Fri, Dec 26, 2025
[Archive]
Volume 8, Issue 1 (Winter 2022)
JCCNC 2022, 8(1): 1-8 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadi N, Abdi M, Dinmohammadi M. The Association Between Quality of Nursing Care in the ICU and Severity of Illness. JCCNC 2022; 8 (1) :1-8
URL: http://jccnc.iums.ac.ir/article-1-337-en.html
URL: http://jccnc.iums.ac.ir/article-1-337-en.html
1- Department of Critical Care Nursing, School of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran.
2- Department of Critical Care Nursing, School of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran. ,mdinmohammadi@zums.ac.ir
2- Department of Critical Care Nursing, School of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran. ,
Full-Text [PDF 616 kb]
(1279 Downloads)
| Abstract (HTML) (3331 Views)
Full-Text: (836 Views)
1. Introduction
Today, attention has been paid to improving the quality of care and its evaluation in health care systems (Izumi, Baggs, & Knafl, 2010; Bilgin, & Gozum, 2018; Rice, Say, & Betihavas, 2018). The quality of nursing care is one of the most important criteria for meeting treatment expectations (Piotrkowska et al., 2020). Nursing care in Intensive Care Units (ICUs) requires a holistic and client-centered care model to deliver a higher quality of care (Morgan, & Yoder, 2012; Zamanzadeh et al., 2015). The quality of care provided by nurses are influenced by some factors of the workplace (infection control, equipment, and specialized performance), personal factors of nurses (age, education, skills, and critical thinking), and specific patient conditions (contagious disease, severity of illness, and level of consciousness) (Wiechula et al., 2016; Evans and Stoddart, 2017).
Amongst other health care professionals, nurses provide the highest volume of care services (Berwick, 2016). According to the US Department of Labor (2014) and World Health Organization (WHO) (2015), nurses, as the largest group of health care providers, play an essential and pivotal role in providing health care (Ma, Olds, & Dunton, 2015).
The Severity of Illness (SOI) is an indicator of patient mortality and assesses the quality of care (Gabrielli et al., 2009; Hall, & Doran, 2015). It assesses the extent of organ system derangement or physiologic decompensation of a patient (Tan, Montagnese, & Mani, 2020). The high severity of illness, high mortality, and low chance of survival may cause staff burnout and affect the quality of care (Bingold et al., 2015). Assessing the severity of the disease and monitoring the quality of care play an important role in promoting patient care (Wong et al., 2016; La Sala et al., 2017).
Critically ill patients are more prone to treatment complications because of the severity of their illnesses. Cremasco et al. conducted a study to investigate the correlation between nursing workload and illness severity among ICU patients. The multivariate logistic regression showed that nursing workload is significantly correlated with the severity of illness and acts as a protective factor (Cremasco et al., 2013). In another study, the correlation between nursing workload and severity of illness was measured by the simplified acute physiology score II. The results showed that nursing staffing use score had been positively associated with disease severity, while nursing activities score was not associated with illness severity (Kraljic et al., 2017).
In most ICUs of Iran, the beds’ occupancy ratio is more than 90%; consequently, nurses’ performance in these wards is crucial to the quality of patient care (Zeraati and Alavi, 2014). Despite numerous studies on the quality of patient care, few studies have addressed the relationship between quality of care and the SOI. Accordingly, this study aimed to determine the relationship between the quality of nursing care and the severity of illness during a patient’s hospitalization in the ICU.
Amongst other health care professionals, nurses provide the highest volume of care services (Berwick, 2016). According to the US Department of Labor (2014) and World Health Organization (WHO) (2015), nurses, as the largest group of health care providers, play an essential and pivotal role in providing health care (Ma, Olds, & Dunton, 2015).
The Severity of Illness (SOI) is an indicator of patient mortality and assesses the quality of care (Gabrielli et al., 2009; Hall, & Doran, 2015). It assesses the extent of organ system derangement or physiologic decompensation of a patient (Tan, Montagnese, & Mani, 2020). The high severity of illness, high mortality, and low chance of survival may cause staff burnout and affect the quality of care (Bingold et al., 2015). Assessing the severity of the disease and monitoring the quality of care play an important role in promoting patient care (Wong et al., 2016; La Sala et al., 2017).
Critically ill patients are more prone to treatment complications because of the severity of their illnesses. Cremasco et al. conducted a study to investigate the correlation between nursing workload and illness severity among ICU patients. The multivariate logistic regression showed that nursing workload is significantly correlated with the severity of illness and acts as a protective factor (Cremasco et al., 2013). In another study, the correlation between nursing workload and severity of illness was measured by the simplified acute physiology score II. The results showed that nursing staffing use score had been positively associated with disease severity, while nursing activities score was not associated with illness severity (Kraljic et al., 2017).
In most ICUs of Iran, the beds’ occupancy ratio is more than 90%; consequently, nurses’ performance in these wards is crucial to the quality of patient care (Zeraati and Alavi, 2014). Despite numerous studies on the quality of patient care, few studies have addressed the relationship between quality of care and the SOI. Accordingly, this study aimed to determine the relationship between the quality of nursing care and the severity of illness during a patient’s hospitalization in the ICU.
2. Materials and Methods
This descriptive-correlational study was performed in the general ICU of 540-bed Ayatollah Mousavi Hospital. The trauma center of Zanjan Province is located in the northwestern part of Iran and accepts referral patients from the Zanjan Province and neighboring western and northwestern provinces of Iran.
After conducting a pilot study and obtaining a correlation coefficient of 0.4 between main study variables, 47 samples were estimated for the study. Initially, 62 eligible patients were included in the study. Twelve patients were excluded due to death (n=6), discharge, or transfer to another ward (n=6) during the study. Thus, the study was completed with 50 patients. The inclusion criteria were the willingness of patients or their caregivers to participate in the study, over 18 years old and more than 24 hours stay in the ICU. The patients were excluded in case of death or transfer to other wards before the end of the study. The data were collected during 70 days (November 2018 to January 2019) using the Quality of Nursing Care Scale in ICU (QNCS-ICU) and Sequential Organ Failure Assessment (SOFA) for each patient in the first seven days of hospitalization.
The QNCS-ICU as an observational tool consists of 46 items and eight domains (in this study, the total score was used). The items are scored on a 4-point Likert scale (not applicable = 0, undesirable = 1, relatively desirable = 2, desirable = 3) (Zeraati, & Alavi, 2014). In this tool, items that are not applicable (for example, when the patient separates from the ventilator) are given a score of 0 and are not considered in the calculation of scores; therefore, the cut point of the tool cannot be determined. Zeraati and Alavi (2014) reported the Content Validity Index (CVI) and Content Validity Ratio (CVR) of this scale as 0.898 and 0.725, respectively. Its reliability was also determined by the Cronbach α coefficient of 0.726 (Zeraati, & Alavi, 2014).
The SOFA as a mortality prediction scale is a valid and reliable tool used in most countries. It examines the body’s six vital organs of lung, liver, heart, brain, kidneys, and blood. The instrument is scored on a 5-point Likert type scale from 0 to 4, with a score of 0 indicating that the organ is healthy and 4 representing organ failure. The score is calculated at admission and every 24 hours until discharge using the worst parameters measured in the previous 24 hours. The sum of these numbers in six vital organs is the patient’s daily score. The total score ranges from 0 to 24. The SOFA scores of 0-1, 2-3, 4-5, 6-7, 8-9, 10-11, 12-14, and more than 14 have the mortality rates of 0%, 6.4%, 20%, 21.5%, 33%, 50%, 95% and more than 95%, respectively (Vincent et al., 1996; Zeraati, & Alavi, 2014). The reliability of the SOFA scale has been confirmed in various studies with the Cronbach α above 0.88 (Tobar et al., 2010). Mahjoubipour et al. (2012) confirmed the reliability of the Persian version of this tool with the Cronbach α of 0.92.
The study data were collected by one of the researchers from December 11 to February 20, 2017, for 70 consecutive days. The quality of care data was recorded according to the daily observation of the patients and what has been documented by nurses in line with QNCS-ICU. To record SOI, the related data were collected according to the criteria for each organ. For example, the measurement criterion in the blood system was the patient’s platelet count; in the renal system, it was the creatinine level, and in the central nervous system, the Glasgow Coma Scale (GCS) was measured. Also, the heart rate was measured by the central monitoring system, the respiratory system by PaO2/FIO2 through measuring arterial blood gases, and the liver system by bilirubin and inotropes.
To determine the normality of the data, the Kolmogorov-Smirnov test was performed. Since the data distribution was not normal, equivalent non-parametric tests were used. Data were analyzed using descriptive statistics, non-parametric inferential statistics (the Friedman test, Wilcoxon signed-rank test, and Spearman’s rho) using SPSS 16 software. The significance level was considered 0.05.
After conducting a pilot study and obtaining a correlation coefficient of 0.4 between main study variables, 47 samples were estimated for the study. Initially, 62 eligible patients were included in the study. Twelve patients were excluded due to death (n=6), discharge, or transfer to another ward (n=6) during the study. Thus, the study was completed with 50 patients. The inclusion criteria were the willingness of patients or their caregivers to participate in the study, over 18 years old and more than 24 hours stay in the ICU. The patients were excluded in case of death or transfer to other wards before the end of the study. The data were collected during 70 days (November 2018 to January 2019) using the Quality of Nursing Care Scale in ICU (QNCS-ICU) and Sequential Organ Failure Assessment (SOFA) for each patient in the first seven days of hospitalization.
The QNCS-ICU as an observational tool consists of 46 items and eight domains (in this study, the total score was used). The items are scored on a 4-point Likert scale (not applicable = 0, undesirable = 1, relatively desirable = 2, desirable = 3) (Zeraati, & Alavi, 2014). In this tool, items that are not applicable (for example, when the patient separates from the ventilator) are given a score of 0 and are not considered in the calculation of scores; therefore, the cut point of the tool cannot be determined. Zeraati and Alavi (2014) reported the Content Validity Index (CVI) and Content Validity Ratio (CVR) of this scale as 0.898 and 0.725, respectively. Its reliability was also determined by the Cronbach α coefficient of 0.726 (Zeraati, & Alavi, 2014).
The SOFA as a mortality prediction scale is a valid and reliable tool used in most countries. It examines the body’s six vital organs of lung, liver, heart, brain, kidneys, and blood. The instrument is scored on a 5-point Likert type scale from 0 to 4, with a score of 0 indicating that the organ is healthy and 4 representing organ failure. The score is calculated at admission and every 24 hours until discharge using the worst parameters measured in the previous 24 hours. The sum of these numbers in six vital organs is the patient’s daily score. The total score ranges from 0 to 24. The SOFA scores of 0-1, 2-3, 4-5, 6-7, 8-9, 10-11, 12-14, and more than 14 have the mortality rates of 0%, 6.4%, 20%, 21.5%, 33%, 50%, 95% and more than 95%, respectively (Vincent et al., 1996; Zeraati, & Alavi, 2014). The reliability of the SOFA scale has been confirmed in various studies with the Cronbach α above 0.88 (Tobar et al., 2010). Mahjoubipour et al. (2012) confirmed the reliability of the Persian version of this tool with the Cronbach α of 0.92.
The study data were collected by one of the researchers from December 11 to February 20, 2017, for 70 consecutive days. The quality of care data was recorded according to the daily observation of the patients and what has been documented by nurses in line with QNCS-ICU. To record SOI, the related data were collected according to the criteria for each organ. For example, the measurement criterion in the blood system was the patient’s platelet count; in the renal system, it was the creatinine level, and in the central nervous system, the Glasgow Coma Scale (GCS) was measured. Also, the heart rate was measured by the central monitoring system, the respiratory system by PaO2/FIO2 through measuring arterial blood gases, and the liver system by bilirubin and inotropes.
To determine the normality of the data, the Kolmogorov-Smirnov test was performed. Since the data distribution was not normal, equivalent non-parametric tests were used. Data were analyzed using descriptive statistics, non-parametric inferential statistics (the Friedman test, Wilcoxon signed-rank test, and Spearman’s rho) using SPSS 16 software. The significance level was considered 0.05.
3. Results
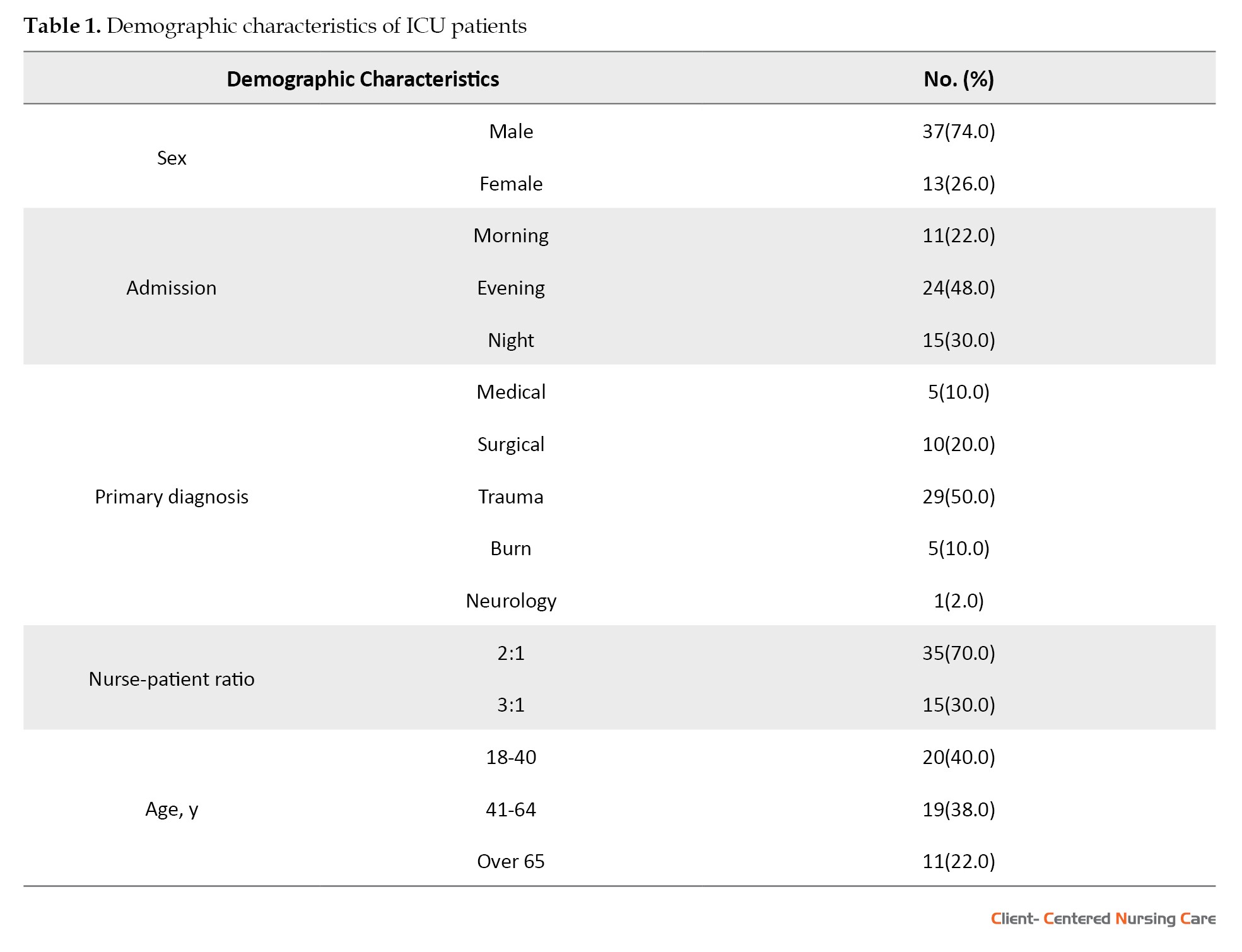
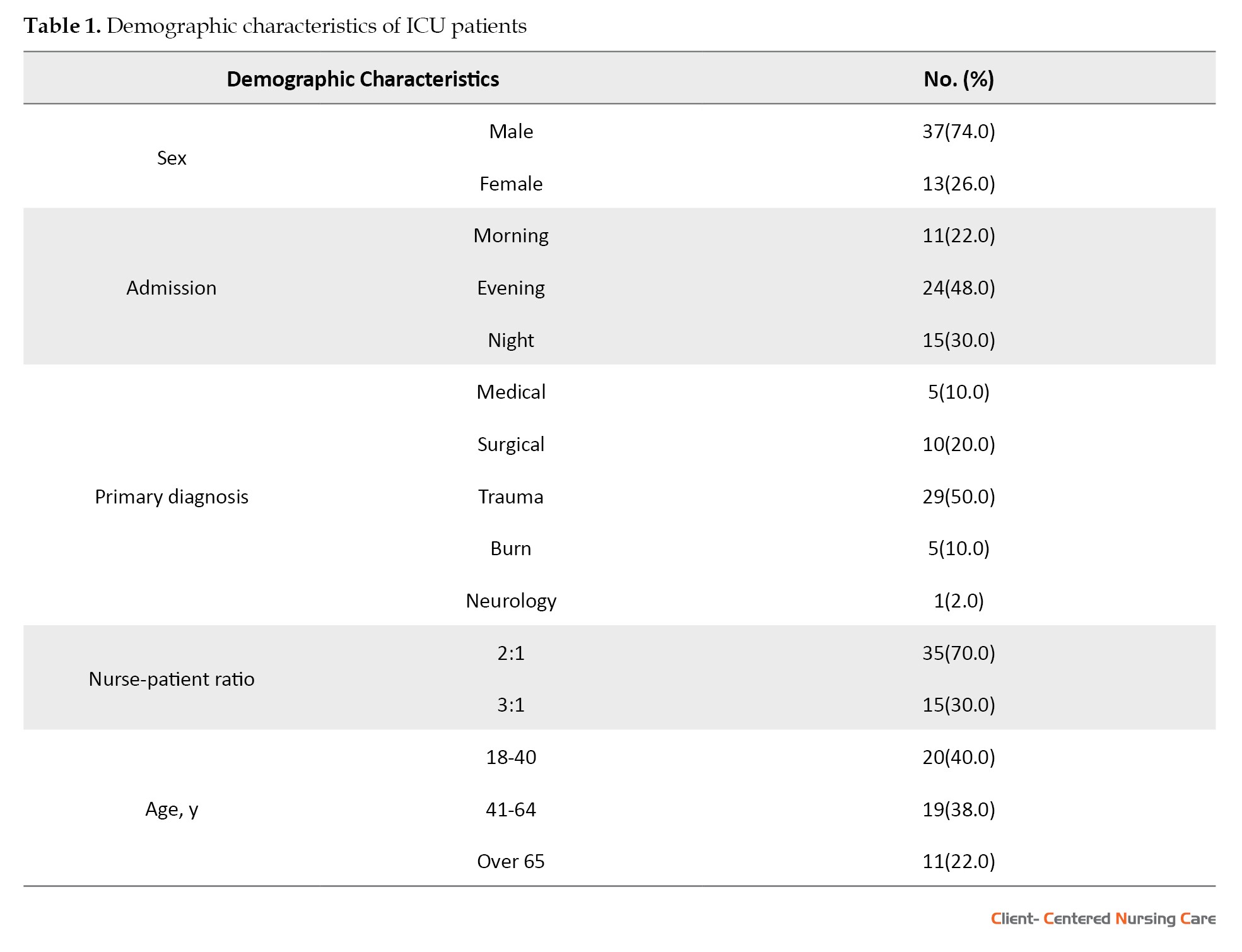
The Mean±SD age of the patients was 46.46±2.74 years. The results showed that the majority of the patients were male (74%) and were often admitted in the evening shift (48%) with trauma diagnosis (58%) (Table 1).
The Mean±SD score of the quality of nursing care in the ICU was 86.62±2.19. Also, analysis of data during the first seven days of hospitalization by the Friedman test revealed that the quality of nursing care was significantly different during these days (χ2= 36.56, df=6, P<0.001). To see which differences existed on any given day, pairwise comparisons were performed using the Wilcoxon signed-rank test. The analysis results showed a significant difference in the quality of care on the first day with the rest of the days (the first day with the second to sixth day P<0.001, and the first day with the seventh day P=0.004). In other words, the quality of nursing care did not differ significantly from the second day onwards.
Also, the Mean±SD SOFA score was 6.4±2.31, and the Friedman test showed that the severity of illness was significantly different during the seven days (χ2=53.69, df=6, P<0.001). To compare the differences between the days, pairwise comparisons were performed using the Wilcoxon signed-rank test. The analysis results showed a significant difference in the severity of the illness on the first, second and third days with the rest of the days (P<0.01). In other words, the disease severity remained constant until day three and decreased from day 4.
The correlation between nursing care quality and disease severity during the first seven days of hospitalization was determined using the Spearman’s rho test. The correlation was reversed and significant. In other words, from the fourth to the seventh day of hospitalization, despite the improvement in SOI, the quality of care was increasing (Table 2, Figure 1).


The Mean±SD score of the quality of nursing care in the ICU was 86.62±2.19. Also, analysis of data during the first seven days of hospitalization by the Friedman test revealed that the quality of nursing care was significantly different during these days (χ2= 36.56, df=6, P<0.001). To see which differences existed on any given day, pairwise comparisons were performed using the Wilcoxon signed-rank test. The analysis results showed a significant difference in the quality of care on the first day with the rest of the days (the first day with the second to sixth day P<0.001, and the first day with the seventh day P=0.004). In other words, the quality of nursing care did not differ significantly from the second day onwards.
Also, the Mean±SD SOFA score was 6.4±2.31, and the Friedman test showed that the severity of illness was significantly different during the seven days (χ2=53.69, df=6, P<0.001). To compare the differences between the days, pairwise comparisons were performed using the Wilcoxon signed-rank test. The analysis results showed a significant difference in the severity of the illness on the first, second and third days with the rest of the days (P<0.01). In other words, the disease severity remained constant until day three and decreased from day 4.
The correlation between nursing care quality and disease severity during the first seven days of hospitalization was determined using the Spearman’s rho test. The correlation was reversed and significant. In other words, from the fourth to the seventh day of hospitalization, despite the improvement in SOI, the quality of care was increasing (Table 2, Figure 1).


4. Discussion
The study’s findings showed that the quality of care on the first day of admission was better than the rest of the days, and this trend declined until day five, but it increased with a gentle slope until day seven. Moreover, changes in the SOI in the first to fourth days of hospitalization were constant and relatively high and declined from the fifth day onwards. The results showed no significant correlation between the quality of nursing care and the SOI in the first to third days. In contrast, this correlation was reversed and statistically significant from day four. In other words, there was no significant relationship between quality of care and changes in disease severity in the first to third days, whereas from the fourth to seventh day of hospitalization, despite the improvement in disease severity, the quality of care increased.
In the Muehler et al. study (2010), surgical patients received the highest score on the Therapeutic Intervention Scoring System (TISS)-28 on the first day of admission to the ICU. There was a gradual decrease in the TISS-28 score after the first day to two weeks which is in line with the present study results. In the Muehler et al. study, TISS-28 correlates moderately with disease severity and outcome in surgical patients admitted to the ICU (Muehler et al., 2010), which contradicts the present study’s findings. The reason for this discrepancy can be attributed to the type of initial diagnosis of patients in our study that included a combination of patients with a primary diagnosis of surgical, medical, trauma, and burn. However, differences in care delivery patterns, nurse-patient ratio, and care team composition in the two studies might have also contributed to this difference. Other studies also reported a good correlation between TISS-28 score and disease severity (Elias et al., 2006; Moreno, & Morais, 1997; Padilha et al., 2007; Seker et al., 2018). In more severe conditions, clients should receive more therapeutic interventions. Numerous studies have reported the role of nursing care provision (Aiken et al., 2014; Cho, & Yun, 2009; Falk, & Wallin, 2016; Glance et al., 2012; Hall, & Doran, 2004; Jansson, Syrjälä, & Ala-Kokko, 2019; Needleman et al., 2011) and care delivery models (Falk, & Wallin, 2016; Hall , & Doran, 2004; Kendall-Gallagher and Blegen, 2009) in the quality of patient care. Meanwhile, the impact of workload and care burden on intensive care units cannot be ignored (Bruyneel et al., 2019; Giuliani et al., 2018; Kraljic et al., 2017; Kaymak et al., 2018).
One of the reasons for the high quality of nursing care on the first day of admission may be teamwork. At new admissions, nurses usually help each other to reduce workloads. Occasionally, a task is assigned to 4 to 5 nurses. Teamwork and a high nurse-to-patient ratio are factors that might have improved the quality of nursing care on the first day. From the second day onward, the case method continues with two to three patients per nurse, which could justify the steady and downward trend in the quality of care up to the fourth day of admission. The noteworthy point in this study is decreased quality of care from the fifth day of hospitalization onwards, which requires further investigation. Inadequacy of nurse-patient ratio and the lack of implementing a nursing process to care for the patients could also explain the fluctuations in the quality of care. In the present study, the severity of illness was high and relatively constant in the first to third days and decreased from day four onwards. Chantry et al. (2015) also reported a decrease in disease severity over time (Chantry et al., 2015), which is in line with the present study’s findings. In contrast, Kaukonen et al. (2014) reported that the SOI in the ICU increases over time (Kaukonen et al., 2014). Perhaps the leading cause of this difference can be traced to the kind of patients under study because, in the study of Kaukonen et al. (2014), most patients with sepsis were less likely to survive. Different diagnoses (medical, surgical, trauma, and burns) of our patients might have affected the severity of the disease. This study has limitations of generalizability because of its findings from a single medical center and small sample size. It is suggested that further studies be conducted with a multicenter approach and larger samples.
In the Muehler et al. study (2010), surgical patients received the highest score on the Therapeutic Intervention Scoring System (TISS)-28 on the first day of admission to the ICU. There was a gradual decrease in the TISS-28 score after the first day to two weeks which is in line with the present study results. In the Muehler et al. study, TISS-28 correlates moderately with disease severity and outcome in surgical patients admitted to the ICU (Muehler et al., 2010), which contradicts the present study’s findings. The reason for this discrepancy can be attributed to the type of initial diagnosis of patients in our study that included a combination of patients with a primary diagnosis of surgical, medical, trauma, and burn. However, differences in care delivery patterns, nurse-patient ratio, and care team composition in the two studies might have also contributed to this difference. Other studies also reported a good correlation between TISS-28 score and disease severity (Elias et al., 2006; Moreno, & Morais, 1997; Padilha et al., 2007; Seker et al., 2018). In more severe conditions, clients should receive more therapeutic interventions. Numerous studies have reported the role of nursing care provision (Aiken et al., 2014; Cho, & Yun, 2009; Falk, & Wallin, 2016; Glance et al., 2012; Hall, & Doran, 2004; Jansson, Syrjälä, & Ala-Kokko, 2019; Needleman et al., 2011) and care delivery models (Falk, & Wallin, 2016; Hall , & Doran, 2004; Kendall-Gallagher and Blegen, 2009) in the quality of patient care. Meanwhile, the impact of workload and care burden on intensive care units cannot be ignored (Bruyneel et al., 2019; Giuliani et al., 2018; Kraljic et al., 2017; Kaymak et al., 2018).
One of the reasons for the high quality of nursing care on the first day of admission may be teamwork. At new admissions, nurses usually help each other to reduce workloads. Occasionally, a task is assigned to 4 to 5 nurses. Teamwork and a high nurse-to-patient ratio are factors that might have improved the quality of nursing care on the first day. From the second day onward, the case method continues with two to three patients per nurse, which could justify the steady and downward trend in the quality of care up to the fourth day of admission. The noteworthy point in this study is decreased quality of care from the fifth day of hospitalization onwards, which requires further investigation. Inadequacy of nurse-patient ratio and the lack of implementing a nursing process to care for the patients could also explain the fluctuations in the quality of care. In the present study, the severity of illness was high and relatively constant in the first to third days and decreased from day four onwards. Chantry et al. (2015) also reported a decrease in disease severity over time (Chantry et al., 2015), which is in line with the present study’s findings. In contrast, Kaukonen et al. (2014) reported that the SOI in the ICU increases over time (Kaukonen et al., 2014). Perhaps the leading cause of this difference can be traced to the kind of patients under study because, in the study of Kaukonen et al. (2014), most patients with sepsis were less likely to survive. Different diagnoses (medical, surgical, trauma, and burns) of our patients might have affected the severity of the disease. This study has limitations of generalizability because of its findings from a single medical center and small sample size. It is suggested that further studies be conducted with a multicenter approach and larger samples.
5. Conclusion
There was a significant indirect relationship between quality of care and SOI from the fourth to seventh days of hospitalization. In other words, from the fourth to the seventh day of hospitalization, the quality of care is increasing despite the improvement in SOI. In our study, it seems that the provision of nursing care is mostly routine and is not planned and provided based on the patients’ needs. Other reasons, however, can be the nursing shortage and, consequently, a decrease in the nurse-to-patient ratio. It seems that the care models in this unit should be revised and requires training policies to improve the knowledge and quality of services provided by supervisors. It is suggested that special education policies be adopted to improve the management quality of head nurses and supervisors in the form of continuing professional development programs.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Zanjan University of Medical Sciences (Code: IR.ZUMS.REC.1397.304). Informed consent was obtained from the patients or their relatives.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualizatio, methodology, and data collection: Mohammadreza Dinmohammadi and Narges Mohammadi; Writing – review & editing and funding acquisition and resources: Mohammadreza Dinmohammadi; Data analysis and writing – original draft: Mohammadreza Dinmohammadi, Narges Mohammadi, and Mohammad Abdi; Approval of final manuscript: Mohammadreza Dinmohammadi and Mohammad Abdi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank and appreciate the ICU Nurses of Ayatollah Mousavi Teaching Hospital, Zanjan, for their cooperation. Also, The authors wish to thank the Vice-Chancellor for Research and Technology of Zanjan University of Medical Sciences for the financial support.
This study was approved by the Research Ethics Committee of Zanjan University of Medical Sciences (Code: IR.ZUMS.REC.1397.304). Informed consent was obtained from the patients or their relatives.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualizatio, methodology, and data collection: Mohammadreza Dinmohammadi and Narges Mohammadi; Writing – review & editing and funding acquisition and resources: Mohammadreza Dinmohammadi; Data analysis and writing – original draft: Mohammadreza Dinmohammadi, Narges Mohammadi, and Mohammad Abdi; Approval of final manuscript: Mohammadreza Dinmohammadi and Mohammad Abdi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank and appreciate the ICU Nurses of Ayatollah Mousavi Teaching Hospital, Zanjan, for their cooperation. Also, The authors wish to thank the Vice-Chancellor for Research and Technology of Zanjan University of Medical Sciences for the financial support.
References
Aiken, L. H., et al. 2014. Nurse staffing and education and hospital mortality in nine European countries: aretrospective observational study. The Lancet, 383(9931), pp. 1824-30. [DOI:10.1016/S0140-6736(13)62631-8]
Berwick, D. M., 2016. Era 3 for medicine and health care. JAMA, 315(13), pp. 1329-30. [DOI:10.1001/jama.2016.1509] [PMID]
Bilgin, S. & Gozum, S., 2018. Effect of nursing care given at home on the quality of life of patients with stomach cancer and their family caregivers’ nursing care. European Journal of Cancer Care, 27(2), p. e12567. [DOI:10.1111/ecc.12567] [PMID]
Bingold, T. M., et al. 2015. Individual organ failure and concomitant risk of mortality differs according to the type of admission to ICU-a retrospective study of SOFA score of 23,795 patients. PLoS One, 10(8), p. e0134329. [DOI:10.1371/journal.pone.0134329] [PMID] [PMCID]
Bruyneel, A., et al. 2019. Measuring the nursing workload in intensive care with the Nursing Activities Score (NAS): A prospective study in 16 hospitals in Belgium. Journal of Critical Care, 54, pp. 205-11. [DOI:10.1016/j.jcrc.2019.08.032] [PMID]
Chantry, A. A., et al. 2015. Pregnancy-related ICU admissions in France: Trends in rate and severity, 2006-2009. Critical Care Medicine, 43(1), pp. 78-86. [DOI:10.1097/CCM.0000000000000601] [PMID]
Cho, S. H. & Yun, S. C., 2009. Bed-to-nurse ratios, provision of basic nursing care, and in-hospital and 30-day mortality among acute stroke patients admitted to an intensive care unit: Cross-sectional analysis of survey and administrative data. International Journal of Nursing Studies, 46(8), pp. 1092-101. [DOI:10.1016/j.ijnurstu.2009.02.001] [PMID]
Cremasco, M. F., Wenzel, F., Zanei, S. S. & Whitaker, I. Y. 2013. Pressure ulcers in the intensive care unit: the relationship between nursing workload, illness severity and pressure ulcer risk. Journal of Clinical Nursing, 22, 2183-2191. [DOI:10.1111/j.1365-2702.2012.04216.x] [PMID]
Elias, A. C., et al. 2006. [Application of the therapeutic intervention scoring system (TISS 28) at an intensive care unit to evaluate the severity of the patient (Portuguese)]. Revista Latino-Americana de Enfermagem, 14(3), pp. 324-9. [DOI:10.1590/S0104-11692006000300004] [PMID]
Evans, R. G. & Stoddart, G. L., 2017. Producing health, consuming health care. Why are some people healthy and others not? Milton Park: Routledge. [DOI:10.4324/9781315135755-3]
Falk, A. C. & Wallin, E. M., 2016. Quality of patient care in the critical care unit in relation to nurse patient ratio: A descriptive study. Intensive and Critical Care Nursing, 35, pp. 74-9. [DOI:10.1016/j.iccn.2016.01.002] [PMID]
Giuliani, E., et al. 2018. The burden of not-weighted factors-nursing workload in a medical intensive care unit. Intensive and Critical Care Nursing, 47, pp. 98-101. [DOI:10.1016/j.iccn.2018.02.009] [PMID]
Glance, L. G., et al. 2012. The association between nurse staffing and hospital outcomes in injured patients. BMC Health Services Research, 12, p. 247. [DOI:10.1186/1472-6963-12-247] [PMID] [PMCID]
Hall, L. M. & Doran, D. 2004. Nurse staffing, care delivery model, and patient care quality. Journal of Nursing Care Quality, 19(1), pp. 27-33. [DOI:10.1097/00001786-200401000-00007] [PMID]
Izumi, S., Baggs, J. G. & Knafl, K. A., 2010. Quality nursing care for hospitalized patients with advanced illness: Concept development. Research in Nursing & Health, 33(4), pp. 299-315. [DOI:10.1002/nur.20391] [PMID] [PMCID]
Jansson, M. M., Syrjälä, H. P. & Ala-Kokko, T. I., 2019. Association of nurse staffing and nursing workload with ventilator-associated pneumonia and mortality: A prospective, single-center cohort study. Journal of Hospital Infection, 101(3), pp. 257-63. [DOI:10.1016/j.jhin.2018.12.001] [PMID]
Kaukonen, K. M., et al. 2014. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA, 311(13), pp. 1308-16. [DOI:10.1001/jama.2014.2637] [PMID]
Kaymak, C., et al. 2018. Mortality of adult intensive care units in Turkey using the APACHE II and SOFA systems (outcome assessment in Turkish intensive care units). Archives of Medical Science, 14(3), pp. 510-5. [DOI:10.5114/aoms.2016.59709] [PMID] [PMCID]
Kendall-Gallagher, D. & Blegen, M. A., 2009. Competence and certification of registered nurses and safety of patients in intensive care units. American Journal of Critical Care, 18(2), pp. 106-13. [DOI:10.4037/ajcc2009487] [PMID] [PMCID]
Kraljic, S., et al. 2017. Evaluation of nurses’ workload in intensive care unit of a tertiary care university hospital in relation to the patients’ severity of illness: A prospective study. International Journal of Nursing Studies, 76, pp. 100-5. [DOI:10.1016/j.ijnurstu.2017.09.004] [PMID]
La Sala, R., et al. 2017. The quality of nursing in intensive care: A development of a rating scale. Acta Biomedica, 88(1S), pp. 61-8. [PMID]
Ma, C., Olds, D. M. & Dunton, N. E., 2015. Nurse work environment and quality of care by unit types: A cross-sectional study. International Journal of Nursing Studies, 52(10), pp. 1565-72. [DOI:10.1016/j.ijnurstu.2015.05.011] [PMID]
Mahjoubipour, H., et al. 2012. [Efficiency of SOFA scoring system on predicting mortality rate and stay length in intensive care unit for patients of Al-Zahra hospital of Isfahan (Persian)]. Medical-Surgical Nursing Journal, 1(2), pp. 6-10. https://brief.land/msnj/articles/87468.html
Moreno, R. & Morais, P., 1997. Validation of the simplified therapeutic intervention scoring system on an independent database. Intensive Care Medicine, 23(6), pp. 640-4. [DOI:10.1007/s001340050387] [PMID]
Morgan, S. & Yoder, L. H., 2012. A concept analysis of person-centered care. Journal of Holistic Nursing, 30(1), pp. 6-15. [DOI:10.1177/0898010111412189] [PMID]
Muehler, N., et al. 2010. Serial measurement of Therapeutic Intervention Scoring System-28 (TISS-28) in a surgical intensive care unit. Journal of Critical Care, 25(4), pp. 620-7. [DOI:10.1016/j.jcrc.2010.03.008] [PMID]
Needleman, J., et al. 2011. Nurse staffing and inpatient hospital mortality. The New England Journal of Medicine, 364(11), pp. 1037-45. [DOI:10.1056/NEJMsa1001025] [PMID]
Padilha, K. G., et al. 2007. Nursing workload in intensive care units: A study using the Therapeutic Intervention Scoring System-28 (TISS-28). Intensive and Critical Care Nursing, 23(3), pp. 162-9. [DOI:10.1016/j.iccn.2006.07.004] [PMID]
Piotrkowska, R., et al. 2020. Assessment of the quality of nursing care of postoperative pain in patients undergoing vascular procedures. Journal of PeriAnesthesia Nursing, 35(5), pp. 484-90. [DOI:10.1016/j.jopan.2020.03.010] [PMID]
Rice, H., Say, R. & Betihavas, V., 2018. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review. Patient Education and Counseling, 101(3), pp. 363-74. [DOI:10.1016/j.pec.2017.10.002] [PMID]
Seker, Y. T., Hergunsel, O., Bostanci, I., & Zeydan, A. 2018. Utility of the Therapeutic Intervention Scoring System-28 to Predict Mortality in Intensive Care Units. EJMO, 2(1), pp. 35-3. https://www.researchgate.net/publication/321585013_Utility_of_using_the__System-
Tan, Y. Y., Montagnese, S. & Mani, A. R., 2020. Organ system network disruption is associated with poor prognosis in patients with chronic liver failure. Frontiers in Physiology, 11, p. 983. [DOI:10.3389/fphys.2020.00983] [PMID] [PMCID]
Tobar, E., et al. 2010. [Confusion Assessment Method for diagnosing delirium in ICU patients (CAM-ICU): Cultural adaptation and validation of the Spanish version (Spanish)]. Medicina Intensiva, 34(1), pp. 4-13. [DOI:10.1016/j.medin.2009.04.003] [PMID]
Vincent, J. L., et al. 1996. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Medicine, 22(7), pp. 707-10. [DOI:10.1007/BF01709751] [PMID]
Wiechula, R., et al. 2016. Umbrella review of the evidence: What factors influence the caring relationship between a nurse and patient? Journal of Advanced Nursing, 72(4), pp. 723-34. [DOI:10.1111/jan.12862] [PMID]
Wong, E. G., et al. 2016. Association of severity of illness and intensive care unit readmission: A systematic review. Heart & Lung, 45(1), pp. 3-9e2. [DOI:10.1016/j.hrtlng.2015.10.040] [PMID] [PMCID]
Zamanzadeh, V., et al. 2015. Effective factors in providing holistic care: A qualitative study. Indian Journal of Palliative Care, 21(2), pp. 214-24. [DOI:10.4103/0973-1075.156506] [PMID] [PMCID]
Zeraati, M. & Alavi, N. M., 2014. Designing and validity evaluation of quality of nursing care scale in intensive care units. Journal of Nursing Measurement, 22(3), pp. 461-71. [DOI:10.1891/1061-3749.22.3.461] [PMID]
Berwick, D. M., 2016. Era 3 for medicine and health care. JAMA, 315(13), pp. 1329-30. [DOI:10.1001/jama.2016.1509] [PMID]
Bilgin, S. & Gozum, S., 2018. Effect of nursing care given at home on the quality of life of patients with stomach cancer and their family caregivers’ nursing care. European Journal of Cancer Care, 27(2), p. e12567. [DOI:10.1111/ecc.12567] [PMID]
Bingold, T. M., et al. 2015. Individual organ failure and concomitant risk of mortality differs according to the type of admission to ICU-a retrospective study of SOFA score of 23,795 patients. PLoS One, 10(8), p. e0134329. [DOI:10.1371/journal.pone.0134329] [PMID] [PMCID]
Bruyneel, A., et al. 2019. Measuring the nursing workload in intensive care with the Nursing Activities Score (NAS): A prospective study in 16 hospitals in Belgium. Journal of Critical Care, 54, pp. 205-11. [DOI:10.1016/j.jcrc.2019.08.032] [PMID]
Chantry, A. A., et al. 2015. Pregnancy-related ICU admissions in France: Trends in rate and severity, 2006-2009. Critical Care Medicine, 43(1), pp. 78-86. [DOI:10.1097/CCM.0000000000000601] [PMID]
Cho, S. H. & Yun, S. C., 2009. Bed-to-nurse ratios, provision of basic nursing care, and in-hospital and 30-day mortality among acute stroke patients admitted to an intensive care unit: Cross-sectional analysis of survey and administrative data. International Journal of Nursing Studies, 46(8), pp. 1092-101. [DOI:10.1016/j.ijnurstu.2009.02.001] [PMID]
Cremasco, M. F., Wenzel, F., Zanei, S. S. & Whitaker, I. Y. 2013. Pressure ulcers in the intensive care unit: the relationship between nursing workload, illness severity and pressure ulcer risk. Journal of Clinical Nursing, 22, 2183-2191. [DOI:10.1111/j.1365-2702.2012.04216.x] [PMID]
Elias, A. C., et al. 2006. [Application of the therapeutic intervention scoring system (TISS 28) at an intensive care unit to evaluate the severity of the patient (Portuguese)]. Revista Latino-Americana de Enfermagem, 14(3), pp. 324-9. [DOI:10.1590/S0104-11692006000300004] [PMID]
Evans, R. G. & Stoddart, G. L., 2017. Producing health, consuming health care. Why are some people healthy and others not? Milton Park: Routledge. [DOI:10.4324/9781315135755-3]
Falk, A. C. & Wallin, E. M., 2016. Quality of patient care in the critical care unit in relation to nurse patient ratio: A descriptive study. Intensive and Critical Care Nursing, 35, pp. 74-9. [DOI:10.1016/j.iccn.2016.01.002] [PMID]
Giuliani, E., et al. 2018. The burden of not-weighted factors-nursing workload in a medical intensive care unit. Intensive and Critical Care Nursing, 47, pp. 98-101. [DOI:10.1016/j.iccn.2018.02.009] [PMID]
Glance, L. G., et al. 2012. The association between nurse staffing and hospital outcomes in injured patients. BMC Health Services Research, 12, p. 247. [DOI:10.1186/1472-6963-12-247] [PMID] [PMCID]
Hall, L. M. & Doran, D. 2004. Nurse staffing, care delivery model, and patient care quality. Journal of Nursing Care Quality, 19(1), pp. 27-33. [DOI:10.1097/00001786-200401000-00007] [PMID]
Izumi, S., Baggs, J. G. & Knafl, K. A., 2010. Quality nursing care for hospitalized patients with advanced illness: Concept development. Research in Nursing & Health, 33(4), pp. 299-315. [DOI:10.1002/nur.20391] [PMID] [PMCID]
Jansson, M. M., Syrjälä, H. P. & Ala-Kokko, T. I., 2019. Association of nurse staffing and nursing workload with ventilator-associated pneumonia and mortality: A prospective, single-center cohort study. Journal of Hospital Infection, 101(3), pp. 257-63. [DOI:10.1016/j.jhin.2018.12.001] [PMID]
Kaukonen, K. M., et al. 2014. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA, 311(13), pp. 1308-16. [DOI:10.1001/jama.2014.2637] [PMID]
Kaymak, C., et al. 2018. Mortality of adult intensive care units in Turkey using the APACHE II and SOFA systems (outcome assessment in Turkish intensive care units). Archives of Medical Science, 14(3), pp. 510-5. [DOI:10.5114/aoms.2016.59709] [PMID] [PMCID]
Kendall-Gallagher, D. & Blegen, M. A., 2009. Competence and certification of registered nurses and safety of patients in intensive care units. American Journal of Critical Care, 18(2), pp. 106-13. [DOI:10.4037/ajcc2009487] [PMID] [PMCID]
Kraljic, S., et al. 2017. Evaluation of nurses’ workload in intensive care unit of a tertiary care university hospital in relation to the patients’ severity of illness: A prospective study. International Journal of Nursing Studies, 76, pp. 100-5. [DOI:10.1016/j.ijnurstu.2017.09.004] [PMID]
La Sala, R., et al. 2017. The quality of nursing in intensive care: A development of a rating scale. Acta Biomedica, 88(1S), pp. 61-8. [PMID]
Ma, C., Olds, D. M. & Dunton, N. E., 2015. Nurse work environment and quality of care by unit types: A cross-sectional study. International Journal of Nursing Studies, 52(10), pp. 1565-72. [DOI:10.1016/j.ijnurstu.2015.05.011] [PMID]
Mahjoubipour, H., et al. 2012. [Efficiency of SOFA scoring system on predicting mortality rate and stay length in intensive care unit for patients of Al-Zahra hospital of Isfahan (Persian)]. Medical-Surgical Nursing Journal, 1(2), pp. 6-10. https://brief.land/msnj/articles/87468.html
Moreno, R. & Morais, P., 1997. Validation of the simplified therapeutic intervention scoring system on an independent database. Intensive Care Medicine, 23(6), pp. 640-4. [DOI:10.1007/s001340050387] [PMID]
Morgan, S. & Yoder, L. H., 2012. A concept analysis of person-centered care. Journal of Holistic Nursing, 30(1), pp. 6-15. [DOI:10.1177/0898010111412189] [PMID]
Muehler, N., et al. 2010. Serial measurement of Therapeutic Intervention Scoring System-28 (TISS-28) in a surgical intensive care unit. Journal of Critical Care, 25(4), pp. 620-7. [DOI:10.1016/j.jcrc.2010.03.008] [PMID]
Needleman, J., et al. 2011. Nurse staffing and inpatient hospital mortality. The New England Journal of Medicine, 364(11), pp. 1037-45. [DOI:10.1056/NEJMsa1001025] [PMID]
Padilha, K. G., et al. 2007. Nursing workload in intensive care units: A study using the Therapeutic Intervention Scoring System-28 (TISS-28). Intensive and Critical Care Nursing, 23(3), pp. 162-9. [DOI:10.1016/j.iccn.2006.07.004] [PMID]
Piotrkowska, R., et al. 2020. Assessment of the quality of nursing care of postoperative pain in patients undergoing vascular procedures. Journal of PeriAnesthesia Nursing, 35(5), pp. 484-90. [DOI:10.1016/j.jopan.2020.03.010] [PMID]
Rice, H., Say, R. & Betihavas, V., 2018. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review. Patient Education and Counseling, 101(3), pp. 363-74. [DOI:10.1016/j.pec.2017.10.002] [PMID]
Seker, Y. T., Hergunsel, O., Bostanci, I., & Zeydan, A. 2018. Utility of the Therapeutic Intervention Scoring System-28 to Predict Mortality in Intensive Care Units. EJMO, 2(1), pp. 35-3. https://www.researchgate.net/publication/321585013_Utility_of_using_the__System-
Tan, Y. Y., Montagnese, S. & Mani, A. R., 2020. Organ system network disruption is associated with poor prognosis in patients with chronic liver failure. Frontiers in Physiology, 11, p. 983. [DOI:10.3389/fphys.2020.00983] [PMID] [PMCID]
Tobar, E., et al. 2010. [Confusion Assessment Method for diagnosing delirium in ICU patients (CAM-ICU): Cultural adaptation and validation of the Spanish version (Spanish)]. Medicina Intensiva, 34(1), pp. 4-13. [DOI:10.1016/j.medin.2009.04.003] [PMID]
Vincent, J. L., et al. 1996. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Medicine, 22(7), pp. 707-10. [DOI:10.1007/BF01709751] [PMID]
Wiechula, R., et al. 2016. Umbrella review of the evidence: What factors influence the caring relationship between a nurse and patient? Journal of Advanced Nursing, 72(4), pp. 723-34. [DOI:10.1111/jan.12862] [PMID]
Wong, E. G., et al. 2016. Association of severity of illness and intensive care unit readmission: A systematic review. Heart & Lung, 45(1), pp. 3-9e2. [DOI:10.1016/j.hrtlng.2015.10.040] [PMID] [PMCID]
Zamanzadeh, V., et al. 2015. Effective factors in providing holistic care: A qualitative study. Indian Journal of Palliative Care, 21(2), pp. 214-24. [DOI:10.4103/0973-1075.156506] [PMID] [PMCID]
Zeraati, M. & Alavi, N. M., 2014. Designing and validity evaluation of quality of nursing care scale in intensive care units. Journal of Nursing Measurement, 22(3), pp. 461-71. [DOI:10.1891/1061-3749.22.3.461] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2021/10/18 | Accepted: 2021/11/13 | Published: 2022/02/1
Received: 2021/10/18 | Accepted: 2021/11/13 | Published: 2022/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






