Fri, Feb 20, 2026
[Archive]
Volume 5, Issue 1 (Winter 2019)
JCCNC 2019, 5(1): 25-32 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Moosavi A, Shoghi M, Haghani H, Borimnejad L. The Effect of Medical-Directed Play on the Severity of Pediatric Pain During Burn Dressing Change in Children: A Clinical Randomized Trial. JCCNC 2019; 5 (1) :25-32
URL: http://jccnc.iums.ac.ir/article-1-194-en.html
URL: http://jccnc.iums.ac.ir/article-1-194-en.html
1- Department of Pediatric Nursing, School of Nursing and Midwhfery, Iran Universtiy of Medical Sciences, Tehran, Iran.
2- Department of Pediatric Nursing, School of Nursing and Midwhfery, Iran Universtiy of Medical Sciences, Tehran, Iran.; Nursing Care Research Center, Iran Universtiy of Medical Sciences, Tehran, Iran.
3- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
4- Nursing Care Research Center, School of Nursing & Midwifery, Iran Unversity of Medical Sciences, Tehran, Iran. ,Borimnejad.l@iums.ac.ir
2- Department of Pediatric Nursing, School of Nursing and Midwhfery, Iran Universtiy of Medical Sciences, Tehran, Iran.; Nursing Care Research Center, Iran Universtiy of Medical Sciences, Tehran, Iran.
3- Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
4- Nursing Care Research Center, School of Nursing & Midwifery, Iran Unversity of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 619 kb]
(1632 Downloads)
| Abstract (HTML) (5027 Views)
● Guided games before dressing change could reduce procedural pain in 3-6 years old children.
● Pain management in preschool children needs more attention.
● Pediatric nurses can use games with available devices and without any specialized training for children.
Plain Language Summary
We studied the effect of the game on the severity of pain in children's burning dressing change. The results showed that performing the game before changing the dressing and explaining the procedure to children could reduce the amount of pain caused by the dressing change. Given the importance of reducing pain in burned patients, relaxation, and pain relief can result in a better outcome. Replacing the game with a guided game method can be useful and better than drug interventions to reduce the pain associated with burns.
● Guided games before dressing change could reduce procedural pain in 3-6 years old children.
● Pain management in preschool children needs more attention.
● Pediatric nurses can use games with available devices and without any specialized training for children.
Plain Language Summary
We studied the effect of the game on the severity of pain in children's burning dressing change. The results showed that performing the game before changing the dressing and explaining the procedure to children could reduce the amount of pain caused by the dressing change. Given the importance of reducing pain in burned patients, relaxation, and pain relief can result in a better outcome. Replacing the game with a guided game method can be useful and better than drug interventions to reduce the pain associated with burns.
Full-Text: (1269 Views)
1. Background
Burns are among serious health problems worldwide (Hasimi et al. 2014), which occur daily and generate several problems. Burn injury is the third most common cause of death after traffic accidents and drowning (Sadeghi-Bazargani & Mohammadi 2012). The frequency of severe burn and the consequences of this damage in terms of mortality, illness, long-term admission, disability, social stigma, and economic costs to society are rational reasons for paying special attention of healthcare staff to these victims (Sanchez et al. 2008). A total of 265 people die each year because of burn accidents; deaths caused by burns in low- and middle-income countries are more than that of high-income countries (Ringo & Chilonga 2014).
Statistics in Iran have also revealed that of 18000 people referred to Shahid Motahari Burn Center in Tehran City, Iran, in 2016, 1800 were hospitalized. Moreover, 3850 children under the age of 12 years referred to the hospital, and 468 of them were hospitalized. Burn wound is associated with severe pain and causes several biopsychological problems in the patient (Sadeghi-Bazargani & Mohammadi 2012; Forjuoh 2006). Among the psychological effects of burn injury are depression, reduced self-confidence, and anxiety related to remaining scars (Liang et al. 2012).
The International Association of Pain has defined pain as an unpleasant sensory and emotional experience along with damage to the actual or potential tissues (Mohan et al. 2015; Rafii et al. 2010). Patients suffering from burn injury require supportive and therapeutic measures. Burn injuries not only influence the child but also the parent and the caregiver (Moore et al. 2015). The most pain that is experienced during the treatment measures relates to the time of dressing changes (Sil, Dahlquist & Burns, 2013).
Child pain management during dressing changes has been reported as insufficiently (Gandhi et al. 2010). If burn pain relief does not occur properly, it creates harmful effects beyond the patient’s discomfort, including a defect in the child’s immune system, increased body metabolism leading to malnutrition, susceptibility to infection, and delayed burn wound healing (Guo & DiPietr 2010).
Therefore, using appropriate measures for pain management seems necessary (Miller et al. 2011). Although medications, like sedatives and opioids, reduce burn pain are inadequate for pain control (Lalehgani et al. 2014). Moreover, they are accompanied by complications such as breathing weakness, drowsiness, nausea, vomiting, and constipation; an increased dose of these medicines may result in physical dependence of the individual (Hoffman et al. 2011). Some authorities even believe that non-pharmacological methods should be employed prior to pharmacotherapy (Ullan et al. 2014).
Game is the most practical, most straightforward and least costly non-pharmacological method, in this regard. While having a positive effect on the child patient, the game can affect parental anxiety and their satisfaction of care. It can also be used to prepare children for procedures and enhance their cooperation during the process. The effect of playing games has been studied in reducing the pain caused by various procedures like venipuncture in burn and oncology among children of different ages. In addition, it provides the opportunity to get acquainted with medical equipment (Moore et al. 2015; Scarponi 2016; Noruzi Koushali et al. 2017).
Concerning the importance of pain relief in children with burn as well as data limitation on the effect of playing games on pain severity during dressing changes; this study investigated the effect of medical directed play on the severity of pediatric pain during burn dressing changes in children referred to the Burn Clinic of Shahid Motahari Hospital.
2. Materials and Methods
This randomized clinical trial was conducted on 82 children aged 3-6 years, referring to the Burn Clinic of Shahid Motahari Burn Center. This center is the largest referral center for burn patients of different ages in Tehran city, Iran. Considering 95% confidence interval (i.e. 1.96) and a test power of 80%, the sample size for each group was calculated as 41 patients. Moreover, 10% was considered for attrition.
Based on similar studies, the standard deviation was estimated to be 2.78. The children were selected using convenience sampling method in 6 months. After explaining the goals of the parental partnership plan, all the parents signed written informed consent forms. Then, the children were randomly assigned to the control and intervention groups, using a block size of 4 randomizations. In both groups, the parents accompanied their children. The Inclusion criteria were 3-6 years old children of both genders, referring to the burn clinic for the first dressing change, first and second, degree burns, being fully aware of time, place and people, no audio-visual problems and intellectual disabilities, being able to communicate verbally, and had no pain other than burn pain; they also should not have received any pain medicines.
The children were excluded in case of an electrical burn, chemical burn, and burn with tar. Children with burn in the perineal area or on the head and neck were also excluded from the study. After ensuring confidentiality, the required information was documented using patient records, observation, interview, completing the questionnaires (demographic characteristics, pain intensity, number of pulse, and arterial oxygen levels).
Games were played with the consent of the child and parents before entering the dressing room when the child was away from tension. The game was initiated by the researcher before dressing for 15 minutes as follows: first, all the dressing steps were explained for the child and conducted on a doll with a burn. A child’s dressing package was also provided to the subjects. The child helped removing the previous dressing and re-dressing the doll using children’s medical tools. The doll was given to the child at the end of the procedure. Pulse oximetry probe was connected to the child’s hand before starting the dressing in both groups.
To prevent the child’s fear, the probe was first connected to the researcher and parents’ hands. Before starting the dressing, the heart rate, pain intensity, and arterial oxygen levels of the subjects were recorded. Their pain was measured by an assistant researcher before dressing using the FLACC scale. Concurrent with removing the previous dressing, the intensity of pain, heart rate, and arterial blood oxygen levels were recorded again while the pulse oximetry was still connected to the child. To make the study blind, an assistant researcher, was employed in both groups to measure the pain. At the end of the dressing, a gift was given to each child in both groups.
FLACC scale is a measurement used to assess pain for children between the ages of 2 months and 7 years or individuals that are unable to communicate their pain. The scale is scored in a range of 0-10, with 0 representing no pain. The scale has 5 criteria (face legs, activity, cry, consolability) which are each assigned a score of 0, 1, or 2. It measures pain intensity from the reactions of the face, legs, mobility, crying, and relaxation. The final score is obtained by calculating the scores of the 5 criteria. Zero scores in this scale indicate the lack of pain, and score 10 indicates the most severe pain.
The overall score was divided into three categories as 0-3 (weak pain), 4-7 (moderate pain), and 7-10 (severe pain). This scale was constructed by Merkel, Voepel-Lewis & Malviya (2002). The validity and reliability of this tool have been confirmed in various studies (Voepel-Lewis et al. 2002; Merkel 2002). Reliability of the Persian version of the FLACC scale has been confirmed using a parallel form on 20 children in Iran (P<0.001, r=0.707). (Sadeghi et al. 2013). To assess the reliability of pulse oximetry, the device showed constant values in three consecutive measurements. The obtained data were analyzed using SPSS and Independent Samples t-test, Paired Samples t-test, Chi-squared test, and Fisher’s Exact-test.
3. Results
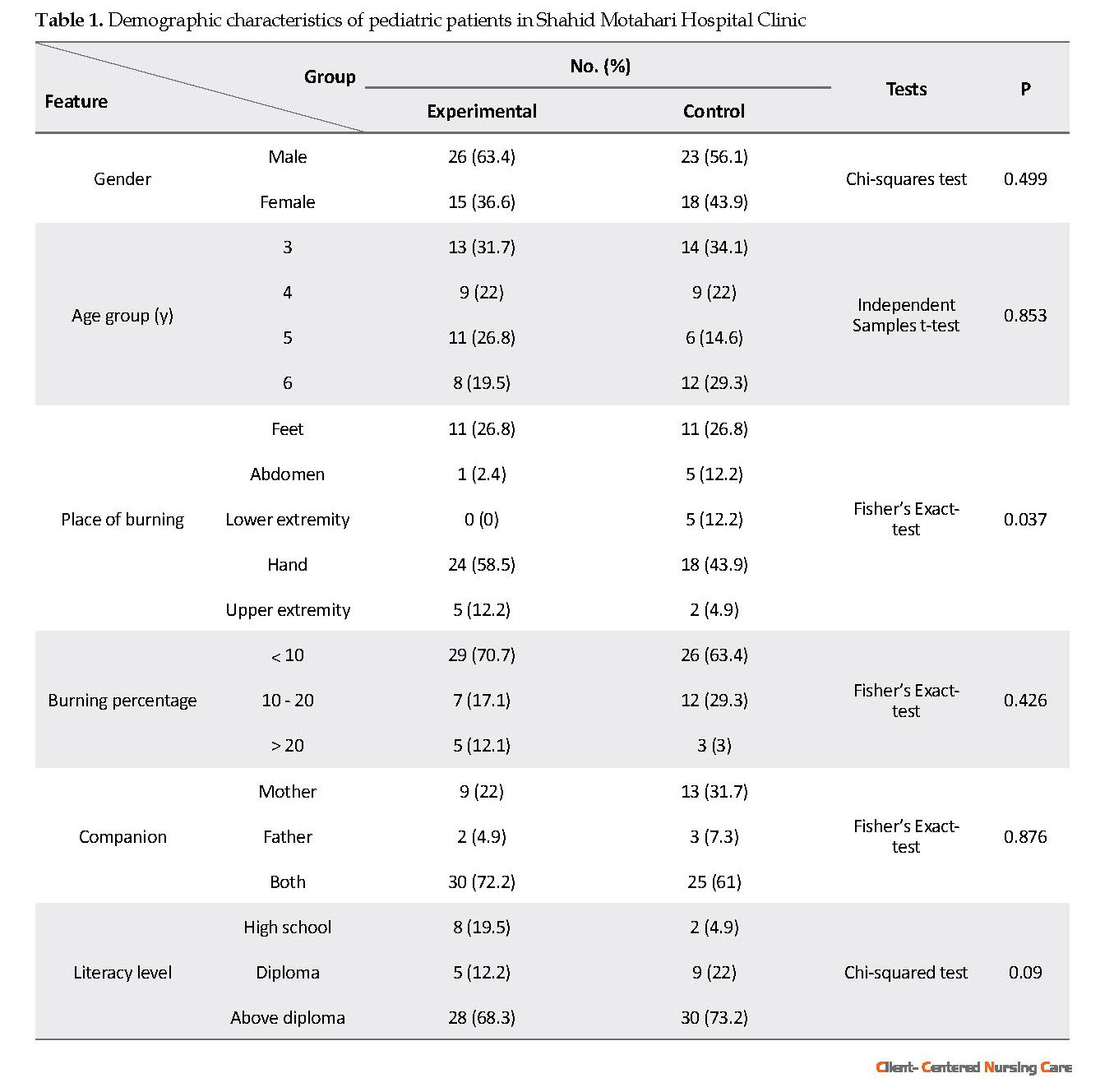
The Mean±SD age of children in the intervention and control groups was 4.34±1.13 and 4.39±1.24 years, respectively. Male gender distribution was 63.4% in the intervention group and 56.1% in the control group. The educational level of the majority of mothers was above diploma in both groups. Both groups were homogenous in terms of demographic characteristics (Table 1). Chi-squared test results revealed no significant difference between the groups in terms of all the variables mentioned above as well as the area and percentage of burn (1-25%) and the lack of analgesic use before dressing (P>0.05). The test results suggested no significant difference in the mean score of pain intensity between the groups before dressing change; most of the children had experienced moderate pain (P=0.307).
Burns are among serious health problems worldwide (Hasimi et al. 2014), which occur daily and generate several problems. Burn injury is the third most common cause of death after traffic accidents and drowning (Sadeghi-Bazargani & Mohammadi 2012). The frequency of severe burn and the consequences of this damage in terms of mortality, illness, long-term admission, disability, social stigma, and economic costs to society are rational reasons for paying special attention of healthcare staff to these victims (Sanchez et al. 2008). A total of 265 people die each year because of burn accidents; deaths caused by burns in low- and middle-income countries are more than that of high-income countries (Ringo & Chilonga 2014).
Statistics in Iran have also revealed that of 18000 people referred to Shahid Motahari Burn Center in Tehran City, Iran, in 2016, 1800 were hospitalized. Moreover, 3850 children under the age of 12 years referred to the hospital, and 468 of them were hospitalized. Burn wound is associated with severe pain and causes several biopsychological problems in the patient (Sadeghi-Bazargani & Mohammadi 2012; Forjuoh 2006). Among the psychological effects of burn injury are depression, reduced self-confidence, and anxiety related to remaining scars (Liang et al. 2012).
The International Association of Pain has defined pain as an unpleasant sensory and emotional experience along with damage to the actual or potential tissues (Mohan et al. 2015; Rafii et al. 2010). Patients suffering from burn injury require supportive and therapeutic measures. Burn injuries not only influence the child but also the parent and the caregiver (Moore et al. 2015). The most pain that is experienced during the treatment measures relates to the time of dressing changes (Sil, Dahlquist & Burns, 2013).
Child pain management during dressing changes has been reported as insufficiently (Gandhi et al. 2010). If burn pain relief does not occur properly, it creates harmful effects beyond the patient’s discomfort, including a defect in the child’s immune system, increased body metabolism leading to malnutrition, susceptibility to infection, and delayed burn wound healing (Guo & DiPietr 2010).
Therefore, using appropriate measures for pain management seems necessary (Miller et al. 2011). Although medications, like sedatives and opioids, reduce burn pain are inadequate for pain control (Lalehgani et al. 2014). Moreover, they are accompanied by complications such as breathing weakness, drowsiness, nausea, vomiting, and constipation; an increased dose of these medicines may result in physical dependence of the individual (Hoffman et al. 2011). Some authorities even believe that non-pharmacological methods should be employed prior to pharmacotherapy (Ullan et al. 2014).
Game is the most practical, most straightforward and least costly non-pharmacological method, in this regard. While having a positive effect on the child patient, the game can affect parental anxiety and their satisfaction of care. It can also be used to prepare children for procedures and enhance their cooperation during the process. The effect of playing games has been studied in reducing the pain caused by various procedures like venipuncture in burn and oncology among children of different ages. In addition, it provides the opportunity to get acquainted with medical equipment (Moore et al. 2015; Scarponi 2016; Noruzi Koushali et al. 2017).
Concerning the importance of pain relief in children with burn as well as data limitation on the effect of playing games on pain severity during dressing changes; this study investigated the effect of medical directed play on the severity of pediatric pain during burn dressing changes in children referred to the Burn Clinic of Shahid Motahari Hospital.
2. Materials and Methods
This randomized clinical trial was conducted on 82 children aged 3-6 years, referring to the Burn Clinic of Shahid Motahari Burn Center. This center is the largest referral center for burn patients of different ages in Tehran city, Iran. Considering 95% confidence interval (i.e. 1.96) and a test power of 80%, the sample size for each group was calculated as 41 patients. Moreover, 10% was considered for attrition.
Based on similar studies, the standard deviation was estimated to be 2.78. The children were selected using convenience sampling method in 6 months. After explaining the goals of the parental partnership plan, all the parents signed written informed consent forms. Then, the children were randomly assigned to the control and intervention groups, using a block size of 4 randomizations. In both groups, the parents accompanied their children. The Inclusion criteria were 3-6 years old children of both genders, referring to the burn clinic for the first dressing change, first and second, degree burns, being fully aware of time, place and people, no audio-visual problems and intellectual disabilities, being able to communicate verbally, and had no pain other than burn pain; they also should not have received any pain medicines.
The children were excluded in case of an electrical burn, chemical burn, and burn with tar. Children with burn in the perineal area or on the head and neck were also excluded from the study. After ensuring confidentiality, the required information was documented using patient records, observation, interview, completing the questionnaires (demographic characteristics, pain intensity, number of pulse, and arterial oxygen levels).
Games were played with the consent of the child and parents before entering the dressing room when the child was away from tension. The game was initiated by the researcher before dressing for 15 minutes as follows: first, all the dressing steps were explained for the child and conducted on a doll with a burn. A child’s dressing package was also provided to the subjects. The child helped removing the previous dressing and re-dressing the doll using children’s medical tools. The doll was given to the child at the end of the procedure. Pulse oximetry probe was connected to the child’s hand before starting the dressing in both groups.
To prevent the child’s fear, the probe was first connected to the researcher and parents’ hands. Before starting the dressing, the heart rate, pain intensity, and arterial oxygen levels of the subjects were recorded. Their pain was measured by an assistant researcher before dressing using the FLACC scale. Concurrent with removing the previous dressing, the intensity of pain, heart rate, and arterial blood oxygen levels were recorded again while the pulse oximetry was still connected to the child. To make the study blind, an assistant researcher, was employed in both groups to measure the pain. At the end of the dressing, a gift was given to each child in both groups.
FLACC scale is a measurement used to assess pain for children between the ages of 2 months and 7 years or individuals that are unable to communicate their pain. The scale is scored in a range of 0-10, with 0 representing no pain. The scale has 5 criteria (face legs, activity, cry, consolability) which are each assigned a score of 0, 1, or 2. It measures pain intensity from the reactions of the face, legs, mobility, crying, and relaxation. The final score is obtained by calculating the scores of the 5 criteria. Zero scores in this scale indicate the lack of pain, and score 10 indicates the most severe pain.
The overall score was divided into three categories as 0-3 (weak pain), 4-7 (moderate pain), and 7-10 (severe pain). This scale was constructed by Merkel, Voepel-Lewis & Malviya (2002). The validity and reliability of this tool have been confirmed in various studies (Voepel-Lewis et al. 2002; Merkel 2002). Reliability of the Persian version of the FLACC scale has been confirmed using a parallel form on 20 children in Iran (P<0.001, r=0.707). (Sadeghi et al. 2013). To assess the reliability of pulse oximetry, the device showed constant values in three consecutive measurements. The obtained data were analyzed using SPSS and Independent Samples t-test, Paired Samples t-test, Chi-squared test, and Fisher’s Exact-test.
3. Results
The Mean±SD age of children in the intervention and control groups was 4.34±1.13 and 4.39±1.24 years, respectively. Male gender distribution was 63.4% in the intervention group and 56.1% in the control group. The educational level of the majority of mothers was above diploma in both groups. Both groups were homogenous in terms of demographic characteristics (Table 1). Chi-squared test results revealed no significant difference between the groups in terms of all the variables mentioned above as well as the area and percentage of burn (1-25%) and the lack of analgesic use before dressing (P>0.05). The test results suggested no significant difference in the mean score of pain intensity between the groups before dressing change; most of the children had experienced moderate pain (P=0.307).
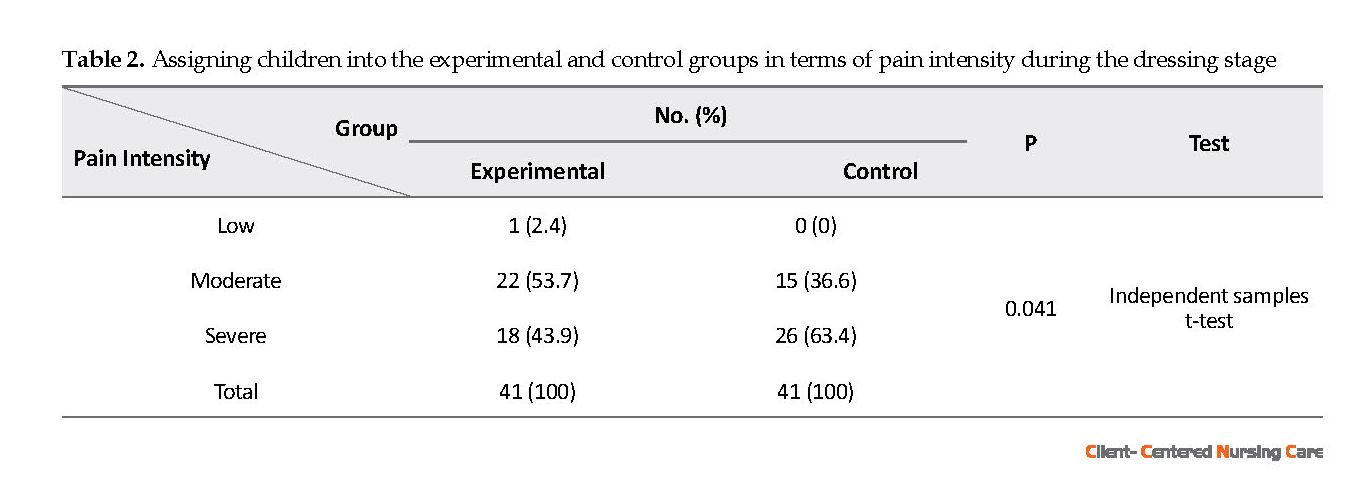
Severe pain was reported by 63.4% of the children in the control group, while 43.9% of children in the intervention group had experienced that. Moreover, 53.7% of the children in the intervention group reported moderate pain. The Mean±SD score of pain was 7.36±1.51 in the control group during dressing; while it was 6.56±1.66 in the intervention group. Independent Samples t-test results revealed a significant difference between the groups in terms of the mean score of pain during dressing (P=0.041) (Table 2).
Independent Samples t-test indicated no significant difference between the heart rate of the groups in the pre-intervention phase; however, Paired Samples t-test revealed a significant difference between the average heart rate of the groups during dressing change. The mean heart rate was higher in the control group (P<0.001). There were no significant differences between the groups in terms of the level of arterial oxygen saturation before and during dressing (P=1) (Table 3).
4. Discussion
The obtained results revealed that guided game before dressing change could reduce burn pain in children of 3-6 years of age. The findings were in line with a similar study which examined the effect of playing games on the pain severity of burn dressing change (Moore et al. 2015).
A study examined the effects of 4 methods (Entonox, Game Therapy, combination of game and Entonox, and non-interventional standardized method) before elective surgery; pain intensity in the experimental groups was less than that of controls; however, no significant difference was observed between the 3 experimental groups (using Entonox, playing and combination of both) (Mohan et al. 2015).
A prospective randomized control trial in a pediatric burn outpatient clinic was performed to investigate the effects of MMD (Multi-modal distraction) procedural preparation (MMD-PP) and distraction (MMD-D) on child pain reduction, compared to standard deviation (SD) and video game (VG) distraction. The results revealed that both MMD-D and MMD-PP have significantly reduced pain intensity (P<OR=0.05) (Miller et al. 2010).
These findings suggested that guided game before changing burn dressing or surgery can effectively reduce pain. The guided game prepares and familiarizes the child with medical equipment and the planned process for him/her. This preparation is effective in reducing pain.
Some researchers have reported results in contrast with those of this study about O2 saturation. The authors found that non-pharmacological pain control methods affect O2sat; where the experimental group had a more balanced situation in terms of oxygen saturation of arterial blood after and during the intervention. This difference may be due to the type of procedure; because the pain of venipuncture and injections is very different from that of burn. Additionally, in these studies, the O2 level was measured after the painful procedure (Lal et al. 2001; Sajedi et al. 2007; Mott et al. 2008).
A study on the effect of virtual reality on pain of burn dressing in children reported that using non-pharmacological methods is effective in controlling such pain; however, it has no effects on the physiological indicators. The study concluded that changes of O2saturation dependent on pulmonary function and the effects on the lung like sedatives. Moreover, the different results could be related to the kind of entertainment, the processing time for each child, the time of heart rate measurement, and O2sat in the two studies. In the study of Mott, the measurement was conducted after the procedure (Mott et al. 2008).
A study determined the effect of two non-pharmacological methods on the pain intensity and physiological indicators of children; it reported similar results in heart rate;i.e. thought distortion has
been effective on balancing heart rate and reducing pain intensity (Hasanpour et al. 2006). A study compared the effect of music on pain and changes in physiological parameters; it concluded that a non-pharmacological method balanced heart rate in the experimental group in addition to reducing pain and it did not affect other indicators (Naderi et al. 2014). In another study which examined analgesic effects on O2 saturation level and the number of breathing, it was observed that pain control did not affect O2 saturation (Alimohammadi et al. 2014).
According to the obtained results, future studies are suggested to investigate the effect of playing games on the level of children’s anxiety and parental satisfaction. The findings of this study can be beneficial for nurses working in pediatric wards to provide an opportunity to relieve the pain of children while taking care of them. Games can be used without any special training for children, and with small and available devices. This method is entirely non-invasive and has no adverse effects. In addition to reducing pain, this method causes children to collaborate and creates a positive experience of the hospital for the child. Therefore, it is recommended that this non-pharmacological and non- invasive method be used by nurses to reduce the procedural pain of children with a burn.
Ethical Considerations
Compliance with ethical guidelines
This project was approved by the Ethics Board of Iran University of Medical Sciences (IUMS) Committee (IR. IEC. 1391.9311687009), and has been registered at Iran Clinical Trials Center (IRCT201602281788N15). All the parents of the children in this study were confirmed about the confidentiality of their data and signed the written consent.
Funding
This project was supported by the Nursing care research center of Iran University of Medical Sciences.
Authors' contributions
Substantial contribution to the conception, research, data acquisition: Atefeh Moosavi; Data analysis/interpretation: Hamid Haghani; Collaboration in the preparation of the submitted manuscript: Mahnaz Shoghi; Preparation and revision of the submitted manuscript/ participation in reaching the approval for the publishable manuscript version; participation in reaching the approval for the publishable manuscript version: Leili Borimnejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We express our thanks and gratitude towards Deputy of Research of Iran University of Medical Sciences which funded this project as a student dissertation and all hospital officials and nurses in Shahid Motahari Children Clinic Department as well as all the parents and children who participated in the study.
References
Alimohammadi, H., et al., 2014. Effects of pain relief on arterial blood o2 saturation. Trauma Monthly, 19(1), p. e14034. [DOI:10.5812/traumamon.14034] [PMID] [PMCID]
Forjuoh, S.N., 2006. Burns in low-and middle-income countries: A review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns, 32(5), pp. 529-37. [DOI:10.1016/j.burns.2006.04.002] [PMID]
Gandhi, M., et al., 2010. Management of pain in children with burns. International Journal of Pediatrics, 2010(825657), pp. 1-8. [DOI:10.1155/2010/825657] [PMID] [PMCID]
Guo, S. A. & DiPietro, L.A., 2010. Factors affecting wound healing. Journal of Dental Research, 89(3), pp. 219-29. [DOI:10.1177/0022034509359125] [PMID] [PMCID]
Hasanpour, M., et al., 2006. The effects of two non-pharmacologic pain management methods for intramuscular injection pain in children. Acute Pain, 8(1), pp. 7-12. [DOI:10.1016/j.acpain.2005.11.001]
Hasimi, L., et al., 2014. [The effect of applying organizational culture improvement model of patient education on anxiety and satisfaction of burned hospitalized patients: A clinical trial (Persian)]. Journal of Clinical Nursing and Midwifery, 3(3), pp. 16-28.
Hoffman, H.G., et al. 2011. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annals of Behavioral Medicine, 41(2), pp.183-91. [DOI:10.1007/s12160-010-9248-7] [PMID] [PMCID]
Lal, M.K., et al., 2001. Comparison of EMLA cream versus placebo in children receiving distraction therapy for venepuncture. Acta Paediatrica, 90(2), pp. 154-9. [DOI:10.1080/080352501300049307]
Lalehgani, H., et al. The effect of deep-slow and regular breathing on pain intensity of burn dressing. Iran Journal of Critical Care Nursing. 2014. 6(4), pp. 223–8.
Liang, C. Y., et al., 2012. Predictors of health-care needs in discharged burn patients. Burns, 38(2), pp.172-9. [DOI:10.1016/j.burns.2011.09.010] [PMID]
Merkel, S., et al., 2002. Pain control: Pain assessment in infants and young children: The FLACC scale. The American Journal of Nursing, 102(10), pp. 55-8. [DOI:10.1097/00000446-200210000-00024] [PMID]
Miller, K., et al., 2010. Multi-modal distraction. Using technology to combat pain in young children with burn injuries. Burns, 36(5), pp. 647-58. [DOI:10.1016/j.burns.2009.06.199] [PMID]
Miller, K., et al., 2011. A novel technology approach to pain management in children with burns: A prospective randomized controlled trial. Burns, 37(3), pp. 395-405. [DOI:10.1016/j.burns.2010.12.008] [PMID]
Mohan, S., et al., 2015. The effect of Entonox, play therapy and a combination on pain relief in children: A randomized controlled trial. Pain Management Nursing, 16(6), pp. 938-43. [DOI:10.1016/j.pmn.2015.08.004] [PMID]
Moore, E. R., et al., 2015. The effect of directed medical play on young children’s pain and distress during burn wound care. Journal of Pediatric Health Care, 29(3), pp. 265-73. [DOI:10.1016/j.pedhc.2014.12.006] [PMID] [PMCID]
Mott, J., et al., 2008. The efficacy of an augmented virtual reality system to alleviate pain in children undergoing burns dressing changes: A randomised controlled trial. Burns, 34(6), pp. 803-8. [DOI:10.1016/j.burns.2007.10.010] [PMID]
Naderi, F., et al., 2014. [Comparing the effect of music on pain threshold, anxiety, behavioral responses to pain and the hemodynamic parameters during dressing change in burn patients (Persian)]. Quarterly of the Horizon of Medical Sciences, 20(1), pp. 63-8.
Noruzi Koushali, A., et al., 2017. The effect of a multi-dimensional play program on children’s pain intensity during burn dressing change in burn intensive care units: A clinical trial. Critical Care Nursing, 10(4), p. e58845. [DOI:10.5812/ccn.58845] [PMID]
Rafii, F., et al., 2010. [Effect of jaw relaxation on pain intensity of burn dressing (Persian)]. Iranian Journal of Critical Care Nursing, 3(2), pp. 51-6.
Ringo, Y., Chilonga, K., 2014. Burns at KCMC: Epidemiology, presentation, management and treatment outcome. Burns, 40(5), pp. 1024-9. [DOI:10.1016/j.burns.2013.10.019] [PMID]
Sadeghi-Bazargani, H. & Mohammadi, R., 2012. Epidemiology of burns in Iran during the last decade (2000–2010): Review of literature and methodological considerations. Burns, 38(3), pp.319-29. [DOI:10.1016/j.burns.2011.09.025] [PMID]
Sadeghi, T., et al., 2013. Effect of distraction on children’s behavioral responses to pain during IV catheter insertion. Hayat, 18(4), pp. 1-9. [DOI:10.1111/jspn.12018] [PMID]
Sajedi, F., et al, 2007. The effect of Kangaroo care on physiologic responses to pain of an intramuscular injection in neonates. Iranian Journal of Pediatrics, 17(4), pp. 339-44.
Sanchez, J. L. et al., 2008. Socio-economic cost and health-related quality of life of burn victims in Spain. Burns, 34(7), pp. 975-81. [DOI:10.1016/j.burns.2007.12.011] [PMID]
Scarponi, D., 2016. Play therapy to control pain and suffering in paediatric oncology. Frontiers in Pediatrics, 4, p.132. [DOI:10.3389/fped.2016.00132] [PMID] [PMCID]
Sil, S., Dahlquist, L. M. & Burns, A. J., 2012. Case study: Videogame distraction reduces behavioral distress in a preschool-aged child undergoing repeated burn dressing changes: A single-subject design. Journal of Pediatric Psychology, 38(3), pp. 330-41. [DOI:10.1093/jpepsy/jss128] [PMID] [PMCID]
Ullán, A. M., et al., 2014. The effect of a program to promote play to reduce children’s post-surgical pain: With plush toys, it hurts less. Pain Management Nursing, 15(1), pp. 273-82. [DOI:10.1016/j.pmn.2012.10.004] [PMID]
Voepel-Lewis, T., et al, S., 2010. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. American Journal of Critical Care, 19(1), pp. 55-61. [DOI:10.1097/00000539-200211000-00020]
The obtained results revealed that guided game before dressing change could reduce burn pain in children of 3-6 years of age. The findings were in line with a similar study which examined the effect of playing games on the pain severity of burn dressing change (Moore et al. 2015).
A study examined the effects of 4 methods (Entonox, Game Therapy, combination of game and Entonox, and non-interventional standardized method) before elective surgery; pain intensity in the experimental groups was less than that of controls; however, no significant difference was observed between the 3 experimental groups (using Entonox, playing and combination of both) (Mohan et al. 2015).
A prospective randomized control trial in a pediatric burn outpatient clinic was performed to investigate the effects of MMD (Multi-modal distraction) procedural preparation (MMD-PP) and distraction (MMD-D) on child pain reduction, compared to standard deviation (SD) and video game (VG) distraction. The results revealed that both MMD-D and MMD-PP have significantly reduced pain intensity (P<OR=0.05) (Miller et al. 2010).
These findings suggested that guided game before changing burn dressing or surgery can effectively reduce pain. The guided game prepares and familiarizes the child with medical equipment and the planned process for him/her. This preparation is effective in reducing pain.
Some researchers have reported results in contrast with those of this study about O2 saturation. The authors found that non-pharmacological pain control methods affect O2sat; where the experimental group had a more balanced situation in terms of oxygen saturation of arterial blood after and during the intervention. This difference may be due to the type of procedure; because the pain of venipuncture and injections is very different from that of burn. Additionally, in these studies, the O2 level was measured after the painful procedure (Lal et al. 2001; Sajedi et al. 2007; Mott et al. 2008).
A study on the effect of virtual reality on pain of burn dressing in children reported that using non-pharmacological methods is effective in controlling such pain; however, it has no effects on the physiological indicators. The study concluded that changes of O2saturation dependent on pulmonary function and the effects on the lung like sedatives. Moreover, the different results could be related to the kind of entertainment, the processing time for each child, the time of heart rate measurement, and O2sat in the two studies. In the study of Mott, the measurement was conducted after the procedure (Mott et al. 2008).
A study determined the effect of two non-pharmacological methods on the pain intensity and physiological indicators of children; it reported similar results in heart rate;i.e. thought distortion has
been effective on balancing heart rate and reducing pain intensity (Hasanpour et al. 2006). A study compared the effect of music on pain and changes in physiological parameters; it concluded that a non-pharmacological method balanced heart rate in the experimental group in addition to reducing pain and it did not affect other indicators (Naderi et al. 2014). In another study which examined analgesic effects on O2 saturation level and the number of breathing, it was observed that pain control did not affect O2 saturation (Alimohammadi et al. 2014).
According to the obtained results, future studies are suggested to investigate the effect of playing games on the level of children’s anxiety and parental satisfaction. The findings of this study can be beneficial for nurses working in pediatric wards to provide an opportunity to relieve the pain of children while taking care of them. Games can be used without any special training for children, and with small and available devices. This method is entirely non-invasive and has no adverse effects. In addition to reducing pain, this method causes children to collaborate and creates a positive experience of the hospital for the child. Therefore, it is recommended that this non-pharmacological and non- invasive method be used by nurses to reduce the procedural pain of children with a burn.
Ethical Considerations
Compliance with ethical guidelines
This project was approved by the Ethics Board of Iran University of Medical Sciences (IUMS) Committee (IR. IEC. 1391.9311687009), and has been registered at Iran Clinical Trials Center (IRCT201602281788N15). All the parents of the children in this study were confirmed about the confidentiality of their data and signed the written consent.
Funding
This project was supported by the Nursing care research center of Iran University of Medical Sciences.
Authors' contributions
Substantial contribution to the conception, research, data acquisition: Atefeh Moosavi; Data analysis/interpretation: Hamid Haghani; Collaboration in the preparation of the submitted manuscript: Mahnaz Shoghi; Preparation and revision of the submitted manuscript/ participation in reaching the approval for the publishable manuscript version; participation in reaching the approval for the publishable manuscript version: Leili Borimnejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We express our thanks and gratitude towards Deputy of Research of Iran University of Medical Sciences which funded this project as a student dissertation and all hospital officials and nurses in Shahid Motahari Children Clinic Department as well as all the parents and children who participated in the study.
References
Alimohammadi, H., et al., 2014. Effects of pain relief on arterial blood o2 saturation. Trauma Monthly, 19(1), p. e14034. [DOI:10.5812/traumamon.14034] [PMID] [PMCID]
Forjuoh, S.N., 2006. Burns in low-and middle-income countries: A review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns, 32(5), pp. 529-37. [DOI:10.1016/j.burns.2006.04.002] [PMID]
Gandhi, M., et al., 2010. Management of pain in children with burns. International Journal of Pediatrics, 2010(825657), pp. 1-8. [DOI:10.1155/2010/825657] [PMID] [PMCID]
Guo, S. A. & DiPietro, L.A., 2010. Factors affecting wound healing. Journal of Dental Research, 89(3), pp. 219-29. [DOI:10.1177/0022034509359125] [PMID] [PMCID]
Hasanpour, M., et al., 2006. The effects of two non-pharmacologic pain management methods for intramuscular injection pain in children. Acute Pain, 8(1), pp. 7-12. [DOI:10.1016/j.acpain.2005.11.001]
Hasimi, L., et al., 2014. [The effect of applying organizational culture improvement model of patient education on anxiety and satisfaction of burned hospitalized patients: A clinical trial (Persian)]. Journal of Clinical Nursing and Midwifery, 3(3), pp. 16-28.
Hoffman, H.G., et al. 2011. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annals of Behavioral Medicine, 41(2), pp.183-91. [DOI:10.1007/s12160-010-9248-7] [PMID] [PMCID]
Lal, M.K., et al., 2001. Comparison of EMLA cream versus placebo in children receiving distraction therapy for venepuncture. Acta Paediatrica, 90(2), pp. 154-9. [DOI:10.1080/080352501300049307]
Lalehgani, H., et al. The effect of deep-slow and regular breathing on pain intensity of burn dressing. Iran Journal of Critical Care Nursing. 2014. 6(4), pp. 223–8.
Liang, C. Y., et al., 2012. Predictors of health-care needs in discharged burn patients. Burns, 38(2), pp.172-9. [DOI:10.1016/j.burns.2011.09.010] [PMID]
Merkel, S., et al., 2002. Pain control: Pain assessment in infants and young children: The FLACC scale. The American Journal of Nursing, 102(10), pp. 55-8. [DOI:10.1097/00000446-200210000-00024] [PMID]
Miller, K., et al., 2010. Multi-modal distraction. Using technology to combat pain in young children with burn injuries. Burns, 36(5), pp. 647-58. [DOI:10.1016/j.burns.2009.06.199] [PMID]
Miller, K., et al., 2011. A novel technology approach to pain management in children with burns: A prospective randomized controlled trial. Burns, 37(3), pp. 395-405. [DOI:10.1016/j.burns.2010.12.008] [PMID]
Mohan, S., et al., 2015. The effect of Entonox, play therapy and a combination on pain relief in children: A randomized controlled trial. Pain Management Nursing, 16(6), pp. 938-43. [DOI:10.1016/j.pmn.2015.08.004] [PMID]
Moore, E. R., et al., 2015. The effect of directed medical play on young children’s pain and distress during burn wound care. Journal of Pediatric Health Care, 29(3), pp. 265-73. [DOI:10.1016/j.pedhc.2014.12.006] [PMID] [PMCID]
Mott, J., et al., 2008. The efficacy of an augmented virtual reality system to alleviate pain in children undergoing burns dressing changes: A randomised controlled trial. Burns, 34(6), pp. 803-8. [DOI:10.1016/j.burns.2007.10.010] [PMID]
Naderi, F., et al., 2014. [Comparing the effect of music on pain threshold, anxiety, behavioral responses to pain and the hemodynamic parameters during dressing change in burn patients (Persian)]. Quarterly of the Horizon of Medical Sciences, 20(1), pp. 63-8.
Noruzi Koushali, A., et al., 2017. The effect of a multi-dimensional play program on children’s pain intensity during burn dressing change in burn intensive care units: A clinical trial. Critical Care Nursing, 10(4), p. e58845. [DOI:10.5812/ccn.58845] [PMID]
Rafii, F., et al., 2010. [Effect of jaw relaxation on pain intensity of burn dressing (Persian)]. Iranian Journal of Critical Care Nursing, 3(2), pp. 51-6.
Ringo, Y., Chilonga, K., 2014. Burns at KCMC: Epidemiology, presentation, management and treatment outcome. Burns, 40(5), pp. 1024-9. [DOI:10.1016/j.burns.2013.10.019] [PMID]
Sadeghi-Bazargani, H. & Mohammadi, R., 2012. Epidemiology of burns in Iran during the last decade (2000–2010): Review of literature and methodological considerations. Burns, 38(3), pp.319-29. [DOI:10.1016/j.burns.2011.09.025] [PMID]
Sadeghi, T., et al., 2013. Effect of distraction on children’s behavioral responses to pain during IV catheter insertion. Hayat, 18(4), pp. 1-9. [DOI:10.1111/jspn.12018] [PMID]
Sajedi, F., et al, 2007. The effect of Kangaroo care on physiologic responses to pain of an intramuscular injection in neonates. Iranian Journal of Pediatrics, 17(4), pp. 339-44.
Sanchez, J. L. et al., 2008. Socio-economic cost and health-related quality of life of burn victims in Spain. Burns, 34(7), pp. 975-81. [DOI:10.1016/j.burns.2007.12.011] [PMID]
Scarponi, D., 2016. Play therapy to control pain and suffering in paediatric oncology. Frontiers in Pediatrics, 4, p.132. [DOI:10.3389/fped.2016.00132] [PMID] [PMCID]
Sil, S., Dahlquist, L. M. & Burns, A. J., 2012. Case study: Videogame distraction reduces behavioral distress in a preschool-aged child undergoing repeated burn dressing changes: A single-subject design. Journal of Pediatric Psychology, 38(3), pp. 330-41. [DOI:10.1093/jpepsy/jss128] [PMID] [PMCID]
Ullán, A. M., et al., 2014. The effect of a program to promote play to reduce children’s post-surgical pain: With plush toys, it hurts less. Pain Management Nursing, 15(1), pp. 273-82. [DOI:10.1016/j.pmn.2012.10.004] [PMID]
Voepel-Lewis, T., et al, S., 2010. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. American Journal of Critical Care, 19(1), pp. 55-61. [DOI:10.1097/00000539-200211000-00020]
Type of Study: Research |
Subject:
General
Received: 2018/09/2 | Accepted: 2018/12/28 | Published: 2019/02/1
Received: 2018/09/2 | Accepted: 2018/12/28 | Published: 2019/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |