Sat, Aug 9, 2025
[Archive]
Volume 8, Issue 4 (Autumn 2022)
JCCNC 2022, 8(4): 291-302 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shoghi M, Karimzadeh P, Mohammadi R. Mental Status and Fear of COVID-19 in Mothers of Hospitalized Children With Chronic Diseases During the Pandemic. JCCNC 2022; 8 (4) :291-302
URL: http://jccnc.iums.ac.ir/article-1-387-en.html
URL: http://jccnc.iums.ac.ir/article-1-387-en.html
1- Nursing Care Research Center, Faculty of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. , shoghi.m@iums.ac.ir
2- Iran University of Medical Sciences, Tehran, Iran.
3- Department of Pediatric Nursing, School of Nursing and Midwifery, Ardabil University of Medical Sciences, Ardabil, Iran.
2- Iran University of Medical Sciences, Tehran, Iran.
3- Department of Pediatric Nursing, School of Nursing and Midwifery, Ardabil University of Medical Sciences, Ardabil, Iran.
Full-Text [PDF 604 kb]
(565 Downloads)
| Abstract (HTML) (2285 Views)
Full-Text: (548 Views)
1. Introduction
Frequent hospitalization of a child with a chronic disease is one of the challenging life stressors for parents and family (Stremler et al., 2017). Evidence shows that the parents of these children suffer from post-traumatic stress disorder (TSD) and experience higher stress compared to other parents of hospitalized children during their stay in the hospital (Nabors et al., 2018; Iranmanesh et al., 2015). Fear and anxiety are common in the parents of hospitalized children with chronic and life-threatening disorders and it mostly occurs at the time of disease diagnosis and adverse changes in the treatment process (Masa’Deh et al., 2012). Moreover, depression is a significant issue for these parents. Persistent parental depression and anxiety can interfere with subsequent decisions, affect the treatment process, and disrupt the child-parent relationship. Researchers have reported psychological reactions, such as anxiety, depression, denial, anger, sleep disorders, and loss of confidence in caregivers of children with chronic disease. As the most substantial people in the child support system, parents, especially mothers, experience high levels of stress and anxiety and transfer it to the child (Tan et al., 2021).
Tolerating anxiety and stress for a long time will have many negative consequences for the child and the family (Nabors, 2020). Issues that put parents, especially mothers as primary caregivers under psychosocial tension include role strain, financial pressures, lifestyle changes, following complicated and lengthy treatments, changes in family planning, the physical and psychological condition of the child, and uncertainty of the disease consequences (Burke et al., 2016).
The treatment of children with chronic diseases usually follows a specific schedule. The parents know in advance when to go to the hospital, except at the beginning of the diagnosis, some exceptions, and emergency conditions; therefore, they can plan and be prepared for hospitalization. However, any change in the child’s treatment and care program will surge the parents’ stress. On the other hand, the stress due to natural disasters and pandemics, such as COVID-19 affects all aspects of family life. It can be overwhelming for caregivers of children with chronic diseases. Studies have shown that 5-12% of people experience PTSD after each traumatic event (Ursano et al., 2009)
The dramatic COVID-19 outbreak and its rapid pandemic raised healthcare providers’ concerns in hospitals and clinics (Wang et al., 2020). However, this global event has affected people with chronic diseases and their families more than the ordinary population (Yuan et al., 2020), because evidence reveals that death from COVID-19 in people with underlying diseases has been higher than in the healthy population. Therefore, they are considered high-risk populations in this pandemic (Cheng et al., 2020). In addition, the occurrence and continuation of this pandemic can complicate the life of families of children with chronic diseases who have already experienced some degrees of anxiety and stress.
The factors that imposed many challenges on parents, especially mothers who are responsible for caring for their children during hospitalization are the rapid conversion of public healthcare centers to centers for patients with COVID-19, non-admission of people with chronic diseases in many healthcare centers, and fear of child contact with COVID-19-infected people or carriers. This persistent and intense fear can affect mothers’ daily function, care for their children, and ability to think and decide. Enduring stress and anxiety at a child’s admission affect the mother’s mental health and may lead to more unfavorable psychosocial conditions. The fear of the child becoming infected with COVID-19 disease during the hospital stay due to contact with healthcare workers, other patients, and visitors influence their decision to continue treatment and makes the child’s physical and mental condition more complex (Raphael et al., 2021; Yuan et al., 2020; Fong and Iarocci, 2020).
Mothers seem to experience high levels of anxiety and depression during their child’s hospitalization; however, there is insufficient evidence for the relationship between the experience of the hospital anxiety and depression with the fear of COVID-19 in mothers of children with a chronic disease. Conducting this study can increase the awareness of healthcare workers, especially nurses working in children’s hospitals, regarding the role of the anxiety and stress levels of the mothers of these children in the fear of the COVID-19 pandemic. It can also provide valuable fundamental knowledge for future pandemics and crises. Moreover, it answers whether fear of COVID-19 is associated with hospital anxiety and depression in these mothers. Thus, this study was conducted to determine the relationship between anxiety and depression, and fear of COVID-19 in mothers of children with chronic diseases hospitalized during the pandemic.
2. Materials and Methods
This was a descriptive correlational study that was conducted in 2021. The study sample was 194 mothers of children with chronic illness hospitalized in two educational-therapeutic hospitals (Rasoul Akram and Ali Asghar hospitals) affiliated with the Iran University of Medical Sciences (IUMS) in Tehran, Iran. The children were under treatment in the internal medicine, surgery, oncology, and urology wards of the mentioned hospitals (Equation 1).
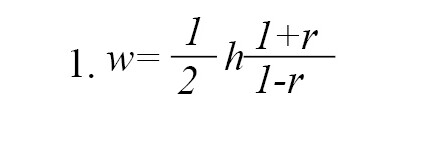
Considering the confidence level of 95% and the test power of 80% and assuming a correlation coefficient of 0.2 between mental status and fear of COVID-19 in mothers of children hospitalized with chronic diseases in the hospital, the desired sample size was estimated to be 194 people according to Equation 2:

Inclusion criteria for the mothers were being at least 18 years old, being literate, not having a mental illness based on the mother’s self-report, and not experiencing another stressful event in the last six months. In the case of children, it was necessary that six months had passed since the diagnosis of the disease and at least one week had passed since the child was hospitalized. Subjects were selected by convenience sampling method. To collect data, the researcher visited both hospitals every day (morning or afternoon) and invited eligible mothers to cooperate. Sampling continued until the required sample size was reached.
The questionnaire consisted of three parts. The first part included demographic information of the mothers (age, education, and occupation) and the child (age, gender, length of hospital stays, diagnosis, and the frequency of hospitalizations). In the second part, the researchers used the hospital anxiety and depression scale (HADS). This scale includes two subscales of anxiety and depression, each with seven items. To lessen the possible effects of physical illnesses, no items relating to symptoms that might stem from a somatic condition, such as dizziness and loss of appetite are included in the scale. There are two ways of interpreting the HADS scores; either by comparing an individual’s score to normative values obtained from a sample of the general population, or by using cut-off scores that indicate different levels of clinically relevant distress. Each question is scored on a 0-3 scale. The total score ranges from 0 to 21. Scores higher than eight in each section indicate borderline and abnormal anxiety/depression (Zigmond and Snaith, 1983). This scale has different classifications (Emons et al., 2019); Snaith and Zigmond identified three cut-off levels: Scores 0-7, 8-14, and 15-21 indicate normal, moderate, and severe anxiety/depression, respectively (Zigmond and Snaith, 1983). Kaviani et al. (2009) showed that the internal consistency of the total scale is 0.91 (α=0.70 in the depression subscale and 0.85 in the anxiety subscale) (Kaviani et al., 2009). In this study, Cronbach’s alpha coefficient was estimated at 0.87 for the anxiety subscale, 0.85 for the depression subscale, and 0.89 for the whole scale. The findings of a validation study indicate that the Iranian version of the HADS is a reliable and valid measure of anxiety and depression (Montazeri, et al., 2003.).
The Fear of COVID-19 Scale was developed by an Iranian researcher with seven items. It is scored on a 5-point Likert scale from strongly disagree=1 to strongly agree=5. The total score ranges from 7 to 35. The higher scores are indicative of greater fear of COVID-19 (Ahorsu et al., 2020). The psychometric properties of this scale has been measured on 717 Iranians. Its internal reliability was approved by α=0.82 and its test-retest reliability by ICC=0.72 Ahorsu et al., 2020). The Cronbach’s alpha coefficient of this scale was estimated at 0.85 in our study. The content validity of the scale was also confirmed by three doctoral nursing experts.
The subjects were asked to complete the scales based on their last week’s emotions. To prevent sample attrition and incomplete responses, they were asked to complete them immediately. The researcher was present in the ward to answer any ambiguities and checked the returned questionnaires to ensure complete answers. Health protocols were followed in the data collection process; therefore, the mothers had less stress concerning the transfer of COVID-19 and were more willing to participate. If the mother was bored or the child’s physical condition was poor, the researcher would delay completing the questionnaire. Because most of the diagnostic and treatment procedures and doctor visits take place in the morning, mothers were more willing to participate in the study in the evening (5-9 pm). Therefore, the researcher collected the data at that time.
Data were analyzed using descriptive statistics, and parametric inferential statistics (analysis of variance, independent t-test, Pearson correlation coefficient, and regression analysis) using SPSS software, version 22. The significance level was considered at 0.05.
3. Results
According to the findings, the age of 44.9% of mothers was 30-39 years and their average age was 34.45±6.93 years. It was also found that 39.8% of children aged 7-12 years, with girls (51.5%) outnumbering boys; 36.7% of the children had leukemia. Table 1 summarizes the demographic characteristics of the mothers and children.
.jpg)
Table 2 shows the mothers’ mental status and the level of their fear of COVID-19. According to this table, the hospital anxiety and depression of most of these mothers were at a borderline level. Also, their fear of COVID-19 was at a high level.
.jpg)
According to Table 3, there was a direct and positive correlation between hospital depression and hospital anxiety with the fear of COVID-19 in the mothers of children hospitalized with the chronic disease during the pandemic (P=0.001).
.jpg)
The results of the regression analysis of the correlation between these variables are shown in Table 4.
.jpg)
There was a significant correlation between the mother’s hospital anxiety with the child’s disease and the length of hospitalization. In addition, their hospital depression was significantly correlated with the child’s disease and length and frequency of hospitalization. Finally, the mother’s fear of COVID-19 had a significant correlation with the child’s age, disease, and length and frequency of hospitalization (Table 5).
.jpg)
4. Discussion
This study showed that mothers of children with chronic diseases suffer from borderline hospital anxiety and depression. Few studies have worked on this issue during the pandemic; however, their results are consistent with the results of this study; that is, they have reported considerable depression and anxiety in this group of mothers whether their child is hospitalized or not (Pınar Senkalfa et al., 2020; Durcan et al., 2021; Farajzadeh et al., 2021; Althiabi, 2021).
Studies have shown that during the COVID-19 pandemic, anxiety, and depression levels have increased in people from different communities for various reasons, including quarantine conditions, disruption of routine work, the need to strictly follow health protocols, constant shifts in government decisions about pandemic laws, distressing news from the media, high mortality rates, and difficult hospitalization and treatment (Özdin & Bayrak Özdin, 2020; Choi et al., 2020; Dozois, 2021; Ustun, 2021). The psychological condition of mothers of children with chronic diseases is no exception. They have already suffered from various psychological stressors and had degrees of depression and anxiety due to their children’s disease. The COVID-19 pandemic has doubled their challenges related to the deterioration of the illness or continuing the treatment and threatened their psychological status due to difficult situations (Pınar Senkalfa et al., 2020).
The prolonged pandemic of COVID-19 and its long-term psychological, economic, and social pressures can leave lasting negative effects on the mental state of this group of mothers (Farajzadeh et al., 2021; Althiabi, 2021). The lack of attention of healthcare providers to the mental state of these mothers and the failure to provide timely support by specialists can have a negative effect on the mother and the child. In other words, the mothers’ increased anxiety and depression reduce the children’s quality of care, nutrition, and treatment, anwwd result in irreversible adverse effects (Fong & Iarocci, 2020; Corsi et al., 2021; Araújo et al., 2021).
The study results were indicative of a fear of COVID-19 disease in the mothers. In a similar study conducted in China, it was found that parents of children admitted during the COVID-19 pandemic had considerable fear of COVID-19 (Yuan et al., 2020). Similarly, other studies have shown that the fear of COVID-19 is so great in all involved countries that it has led to the emergence of physical and psychosocial manifestations in many people (Pakpour & Griffiths, 2020; Harper et al., 2021).
According to the evidence, fear and anxiety have been the principal psychological consequences of the COVID-19 pandemic (Presti et al., 2020; Corsi et al., 2021). During the COVID-19 pandemic, most parents avoid hospitalizing their children, even in emergencies if possible, and prefer to continue treatment at home. The need for a child’s hospitalization during the COVID-19 pandemic seems to put parents, especially the mother, under pressure and makes them vulnerable to different psychosocial problems. On the other hand, the family’s strong tendency to avoid hospitalizing the child due to fear of COVID-19 can result in irreparable consequences for children with chronic conditions who require hospitalization (Fong & Iarocci, 2020; Corsi et al., 2021).
The present study showed a positive and significant relationship between hospital anxiety and depression with fear of COVID-19 in these mothers. This can make it difficult for mothers to make decisions about admitting the child and continuing the treatment (Yuan et al., 2020). Correspondingly, the results of other studies have shown that fear of COVID-19 is associated with hospital depression and anxiety in patients with chronic conditions, such as asthma, heart failure, and multiple sclerosis (de Boer et al., 2021; Alyami et al., 2020; Wieteska-Miłek et al., 2021; Ramezani et al., 2021).
Pre-pandemic evidence suggests that parents of children with chronic diseases experience high levels of depression and anxiety during childcare at home and in the hospital (Al Awaji et al., 2021; Pınar Senkalfa et al., 2020). The coronavirus pandemic has increased challenges, concerns, and tensions in society and has put further pressure on this group of families (Gassman-Pines et al., 2020). Confusion about the treatment and prevention of COVID-19, the physical and mental condition of a child with chronic disease, and the uncertainty about future situations have increasingly upset the balance in the family. On the other hand, the fear of COVID-19 and transmitting it to other family members when the child is hospitalized and the heavy financial burden of COVID-19 are issues that can increase depression and anxiety (Talevi et al., 2020). During the COVID-19 pandemic, parents of children with special diseases are more concerned about their children’s physical and mental health than parents of healthy children. In addition, they have other worries due to pandemic conditions, such as job loss, finding a person to take care of the child, and long-term isolation that exacerbates their anxiety and negatively affects their well-being (Lateef et al., 2021). In this situation, vulnerable families (i.e., those who have lived in stressful and complex conditions due to having a child with chronic disease and suffered from some degree of depression and anxiety before the COVID-19) will be more prone to psycho-emotional problems (Fong and Iarocci, 2020; Pınar Senkalfa et al., 2020; Yuan et al., 2020).
Meeting the needs of mothers who take care of such children is essential, as their well-being greatly affects their capacity to support and protect their children. Health managers should not ignore the special needs of these mothers during the pandemic. Loss of support resources during the pandemic may put their mental health in critical condition and increase their fear of children’s hospitalization. Researchers have advised healthcare providers, including nurses, to pay attention to the mothers’ needs during the COVID-19 pandemic and provide services using interprofessional approaches to maintain the mental health of these families, including mothers (Al Awaji et al., 2021; Durcan et al., 2021; Racine et al., 2020).
According to the results of this study, mothers’ hospital anxiety was associated with their children’s disease and the length of hospitalization. For example, mothers of children with leukemia experienced higher hospital anxiety, and it increased with the length of hospital stay. Likewise, other studies have shown that mothers’ hospital anxiety increases with hospital stay (Yuan et al., 2020; Toledano-Toledano & Moral de la Rubia, 2018). Similar to the findings of this study, other studies have shown that mothers of children with life-threatening diseases suffer from a high level of depression and this depression is related to the duration and frequency of hospitalization; as the child’s physical condition worsens, this depression increases. In the same way, families of children with cancer have more complicated living conditions and psychologically need more support from society during the pandemic (Embregts et al., 2021).
The results of the study showed a significant relationship between age, disease, and duration and frequency of hospitalization of the child and mothers’ fear of COVID-19. Similarly, other studies have shown that fear of COVID-19 is associated with the type of disease, length of hospital stay, and frequency of hospitalizations (Durcan et al., 2021). Evidence shows that fear of COVID-19 has been high in the pandemic, and factors, such as age, type of disease, and length and frequency of hospitalization are risk factors for the family, especially the caregiver because they are exposed to coronavirus (Fong & Iarocci, 2020). On the other hand, a child suffering from a life-threatening illness has a weakened immune system and is on immunosuppressive medications, which is a risk factor for these children to contract COVID-19. Meanwhile, the mother’s fear increases when the child is younger (Galeotti and Bayry, 2020).
Based on the study results, it is suggested that future studies investigate the fear of COVID-19 and the mental status of parents of children with chronic obstructive pulmonary disease, such as asthma or cystic fibrosis. Studying other aspects of mental health, well-being, and quality of life of mothers of chronically ill children in inpatient and outpatient settings would also be useful during the COVID-19 pandemic. According to the obtained knowledge, interventional studies investigating how to control the fear of COVID-19 and improve the mental status of mothers of these children during the pandemic are also suggested.
Among the limitations of this study, it can be mentioned that some mothers were not willing to answer the questionnaire due to their concern about the physical condition of their children, which could have influenced their answers. Another limitation was the COVID-19 pandemic and strict adherence to health protocols, which made it difficult to communicate with mothers.
5. Conclusion
The relationship between hospital anxiety and depression with the fear of COVID-19 highlights the need for sustained psychological and emotional support for mothers of children with chronic disease during the pandemic and child’s hospitalization. Establishing a center in the hospital with psychologists, counselors, and social workers to provide supportive services is essential.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Iran University of Medical Sciences (IUMS) (Code: IR.IUMS.REC.1399.805). Informed consent was obtained from all the mothers before completing the questionnaires.
Funding
This study was funded by Iran University of Medical Sciences (IUMS).
Authors' contributions
Conceptualization and methodology: Mahnaz Shoghi; Data collection: Parisa Karimzadeh; Writing--review & editing, and funding acquisition and resources: Mahnaz Shoghi, Parisa Karimzadeh, Raheleh Mohamadi; Data analysis and Writing--original draft: Mahnaz Shoghi, Parisa Karimzadeh, Raheleh Mohamadi; Approval of final manuscript: All the authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
This article is taken from the master’s thesis of the second author in the field of pediatric nursing. The researchers appreciate the financial support of Iran University of Medical Sciences (IUMS), all the mothers participating in the study, and the research centers of Hazrat Rasool Akram (PBUH) and Ali Asghar (PBUH) Hospitals for their cooperation in this study.
References
Ahorsu, D. K., et al., 2020. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, pp. 1-9. [DOI:10.1037/t78404-000]
Al Awaji, N., et al., 2021. Quality of life, needs and fears of mothers of children with disabilities in Saudi Arabia during the COVID-19 Lockdown. International Journal of Environmental Research and Public Health, 18, pp. 11442. [DOI:10.3390/ijerph182111442] [PMID] [PMCID]
Althiabi, Y., 2021. Attitude, anxiety and perceived mental health care needs among parents of children with Autism Spectrum Disorder (ASD) in Saudi Arabia during COVID-19 pandemic. Research in Developmental Disabilities, 111, pp. 103873. [DOI:10.1016/j.ridd.2021.103873] [PMID]
Alyami, M., et al., 2020. Effects of fear of COVID-19 on mental well-being and quality of life: A path analysis. Saudi Journal of Medicine & Medical Sciences, 9(1), pp. 24. [DOI:10.21203/rs.3.rs-59161/v1]
Araújo, L. A. D., et al., 2021. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. Jornal de Pediatria, 97, pp. 369-377. [DOI:10.1016/j.jped.2020.08.008] [PMID] [PMCID]
Burke, S. O., et al., 2016. Parents’ perceptions of chronic illness trajectories. The Canadian Journal of Nursing Research, 32(3), pp. 19–36. [PMID]
Cheng, Y., et al., 2020. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney International, 97(5), pp. 829–838. . [DOI:10.1101/2020.02.18.20023242]
Choi, E. P. H., Hui, B. P. H. & Wan, E. Y. F., 2020. Depression and anxiety in Hong Kong during COVID-19. International Journal of Environmental Research and Public Health, 17(10), pp. 3740. [DOI:10.3390/ijerph17103740] [PMID] [PMCID]
Corsi, M., et al., 2021. PTSD in parents of children with severe diseases: A systematic review to face Covid-19 impact. Italian Journal of Pediatrics, 47(1), pp. 8. [DOI:10.1186/s13052-021-00957-1] [PMID] [PMCID]
De Boer, G. M., et al., 2021. Asthma patients experience increased symptoms of anxiety, depression and fear during the COVID-19 pandemic. Chronic Respiratory Disease, 18, pp. 14799731211029658. [DOI:10.1177/14799731211029658] [PMID] [PMCID]
Dozois, D. J. A. & Mental Health Research Canada., 2021. Anxiety and depression in Canada during the COVID-19 pandemic: A national survey. Canadian Psychology/Psychologie Canadienne, 62(1), pp. 136-42. [DOI:10.1037/cap0000251]
Durcan, G., et al., 2021. Psychosocial and clinical effects of the COVID-19 pandemic in patients with childhood rheumatic diseases and their parents. Rheumatology International, 41(3), pp. 575-83. [DOI:10.1007/s00296-021-04790-x] [PMID] [PMCID]
Embregts, P., et al., 2021. Experiences of mothers caring for a child with an intellectual disability during the COVID‐19 pandemic in the Netherlands. Journal of Intellectual Disability Research, 65(8), pp. 760–71. [DOI:10.1111/jir.12859] [PMID] [PMCID]
Emons, W. H., Habibović, M. & Pedersen, S. S., 2019. Prevalence of anxiety in patients with an implantable cardioverter defibrillator: Measurement equivalence of the HADS-A and the STAI-S. Quality of Life Research, 28(11), pp. 3107-16. [DOI:10.1007/s11136-019-02237-2] [PMID] [PMCID]
Farajzadeh, A., et al., 2021. Predictors of mental health among parents of children with cerebral palsy during the COVID-19 pandemic in Iran: A web-based cross-sectional study. Research in Developmental Disabilities, 112, pp. 103890. [DOI:10.1016/j.ridd.2021.103890] [PMID]
C Fong, V. & Iarocci, G., 2020. Child and family outcomes following pandemics: A systematic review and recommendations on COVID-19 policies. Journal of Pediatric Psychology, 45(10), pp. 1124-43. [DOI:10.1093/jpepsy/jsaa092] [PMID] [PMCID]
Galeotti, C. & Bayry, J., 2020. Autoimmune and inflammatory diseases following COVID-19. Nature Reviews Rheumatology, 16(8), pp. 413-4. [DOI:10.1038/s41584-020-0448-7] [PMID] [PMCID]
Gassman-Pines, A., Ananat, E. O. & Fitz-Henley, J., 2020. COVID-19 and parent-child psychological well-being. Pediatrics, 146(4), pp. e2020007294. [PMID] [PMCID]
Harper, C. A., et al., 2021. Functional fear predicts public health compliance in the COVID-19 pandemic. International Journal of Mental Health and Addiction, 19(5), pp. 1875-88. [DOI:10.1007/s11469-020-00281-5] [PMID] [PMCID]
Iranmanesh, S., Shamsi, A. & Dehghan, M., 2015. Post-traumatic stress symptoms among Iranian parents of children during cancer treatment. Issues in Mental Health Nursing, 36(4), pp. 279–285. [PMID]
Kaviani, H., Seyfourian, H., Sharifi, V. & Ebrahimkhani, N., 2009. Reliability and validity of Anxiety and Depression Hospital Scales (HADS): Iranian patients with anxiety and depression disorders. Tehran University Medical Journal, 67(5), pp. 379-85. [Link]
Lateef, R., Alaggia, R. & Collin-Vézina, D., 2021. A scoping review on psychosocial consequences of pandemics on parents and children: Planning for today and the future. Children and Youth Services Review, 125, pp. 106002. [DOI:10.1016/j.childyouth.2021.106002] [PMID] [PMCID]
Masa'Deh, R., Collier, J. & Hall, C., 2012. Parental stress when caring for a child with cancer in Jordan: A cross-sectional survey. Health and Quality of Life Outcomes, 10, pp. 88. [DOI:10.1186/1477-7525-10-88] [PMID] [PMCID]
Montazeri, A., et al., 2003. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health and Quality of Life Outcomes, 1, pp. 14. [DOI:10.1186/1477-7525-1-14] [PMID] [PMCID]
Nabors, L., 2020. Chronic illness and anxiety in children. In: L. Nabors (ed), Anxiety management in children with mental and physical health problems. Berlin: Springer. [DOI:10.1007/978-3-030-35606-4]
Nabors, L., et al., 2018. Family coping during hospitalization of children with chronic illnesses. Journal of Child and Family Studies, 27, pp. 1482-91. [DOI:10.1007/s10826-017-0986-z]
Özdin, S. & Bayrak Özdin, Ş., 2020. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. The International Journal of Social Psychiatry, 66(5), pp. 504-11. [DOI:10.1177/0020764020927051] [PMID] [PMCID]
Pakpour, A. & Griffiths, M. D., 2020. The fear of COVID-19 and its role in preventive behaviors. Journal of Concurrent Disorders, 2(1), pp. 58-63. [DOI:10.54127/WCIC8036]
Pınar Senkalfa, B., et al., 2020. Effect of the COVID‐19 pandemic on anxiety among children with cystic fibrosis and their mothers. Pediatric Pulmonology, 55(8), pp. 2128-34. [DOI:10.1002/ppul.24900] [PMID] [PMCID]
Presti, G., et al., 2020. The dynamics of fear at the time of covid-19: a contextual behavioral science perspective. Clinical Neuropsychiatry, 17(2), pp. 65–71. [PMID]
Racine, N., Birken, C. & Madigan, S., 2020. Supporting the mental health of parents and children during and after coronovirus. Journal of Developmental & Behavioral Pediatrics, 41(7), pp. 508-10. [PMID]
Ramezani, N., et al., 2021. Fear and anxiety in patients with multiple sclerosis during COVID-19 pandemic; report of an Iranian population. Multiple Sclerosis and Related Disorders, 50, pp. 102798. [DOI:10.1016/j.msard.2021.102798] [PMID] [PMCID]
Raphael, J. L., Kessel, W. & Patel, M., 2021. Unintended consequences of restrictive visitation policies during the COVID-19 pandemic: Implications for hospitalized children. Pediatric Research, 89(6), pp. 1333–5. [DOI:10.1038/s41390-021-01439-0] [PMID] [PMCID]
Stremler, R., et al., 2017. Psychological outcomes in parents of critically ill hospitalized children. Journal of Pediatric Nursing, 34, pp. 36-43. [PMID]
Talevi, D., et al., 2020. Mental health outcomes of the COVID-19 pandemic. Rivista di Psichiatria, 55(3), pp. 137-44. [PMID]
Isabel Tan, X. W., et al., 2021. Psychological distress in parents of children with cancer: A descriptive correlational study. Asia-Pacific Journal of Oncology Nursing, 8(1), pp. 94-102. [PMID] [PMCID]
Toledano-Toledano, F. & Moral de la Rubia, J., 2018. Factors associated with anxiety in family caregivers of children with chronic diseases. BioPsychoSocial Medicine, 12, pp. 20. [DOI:10.1186/s13030-018-0139-7] [PMID] [PMCID]
Ursano, R. J., et al., 2009. PTSD and traumatic stress: From gene to community and bench to bedside. Brain Research, 1293, pp. 2-12. [DOI:10.1016/j.brainres.2009.03.030] [PMID]
Ustun, G., 2021. Determining depression and related factors in a society affected by COVID-19 pandemic. The International Journal of Social Psychiatry, 67(1), pp. 54-63. [PMID] [PMCID]
Wang, C., et al., 2020. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), pp. 1729. [DOI:10.3390/ijerph17051729] [PMID] [PMCID]
Wieteska-Miłek, M., et al., 2021. Fear of COVID-19, anxiety and depression in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension during the pandemic. Journal of Clinical Medicine, 10(18), pp. 4195. [PMID] [PMCID]
YuYuanan, R., et al., 2020. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Research, 288, pp. 112953. [PMID] [PMCID]
Zigmond, A. S. & Snaith, R. P., 1983. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), pp. 361-70. [DOI:10.1111/j.1600-0447.1983.tb09716.x] [PMID]
Frequent hospitalization of a child with a chronic disease is one of the challenging life stressors for parents and family (Stremler et al., 2017). Evidence shows that the parents of these children suffer from post-traumatic stress disorder (TSD) and experience higher stress compared to other parents of hospitalized children during their stay in the hospital (Nabors et al., 2018; Iranmanesh et al., 2015). Fear and anxiety are common in the parents of hospitalized children with chronic and life-threatening disorders and it mostly occurs at the time of disease diagnosis and adverse changes in the treatment process (Masa’Deh et al., 2012). Moreover, depression is a significant issue for these parents. Persistent parental depression and anxiety can interfere with subsequent decisions, affect the treatment process, and disrupt the child-parent relationship. Researchers have reported psychological reactions, such as anxiety, depression, denial, anger, sleep disorders, and loss of confidence in caregivers of children with chronic disease. As the most substantial people in the child support system, parents, especially mothers, experience high levels of stress and anxiety and transfer it to the child (Tan et al., 2021).
Tolerating anxiety and stress for a long time will have many negative consequences for the child and the family (Nabors, 2020). Issues that put parents, especially mothers as primary caregivers under psychosocial tension include role strain, financial pressures, lifestyle changes, following complicated and lengthy treatments, changes in family planning, the physical and psychological condition of the child, and uncertainty of the disease consequences (Burke et al., 2016).
The treatment of children with chronic diseases usually follows a specific schedule. The parents know in advance when to go to the hospital, except at the beginning of the diagnosis, some exceptions, and emergency conditions; therefore, they can plan and be prepared for hospitalization. However, any change in the child’s treatment and care program will surge the parents’ stress. On the other hand, the stress due to natural disasters and pandemics, such as COVID-19 affects all aspects of family life. It can be overwhelming for caregivers of children with chronic diseases. Studies have shown that 5-12% of people experience PTSD after each traumatic event (Ursano et al., 2009)
The dramatic COVID-19 outbreak and its rapid pandemic raised healthcare providers’ concerns in hospitals and clinics (Wang et al., 2020). However, this global event has affected people with chronic diseases and their families more than the ordinary population (Yuan et al., 2020), because evidence reveals that death from COVID-19 in people with underlying diseases has been higher than in the healthy population. Therefore, they are considered high-risk populations in this pandemic (Cheng et al., 2020). In addition, the occurrence and continuation of this pandemic can complicate the life of families of children with chronic diseases who have already experienced some degrees of anxiety and stress.
The factors that imposed many challenges on parents, especially mothers who are responsible for caring for their children during hospitalization are the rapid conversion of public healthcare centers to centers for patients with COVID-19, non-admission of people with chronic diseases in many healthcare centers, and fear of child contact with COVID-19-infected people or carriers. This persistent and intense fear can affect mothers’ daily function, care for their children, and ability to think and decide. Enduring stress and anxiety at a child’s admission affect the mother’s mental health and may lead to more unfavorable psychosocial conditions. The fear of the child becoming infected with COVID-19 disease during the hospital stay due to contact with healthcare workers, other patients, and visitors influence their decision to continue treatment and makes the child’s physical and mental condition more complex (Raphael et al., 2021; Yuan et al., 2020; Fong and Iarocci, 2020).
Mothers seem to experience high levels of anxiety and depression during their child’s hospitalization; however, there is insufficient evidence for the relationship between the experience of the hospital anxiety and depression with the fear of COVID-19 in mothers of children with a chronic disease. Conducting this study can increase the awareness of healthcare workers, especially nurses working in children’s hospitals, regarding the role of the anxiety and stress levels of the mothers of these children in the fear of the COVID-19 pandemic. It can also provide valuable fundamental knowledge for future pandemics and crises. Moreover, it answers whether fear of COVID-19 is associated with hospital anxiety and depression in these mothers. Thus, this study was conducted to determine the relationship between anxiety and depression, and fear of COVID-19 in mothers of children with chronic diseases hospitalized during the pandemic.
2. Materials and Methods
This was a descriptive correlational study that was conducted in 2021. The study sample was 194 mothers of children with chronic illness hospitalized in two educational-therapeutic hospitals (Rasoul Akram and Ali Asghar hospitals) affiliated with the Iran University of Medical Sciences (IUMS) in Tehran, Iran. The children were under treatment in the internal medicine, surgery, oncology, and urology wards of the mentioned hospitals (Equation 1).
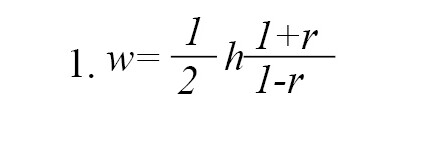
Considering the confidence level of 95% and the test power of 80% and assuming a correlation coefficient of 0.2 between mental status and fear of COVID-19 in mothers of children hospitalized with chronic diseases in the hospital, the desired sample size was estimated to be 194 people according to Equation 2:

Inclusion criteria for the mothers were being at least 18 years old, being literate, not having a mental illness based on the mother’s self-report, and not experiencing another stressful event in the last six months. In the case of children, it was necessary that six months had passed since the diagnosis of the disease and at least one week had passed since the child was hospitalized. Subjects were selected by convenience sampling method. To collect data, the researcher visited both hospitals every day (morning or afternoon) and invited eligible mothers to cooperate. Sampling continued until the required sample size was reached.
The questionnaire consisted of three parts. The first part included demographic information of the mothers (age, education, and occupation) and the child (age, gender, length of hospital stays, diagnosis, and the frequency of hospitalizations). In the second part, the researchers used the hospital anxiety and depression scale (HADS). This scale includes two subscales of anxiety and depression, each with seven items. To lessen the possible effects of physical illnesses, no items relating to symptoms that might stem from a somatic condition, such as dizziness and loss of appetite are included in the scale. There are two ways of interpreting the HADS scores; either by comparing an individual’s score to normative values obtained from a sample of the general population, or by using cut-off scores that indicate different levels of clinically relevant distress. Each question is scored on a 0-3 scale. The total score ranges from 0 to 21. Scores higher than eight in each section indicate borderline and abnormal anxiety/depression (Zigmond and Snaith, 1983). This scale has different classifications (Emons et al., 2019); Snaith and Zigmond identified three cut-off levels: Scores 0-7, 8-14, and 15-21 indicate normal, moderate, and severe anxiety/depression, respectively (Zigmond and Snaith, 1983). Kaviani et al. (2009) showed that the internal consistency of the total scale is 0.91 (α=0.70 in the depression subscale and 0.85 in the anxiety subscale) (Kaviani et al., 2009). In this study, Cronbach’s alpha coefficient was estimated at 0.87 for the anxiety subscale, 0.85 for the depression subscale, and 0.89 for the whole scale. The findings of a validation study indicate that the Iranian version of the HADS is a reliable and valid measure of anxiety and depression (Montazeri, et al., 2003.).
The Fear of COVID-19 Scale was developed by an Iranian researcher with seven items. It is scored on a 5-point Likert scale from strongly disagree=1 to strongly agree=5. The total score ranges from 7 to 35. The higher scores are indicative of greater fear of COVID-19 (Ahorsu et al., 2020). The psychometric properties of this scale has been measured on 717 Iranians. Its internal reliability was approved by α=0.82 and its test-retest reliability by ICC=0.72 Ahorsu et al., 2020). The Cronbach’s alpha coefficient of this scale was estimated at 0.85 in our study. The content validity of the scale was also confirmed by three doctoral nursing experts.
The subjects were asked to complete the scales based on their last week’s emotions. To prevent sample attrition and incomplete responses, they were asked to complete them immediately. The researcher was present in the ward to answer any ambiguities and checked the returned questionnaires to ensure complete answers. Health protocols were followed in the data collection process; therefore, the mothers had less stress concerning the transfer of COVID-19 and were more willing to participate. If the mother was bored or the child’s physical condition was poor, the researcher would delay completing the questionnaire. Because most of the diagnostic and treatment procedures and doctor visits take place in the morning, mothers were more willing to participate in the study in the evening (5-9 pm). Therefore, the researcher collected the data at that time.
Data were analyzed using descriptive statistics, and parametric inferential statistics (analysis of variance, independent t-test, Pearson correlation coefficient, and regression analysis) using SPSS software, version 22. The significance level was considered at 0.05.
3. Results
According to the findings, the age of 44.9% of mothers was 30-39 years and their average age was 34.45±6.93 years. It was also found that 39.8% of children aged 7-12 years, with girls (51.5%) outnumbering boys; 36.7% of the children had leukemia. Table 1 summarizes the demographic characteristics of the mothers and children.
.jpg)
Table 2 shows the mothers’ mental status and the level of their fear of COVID-19. According to this table, the hospital anxiety and depression of most of these mothers were at a borderline level. Also, their fear of COVID-19 was at a high level.
.jpg)
According to Table 3, there was a direct and positive correlation between hospital depression and hospital anxiety with the fear of COVID-19 in the mothers of children hospitalized with the chronic disease during the pandemic (P=0.001).
.jpg)
The results of the regression analysis of the correlation between these variables are shown in Table 4.
.jpg)
There was a significant correlation between the mother’s hospital anxiety with the child’s disease and the length of hospitalization. In addition, their hospital depression was significantly correlated with the child’s disease and length and frequency of hospitalization. Finally, the mother’s fear of COVID-19 had a significant correlation with the child’s age, disease, and length and frequency of hospitalization (Table 5).
.jpg)
4. Discussion
This study showed that mothers of children with chronic diseases suffer from borderline hospital anxiety and depression. Few studies have worked on this issue during the pandemic; however, their results are consistent with the results of this study; that is, they have reported considerable depression and anxiety in this group of mothers whether their child is hospitalized or not (Pınar Senkalfa et al., 2020; Durcan et al., 2021; Farajzadeh et al., 2021; Althiabi, 2021).
Studies have shown that during the COVID-19 pandemic, anxiety, and depression levels have increased in people from different communities for various reasons, including quarantine conditions, disruption of routine work, the need to strictly follow health protocols, constant shifts in government decisions about pandemic laws, distressing news from the media, high mortality rates, and difficult hospitalization and treatment (Özdin & Bayrak Özdin, 2020; Choi et al., 2020; Dozois, 2021; Ustun, 2021). The psychological condition of mothers of children with chronic diseases is no exception. They have already suffered from various psychological stressors and had degrees of depression and anxiety due to their children’s disease. The COVID-19 pandemic has doubled their challenges related to the deterioration of the illness or continuing the treatment and threatened their psychological status due to difficult situations (Pınar Senkalfa et al., 2020).
The prolonged pandemic of COVID-19 and its long-term psychological, economic, and social pressures can leave lasting negative effects on the mental state of this group of mothers (Farajzadeh et al., 2021; Althiabi, 2021). The lack of attention of healthcare providers to the mental state of these mothers and the failure to provide timely support by specialists can have a negative effect on the mother and the child. In other words, the mothers’ increased anxiety and depression reduce the children’s quality of care, nutrition, and treatment, anwwd result in irreversible adverse effects (Fong & Iarocci, 2020; Corsi et al., 2021; Araújo et al., 2021).
The study results were indicative of a fear of COVID-19 disease in the mothers. In a similar study conducted in China, it was found that parents of children admitted during the COVID-19 pandemic had considerable fear of COVID-19 (Yuan et al., 2020). Similarly, other studies have shown that the fear of COVID-19 is so great in all involved countries that it has led to the emergence of physical and psychosocial manifestations in many people (Pakpour & Griffiths, 2020; Harper et al., 2021).
According to the evidence, fear and anxiety have been the principal psychological consequences of the COVID-19 pandemic (Presti et al., 2020; Corsi et al., 2021). During the COVID-19 pandemic, most parents avoid hospitalizing their children, even in emergencies if possible, and prefer to continue treatment at home. The need for a child’s hospitalization during the COVID-19 pandemic seems to put parents, especially the mother, under pressure and makes them vulnerable to different psychosocial problems. On the other hand, the family’s strong tendency to avoid hospitalizing the child due to fear of COVID-19 can result in irreparable consequences for children with chronic conditions who require hospitalization (Fong & Iarocci, 2020; Corsi et al., 2021).
The present study showed a positive and significant relationship between hospital anxiety and depression with fear of COVID-19 in these mothers. This can make it difficult for mothers to make decisions about admitting the child and continuing the treatment (Yuan et al., 2020). Correspondingly, the results of other studies have shown that fear of COVID-19 is associated with hospital depression and anxiety in patients with chronic conditions, such as asthma, heart failure, and multiple sclerosis (de Boer et al., 2021; Alyami et al., 2020; Wieteska-Miłek et al., 2021; Ramezani et al., 2021).
Pre-pandemic evidence suggests that parents of children with chronic diseases experience high levels of depression and anxiety during childcare at home and in the hospital (Al Awaji et al., 2021; Pınar Senkalfa et al., 2020). The coronavirus pandemic has increased challenges, concerns, and tensions in society and has put further pressure on this group of families (Gassman-Pines et al., 2020). Confusion about the treatment and prevention of COVID-19, the physical and mental condition of a child with chronic disease, and the uncertainty about future situations have increasingly upset the balance in the family. On the other hand, the fear of COVID-19 and transmitting it to other family members when the child is hospitalized and the heavy financial burden of COVID-19 are issues that can increase depression and anxiety (Talevi et al., 2020). During the COVID-19 pandemic, parents of children with special diseases are more concerned about their children’s physical and mental health than parents of healthy children. In addition, they have other worries due to pandemic conditions, such as job loss, finding a person to take care of the child, and long-term isolation that exacerbates their anxiety and negatively affects their well-being (Lateef et al., 2021). In this situation, vulnerable families (i.e., those who have lived in stressful and complex conditions due to having a child with chronic disease and suffered from some degree of depression and anxiety before the COVID-19) will be more prone to psycho-emotional problems (Fong and Iarocci, 2020; Pınar Senkalfa et al., 2020; Yuan et al., 2020).
Meeting the needs of mothers who take care of such children is essential, as their well-being greatly affects their capacity to support and protect their children. Health managers should not ignore the special needs of these mothers during the pandemic. Loss of support resources during the pandemic may put their mental health in critical condition and increase their fear of children’s hospitalization. Researchers have advised healthcare providers, including nurses, to pay attention to the mothers’ needs during the COVID-19 pandemic and provide services using interprofessional approaches to maintain the mental health of these families, including mothers (Al Awaji et al., 2021; Durcan et al., 2021; Racine et al., 2020).
According to the results of this study, mothers’ hospital anxiety was associated with their children’s disease and the length of hospitalization. For example, mothers of children with leukemia experienced higher hospital anxiety, and it increased with the length of hospital stay. Likewise, other studies have shown that mothers’ hospital anxiety increases with hospital stay (Yuan et al., 2020; Toledano-Toledano & Moral de la Rubia, 2018). Similar to the findings of this study, other studies have shown that mothers of children with life-threatening diseases suffer from a high level of depression and this depression is related to the duration and frequency of hospitalization; as the child’s physical condition worsens, this depression increases. In the same way, families of children with cancer have more complicated living conditions and psychologically need more support from society during the pandemic (Embregts et al., 2021).
The results of the study showed a significant relationship between age, disease, and duration and frequency of hospitalization of the child and mothers’ fear of COVID-19. Similarly, other studies have shown that fear of COVID-19 is associated with the type of disease, length of hospital stay, and frequency of hospitalizations (Durcan et al., 2021). Evidence shows that fear of COVID-19 has been high in the pandemic, and factors, such as age, type of disease, and length and frequency of hospitalization are risk factors for the family, especially the caregiver because they are exposed to coronavirus (Fong & Iarocci, 2020). On the other hand, a child suffering from a life-threatening illness has a weakened immune system and is on immunosuppressive medications, which is a risk factor for these children to contract COVID-19. Meanwhile, the mother’s fear increases when the child is younger (Galeotti and Bayry, 2020).
Based on the study results, it is suggested that future studies investigate the fear of COVID-19 and the mental status of parents of children with chronic obstructive pulmonary disease, such as asthma or cystic fibrosis. Studying other aspects of mental health, well-being, and quality of life of mothers of chronically ill children in inpatient and outpatient settings would also be useful during the COVID-19 pandemic. According to the obtained knowledge, interventional studies investigating how to control the fear of COVID-19 and improve the mental status of mothers of these children during the pandemic are also suggested.
Among the limitations of this study, it can be mentioned that some mothers were not willing to answer the questionnaire due to their concern about the physical condition of their children, which could have influenced their answers. Another limitation was the COVID-19 pandemic and strict adherence to health protocols, which made it difficult to communicate with mothers.
5. Conclusion
The relationship between hospital anxiety and depression with the fear of COVID-19 highlights the need for sustained psychological and emotional support for mothers of children with chronic disease during the pandemic and child’s hospitalization. Establishing a center in the hospital with psychologists, counselors, and social workers to provide supportive services is essential.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Iran University of Medical Sciences (IUMS) (Code: IR.IUMS.REC.1399.805). Informed consent was obtained from all the mothers before completing the questionnaires.
Funding
This study was funded by Iran University of Medical Sciences (IUMS).
Authors' contributions
Conceptualization and methodology: Mahnaz Shoghi; Data collection: Parisa Karimzadeh; Writing--review & editing, and funding acquisition and resources: Mahnaz Shoghi, Parisa Karimzadeh, Raheleh Mohamadi; Data analysis and Writing--original draft: Mahnaz Shoghi, Parisa Karimzadeh, Raheleh Mohamadi; Approval of final manuscript: All the authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
This article is taken from the master’s thesis of the second author in the field of pediatric nursing. The researchers appreciate the financial support of Iran University of Medical Sciences (IUMS), all the mothers participating in the study, and the research centers of Hazrat Rasool Akram (PBUH) and Ali Asghar (PBUH) Hospitals for their cooperation in this study.
References
Ahorsu, D. K., et al., 2020. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, pp. 1-9. [DOI:10.1037/t78404-000]
Al Awaji, N., et al., 2021. Quality of life, needs and fears of mothers of children with disabilities in Saudi Arabia during the COVID-19 Lockdown. International Journal of Environmental Research and Public Health, 18, pp. 11442. [DOI:10.3390/ijerph182111442] [PMID] [PMCID]
Althiabi, Y., 2021. Attitude, anxiety and perceived mental health care needs among parents of children with Autism Spectrum Disorder (ASD) in Saudi Arabia during COVID-19 pandemic. Research in Developmental Disabilities, 111, pp. 103873. [DOI:10.1016/j.ridd.2021.103873] [PMID]
Alyami, M., et al., 2020. Effects of fear of COVID-19 on mental well-being and quality of life: A path analysis. Saudi Journal of Medicine & Medical Sciences, 9(1), pp. 24. [DOI:10.21203/rs.3.rs-59161/v1]
Araújo, L. A. D., et al., 2021. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. Jornal de Pediatria, 97, pp. 369-377. [DOI:10.1016/j.jped.2020.08.008] [PMID] [PMCID]
Burke, S. O., et al., 2016. Parents’ perceptions of chronic illness trajectories. The Canadian Journal of Nursing Research, 32(3), pp. 19–36. [PMID]
Cheng, Y., et al., 2020. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney International, 97(5), pp. 829–838. . [DOI:10.1101/2020.02.18.20023242]
Choi, E. P. H., Hui, B. P. H. & Wan, E. Y. F., 2020. Depression and anxiety in Hong Kong during COVID-19. International Journal of Environmental Research and Public Health, 17(10), pp. 3740. [DOI:10.3390/ijerph17103740] [PMID] [PMCID]
Corsi, M., et al., 2021. PTSD in parents of children with severe diseases: A systematic review to face Covid-19 impact. Italian Journal of Pediatrics, 47(1), pp. 8. [DOI:10.1186/s13052-021-00957-1] [PMID] [PMCID]
De Boer, G. M., et al., 2021. Asthma patients experience increased symptoms of anxiety, depression and fear during the COVID-19 pandemic. Chronic Respiratory Disease, 18, pp. 14799731211029658. [DOI:10.1177/14799731211029658] [PMID] [PMCID]
Dozois, D. J. A. & Mental Health Research Canada., 2021. Anxiety and depression in Canada during the COVID-19 pandemic: A national survey. Canadian Psychology/Psychologie Canadienne, 62(1), pp. 136-42. [DOI:10.1037/cap0000251]
Durcan, G., et al., 2021. Psychosocial and clinical effects of the COVID-19 pandemic in patients with childhood rheumatic diseases and their parents. Rheumatology International, 41(3), pp. 575-83. [DOI:10.1007/s00296-021-04790-x] [PMID] [PMCID]
Embregts, P., et al., 2021. Experiences of mothers caring for a child with an intellectual disability during the COVID‐19 pandemic in the Netherlands. Journal of Intellectual Disability Research, 65(8), pp. 760–71. [DOI:10.1111/jir.12859] [PMID] [PMCID]
Emons, W. H., Habibović, M. & Pedersen, S. S., 2019. Prevalence of anxiety in patients with an implantable cardioverter defibrillator: Measurement equivalence of the HADS-A and the STAI-S. Quality of Life Research, 28(11), pp. 3107-16. [DOI:10.1007/s11136-019-02237-2] [PMID] [PMCID]
Farajzadeh, A., et al., 2021. Predictors of mental health among parents of children with cerebral palsy during the COVID-19 pandemic in Iran: A web-based cross-sectional study. Research in Developmental Disabilities, 112, pp. 103890. [DOI:10.1016/j.ridd.2021.103890] [PMID]
C Fong, V. & Iarocci, G., 2020. Child and family outcomes following pandemics: A systematic review and recommendations on COVID-19 policies. Journal of Pediatric Psychology, 45(10), pp. 1124-43. [DOI:10.1093/jpepsy/jsaa092] [PMID] [PMCID]
Galeotti, C. & Bayry, J., 2020. Autoimmune and inflammatory diseases following COVID-19. Nature Reviews Rheumatology, 16(8), pp. 413-4. [DOI:10.1038/s41584-020-0448-7] [PMID] [PMCID]
Gassman-Pines, A., Ananat, E. O. & Fitz-Henley, J., 2020. COVID-19 and parent-child psychological well-being. Pediatrics, 146(4), pp. e2020007294. [PMID] [PMCID]
Harper, C. A., et al., 2021. Functional fear predicts public health compliance in the COVID-19 pandemic. International Journal of Mental Health and Addiction, 19(5), pp. 1875-88. [DOI:10.1007/s11469-020-00281-5] [PMID] [PMCID]
Iranmanesh, S., Shamsi, A. & Dehghan, M., 2015. Post-traumatic stress symptoms among Iranian parents of children during cancer treatment. Issues in Mental Health Nursing, 36(4), pp. 279–285. [PMID]
Kaviani, H., Seyfourian, H., Sharifi, V. & Ebrahimkhani, N., 2009. Reliability and validity of Anxiety and Depression Hospital Scales (HADS): Iranian patients with anxiety and depression disorders. Tehran University Medical Journal, 67(5), pp. 379-85. [Link]
Lateef, R., Alaggia, R. & Collin-Vézina, D., 2021. A scoping review on psychosocial consequences of pandemics on parents and children: Planning for today and the future. Children and Youth Services Review, 125, pp. 106002. [DOI:10.1016/j.childyouth.2021.106002] [PMID] [PMCID]
Masa'Deh, R., Collier, J. & Hall, C., 2012. Parental stress when caring for a child with cancer in Jordan: A cross-sectional survey. Health and Quality of Life Outcomes, 10, pp. 88. [DOI:10.1186/1477-7525-10-88] [PMID] [PMCID]
Montazeri, A., et al., 2003. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health and Quality of Life Outcomes, 1, pp. 14. [DOI:10.1186/1477-7525-1-14] [PMID] [PMCID]
Nabors, L., 2020. Chronic illness and anxiety in children. In: L. Nabors (ed), Anxiety management in children with mental and physical health problems. Berlin: Springer. [DOI:10.1007/978-3-030-35606-4]
Nabors, L., et al., 2018. Family coping during hospitalization of children with chronic illnesses. Journal of Child and Family Studies, 27, pp. 1482-91. [DOI:10.1007/s10826-017-0986-z]
Özdin, S. & Bayrak Özdin, Ş., 2020. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. The International Journal of Social Psychiatry, 66(5), pp. 504-11. [DOI:10.1177/0020764020927051] [PMID] [PMCID]
Pakpour, A. & Griffiths, M. D., 2020. The fear of COVID-19 and its role in preventive behaviors. Journal of Concurrent Disorders, 2(1), pp. 58-63. [DOI:10.54127/WCIC8036]
Pınar Senkalfa, B., et al., 2020. Effect of the COVID‐19 pandemic on anxiety among children with cystic fibrosis and their mothers. Pediatric Pulmonology, 55(8), pp. 2128-34. [DOI:10.1002/ppul.24900] [PMID] [PMCID]
Presti, G., et al., 2020. The dynamics of fear at the time of covid-19: a contextual behavioral science perspective. Clinical Neuropsychiatry, 17(2), pp. 65–71. [PMID]
Racine, N., Birken, C. & Madigan, S., 2020. Supporting the mental health of parents and children during and after coronovirus. Journal of Developmental & Behavioral Pediatrics, 41(7), pp. 508-10. [PMID]
Ramezani, N., et al., 2021. Fear and anxiety in patients with multiple sclerosis during COVID-19 pandemic; report of an Iranian population. Multiple Sclerosis and Related Disorders, 50, pp. 102798. [DOI:10.1016/j.msard.2021.102798] [PMID] [PMCID]
Raphael, J. L., Kessel, W. & Patel, M., 2021. Unintended consequences of restrictive visitation policies during the COVID-19 pandemic: Implications for hospitalized children. Pediatric Research, 89(6), pp. 1333–5. [DOI:10.1038/s41390-021-01439-0] [PMID] [PMCID]
Stremler, R., et al., 2017. Psychological outcomes in parents of critically ill hospitalized children. Journal of Pediatric Nursing, 34, pp. 36-43. [PMID]
Talevi, D., et al., 2020. Mental health outcomes of the COVID-19 pandemic. Rivista di Psichiatria, 55(3), pp. 137-44. [PMID]
Isabel Tan, X. W., et al., 2021. Psychological distress in parents of children with cancer: A descriptive correlational study. Asia-Pacific Journal of Oncology Nursing, 8(1), pp. 94-102. [PMID] [PMCID]
Toledano-Toledano, F. & Moral de la Rubia, J., 2018. Factors associated with anxiety in family caregivers of children with chronic diseases. BioPsychoSocial Medicine, 12, pp. 20. [DOI:10.1186/s13030-018-0139-7] [PMID] [PMCID]
Ursano, R. J., et al., 2009. PTSD and traumatic stress: From gene to community and bench to bedside. Brain Research, 1293, pp. 2-12. [DOI:10.1016/j.brainres.2009.03.030] [PMID]
Ustun, G., 2021. Determining depression and related factors in a society affected by COVID-19 pandemic. The International Journal of Social Psychiatry, 67(1), pp. 54-63. [PMID] [PMCID]
Wang, C., et al., 2020. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), pp. 1729. [DOI:10.3390/ijerph17051729] [PMID] [PMCID]
Wieteska-Miłek, M., et al., 2021. Fear of COVID-19, anxiety and depression in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension during the pandemic. Journal of Clinical Medicine, 10(18), pp. 4195. [PMID] [PMCID]
YuYuanan, R., et al., 2020. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Research, 288, pp. 112953. [PMID] [PMCID]
Zigmond, A. S. & Snaith, R. P., 1983. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), pp. 361-70. [DOI:10.1111/j.1600-0447.1983.tb09716.x] [PMID]
Type of Study: Research |
Subject:
General
Received: 2022/07/23 | Accepted: 2022/08/15 | Published: 2022/11/25
Received: 2022/07/23 | Accepted: 2022/08/15 | Published: 2022/11/25
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |