled visits, reducing noise, alarms, and overhead paging, moderate lighting, providing a radio, glasses and hearing aids for the patient, and allowing the patient to leave the bed early, may reduce the rate of delirium occurrence among the patients who underwent hip fracture surgery (Marcantonio et al. 2002).
In a similar study, Tomas Martins et al. Concluded that training the medical staff and the patient’s family, along with the environmental modifications could reduce the delirium occurrence rate (Martinez et al. 2012). However, Kalani et al. Found that listening to the radio and visiting relatives were not effective in delirium prevention among the patients in CCU (Kalani, Tavangar & Rahimi 2013). Hence, this study aimed to determine the potential effect of modifying sensory stimuli in reducing the occurrence of delirium among the patients hospitalized in CCU. It our study results confirm the positive effect of modifying sensory stimulation, the medical staff working at CCU wards may take the necessary measures to provide a favorable environment along with suitable sensory stimulation for the patients to reduce the occurrence rate of delirium among them.
2. Materials and Methods
This was a clinical trial study with control group. The study population consisted of the patients hospitalized in the CCU of Vasei Hospital at Sabzevar City, Iran. A sample of 80 subjects was selected and assigned into 2 equal groups (at a significance level of 5% and a test power of 80%). The inclusion criteria consisted of being 18 years or older and being able to communicate in Persian. Subjects were excluded from the study if they suffered from a low consciousness level, delirium, or any brain syndromes and brain vessel problems, and having a history of taking psychiatric medication in the last 6 months. Moreover, patients with visual-auditory deficits, and those who had undergone Cardiopulmonary Resuscitation (CPR) in the previous 24 hours but were still unconscious were excluded from the study. The standard instruments used in the present study were as follows:
Richmond Agitation-Sedation Scale (RASS)
It was used as a research unit selection form for alertness (sleepiness to restlessness). This is a 10-point scale translated by Tedris et al. (2009). It has a 1-digit numerical structure and prevents the complexity of multiple criteria. It can be completed within 30 to 60 seconds using 3 consecutive steps: observation, response to auditory stimuli and reactions to physical stimuli. First, restlessness, unrest and then drowsiness are evaluated. If the samples were taken scores -4 and -5 or +3 and +4 were not included in the study.
NeeCham 30-Point Confusion Tool
It was administered at the beginning of the study to check the participant’s delirium. NeeCham Tool consists of three basic (Main) parts of: process (0 to 14 points), behavior (0 to 10 points), and physiological control (0 to 6 points). Based on the obtained scores, the patients are categorized into 4 classes: normal, not confused (27-30), not confused but at risk of delirium-confusion (25-26), mild delirium-confusion (20-24), moderate to severe delirium-confusion (0-19).
On average, it takes 8 to 10 minutes for a nurse to complete the scale based on his or her daily observations and activities. This questionnaire (tool) has been validated with DSM III-R diagnosis and the 24-hour daily reports of nurses, and thus is a reliable and valid tool to measure the delirium status of the patients by nurses in CCUs. Moreover, it is used for non-intubated patients. This tool has the potential to identify patients susceptible to delirium, and thus enable the medical staff to take suitable preventive measures to reduce the occurrence rate of delirium. This tool with a sensitivity of 87% and a specificity of 95% is the most suitable ones for the assessment of CCU patients.
The reliability and validity of this tool were established by Janati and associates. In order to measure the reliability of this tool, internal consistency and balance were used. Internal consistency was evaluated using Cronbach’s alpha coefficient on 30 patients (0.96). In order to measure the balance, 2 nurses independently evaluated 15 patients using the questionnaire without being aware of the assessment score. The Pearson coefficient was calculated as 0.99.
Since all the subjects were hospitalized in the same ward, assigning the subjects into 2 groups and running the study at the same time on both groups was not possible. Therefore, the first 40 subjects hospitalized at the CCU were randomly considered as the control group and their delirium status was measured without any medical interventions. The next 40 patients were considered as the experimental group and received the pre-planned interventions.
More specifically, a set of predetermined environmental modifications including suitable lighting, low noise, and modified medical and nursing measures were prepared to prevent sleep disturbances of the patients. Also, the staff talked to the patients and described the alarming sounds of the equipment. The patients were allowed to see their relatives and friends outside the regular visiting hours. The patients’ family members were asked to bring the patient’s glasses, hearing aids and canes, so that the patients could behave as normally as before. Additionally, the patients were provided telephone numbers to talk to their families as desired.
Nursing care was routinely administered in both groups. Most studies have reported the highest delirium incidence within 48 to 72 hours after hospital admission. Therefore, every patient was examined for up to 3 days, two times per day (in the morning and in the afternoon), since their admission. Only one CCU was available in the hospitals of the city. Therefore, according to the lottery, the control group was first examined. NeeCham Questionnaire was completed for every patient twice a day (morning and afternoon) for 3 consecutive days for both groups.
The collected data were analyzed by descriptive and inferential statistical tests (Statistical Analysis System), using SAS. In order to describe the quantitative variables, the Mean±SD or the Inter Quartile Range (IQR) were used, according to the conditions. For qualitative variables, frequency report (percentages) was used. The Chi-Square and Shapiro-Wilk Tests were used to check the normal distribution of the data. To compare the mean score of quantitative variables between the 2 groups, we used the Independent t test or its nonparametric equivalent, i.e. Mann-Whitney Test. We used a logarithmic link to fit the model, in order to control the effect of variables on each other.
3. Results
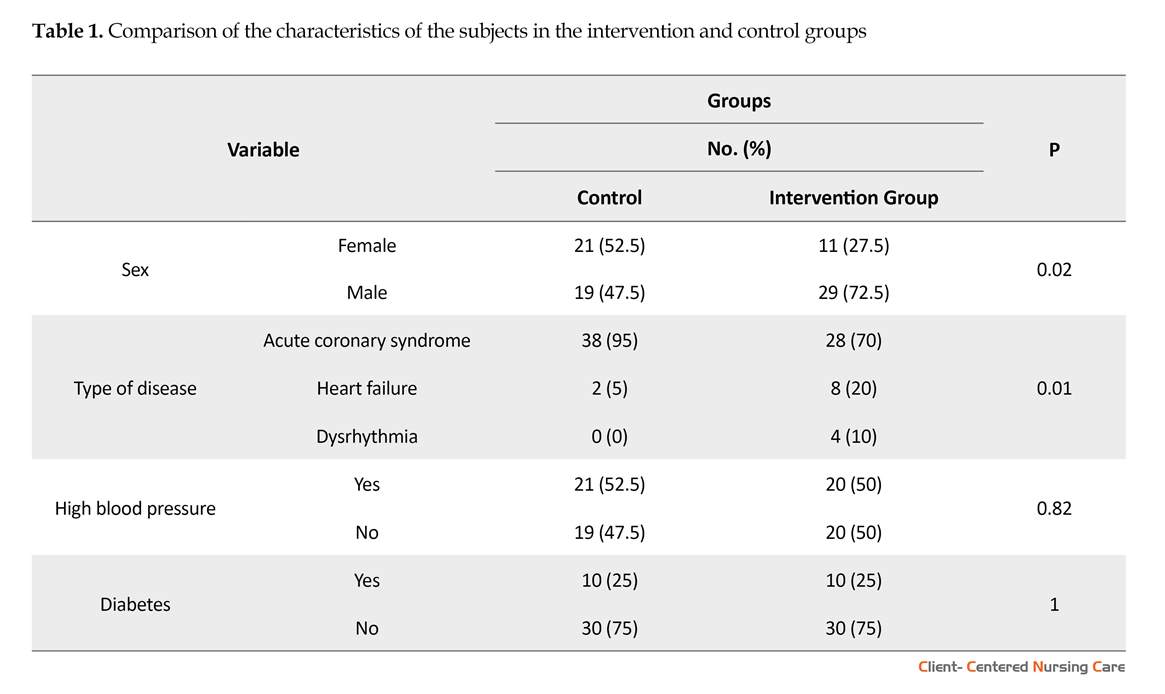
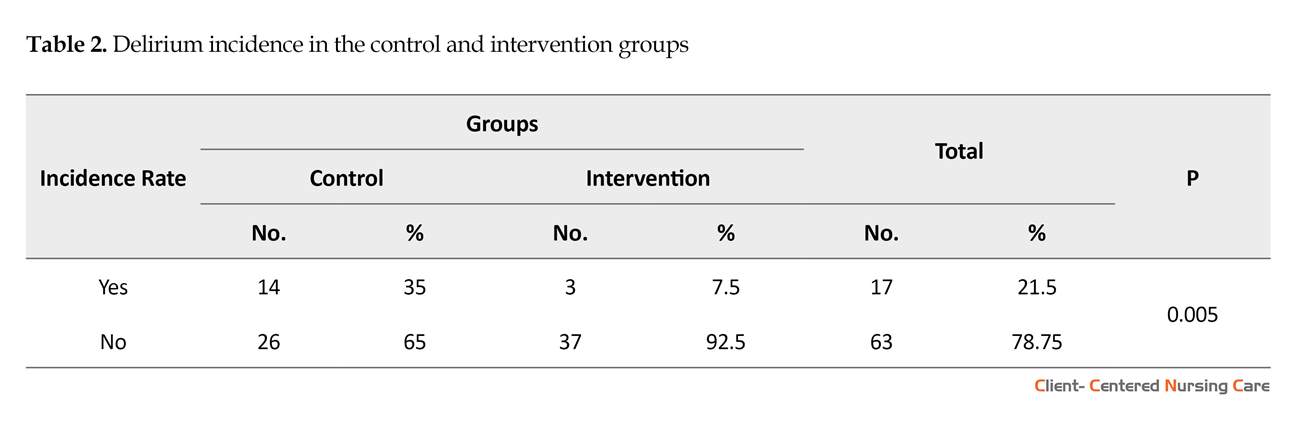
The results of descriptive statistical analyses performed on the demographic data collected from the subjects in both groups showed that the subjects aged between 35 and 92 years, with the Mean±SD age of 62.37±13.2, and 62±13.65 years, for the control and experimental groups, respectively. The Independent t-test result indicate that the 2 groups were homogeneous, in terms of age. Moreover, the results of Mann-Whitney U Test, Chi-square test and Fisher Exact test showed no statistically significant differences between the 2 groups in terms of marital status, educational level, diabetes and hypertension (Table 1). Nevertheless, the 2 groups were different in terms of sex. However, the study of the logarithmic model of the data indicate that the difference has no significant effects on the possible influence of the intervention on delirium, in the presence of the other variables. Overall, 14 (35%) cases of delirium were observed in the control group, while there were only 3 (7.5%) cases of delirium were reported in the experimental group.
The results of Fisher Exact test revealed a significant difference between the 2 groups, in terms of the delirium occurrence rate (P=0.005) (Table 2). Moreover, there were 5 (12.5 %) cases of hypoactive, 5 (12.5%) cases of hyperactive, and 4 (10%) cases of mixed delirium, in the control group. However, there were 2 (5%) cases of hypo active, 1 (2.5%) case of hyperactive, and no mixed cases in the experimental group. Fisher Exact test results showed a significant difference between the 2 groups in terms of the occurrence of the 3 subtypes of delirium (P=0.001) (Table 3). In addition, the results suggested that, the intervention had no significant effect on the delirium occurrence rate, in the first 24 hours. However, the analysis of the data based on logarithmic link in the fit model showed that providing the intervention during the second (P=0.003) and third (P=0.003) days, led to a statistically significant difference in the cognitive score of the patients, measured by Neecham Scale.
Delirium is a syndrome resulting from impairments in the central nervous system. It is associated with an array of neuropsychiatric, and bio-behavioral symptoms (Inouye 2006). It initiates with impairments in cognitive functioning, disturbance in consciousness, adverse physiological and psychomotor changes, along with instability in the central autonomic nervous system (Inouye 2006; Clary & Krishnan 2001).
Delirium is associated with adverse consequences like death (Kiely et al. 2007). Old age and dementia are among important predisposing factors which make individuals susceptible to delirium. In addition, infection, hypoxia, sleep disturbances, and severe illnesses are considered important precipitating factors for this disease (Yamaguchi, Tsukioka & Kishi 2014). Delirium has a prevalence rate of 10% to 80% among the severely and terminally ill hospitalized patients (Uguz et al. 2010). In different countries, delirium has a prevalence of 10% to 40% among the patients in Coronary Care Units (CCUs) (Kalani, Tavangar & Rahimi 2013).
Patients suffering from delirium during hospitalization have a 62% higher chance of death, compared to those without delirium (Leslie et al. 2005). McPherson et al. Reported a prevalence rate of 29% among the patients at CCU with a death rate of 9%, while the prevalence rate for the patients at Intensive Care Units (ICUs) was 24% with a death rate of 0. Similarly, in another study, the prevalence rate of delirium among the patients at ICUs was reported 27.8 % in Japan (McPherson et al. 2013). A study in Iran showed that delirium had a prevalence rate of 13.4% among the patients at CCUs (Modabernia, Khalkhali & Najafi 2002).
Studies show that the prevalence rate of delirium at ICU is 89%, which causes a marked increase of 39% in the treatment costs (Zolfaghari et al. 2012). Delirium imposed an annual cost of 4 to 19 billion dollars in the United States (Barr et al. 2013). Moreover, in the long run, delirium can lead to permanent cognitive disorders like dementia (Pisani et al. 2009).
Patients become more susceptible and vulnerable to delirium by a number of factors such as bed rest, fewer visitors, less agitation, lower cardiac output, electrolyte imbalance, infections, treatment with sedatives and opiates, fear of death and illness, and sensory deprivation (separation from the family, limited oral communication, and reduced orientation) (Tsios & Alichanidou 2008). Thus, it seems that providing an appropriate level of sensory stimulation at CCU can reduce the risk for delirium.
A number of studies have investigated the potential effects of various nursing interventions including reducing noise, providing moderate lighting and suitable conditions at night (for the patients to have sufficient sleep) on delirium occurrence. Zolfaghari et al. Reported that providing instructions to the clinical staff could reduce the incidence of delirium up to 25% among the patients who underwent open heart surgery (Zolfaghari et al. 2012). Moreover, Marcantonio et al. (2002) concluded that putting a clock or calendar at the patient’s bedside, controlled visits, reducing noise, alarms, and overhead paging, moderate lighting, providing a radio, glasses and hearing aids for the patient, and allowing the patient to leave the bed early, may reduce the rate of delirium occurrence among the patients who underwent hip fracture surgery (Marcantonio et al. 2002).
In a similar study, Tomas Martins et al. Concluded that training the medical staff and the patient’s family, along with the environmental modifications could reduce the delirium occurrence rate (Martinez et al. 2012). However, Kalani et al. Found that listening to the radio and visiting relatives were not effective in delirium prevention among the patients in CCU (Kalani, Tavangar & Rahimi 2013). Hence, this study aimed to determine the potential effect of modifying sensory stimuli in reducing the occurrence of delirium among the patients hospitalized in CCU. It our study results confirm the positive effect of modifying sensory stimulation, the medical staff working at CCU wards may take the necessary measures to provide a favorable environment along with suitable sensory stimulation for the patients to reduce the occurrence rate of delirium among them.
2. Materials and Methods
This was a clinical trial study with control group. The study population consisted of the patients hospitalized in the CCU of Vasei Hospital at Sabzevar City, Iran. A sample of 80 subjects was selected and assigned into 2 equal groups (at a significance level of 5% and a test power of 80%). The inclusion criteria consisted of being 18 years or older and being able to communicate in Persian. Subjects were excluded from the study if they suffered from a low consciousness level, delirium, or any brain syndromes and brain vessel problems, and having a history of taking psychiatric medication in the last 6 months. Moreover, patients with visual-auditory deficits, and those who had undergone Cardiopulmonary Resuscitation (CPR) in the previous 24 hours but were still unconscious were excluded from the study. The standard instruments used in the present study were as follows:
Richmond Agitation-Sedation Scale (RASS)
It was used as a research unit selection form for alertness (sleepiness to restlessness). This is a 10-point scale translated by Tedris et al. (2009). It has a 1-digit numerical structure and prevents the complexity of multiple criteria. It can be completed within 30 to 60 seconds using 3 consecutive steps: observation, response to auditory stimuli and reactions to physical stimuli. First, restlessness, unrest and then drowsiness are evaluated. If the samples were taken scores -4 and -5 or +3 and +4 were not included in the study.
NeeCham 30-Point Confusion Tool
It was administered at the beginning of the study to check the participant’s delirium. NeeCham Tool consists of three basic (Main) parts of: process (0 to 14 points), behavior (0 to 10 points), and physiological control (0 to 6 points). Based on the obtained scores, the patients are categorized into 4 classes: normal, not confused (27-30), not confused but at risk of delirium-confusion (25-26), mild delirium-confusion (20-24), moderate to severe delirium-confusion (0-19).
On average, it takes 8 to 10 minutes for a nurse to complete the scale based on his or her daily observations and activities. This questionnaire (tool) has been validated with DSM III-R diagnosis and the 24-hour daily reports of nurses, and thus is a reliable and valid tool to measure the delirium status of the patients by nurses in CCUs. Moreover, it is used for non-intubated patients. This tool has the potential to identify patients susceptible to delirium, and thus enable the medical staff to take suitable preventive measures to reduce the occurrence rate of delirium. This tool with a sensitivity of 87% and a specificity of 95% is the most suitable ones for the assessment of CCU patients.
The reliability and validity of this tool were established by Janati and associates. In order to measure the reliability of this tool, internal consistency and balance were used. Internal consistency was evaluated using Cronbach’s alpha coefficient on 30 patients (0.96). In order to measure the balance, 2 nurses independently evaluated 15 patients using the questionnaire without being aware of the assessment score. The Pearson coefficient was calculated as 0.99.
Since all the subjects were hospitalized in the same ward, assigning the subjects into 2 groups and running the study at the same time on both groups was not possible. Therefore, the first 40 subjects hospitalized at the CCU were randomly considered as the control group and their delirium status was measured without any medical interventions. The next 40 patients were considered as the experimental group and received the pre-planned interventions.
More specifically, a set of predetermined environmental modifications including suitable lighting, low noise, and modified medical and nursing measures were prepared to prevent sleep disturbances of the patients. Also, the staff talked to the patients and described the alarming sounds of the equipment. The patients were allowed to see their relatives and friends outside the regular visiting hours. The patients’ family members were asked to bring the patient’s glasses, hearing aids and canes, so that the patients could behave as normally as before. Additionally, the patients were provided telephone numbers to talk to their families as desired.
Nursing care was routinely administered in both groups. Most studies have reported the highest delirium incidence within 48 to 72 hours after hospital admission. Therefore, every patient was examined for up to 3 days, two times per day (in the morning and in the afternoon), since their admission. Only one CCU was available in the hospitals of the city. Therefore, according to the lottery, the control group was first examined. NeeCham Questionnaire was completed for every patient twice a day (morning and afternoon) for 3 consecutive days for both groups.
The collected data were analyzed by descriptive and inferential statistical tests (Statistical Analysis System), using SAS. In order to describe the quantitative variables, the Mean±SD or the Inter Quartile Range (IQR) were used, according to the conditions. For qualitative variables, frequency report (percentages) was used. The Chi-Square and Shapiro-Wilk Tests were used to check the normal distribution of the data. To compare the mean score of quantitative variables between the 2 groups, we used the Independent t test or its nonparametric equivalent, i.e. Mann-Whitney Test. We used a logarithmic link to fit the model, in order to control the effect of variables on each other.
3. Results
The results of descriptive statistical analyses performed on the demographic data collected from the subjects in both groups showed that the subjects aged between 35 and 92 years, with the Mean±SD age of 62.37±13.2, and 62±13.65 years, for the control and experimental groups, respectively. The Independent t-test result indicate that the 2 groups were homogeneous, in terms of age. Moreover, the results of Mann-Whitney U Test, Chi-square test and Fisher Exact test showed no statistically significant differences between the 2 groups in terms of marital status, educational level, diabetes and hypertension (Table 1). Nevertheless, the 2 groups were different in terms of sex. However, the study of the logarithmic model of the data indicate that the difference has no significant effects on the possible influence of the intervention on delirium, in the presence of the other variables. Overall, 14 (35%) cases of delirium were observed in the control group, while there were only 3 (7.5%) cases of delirium were reported in the experimental group.
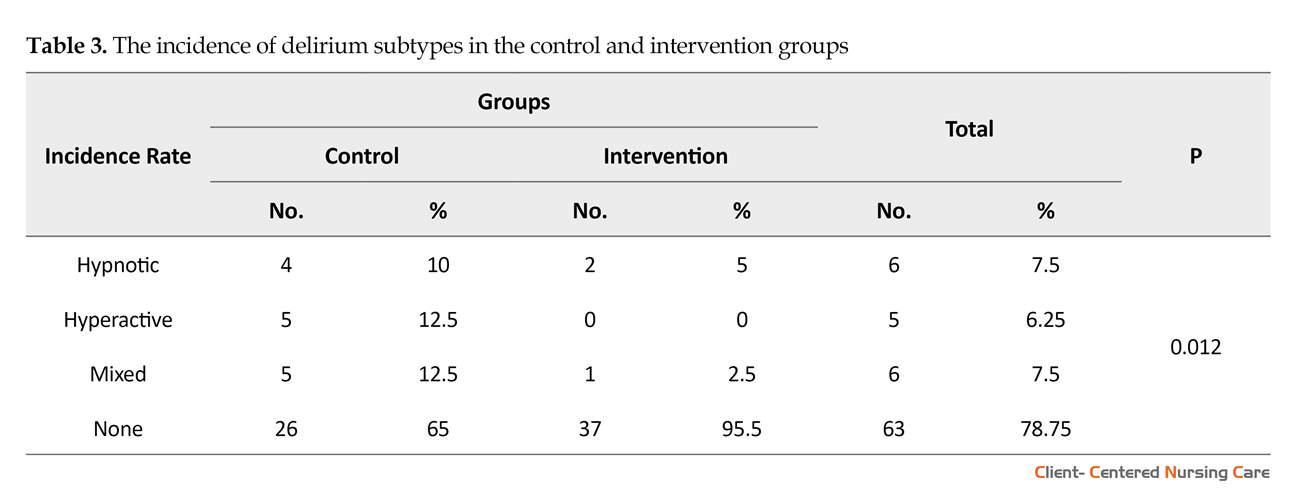
The results of Fisher Exact test revealed a significant difference between the 2 groups, in terms of the delirium occurrence rate (P=0.005) (Table 2). Moreover, there were 5 (12.5 %) cases of hypoactive, 5 (12.5%) cases of hyperactive, and 4 (10%) cases of mixed delirium, in the control group. However, there were 2 (5%) cases of hypo active, 1 (2.5%) case of hyperactive, and no mixed cases in the experimental group. Fisher Exact test results showed a significant difference between the 2 groups in terms of the occurrence of the 3 subtypes of delirium (P=0.001) (Table 3). In addition, the results suggested that, the intervention had no significant effect on the delirium occurrence rate, in the first 24 hours. However, the analysis of the data based on logarithmic link in the fit model showed that providing the intervention during the second (P=0.003) and third (P=0.003) days, led to a statistically significant difference in the cognitive score of the patients, measured by Neecham Scale.
4. Discussion
Based on the study results the occurrence rate of delirium has reduced due to the environmental modifications in CCU. These modifications included providing suitable lighting, eliminating noise, encouraging medical staff to promote favorable conditions for the patient’s sleep, describing the equipment alarms to the patient, allowing relatives to visit the patient outside the regular visiting hours. In addition, the patient’s relatives were allowed to bring patient’s glasses, hearing aids and cane so that the patient can have a normal and full life like outside the hospital. Finally the hospital provided a telephone number to the family so that they can talk to the patient in the presence of the researcher at the ward.
A clinical trial by Zolfaghari et al. (2012) Investigated the effect of a multifactorial intervention program on the prevention of delirium among 90 patients who underwent an elective open heart surgery during their stay at Cardiac Surgical Wards of Imam Khomeini Hospital. They showed that the prevalence rate of delirium was 35.6% in the control group. However, the multifactorial intervention was associated with 11.1% reduction in the delirium occurrence rate. Their study also confirmed that the modification of the sensory stimulations can lead to a significant reduction of the delirium rate among the patients hospitalized at CCUs.
In another randomized clinical trial study, Marcontonio et al. (2002) studied the reduction of delirium among the patients with hip fracture. The study was performed on 126 patients (62 in the experimental group, 64 in the control group) who suffered from hip fracture and were taken to the emergency room of Boston Hospital in the United States. The intervention consisted of a large array of measures including environmental modifications such as putting a clock and a calendar at the patient’s sight, allowing controlled visits, reducing noises and alarms in the ward, using moderate lighting, providing a radio, glasses, and hearing aids if needed, and allowing the patients to get out of the bed early.
The obtained results suggested that these interventions have led to a significant reduction of delirium occurrence rate in the experimental group. More specifically, out of 64 patients in the control group, 32 (50%) suffered from delirium, while, out of 62 patients in the experimental group, only 20 (32%) suffered from delirium (P=0.04) (Marcantonio et al. 2002). Their results are consistent with the present study results and confirm the impact of adjusted environment on the reduction of delirium in patients in the special hospital wards.
A study by Naughton et al. (2005) on internal patients, showed that the incidence of delirium in the first stage and before the intervention was 40.9%, and 22.7% at 4 months after intervention, and 19%, at 9 months after the intervention. Also, the study of Vidan et al. Conducted on patients admitted to the elderly and the public health sector, showed that the incidence of delirium reduced in the test group, compared to the control group (7.11% vs. 18.5%) (Tabet et al. 2005). In a study by Modabernia, Khalkhali and Najafi (2002) On patients admitted to the special department of heart, the incidence of delirium was reported as 13.13%. Interventions in the above studies mainly aimed at modifying the risk factors for delirium and informing the care staff in the early detection of delirium, which are consistent with the present study results.
Kalani, Tavangar and Rahimi (2013) Examined the effect of nursing measures on the occurrence rate of delirium among the patients hospitalized at CCUs of Shiraz hospitals. This randomized clinical trial was performed on 120 patients (60 in the control group, 60 in the experimental group) hospitalized at the CCUs of the state hospitals in Shiraz. Their results showed no statistically significant differences between the 2 groups, with one case of delirium observed in the control group and no delirium cases occurring in the experimental group. It seems that the inappropriate exclusion criteria used in that study could have partly accounted for the low rate of delirium occurrence in both study groups. These results were inconsistent with the results of the present study, which is probably due to the differences in the exclusion criteria.
Martinez et al. (2012) studied the effectiveness of a non-pharmacological intervention in preventing delirium among hospitalized patients. It was a single-blind randomized clinical trial and performed on 287 patients (144 in the experimental group, 143 in the control group) hospitalized at the internal ward of Naval Hospital at Elmirant, USA. In total, 27 cases of delirium, 6 (22%) hyperactive cases, 10 (37%) hypoactive cases, and 11 (41%) mixed cases, were observed. Of the 27 cases of delirium, 8 (5.6%) occurred in the experimental group, while the remaining 19 cases were observed in the control group. The results showed a statistically significant difference (P=0.027). A logarithmic test was performed on the collected data to control the potential effect of other variables (P=0.008). Their study also emphasized the use of non-pharmacological methods to reduce the incidence of delirium.
Van Rompaey et al. (2012) Examined the effect of wearing earplugs at night on the onset of delirium and sleep perception. Their randomized clinical trial included adult intensive care patients in an intervention group of 69 patients sleeping with earplugs at night and a control group of 67 patients sleeping without earplugs. The researchers were blinded during data collection. Eligible patients had an expected length of stay in the ICU for more than 24 hours, were Dutch- or English-speaking and scored a minimum Glasgow Coma Scale of 10. Delirium was assessed using the validated Neecham Scale, sleep perception was reported by the patients in response to 5 questions.
The use of earplugs during the night lowered the incidence of confusion in the studied intensive care patients. A vast improvement was shown by a hazard ratio of 0.47 (95% CI: 0.27 to 0.82). Also, patients sleeping with earplugs developed confusion later than the patients sleeping without earplugs. After the first night in the ICU, patients sleeping with earplugs reported a better sleep perception (Van Rompaey et al. 2012). This study also highlights non-pharmacological methods to reduce the incidence of delirium which is in line with the results of the current study.
The present study results indicate that the modification of sensory stimulations had a statistically positive and significant effect on preventing the occurrence of delirium among the participating patients. These modifications included the presence of the nurse researcher and interacting with the patient, explaining the reason for the patient’s transfer to CCU and the advantages of staying here, familiarizing the patient with the personnel and the atmosphere of the ward, providing a telephone number to the patient’s family members and friends to talk to him/her twice a day, asking them to bring the patient’s necessary items such as, glasses, hearing aids and, cane, so that the patient can continue his/her routines like reading and listening to the radio, and taking into account the patient’s sleep habits, too. Therefore, these measures could be safe methods to reduce the side effects of illnesses and the treatment costs imposed on the medical staff and the patients’ families.
Some factors prolonged the data collection phase of the present study, including not meeting the inclusion criteria, transferring some patients to other hospitals, some patients’ leaving the hospital, patient’s death, and transferring of the patients to other wards (within the first 24 hours of their stay at the ward). Moreover, the limitations set by the hospital for the families to visit their patients were another limitation of this study. There was also no possibility for randomized allocation of the subjects, due to the presence of only one CCU in the hospital.
Implications for practice
The evidence-based results of the present study can help ICU nurses to prevent delirium in the patients by taking measures and modify sensory inputs.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (code: IR.MEDSAB.REC.1394.81) and was registered at the Iranian Registry of Clinical Trials (IRCT2015101424536N1). All the participants meeting the inclusion criteria provided written consent forms before conducting the study.
Funding
This article was the result of MSc. thesis of Moslem Mansoori in Department of Nursing, Sabzevar University of Medical Sciences.
Authors contributions
Authors contribution is as follows: Investigation: Moslem Mansoori and Mohsen Koushan; Writing original draft: Moslem Mansoori, Mohsen Koushan, Mohammad Hasan Rakhshani, and Mohammadreza Shegarf-Nakhaie; Writing, review and editing: Moslem Mansoori and Mohsen Koushan; Funding Acquisition: Mohsen Koushan and Moslem Mansoori; Resources: Moslem Mansoori and Mohsen Koushan; Supervision: Mohammadreza Shegarf-Nakhaie, Mohsen Koushan, and Mohammad Hasan Rakhshani.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
We would like to express our sincere gratitude to the Research Department of Sabzevar Medical University, the Dean of the Nursing Faculty, and the Manager of Vasei Hospital, the medical staff and the head nurse of the hospital, also the patients and their families for their cooperation in conducting this research.
References
- Barr, J., et al., 2013. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical Care Medicine, 41(1), pp. 263-306. [DOI:10.1097/CCM.0b013e3182783b72] [PMID]
- Clary, G. L., & Krishnan, K. R., 2001. Delirium: Diagnosis, neuropathogenesis, and treatment. Journal of Psychiatric Practice, 7(5), pp. 310-23. [DOI:10.1097/00131746-200109000-00004] [PMID]
- Inouye, S. K., 2006. Delirium in older persons. New England Journal of Medicine, 354(11), pp. 1157-65. [DOI:10.1056/NEJMra052321] [PMID]
- Kalani, Z., Tavangar, H. & Rahimi, A., 2013. [Effectiveness of nursing interventions on incidence of delirium in patients hospitalized to intensive cardiac care units, Shiraz hospitals, 2012 (Persian)]. Medical-Surgical Nursing Journal, 2(3-4), pp. 93-100.
- Kiely, D. K., Jones, R. N., Bergmann, M. A. & Marcantonio, E. R., 2007. Association between psychomotor activity delirium subtypes and mortality among newly admitted postacute facility patients. The Journals of Gerontology, 62(2), pp. 174-9. [DOI:10.1093/gerona/62.2.174]
- Leslie, D. L., et al., 2005. Premature death associated with delirium at 1-year follow-up. Archives of Internal Medicine, 165(14), pp. 1657-62. [DOI:10.1001/archinte.165.14.1657] [PMID]
- Marcantonio, E., et al., 2002. Delirium severity and psychomotor types: Their relationship with outcomes after hip fracture repair. Journal of the American Geriatrics Society, 50(5), pp. 850-7. [DOI:10.1046/j.1532-5415.2002.50210.x] [PMID]
- Martinez, F. T., et al., 2012. Preventing delirium in an acute hospital using a non-pharmacological intervention. Age and Ageing, 41(5), pp. 629-34. [DOI:10.1093/ageing/afs060] [PMID]
- McPherson J. A., et al., 2013. Delirium in the cardiovascular intensive care unit: Exploring modifiable risk factors. Critcal Care Medicine, 41(2), pp. 405-13. [DOI:10.1097/CCM.0b013e31826ab49b] [PMID] [PMCID]
- Modabernia, M. J., Khalkhali, S. M. R. & Najafi, K., 2002. [Delirium in CCU (Persian)]. Journal of Guilan University of Medical Sciences, 11(41), pp. 1-6.
- Naughton, B. J., et al., 2005. A multifactorial intervention to reduce prevalence of delirium and shorten hospital length of stay. Journal of the American Geriatrics Society, 53(1), pp. 18-23. [DOI:10.1111/j.1532-5415.2005.53005.x] [PMID]
- Pisani, M. A., et al., 2009. Days of delirium are associated with 1-year mortality in an older intensive care unit population. American Journal of Respiratory and Critical Care Medicine, 180(11), pp. 1092-7. [DOI:10.1164/rccm.200904-0537OC] [PMID] [PMCID]
- Tabet, N., et al., 2005. An educational intervention can prevent delirium on acute medical wards. Age and Ageing, 34(2), pp. 152-6. [DOI:10.1093/ageing/afi031] [PMID]
- Tadrisi, S. et al., 2009. Richmond agitation¨Csedation scale validity and reliability in intensive care unit adult patients Persian version. Journal of Critical Care Nursing, 2(1), pp. 15-21.
- Tsios, A. & Alichanidou, E., 2009. Coronary Care Unit (CCU) psychosis syndrome. Hospital Chronicles, 4(3), pp. 32-4.
- Uguz, F., et al., 2010. Delirium following acute myocardial infarction: Incidence, clinical profiles, and predictors. Perspectives in Psychiatric Care, 46(2), pp. 135-42. [DOI:10.1111/j.1744-6163.2010.00249.x] [PMID]
- Van Rompaey, B., et al., 2012. The effect of earplugs during the night on the onset of delirium and sleep perception: A randomized controlled trial in intensive care patients. Critical Care, 16(3), p. R73. [DOI:10.1186/cc11330] [PMID] [PMCID]
- Yamaguchi, T., Tsukioka, E. & Kishi, Y., 2014. Outcomes after delirium in a Japanese intensive care unit. General Hospital Psychiatry, 36(6), pp. 634-6. [DOI:10.1016/j.genhosppsych.2014.09.006] [PMID]
- Zolfaghari, M., et al., 2012. [Effectiveness of a multifactor educational intervention on delirium incidence and length of stay in patients with cardiac surgery (Persian)]. Journal of Hayat, 18(1), pp. 67-78.
Type of Study: Research |
Subject:
Special
Received: 2017/12/2 | Accepted: 2018/02/25 | Published: 2018/05/1
Received: 2017/12/2 | Accepted: 2018/02/25 | Published: 2018/05/1
References
1. Barr, J., et al., 2013. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical Care Medicine, 41(1), pp. 263-306. [DOI:10.1097/CCM.0b013e3182783b72] [PMID] [DOI:10.1097/CCM.0b013e3182783b72]
2. Clary, G. L., & Krishnan, K. R., 2001. Delirium: Diagnosis, neuropathogenesis, and treatment. Journal of Psychiatric Practice, 7(5), pp. 310-23. [DOI:10.1097/00131746-200109000-00004] [PMID] [DOI:10.1097/00131746-200109000-00004]
3. Inouye, S. K., 2006. Delirium in older persons. New England Journal of Medicine, 354(11), pp. 1157-65. [DOI:10.1056/NEJMra052321] [PMID] [DOI:10.1056/NEJMra052321]
4. Kalani, Z., Tavangar, H. & Rahimi, A., 2013. [Effectiveness of nursing interventions on incidence of delirium in patients hospitalized to intensive cardiac care units, Shiraz hospitals, 2012 (Persian)]. Medical-Surgical Nursing Journal, 2(3-4), pp. 93-100.
5. Kiely, D. K., Jones, R. N., Bergmann, M. A. & Marcantonio, E. R., 2007. Association between psychomotor activity delirium subtypes and mortality among newly admitted postacute facility patients. The Journals of Gerontology, 62(2), pp. 174-9. [DOI:10.1093/gerona/62.2.174] [DOI:10.1093/gerona/62.2.174]
6. Leslie, D. L., et al., 2005. Premature death associated with delirium at 1-year follow-up. Archives of Internal Medicine, 165(14), pp. 1657-62. [DOI:10.1001/archinte.165.14.1657] [PMID] [DOI:10.1001/archinte.165.14.1657]
7. Marcantonio, E., et al., 2002. Delirium severity and psychomotor types: Their relationship with outcomes after hip fracture repair. Journal of the American Geriatrics Society, 50(5), pp. 850-7. [DOI:10.1046/j.1532-5415.2002.50210.x] [PMID] [DOI:10.1046/j.1532-5415.2002.50210.x]
8. Martinez, F. T., et al., 2012. Preventing delirium in an acute hospital using a non-pharmacological intervention. Age and Ageing, 41(5), pp. 629-34. [DOI:10.1093/ageing/afs060] [PMID] [DOI:10.1093/ageing/afs060]
9. McPherson J. A., et al., 2013. Delirium in the cardiovascular intensive care unit: Exploring modifiable risk factors. Critcal Care Medicine, 41(2), pp. 405-13. [DOI:10.1097/CCM.0b013e31826ab49b] [PMID] [PMCID] [DOI:10.1097/CCM.0b013e31826ab49b]
10. Modabernia, M. J., Khalkhali, S. M. R. & Najafi, K., 2002. [Delirium in CCU (Persian)]. Journal of Guilan University of Medical Sciences, 11(41), pp. 1-6.
11. Naughton, B. J., et al., 2005. A multifactorial intervention to reduce prevalence of delirium and shorten hospital length of stay. Journal of the American Geriatrics Society, 53(1), pp. 18-23. [DOI:10.1111/j.1532-5415.2005.53005.x] [PMID] [DOI:10.1111/j.1532-5415.2005.53005.x]
12. Pisani, M. A., et al., 2009. Days of delirium are associated with 1-year mortality in an older intensive care unit population. American Journal of Respiratory and Critical Care Medicine, 180(11), pp. 1092-7. [DOI:10.1164/rccm.200904-0537OC] [PMID] [PMCID] [DOI:10.1164/rccm.200904-0537OC]
13. Tabet, N., et al., 2005. An educational intervention can prevent delirium on acute medical wards. Age and Ageing, 34(2), pp. 152-6. [DOI:10.1093/ageing/afi031] [PMID] [DOI:10.1093/ageing/afi031]
14. Tadrisi, S. et al., 2009. Richmond agitation¨Csedation scale validity and reliability in intensive care unit adult patients Persian version. Journal of Critical Care Nursing, 2(1), pp. 15-21.
15. Tsios, A. & Alichanidou, E., 2009. Coronary Care Unit (CCU) psychosis syndrome. Hospital Chronicles, 4(3), pp. 32-4.
16. Uguz, F., et al., 2010. Delirium following acute myocardial infarction: Incidence, clinical profiles, and predictors. Perspectives in Psychiatric Care, 46(2), pp. 135-42. [DOI:10.1111/j.1744-6163.2010.00249.x] [PMID] [DOI:10.1111/j.1744-6163.2010.00249.x]
17. Van Rompaey, B., et al., 2012. The effect of earplugs during the night on the onset of delirium and sleep perception: A randomized controlled trial in intensive care patients. Critical Care, 16(3), p. R73. [DOI:10.1186/cc11330] [PMID] [PMCID] [DOI:10.1186/cc11330]
18. Yamaguchi, T., Tsukioka, E. & Kishi, Y., 2014. Outcomes after delirium in a Japanese intensive care unit. General Hospital Psychiatry, 36(6), pp. 634-6. [DOI:10.1016/j.genhosppsych.2014.09.006] [PMID] [DOI:10.1016/j.genhosppsych.2014.09.006]
19. Zolfaghari, M., et al., 2012. [Effectiveness of a multifactor educational intervention on delirium incidence and length of stay in patients with cardiac surgery (Persian)]. Journal of Hayat, 18(1), pp. 67-78.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |