Sat, Aug 9, 2025
[Archive]
Volume 8, Issue 2 (Spring 2022)
JCCNC 2022, 8(2): 139-146 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sajedi S, Jafarjalal E, Haghani S. Relationship between Psychological Capital and Sleep Quality in Intensive Care Unit Nurses. JCCNC 2022; 8 (2) :139-146
URL: http://jccnc.iums.ac.ir/article-1-350-en.html
URL: http://jccnc.iums.ac.ir/article-1-350-en.html
1- Department of Intensive Care Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Nursing Management, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,jafarjalal.e@iums.ac.ir
3- Department of Biostatistics, School of Health, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Nursing Management, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Biostatistics, School of Health, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 593 kb]
(740 Downloads)
| Abstract (HTML) (2159 Views)
Full-Text: (595 Views)
1. Introduction
In the health care system, nurses play an important role in improving healthcare services. (Ebrahimi Monfared, Sadegh, & Gohar, 2017). Due to heavy workload and stressful work environment as well as some individual and family problems, nurses experience high psychological problems which can reduce their job satisfaction, commitment and attachment (Adib-Hajbaghery, Izadi-Avanji, & Akbari, 2012). Experiencing high work stress puts them at risk for illness and mental health problems (Farahati 2020). Therefore, it is necessary to study the mental health status of nurses and identify the psychological factors affecting their mental health (Jafari 2015). Sleep plays an important role in humans’ health, learning process, and memory, and can affect their quality of life. Nursing is among the occupations that require night shift work associated with sleep disorders (Babamiri et al., 2017). Sleep quality is a key factor for overall health and well-being. Poor sleep quality is one of the important factors associated with chronic fatigue and a negative impact on job performance in nurses and can reduce both the quality and quantity of their works which affects their responses to the patients’ needs (Samaha et al., 2007).
In recent years, Psychological Capital (PsyCap) is one of the phenomena that has shown a high potential in improving the health and performance of people in different work environments (Gohel 2012). PsyCap emphasizes one’s abilities and positive psychological states such as well-being, happiness, emotional intelligence, wisdom, self-awareness, creativity, and optimism (Salehi et al., 2012). PsyCap term was coined by Fred Luthans and Carolyn Youssef. In developing the framework of positive organizational behavior, they introduced positive PsyCap as a source of competitive advantage for organizations (Luthans, Youssef-Morgan & Avolio, 2007). PsyCap can play a very important role in improving the nurses’ work performance. A study showed that PsyCap is associated with a variety of variables such as job performance, job commitment, job satisfaction, anxiety, and the ability to cope with stress and problems (Peterson, & Byron 2008; Ucol-Ganiron Jr, 2012). In PsyCap, the four components of resilience, self-efficacy, optimism, and hope with a positive interaction with each other, can improve the performance of medical staff, especially nurses (Kim, 2008). Considering the importance of PsyCap in nurses’ performance and its key role in the quality of nursing care as well as the effect of nurses’ sleep quality on their mental status especially in those working in Intensive Care Units (ICUs), there is a need for more study on nurses’ PsyCap and sleep quality to gain insight. This insight is necessary not only to assess the current state of PsyCap and sleep quality in nurses, but also to draw the attention of health authorities to this issue and conduct more studies. This study aims to determine the relationship between PsyCap and sleep quality in ICU nurses.
2. Materials and Methods
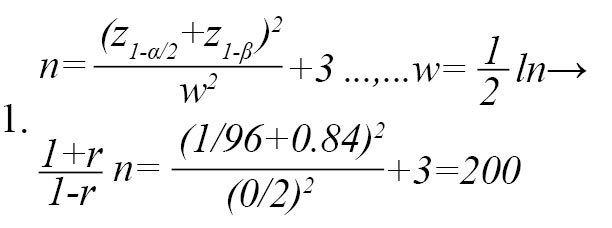
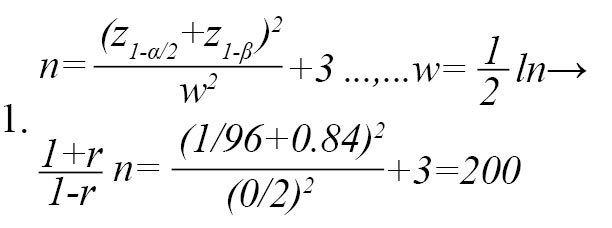
This descriptive correlational study was conducted in 2021 on 200 ICU nurses selected from the hospitals affiliated to Iran University of Medical Sciences using a proportionate stratified sampling method. The sample size was determined using the following formula at 95% confidence level and considering a test power of 80% and assuming that the correlation coefficient between PsyCap and sleep quality in nurses is at least 0.2 so that the relationship be statistically significant (Equations 1):
The data were collected using a three-part questionnaire. The first part surveys the nurses’ demographic information including: age, gender, educational level, marital status, shiftwork status, work experience, work experience in ICUs, overtime work, and underlying illness. The second part was the Psychological Capital Questionnaire (PCQ). This questionnaire has been developed by McGee (2011) and translated into Persian and validated by Golparvar (2013). The PCQ consists of 26 items and four subscales of self-efficacy (items 1-7), hope (items 8-14), resilience (items 15-20), and optimism (items 21-26), which are rated on a 6-point Likert scale (From 1=strongly disagree to 6=strongly agree). To obtain the total PCQ score, the subscale scores are summed up. The total score ranges from 26 to 156, with higher scores indicating a higher level of PsyCap. To compare the components of PCQ, the mean score of each component was calculated ranging from 0 to 100, and the results showed that the highest and lowest mean scores were related to the self-efficacy (76.52) and optimism (69.83), respectively. The validity and reliability of PCQ along with other forms of PsyCap have been examined in many studies where its acceptable validity and reliability has been reported. McGee (2011) determined the validity of this questionnaire by exploratory factor analysis and Varimax rotation on 26 questions. The Cronbach’s alpha for self-efficacy, hope, resilience and optimism were obtained 0.88, 0.86, 0.83, and 0.83, respectively. The acceptable construct validity of the Persian version of PCQ using the exploratory factor analysis has been reported and the Cronbach’s alpha of its subscales are reported 0.81, 0.86, 0.79, and 0.75, respectively (Golparvar, 2013). The internal consistency of the Persian version PCQ was assessed in the present study. The Cronbach’s alpha coefficients for self-efficacy, hope, resilience and optimism were obtained 0.81, 0.91, 0.80, and 0.87, respectively. The third part is the Pittsburgh Sleep Quality Index (PSQI) which was developed by Buysse et al. (1989) at the Pittsburgh Institute of Psychiatry and has 18 items and seven subscales including subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medications, and daytime drowsiness. Each subscale yields a score from 0=no difficulty to 3=severe difficulty and the total score ranges from 0 to 21. A score >5 is considered as a significant sleep disturbance. The internal consistency of PSQI using Cronbach’s alpha is 0.83 (Buysse et al., 1989). The reliability of the Persian version of PSQI using Cronbach’s alpha coefficient is 0.89 (Ehteshamzadeh, 2010). Due to the frequent use of PSQI in the nursing community, there was no need to re-evaluate reliability in the present study.
To perform sampling, first, the total sample size (n=200) was divided by the total number of population and multiplied by the number of nurses in ICUs of each hospital; hence, the share of each hospital in samples was determined. The researcher then referred to each hospital and selected nurses who met the inclusion criteria (One year experience) and were willing to participate in the study. Sampling and completion of questionnaires took about three months. The obtained data were analyzed using descriptive (frequency, mean, and standard deviation) and inferential (Pearson correlation test) statistics in SPSS software v.16.
3. Results
Most of nurses were in the age range of 30-39 years (43.2%) and female (83.5%). Moreover, 85.5% of them held a bachelor’s degree, 14.5% held a master’s degree, and 69.5% were married. Most of the nurses had rotational shiftwork, a work experience of 6-10 years and had less than 5 years of experience in ICUs (Table 1).
.jpg)
Most of them worked overtime for <50 hours, and had no any underlying disease. Table 2 presents the Mean±SD PCQ and PSQI scores.
.jpg)
The Mean±SD PCQ score was 120.61±17.68. The highest and lowest means belonged to the components of self-efficacy (33.79) and optimism (26.95), respectively. The Mean±SD score of PSQI was 8.81±3.62. The highest and lowest means belonged to the components of sleep duration (1.67), and use of sleep medications (0.41), respectively.
Table 3 represents the results of assessing correlation between the components of PCQ and PSQI.
.jpg)
As can be seen, the correlation coefficients of self-efficacy (the first component of PCQ) with subjective sleep quality, sleep latency, sleep disturbances, daytime drowsiness, and the total score of sleep quality were -0.16, -0.32, -0.24, -0.26, and, -0.28, respectively (P<0.05) which indicates a statistically significant negative correlation between them. Therefore, it can be said that the reduction in these domains and improvement in sleep quality, causes an increase in self-efficacy.
The correlation coefficients of hope (the second component of PCQ) with subjective sleep quality, sleep latency, sleep disturbances, daytime drowsiness, and the total score of sleep quality were -0.17, -0.22, -0.17, -0.33, and -0.24, respectively (P<0.05) which indicates a significant negative correlation between them, and it can be said that hope increases by the reduction in these domains and improvement in sleep quality.
The correlation coefficients of resilience (the third component of PCQ) with subjective sleep quality, sleep latency, sleep disturbances, daytime drowsiness, and the total score of sleep quality were -0.16, -0.16, -0.14, -0.33, and -0.2, respectively (P<0.05) which indicates a significant negative correlation between them; therefore, resilience increases by a decrease in these domains and improvement in sleep quality.
The correlation coefficients of optimism (the fourth component of PCQ) with daytime drowsiness and the total score of sleep quality were -0.26 and -0.15, respectively (P<0.05) which indicates a significant negative correlation between them; hence, with a decrease in daytime drowsiness and improvement of sleep quality, optimism increases.
Finally, the correlation coefficients of total PCQ score with subjective sleep quality, sleep latency, sleep disorders, sleep disturbances, daytime drowsiness, the total score of sleep quality were -0.16, -0.22, -0.18, -0.33, and -0.24, respectively (P<0.05) which indicates a significant negative correlation between them; therefore, with a decrease in these domains and improvement of sleep quality, PsyCap increases.
4. Discussion
The findings of the current study showed that the Mean±SD PsyCap score of ICU nurses was 120.61±17.68. which is close to the value reported in other study (17.86) (Jafarizadeh, Sadeghi, & Azarbarzin, 2019). A study was found that nurses had a relatively high level of PsyCap; among the components of PsyCap, the highest score belonged to self-efficacy, and the lowest score belonged to resilience (Jafar Jalal et al., 2021). This is consistent with our results. In our study, nurses also had a high level of PsyCap and the highest and lowest means of PsyCap were related to self-efficacy and optimism components, respectively.
Another result of our study was the relationship between PsyCap and sleep quality such that better sleep quality was associated with more PsyCap. This is consistent with the results of other studies. A study emphasized that PsyCap is a strong predictor of sleep quality (Hystad and Eid 2016). Since training programs can help modify dysfunctional beliefs about sleep (Morin, Blais, & Savard, 2002; Thakral et al., 2020), future experimental research as part of targeted sleep education programs can explore whether PsyCap training can minimize the impact of poor sleep quality (Sabot and Hicks 2020). A study was found that mental health, the quality of life, and hardship can predict the quality of sleep in nurses. Therefore, it was suggested that evaluating the sleep quality and its relationship with mental health, the quality of life, and hardship can provide valuable guidelines for improving nurses’ sleep quality (Fatehi & Dobaradaran 2020). A study showed that psychological well-being is directly associated with optimal sleep quality and may moderate the effects of psychological risk factors. In this regard, the level of psychological well-being increases when the effects of psychological risk factors are moderated. Disturbed sleep is likely to lead to decreased levels of psychological well-being, and positive mental states can lead to improved sleep quality (Barber, Rupprecht, & Munz, 2014). On the other hand, a study reported that sleep disorders and mental health are related to each other, and one can be the cause of other (Mansouri, Mokhayeri, & Tavakol, 2016). According to the findings of the present study, the sleep quality of ICU nurses can be increased through improving their PsyCap. Due to the adverse effects of low sleep quality on the quality of care for patients, appropriate planning to improve the sleep quality of these nurses is necessary.
There were some limitations in this study. The first limitation was the use of a descriptive correlational method; hence, a cause-and-effect analysis is not logical. The second limitation was the mental preoccupation and high workload of nurses, which can affect the accuracy of their answers to the questions.
5. Conclusion
Improved sleep quality is associated with increased PsyCap in ICU nurses. In other words, the nurses’ sleep quality can be improved by increasing their PsyCap. Therefore, they should have adequate and quality sleep for proper performance and success at workplace. In order to improve their PsyCap, it is suggested that educational and motivational courses be held periodically for them. Nurse managers and policymakers can use the findings, especially by considering PsyCap and its self-efficacy component, to develop programs to improve the quality of sleep in nurses.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1399.1161). The study objectives were explained to the participants and they were assured that their information would be kept confidential. Written informed consent was obtained from them before completing the questionnaires.
Funding
Iran University of Medical Sciences financially supported the study.
Authors' contributions
Conceptualization, investigation, writing - original draft: Jafar Jalal and Sahar Sajedi; Methodology, writing - editing, and final approval: All authors; Supervision: Jafar Jalal.
Conflict of interest
The authors declare no conflict of interests.
Acknowledgments
The authors would like to thank Iran University of Medical Sciences for the financial support, the staff of Haft-e-Tir, Shohadae Yaftabad, Firoozgar, and Rasool-e- Akram hospitals and the nurses who participated in this study for their valuable support and cooperation.
References
Adib-Hajbaghery, M., Izadi-Avanji, F. & Akbari, H., 2012. Quality of sleep and its related risk factors in hospitalized older patients in Kashan’s Hospitals, Iran 2009. Iranian Journal of Nursing and Midwifery Research, 17(6), pp. 414-20. [PMID]
Babamiri, M., et al., 2017. [The study of sleep health education effect on sleep quality among Lorestan nursing personnel (Persian)]. Journal of Ergonomics, 4(4), pp. 8-13. [DOI:10.21859/joe-04042]
Barber, L. K., Rupprecht, E. A. & Munz, D. C., 2014. Sleep habits may undermine well-being through the stressor appraisal process. Journal of Happiness Studies, 15(2), pp. 285-99. [DOI:10.1007/s10902-013-9422-2]
Buysse, D. J., et al., 1989. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), pp. 193-213. [DOI:10.1016/0165-1781(89)90047-4]
Ebrahimi Monfared, M., Sadegh, M. & Gohari, Z., 2017. [Effect of melatonin and vitamin E on EEG, sleep quality and quality of life of shift-working nurses in Arak hospitals (Persian)]. Journal of Arak University of Medical Sciences, 19(12), pp. 1-11. http://jams.arakmu.ac.ir/article-1-4602-en.html
Ehteshamzadeh, P. & Marashi, M., 2010. [The relation between the intensity of insomnia, sleep quality sleepiness and mind mental health with educational operation in Ahwaz male teenager (Persian)]. Journal Of Social Psychology (New Findings in Psychology), 5(15), pp. 65-76. https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=218302
Farahati, M., 2020. [Psychological impacts of the spread of coronavirus in society (Persian)]. Social Impact Assessment, 1(2), pp. 207-25. https://www.sid.ir/en/journal/ViewPaper.aspx?ID=739461
Fatehi, S. & Dobaradaran, S., 2020. [The relationship between mental health, quality of life and hardship with the quality of nurses’ sleep (Persian)]. Journal of New Strategies in Psychology and Educational Sciences, 6(3), pp. 1-12. https://www.ijpk.ir/fa/showart-dc41695af0a8b54ad72a245b6e4ac98f
Gohel, K., 2012. Psychological capital as a determinant of employee satisfaction. International Referred Research Journal, 3(36), pp. 34-37.
Golparvar, M., 2013. Translate and validation of psychological capital questionnaire-26 items. Unpublished Manuscript, Islamic Azad University, Esfahan Branch, Esfahan, Iran.
Hystad, S. W. & Eid, J., 2016. Sleep and fatigue among seafarers: The role of environmental stressors, duration at sea and psychological capital. Safety and Health at Work, 7(4), pp. 363-71. [DOI:10.1016/j.shaw.2016.05.006] [PMID] [PMCID]
Jafar Jalal, E., et al., 2021. [Psychological capital of nurses working in Academic Medical Centers of Iran University of Medical Sciences (Persian)]. Iran Journal of Nursing, 34(129), pp. 27-38. [DOI:10.52547/ijn.34.129.27]
Jafari, E., 2015. [Spiritual predictors of mental health in nurses: The meaning in life, religious well-being and existential well-being (Persian)]. Nursing and Midwifery Journal, 13(8), pp. 676-84. http://unmf.umsu.ac.ir/article-1-1606-en.html
Jafarizadeh, R., Sadeghi, N. & Azarbarzin, M., 2019. [Dimensions of psychological capital in the nurses employed in psychiatric hospitals and the correlations with demographical variables (Persian)]. Iran Journal of Nursing, 31(116), pp. 40-8. [DOI:10.29252/ijn.31.116.40]
Kim, J. U., 2008. The effect of a R/T group counseling program on the internet addiction level and self-esteem of Internet addiction university students. International Journal of Reality Therapy, 27(2), pp. 4-12. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.520.6598&rep=rep1&type=pdf
Luthans, F., Youssef, C. M, & Avolio, B. J., 2007. Psychological capital: Developing the human competitive edge. Oxford: Oxford University Press. [DOI:10.1093/acprof:oso/9780195187526.001.0001]
McGee, EA., 2011. An examination of the stability of positive psychological capital using frequency-based measurement [PhD dissertation]. Knoxville: University of Tennessee. https://trace.tennessee.edu/cgi/viewcontent.cgi?article=2049&context=utk_graddiss
Mansouri, A., Mokhayeri, Y. & Tavakol, Z., 2016. Sleep onset latency in students living in dormitories at Tehran University of Medical Sciences: A survival analysis. Research Journal of Pharmaceutical, Biological and Chemical Sciences, 7(2), pp. 2127-35. http://eprints.skums.ac.ir/1040/1/%5B289%5D.pdf
Morin, C., Blais, F. & Savard, J., 2002. Are changes in beliefs and attitudes about sleep related to sleep improvements in the treatment of insomnia? Behaviour Research and Therapy, 40(7), pp. 741-52. [DOI:10.1016/S0005-7967(01)00055-9]
Peterson, S. J. & Byron, K., 2007. Exploring the role of hope in job performance: Results from four studies. Journal of Organizational Behavior, 29(6), pp. 785-803. [DOI:10.1002/job.492]
Sabot, D. L. & Hicks R. E., 2020. Does psychological capital mediate the impact of dysfunctional sleep beliefs on well-being? Heliyon, 6(6), pp. e04314. [DOI:10.1016/j.heliyon.2020.e04314] [PMID] [PMCID]
Salehi, A., et al., 2012. [Improvement organizational commitment and job satisfaction in Iranian public organizations: Study and explanation the role of psychological capital (Persian)]. Organizational Resources Management Researchs, 2(2), pp. 1-21. http://ormr.modares.ac.ir/article-28-12029-en.html
Samaha, E., et al., 2007. Psychological, lifestyle and coping contributors to chronic fatigue in shift-worker nurses. Journal of Advanced Nursing, 59(3), pp. 221-32. [DOI:10.1111/j.1365-2648.2007.04338.x] [PMID]
Thakral, M., et al., 2020. Changes in dysfunctional beliefs about sleep after cognitive behavioral therapy for insomnia: A systematic literature review and meta-analysis. Sleep Medicine Reviews, 49, pp. 101230. [DOI:10.1016/j.smrv.2019.101230] [PMID] [PMCID]
Ucol-Ganiron Jr, T., 2012. The additive value of psychological capital in predicting structural project success and life satisfaction of structural engineers. International Journal of Social Science and Humanity, 2(4), pp. 291-5. [DOI:10.7763/IJSSH.2012.V2.112]
In the health care system, nurses play an important role in improving healthcare services. (Ebrahimi Monfared, Sadegh, & Gohar, 2017). Due to heavy workload and stressful work environment as well as some individual and family problems, nurses experience high psychological problems which can reduce their job satisfaction, commitment and attachment (Adib-Hajbaghery, Izadi-Avanji, & Akbari, 2012). Experiencing high work stress puts them at risk for illness and mental health problems (Farahati 2020). Therefore, it is necessary to study the mental health status of nurses and identify the psychological factors affecting their mental health (Jafari 2015). Sleep plays an important role in humans’ health, learning process, and memory, and can affect their quality of life. Nursing is among the occupations that require night shift work associated with sleep disorders (Babamiri et al., 2017). Sleep quality is a key factor for overall health and well-being. Poor sleep quality is one of the important factors associated with chronic fatigue and a negative impact on job performance in nurses and can reduce both the quality and quantity of their works which affects their responses to the patients’ needs (Samaha et al., 2007).
In recent years, Psychological Capital (PsyCap) is one of the phenomena that has shown a high potential in improving the health and performance of people in different work environments (Gohel 2012). PsyCap emphasizes one’s abilities and positive psychological states such as well-being, happiness, emotional intelligence, wisdom, self-awareness, creativity, and optimism (Salehi et al., 2012). PsyCap term was coined by Fred Luthans and Carolyn Youssef. In developing the framework of positive organizational behavior, they introduced positive PsyCap as a source of competitive advantage for organizations (Luthans, Youssef-Morgan & Avolio, 2007). PsyCap can play a very important role in improving the nurses’ work performance. A study showed that PsyCap is associated with a variety of variables such as job performance, job commitment, job satisfaction, anxiety, and the ability to cope with stress and problems (Peterson, & Byron 2008; Ucol-Ganiron Jr, 2012). In PsyCap, the four components of resilience, self-efficacy, optimism, and hope with a positive interaction with each other, can improve the performance of medical staff, especially nurses (Kim, 2008). Considering the importance of PsyCap in nurses’ performance and its key role in the quality of nursing care as well as the effect of nurses’ sleep quality on their mental status especially in those working in Intensive Care Units (ICUs), there is a need for more study on nurses’ PsyCap and sleep quality to gain insight. This insight is necessary not only to assess the current state of PsyCap and sleep quality in nurses, but also to draw the attention of health authorities to this issue and conduct more studies. This study aims to determine the relationship between PsyCap and sleep quality in ICU nurses.
2. Materials and Methods
This descriptive correlational study was conducted in 2021 on 200 ICU nurses selected from the hospitals affiliated to Iran University of Medical Sciences using a proportionate stratified sampling method. The sample size was determined using the following formula at 95% confidence level and considering a test power of 80% and assuming that the correlation coefficient between PsyCap and sleep quality in nurses is at least 0.2 so that the relationship be statistically significant (Equations 1):
The data were collected using a three-part questionnaire. The first part surveys the nurses’ demographic information including: age, gender, educational level, marital status, shiftwork status, work experience, work experience in ICUs, overtime work, and underlying illness. The second part was the Psychological Capital Questionnaire (PCQ). This questionnaire has been developed by McGee (2011) and translated into Persian and validated by Golparvar (2013). The PCQ consists of 26 items and four subscales of self-efficacy (items 1-7), hope (items 8-14), resilience (items 15-20), and optimism (items 21-26), which are rated on a 6-point Likert scale (From 1=strongly disagree to 6=strongly agree). To obtain the total PCQ score, the subscale scores are summed up. The total score ranges from 26 to 156, with higher scores indicating a higher level of PsyCap. To compare the components of PCQ, the mean score of each component was calculated ranging from 0 to 100, and the results showed that the highest and lowest mean scores were related to the self-efficacy (76.52) and optimism (69.83), respectively. The validity and reliability of PCQ along with other forms of PsyCap have been examined in many studies where its acceptable validity and reliability has been reported. McGee (2011) determined the validity of this questionnaire by exploratory factor analysis and Varimax rotation on 26 questions. The Cronbach’s alpha for self-efficacy, hope, resilience and optimism were obtained 0.88, 0.86, 0.83, and 0.83, respectively. The acceptable construct validity of the Persian version of PCQ using the exploratory factor analysis has been reported and the Cronbach’s alpha of its subscales are reported 0.81, 0.86, 0.79, and 0.75, respectively (Golparvar, 2013). The internal consistency of the Persian version PCQ was assessed in the present study. The Cronbach’s alpha coefficients for self-efficacy, hope, resilience and optimism were obtained 0.81, 0.91, 0.80, and 0.87, respectively. The third part is the Pittsburgh Sleep Quality Index (PSQI) which was developed by Buysse et al. (1989) at the Pittsburgh Institute of Psychiatry and has 18 items and seven subscales including subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medications, and daytime drowsiness. Each subscale yields a score from 0=no difficulty to 3=severe difficulty and the total score ranges from 0 to 21. A score >5 is considered as a significant sleep disturbance. The internal consistency of PSQI using Cronbach’s alpha is 0.83 (Buysse et al., 1989). The reliability of the Persian version of PSQI using Cronbach’s alpha coefficient is 0.89 (Ehteshamzadeh, 2010). Due to the frequent use of PSQI in the nursing community, there was no need to re-evaluate reliability in the present study.
To perform sampling, first, the total sample size (n=200) was divided by the total number of population and multiplied by the number of nurses in ICUs of each hospital; hence, the share of each hospital in samples was determined. The researcher then referred to each hospital and selected nurses who met the inclusion criteria (One year experience) and were willing to participate in the study. Sampling and completion of questionnaires took about three months. The obtained data were analyzed using descriptive (frequency, mean, and standard deviation) and inferential (Pearson correlation test) statistics in SPSS software v.16.
3. Results
Most of nurses were in the age range of 30-39 years (43.2%) and female (83.5%). Moreover, 85.5% of them held a bachelor’s degree, 14.5% held a master’s degree, and 69.5% were married. Most of the nurses had rotational shiftwork, a work experience of 6-10 years and had less than 5 years of experience in ICUs (Table 1).
.jpg)
Most of them worked overtime for <50 hours, and had no any underlying disease. Table 2 presents the Mean±SD PCQ and PSQI scores.
.jpg)
The Mean±SD PCQ score was 120.61±17.68. The highest and lowest means belonged to the components of self-efficacy (33.79) and optimism (26.95), respectively. The Mean±SD score of PSQI was 8.81±3.62. The highest and lowest means belonged to the components of sleep duration (1.67), and use of sleep medications (0.41), respectively.
Table 3 represents the results of assessing correlation between the components of PCQ and PSQI.
.jpg)
As can be seen, the correlation coefficients of self-efficacy (the first component of PCQ) with subjective sleep quality, sleep latency, sleep disturbances, daytime drowsiness, and the total score of sleep quality were -0.16, -0.32, -0.24, -0.26, and, -0.28, respectively (P<0.05) which indicates a statistically significant negative correlation between them. Therefore, it can be said that the reduction in these domains and improvement in sleep quality, causes an increase in self-efficacy.
The correlation coefficients of hope (the second component of PCQ) with subjective sleep quality, sleep latency, sleep disturbances, daytime drowsiness, and the total score of sleep quality were -0.17, -0.22, -0.17, -0.33, and -0.24, respectively (P<0.05) which indicates a significant negative correlation between them, and it can be said that hope increases by the reduction in these domains and improvement in sleep quality.
The correlation coefficients of resilience (the third component of PCQ) with subjective sleep quality, sleep latency, sleep disturbances, daytime drowsiness, and the total score of sleep quality were -0.16, -0.16, -0.14, -0.33, and -0.2, respectively (P<0.05) which indicates a significant negative correlation between them; therefore, resilience increases by a decrease in these domains and improvement in sleep quality.
The correlation coefficients of optimism (the fourth component of PCQ) with daytime drowsiness and the total score of sleep quality were -0.26 and -0.15, respectively (P<0.05) which indicates a significant negative correlation between them; hence, with a decrease in daytime drowsiness and improvement of sleep quality, optimism increases.
Finally, the correlation coefficients of total PCQ score with subjective sleep quality, sleep latency, sleep disorders, sleep disturbances, daytime drowsiness, the total score of sleep quality were -0.16, -0.22, -0.18, -0.33, and -0.24, respectively (P<0.05) which indicates a significant negative correlation between them; therefore, with a decrease in these domains and improvement of sleep quality, PsyCap increases.
4. Discussion
The findings of the current study showed that the Mean±SD PsyCap score of ICU nurses was 120.61±17.68. which is close to the value reported in other study (17.86) (Jafarizadeh, Sadeghi, & Azarbarzin, 2019). A study was found that nurses had a relatively high level of PsyCap; among the components of PsyCap, the highest score belonged to self-efficacy, and the lowest score belonged to resilience (Jafar Jalal et al., 2021). This is consistent with our results. In our study, nurses also had a high level of PsyCap and the highest and lowest means of PsyCap were related to self-efficacy and optimism components, respectively.
Another result of our study was the relationship between PsyCap and sleep quality such that better sleep quality was associated with more PsyCap. This is consistent with the results of other studies. A study emphasized that PsyCap is a strong predictor of sleep quality (Hystad and Eid 2016). Since training programs can help modify dysfunctional beliefs about sleep (Morin, Blais, & Savard, 2002; Thakral et al., 2020), future experimental research as part of targeted sleep education programs can explore whether PsyCap training can minimize the impact of poor sleep quality (Sabot and Hicks 2020). A study was found that mental health, the quality of life, and hardship can predict the quality of sleep in nurses. Therefore, it was suggested that evaluating the sleep quality and its relationship with mental health, the quality of life, and hardship can provide valuable guidelines for improving nurses’ sleep quality (Fatehi & Dobaradaran 2020). A study showed that psychological well-being is directly associated with optimal sleep quality and may moderate the effects of psychological risk factors. In this regard, the level of psychological well-being increases when the effects of psychological risk factors are moderated. Disturbed sleep is likely to lead to decreased levels of psychological well-being, and positive mental states can lead to improved sleep quality (Barber, Rupprecht, & Munz, 2014). On the other hand, a study reported that sleep disorders and mental health are related to each other, and one can be the cause of other (Mansouri, Mokhayeri, & Tavakol, 2016). According to the findings of the present study, the sleep quality of ICU nurses can be increased through improving their PsyCap. Due to the adverse effects of low sleep quality on the quality of care for patients, appropriate planning to improve the sleep quality of these nurses is necessary.
There were some limitations in this study. The first limitation was the use of a descriptive correlational method; hence, a cause-and-effect analysis is not logical. The second limitation was the mental preoccupation and high workload of nurses, which can affect the accuracy of their answers to the questions.
5. Conclusion
Improved sleep quality is associated with increased PsyCap in ICU nurses. In other words, the nurses’ sleep quality can be improved by increasing their PsyCap. Therefore, they should have adequate and quality sleep for proper performance and success at workplace. In order to improve their PsyCap, it is suggested that educational and motivational courses be held periodically for them. Nurse managers and policymakers can use the findings, especially by considering PsyCap and its self-efficacy component, to develop programs to improve the quality of sleep in nurses.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1399.1161). The study objectives were explained to the participants and they were assured that their information would be kept confidential. Written informed consent was obtained from them before completing the questionnaires.
Funding
Iran University of Medical Sciences financially supported the study.
Authors' contributions
Conceptualization, investigation, writing - original draft: Jafar Jalal and Sahar Sajedi; Methodology, writing - editing, and final approval: All authors; Supervision: Jafar Jalal.
Conflict of interest
The authors declare no conflict of interests.
Acknowledgments
The authors would like to thank Iran University of Medical Sciences for the financial support, the staff of Haft-e-Tir, Shohadae Yaftabad, Firoozgar, and Rasool-e- Akram hospitals and the nurses who participated in this study for their valuable support and cooperation.
References
Adib-Hajbaghery, M., Izadi-Avanji, F. & Akbari, H., 2012. Quality of sleep and its related risk factors in hospitalized older patients in Kashan’s Hospitals, Iran 2009. Iranian Journal of Nursing and Midwifery Research, 17(6), pp. 414-20. [PMID]
Babamiri, M., et al., 2017. [The study of sleep health education effect on sleep quality among Lorestan nursing personnel (Persian)]. Journal of Ergonomics, 4(4), pp. 8-13. [DOI:10.21859/joe-04042]
Barber, L. K., Rupprecht, E. A. & Munz, D. C., 2014. Sleep habits may undermine well-being through the stressor appraisal process. Journal of Happiness Studies, 15(2), pp. 285-99. [DOI:10.1007/s10902-013-9422-2]
Buysse, D. J., et al., 1989. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), pp. 193-213. [DOI:10.1016/0165-1781(89)90047-4]
Ebrahimi Monfared, M., Sadegh, M. & Gohari, Z., 2017. [Effect of melatonin and vitamin E on EEG, sleep quality and quality of life of shift-working nurses in Arak hospitals (Persian)]. Journal of Arak University of Medical Sciences, 19(12), pp. 1-11. http://jams.arakmu.ac.ir/article-1-4602-en.html
Ehteshamzadeh, P. & Marashi, M., 2010. [The relation between the intensity of insomnia, sleep quality sleepiness and mind mental health with educational operation in Ahwaz male teenager (Persian)]. Journal Of Social Psychology (New Findings in Psychology), 5(15), pp. 65-76. https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=218302
Farahati, M., 2020. [Psychological impacts of the spread of coronavirus in society (Persian)]. Social Impact Assessment, 1(2), pp. 207-25. https://www.sid.ir/en/journal/ViewPaper.aspx?ID=739461
Fatehi, S. & Dobaradaran, S., 2020. [The relationship between mental health, quality of life and hardship with the quality of nurses’ sleep (Persian)]. Journal of New Strategies in Psychology and Educational Sciences, 6(3), pp. 1-12. https://www.ijpk.ir/fa/showart-dc41695af0a8b54ad72a245b6e4ac98f
Gohel, K., 2012. Psychological capital as a determinant of employee satisfaction. International Referred Research Journal, 3(36), pp. 34-37.
Golparvar, M., 2013. Translate and validation of psychological capital questionnaire-26 items. Unpublished Manuscript, Islamic Azad University, Esfahan Branch, Esfahan, Iran.
Hystad, S. W. & Eid, J., 2016. Sleep and fatigue among seafarers: The role of environmental stressors, duration at sea and psychological capital. Safety and Health at Work, 7(4), pp. 363-71. [DOI:10.1016/j.shaw.2016.05.006] [PMID] [PMCID]
Jafar Jalal, E., et al., 2021. [Psychological capital of nurses working in Academic Medical Centers of Iran University of Medical Sciences (Persian)]. Iran Journal of Nursing, 34(129), pp. 27-38. [DOI:10.52547/ijn.34.129.27]
Jafari, E., 2015. [Spiritual predictors of mental health in nurses: The meaning in life, religious well-being and existential well-being (Persian)]. Nursing and Midwifery Journal, 13(8), pp. 676-84. http://unmf.umsu.ac.ir/article-1-1606-en.html
Jafarizadeh, R., Sadeghi, N. & Azarbarzin, M., 2019. [Dimensions of psychological capital in the nurses employed in psychiatric hospitals and the correlations with demographical variables (Persian)]. Iran Journal of Nursing, 31(116), pp. 40-8. [DOI:10.29252/ijn.31.116.40]
Kim, J. U., 2008. The effect of a R/T group counseling program on the internet addiction level and self-esteem of Internet addiction university students. International Journal of Reality Therapy, 27(2), pp. 4-12. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.520.6598&rep=rep1&type=pdf
Luthans, F., Youssef, C. M, & Avolio, B. J., 2007. Psychological capital: Developing the human competitive edge. Oxford: Oxford University Press. [DOI:10.1093/acprof:oso/9780195187526.001.0001]
McGee, EA., 2011. An examination of the stability of positive psychological capital using frequency-based measurement [PhD dissertation]. Knoxville: University of Tennessee. https://trace.tennessee.edu/cgi/viewcontent.cgi?article=2049&context=utk_graddiss
Mansouri, A., Mokhayeri, Y. & Tavakol, Z., 2016. Sleep onset latency in students living in dormitories at Tehran University of Medical Sciences: A survival analysis. Research Journal of Pharmaceutical, Biological and Chemical Sciences, 7(2), pp. 2127-35. http://eprints.skums.ac.ir/1040/1/%5B289%5D.pdf
Morin, C., Blais, F. & Savard, J., 2002. Are changes in beliefs and attitudes about sleep related to sleep improvements in the treatment of insomnia? Behaviour Research and Therapy, 40(7), pp. 741-52. [DOI:10.1016/S0005-7967(01)00055-9]
Peterson, S. J. & Byron, K., 2007. Exploring the role of hope in job performance: Results from four studies. Journal of Organizational Behavior, 29(6), pp. 785-803. [DOI:10.1002/job.492]
Sabot, D. L. & Hicks R. E., 2020. Does psychological capital mediate the impact of dysfunctional sleep beliefs on well-being? Heliyon, 6(6), pp. e04314. [DOI:10.1016/j.heliyon.2020.e04314] [PMID] [PMCID]
Salehi, A., et al., 2012. [Improvement organizational commitment and job satisfaction in Iranian public organizations: Study and explanation the role of psychological capital (Persian)]. Organizational Resources Management Researchs, 2(2), pp. 1-21. http://ormr.modares.ac.ir/article-28-12029-en.html
Samaha, E., et al., 2007. Psychological, lifestyle and coping contributors to chronic fatigue in shift-worker nurses. Journal of Advanced Nursing, 59(3), pp. 221-32. [DOI:10.1111/j.1365-2648.2007.04338.x] [PMID]
Thakral, M., et al., 2020. Changes in dysfunctional beliefs about sleep after cognitive behavioral therapy for insomnia: A systematic literature review and meta-analysis. Sleep Medicine Reviews, 49, pp. 101230. [DOI:10.1016/j.smrv.2019.101230] [PMID] [PMCID]
Ucol-Ganiron Jr, T., 2012. The additive value of psychological capital in predicting structural project success and life satisfaction of structural engineers. International Journal of Social Science and Humanity, 2(4), pp. 291-5. [DOI:10.7763/IJSSH.2012.V2.112]
Type of Study: Research |
Subject:
Special
Received: 2022/01/22 | Accepted: 2022/04/4 | Published: 2022/04/21
Received: 2022/01/22 | Accepted: 2022/04/4 | Published: 2022/04/21
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |