Sat, Jul 27, 2024
[Archive]
Volume 8, Issue 1 (Winter 2022)
JCCNC 2022, 8(1): 23-32 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abeasi D A, Abugri D, Akumiah P O. Predictors of Medication Adherence Among Adults With Hypertension in Ghana. JCCNC 2022; 8 (1) :23-32
URL: http://jccnc.iums.ac.ir/article-1-333-en.html
URL: http://jccnc.iums.ac.ir/article-1-333-en.html
1- Department of Nursing and Midwifery, Presbyterian University College, Abetefi, Ghana. , reenasantewa@gmail.com
2- Department of Nursing and Midwifery, Presbyterian University College, Abetefi, Ghana.
2- Department of Nursing and Midwifery, Presbyterian University College, Abetefi, Ghana.
Full-Text [PDF 667 kb]
(788 Downloads)
| Abstract (HTML) (2087 Views)
Full-Text: (906 Views)
1. Introduction
Globally, the estimates regarding the total number of people living with hypertension are considered high. A recent study suggests that people with high blood pressure increased from 594 million in 1975 to approximately 1.13 billion in 2015. Out of this number, low- and middle-income countries contribute to a majority of the cases (NCD Risk Factor Collaboration [NCD-RisC], 2017). The prevalence of hypertension in Africa is higher than in Europe and the USA (van de Vijver et al., 2013), suggesting an increased burden, which requires proper awareness, control, and management among those diagnosed with hypertension. To achieve long-lasting control of hypertension, the recommended therapy is the use of antihypertensive medications (Alsolami, Hou, & Correa-Velez, 2015). One of the indispensable tools in making this therapy successful is the adherence to antihypertensive drugs (Choi et al., 2018; Bochkareva et al., 2019). Adherence is described as the degree to which the behavior of an individual’s medication-taking correlates with the advice given by a healthcare professional in managing a disease (Lee, Jang, & Park, 2017; Dillon et al., 2018). This behavior is associated with good clinical outcomes (Chowdhury et al., 2013).
On the other hand, non-adherence is associated with poor blood pressure control and poor clinical outcomes. Lee, Jang, and Park (2017) reported that patients with intermediate or poor adherence to antihypertensive medication had 1.13 times and 1.27 times higher risk of stroke, respectively than those with high adherence. Additionally, patients with non-adherence to antihypertensive medication have higher odds of cerebrovascular disease-related hospitalization, emergency department visits, treatment failure (Pittman et al., 2010; Shin et al., 2013; Kolandaivelu, 2014), myocardial infarction, heart failure, and cardiovascular-related deaths (Lee et al., 2021). Non-adherence to antihypertensive medication could occur due to drug-related factors or patient-related factors (Lee, Jang & Park, 2017). Drug-related factors include side effects like sexual dysfunction associated with antihypertensive usage (Kretchy et al., 2015) and the number and types of medications taken by the patient (Lee, Jang & Park, 2017). Patient-related factors include emotional factors (Bautista et al., 2012), age, sex, and income (Bader et al., 2015; Lo et al., 2016; Khwaja, Ansari, & Mehnaz, 2017; Okai et al., 2020). Owing to the diversity of factors contributing to non-adherence and its unfavorable results, it is important to identify factors contributing to non-adherence to mitigate its adverse outcomes.
In this regard, some studies have been conducted in the Ghanaian context. However, the reported level of non-adherence to antihypertensive medications in Ghana varies across studies (52%-93%) (Buabeng, Motowe & Plangue-Rule, 2004; Boima et al., 2015). Other studies conducted in Ghana have looked at hypertension control and not necessarily adherence to antihypertensive medications (Okai et al., 2020). Most studies have been conducted in the southern part of Ghana (Okai et al., 2020; Kretchy et al., 2015; Atinga, Yarney, & Gavu, 2018). Some studies have also considered adherence only in male hypertensive patients (Kretchy et al., 2015). The current study, however, aims at bridging the gap in three main ways. First, the study used a more reliable and valid tool for assessing the level of adherence. Most studies were done in the Ghanaian context used researcher-made self-report tools for measuring the level of non-adherence, which has its limitations. Furthermore, the study was conducted in the northern part of the country, which may have different predictors than those done in the southern belt of the country. This difference may be due to the socio-economic differences between the two geographical areas. Third, the study was conducted in a setting that serves rural communities. In a systematic review, it was reported that the burden of hypertension in the urban communities was higher than the rural (Atibila et al., 2021). However, the authors conclude that the gap between the two are gradually closing up. Based on this premise, the study investigates the predictors of medication adherence among adult patients with hypertension referring to the Hypertension Clinic of the Bawku Presbyterian Hospital in Ghana.
On the other hand, non-adherence is associated with poor blood pressure control and poor clinical outcomes. Lee, Jang, and Park (2017) reported that patients with intermediate or poor adherence to antihypertensive medication had 1.13 times and 1.27 times higher risk of stroke, respectively than those with high adherence. Additionally, patients with non-adherence to antihypertensive medication have higher odds of cerebrovascular disease-related hospitalization, emergency department visits, treatment failure (Pittman et al., 2010; Shin et al., 2013; Kolandaivelu, 2014), myocardial infarction, heart failure, and cardiovascular-related deaths (Lee et al., 2021). Non-adherence to antihypertensive medication could occur due to drug-related factors or patient-related factors (Lee, Jang & Park, 2017). Drug-related factors include side effects like sexual dysfunction associated with antihypertensive usage (Kretchy et al., 2015) and the number and types of medications taken by the patient (Lee, Jang & Park, 2017). Patient-related factors include emotional factors (Bautista et al., 2012), age, sex, and income (Bader et al., 2015; Lo et al., 2016; Khwaja, Ansari, & Mehnaz, 2017; Okai et al., 2020). Owing to the diversity of factors contributing to non-adherence and its unfavorable results, it is important to identify factors contributing to non-adherence to mitigate its adverse outcomes.
In this regard, some studies have been conducted in the Ghanaian context. However, the reported level of non-adherence to antihypertensive medications in Ghana varies across studies (52%-93%) (Buabeng, Motowe & Plangue-Rule, 2004; Boima et al., 2015). Other studies conducted in Ghana have looked at hypertension control and not necessarily adherence to antihypertensive medications (Okai et al., 2020). Most studies have been conducted in the southern part of Ghana (Okai et al., 2020; Kretchy et al., 2015; Atinga, Yarney, & Gavu, 2018). Some studies have also considered adherence only in male hypertensive patients (Kretchy et al., 2015). The current study, however, aims at bridging the gap in three main ways. First, the study used a more reliable and valid tool for assessing the level of adherence. Most studies were done in the Ghanaian context used researcher-made self-report tools for measuring the level of non-adherence, which has its limitations. Furthermore, the study was conducted in the northern part of the country, which may have different predictors than those done in the southern belt of the country. This difference may be due to the socio-economic differences between the two geographical areas. Third, the study was conducted in a setting that serves rural communities. In a systematic review, it was reported that the burden of hypertension in the urban communities was higher than the rural (Atibila et al., 2021). However, the authors conclude that the gap between the two are gradually closing up. Based on this premise, the study investigates the predictors of medication adherence among adult patients with hypertension referring to the Hypertension Clinic of the Bawku Presbyterian Hospital in Ghana.
2. Materials and Methods
Study design
This study employed a cross-sectional design. The researchers assessed the sample at one specific period (March to May 2020) for a defined population.
Setting and sample
The study was conducted in Bawku Presbyterian Hospital among adult hypertensive patients. Bawku Presbyterian Hospital is a district hospital located in the Bawku East District, in the Upper East Region of Ghana. The hospital is managed by the Presbyterian Church of Ghana and serves mainly farming communities, and runs a Hypertensive Clinic on Wednesdays. The average clinic attendance per week is 80 patients. Individuals diagnosed with hypertension who were 18 years or older and on antihypertensive medications for at least six months were included in the study.
Sampling procedure
The sample size was estimated using Yamane’s formula (1967) for calculating sample size. Based on the hypertension clinic medical records, it was estimated that 817 patients with hypertension seek treatment in the facility. Using the study’s population size, the calculated sample size was 269 (at 95% confidence and 5% margin of error). Considering the daily attendance at the hypertensive clinic and the targeted sample size to be collected, every patient who fulfilled the inclusion criteria was enrolled. Patients were approached during the clinic visits using the convenience sampling method until the required sample size was reached.
Data collection
The study data were collected from March to May 2020 using a self-administered questionnaire that was well-reviewed and pre-tested before the study. The questionnaire included three sections:
Section A was a researcher-made form seeking the sociodemographic information of the study participants.
Section B was the Hill-Bone Medication Adherence Scale (HB-MAS). The scale measures adherence to medication in hypertensive patients. HB-MAS consists of 9 questions, such as “how often do you forget to take your medication”. The scale is scored on a 4-point Likert scale ranging from “none of the time”=1 to “all the time”=4. The items on the scale are summed up to produce an overall adherence score of 9 to 36 (Koschack, et al., 2010). Higher scores indicate poor adherence to an antihypertensive medication regimen and vice versa. Adherence level was divided into two: perfect adherence (score of 9) and imperfect adherence (score of >9-36). All responses for “some of the time, most of the time, and all of the time” were grouped and coded as imperfect adherence. On the other hand, “none of the time” responses were grouped and coded as perfect adherence. This classification was based on a previous study that used the HB-MAS since the authors of the scale do not provide strict categorization (Koschack, et al., 2010). The validity and internal consistency for a modified Hill-Bone compliance scale have been confirmed in black, urban, hypertensive, South African patients (standardized Cronbach α=0.74-0.84) (Lambert et al., 2006). Before using the questionnaire, it was subjected to evaluation. The Cronbach α was calculated to be 0.795, reflecting good internal consistency and reliability of the HB-MAS.
Section C examined perceived factors influencing medication adherence. The inclusion of factors in the questionnaire was guided by the findings of previous studies. The questionnaire was developed by the researchers and comprised six items. Participants were required to agree or disagree with statements in the questionnaire. Before using the questionnaire, it was subjected to evaluation. The Cronbach α was calculated to be 0.81, reflecting good internal consistency and reliability.
Data analysis
SPSS software v. 22.0 (IBM Corporation, Armonk, NY, USA) was used for data analysis. The normality of the data was determined using the Kolmogorov-Smirnov test. The level of significance for all inferential statistics was set at 0.05. Regression analysis was done to determine factors that could predict medication adherence. Descriptive statistics of the demographic variables and influencing factors were described using frequencies and percentages.
This study employed a cross-sectional design. The researchers assessed the sample at one specific period (March to May 2020) for a defined population.
Setting and sample
The study was conducted in Bawku Presbyterian Hospital among adult hypertensive patients. Bawku Presbyterian Hospital is a district hospital located in the Bawku East District, in the Upper East Region of Ghana. The hospital is managed by the Presbyterian Church of Ghana and serves mainly farming communities, and runs a Hypertensive Clinic on Wednesdays. The average clinic attendance per week is 80 patients. Individuals diagnosed with hypertension who were 18 years or older and on antihypertensive medications for at least six months were included in the study.
Sampling procedure
The sample size was estimated using Yamane’s formula (1967) for calculating sample size. Based on the hypertension clinic medical records, it was estimated that 817 patients with hypertension seek treatment in the facility. Using the study’s population size, the calculated sample size was 269 (at 95% confidence and 5% margin of error). Considering the daily attendance at the hypertensive clinic and the targeted sample size to be collected, every patient who fulfilled the inclusion criteria was enrolled. Patients were approached during the clinic visits using the convenience sampling method until the required sample size was reached.
Data collection
The study data were collected from March to May 2020 using a self-administered questionnaire that was well-reviewed and pre-tested before the study. The questionnaire included three sections:
Section A was a researcher-made form seeking the sociodemographic information of the study participants.
Section B was the Hill-Bone Medication Adherence Scale (HB-MAS). The scale measures adherence to medication in hypertensive patients. HB-MAS consists of 9 questions, such as “how often do you forget to take your medication”. The scale is scored on a 4-point Likert scale ranging from “none of the time”=1 to “all the time”=4. The items on the scale are summed up to produce an overall adherence score of 9 to 36 (Koschack, et al., 2010). Higher scores indicate poor adherence to an antihypertensive medication regimen and vice versa. Adherence level was divided into two: perfect adherence (score of 9) and imperfect adherence (score of >9-36). All responses for “some of the time, most of the time, and all of the time” were grouped and coded as imperfect adherence. On the other hand, “none of the time” responses were grouped and coded as perfect adherence. This classification was based on a previous study that used the HB-MAS since the authors of the scale do not provide strict categorization (Koschack, et al., 2010). The validity and internal consistency for a modified Hill-Bone compliance scale have been confirmed in black, urban, hypertensive, South African patients (standardized Cronbach α=0.74-0.84) (Lambert et al., 2006). Before using the questionnaire, it was subjected to evaluation. The Cronbach α was calculated to be 0.795, reflecting good internal consistency and reliability of the HB-MAS.
Section C examined perceived factors influencing medication adherence. The inclusion of factors in the questionnaire was guided by the findings of previous studies. The questionnaire was developed by the researchers and comprised six items. Participants were required to agree or disagree with statements in the questionnaire. Before using the questionnaire, it was subjected to evaluation. The Cronbach α was calculated to be 0.81, reflecting good internal consistency and reliability.
Data analysis
SPSS software v. 22.0 (IBM Corporation, Armonk, NY, USA) was used for data analysis. The normality of the data was determined using the Kolmogorov-Smirnov test. The level of significance for all inferential statistics was set at 0.05. Regression analysis was done to determine factors that could predict medication adherence. Descriptive statistics of the demographic variables and influencing factors were described using frequencies and percentages.
3. Results
Table 1 presents that the majority of the participants were above 40 years (87.4%), males (60.2%), Christians (85.1%), cohabited, or married (63.5%). Most patients had below senior high school education (62.0%), farming/trading jobs (75.8%), paid for their medication themselves or by friends/family (63.2%). Most had lived with the disease for more than 8 years (59.1%) and had a monthly income below 700 cedis (79.2%).
.jpg)
The findings showed that 40.5% have perfectly adhered to antihypertensive medicines, while the adherence was imperfect in 59.5% of the subjects (Table 2).
.jpg)
Results from the regression analysis showed a positive correlation (r=0.721) between medication adherence and variables of educational level (P=0.0001), monthly income (P=0.003), duration of being on antihypertensive medication (P=0.021). However, no significant relationship (P=0.134) was found between age and medication adherence (Table 3).
.jpg)
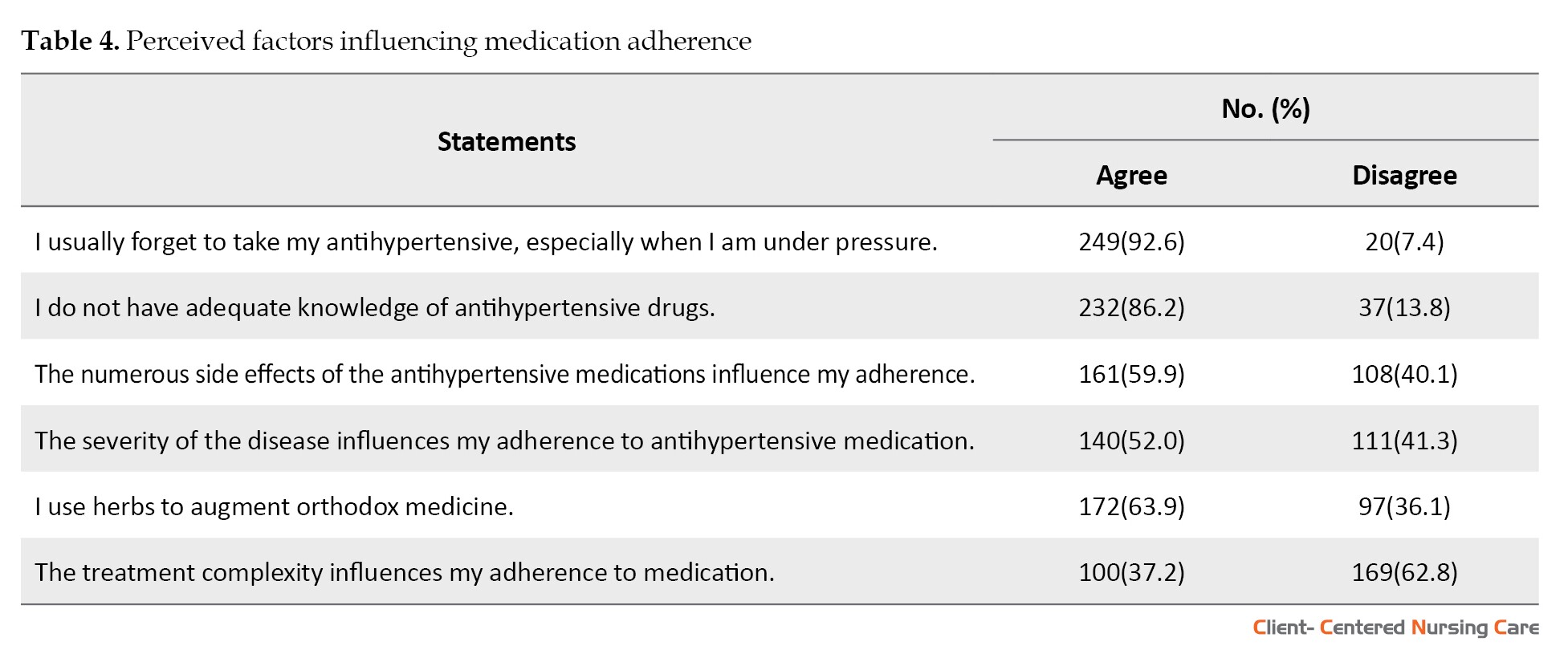
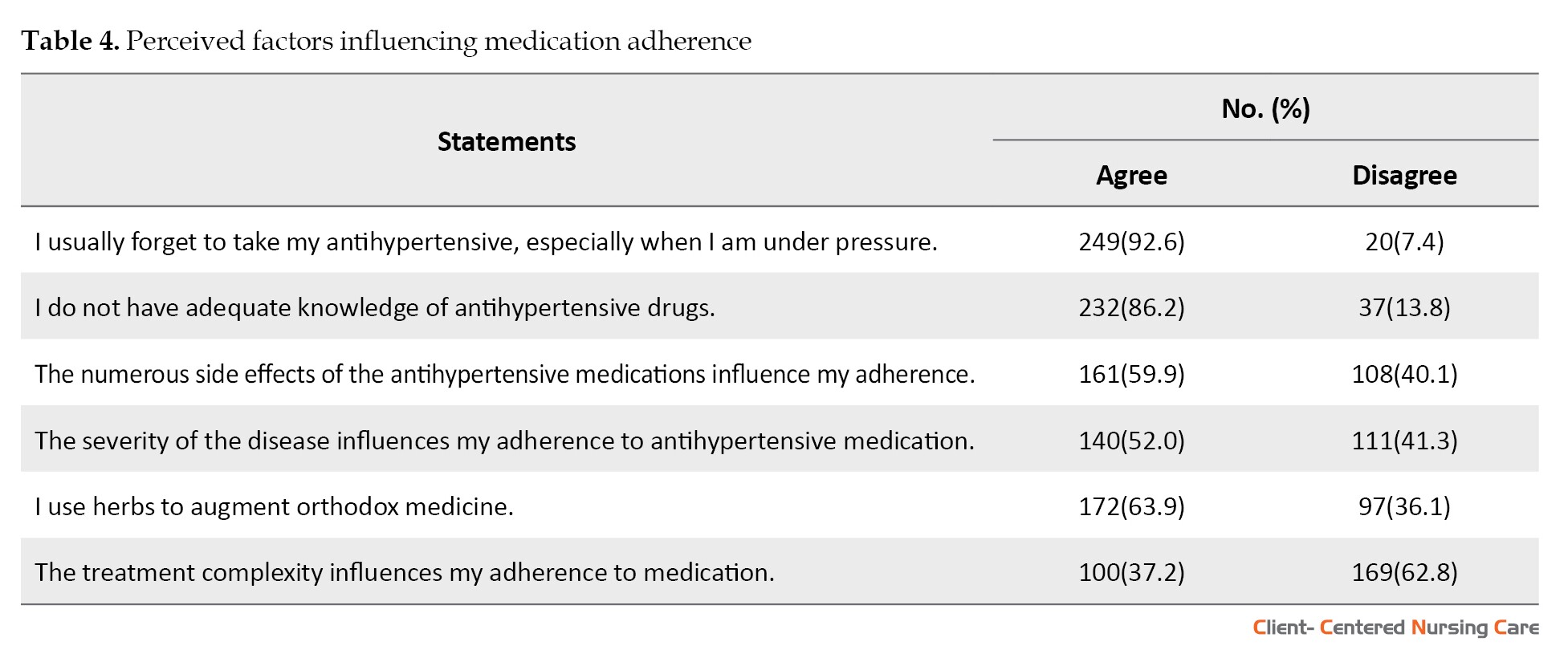
The findings of the study indicated that forgetfulness was the main factor influencing adherence to antihypertensive medication (92.6%), followed by inadequate knowledge (86.2%) (Table 4).
.jpg)
The findings showed that 40.5% have perfectly adhered to antihypertensive medicines, while the adherence was imperfect in 59.5% of the subjects (Table 2).
.jpg)
Results from the regression analysis showed a positive correlation (r=0.721) between medication adherence and variables of educational level (P=0.0001), monthly income (P=0.003), duration of being on antihypertensive medication (P=0.021). However, no significant relationship (P=0.134) was found between age and medication adherence (Table 3).
.jpg)
The findings of the study indicated that forgetfulness was the main factor influencing adherence to antihypertensive medication (92.6%), followed by inadequate knowledge (86.2%) (Table 4).
4. Discussion
Adherence to medication, especially in patients with chronic conditions, will result in positive outcomes. The current study sought to identify predictors of medication adherence and related factors influencing hypertensive patients referring to the outpatient clinic at the Bawku Presbyterian Hospital. Perfect medication adherence was low (40.5%), while imperfect adherence was high (59.5%) among the participants based on the scores on the Hill Bone medication adherence scale. Various studies have reported high levels of medication adherence among patients with hypertension (Choi et al., 2018; Boratas & Killc, 2018; Vatansever & Unsar, 2014). On the contrary, others have reported low levels of medication adherence (Alsolami, Hou, & Correa-Velez, 2015). Lo et al. (2016) found that only 44.1% of participants adhered to antihypertensive treatment. Another study conducted in the Southern part of Ghana found low medication adherence among the participants (42.18%) (Kretchy et al., 2015).
The demographic characteristics that predicted adherence to antihypertensive therapy were level of education, income, and duration of being on antihypertensive medications. In the current study, age was not significantly related to medication adherence. Similarly, Sarkodie et al. (2020) did not find any relationship between age and medication adherence. Conversely, Lo et al. (2016) reported that older persons were more likely to adhere to antihypertensive therapy. Kretchy et al. (2015) also found high levels of medication adherence among younger persons compared to older ones.
The level of income was found to predict medication adherence. In other words, participants with a high-income level were more likely to adhere to antihypertensive therapy and vice versa. This finding is in line with previous studies that found medication adherence was associated with income levels (Kretchy et al., 2015; Hussein, Awad, & Mahmoud, 2020). Patients with high-income levels can afford their medications or easily subscribe to the National Health Insurance Scheme (NHIS), which may cater to some treatment costs. Quite a number of the participants (36.8%) reported that they have not subscribed to the NHIS, thus, paid the medication cost themselves (46.5%). In this case, because the level of income for most participants (79.2%) was average (below 700 Ghanaian Cedi [GHC]), it may be difficult to purchase all treatment prescribed consistently. Though the study did not consider the number of dependents for each participant, the number of married and cohabiting participants (63.6%) outweighed single and widowed (36.4%). This fact may increase the number of dependents and responsibilities that put pressure on their income and reduce their ability to purchase antihypertensive drugs.
Furthermore, the duration of being on antihypertensive medications was found to predict adherence. In other words, a longer course of being on antihypertensive medicines was found to affect adherence positively. This finding is consistent with the study of Lee et al., who reported that a shorter duration of antihypertensive use was negatively correlated to medication adherence (Lee et al., 2013). It was found in the current study that most participants were on antihypertensive medications for eight years or more. They seemed to have gained some experience and identified ways of coping with the medication intake (Lee et al., 2013) compared with those who had recently commenced their treatment.
Another factor that was found to predict medication adherence was education. As one’s level of education increases, adherence to antihypertensive therapy increases and vice versa. Consistent with the current findings, other studies have also reported on the relationship between increasing educational attainment and increasing medication adherence, though the relationship was not significant (Basheti et al., 2016). Hypertensive patients with a high level of education may seek information from other sources like the Internet without necessarily relying on the health care providers. Most participants in the current study had an educational level that was quite low and may have relied on health care providers for adequate knowledge on hypertension and its management. Thus, if they have not received sufficient information, they may not adhere to the medication.
Other factors were reported as influencing medication adherence, including forgetfulness, inadequate knowledge on the antihypertensive medications, use of herbal medicines, side effects of the antihypertensive medications, and disease severity. The majority of the participants disagreed that treatment complexity influenced their adherence to antihypertensive drugs.
Most participants (92.6%) in the current study mentioned forgetfulness as the main factor influencing their adherence to their antihypertensive therapy. Similarly, Atinga, Yarney, and Gavu (2018) found that busy schedules which led to forgetfulness influences adherence. Okai et al. (2020) also cited forgetfulness as the reason for missing medication in the majority of the participants (70.5%). Most people develop routines for their daily schedule and may not need a reminder to carry out those routines. Being diagnosed with a chronic condition like hypertension and using antihypertensive medications for life may mean adjusting those routines. This change may be difficult and explain why most participants forget to take their antihypertensive drugs.
In the current study, most participants (82.6%) lacked adequate knowledge of antihypertensive medications; hence their level of adherence was low. Sufficient knowledge has been reported to influence good adherence (Jankowska-Polańska et al., 2016; Ayodapo et al., 2020). The setting of the study and low levels of education in most participants implies a robust approach by health professionals to explain the adherence to the antihypertensive treatment regimen for the patients. Most participants (63.9%) in our study confirmed the usage of herbal medicine in addition to orthodox medicine. Okai et al. (2020) reported that only 5.5% of the participants in their study did not believe in orthodox medicine. In qualitative research by Atinga, Yarney, and Gavu (2018), one of the themes that emerged was the poor perception of the efficacy of antihypertensive medications by some participants. The study participants claimed that they did not feel relieved when they took the antihypertensive drugs and subsequently discontinued their usage. Participants in the same study affirmed herbal medicine usage as an alternative to antihypertensive because of its perceived efficacy. The participants in the current study may be influenced by similar perceptions on the effectiveness and efficacy of orthodox antihypertensive medications in the management of hypertension. People’s perception ultimately influences their behavior which may explain why they were non-adherent.
The side effects of antihypertensive medications were also identified as factors influencing medication adherence. In their study, Tedla and Bautista mentioned excessive urination and decreased sexual drive as side effects contributing to non-adherence (Tedla & Bautista, 2016). Other medication side effects associated with non-adherence are muscle pain, tiredness, and poor sleep (Gebreyohannes et al., 2019). Perceived severity of hypertension also influenced adherence. Increased severity is perceived to be associated with more negative health outcomes. As expected, 52% mentioned that they adhere to their medications only when they perceive the condition to be serious. This finding is contrary to Sarkodie et al.’s study (Sarkodie et al., 2020).
Patients who start the antihypertensive treatment regimen may begin to feel much better, which may translate as improvement in their condition. They may subsequently discontinue the treatment or may not be taking medicine on schedule, which leads to poor adherence.
It is recommended that the healthcare team, especially nurses, when facing patients with hypertension, investigate the predictive and influencing factors found in this study and take appropriate measures to ensure that patients adhere to their drugs. Moreover, the government of Ghana, in collaboration with the National Health Insurance Authority, can put in place a system where individuals with chronic conditions like hypertension would be automatically enrolled in the health insurance scheme without having to pay any amounts, and also the insurance should cover the total cost.
The demographic characteristics that predicted adherence to antihypertensive therapy were level of education, income, and duration of being on antihypertensive medications. In the current study, age was not significantly related to medication adherence. Similarly, Sarkodie et al. (2020) did not find any relationship between age and medication adherence. Conversely, Lo et al. (2016) reported that older persons were more likely to adhere to antihypertensive therapy. Kretchy et al. (2015) also found high levels of medication adherence among younger persons compared to older ones.
The level of income was found to predict medication adherence. In other words, participants with a high-income level were more likely to adhere to antihypertensive therapy and vice versa. This finding is in line with previous studies that found medication adherence was associated with income levels (Kretchy et al., 2015; Hussein, Awad, & Mahmoud, 2020). Patients with high-income levels can afford their medications or easily subscribe to the National Health Insurance Scheme (NHIS), which may cater to some treatment costs. Quite a number of the participants (36.8%) reported that they have not subscribed to the NHIS, thus, paid the medication cost themselves (46.5%). In this case, because the level of income for most participants (79.2%) was average (below 700 Ghanaian Cedi [GHC]), it may be difficult to purchase all treatment prescribed consistently. Though the study did not consider the number of dependents for each participant, the number of married and cohabiting participants (63.6%) outweighed single and widowed (36.4%). This fact may increase the number of dependents and responsibilities that put pressure on their income and reduce their ability to purchase antihypertensive drugs.
Furthermore, the duration of being on antihypertensive medications was found to predict adherence. In other words, a longer course of being on antihypertensive medicines was found to affect adherence positively. This finding is consistent with the study of Lee et al., who reported that a shorter duration of antihypertensive use was negatively correlated to medication adherence (Lee et al., 2013). It was found in the current study that most participants were on antihypertensive medications for eight years or more. They seemed to have gained some experience and identified ways of coping with the medication intake (Lee et al., 2013) compared with those who had recently commenced their treatment.
Another factor that was found to predict medication adherence was education. As one’s level of education increases, adherence to antihypertensive therapy increases and vice versa. Consistent with the current findings, other studies have also reported on the relationship between increasing educational attainment and increasing medication adherence, though the relationship was not significant (Basheti et al., 2016). Hypertensive patients with a high level of education may seek information from other sources like the Internet without necessarily relying on the health care providers. Most participants in the current study had an educational level that was quite low and may have relied on health care providers for adequate knowledge on hypertension and its management. Thus, if they have not received sufficient information, they may not adhere to the medication.
Other factors were reported as influencing medication adherence, including forgetfulness, inadequate knowledge on the antihypertensive medications, use of herbal medicines, side effects of the antihypertensive medications, and disease severity. The majority of the participants disagreed that treatment complexity influenced their adherence to antihypertensive drugs.
Most participants (92.6%) in the current study mentioned forgetfulness as the main factor influencing their adherence to their antihypertensive therapy. Similarly, Atinga, Yarney, and Gavu (2018) found that busy schedules which led to forgetfulness influences adherence. Okai et al. (2020) also cited forgetfulness as the reason for missing medication in the majority of the participants (70.5%). Most people develop routines for their daily schedule and may not need a reminder to carry out those routines. Being diagnosed with a chronic condition like hypertension and using antihypertensive medications for life may mean adjusting those routines. This change may be difficult and explain why most participants forget to take their antihypertensive drugs.
In the current study, most participants (82.6%) lacked adequate knowledge of antihypertensive medications; hence their level of adherence was low. Sufficient knowledge has been reported to influence good adherence (Jankowska-Polańska et al., 2016; Ayodapo et al., 2020). The setting of the study and low levels of education in most participants implies a robust approach by health professionals to explain the adherence to the antihypertensive treatment regimen for the patients. Most participants (63.9%) in our study confirmed the usage of herbal medicine in addition to orthodox medicine. Okai et al. (2020) reported that only 5.5% of the participants in their study did not believe in orthodox medicine. In qualitative research by Atinga, Yarney, and Gavu (2018), one of the themes that emerged was the poor perception of the efficacy of antihypertensive medications by some participants. The study participants claimed that they did not feel relieved when they took the antihypertensive drugs and subsequently discontinued their usage. Participants in the same study affirmed herbal medicine usage as an alternative to antihypertensive because of its perceived efficacy. The participants in the current study may be influenced by similar perceptions on the effectiveness and efficacy of orthodox antihypertensive medications in the management of hypertension. People’s perception ultimately influences their behavior which may explain why they were non-adherent.
The side effects of antihypertensive medications were also identified as factors influencing medication adherence. In their study, Tedla and Bautista mentioned excessive urination and decreased sexual drive as side effects contributing to non-adherence (Tedla & Bautista, 2016). Other medication side effects associated with non-adherence are muscle pain, tiredness, and poor sleep (Gebreyohannes et al., 2019). Perceived severity of hypertension also influenced adherence. Increased severity is perceived to be associated with more negative health outcomes. As expected, 52% mentioned that they adhere to their medications only when they perceive the condition to be serious. This finding is contrary to Sarkodie et al.’s study (Sarkodie et al., 2020).
Patients who start the antihypertensive treatment regimen may begin to feel much better, which may translate as improvement in their condition. They may subsequently discontinue the treatment or may not be taking medicine on schedule, which leads to poor adherence.
It is recommended that the healthcare team, especially nurses, when facing patients with hypertension, investigate the predictive and influencing factors found in this study and take appropriate measures to ensure that patients adhere to their drugs. Moreover, the government of Ghana, in collaboration with the National Health Insurance Authority, can put in place a system where individuals with chronic conditions like hypertension would be automatically enrolled in the health insurance scheme without having to pay any amounts, and also the insurance should cover the total cost.
5. Conclusion
Medication adherence in the current study was found low. The level of education, monthly income, and duration of being on antihypertensive therapy were significantly related to medication adherence. The most perceived factors influencing medication non-adherence were forgetfulness, inadequate knowledge of antihypertensive drugs, and herbal medicines.
Ethical Considerations
Compliance with ethical guidelines
We observed the ethical principles for medical research involving humans based on the Declaration of Helsinki. Adequate information was given to the participants regarding the research objectives, benefits, and risks of participating in the study. The participants were further informed that they could participate or not to participate in the study without incurring any penalty or pre-judicial treatment. Additionally, they were asked to sign a consent form before being given the questionnaire. Approval was sought from the study Hospital. The data collected were kept confidential, and anonymity was ensured. Coding systems were developed so that various data sources were identified only by the researcher.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the study participants. Dr. Paul Agyei Kwakwa is acknowledged for reading the manuscript, and Mr. Prosper Nyatuame for his administrative assistant.
We observed the ethical principles for medical research involving humans based on the Declaration of Helsinki. Adequate information was given to the participants regarding the research objectives, benefits, and risks of participating in the study. The participants were further informed that they could participate or not to participate in the study without incurring any penalty or pre-judicial treatment. Additionally, they were asked to sign a consent form before being given the questionnaire. Approval was sought from the study Hospital. The data collected were kept confidential, and anonymity was ensured. Coding systems were developed so that various data sources were identified only by the researcher.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the study participants. Dr. Paul Agyei Kwakwa is acknowledged for reading the manuscript, and Mr. Prosper Nyatuame for his administrative assistant.
References
Alsolami, F., Hou, X. Y. & Correa-Velez, I., 2015. Factors affecting antihypertensive treatment adherence: A Saudi Arabian Perspective. Clinical Medicine and Diagnostics, 2(4), pp. 27-32. [DOI:10.5923/j.cmd.20120204.02]
Atibila, F., et al. 2021. Prevalence of hypertension in Ghanaian society: A systematic review, meta-analysis, and GRADE assessment. Systematic Review, 10, 220, pp. 1-15. [DOI:10.1186/s13643-021-01770-x]
Atinga, R. A., Yarney, L. & Gavu, N. M., 2018. Factors influencing long-term medication non-adherence among diabetes and hypertensive patients in Ghana: A qualitative investigation. PloS One, 13(3), p. e0193995. [DOI:10.1371/journal.pone.0193995] [PMID] [PMCID]
Ayodapo, A. O., et al. 2020. Patient education and medication adherence among hypertensives in a tertiary hospital, South Western Nigeria. Ethiopian Journal of Health Sciences, 30(2), pp. 243-50. [DOI:10.4314/ejhs.v30i2.12] [PMID] [PMCID]
Bader, R. J. K., et al. 2015. Predictors of adherence to antihypertensive medication in northern United Arab Emirates. Eastern Mediterranean Health Journal, 21(5), pp. 309-18. [DOI:10.26719/2015.21.5.309] [PMID]
Basheti, I. A., et al. 2016. Associations between patient factors and medication adherence: A Jordanian experience. Pharmacy Practice, 14(1), p. 639. [DOI:10.18549/PharmPract.2016.01.639] [PMID] [PMCID]
Bautista, D., 2012. Response to “depression and adherence to antihypertensive therapy”. American Journal of Hypertension, 21(7), p. 726. [DOI:10.1038/ajh.2008.195]
Boima, V., et al. 2015. Factors associated with medication non-adherence among hypertensives in Ghana and Nigeria. International Journal of Hypertension, 2015, p. 205716. [DOI:10.1155/2015/205716] [PMID] [PMCID]
Bochkareva, E. V., et al. 2019. Adherence to antihypertensive medication in Russia: A scoping review of studies on levels, determinants and intervention strategies published between 2000 and 2017. Archives of Public Health, 77, p. 43. [DOI:10.1186/s13690-019-0366-9] [PMID] [PMCID]
Boratas, S., & Kilic, H. F. 2018. Evaluation of medication adherence in hypertensive patients and influential factors. Pakistan Journal of Medical Sciences, 34(4), pp. 959–63. [DOI:10.12669/pjms.344.14994] [PMID] [PMCID]
Buabeng, K. O., Matowe, L. & Plange-Rhule, J., 2004. Unaffordable drug prices: The major cause of non-compliance with hypertension medication in Ghana. Journal of Pharmacy & Pharmaceutical Sciences, 7(3), pp. 350-2. [PMID]
Choi, H. Y., et al. 2018. Factors affecting adherence to antihypertensive medication. Korean Journal of Family Medicine, 39(6), pp. 325-32. [DOI:10.4082/kjfm.17.0041] [PMID] [PMCID]
Chowdhury, R., et al. 2013. Adherence to cardiovascular therapy: A meta-analysis of prevalence and clinical consequences. European Heart Journal, 34(38), pp. 2940-8. [DOI:10.1093/eurheartj/eht295.] [PMID]
Dillon, P., et al. 2018. Group-based trajectory models: Assessing adherence to antihypertensive medication in older adults in a community pharmacy setting. Clinical Pharmacology and Therapeutics, 103(6), pp. 1052-60. [DOI:10.1002/cpt.865] [PMID] [PMCID]
Gebreyohannes, E. A., et al. 2019. Adverse effects and non-adherence to antihypertensive medications in University of Gondar Comprehensive Specialized Hospital. Clinical Hypertension, 25, p. 1. [DOI:10.1186/s40885-018-0104-6] [PMID] [PMCID]
Hussein, A., Awad, M. S. & Mahmoud, H. E. M., 2020. Patient adherence to antihypertensive medications in upper Egypt: A cross-sectional study. The Egyptian Heart Journal, 72(1), p. 29. [DOI:10.1186/s43044-020-00066-0] [PMID] [PMCID]
Jankowska-Polańska, B., et al. 2016. Relationship between patients' knowledge and medication adherence among patients with hypertension. Patient preference and adherence, 10, pp. 2437–47. [DOI:10.2147/PPA.S117269] [PMID] [PMCID]
Kolandaivelu, K., et al. 2014. Non-adherence to cardiovascular medications. European Heart Journal, 35(46), pp. 3267-76. [DOI:10.1093/eurheartj/ehu364.] [PMID]
Koschack, J., et al. 2010. Comparison of two self-rating instruments for medication adherence assessment in hypertension revealed insufficient psychometric properties. Journal of Clinical Epidemiology, 63(3), pp. 299-306. [DOI:10.1016/j.jclinepi.2009.06.011] [PMID]
Kretchy, I. A., et al. 2015. A psychosocial perspective of medication side effects, experiences, coping approaches and implications or adherence in hypertension management. Clinical Hypertension, 21, p. 19. [DOI:10.1186/s40885-015-0028-3] [PMID] [PMCID]
Lambert, E. V., et al. 2006. Cross-cultural validation of the hill-bone compliance to high blood pressure therapy scale in a South African, primary healthcare setting. Ethnicity and Disease, 16(1), pp. 286-91. [PMID]
Khwaja, M., Ansari, M. A. & Mehnaz, S., 2017. Compliance to antihypertensive medication: A cross-sectional study in Aligarh. International Journal of Community Medicine and Public Health, 4(10), pp. 3698-704. [DOI:10.18203/2394-6040.ijcmph20174236]
Lee, H. J., Jang, S. I. & Park, E. C., 2017. Effect of adherence to antihypertensive medication on stroke incidence in patients with hypertension: A population-based retrospective cohort study. BMJ Open, 7(6), p. e014486. [DOI:10.1136/bmjopen-2016-014486] [PMID] [PMCID]
Lee, H., et al. 2021. Adherence to antihypertensive medication and incident cardiovascular events in young adults with hypertension. Hypertension, 77(4), pp. 1341-9. [DOI:10.1161/HYPERTENSIONAHA.120.16784] [PMID]
Lee, G. K. Y., et al. 2013. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS ONE, 8(4), p. e62775. [DOI:10.1371/journal.pone.0062775] [PMID] [PMCID]
NCD Risk Factor Collaboration (NCD-RisC), 2017. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet, 390(10113), pp. 2627-42. [DOI:10.1016/S0140-6736(17)32129-3]
Okai, D. E., et al. 2020. Patient-level factors influencing hypertension control in adults in Accra, Ghana. BMC Cardiovasc Disord, 20, 123, pp. 1-7. [DOI:10.1186/s12872-020-01370-y]
Pittman, D. G., et al. 2010. Antihypertensive medication adherence and subsequent healthcare utilization and costs. The American Journal of Managed Care, 16(8), pp. 568-76. [PMID]
Sarkodie, E., et al. 2020. Adherence to drug therapy among hypertensive patients attending two district hospitals in Ghana. African Health Sciences, 20(3), pp. 1355–67. [DOI:10.4314/ahs.v20i3.42] [PMID] [PMCID]
Shin, S., et al. 2013. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertension Research, 36(11), pp. 1000-5. [DOI:10.1038/hr.2013.85] [PMID]
Tedla, Y. G., & Bautista, L. E. 2016. Drug Side Effect Symptoms and Adherence to Antihypertensive Medication. American Journal of Hypertension, 29(6), pp. 772–9. [DOI:10.1093/ajh/hpv185] [PMID] [PMCID]
van de Vijver, S., et al. 2013. Status report on hypertension in Africa--consultative review for the 6th Session of the African :union: Conference of Ministers of Health on NCD’s. The Pan African Medical Journal, 16, p. 38. [DOI:10.11604/pamj.2013.16.38.3100] [PMID] [PMCID]
Vatansever, O., & Unsar, S. 2014. Determination of medical treatment adherence, self-efficacy levels of patients with essential hypertension and affecting factors. Turkish Journal of Cardiovascular Nursing, 5(8), pp. 66–74. [DOI:10.5543/khd.2014.008]
Yamane, T., 1967. Statistics: An Introductory Analysis, 2nd Edition. New York: Harper and Row. https://www.google.com/books/edition/Statistics/Wr7rAAAAMAAJ?hl=en
Atibila, F., et al. 2021. Prevalence of hypertension in Ghanaian society: A systematic review, meta-analysis, and GRADE assessment. Systematic Review, 10, 220, pp. 1-15. [DOI:10.1186/s13643-021-01770-x]
Atinga, R. A., Yarney, L. & Gavu, N. M., 2018. Factors influencing long-term medication non-adherence among diabetes and hypertensive patients in Ghana: A qualitative investigation. PloS One, 13(3), p. e0193995. [DOI:10.1371/journal.pone.0193995] [PMID] [PMCID]
Ayodapo, A. O., et al. 2020. Patient education and medication adherence among hypertensives in a tertiary hospital, South Western Nigeria. Ethiopian Journal of Health Sciences, 30(2), pp. 243-50. [DOI:10.4314/ejhs.v30i2.12] [PMID] [PMCID]
Bader, R. J. K., et al. 2015. Predictors of adherence to antihypertensive medication in northern United Arab Emirates. Eastern Mediterranean Health Journal, 21(5), pp. 309-18. [DOI:10.26719/2015.21.5.309] [PMID]
Basheti, I. A., et al. 2016. Associations between patient factors and medication adherence: A Jordanian experience. Pharmacy Practice, 14(1), p. 639. [DOI:10.18549/PharmPract.2016.01.639] [PMID] [PMCID]
Bautista, D., 2012. Response to “depression and adherence to antihypertensive therapy”. American Journal of Hypertension, 21(7), p. 726. [DOI:10.1038/ajh.2008.195]
Boima, V., et al. 2015. Factors associated with medication non-adherence among hypertensives in Ghana and Nigeria. International Journal of Hypertension, 2015, p. 205716. [DOI:10.1155/2015/205716] [PMID] [PMCID]
Bochkareva, E. V., et al. 2019. Adherence to antihypertensive medication in Russia: A scoping review of studies on levels, determinants and intervention strategies published between 2000 and 2017. Archives of Public Health, 77, p. 43. [DOI:10.1186/s13690-019-0366-9] [PMID] [PMCID]
Boratas, S., & Kilic, H. F. 2018. Evaluation of medication adherence in hypertensive patients and influential factors. Pakistan Journal of Medical Sciences, 34(4), pp. 959–63. [DOI:10.12669/pjms.344.14994] [PMID] [PMCID]
Buabeng, K. O., Matowe, L. & Plange-Rhule, J., 2004. Unaffordable drug prices: The major cause of non-compliance with hypertension medication in Ghana. Journal of Pharmacy & Pharmaceutical Sciences, 7(3), pp. 350-2. [PMID]
Choi, H. Y., et al. 2018. Factors affecting adherence to antihypertensive medication. Korean Journal of Family Medicine, 39(6), pp. 325-32. [DOI:10.4082/kjfm.17.0041] [PMID] [PMCID]
Chowdhury, R., et al. 2013. Adherence to cardiovascular therapy: A meta-analysis of prevalence and clinical consequences. European Heart Journal, 34(38), pp. 2940-8. [DOI:10.1093/eurheartj/eht295.] [PMID]
Dillon, P., et al. 2018. Group-based trajectory models: Assessing adherence to antihypertensive medication in older adults in a community pharmacy setting. Clinical Pharmacology and Therapeutics, 103(6), pp. 1052-60. [DOI:10.1002/cpt.865] [PMID] [PMCID]
Gebreyohannes, E. A., et al. 2019. Adverse effects and non-adherence to antihypertensive medications in University of Gondar Comprehensive Specialized Hospital. Clinical Hypertension, 25, p. 1. [DOI:10.1186/s40885-018-0104-6] [PMID] [PMCID]
Hussein, A., Awad, M. S. & Mahmoud, H. E. M., 2020. Patient adherence to antihypertensive medications in upper Egypt: A cross-sectional study. The Egyptian Heart Journal, 72(1), p. 29. [DOI:10.1186/s43044-020-00066-0] [PMID] [PMCID]
Jankowska-Polańska, B., et al. 2016. Relationship between patients' knowledge and medication adherence among patients with hypertension. Patient preference and adherence, 10, pp. 2437–47. [DOI:10.2147/PPA.S117269] [PMID] [PMCID]
Kolandaivelu, K., et al. 2014. Non-adherence to cardiovascular medications. European Heart Journal, 35(46), pp. 3267-76. [DOI:10.1093/eurheartj/ehu364.] [PMID]
Koschack, J., et al. 2010. Comparison of two self-rating instruments for medication adherence assessment in hypertension revealed insufficient psychometric properties. Journal of Clinical Epidemiology, 63(3), pp. 299-306. [DOI:10.1016/j.jclinepi.2009.06.011] [PMID]
Kretchy, I. A., et al. 2015. A psychosocial perspective of medication side effects, experiences, coping approaches and implications or adherence in hypertension management. Clinical Hypertension, 21, p. 19. [DOI:10.1186/s40885-015-0028-3] [PMID] [PMCID]
Lambert, E. V., et al. 2006. Cross-cultural validation of the hill-bone compliance to high blood pressure therapy scale in a South African, primary healthcare setting. Ethnicity and Disease, 16(1), pp. 286-91. [PMID]
Khwaja, M., Ansari, M. A. & Mehnaz, S., 2017. Compliance to antihypertensive medication: A cross-sectional study in Aligarh. International Journal of Community Medicine and Public Health, 4(10), pp. 3698-704. [DOI:10.18203/2394-6040.ijcmph20174236]
Lee, H. J., Jang, S. I. & Park, E. C., 2017. Effect of adherence to antihypertensive medication on stroke incidence in patients with hypertension: A population-based retrospective cohort study. BMJ Open, 7(6), p. e014486. [DOI:10.1136/bmjopen-2016-014486] [PMID] [PMCID]
Lee, H., et al. 2021. Adherence to antihypertensive medication and incident cardiovascular events in young adults with hypertension. Hypertension, 77(4), pp. 1341-9. [DOI:10.1161/HYPERTENSIONAHA.120.16784] [PMID]
Lee, G. K. Y., et al. 2013. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS ONE, 8(4), p. e62775. [DOI:10.1371/journal.pone.0062775] [PMID] [PMCID]
NCD Risk Factor Collaboration (NCD-RisC), 2017. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet, 390(10113), pp. 2627-42. [DOI:10.1016/S0140-6736(17)32129-3]
Okai, D. E., et al. 2020. Patient-level factors influencing hypertension control in adults in Accra, Ghana. BMC Cardiovasc Disord, 20, 123, pp. 1-7. [DOI:10.1186/s12872-020-01370-y]
Pittman, D. G., et al. 2010. Antihypertensive medication adherence and subsequent healthcare utilization and costs. The American Journal of Managed Care, 16(8), pp. 568-76. [PMID]
Sarkodie, E., et al. 2020. Adherence to drug therapy among hypertensive patients attending two district hospitals in Ghana. African Health Sciences, 20(3), pp. 1355–67. [DOI:10.4314/ahs.v20i3.42] [PMID] [PMCID]
Shin, S., et al. 2013. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertension Research, 36(11), pp. 1000-5. [DOI:10.1038/hr.2013.85] [PMID]
Tedla, Y. G., & Bautista, L. E. 2016. Drug Side Effect Symptoms and Adherence to Antihypertensive Medication. American Journal of Hypertension, 29(6), pp. 772–9. [DOI:10.1093/ajh/hpv185] [PMID] [PMCID]
van de Vijver, S., et al. 2013. Status report on hypertension in Africa--consultative review for the 6th Session of the African :union: Conference of Ministers of Health on NCD’s. The Pan African Medical Journal, 16, p. 38. [DOI:10.11604/pamj.2013.16.38.3100] [PMID] [PMCID]
Vatansever, O., & Unsar, S. 2014. Determination of medical treatment adherence, self-efficacy levels of patients with essential hypertension and affecting factors. Turkish Journal of Cardiovascular Nursing, 5(8), pp. 66–74. [DOI:10.5543/khd.2014.008]
Yamane, T., 1967. Statistics: An Introductory Analysis, 2nd Edition. New York: Harper and Row. https://www.google.com/books/edition/Statistics/Wr7rAAAAMAAJ?hl=en
Type of Study: Research |
Subject:
General
Received: 2021/10/8 | Accepted: 2021/10/25 | Published: 2022/02/1
Received: 2021/10/8 | Accepted: 2021/10/25 | Published: 2022/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |