Wed, Nov 26, 2025
[Archive]
Volume 7, Issue 1 (Winter 2021)
JCCNC 2021, 7(1): 75-86 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Chinedu Chichi A C. Organizational Factors Associated With Nurses’ Competence in Averting Failure to Rescue in Acute Care Settings. JCCNC 2021; 7 (1) :75-86
URL: http://jccnc.iums.ac.ir/article-1-298-en.html
URL: http://jccnc.iums.ac.ir/article-1-298-en.html
Department of Adult Health, School of Nursing, Babcock University, Ilishan-Remo, Nigeria. , christianasonye1@gmail.com
Full-Text [PDF 653 kb]
(1057 Downloads)
| Abstract (HTML) (3163 Views)
● The development of competence in deciphering subtle cues, indicative of deterioration to avert failure-to-rescue in acute care settings is essential in nursing practice.
● Organizational characteristics are central to nursing practice in acute care settings.
● Most nurses in this study presented a high-level knowledge regarding failure to rescue in acute care settings.
● There was a significant association between organizational characteristics and nurses’ level of competence in averting failure to rescue in the acute care setting.
Plain Language Summary
Failure to rescue entails the idea that not all complications developed by patients are preventable, but nurses by the virtue of their close proximity to patients should be able to promptly identify and institute appropriate measures immediately after they occur. The present study assessed the organizational factors affecting nurses’ competence in averting failure to rescue in acute care settings. The study results suggested an association between organizational characteristics and nurses’ level of competence in averting failure to rescue in acute care settings. Therefore, organizational characteristics must be adjusted or modified in the bid to increase nurses’ competence averting failure to rescue in acute care settings.
● Organizational characteristics are central to nursing practice in acute care settings.
● Most nurses in this study presented a high-level knowledge regarding failure to rescue in acute care settings.
● There was a significant association between organizational characteristics and nurses’ level of competence in averting failure to rescue in the acute care setting.
Plain Language Summary
Failure to rescue entails the idea that not all complications developed by patients are preventable, but nurses by the virtue of their close proximity to patients should be able to promptly identify and institute appropriate measures immediately after they occur. The present study assessed the organizational factors affecting nurses’ competence in averting failure to rescue in acute care settings. The study results suggested an association between organizational characteristics and nurses’ level of competence in averting failure to rescue in acute care settings. Therefore, organizational characteristics must be adjusted or modified in the bid to increase nurses’ competence averting failure to rescue in acute care settings.
Full-Text: (1200 Views)
1. Introduction
The characteristics of an organization are the main concerns of practice development, especially in the healthcare industry. It has the potential of impacting the employees (nurses) and the patients. Nurses, by their proximity to the patients, are at the frontline of distinguishing alteration in the health status of a patient to improve therapeutic outcomes during patient care. Therefore, they have a profound task of promptly identifying subtle cues; thus, it is suggestive of the patient’s health deterioration and institute measures to avert Failure to Rescue (FTR) (Purling & King 2012).
The concept of FTR entails the idea that not all complications developed by patients are preventable; however, nurses and other healthcare teams should be able to promptly identify and treat complications immediately after they occur. According to the Agency for Healthcare Research and Quality (AHRQ), high-quality hospitals have better chances of averting patient death from complications, even though they care for patient populations with significant surgical risk factors. This is because the variation in complication rates may depend on the patient’s characteristics; such factors may be present on admission, whereas the ability to rescue patients (prevent death from complications) may reflect the resources and preparedness of the organizational characteristics. Such characteristics include resource management, communication pattern, the culture of practice environment, as well as educational and career development.
The organization in which a nurse works has the potential of impacting competence, productivity, and personal life. Clinical competence can be achieved in a hospital with a favorable work environment and culture (Benner, 1984). Organizational factors that adversely affect patient satisfaction may include nurse-to-patient ratio, the culture of the practice environment, remuneration, career development, autonomy, relationship and communication patterns, and hospital resources. Hospitals that embrace a culture of desirable work environment and promote nursing autonomy, educational progress, and career advancement have demonstrated reduced patient morbidity and mortality, and a better quality of care (Aiken et al. 2011).
Medical equipment or instrument is among the pivotal components of the healthcare system, i.e. mostly employed by nurses to monitor, diagnose, and treat patients. The process by which a health organization manages its resources concerning equipment, instrument, and other materials has the potential to hinder or promote care delivered by nurses. However, access to efficient medical equipment is a challenge in low- and middle-income countries, like Nigeria. The World Health Organization (WHO) estimated that 50%-80% of medical equipment in developing countries is out of order, creating a barrier to the ability of the healthcare system to deliver health services to patients (Moyimane, Matlala & Kekana 2017).
Proper monitoring of patients can be possible with a balance in the nurse-to-patient ratio. Hospitals with adequate staff and better wages have fewer incidences of burnout, job dissatisfaction, and nurses’ turnover, and better patient care outcomes (ANA, 2017; McHugh & Ma 2014). Higher staffing of competent nurses is associated with a lower hospital-acquired infection, lower incidence of FTR, as well as reduced mortality and hospitalization (Finkelman 2017; McGahan, Kucharski & Coyer 2012). Furthermore, hospitals that embrace a culture of desirable work environment and promote nursing autonomy, educational and career advancement, experience lower burnout of nurses, reduced job dissatisfaction, reduced intent to discontinue the nursing profession, reduced patient morbidity, and mortality, and a better quality of care (Aiken et al. 2011; Weston 2010).
Information sharing between healthcare professionals is essential in developing clinical competence. Appropriate communication encourages collaboration among the healthcare team and helps prevent errors, the commencement of effective treatment plan, prevents complications and even death. Therefore, it is critical for healthcare organizations to assess possible setups for poor communication and be diligent about offering programs and outlets to assist foster team collaboration for improving therapeutic outcomes and the quality of care (Reeves et al. 2008; Reeves et al. 2013; Tsakitzidis et al. 2016; Bailey 2016; Kieft et al. 2014).
Nurses are present in every healthcare setting with greater qualifications and possess a unique role in formulating policy. The quality of care is associated with nurses’ extent of involvement in the plan of care as well as the active and central role they play in the organizational decision or policymaking, and vice versa (Jaafarpour & Khani 2010). The WHO and the International Council of Nurses (ICN) suggested that nurses can and should be involved in policy development by the virtue of their proximity to the patients and education. This is because they can provide valuable policy information and the health policies often directly impact the nurses (Juma, Edwards & Spitzer 2014; Asonye et al. 2019; Gaberson, Oermann & Shellenbarger 2014; Massey, Chaboyer & Aitken 2014; Kunaviktikul et al. 2010).
Studies on the organizational factors associated with nurses’ competence in the averting of FTR cases in Olabisi Onabanjo University Teaching Hospital (OOUTH) Sagamu are scarce; however, recent eyewitness accounts of the state of the hospital with hashtag #SAVEOOUTH is a pointer that injuries and deaths from preventable complications among patients may occur more than likely to be acknowledged by the management. According to an article titled “Restoring Olabisi Onabanjo Varsity Teaching Hospital’s Past Glory” published by THISDAY after its visit on September 25, 2019, the tertiary hospital is in a deplorable state. Thus, it required urgent attention, adding, “most of the medical equipment is obsolete and others are not functional” and “has no working medical equipment for accident victims, besieged with the shortage of staff, insufficient testing kits, and a near-dead maternity ward” (Thisday 2019). With the intent of improving competence in nursing practice, there is a need for research to expound the concept of FTR and identify its associated organizational factors. Accordingly, the present study aimed to determine the organizational factors associated with nurses’ competence in averting FTR in acute care settings. It is hoped that by delving into this complicated clinical problem, the lacunae in the knowledge gap will be illuminated and better understood.
The main objective of the present study was to describe the organizational factors associated with nurses’ competence in averting FTR in acute care settings at OOUTH, Sagamu. The specific objectives of the current research were as follows: assess the knowledge level of the nurses on FTR; determine nurses’ level of competence in averting FTR, and determine the organizational characteristics associated with nurses’ level of competence in averting FTR.
2. Materials and Methods
A descriptive correlational design was used for this study. The study population consisted of about 230 nurses. The target population for this study was 204 registered nurses providing sudden, urgent, and emergency direct care to patients in the acute care settings of the study hospital. The total enumeration method was used to determine the sample frame or size for this research; the study sample was of small size and the study participants shared similar characteristics of interest to the researcher.
A 38-item researcher-made questionnaire was implemented for data collection. The instrument has 4 sections, as follows:
Section A: It contains the respondent’s demographic data as well as questions related to the independent variables –nurses’ educational level, the years of nursing practice, the area of nursing practice, the number of certificated specialty areas, and certificated specialty areas.
Section B: It entails questions to test the nurses’ knowledge on FTR derived from the extensive literature reviewed in this study. This section has 6 items, i.e. knowledge on the definition as well as the contributing factors and preventive measures of FTR. The responses are answered on a true/false scale. The correct and incorrect responses were scored as 1 and 0, respectively; thus, the maximum and minimum attainable scores were 6and 0, respectively. The mean value was used to determine the level of knowledge of the respondents on a further dichotomized scale, as follows:
Low – 0 to 2; Moderate – 3 to 4; High – 5 to 6
Section C: It contains 12 questions on nurses’ opinions regarding their competence in promptly deciphering signs and symptoms, suggestive of patient’s deterioration and appropriately responding to averting FTR in acute care settings. Seven questions were formulated under the category of managing situations and 5 questions under the therapeutic interventions. However, the respondents were expected to assign a score to each statement on a scale of 1-4, with 1 as the lowest score and 4 as the highest score. The maximum score attainable was 48 and the minimum was 12. The nurses’ responses were further dichotomized and assigned a numerical score (mean) depicting their levels of competence in averting FTR, as follows: incompetent (1-12); moderately competent (13-24); competent (25-36), and highly competent (37-48).
Section D: It encompasses 12 questions on organizational characteristics associated with the study nurses’ competence in averting FTR. These questions were adapted from the Practice Environment Scale of the Nursing Work Index (PES-NWI) (Swiger et al. 2017). However, the respondents were expected to assign a score to each statement on a 4-point Likert-type scale (strongly agree, agree, disagree, & strongly disagree), with 1 as the lowest and 4 as the highest scores. The maximum score attainable was 48 and the minimum was 12.
The researcher submitted the questionnaire to the supervisor and 3 expert nurses in Babcock University Teaching Hospital, Ilisan Remo, Ogun State, to make necessary inputs. The internal consistency reliability using Cronbach’s Alpha (α) coefficient (total) was equal to 0.938.
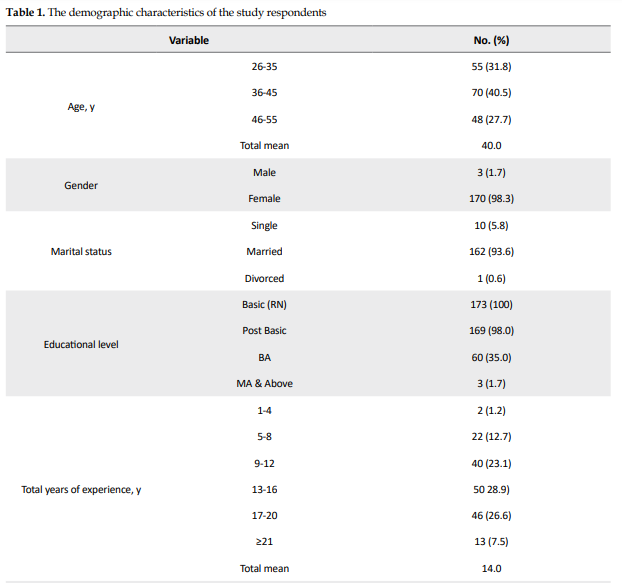
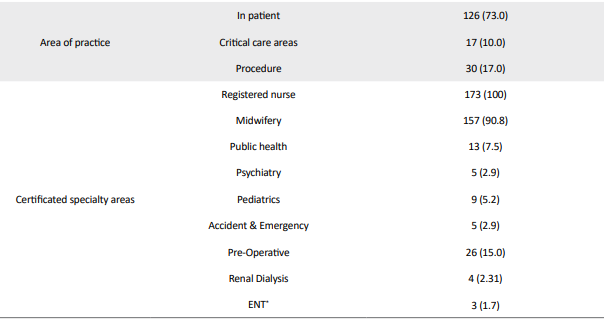
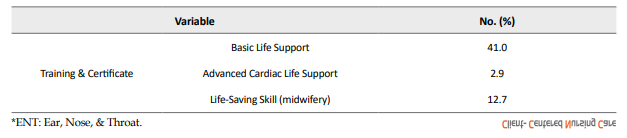
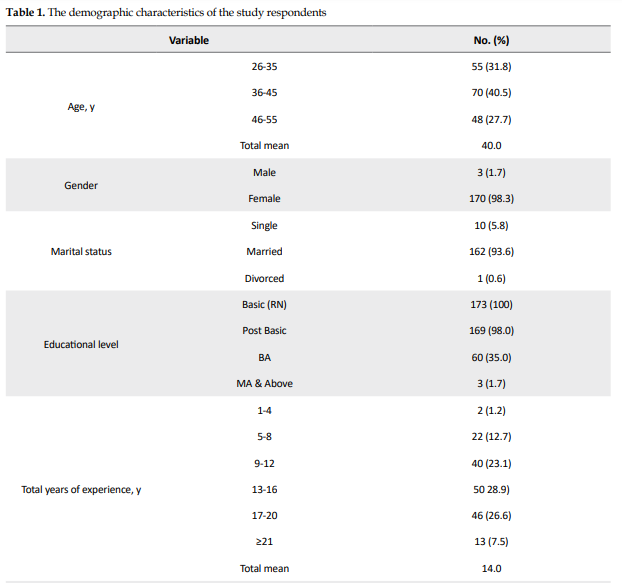
Information retrieved at the end of the study (173 completed questionnaires) was coded; subsequently, statistical analysis was performed in SPSS V. 22. The descriptive statistics included frequency, percentage, mean, standard deviation, and tables. Spearman’s Rho correlation was used to test the hypotheses based on the assumption that the variables are measured on an ordinal scale at P<0.05 (Table 1).
3. Results
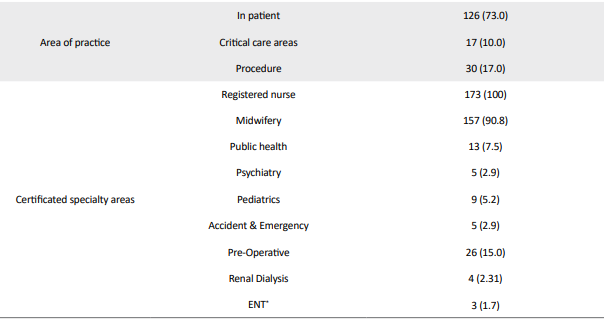
Generally, the respondents’ knowledge regarding FTR was high with a mean score of 5.91 (98.5%). Specifically, the relevant results revealed that the majority (96.5%) of the study participants understood that FTR is a measure of the degree to which a nurse responds to adverse events that develop in a patient under care. Besides, FTR is an outcome measure of the hospital quality of care rendered to hospitalized patients (95.9%) (Table 2).
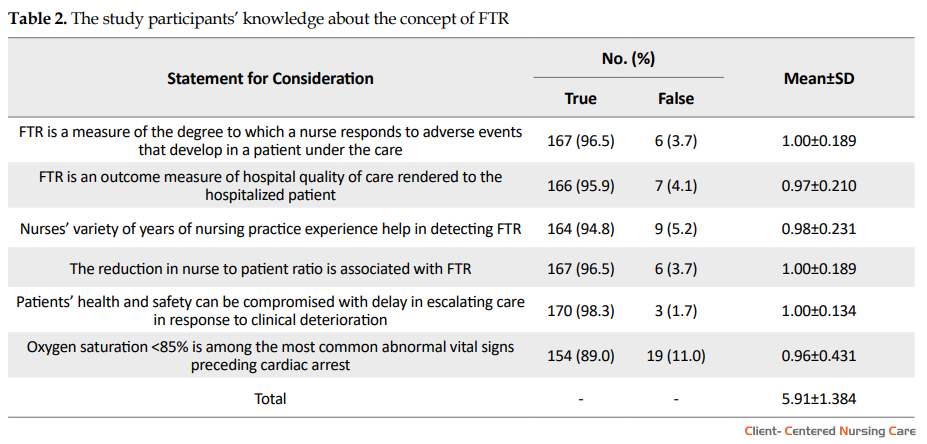
In most (94.8%) of the nurses, the variety of years of nursing practice experience helped in detecting FTR. Other 96.5% of the study subjects believed that the reduction in nurse to patient ratio is associated with FTR. Furthermore, 98.3% of the study subjects indicated that patients’ health and safety can be compromised with delay in escalating care in response to clinical deterioration. Besides, 89.0% of the respondents also indicated that an oxygen saturation of <85% is among the most common abnormal vital signs preceding cardiac arrest.
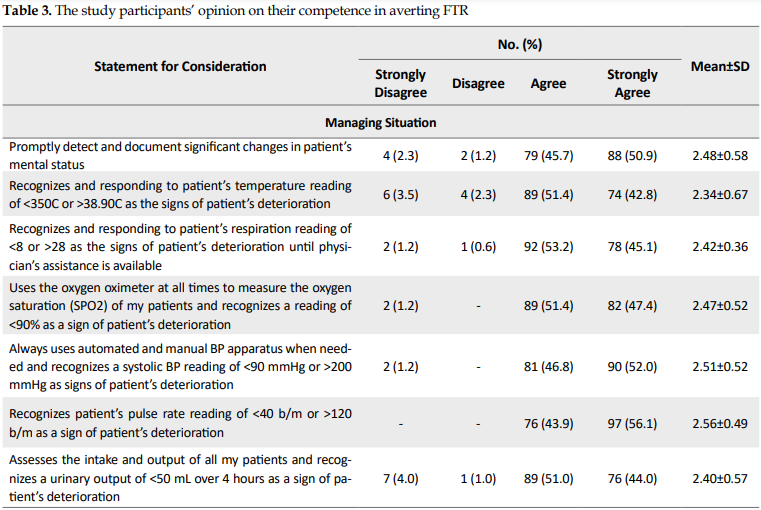
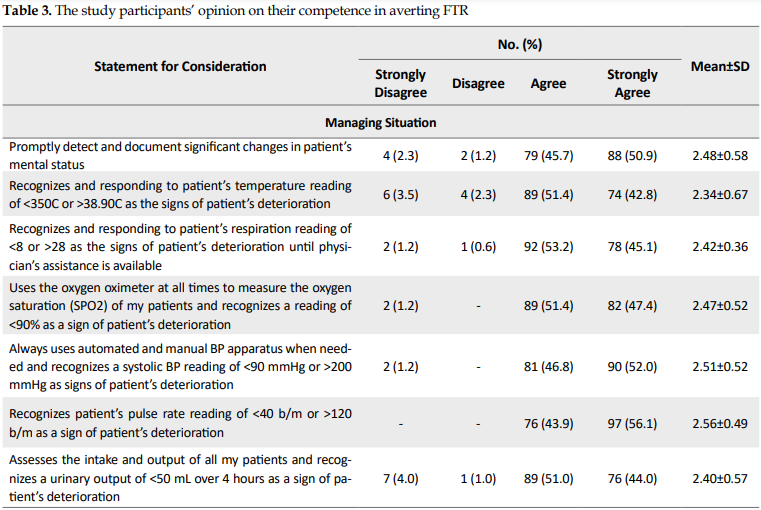
Using the obtained data, an outcome variable summarizing nurses’ competence in averting FTR was created. Generally, the study subjects’ competence in averting FTR was moderate with a mean score of 29.34 measured on a 48-point reference scale (Table 3).
.PNG)
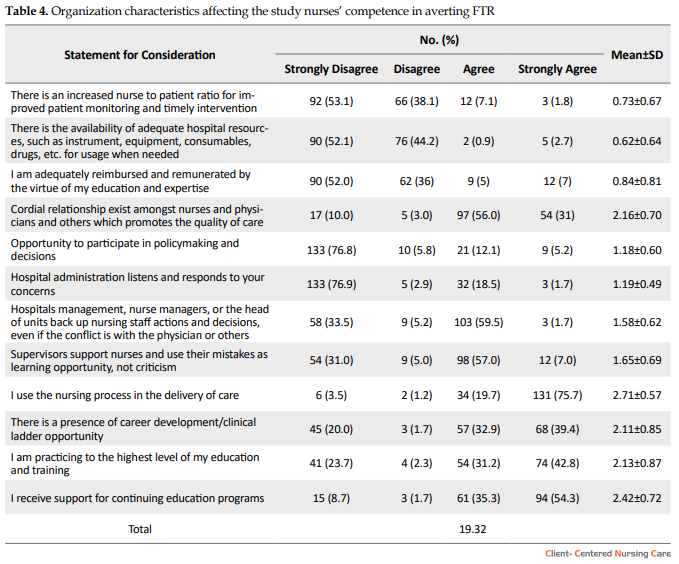
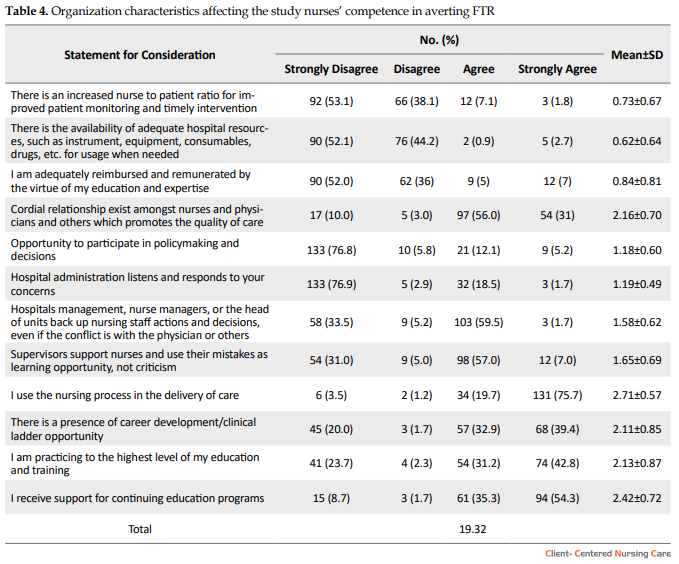
Organizational characteristics affecting nurses’ competence in averting FTR presented a mean value of 19.32 measured on a 48-point reference scale. Thus, organizational factors, such as resource management (manpower and equipment/instrument), remuneration, interrelationship amongst healthcare professionals, and involvement in policymaking, as well as listening and responding to nurses’ concerns have the potential of affecting nurses’ competence in averting FTR in acute care settings.
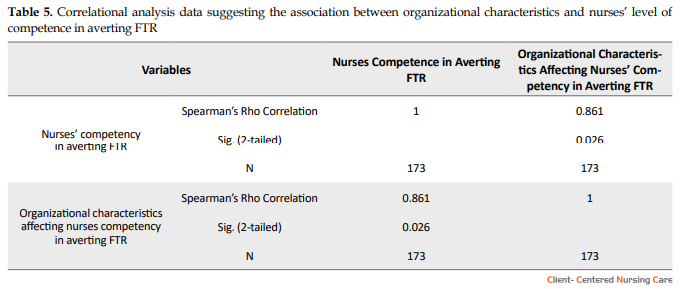
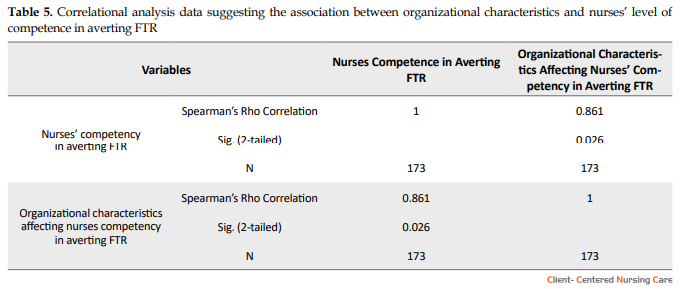
Using a correlation statistical test, the relationship between organizational characteristics and nurses’ competence in averting FTR was computed. Spearman’s Rho correlation coefficient (p)=0.861 and P=0.026 were recorded (Table 4).
The computed result revealed a strong and positive association between organizational characteristics and nurses’ level of competence in averting FTR with a P=0.026 at 0.05 level of significance (Table 5).
4. Discussion
In total, 173 (85%) study subjects (of a sample size of 204) completed the relevant questionnaires. A majority of the study respondents were predominantly female nurses, as it is considered a female profession (Zamanzadeh et al. 2013). A large frequency (98%) of the respondents had the additional post-basic qualifications, i.e. presented to increase knowledge, competence, and confidence (Haskins, Hnatiuk & Yoder 2011). According to Benner, theoretical knowledge has the potential of impacting clinical nursing practice. Thus, the higher a nurse’s level of educational attainment and some specific professional training, the better their clinical competence or expertise. Increased educational preparation for nurses was linked to improved patient care outcomes (McHugh & Lake 2010).
About 86.1% of the research respondents reported a job experience of >9 years. This result was consistent with that of another study (Lehwaldt 2016) suggesting that nurses’ years of experience was associated with the acquisition of expertise, i.e. necessary for better patient outcome. Additionally, approximately 73% of the study respondent worked in the in-patient wards of the hospital; this finding may reflect a growing need for inpatient nurses to take cognizance of the ward complexities involved in the variety of patient’s clinical status, signs, and symptoms of deterioration, as well as nursing actions in those situations.
The research findings indicated that the explored nurses had a high knowledge regarding FTR with a mean score of 5.91 measured on a 6-point referent scale. This may be attributed to post-basic qualifications, increased educational level, and training/certifications in capacity-building skills among the study samples. This finding is consistent with the results of several studies (Blegen et al. 2013; Kendall-Gallagher et al. 2011) that have identified nurses’ educational preparedness and certification in nursing specialty areas as means of increasing nurse’s competence. Furthermore, nurses, irrespective of their educational preparation and experience, possess some knowledge in identifying patient deterioration; however, often fail to respond appropriately (McCarthy et al. 2013).
The nurses’ competence in averting FTR was found to be moderate with a mean score of 29.3 measured on a 48-point reference scale (i.e. an 81% prevalence rate of performance). This implies that 81% of the total respondents’ competence in averting FTR was moderate, but not excellent. This may be attributed to the respondents’ higher educational level, the years of practice, certification in nursing specialty areas, and receiving training in capacity building skills; these were identified by various studies to enhance nurse’s competence in practice (Blegen et al. 2013; Kendall-Gallagher et al. 2011).
A strong positive correlation was detected between organizational characteristics and nurses’ level of competence in averting FTR, i.e. statistically significant (p=0.861; P=0.026). Moreover, these data were consistent with those of the previous studies (Johnston et al. 2015; National Academies of Sciences, Engineering, & Medicine, 2015). Nurses’ competence and work dissatisfaction remained correlated to organizational issues, such as inadequate staffing, salary compression, cohesive nurse-physician relations, nurse-manager support, the lack of opportunity for professional and career advancement, as well as the disregard of nurses’ opinions and inputs (Morgan & Somera 2014).
Additionally, poor resource management concerning manpower and equipment/material by the organization was identified as a bane to the development of competence in averting FTR; this finding was in line with a previous study (Aiken et al. 2014). A higher nurse-to-patient ratio leads to nurses’ job satisfaction, better assessment and monitoring, increased quality of care, and decreased mortality. Previous investigations have linked hospitals staffed with licensed registered nurses to reduced incidence of complication and patient mortality to about one-fifth of the entire hospital patient mortality (Griffiths et al. 2016; Needleman et al. 2011).
Failure of the hospital administration to listen and respond to nurses’ concerns was also elicited in this study as an organizational characteristic associated with nurses’ competence in averting FTR. The present study results corroborated with previous study findings; it was suggested that poor communication patterns and culture within the organization tend to inhibit the acquisition of competence in averting FTR.
Furthermore, low opportunity to participate in policymaking was also revealed as an organizational characteristic associated with the development of competence in averting FTR. Unfavorable policies bothering the range of working time arrangements, such as extended work shifts, night work, on-call scheduling, remuneration, academic, and career advancement adversely impact nursing personnel’s health, work performance, and family life. Policymakers argue that nurses lack the required experience and political skills to participate in policymaking (Akunja et al. 2012). Moreover, previous studies identified some characteristics that hinder nurses’ involvement in policymaking, including inadequate public relation skills to promote nursing, competing priorities, limited time, inadequate resources, and insufficient participation in policy formulation committees (Akunja et al. 2012; Kunaviktikul et al. 2010; Richter et al. 2012). Nurses are present in every healthcare setting with higher degree qualifications and possess a unique role in formulating policy. The WHO and the International Council of Nurses (ICN) indicated that nurses can and should be involved in policy development by the virtue of their proximity to the patients and education, as they can provide valuable policy information, and the health policy often directly impacts the nurses (Kunaviktikul 2014).
The Institute of Medicine’s report “The Future of Nursing: Leading Change, Advancing Health”, identified the value of this pivotal role and called for nurses to assume leadership in improving the quality of healthcare services (Institute of Medicine (IOM) 2011); several leading nursing organizations also promoted the active participation of nurses in policy formulation. For instance, the role of nursing in policymaking was emphasized by the American Association of Colleges of Nursing (AACN) in its “Essentials” documents, which identifies the expected policy involvement that should be incorporated in educational programs at the BA, MA, and doctoral levels of professional nursing, including advanced practice (Thomas, Servello & Williams 2017).
The study results also revealed moderate educational and career advancement support from the organization; accordingly, this is congruent with a previous study finding, revealing that organizations in which nurses work influence their career advancement and competence via empowerment (Coventry, Maslin-Prothero & Smith 2015). A similar study result further revealed that nurses’ healthy work environment act as a facilitator and an unhealthy work environment act as an inhibitor of nurses’ educational and career advancement as well as their competence development.
5. Conclusion
The studied nurses possessed high knowledge and were moderately competent in averting FTR; however, it may be because a majority of them had additional post-basic qualifications and BA degrees, as well as >9 years of practice experience. However, the organizational characteristics, such as resources management (manpower and equipment/material) and communication pattern (support, involvement in policy and decision, interprofessional relationship) tend to influence nurses’ competence in averting FTR. Therefore, organizational characteristics must be modified in the bid to increase nurses’ competence concerning averting FTR in acute care settings.
Workforce issues related to the shortages and effective deployment of professional nurses, and the availability of functional instruments/equipment need to be addressed before the quality of care is further compromised. Additionally, more attention must be paid to developing a positive hospital organizational culture to facilitate the development of competence in identifying early warning signs, suggestive of patient deterioration in acute care settings. This can be achieved by cultivating an environment that promotes nurses’ autonomy, capacity building, and career development, as well as teamwork/collaboration in healthcare professionals. Creating an organization-specific positive culture environment, i.e. tailored to the competencies of nurses in enhancing their independent ability or competence in recognizing subtle cues suggestive of deterioration in the patient’s status in clinical practice would be essential to promote and maintain high levels of patient safety and satisfaction.
Ethical Considerations
Compliance with ethical guidelines
An introduction letter was presented to Olabisi Onabanjo University Teaching Hospital Health Research and Ethics Committee before the commencement of the study and all nurses who wished to participate in the study were duly informed regarding the study and that they have the right and privileges of withdrawing from the study at any time without any penalty. The confidentiality of the participants, as well as the information provided, was guaranteed by the researcher.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The author declared no conflicts of interest.
Acknowledgments
I would like to thank the management of Babcock University Teaching Hospital (BUTH), Ilisan Remo, Ogun State Nigeria, and Olabisi Onabanjo University Teaching Hospital (OOUTH), Sagamu, Ogun State, Nigeria. Finally, I would like to thank Prof. F Ojewole and Dr. J. Wennie for their supervisory roles in this study.
References
Aiken, L. H., et al., 2011. Importance of work environment on hospital outcomes in nine countries. International Journal of Quality in Health Care, 23(4), pp. 357-64. [DOI:10.1093/intqhc/mzr022] [PMID] [PMCID]
Aiken, L. H., et al., 2014. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. The Lancet, 383(9931), pp. 1824-30, [DOI:10.1016/S0140-6736(13)62631-8]
Akunja, E., et al., 2012. Involvement of hub nurses in HIV policy development: Case study of Nyanza province, Kenya. Research in Humanities Social Sciences, 2(6), pp. 24-34. https://www.iiste.org/Journals/index.php/RHSS/article/view/2387
Asonye, Christian C. C., et al., 2019. Factors associated with nurses’ competence in averting failure-to-rescue in acute care settings of a tertiary institution, Ogun State, Nigeria. International Journal of Science & Technoledge, 7(10), pp. 1-21. [DOI:10.24940/theijst/2019/v7/i10/ST1910-004]
Bailey, M., 2016. Communication failures linked to 1,744 deaths in five years, US malpractice study finds [Internet]. Cited 10 March 2018, https://www.statnews.com/2016/02/01/communication-failures-malpractice-study/
Benner, P. A., 1984. From novice to expert: Excellence and power in clinical nursing practice. American Journal of Nursing, 84(12), p. 1479. [DOI:10.1097/00000446-198412000-00025]
Blegen, M. A., et al., 2013. Baccalaureate education in nursing and patient outcome, The Journal of Nursing Administration, 43(2), pp. 89-94 [DOI:10.1097/NNA.0b013e31827f2028] [PMID]
Coventry, T. H., Maslin-Prothero, S. E., & Smith, G., 2015. Organizational impact of nurse supply and workload on nurses continuing professional development opportunities: An integrative review. Journal of Advanced Nursing, 71(12), pp. 2715-27. [DOI:10.1111/jan.12724] [PMID]
Finkelman, A., 2017. Quality improvement: A guide for integration in nursing, Jones & Bartlett Learning, Burlington. https://books.google.com/books?id=Kr3lDQAAQBAJ&dq
Gaberson, K, B., Oermann, H., & Shellenbarger, T., 2014. Clinical teaching strategies in nursing, Springer Publishing, New York. https://books.google.com/books?id=cR7yAgAAQBAJ&dq
Griffiths, P., et al., 2016. Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: A cross-sectional study. BMJ Open, 6(2), p. e008751, [DOI:10.1136/bmjopen-2015-008751] [PMID] [PMCID]
Haskins, M., Hnatiuk, C. N., & Yoder, L. H., 2011. Medical-surgical nurses’ perceived value of certification study. Medsurg Nursing, 20(2), pp, 71-93. [PMID]
Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine. 2011. The future of nursing: Leading change, advancing health, Washington D. C., National Academies Press (US). [DOI:10.17226/12956] [PMID]
Johnston, M. J., et al., 2015. Systematic review to identify the factors that affect failure to rescue and escalation of care in surgery. Surgery, 157(4), pp. 752-63. [DOI:10.1016/j.surg.2014.10.017] [PMID]
Juma, P. A., Edwards, N., & Spitzer, D., 2014. Kenya nurse involvement in national policy development process. Nursing Research and Practice, 2014, p. 236573. [DOI:10.1155/2014/236573] [PMID] [PMCID]
Kendall-Gallagher, D., et al., 2011. Nurse specialty certification, inpatient mortality, and failure-to-rescue. Journal of Nursing Scholarship, 43(2), pp. 188-94. [DOI:10.1111/j.1547-5069.2011.01391.x] [PMID] [PMCID]
Kieft, R., A., et al., 2014. How nurses and their work environment affect patient experiences of the quality of care: A Qualitative Study. BMC Health Services Research, 14, p. 249. [DOI:10.1186/1472-6963-14-249] [PMID] [PMCID]
Kunaviktikul, W., 2014. Moving towards the greater involvement of nurses in policy development. International Nursing Review, 61(1), pp. 1-2. [DOI:10.1111/inr.12092] [PMID]
Kunaviktikul, W., et al., 2010. Knowledge and involvement of nurses regarding health policy development in Thailand. Nursing & Health Sciences, 12(2), pp. 221-7 [DOI:10.1111/j.1442-2018.2010.00523.x] [PMID]
Lehwaldt, D., 2016. The role of nurse education in improving patient outcomes and patient satisfaction with nursing care: A multiple case study of nursing teams in three hospitals across Ireland and Germany [PhD dissertation]. Dublin City University, Dublin. http://doras.dcu.ie/21009/
Massey, D., Chaboyer, W., & Aitken, L., 2014. Nurses’ perceptions of accessing a medical emergency team: A qualitative study. Australian Critical Care, 27(3), pp. 133-8. [DOI:10.1016/j.aucc.2013.11.001] [PMID]
McCarthy, G., et al., 2013, Emergency nurses: Procedures performed and competence in practice. International Emergency Nursing, 21(1), pp. 50-7. [DOI:10.1016/j.ienj.2012.01.003] [PMID]
McGahan, M., Kucharski, G., & Coyer, F., 2012. Nurse staffing levels and the incidence of mortality and morbidity in the adult intensive care unit: A literature review. Australian Critical Care, 25(2), pp. 64-77. [DOI:10.1016/j.aucc.2012.03.003] [PMID]
McHugh, M. D., & Ma, C., 2014. Wage, work environment, and staffing: Effects on nurse outcomes. Policy, Politics & Nursing Practice, 15(3-4), pp. 72-80. [DOI:10.1177/1527154414546868] [PMID] [PMCID]
McHugh, M., D., & Lake, E., T., 2010. Understanding clinical expertise: Nurse Education, experience, and the hospital context. Research in Nursing & Health, 33(4), pp. 276-87. [DOI:10.1002/nur.20388] [PMID] [PMCID]
Moyimane, M. B., Matlala S. F., & Kekana, M. P., 2017. Experience of nurses on the critical shortage of medical equipment at a rural district hospital in South Africa: A qualitative study. The Pan African Medical Journal, 28, p. 100. [DOI:10.11604/pamj.2017.28.100.11641] [PMID] [PMCID]
Jaafarpour, M., & Khani, A., 2010. The participation of nurses in decision making. Journal of Critical and Diagnostic Research, 5(1), pp. 16-9. https://www.jcdr.net/articles/pdf/1107/1468_E(C)_F(J)_R(S)_PF(A)_P(16-19)_LowRes.pdf
Morgan, D., & Somera, P., 2014. The future shortage of doctoral prepaid nurses and the impact on the nursing shortage. Nursing Administration Quarterly, 38(1), pp. 22-6. [DOI:10.1097/NAQ.0000000000000001] [PMID]
National Academies of Sciences, Engineering, & Medicine., 2015. Improving diagnosis in health care. The National Academies Press, Washington D.C. [DOI:10.17226/21794]
Needleman, J., et al., 2011. Nurse staffing and inpatient hospital mortality. New England Journal of Medicine, 364(11), pp. 1037-45. [DOI:10.1056/NEJMsa1001025] [PMID]
Purling, A., & King, L. A., 2012. Literature review: Graduate nurses’ preparedness for recognizing and responding to the deteriorating patient. Journal of Clinical Nursing, 21(23-24), pp. 3451-65. [DOI:10.1111/j.1365-2702.2012.04348.x] [PMID]
Reeves, S., et al., 2008. Interprofessional education: Effect on professional practice and health care outcomes. Cochrane Database Systematic Reviews, 1, p. CD002213. [DOI:10.1002/14651858.CD002213.pub2]
Reeves, S., et al., 2013. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Systematic Reviews, 2013(3), p. CD002213. [DOI:10.1002/14651858.CD002213.pub3] [PMID] [PMCID]
Richter, M, S., et al., 2012. Nurses’ engagement in AIDS policy development. International Nursing Review, 60(1), pp. 52-8. [DOI:10.1111/j.1466-7657.2012.01010.x] [PMID]
Swiger, P. A., et al., 2017. The practice environment scale of the nursing work index: An updated review and recommendations for use. International Journal of Nursing Studies, 74, pp. 76-84. [DOI:10.1016/j.ijnurstu.2017.06.003] [PMID]
Thisday. 2019. Restoring olabisi onabanjo varsity teaching hospital’s past glory. Cited 24 March 2021, https://www.thisdaylive.com/index.php/2019/09/25/restoring-olabisi-onabanjo-varsity-teaching-hospitals-past-glory/
Thomas, P., Servello, D., & Williams, J., 2017. Baccalaureate education: The foundation for healthcare board participation. Nursing Forum, 52(4), pp. 289-97. [DOI:10.1111/nuf.12201] [PMID]
Tsakitzidis, G., et al., 2016. Outcome indicators on interprofessional collaboration interventions for elderly. International Journal of Integrated Care, 16(2), p. 5. [DOI:10.5334/ijic.2017] [PMID] [PMCID]
Weston, M., J., 2010. Strategies for enhancing autonomy and control over nursing practice. The Online Journal of Issues in Nursing, 15(1). http://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol152010/No1Jan2010/Enhancing-Autonomy-and-Control-and-Practice.aspx
Zamanzadeh, V., et al., 2013. Factors influencing men entering the nursing profession, and understanding the challenges faced by them: Iranian and developed countries’ perspectives. Nursing and Midwifery Studies, 2(4), pp. 49-56. [DOI:10.5812/nms.12583] [PMID] [PMCID]
The characteristics of an organization are the main concerns of practice development, especially in the healthcare industry. It has the potential of impacting the employees (nurses) and the patients. Nurses, by their proximity to the patients, are at the frontline of distinguishing alteration in the health status of a patient to improve therapeutic outcomes during patient care. Therefore, they have a profound task of promptly identifying subtle cues; thus, it is suggestive of the patient’s health deterioration and institute measures to avert Failure to Rescue (FTR) (Purling & King 2012).
The concept of FTR entails the idea that not all complications developed by patients are preventable; however, nurses and other healthcare teams should be able to promptly identify and treat complications immediately after they occur. According to the Agency for Healthcare Research and Quality (AHRQ), high-quality hospitals have better chances of averting patient death from complications, even though they care for patient populations with significant surgical risk factors. This is because the variation in complication rates may depend on the patient’s characteristics; such factors may be present on admission, whereas the ability to rescue patients (prevent death from complications) may reflect the resources and preparedness of the organizational characteristics. Such characteristics include resource management, communication pattern, the culture of practice environment, as well as educational and career development.
The organization in which a nurse works has the potential of impacting competence, productivity, and personal life. Clinical competence can be achieved in a hospital with a favorable work environment and culture (Benner, 1984). Organizational factors that adversely affect patient satisfaction may include nurse-to-patient ratio, the culture of the practice environment, remuneration, career development, autonomy, relationship and communication patterns, and hospital resources. Hospitals that embrace a culture of desirable work environment and promote nursing autonomy, educational progress, and career advancement have demonstrated reduced patient morbidity and mortality, and a better quality of care (Aiken et al. 2011).
Medical equipment or instrument is among the pivotal components of the healthcare system, i.e. mostly employed by nurses to monitor, diagnose, and treat patients. The process by which a health organization manages its resources concerning equipment, instrument, and other materials has the potential to hinder or promote care delivered by nurses. However, access to efficient medical equipment is a challenge in low- and middle-income countries, like Nigeria. The World Health Organization (WHO) estimated that 50%-80% of medical equipment in developing countries is out of order, creating a barrier to the ability of the healthcare system to deliver health services to patients (Moyimane, Matlala & Kekana 2017).
Proper monitoring of patients can be possible with a balance in the nurse-to-patient ratio. Hospitals with adequate staff and better wages have fewer incidences of burnout, job dissatisfaction, and nurses’ turnover, and better patient care outcomes (ANA, 2017; McHugh & Ma 2014). Higher staffing of competent nurses is associated with a lower hospital-acquired infection, lower incidence of FTR, as well as reduced mortality and hospitalization (Finkelman 2017; McGahan, Kucharski & Coyer 2012). Furthermore, hospitals that embrace a culture of desirable work environment and promote nursing autonomy, educational and career advancement, experience lower burnout of nurses, reduced job dissatisfaction, reduced intent to discontinue the nursing profession, reduced patient morbidity, and mortality, and a better quality of care (Aiken et al. 2011; Weston 2010).
Information sharing between healthcare professionals is essential in developing clinical competence. Appropriate communication encourages collaboration among the healthcare team and helps prevent errors, the commencement of effective treatment plan, prevents complications and even death. Therefore, it is critical for healthcare organizations to assess possible setups for poor communication and be diligent about offering programs and outlets to assist foster team collaboration for improving therapeutic outcomes and the quality of care (Reeves et al. 2008; Reeves et al. 2013; Tsakitzidis et al. 2016; Bailey 2016; Kieft et al. 2014).
Nurses are present in every healthcare setting with greater qualifications and possess a unique role in formulating policy. The quality of care is associated with nurses’ extent of involvement in the plan of care as well as the active and central role they play in the organizational decision or policymaking, and vice versa (Jaafarpour & Khani 2010). The WHO and the International Council of Nurses (ICN) suggested that nurses can and should be involved in policy development by the virtue of their proximity to the patients and education. This is because they can provide valuable policy information and the health policies often directly impact the nurses (Juma, Edwards & Spitzer 2014; Asonye et al. 2019; Gaberson, Oermann & Shellenbarger 2014; Massey, Chaboyer & Aitken 2014; Kunaviktikul et al. 2010).
Studies on the organizational factors associated with nurses’ competence in the averting of FTR cases in Olabisi Onabanjo University Teaching Hospital (OOUTH) Sagamu are scarce; however, recent eyewitness accounts of the state of the hospital with hashtag #SAVEOOUTH is a pointer that injuries and deaths from preventable complications among patients may occur more than likely to be acknowledged by the management. According to an article titled “Restoring Olabisi Onabanjo Varsity Teaching Hospital’s Past Glory” published by THISDAY after its visit on September 25, 2019, the tertiary hospital is in a deplorable state. Thus, it required urgent attention, adding, “most of the medical equipment is obsolete and others are not functional” and “has no working medical equipment for accident victims, besieged with the shortage of staff, insufficient testing kits, and a near-dead maternity ward” (Thisday 2019). With the intent of improving competence in nursing practice, there is a need for research to expound the concept of FTR and identify its associated organizational factors. Accordingly, the present study aimed to determine the organizational factors associated with nurses’ competence in averting FTR in acute care settings. It is hoped that by delving into this complicated clinical problem, the lacunae in the knowledge gap will be illuminated and better understood.
The main objective of the present study was to describe the organizational factors associated with nurses’ competence in averting FTR in acute care settings at OOUTH, Sagamu. The specific objectives of the current research were as follows: assess the knowledge level of the nurses on FTR; determine nurses’ level of competence in averting FTR, and determine the organizational characteristics associated with nurses’ level of competence in averting FTR.
2. Materials and Methods
A descriptive correlational design was used for this study. The study population consisted of about 230 nurses. The target population for this study was 204 registered nurses providing sudden, urgent, and emergency direct care to patients in the acute care settings of the study hospital. The total enumeration method was used to determine the sample frame or size for this research; the study sample was of small size and the study participants shared similar characteristics of interest to the researcher.
A 38-item researcher-made questionnaire was implemented for data collection. The instrument has 4 sections, as follows:
Section A: It contains the respondent’s demographic data as well as questions related to the independent variables –nurses’ educational level, the years of nursing practice, the area of nursing practice, the number of certificated specialty areas, and certificated specialty areas.
Section B: It entails questions to test the nurses’ knowledge on FTR derived from the extensive literature reviewed in this study. This section has 6 items, i.e. knowledge on the definition as well as the contributing factors and preventive measures of FTR. The responses are answered on a true/false scale. The correct and incorrect responses were scored as 1 and 0, respectively; thus, the maximum and minimum attainable scores were 6and 0, respectively. The mean value was used to determine the level of knowledge of the respondents on a further dichotomized scale, as follows:
Low – 0 to 2; Moderate – 3 to 4; High – 5 to 6
Section C: It contains 12 questions on nurses’ opinions regarding their competence in promptly deciphering signs and symptoms, suggestive of patient’s deterioration and appropriately responding to averting FTR in acute care settings. Seven questions were formulated under the category of managing situations and 5 questions under the therapeutic interventions. However, the respondents were expected to assign a score to each statement on a scale of 1-4, with 1 as the lowest score and 4 as the highest score. The maximum score attainable was 48 and the minimum was 12. The nurses’ responses were further dichotomized and assigned a numerical score (mean) depicting their levels of competence in averting FTR, as follows: incompetent (1-12); moderately competent (13-24); competent (25-36), and highly competent (37-48).
Section D: It encompasses 12 questions on organizational characteristics associated with the study nurses’ competence in averting FTR. These questions were adapted from the Practice Environment Scale of the Nursing Work Index (PES-NWI) (Swiger et al. 2017). However, the respondents were expected to assign a score to each statement on a 4-point Likert-type scale (strongly agree, agree, disagree, & strongly disagree), with 1 as the lowest and 4 as the highest scores. The maximum score attainable was 48 and the minimum was 12.
The researcher submitted the questionnaire to the supervisor and 3 expert nurses in Babcock University Teaching Hospital, Ilisan Remo, Ogun State, to make necessary inputs. The internal consistency reliability using Cronbach’s Alpha (α) coefficient (total) was equal to 0.938.
Information retrieved at the end of the study (173 completed questionnaires) was coded; subsequently, statistical analysis was performed in SPSS V. 22. The descriptive statistics included frequency, percentage, mean, standard deviation, and tables. Spearman’s Rho correlation was used to test the hypotheses based on the assumption that the variables are measured on an ordinal scale at P<0.05 (Table 1).
3. Results
Generally, the respondents’ knowledge regarding FTR was high with a mean score of 5.91 (98.5%). Specifically, the relevant results revealed that the majority (96.5%) of the study participants understood that FTR is a measure of the degree to which a nurse responds to adverse events that develop in a patient under care. Besides, FTR is an outcome measure of the hospital quality of care rendered to hospitalized patients (95.9%) (Table 2).
In most (94.8%) of the nurses, the variety of years of nursing practice experience helped in detecting FTR. Other 96.5% of the study subjects believed that the reduction in nurse to patient ratio is associated with FTR. Furthermore, 98.3% of the study subjects indicated that patients’ health and safety can be compromised with delay in escalating care in response to clinical deterioration. Besides, 89.0% of the respondents also indicated that an oxygen saturation of <85% is among the most common abnormal vital signs preceding cardiac arrest.
Using the obtained data, an outcome variable summarizing nurses’ competence in averting FTR was created. Generally, the study subjects’ competence in averting FTR was moderate with a mean score of 29.34 measured on a 48-point reference scale (Table 3).
.PNG)
Organizational characteristics affecting nurses’ competence in averting FTR presented a mean value of 19.32 measured on a 48-point reference scale. Thus, organizational factors, such as resource management (manpower and equipment/instrument), remuneration, interrelationship amongst healthcare professionals, and involvement in policymaking, as well as listening and responding to nurses’ concerns have the potential of affecting nurses’ competence in averting FTR in acute care settings.
Using a correlation statistical test, the relationship between organizational characteristics and nurses’ competence in averting FTR was computed. Spearman’s Rho correlation coefficient (p)=0.861 and P=0.026 were recorded (Table 4).
The computed result revealed a strong and positive association between organizational characteristics and nurses’ level of competence in averting FTR with a P=0.026 at 0.05 level of significance (Table 5).
4. Discussion
In total, 173 (85%) study subjects (of a sample size of 204) completed the relevant questionnaires. A majority of the study respondents were predominantly female nurses, as it is considered a female profession (Zamanzadeh et al. 2013). A large frequency (98%) of the respondents had the additional post-basic qualifications, i.e. presented to increase knowledge, competence, and confidence (Haskins, Hnatiuk & Yoder 2011). According to Benner, theoretical knowledge has the potential of impacting clinical nursing practice. Thus, the higher a nurse’s level of educational attainment and some specific professional training, the better their clinical competence or expertise. Increased educational preparation for nurses was linked to improved patient care outcomes (McHugh & Lake 2010).
About 86.1% of the research respondents reported a job experience of >9 years. This result was consistent with that of another study (Lehwaldt 2016) suggesting that nurses’ years of experience was associated with the acquisition of expertise, i.e. necessary for better patient outcome. Additionally, approximately 73% of the study respondent worked in the in-patient wards of the hospital; this finding may reflect a growing need for inpatient nurses to take cognizance of the ward complexities involved in the variety of patient’s clinical status, signs, and symptoms of deterioration, as well as nursing actions in those situations.
The research findings indicated that the explored nurses had a high knowledge regarding FTR with a mean score of 5.91 measured on a 6-point referent scale. This may be attributed to post-basic qualifications, increased educational level, and training/certifications in capacity-building skills among the study samples. This finding is consistent with the results of several studies (Blegen et al. 2013; Kendall-Gallagher et al. 2011) that have identified nurses’ educational preparedness and certification in nursing specialty areas as means of increasing nurse’s competence. Furthermore, nurses, irrespective of their educational preparation and experience, possess some knowledge in identifying patient deterioration; however, often fail to respond appropriately (McCarthy et al. 2013).
The nurses’ competence in averting FTR was found to be moderate with a mean score of 29.3 measured on a 48-point reference scale (i.e. an 81% prevalence rate of performance). This implies that 81% of the total respondents’ competence in averting FTR was moderate, but not excellent. This may be attributed to the respondents’ higher educational level, the years of practice, certification in nursing specialty areas, and receiving training in capacity building skills; these were identified by various studies to enhance nurse’s competence in practice (Blegen et al. 2013; Kendall-Gallagher et al. 2011).
A strong positive correlation was detected between organizational characteristics and nurses’ level of competence in averting FTR, i.e. statistically significant (p=0.861; P=0.026). Moreover, these data were consistent with those of the previous studies (Johnston et al. 2015; National Academies of Sciences, Engineering, & Medicine, 2015). Nurses’ competence and work dissatisfaction remained correlated to organizational issues, such as inadequate staffing, salary compression, cohesive nurse-physician relations, nurse-manager support, the lack of opportunity for professional and career advancement, as well as the disregard of nurses’ opinions and inputs (Morgan & Somera 2014).
Additionally, poor resource management concerning manpower and equipment/material by the organization was identified as a bane to the development of competence in averting FTR; this finding was in line with a previous study (Aiken et al. 2014). A higher nurse-to-patient ratio leads to nurses’ job satisfaction, better assessment and monitoring, increased quality of care, and decreased mortality. Previous investigations have linked hospitals staffed with licensed registered nurses to reduced incidence of complication and patient mortality to about one-fifth of the entire hospital patient mortality (Griffiths et al. 2016; Needleman et al. 2011).
Failure of the hospital administration to listen and respond to nurses’ concerns was also elicited in this study as an organizational characteristic associated with nurses’ competence in averting FTR. The present study results corroborated with previous study findings; it was suggested that poor communication patterns and culture within the organization tend to inhibit the acquisition of competence in averting FTR.
Furthermore, low opportunity to participate in policymaking was also revealed as an organizational characteristic associated with the development of competence in averting FTR. Unfavorable policies bothering the range of working time arrangements, such as extended work shifts, night work, on-call scheduling, remuneration, academic, and career advancement adversely impact nursing personnel’s health, work performance, and family life. Policymakers argue that nurses lack the required experience and political skills to participate in policymaking (Akunja et al. 2012). Moreover, previous studies identified some characteristics that hinder nurses’ involvement in policymaking, including inadequate public relation skills to promote nursing, competing priorities, limited time, inadequate resources, and insufficient participation in policy formulation committees (Akunja et al. 2012; Kunaviktikul et al. 2010; Richter et al. 2012). Nurses are present in every healthcare setting with higher degree qualifications and possess a unique role in formulating policy. The WHO and the International Council of Nurses (ICN) indicated that nurses can and should be involved in policy development by the virtue of their proximity to the patients and education, as they can provide valuable policy information, and the health policy often directly impacts the nurses (Kunaviktikul 2014).
The Institute of Medicine’s report “The Future of Nursing: Leading Change, Advancing Health”, identified the value of this pivotal role and called for nurses to assume leadership in improving the quality of healthcare services (Institute of Medicine (IOM) 2011); several leading nursing organizations also promoted the active participation of nurses in policy formulation. For instance, the role of nursing in policymaking was emphasized by the American Association of Colleges of Nursing (AACN) in its “Essentials” documents, which identifies the expected policy involvement that should be incorporated in educational programs at the BA, MA, and doctoral levels of professional nursing, including advanced practice (Thomas, Servello & Williams 2017).
The study results also revealed moderate educational and career advancement support from the organization; accordingly, this is congruent with a previous study finding, revealing that organizations in which nurses work influence their career advancement and competence via empowerment (Coventry, Maslin-Prothero & Smith 2015). A similar study result further revealed that nurses’ healthy work environment act as a facilitator and an unhealthy work environment act as an inhibitor of nurses’ educational and career advancement as well as their competence development.
5. Conclusion
The studied nurses possessed high knowledge and were moderately competent in averting FTR; however, it may be because a majority of them had additional post-basic qualifications and BA degrees, as well as >9 years of practice experience. However, the organizational characteristics, such as resources management (manpower and equipment/material) and communication pattern (support, involvement in policy and decision, interprofessional relationship) tend to influence nurses’ competence in averting FTR. Therefore, organizational characteristics must be modified in the bid to increase nurses’ competence concerning averting FTR in acute care settings.
Workforce issues related to the shortages and effective deployment of professional nurses, and the availability of functional instruments/equipment need to be addressed before the quality of care is further compromised. Additionally, more attention must be paid to developing a positive hospital organizational culture to facilitate the development of competence in identifying early warning signs, suggestive of patient deterioration in acute care settings. This can be achieved by cultivating an environment that promotes nurses’ autonomy, capacity building, and career development, as well as teamwork/collaboration in healthcare professionals. Creating an organization-specific positive culture environment, i.e. tailored to the competencies of nurses in enhancing their independent ability or competence in recognizing subtle cues suggestive of deterioration in the patient’s status in clinical practice would be essential to promote and maintain high levels of patient safety and satisfaction.
Ethical Considerations
Compliance with ethical guidelines
An introduction letter was presented to Olabisi Onabanjo University Teaching Hospital Health Research and Ethics Committee before the commencement of the study and all nurses who wished to participate in the study were duly informed regarding the study and that they have the right and privileges of withdrawing from the study at any time without any penalty. The confidentiality of the participants, as well as the information provided, was guaranteed by the researcher.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The author declared no conflicts of interest.
Acknowledgments
I would like to thank the management of Babcock University Teaching Hospital (BUTH), Ilisan Remo, Ogun State Nigeria, and Olabisi Onabanjo University Teaching Hospital (OOUTH), Sagamu, Ogun State, Nigeria. Finally, I would like to thank Prof. F Ojewole and Dr. J. Wennie for their supervisory roles in this study.
References
Aiken, L. H., et al., 2011. Importance of work environment on hospital outcomes in nine countries. International Journal of Quality in Health Care, 23(4), pp. 357-64. [DOI:10.1093/intqhc/mzr022] [PMID] [PMCID]
Aiken, L. H., et al., 2014. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. The Lancet, 383(9931), pp. 1824-30, [DOI:10.1016/S0140-6736(13)62631-8]
Akunja, E., et al., 2012. Involvement of hub nurses in HIV policy development: Case study of Nyanza province, Kenya. Research in Humanities Social Sciences, 2(6), pp. 24-34. https://www.iiste.org/Journals/index.php/RHSS/article/view/2387
Asonye, Christian C. C., et al., 2019. Factors associated with nurses’ competence in averting failure-to-rescue in acute care settings of a tertiary institution, Ogun State, Nigeria. International Journal of Science & Technoledge, 7(10), pp. 1-21. [DOI:10.24940/theijst/2019/v7/i10/ST1910-004]
Bailey, M., 2016. Communication failures linked to 1,744 deaths in five years, US malpractice study finds [Internet]. Cited 10 March 2018, https://www.statnews.com/2016/02/01/communication-failures-malpractice-study/
Benner, P. A., 1984. From novice to expert: Excellence and power in clinical nursing practice. American Journal of Nursing, 84(12), p. 1479. [DOI:10.1097/00000446-198412000-00025]
Blegen, M. A., et al., 2013. Baccalaureate education in nursing and patient outcome, The Journal of Nursing Administration, 43(2), pp. 89-94 [DOI:10.1097/NNA.0b013e31827f2028] [PMID]
Coventry, T. H., Maslin-Prothero, S. E., & Smith, G., 2015. Organizational impact of nurse supply and workload on nurses continuing professional development opportunities: An integrative review. Journal of Advanced Nursing, 71(12), pp. 2715-27. [DOI:10.1111/jan.12724] [PMID]
Finkelman, A., 2017. Quality improvement: A guide for integration in nursing, Jones & Bartlett Learning, Burlington. https://books.google.com/books?id=Kr3lDQAAQBAJ&dq
Gaberson, K, B., Oermann, H., & Shellenbarger, T., 2014. Clinical teaching strategies in nursing, Springer Publishing, New York. https://books.google.com/books?id=cR7yAgAAQBAJ&dq
Griffiths, P., et al., 2016. Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: A cross-sectional study. BMJ Open, 6(2), p. e008751, [DOI:10.1136/bmjopen-2015-008751] [PMID] [PMCID]
Haskins, M., Hnatiuk, C. N., & Yoder, L. H., 2011. Medical-surgical nurses’ perceived value of certification study. Medsurg Nursing, 20(2), pp, 71-93. [PMID]
Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine. 2011. The future of nursing: Leading change, advancing health, Washington D. C., National Academies Press (US). [DOI:10.17226/12956] [PMID]
Johnston, M. J., et al., 2015. Systematic review to identify the factors that affect failure to rescue and escalation of care in surgery. Surgery, 157(4), pp. 752-63. [DOI:10.1016/j.surg.2014.10.017] [PMID]
Juma, P. A., Edwards, N., & Spitzer, D., 2014. Kenya nurse involvement in national policy development process. Nursing Research and Practice, 2014, p. 236573. [DOI:10.1155/2014/236573] [PMID] [PMCID]
Kendall-Gallagher, D., et al., 2011. Nurse specialty certification, inpatient mortality, and failure-to-rescue. Journal of Nursing Scholarship, 43(2), pp. 188-94. [DOI:10.1111/j.1547-5069.2011.01391.x] [PMID] [PMCID]
Kieft, R., A., et al., 2014. How nurses and their work environment affect patient experiences of the quality of care: A Qualitative Study. BMC Health Services Research, 14, p. 249. [DOI:10.1186/1472-6963-14-249] [PMID] [PMCID]
Kunaviktikul, W., 2014. Moving towards the greater involvement of nurses in policy development. International Nursing Review, 61(1), pp. 1-2. [DOI:10.1111/inr.12092] [PMID]
Kunaviktikul, W., et al., 2010. Knowledge and involvement of nurses regarding health policy development in Thailand. Nursing & Health Sciences, 12(2), pp. 221-7 [DOI:10.1111/j.1442-2018.2010.00523.x] [PMID]
Lehwaldt, D., 2016. The role of nurse education in improving patient outcomes and patient satisfaction with nursing care: A multiple case study of nursing teams in three hospitals across Ireland and Germany [PhD dissertation]. Dublin City University, Dublin. http://doras.dcu.ie/21009/
Massey, D., Chaboyer, W., & Aitken, L., 2014. Nurses’ perceptions of accessing a medical emergency team: A qualitative study. Australian Critical Care, 27(3), pp. 133-8. [DOI:10.1016/j.aucc.2013.11.001] [PMID]
McCarthy, G., et al., 2013, Emergency nurses: Procedures performed and competence in practice. International Emergency Nursing, 21(1), pp. 50-7. [DOI:10.1016/j.ienj.2012.01.003] [PMID]
McGahan, M., Kucharski, G., & Coyer, F., 2012. Nurse staffing levels and the incidence of mortality and morbidity in the adult intensive care unit: A literature review. Australian Critical Care, 25(2), pp. 64-77. [DOI:10.1016/j.aucc.2012.03.003] [PMID]
McHugh, M. D., & Ma, C., 2014. Wage, work environment, and staffing: Effects on nurse outcomes. Policy, Politics & Nursing Practice, 15(3-4), pp. 72-80. [DOI:10.1177/1527154414546868] [PMID] [PMCID]
McHugh, M., D., & Lake, E., T., 2010. Understanding clinical expertise: Nurse Education, experience, and the hospital context. Research in Nursing & Health, 33(4), pp. 276-87. [DOI:10.1002/nur.20388] [PMID] [PMCID]
Moyimane, M. B., Matlala S. F., & Kekana, M. P., 2017. Experience of nurses on the critical shortage of medical equipment at a rural district hospital in South Africa: A qualitative study. The Pan African Medical Journal, 28, p. 100. [DOI:10.11604/pamj.2017.28.100.11641] [PMID] [PMCID]
Jaafarpour, M., & Khani, A., 2010. The participation of nurses in decision making. Journal of Critical and Diagnostic Research, 5(1), pp. 16-9. https://www.jcdr.net/articles/pdf/1107/1468_E(C)_F(J)_R(S)_PF(A)_P(16-19)_LowRes.pdf
Morgan, D., & Somera, P., 2014. The future shortage of doctoral prepaid nurses and the impact on the nursing shortage. Nursing Administration Quarterly, 38(1), pp. 22-6. [DOI:10.1097/NAQ.0000000000000001] [PMID]
National Academies of Sciences, Engineering, & Medicine., 2015. Improving diagnosis in health care. The National Academies Press, Washington D.C. [DOI:10.17226/21794]
Needleman, J., et al., 2011. Nurse staffing and inpatient hospital mortality. New England Journal of Medicine, 364(11), pp. 1037-45. [DOI:10.1056/NEJMsa1001025] [PMID]
Purling, A., & King, L. A., 2012. Literature review: Graduate nurses’ preparedness for recognizing and responding to the deteriorating patient. Journal of Clinical Nursing, 21(23-24), pp. 3451-65. [DOI:10.1111/j.1365-2702.2012.04348.x] [PMID]
Reeves, S., et al., 2008. Interprofessional education: Effect on professional practice and health care outcomes. Cochrane Database Systematic Reviews, 1, p. CD002213. [DOI:10.1002/14651858.CD002213.pub2]
Reeves, S., et al., 2013. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Systematic Reviews, 2013(3), p. CD002213. [DOI:10.1002/14651858.CD002213.pub3] [PMID] [PMCID]
Richter, M, S., et al., 2012. Nurses’ engagement in AIDS policy development. International Nursing Review, 60(1), pp. 52-8. [DOI:10.1111/j.1466-7657.2012.01010.x] [PMID]
Swiger, P. A., et al., 2017. The practice environment scale of the nursing work index: An updated review and recommendations for use. International Journal of Nursing Studies, 74, pp. 76-84. [DOI:10.1016/j.ijnurstu.2017.06.003] [PMID]
Thisday. 2019. Restoring olabisi onabanjo varsity teaching hospital’s past glory. Cited 24 March 2021, https://www.thisdaylive.com/index.php/2019/09/25/restoring-olabisi-onabanjo-varsity-teaching-hospitals-past-glory/
Thomas, P., Servello, D., & Williams, J., 2017. Baccalaureate education: The foundation for healthcare board participation. Nursing Forum, 52(4), pp. 289-97. [DOI:10.1111/nuf.12201] [PMID]
Tsakitzidis, G., et al., 2016. Outcome indicators on interprofessional collaboration interventions for elderly. International Journal of Integrated Care, 16(2), p. 5. [DOI:10.5334/ijic.2017] [PMID] [PMCID]
Weston, M., J., 2010. Strategies for enhancing autonomy and control over nursing practice. The Online Journal of Issues in Nursing, 15(1). http://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol152010/No1Jan2010/Enhancing-Autonomy-and-Control-and-Practice.aspx
Zamanzadeh, V., et al., 2013. Factors influencing men entering the nursing profession, and understanding the challenges faced by them: Iranian and developed countries’ perspectives. Nursing and Midwifery Studies, 2(4), pp. 49-56. [DOI:10.5812/nms.12583] [PMID] [PMCID]
Type of Study: Research |
Subject:
General
Received: 2020/03/13 | Accepted: 2020/08/14 | Published: 2021/02/1
Received: 2020/03/13 | Accepted: 2020/08/14 | Published: 2021/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |