Sun, Nov 30, 2025
[Archive]
Volume 9, Issue 2 (Spring 2023)
JCCNC 2023, 9(2): 89-102 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Monalisa M, Syukri M, Yellyanda Y, Eliezer T B. Factors Involved in Missed Nursing Care: A Systematic Review. JCCNC 2023; 9 (2) :89-102
URL: http://jccnc.iums.ac.ir/article-1-418-en.html
URL: http://jccnc.iums.ac.ir/article-1-418-en.html
1- Department of Nursing, Health Polytechnic, Ministry of Health Jambi, Jambi, Indonesia.
2- Department of Nursing, Health Polytechnic, Ministry of Health Jambi, Jambi, Indonesia. ,syukrimuh290@gmail.com
2- Department of Nursing, Health Polytechnic, Ministry of Health Jambi, Jambi, Indonesia. ,
Keywords: Missed nursing care, Rationed care, Unfinished care, Incomplete care, Nursing care quality
Full-Text [PDF 790 kb]
(1783 Downloads)
| Abstract (HTML) (3296 Views)
• Missed nursing care (MNC) happens in many hospitals worldwide and affects the quality of nursing services.
• Many studies have been conducted on the factors that contribute to the occurrence of MNC, but there is no clear conclusion about these factors.
• Problems with labor resources seem to be the most important aggravating factor for MNC.
• Staffing adequacy as a part of the labor resources factor seems to be the most influencing factor for the occurrence of MNC.
• Many studies have been conducted on the factors that contribute to the occurrence of MNC, but there is no clear conclusion about these factors.
• Problems with labor resources seem to be the most important aggravating factor for MNC.
• Staffing adequacy as a part of the labor resources factor seems to be the most influencing factor for the occurrence of MNC.
Plain Language Summary
MNC in healthcare facilities greatly affects the quality of services and trust of service users. In general, the factors contributing to the occurrence of MNC fall into three categories: Labor resources, material resources, and teamwork and communication. The most influential category is labor resources—staffing adequacy seems the most influential.
Full-Text: (1344 Views)
1. Introduction
Missed nursing care (MNC) refers to unintentionally missing or not completing nursing care (Bragadóttir et al., 2017; Liu et al., 2019). The literature presents a range of definitions, conceptual frameworks, and measurement tools for unfinished, rationed, and missed care. Both the terms “missed care” and “unfinished care” have their origins in the United States (Kalisch et al., 2009; Uchmanowicz, 2017). Schubert et al. (2008) introduced the “rated care” term, and “care left undone” is another term in the literature (Ball et al., 2014). All terms refer to unfinished essential or routine nursing care (Recio-Saucedo et al., 2018). The “nursing care” scope encompasses all the emotional, clinical, and administrative tasks nurses are responsible for completing (Albsoul et al., 2019; Palese et al., 2015).
In the past few years, the frequency of MNC has been recognized as a quality indicator for nursing care and patient safety. It is often a warning sign (red flag) to indicate inadequate staffing levels (Kitson, 2018; Lewis et al., 2009). Nursing care includes activities carried out by nursing personnel, such as administering medication, ambulation and turning the patient, changing the position, bathing the patient, oral care, recording vital signs, documentation of input and output, nutrition, and education for discharge from the hospital. MNC or omission error occurs when this essential care is not provided to the patient (Kalisch, 2006).
MNC happens when standard, required nursing care is not delivered or is significantly delayed, indicating an error or omission. MNC is also referred to by various terms, such as implicitly rationed care, omitted nursing care, unmet patient needs, and unfinished nursing care. All these terms indicate that obligatory nursing care is delayed, uncompleted, or lacking in clinical, emotional, and administrative aspects for some reasons (Campagna et al., 2021; Putra et al., 2021; Scott et al., 2019). MNC has been associated with negative patient outcomes that result from various factors, including the work environment, patient care needs, and staffing problems (Hammad et al., 2021; Janatolmakan & Khatony, 2022; Schubert et al., 2008).
Previously, several studies have been conducted on factors or specific categories related to the incidence of MNC, but the information provided is still noncomprehensive, ungeneralizable, and inconclusive. This systematic review aims to find the factors involved in the incidence of missed nursing care.
2. Materials and Methods
Review protocol
This systematic review follows the preferred reporting items for systematic review and meta-analyses (PRISMA) statement 2020 (Page et al., 2021). It analyzes the factors influencing MNCs based on peer-reviewed studies published from 2012 to 2022.
Eligibility criteria
We included all studies that reported evidence of MNC-related factors published from January 2012 to 2022, written in English and peer-reviewed journals. All studies using hospital nurses directly responsible for patient care were included in this review. Studies on the role of nurses and MNC-related factors, especially factors that focus on nursing activities such as competence, work environment, and teamwork, are also included in this review. Duplicate publications, systematic reviews, books, chapters, commentaries, letters to editors, editorial comments, not full texts, case reports, and dissertations were excluded from this review. Reference manager (Mendeley) was used to identify and remove duplicates.
The participant, intervention/exposure, comparison, outcome, and study design ( population, intervention, comparison, outcomes, and study [PICOS]/ population/problem/patient, exposure, outcome [PEO]) criteria outlined in Table 1 were used to select studies for inclusion in this review.
.jpg)
Search strategy
The databases used in the literature search include ScienceDirect, Cochrane Library, PubMed, ProQuest, and the Wiley Online Library. Other databases could not be used due to inaccessibility. The specified keywords comply with the MeSH terms for health research. The keywords adapted vary according to the compatibility with the type of search engines. The structure of the search keyword arrangement using the Boolean operator “AND” or “OR” is as follows: (“missed nursing care” [title/abstract]) OR (“incomplete care” [title/abstract]) AND (“nurse workload” [title/abstract]) OR (“nurse-patient ratio” [title/abstract]) OR (“work satisfaction” [title/abstract]) OR (“shift schedule” [title/abstract]) OR (“work environment” [title/abstract]) OR (“teamwork” [title/abstract]) OR (team work [title/abstract])) AND (“nursing care quality” [title/abstract]). A summary of the keywords used in each database is shown in Table 2.
.jpg)
Selection process
Two authors independently screened each article (title/abstract), and the first author resolved disagreements. The screening was done by adjusting the title, objectives, and conclusions. Other necessary information was obtained from the main part of the study. The focus of the screening was on the inclusion criteria of the systematic review.
Quality appraisal
We used the NIH Quality assessment tool for observational cohort and cross-sectional studies (NIH, 2019) for quality assessment. It consists of 14 questions regarding the completeness of the reviewed studies. The quality of the studies is categorized as good, fair, and poor. Articles with scores lower than 30% of the criteria were classified as “poor,” scores between 30% and 70% as “fair,” and scores more than 70% as “good” study quality. Articles classified as “fair” and “good” were chosen. Two authors independently assessed the risk of bias using the cochrane collaboration’s risk of bias (ROBINS-I) tool (Higgins et al., 2008). Disagreements were resolved by discussion or reference to a third author. Each potential source of bias was marked as “low risk of bias,” “some concerns,” and “high risk of bias.” Studies with low to moderate risk of bias were included.
Data extraction and synthesis
Three authors (MN, YL, BE) independently performed data extraction. Differences between the authors were resolved by consensus after consulting with other researchers (supervising lecturers). The extraction items consisted of the first author/year, factors, and research design, including observational study (cross-sectional, cohort, retrospective), qualitative, sample size, assessment instrument, and outcomes.
3. Results
Based on the search results from the five databases, 3611 articles were obtained, 217 were duplicates, and 2109 were marked as ineligible by the reference manager (Mendeley). In the title and abstract screening process, 1196 articles were eliminated, leaving 89 articles for thorough screening of the article content. A total of 73 articles were eliminated because they did not meet the inclusion criteria of this review. Only 16 articles were ultimately eligible for further analysis. The search results are based on the PRISMA 2020 flow chart (Figure 1).
.jpg)
Study characteristics
Based on the 16 studies in this review, it is clear that the studies were conducted in several countries, including 5 studies in the USA, 2 studies in Australia, and 1 study each in Iceland, Korea, Philippines, Mexico, Egypt, Jordan, Italy, Iran, and Brazil. The research design used in these 16 studies was descriptive correlational (cross-sectional), focusing on the factors related to or affecting the occurrence of MNCs in nursing services in hospitals. One study used a mixed-method design to explore the MNC phenomenon from a nurse’s perspective.
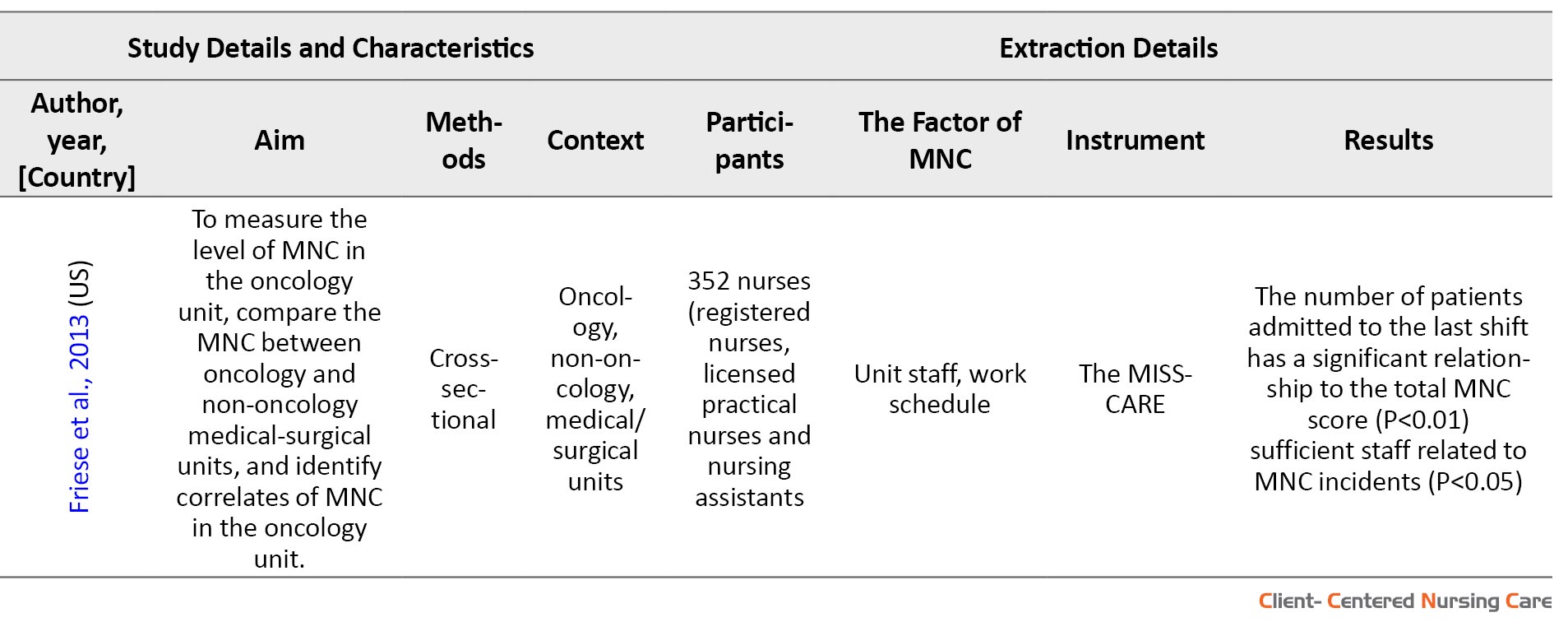
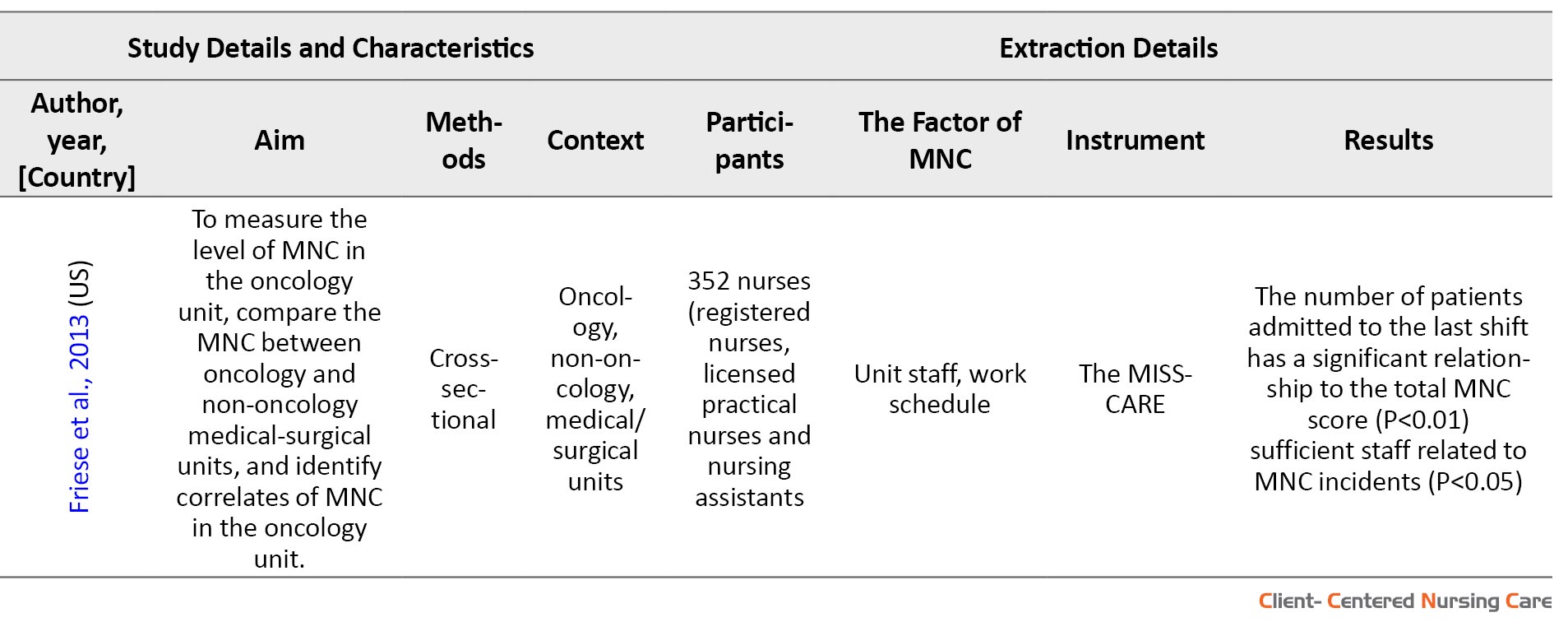
The number of participants used was 33–5, 861 nurses in different levels. The context of the studies included the intensive care unit (ICU), neonatal intensive care unit (NICU), medical, surgical, emergency, telemetry, mother-infant unit, COVID-19 unit, and oncology unit. A total of six studies did not specify the room or field in which the study was conducted (only mentioned treatment rooms) (Table 3).
.jpg)
.jpg)
.jpg)
Study quality
Table 4 summarizes the study quality assessment process based on 14 question items from the NIH assessment tool for observational studies.
.jpg)
The factors associated with MNCs are categorized into three major parts based on Kalisch et al. study. These categories are as follows: Labor resources (number and type of nursing staff, the competence of nursing staff, education, and experience of staff; material resources (availability of medicines and necessary equipment); and teamwork and communication (between the patient care team, nurses, physicians, and support staff) (Kalisch, 2006).
Labor source factor
Among the included studies, a study conducted in the United States showed that nurses with a heavy workload have two to three times the potential for MNC problems compared to nurses with a low workload (Lake et al., 2018). Meanwhile, a study in Australia found that nurses’ retention is simultaneously associated with the workload experienced by them (Blackman et al., 2018). In a study in Italy, workload was mentioned as a protective factor against the incidence of MNC (Palese et al., 2015).
Several studies also mention that the number of nurses and the nursing staff are the factors associated with the incidence of MNC. A study in Iceland stated that unit and staff characteristics are significantly associated with the MNC (Bragadóttir et al., 2017). The same result was also found in a study in the US, where the characteristics of the respondents, including age, position, education, years of experience, overtime hours in the last week, and the number of patients treated in the previous shift, had significant relationships with the total missed care score (Friese & Himes-Ferris, 2013). Among nurses’ characteristics, the bivariate analysis showed that job roles are significantly correlated with MNC. In particular, staff nurses obtained significantly higher mean MNCs scores than nurse managers (Labrague, 2021). A study in Australia states that the presence of new nurses in the treatment room, unfamiliar with existing practices and patients, leads to the development of MNC, especially negligence in drug administration (Albsoul et al., 2019). Nurse shortages in the United States, Mexico, Jordan, and Egypt have led to high nurse-to-patient ratios that significantly support the emergence of MNCs (Campbell et al., 2020; Diab & Ebrahim, 2019; Hernández-Cruz et al., 2017; Saqer & AbuAlRub, 2018). Blackman et al. underlined that shift work is also associated with the incidence of MNC, where nurses on the afternoon shift experience MNC more often than nurses on the morning/afternoon shift (Blackman et al., 2018). Meanwhile, a study in Iran found that the prevalence of MNC was significantly higher among male nurses, older age, and a higher number of patients treated (Chegini et al., 2020). A study in Brazil found no significant relationship between the MISSCARE-BRASIL domain and the variables of age, time since graduation, experience in the unit, and institution (Dutra et al., 2019).
Several studies also assessed the correlation between nurse job satisfaction and MNC. Duffy and colleagues used the PES-NWI (The Practice Environment Scale of the Nursing Work Index) to assess the association between nurse job satisfaction and MNC. They found a significant relationship (Duffy et al., 2018). The current level of job satisfaction of the participating qualified nurses directly influences MNC (Blackman et al., 2018; Palese et al., 2015; Saqer & AbuAlRub, 2018).
Material source
One category is the nurse’s work environment. Several studies in this review have also underlined the existence of a significant relationship between the work environment and the MNC (Albsoul et al., 2019; Campbell et al., 2020; Diab & Ebrahim, 2019; Duffy et al., 2018; Hessels et al., 2015; Kim et al., 2018; Saqer & AbuAlRub, 2018; Lake et al., 2018). Another study reported that MNC was significantly lower in the ICU than in the medical (P<0.001) and surgical (P<0.001) wards (Bragadóttir et al., 2017). Labrague stated that nurses in large hospital facilities had significantly higher mean MNCs scores than small hospital facilities (Labrague, 2021).
Labrague and colleagues conducted their study during the peak period of the COVID-19 pandemic. The results of their research indicated that the availability of personal protective equipment (PPE) greatly influences the occurrence of MNCs (Labrague et al., 2022). Albsoul and colleagues emphasize the importance of mastering how to work with patient care equipment. The occurrence of MNC in several treatment rooms, especially those equipped with high-tech equipment, will greatly increase the incidence of MNC among nurses (Albsoul et al., 2019). In Mexico, nurses reported the unavailability of medication when needed (21.1%) as a significant reason for MNC, followed by supplies and equipment (16.9%) (Hernández-Cruz et al., 2017). Meanwhile, studies in Egypt and Jordan found that material resources associated with all domains of nursing care were missed, especially attending interdisciplinary care conferences (Diab & Ebrahim, 2019; Saqer & AbuAlRub, 2018). Chegini also found that equipment was closely related to MNC incidence (Chegini et al., 2020).
Team work and communication
Several studies in this review analyzed the relationship between teamwork and the incidence of MNC. Overall, studies that discuss these factors show a significant relationship between teamwork, including communication, and the incidence of MNC in patient care in hospitals (Blackman et al., 2018; Duffy et al., 2018; Dutra et al., 2019; Saqer & AbuAlRub, 2018). Albsoul reported that the communication problems most frequently reported by nurses causing MNC were nurse-patient task inequity (38.6%), tension and damaged communication with medical staff (25%), and stress and distraction on the interaction within the nursing team (25%) (Albsoul et al., 2019). Whereas in a study in Mexico, nurses considered the nurse’s absence when the patient called her (22.5%) as a significant reason, followed by tension or errors in communication with medical staff (21.1%) (Hernández-Cruz et al., 2017). According to Diab and Ibrahim, the communication factor is the second most influential factor in the incidence of MNCs in Egypt (Diab & Ebrahim, 2019). Chegini says communication protects against MNC events (Chegini et al., 2020).
4. Discussion
This systematic review provided a real picture of the most important factors affecting the occurrence of MNC in healthcare centers. It has summarized the findings of 16 studies involving 7834 participants. Most studies included in this review are correlational studies that have examined the relationship between different factors and MNC and sometimes have determined the impact of MNC on the quality of nursing care.
Factors associated with MNC
Based on these 16 studies, the factors associated with the incidence of MNC include labor resources (age of staff, workload, job satisfaction, nurse-patient ratio, clinical career, level of nurse education) and material resource factors (work environment, infrastructure, characteristics of hospitals and units, PPE, mastery of technology, management), and teamwork and communication factors (teamwork communication, communication between teamwork members).
Age is an important factor contributing to the incidence of MNC, as shown by Bragadóttir and colleagues in their study. They found that younger nurses have reported significantly more MNCs than older or senior nurses (Bragadóttir et al., 2017). A correlation study also shows a close relationship between the age of nurses or staff and the quality of nursing services (Stalpers et al., 2017).
Lake et al. stated that the percentage of nurses who faced a heavy workload and experienced MNC was two to three times higher than that of nurses with a low workload (Lake et al., 2018). Meanwhile, Blackman and colleagues estimate that the workload will increase if nurses get continuous verbal and non-verbal pressure from managers or other team members (Blackman et al., 2018). Previous systematic reviews have stated that the excessive workload experienced by primary care nurses and the resulting possible burnout affect the nurses’ health status. However, this also affects the patients because their safety is not guaranteed, care errors caused by the heavy workload and fatigue of nurses lead to an increase in patient mortality, and as stated in this review, the quality of received care decreases (Pérez-Francisco et al., 2020). Previous correlational studies have confirmed that heavy workloads cause burnout in nurses, thereby increasing the intention to leave or quit (Holland et al., 2019; Jourdain & Chênevert, 2010; Phillips, 2020).
The work environment is also an important contributing factor to the incidence of MNC, as described in several studies included in this review (Albsoul et al., 2019; Bragadóttir et al., 2017; Campbell et al., 2020; Duffy et al., 2018; Hessels et al., 2015; Kim et al., 2018; Saqer & AbuAlRub, 2018; Lake et al., 2018). A better practice environment is believed to reduce the incidence of MNCs. Improving the work environment will reduce the likelihood that nurses will miss care by 32% and reduce the frequency of missed care by 0.3 activities (Lake et al., 2018). It is also known that the availability of facilities in the treatment room will greatly assist health services in a hospital (Douthit et al., 2015; Moons et al., 2019; Zangrillo et al., 2020).
Improving existing resource management and safety culture in units can reduce MNC levels. In addition, using benchmark data to identify weaknesses in the work environment can also be considered a kind of predictor (Lake et al., 2018). Previous studies have stated that the ability and effectiveness of nurse managers are related to MNC because nurse managers are responsible for managing the work environment/working conditions, assigning assignments, and coordinating available resources. In addition, more effective leadership will increase the work loyalty of nurses and so on will have implications for the quality of nursing services (Manning, 2016).
Improvements in system functionality, such as increasing skills and availability of effective information technology systems, are needed to address inadequate documentation in healthcare systems (Albsoul et al., 2019; Chaboyer et al., 2021; Du et al., 2020; Jarošová et al., 2021). Another factor that contributes greatly to the occurrence of MNC is teamwork and staff communication. Previous studies have shown that teamwork and collaboration between healthcare professionals can lead to better patient education and, thus, patient participation in decision-making and self-care (Morley & Cashell, 2017). Collaboration between doctors and nurses working in teams towards a shared objective is crucial for improving patient care. However, interdisciplinary collaboration is frequently inadequate (Fewster-Thuente, 2015). To enhance the quality and efficacy of clinical teamwork, it is necessary to consider social, cultural, and organizational factors (Gurková et al., 2021; Mahdizadeh et al., 2015). Healthcare professionals, including nurses, must be encouraged to collaborate through education and capacity building, particularly regarding communication (Eskin Bacaksiz et al., 2020; Labrague et al., 2022; Morley & Cashell, 2017).
The impact of MNCs on the quality of nursing services
The finding that some hospitals have significantly more MNCs than others is a matter of safety and quality for the hospital and a concern for patients and families. In particular, patient comfort, parental counseling, and education are the most commonly overlooked activities. Lake et al. suggested that the level of MNC would pose problems for patient-centered care and optimal infant and family outcomes. Every instance of MNC implies that some infants may not receive their planned feeding, miss out on breast milk or timely medication, experience delayed or missed treatments and procedures, and may be subjected to unnecessary pain (Lake et al., 2018). Friese and Himes-ferrishis identified fewer MNCs in the oncology unit, which may explain why oncology nursing staff perceive their quality of care to be higher than that of their fellow nurses in the medico-surgical setting. This study also explains why hospital nursing staff are closely related to complications, failure to save lives, and death (Friese & Himes-Ferris, 2013).
A study conducted in the UK confirmed that MNC is linked to poorer patient outcomes, such as increased mortality and morbidity and lower levels of patient satisfaction with hospital services. MNC has also been associated with decreased staff satisfaction and a higher likelihood of quitting their jobs (Gibbon & Crane, 2018). A previous systematic review concluded that MNC predicts reduced nurse-reported quality of care, decreased patient satisfaction, increased side effects, decreased job satisfaction, and increased intention to leave (Jones et al., 2015).
We had limited access to several databases in our review, which made it impossible to obtain a wider range of relevant studies. This study could not proceed with a meta-analysis because we collected a few low to moderate-quality studies. However, our study is sufficient to provide an overview of factors involved in MNC in high-income and middle-income countries.
5. Conclusion
This systematic review indicated several factors contributing to the incidence of MNC. There were three categories of factors related to MNC: Labor resources (workload, staff adequacy, staff characteristics, nurse-patient ratio, shift work, and nurse job satisfaction), material sources (work environment, personal protective equipment, patient care equipment), and teamwork and communication (communication within nursing team, and communication with medical staff). The most common influencing factor among the reviewed articles seemed to be staffing adequacy. It is suggested that a meta-analysis be conducted using larger databases to determine the most dominant factors affecting the incidence of MNCs in healthcare services.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to preaparing this study.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We want to thank the director of the Jambi Health Polytechnic for supporting this research.
References
Albsoul, R., et al., 2019. Factors influencing missed nursing care in public hospitals in Australia: An exploratory mixed methods study. The International Journal of Health Planning and Management, 34(4), pp. e1820-32. [DOI:10.1002/hpm.2898] [PMID]
Ball, J. E., et al., 2014. Care left undone’during nursing shifts: Associations with workload and perceived quality of care. BMJ Quality & Safety, 23(2), pp. 116-25. [DOI:10.1136/bmjqs-2012-001767] [PMID] [PMCID]
Blackman, I., et al., 2015. Factors influencing why nursing care is missed. Journal of Clinical Nursing, 24(1-2), pp. 47-56. [DOI:10.1111/jocn.12688] [PMID]
Bragadóttir, H., Kalisch, B. J. & Tryggvadóttir, G. B., 2017. Correlates and predictors of missed nursing care in hospitals. Journal of Clinical Nursing, 26(11-12), pp. 1524-34. [DOI:10.1111/jocn.13449] [PMID]
Campagna, S., et al., 2021. Missed nursing care in a sample of high-dependency Italian nursing home residents: Description of nursing care in action. Journal of Patient Safety, 17(8), pp. e1840-5. [DOI:10.1097/PTS.0000000000000643] [PMID]
Campbell, C. M., et al., 2020. Variables associated with missed nursing care in Alabama: A cross‐sectional analysis. Journal of Nursing Management, 28(8), pp. 2174-84. [DOI:10.1111/jonm.12979] [PMID]
Chaboyer, W., et al., 2021. Missed nursing care: An overview of reviews. The Kaohsiung Journal of Medical Sciences, 37(2), pp. 82-91. [DOI:10.1002/kjm2.12308] [PMID]
Chegini, Z., et al., 2020. Missed nursing care and related factors in Iranian hospitals: A cross‐sectional survey. Journal of Nursing Management, 28(8), pp. 2205-15. [DOI:10.1111/jonm.13055] [PMID]
Diab, G. H. & Ebrahim, R. M., 2019. Factors leading to missed nursing care among nurses at selected hospitals. American Journal of Nursing Research, 7(2), pp. 136-47. [Link]
Douthit, N., et al., 2015. Exposing some important barriers to health care access in the rural USA. Public Health, 129(6), pp. 611-20. [DOI:10.1016/j.puhe.2015.04.001]
Du, H., et al., 2020. A cross‐sectional observational study of missed nursing care in hospitals in China. Journal of Nursing Management, 28(7), pp. 1578-88. [DOI:10.1111/jonm.13112] [PMID] [PMCID]
Duffy, J. R., Culp, S. & Padrutt, T., 2018. Description and factors associated with missed nursing care in an acute care community hospital. JONA: The Journal of Nursing Administration, 48(7/8), pp. 361-7. [DOI:10.1097/NNA.0000000000000630] [PMID]
Dutra, C. K., et al., 2019. Situations and reasons for missed nursing care in medical and surgical clinic units. Revista Da Escola de Enfermagem Da USP, 53, pp. e03470. [DOI:10.1590/s1980-220x2017050203470] [PMID]
Eskin Bacaksiz, F., et al., 2020. A cross‐sectional study of the determinants of missed nursing care in the private sector: Hospital/unit/staff characteristics, professional quality of life and work alienation. Journal of Nursing Management, 28(8), pp. 1975-85. [DOI:10.1111/jonm.12999] [PMID]
Fewster-Thuente, L., 2015. Working together toward a common goal: A grounded theory of nurse-physician collaboration. Medsurg Nursing, 24(5). [Link]
Friese, C. R. & Himes-Ferris, L., 2013. Nursing practice environments and job outcomes in ambulatory oncology settings. The Journal of Nursing Administration, 43(3), pp. 149-54. [DOI:10.1097/NNA.0b013e318283dc3f] [PMID] [PMCID]
Gibbon, B. & Crane, J., 2018. The impact of ‘missed care’on the professional socialisation of nursing students: A qualitative research study. Nurse Education Today, 66, pp. 19-24. [DOI:10.1016/j.nedt.2018.04.002] [PMID]
Gurková, E., Mikšová, Z. & Šáteková, L., 2022. Missed nursing care in hospital environments during the COVID‐19 pandemic. International Nursing Review, 69(2), pp. 175–84. [DOI:10.1111/inr.12710] [PMID] [PMCID]
Hammad, M., Guirguis, W. & Mosallam, R., 2021. Missed nursing care, non-nursing tasks, staffing adequacy, and job satisfaction among nurses in a teaching hospital in Egypt. The Journal of the Egyptian Public Health Association, 96(1), pp. 22. [DOI:10.1186/s42506-021-00083-0] [PMID] [PMCID]
Hernández-Cruz, R., et al., 2017. Factors influencing the missed nursing care in patients from a private hospital. Revista Latino-Americana de Enfermagem, 25, pp. e2877. [DOI:10.1590/1518-8345.1227.2877] [PMID] [PMCID]
Hessels, A. J., et al., 2015. The impact of the nursing practice environment on missed nursing care. Clinical Nursing Studies, 3(4), pp. 60-5. [DOI:10.5430/cns.v3n4p60] [PMID] [PMCID]
Higgins, J. P. T. & Altman, D. G., 2008. Assessing risk of bias in included studies. In: J. P. T. Higgins., & S. Green (eds), Cochrane handbook for systematic reviews of interventions. New Jersey: Wiley. [DOI:10.1002/9780470712184.ch8]
Holland, P., et al., 2019. The impact of perceived workload on nurse satisfaction with work-life balance and intention to leave the occupation. Applied Nursing Research, 49, pp. 70-6. [DOI:10.1016/j.apnr.2019.06.001] [PMID]
Janatolmakan, M. & Khatony, A., 2022. Explaining the experience of nurses on missed nursing care: A qualitative descriptive study in Iran. Applied Nursing Research, 63, pp. 151542. [DOI:10.1016/j.apnr.2021.151542] [PMID]
Jarošová, D., et al., 2021. Hospital and unit variables of missed nursing care in acute care hospitals: A cross‐sectional study. Journal of Clinical Nursing, 30(7-8), pp. 1099-110. [DOI:10.1111/jocn.15655] [PMID]
Jones, T. L., Hamilton, P. & Murry, N., 2015. Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. International Journal of Nursing Studies, 52(6), pp. 1121-37. [DOI:10.1016/j.ijnurstu.2015.02.012] [PMID]
Jourdain, G. & Chênevert, D., 2010. Job demands-resources, burnout and intention to leave the nursing profession: A questionnaire survey. International Journal of Nursing Studies, 47(6), pp. 709-22. [DOI:10.1016/j.ijnurstu.2009.11.007] [PMID]
Kalisch, B. J., 2006. Missed nursing care: A qualitative study. Journal of Nursing Care Quality, 21(4), pp. 306-13. [DOI:10.1097/00001786-200610000-00006] [PMID]
Kalisch, B. J., Landstrom, G. L., & Hinshaw, A. S. (2009). Missed nursing care: A concept analysis. Journal of Advanced Nursing, 65(7), 1509-17. [DOI:10.1111/j.1365-2648.2009.05027.x] [PMID]
Kim, K. J., Yoo, M. S. & Seo, E. J., 2018. Exploring the influence of nursing work environment and patient safety culture on missed nursing care in Korea. Asian Nursing Research, 12(2), pp. 121-6. [DOI:10.1016/j.anr.2018.04.003] [PMID]
Kitson, A. L., 2018. The fundamentals of care framework as a point-of-care nursing theory. Nursing Research, 67(2), pp. 99-107. [DOI:10.1097/NNR.0000000000000271] [PMID]
Labrague, L. J., 2021. Linking nurse practice environment, safety climate and job dimensions to missed nursing care. International Nursing Review, 69(3), pp. 350-8. [DOI:10.1111/inr.12736] [PMID]
Labrague, L. J., de Los Santos, J. A. A. & Fronda, D. C., 2022. Factors associated with missed nursing care and nurse‐assessed quality of care during the COVID‐19 pandemic. Journal of Nursing Management, 30(1), pp. 62-70. [PMID] [PMCID]
Lewis, M. & Pettersson, G., 2009. Governance in health care delivery: Raising performance. Washington, D.C.: The World Bank Development Economics Department & Human Development Department [DOI:10.1596/1813-9450-5074]
Liu, J., et al., 2019. Relationship between work environments, nurse outcomes, and quality of care in ICUs: Mediating role of nursing care left undone. Journal of Nursing Care Quality, 34(3), pp. 250-5. [DOI:10.1097/NCQ.0000000000000374] [PMID]
Mahdizadeh, M., Heydari, A. & Moonaghi, H. K., 2015. Clinical interdisciplinary collaboration models and frameworks from similarities to differences: A systematic review. Global Journal of Health Science, 7(6), pp. 170-80. [DOI:10.5539/gjhs.v7n6p170] [PMID] [PMCID]
Manning, J., 2016. The influence of nurse manager leadership style on staff nurse work engagement. The Journal of Nursing Administration, 46(9), pp. 438-43. [DOI:10.1097/NNA.0000000000000372] [PMID]
Moons, K., Waeyenbergh, G. & Pintelon, L., 2019. Measuring the logistics performance of internal hospital supply chains-a literature study. Omega, 82, pp. 205-17. [DOI:10.1016/j.omega.2018.01.007]
Morley, L. & Cashell, A., 2017. Collaboration in health care. Journal of Medical Imaging and Radiation Sciences, 48(2), pp. 207-16. [DOI:10.1016/j.jmir.2017.02.071] [PMID]
National Heart, Lung, and Blood Institute., 2019. Study quality assessment tools [Internet]. Viewed at May 2023, [Link]
Page, M. J., et al., 2021. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, pp. 105906. [DOI:10.1016/j.ijsu.2021.105906] [PMID]
Palese, A., et al., 2015. Missed nursing care and predicting factors in the Italian medical care setting. Internal and Emergency Medicine, 10(6), pp. 693-702. [Link]
Pérez-Francisco, D. H., et al., 2020. Influence of workload on primary care nurses’ health and burnout, patients’ safety, and quality of care: Integrative review. Healthcare, 8(1), pp. 12. [DOI:10.3390/healthcare8010012] [PMID] [PMCID]
Phillips, C., 2020. Relationships between workload perception, burnout, and intent to leave among medical-surgical nurses. JBI Evidence Implementation, 18(2), pp. 265-73. [DOI:10.1097/XEB.0000000000000220] [PMID]
Putra, K. R., et al., 2021. Availability of human resources, facilities, communications and missed nursing care. Jurnal Aisyah: Jurnal Ilmu Kesehatan, 6(2), pp. 279-84. [DOI:10.30604/jika.v6i2.503]
Recio‐Saucedo, A., et al., 2018. What impact does nursing care left undone have on patient outcomes? Review of the literature. Journal of Clinical Nursing, 27(11-12), pp. 2248-59. [DOI:10.1111/jocn.14058] [PMID] [PMCID]
Saqer, T. J. & AbuAlRub, R. F., 2018. Missed nursing care and its relationship with confidence in delegation among hospital nurses. Journal of Clinical Nursing, 27(13-14), pp. 2887-95. [DOI:10.1111/jocn.14380] [PMID]
Schubert, M., et al., 2008. Rationing of nursing care and its relationship to patient outcomes: The Swiss extension of the International Hospital Outcomes Study. International Journal for Quality in Health Care, 20(4), pp. 227-37. [DOI:10.1093/intqhc/mzn017] [PMID] [PMCID]
Scott, P. A., et al., 2019. Resource allocation and rationing in nursing care: A discussion paper. Nursing Ethics, 26(5), pp. 1528-39. [DOI:10.1177/0969733018759831] [PMID] [PMCID]
Stalpers, D., et al., 2017. Nurse‐perceived quality of care in intensive care units and associations with work environment characteristics: A multicentre survey study. Journal of Advanced Nursing, 73(6), pp. 1482-90. [DOI:10.1111/jan.13242] [PMID]
Uchmanowicz, I., 2017. Missed nursing care-what went wrong? Central European Journal of Nursing and Midwifery, 8(2), pp. 609. [DOI:10.15452/CEJNM.2017.08.0008]
Zangrillo, A., et al., 2020. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: Facing the COVID-19 pandemic emergency. Critical Care and Resuscitation, 22(2), pp. 91-4. [DOI:10.51893/2020.2.pov1] [PMID]
Lake, E. T., et al., 2018. Association of patient acuity and missed nursing care in U.S. neonatal intensive care units. Medical Care Research and Review: MCRR, 77(5), pp. 451–60. [DOI:10.1177/1077558718806743] [PMID] [PMCID]
Missed nursing care (MNC) refers to unintentionally missing or not completing nursing care (Bragadóttir et al., 2017; Liu et al., 2019). The literature presents a range of definitions, conceptual frameworks, and measurement tools for unfinished, rationed, and missed care. Both the terms “missed care” and “unfinished care” have their origins in the United States (Kalisch et al., 2009; Uchmanowicz, 2017). Schubert et al. (2008) introduced the “rated care” term, and “care left undone” is another term in the literature (Ball et al., 2014). All terms refer to unfinished essential or routine nursing care (Recio-Saucedo et al., 2018). The “nursing care” scope encompasses all the emotional, clinical, and administrative tasks nurses are responsible for completing (Albsoul et al., 2019; Palese et al., 2015).
In the past few years, the frequency of MNC has been recognized as a quality indicator for nursing care and patient safety. It is often a warning sign (red flag) to indicate inadequate staffing levels (Kitson, 2018; Lewis et al., 2009). Nursing care includes activities carried out by nursing personnel, such as administering medication, ambulation and turning the patient, changing the position, bathing the patient, oral care, recording vital signs, documentation of input and output, nutrition, and education for discharge from the hospital. MNC or omission error occurs when this essential care is not provided to the patient (Kalisch, 2006).
MNC happens when standard, required nursing care is not delivered or is significantly delayed, indicating an error or omission. MNC is also referred to by various terms, such as implicitly rationed care, omitted nursing care, unmet patient needs, and unfinished nursing care. All these terms indicate that obligatory nursing care is delayed, uncompleted, or lacking in clinical, emotional, and administrative aspects for some reasons (Campagna et al., 2021; Putra et al., 2021; Scott et al., 2019). MNC has been associated with negative patient outcomes that result from various factors, including the work environment, patient care needs, and staffing problems (Hammad et al., 2021; Janatolmakan & Khatony, 2022; Schubert et al., 2008).
Previously, several studies have been conducted on factors or specific categories related to the incidence of MNC, but the information provided is still noncomprehensive, ungeneralizable, and inconclusive. This systematic review aims to find the factors involved in the incidence of missed nursing care.
2. Materials and Methods
Review protocol
This systematic review follows the preferred reporting items for systematic review and meta-analyses (PRISMA) statement 2020 (Page et al., 2021). It analyzes the factors influencing MNCs based on peer-reviewed studies published from 2012 to 2022.
Eligibility criteria
We included all studies that reported evidence of MNC-related factors published from January 2012 to 2022, written in English and peer-reviewed journals. All studies using hospital nurses directly responsible for patient care were included in this review. Studies on the role of nurses and MNC-related factors, especially factors that focus on nursing activities such as competence, work environment, and teamwork, are also included in this review. Duplicate publications, systematic reviews, books, chapters, commentaries, letters to editors, editorial comments, not full texts, case reports, and dissertations were excluded from this review. Reference manager (Mendeley) was used to identify and remove duplicates.
The participant, intervention/exposure, comparison, outcome, and study design ( population, intervention, comparison, outcomes, and study [PICOS]/ population/problem/patient, exposure, outcome [PEO]) criteria outlined in Table 1 were used to select studies for inclusion in this review.
.jpg)
Search strategy
The databases used in the literature search include ScienceDirect, Cochrane Library, PubMed, ProQuest, and the Wiley Online Library. Other databases could not be used due to inaccessibility. The specified keywords comply with the MeSH terms for health research. The keywords adapted vary according to the compatibility with the type of search engines. The structure of the search keyword arrangement using the Boolean operator “AND” or “OR” is as follows: (“missed nursing care” [title/abstract]) OR (“incomplete care” [title/abstract]) AND (“nurse workload” [title/abstract]) OR (“nurse-patient ratio” [title/abstract]) OR (“work satisfaction” [title/abstract]) OR (“shift schedule” [title/abstract]) OR (“work environment” [title/abstract]) OR (“teamwork” [title/abstract]) OR (team work [title/abstract])) AND (“nursing care quality” [title/abstract]). A summary of the keywords used in each database is shown in Table 2.
.jpg)
Selection process
Two authors independently screened each article (title/abstract), and the first author resolved disagreements. The screening was done by adjusting the title, objectives, and conclusions. Other necessary information was obtained from the main part of the study. The focus of the screening was on the inclusion criteria of the systematic review.
Quality appraisal
We used the NIH Quality assessment tool for observational cohort and cross-sectional studies (NIH, 2019) for quality assessment. It consists of 14 questions regarding the completeness of the reviewed studies. The quality of the studies is categorized as good, fair, and poor. Articles with scores lower than 30% of the criteria were classified as “poor,” scores between 30% and 70% as “fair,” and scores more than 70% as “good” study quality. Articles classified as “fair” and “good” were chosen. Two authors independently assessed the risk of bias using the cochrane collaboration’s risk of bias (ROBINS-I) tool (Higgins et al., 2008). Disagreements were resolved by discussion or reference to a third author. Each potential source of bias was marked as “low risk of bias,” “some concerns,” and “high risk of bias.” Studies with low to moderate risk of bias were included.
Data extraction and synthesis
Three authors (MN, YL, BE) independently performed data extraction. Differences between the authors were resolved by consensus after consulting with other researchers (supervising lecturers). The extraction items consisted of the first author/year, factors, and research design, including observational study (cross-sectional, cohort, retrospective), qualitative, sample size, assessment instrument, and outcomes.
3. Results
Based on the search results from the five databases, 3611 articles were obtained, 217 were duplicates, and 2109 were marked as ineligible by the reference manager (Mendeley). In the title and abstract screening process, 1196 articles were eliminated, leaving 89 articles for thorough screening of the article content. A total of 73 articles were eliminated because they did not meet the inclusion criteria of this review. Only 16 articles were ultimately eligible for further analysis. The search results are based on the PRISMA 2020 flow chart (Figure 1).
.jpg)
Study characteristics
Based on the 16 studies in this review, it is clear that the studies were conducted in several countries, including 5 studies in the USA, 2 studies in Australia, and 1 study each in Iceland, Korea, Philippines, Mexico, Egypt, Jordan, Italy, Iran, and Brazil. The research design used in these 16 studies was descriptive correlational (cross-sectional), focusing on the factors related to or affecting the occurrence of MNCs in nursing services in hospitals. One study used a mixed-method design to explore the MNC phenomenon from a nurse’s perspective.
The number of participants used was 33–5, 861 nurses in different levels. The context of the studies included the intensive care unit (ICU), neonatal intensive care unit (NICU), medical, surgical, emergency, telemetry, mother-infant unit, COVID-19 unit, and oncology unit. A total of six studies did not specify the room or field in which the study was conducted (only mentioned treatment rooms) (Table 3).
.jpg)
.jpg)
.jpg)
Study quality
Table 4 summarizes the study quality assessment process based on 14 question items from the NIH assessment tool for observational studies.
.jpg)
The factors associated with MNCs are categorized into three major parts based on Kalisch et al. study. These categories are as follows: Labor resources (number and type of nursing staff, the competence of nursing staff, education, and experience of staff; material resources (availability of medicines and necessary equipment); and teamwork and communication (between the patient care team, nurses, physicians, and support staff) (Kalisch, 2006).
Labor source factor
Among the included studies, a study conducted in the United States showed that nurses with a heavy workload have two to three times the potential for MNC problems compared to nurses with a low workload (Lake et al., 2018). Meanwhile, a study in Australia found that nurses’ retention is simultaneously associated with the workload experienced by them (Blackman et al., 2018). In a study in Italy, workload was mentioned as a protective factor against the incidence of MNC (Palese et al., 2015).
Several studies also mention that the number of nurses and the nursing staff are the factors associated with the incidence of MNC. A study in Iceland stated that unit and staff characteristics are significantly associated with the MNC (Bragadóttir et al., 2017). The same result was also found in a study in the US, where the characteristics of the respondents, including age, position, education, years of experience, overtime hours in the last week, and the number of patients treated in the previous shift, had significant relationships with the total missed care score (Friese & Himes-Ferris, 2013). Among nurses’ characteristics, the bivariate analysis showed that job roles are significantly correlated with MNC. In particular, staff nurses obtained significantly higher mean MNCs scores than nurse managers (Labrague, 2021). A study in Australia states that the presence of new nurses in the treatment room, unfamiliar with existing practices and patients, leads to the development of MNC, especially negligence in drug administration (Albsoul et al., 2019). Nurse shortages in the United States, Mexico, Jordan, and Egypt have led to high nurse-to-patient ratios that significantly support the emergence of MNCs (Campbell et al., 2020; Diab & Ebrahim, 2019; Hernández-Cruz et al., 2017; Saqer & AbuAlRub, 2018). Blackman et al. underlined that shift work is also associated with the incidence of MNC, where nurses on the afternoon shift experience MNC more often than nurses on the morning/afternoon shift (Blackman et al., 2018). Meanwhile, a study in Iran found that the prevalence of MNC was significantly higher among male nurses, older age, and a higher number of patients treated (Chegini et al., 2020). A study in Brazil found no significant relationship between the MISSCARE-BRASIL domain and the variables of age, time since graduation, experience in the unit, and institution (Dutra et al., 2019).
Several studies also assessed the correlation between nurse job satisfaction and MNC. Duffy and colleagues used the PES-NWI (The Practice Environment Scale of the Nursing Work Index) to assess the association between nurse job satisfaction and MNC. They found a significant relationship (Duffy et al., 2018). The current level of job satisfaction of the participating qualified nurses directly influences MNC (Blackman et al., 2018; Palese et al., 2015; Saqer & AbuAlRub, 2018).
Material source
One category is the nurse’s work environment. Several studies in this review have also underlined the existence of a significant relationship between the work environment and the MNC (Albsoul et al., 2019; Campbell et al., 2020; Diab & Ebrahim, 2019; Duffy et al., 2018; Hessels et al., 2015; Kim et al., 2018; Saqer & AbuAlRub, 2018; Lake et al., 2018). Another study reported that MNC was significantly lower in the ICU than in the medical (P<0.001) and surgical (P<0.001) wards (Bragadóttir et al., 2017). Labrague stated that nurses in large hospital facilities had significantly higher mean MNCs scores than small hospital facilities (Labrague, 2021).
Labrague and colleagues conducted their study during the peak period of the COVID-19 pandemic. The results of their research indicated that the availability of personal protective equipment (PPE) greatly influences the occurrence of MNCs (Labrague et al., 2022). Albsoul and colleagues emphasize the importance of mastering how to work with patient care equipment. The occurrence of MNC in several treatment rooms, especially those equipped with high-tech equipment, will greatly increase the incidence of MNC among nurses (Albsoul et al., 2019). In Mexico, nurses reported the unavailability of medication when needed (21.1%) as a significant reason for MNC, followed by supplies and equipment (16.9%) (Hernández-Cruz et al., 2017). Meanwhile, studies in Egypt and Jordan found that material resources associated with all domains of nursing care were missed, especially attending interdisciplinary care conferences (Diab & Ebrahim, 2019; Saqer & AbuAlRub, 2018). Chegini also found that equipment was closely related to MNC incidence (Chegini et al., 2020).
Team work and communication
Several studies in this review analyzed the relationship between teamwork and the incidence of MNC. Overall, studies that discuss these factors show a significant relationship between teamwork, including communication, and the incidence of MNC in patient care in hospitals (Blackman et al., 2018; Duffy et al., 2018; Dutra et al., 2019; Saqer & AbuAlRub, 2018). Albsoul reported that the communication problems most frequently reported by nurses causing MNC were nurse-patient task inequity (38.6%), tension and damaged communication with medical staff (25%), and stress and distraction on the interaction within the nursing team (25%) (Albsoul et al., 2019). Whereas in a study in Mexico, nurses considered the nurse’s absence when the patient called her (22.5%) as a significant reason, followed by tension or errors in communication with medical staff (21.1%) (Hernández-Cruz et al., 2017). According to Diab and Ibrahim, the communication factor is the second most influential factor in the incidence of MNCs in Egypt (Diab & Ebrahim, 2019). Chegini says communication protects against MNC events (Chegini et al., 2020).
4. Discussion
This systematic review provided a real picture of the most important factors affecting the occurrence of MNC in healthcare centers. It has summarized the findings of 16 studies involving 7834 participants. Most studies included in this review are correlational studies that have examined the relationship between different factors and MNC and sometimes have determined the impact of MNC on the quality of nursing care.
Factors associated with MNC
Based on these 16 studies, the factors associated with the incidence of MNC include labor resources (age of staff, workload, job satisfaction, nurse-patient ratio, clinical career, level of nurse education) and material resource factors (work environment, infrastructure, characteristics of hospitals and units, PPE, mastery of technology, management), and teamwork and communication factors (teamwork communication, communication between teamwork members).
Age is an important factor contributing to the incidence of MNC, as shown by Bragadóttir and colleagues in their study. They found that younger nurses have reported significantly more MNCs than older or senior nurses (Bragadóttir et al., 2017). A correlation study also shows a close relationship between the age of nurses or staff and the quality of nursing services (Stalpers et al., 2017).
Lake et al. stated that the percentage of nurses who faced a heavy workload and experienced MNC was two to three times higher than that of nurses with a low workload (Lake et al., 2018). Meanwhile, Blackman and colleagues estimate that the workload will increase if nurses get continuous verbal and non-verbal pressure from managers or other team members (Blackman et al., 2018). Previous systematic reviews have stated that the excessive workload experienced by primary care nurses and the resulting possible burnout affect the nurses’ health status. However, this also affects the patients because their safety is not guaranteed, care errors caused by the heavy workload and fatigue of nurses lead to an increase in patient mortality, and as stated in this review, the quality of received care decreases (Pérez-Francisco et al., 2020). Previous correlational studies have confirmed that heavy workloads cause burnout in nurses, thereby increasing the intention to leave or quit (Holland et al., 2019; Jourdain & Chênevert, 2010; Phillips, 2020).
The work environment is also an important contributing factor to the incidence of MNC, as described in several studies included in this review (Albsoul et al., 2019; Bragadóttir et al., 2017; Campbell et al., 2020; Duffy et al., 2018; Hessels et al., 2015; Kim et al., 2018; Saqer & AbuAlRub, 2018; Lake et al., 2018). A better practice environment is believed to reduce the incidence of MNCs. Improving the work environment will reduce the likelihood that nurses will miss care by 32% and reduce the frequency of missed care by 0.3 activities (Lake et al., 2018). It is also known that the availability of facilities in the treatment room will greatly assist health services in a hospital (Douthit et al., 2015; Moons et al., 2019; Zangrillo et al., 2020).
Improving existing resource management and safety culture in units can reduce MNC levels. In addition, using benchmark data to identify weaknesses in the work environment can also be considered a kind of predictor (Lake et al., 2018). Previous studies have stated that the ability and effectiveness of nurse managers are related to MNC because nurse managers are responsible for managing the work environment/working conditions, assigning assignments, and coordinating available resources. In addition, more effective leadership will increase the work loyalty of nurses and so on will have implications for the quality of nursing services (Manning, 2016).
Improvements in system functionality, such as increasing skills and availability of effective information technology systems, are needed to address inadequate documentation in healthcare systems (Albsoul et al., 2019; Chaboyer et al., 2021; Du et al., 2020; Jarošová et al., 2021). Another factor that contributes greatly to the occurrence of MNC is teamwork and staff communication. Previous studies have shown that teamwork and collaboration between healthcare professionals can lead to better patient education and, thus, patient participation in decision-making and self-care (Morley & Cashell, 2017). Collaboration between doctors and nurses working in teams towards a shared objective is crucial for improving patient care. However, interdisciplinary collaboration is frequently inadequate (Fewster-Thuente, 2015). To enhance the quality and efficacy of clinical teamwork, it is necessary to consider social, cultural, and organizational factors (Gurková et al., 2021; Mahdizadeh et al., 2015). Healthcare professionals, including nurses, must be encouraged to collaborate through education and capacity building, particularly regarding communication (Eskin Bacaksiz et al., 2020; Labrague et al., 2022; Morley & Cashell, 2017).
The impact of MNCs on the quality of nursing services
The finding that some hospitals have significantly more MNCs than others is a matter of safety and quality for the hospital and a concern for patients and families. In particular, patient comfort, parental counseling, and education are the most commonly overlooked activities. Lake et al. suggested that the level of MNC would pose problems for patient-centered care and optimal infant and family outcomes. Every instance of MNC implies that some infants may not receive their planned feeding, miss out on breast milk or timely medication, experience delayed or missed treatments and procedures, and may be subjected to unnecessary pain (Lake et al., 2018). Friese and Himes-ferrishis identified fewer MNCs in the oncology unit, which may explain why oncology nursing staff perceive their quality of care to be higher than that of their fellow nurses in the medico-surgical setting. This study also explains why hospital nursing staff are closely related to complications, failure to save lives, and death (Friese & Himes-Ferris, 2013).
A study conducted in the UK confirmed that MNC is linked to poorer patient outcomes, such as increased mortality and morbidity and lower levels of patient satisfaction with hospital services. MNC has also been associated with decreased staff satisfaction and a higher likelihood of quitting their jobs (Gibbon & Crane, 2018). A previous systematic review concluded that MNC predicts reduced nurse-reported quality of care, decreased patient satisfaction, increased side effects, decreased job satisfaction, and increased intention to leave (Jones et al., 2015).
We had limited access to several databases in our review, which made it impossible to obtain a wider range of relevant studies. This study could not proceed with a meta-analysis because we collected a few low to moderate-quality studies. However, our study is sufficient to provide an overview of factors involved in MNC in high-income and middle-income countries.
5. Conclusion
This systematic review indicated several factors contributing to the incidence of MNC. There were three categories of factors related to MNC: Labor resources (workload, staff adequacy, staff characteristics, nurse-patient ratio, shift work, and nurse job satisfaction), material sources (work environment, personal protective equipment, patient care equipment), and teamwork and communication (communication within nursing team, and communication with medical staff). The most common influencing factor among the reviewed articles seemed to be staffing adequacy. It is suggested that a meta-analysis be conducted using larger databases to determine the most dominant factors affecting the incidence of MNCs in healthcare services.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to preaparing this study.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We want to thank the director of the Jambi Health Polytechnic for supporting this research.
References
Albsoul, R., et al., 2019. Factors influencing missed nursing care in public hospitals in Australia: An exploratory mixed methods study. The International Journal of Health Planning and Management, 34(4), pp. e1820-32. [DOI:10.1002/hpm.2898] [PMID]
Ball, J. E., et al., 2014. Care left undone’during nursing shifts: Associations with workload and perceived quality of care. BMJ Quality & Safety, 23(2), pp. 116-25. [DOI:10.1136/bmjqs-2012-001767] [PMID] [PMCID]
Blackman, I., et al., 2015. Factors influencing why nursing care is missed. Journal of Clinical Nursing, 24(1-2), pp. 47-56. [DOI:10.1111/jocn.12688] [PMID]
Bragadóttir, H., Kalisch, B. J. & Tryggvadóttir, G. B., 2017. Correlates and predictors of missed nursing care in hospitals. Journal of Clinical Nursing, 26(11-12), pp. 1524-34. [DOI:10.1111/jocn.13449] [PMID]
Campagna, S., et al., 2021. Missed nursing care in a sample of high-dependency Italian nursing home residents: Description of nursing care in action. Journal of Patient Safety, 17(8), pp. e1840-5. [DOI:10.1097/PTS.0000000000000643] [PMID]
Campbell, C. M., et al., 2020. Variables associated with missed nursing care in Alabama: A cross‐sectional analysis. Journal of Nursing Management, 28(8), pp. 2174-84. [DOI:10.1111/jonm.12979] [PMID]
Chaboyer, W., et al., 2021. Missed nursing care: An overview of reviews. The Kaohsiung Journal of Medical Sciences, 37(2), pp. 82-91. [DOI:10.1002/kjm2.12308] [PMID]
Chegini, Z., et al., 2020. Missed nursing care and related factors in Iranian hospitals: A cross‐sectional survey. Journal of Nursing Management, 28(8), pp. 2205-15. [DOI:10.1111/jonm.13055] [PMID]
Diab, G. H. & Ebrahim, R. M., 2019. Factors leading to missed nursing care among nurses at selected hospitals. American Journal of Nursing Research, 7(2), pp. 136-47. [Link]
Douthit, N., et al., 2015. Exposing some important barriers to health care access in the rural USA. Public Health, 129(6), pp. 611-20. [DOI:10.1016/j.puhe.2015.04.001]
Du, H., et al., 2020. A cross‐sectional observational study of missed nursing care in hospitals in China. Journal of Nursing Management, 28(7), pp. 1578-88. [DOI:10.1111/jonm.13112] [PMID] [PMCID]
Duffy, J. R., Culp, S. & Padrutt, T., 2018. Description and factors associated with missed nursing care in an acute care community hospital. JONA: The Journal of Nursing Administration, 48(7/8), pp. 361-7. [DOI:10.1097/NNA.0000000000000630] [PMID]
Dutra, C. K., et al., 2019. Situations and reasons for missed nursing care in medical and surgical clinic units. Revista Da Escola de Enfermagem Da USP, 53, pp. e03470. [DOI:10.1590/s1980-220x2017050203470] [PMID]
Eskin Bacaksiz, F., et al., 2020. A cross‐sectional study of the determinants of missed nursing care in the private sector: Hospital/unit/staff characteristics, professional quality of life and work alienation. Journal of Nursing Management, 28(8), pp. 1975-85. [DOI:10.1111/jonm.12999] [PMID]
Fewster-Thuente, L., 2015. Working together toward a common goal: A grounded theory of nurse-physician collaboration. Medsurg Nursing, 24(5). [Link]
Friese, C. R. & Himes-Ferris, L., 2013. Nursing practice environments and job outcomes in ambulatory oncology settings. The Journal of Nursing Administration, 43(3), pp. 149-54. [DOI:10.1097/NNA.0b013e318283dc3f] [PMID] [PMCID]
Gibbon, B. & Crane, J., 2018. The impact of ‘missed care’on the professional socialisation of nursing students: A qualitative research study. Nurse Education Today, 66, pp. 19-24. [DOI:10.1016/j.nedt.2018.04.002] [PMID]
Gurková, E., Mikšová, Z. & Šáteková, L., 2022. Missed nursing care in hospital environments during the COVID‐19 pandemic. International Nursing Review, 69(2), pp. 175–84. [DOI:10.1111/inr.12710] [PMID] [PMCID]
Hammad, M., Guirguis, W. & Mosallam, R., 2021. Missed nursing care, non-nursing tasks, staffing adequacy, and job satisfaction among nurses in a teaching hospital in Egypt. The Journal of the Egyptian Public Health Association, 96(1), pp. 22. [DOI:10.1186/s42506-021-00083-0] [PMID] [PMCID]
Hernández-Cruz, R., et al., 2017. Factors influencing the missed nursing care in patients from a private hospital. Revista Latino-Americana de Enfermagem, 25, pp. e2877. [DOI:10.1590/1518-8345.1227.2877] [PMID] [PMCID]
Hessels, A. J., et al., 2015. The impact of the nursing practice environment on missed nursing care. Clinical Nursing Studies, 3(4), pp. 60-5. [DOI:10.5430/cns.v3n4p60] [PMID] [PMCID]
Higgins, J. P. T. & Altman, D. G., 2008. Assessing risk of bias in included studies. In: J. P. T. Higgins., & S. Green (eds), Cochrane handbook for systematic reviews of interventions. New Jersey: Wiley. [DOI:10.1002/9780470712184.ch8]
Holland, P., et al., 2019. The impact of perceived workload on nurse satisfaction with work-life balance and intention to leave the occupation. Applied Nursing Research, 49, pp. 70-6. [DOI:10.1016/j.apnr.2019.06.001] [PMID]
Janatolmakan, M. & Khatony, A., 2022. Explaining the experience of nurses on missed nursing care: A qualitative descriptive study in Iran. Applied Nursing Research, 63, pp. 151542. [DOI:10.1016/j.apnr.2021.151542] [PMID]
Jarošová, D., et al., 2021. Hospital and unit variables of missed nursing care in acute care hospitals: A cross‐sectional study. Journal of Clinical Nursing, 30(7-8), pp. 1099-110. [DOI:10.1111/jocn.15655] [PMID]
Jones, T. L., Hamilton, P. & Murry, N., 2015. Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. International Journal of Nursing Studies, 52(6), pp. 1121-37. [DOI:10.1016/j.ijnurstu.2015.02.012] [PMID]
Jourdain, G. & Chênevert, D., 2010. Job demands-resources, burnout and intention to leave the nursing profession: A questionnaire survey. International Journal of Nursing Studies, 47(6), pp. 709-22. [DOI:10.1016/j.ijnurstu.2009.11.007] [PMID]
Kalisch, B. J., 2006. Missed nursing care: A qualitative study. Journal of Nursing Care Quality, 21(4), pp. 306-13. [DOI:10.1097/00001786-200610000-00006] [PMID]
Kalisch, B. J., Landstrom, G. L., & Hinshaw, A. S. (2009). Missed nursing care: A concept analysis. Journal of Advanced Nursing, 65(7), 1509-17. [DOI:10.1111/j.1365-2648.2009.05027.x] [PMID]
Kim, K. J., Yoo, M. S. & Seo, E. J., 2018. Exploring the influence of nursing work environment and patient safety culture on missed nursing care in Korea. Asian Nursing Research, 12(2), pp. 121-6. [DOI:10.1016/j.anr.2018.04.003] [PMID]
Kitson, A. L., 2018. The fundamentals of care framework as a point-of-care nursing theory. Nursing Research, 67(2), pp. 99-107. [DOI:10.1097/NNR.0000000000000271] [PMID]
Labrague, L. J., 2021. Linking nurse practice environment, safety climate and job dimensions to missed nursing care. International Nursing Review, 69(3), pp. 350-8. [DOI:10.1111/inr.12736] [PMID]
Labrague, L. J., de Los Santos, J. A. A. & Fronda, D. C., 2022. Factors associated with missed nursing care and nurse‐assessed quality of care during the COVID‐19 pandemic. Journal of Nursing Management, 30(1), pp. 62-70. [PMID] [PMCID]
Lewis, M. & Pettersson, G., 2009. Governance in health care delivery: Raising performance. Washington, D.C.: The World Bank Development Economics Department & Human Development Department [DOI:10.1596/1813-9450-5074]
Liu, J., et al., 2019. Relationship between work environments, nurse outcomes, and quality of care in ICUs: Mediating role of nursing care left undone. Journal of Nursing Care Quality, 34(3), pp. 250-5. [DOI:10.1097/NCQ.0000000000000374] [PMID]
Mahdizadeh, M., Heydari, A. & Moonaghi, H. K., 2015. Clinical interdisciplinary collaboration models and frameworks from similarities to differences: A systematic review. Global Journal of Health Science, 7(6), pp. 170-80. [DOI:10.5539/gjhs.v7n6p170] [PMID] [PMCID]
Manning, J., 2016. The influence of nurse manager leadership style on staff nurse work engagement. The Journal of Nursing Administration, 46(9), pp. 438-43. [DOI:10.1097/NNA.0000000000000372] [PMID]
Moons, K., Waeyenbergh, G. & Pintelon, L., 2019. Measuring the logistics performance of internal hospital supply chains-a literature study. Omega, 82, pp. 205-17. [DOI:10.1016/j.omega.2018.01.007]
Morley, L. & Cashell, A., 2017. Collaboration in health care. Journal of Medical Imaging and Radiation Sciences, 48(2), pp. 207-16. [DOI:10.1016/j.jmir.2017.02.071] [PMID]
National Heart, Lung, and Blood Institute., 2019. Study quality assessment tools [Internet]. Viewed at May 2023, [Link]
Page, M. J., et al., 2021. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, pp. 105906. [DOI:10.1016/j.ijsu.2021.105906] [PMID]
Palese, A., et al., 2015. Missed nursing care and predicting factors in the Italian medical care setting. Internal and Emergency Medicine, 10(6), pp. 693-702. [Link]
Pérez-Francisco, D. H., et al., 2020. Influence of workload on primary care nurses’ health and burnout, patients’ safety, and quality of care: Integrative review. Healthcare, 8(1), pp. 12. [DOI:10.3390/healthcare8010012] [PMID] [PMCID]
Phillips, C., 2020. Relationships between workload perception, burnout, and intent to leave among medical-surgical nurses. JBI Evidence Implementation, 18(2), pp. 265-73. [DOI:10.1097/XEB.0000000000000220] [PMID]
Putra, K. R., et al., 2021. Availability of human resources, facilities, communications and missed nursing care. Jurnal Aisyah: Jurnal Ilmu Kesehatan, 6(2), pp. 279-84. [DOI:10.30604/jika.v6i2.503]
Recio‐Saucedo, A., et al., 2018. What impact does nursing care left undone have on patient outcomes? Review of the literature. Journal of Clinical Nursing, 27(11-12), pp. 2248-59. [DOI:10.1111/jocn.14058] [PMID] [PMCID]
Saqer, T. J. & AbuAlRub, R. F., 2018. Missed nursing care and its relationship with confidence in delegation among hospital nurses. Journal of Clinical Nursing, 27(13-14), pp. 2887-95. [DOI:10.1111/jocn.14380] [PMID]
Schubert, M., et al., 2008. Rationing of nursing care and its relationship to patient outcomes: The Swiss extension of the International Hospital Outcomes Study. International Journal for Quality in Health Care, 20(4), pp. 227-37. [DOI:10.1093/intqhc/mzn017] [PMID] [PMCID]
Scott, P. A., et al., 2019. Resource allocation and rationing in nursing care: A discussion paper. Nursing Ethics, 26(5), pp. 1528-39. [DOI:10.1177/0969733018759831] [PMID] [PMCID]
Stalpers, D., et al., 2017. Nurse‐perceived quality of care in intensive care units and associations with work environment characteristics: A multicentre survey study. Journal of Advanced Nursing, 73(6), pp. 1482-90. [DOI:10.1111/jan.13242] [PMID]
Uchmanowicz, I., 2017. Missed nursing care-what went wrong? Central European Journal of Nursing and Midwifery, 8(2), pp. 609. [DOI:10.15452/CEJNM.2017.08.0008]
Zangrillo, A., et al., 2020. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: Facing the COVID-19 pandemic emergency. Critical Care and Resuscitation, 22(2), pp. 91-4. [DOI:10.51893/2020.2.pov1] [PMID]
Lake, E. T., et al., 2018. Association of patient acuity and missed nursing care in U.S. neonatal intensive care units. Medical Care Research and Review: MCRR, 77(5), pp. 451–60. [DOI:10.1177/1077558718806743] [PMID] [PMCID]
Type of Study: Review Article |
Subject:
General
Received: 2022/09/19 | Accepted: 2022/11/26 | Published: 2023/05/1
Received: 2022/09/19 | Accepted: 2022/11/26 | Published: 2023/05/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |