Thu, Oct 23, 2025
[Archive]
Volume 9, Issue 3 (Summer 2023)
JCCNC 2023, 9(3): 183-192 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alinejad-Naeini M, Zamani P, Heidari-Beni F. Relationship Between Maternal Fear and Anxiety About COVID-19 and Maternal Role Attainment in Mothers of Preterm Neonates. JCCNC 2023; 9 (3) :183-192
URL: http://jccnc.iums.ac.ir/article-1-427-en.html
URL: http://jccnc.iums.ac.ir/article-1-427-en.html
1- Department of Neonatal Intensive Care Nursing, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Medical Surgical Nursing, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,heidarifarshad70@yahoo.com
2- Department of Medical Surgical Nursing, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
Keywords: COVID-19, Anxiety, Fear, Maternal role attainment, Preterm neonate, Neonatal intensive care unit
Full-Text [PDF 680 kb]
(724 Downloads)
| Abstract (HTML) (2522 Views)
Full-Text: (690 Views)
1. Introduction
The novel Coronavirus 2019 (COVID-19) outbreak started in China in 2019 and quickly became a menace to global health. The World Health Organization (WHO) has introduced COVID-19 as an international public health emergency (Cucinotta & Vanelli, 2020; Wachs et al., 2009). COVID-19 pandemic is a serious public health emergency, especially in populations that health systems are vulnerable to crisis (Rothe et al., 2020; Mcintosh et al., 2020). The official announcement of the disease outbreak in Iran also caused panic and public concern (Salimi et al., 2020). Mothers are concerned about their children being infected with this virus. Preterm neonates have an immature immune system, which puts them at greater risk for severe infections. Cases of neonatal pneumonia were identified in newborns whose mothers were infected with COVID-19 (Zeng et al., 2020). While mothers and their neonates were not initially identified as high-risk populations, evidence from previous viral outbreaks suggests a risk of adverse outcomes for both mother and infant (Alfaraj et al., 2019). This possibility has given rise to pandemic policies, such as observing social distancing and preventing vertical infection, as well as establishing special considerations to protect the health of mothers and babies and the need to consider unwanted consequences for them (Buekens et al., 2020). The neonatal intensive care unit (NICU) environment appears to facilitate the transmission of the COVID-19 virus, and given the role of asymptomatic persons in the spread of the virus, these dangers cannot be undervalued (Cavicchiolo et al., 2020). Studies on different types of transmission, clinical spectrum, and duration of virus excretion in COVID-19 patients are ongoing. In the absence of sufficient evidence, it is recommended that a cautious approach be taken to close contact between an asymptomatic, suspected, or established COVID-19 mother and her infant (Verma et al., 2020).
The COVID-19 pandemic will negatively affect maternal psychological health, highlighting the need for intervention (Saccone et al., 2020). Several studies have been conducted on the effects of quarantine on maternal psychological health, which have stated a high prevalence of emotional symptoms (Brooks et al., 2020; Liu et al., 2012a). Women are more psychologically affected by the same pandemics, such as severe acute respiratory syndrome and middle eastern respiratory syndrome (Schwartz & Graham, 2020). Concerns related to contracting COVID-19 start from the first hours of birth and continue until the days after delivery, making mothers an emotionally susceptible group (Thapa et al., 2020). Recently, several studies have indicated the negative effect of COVID-19 on maternal psychological health (Zanardo et al., 2020; Suzuki, 2020). Maternal psychological wellbeing difficulties are believed to be related to short-term and long-term risks to the mother-newborn relationship, especially the mother-newborn attachment (Nolvi et al., 2016; Fallon et al., 2021; Tolja et al., 2020). According to the mentioned reasons, healthcare providers must pay more attention to the psychological health of mothers after childbirth (Bassetti et al., 2020). Mothers with premature babies must cope with the unknown stresses of the postpartum period and endure the pressures caused by the pandemic during the critical care period for their children (Dekel et al., 2019). Mothers may also face broader challenges that undermine their ability to care for high-risk infants. Disruption of the social support structure due to the need for social distance may increase the mother’s sense of isolation and symptoms of anxiety and depression (Lemmon et al., 2020). Some studies about Coronavirus pandemic indicated fear, anxiety, depression and the symptoms caused by them through self-reporting and clinical evaluations in the postpartum period (Saccone et al., 2020; Jungari, 2020).
The term “maternal role attainment” is part of the transition process that leads to acquiring maternal role identity. During this period, the mother can fulfill her maternal role and behave appropriately for the determined maternal role (Fouquier, 2013). Achieving the maternal role is one of mothers’ greatest fundamental and significant roles (Sansom, 2010). Mother, neonate, and environment are variables associated with the maternal role. Maternal variables such as marital status, maternal age, maternal confidence, birth experience, stress, and emotional state influence maternal role attainment (Kordi et al., 2017). However, the effects of COVID-19 on maternal stress due to childbirth and subsequent maternal complications are unknown (Mayopoulos et al., 2021). Despite the vulnerability of mothers with preterm infants during the COVID-19 pandemic, no study has been conducted on the fear and anxiety of mothers with preterm newborns admitted to NICU in Iran. Also, the effect of COVID-19 disease on mother-infant relationships and maternal role attainment is unclear. Accordingly, our study will determine the relationship of maternal fear and anxiety about COVID-19 with maternal role development in Iranian mothers with premature neonates admitted to NICUs.
2. Materials and Methods
This descriptive correlational study was conducted in three level-III NICUs affiliated with the Iran University of Medical Sciences (IUMS) in Tehran City, Iran, from June 2021 to July 2022. NICUs in Iran comprise two sections: NICU and post-NICU. Preterm newborns after birth are admitted to the NICU due to dangerous health situations and the need for intensive medical care. Preterm newborns are transported to the post-NICU for continuation of care after recovering and stabilizing their condition. In both areas, access is restricted to prevent transmission of infection, and only parents of preterm neonates can visit their children whenever they wish. The basic principles and policies are the same in both areas.
Sampling was performed from both NICU and post-NICU. This study sample was mothers with their premature neonate in the NICU who were recruited via convenience sampling. The sample size was calculated to be 211 at a 95% confidence interval and 80% test power. Also, for the relationship between maternal role, fear, and anxiety of COVID-19 to be considered statistically significant (considering the absence of a similar study), the amount of the correlation coefficient was considered equal to 0.2. After inserting the values in Equations 1 and 2, the sample size was estimated as follows:

The inclusion criteria were being mothers of neonates admitted to NICU, having a neonate with 28–37 weeks gestational age, having the ability to read and write in Persian, having no previous experience in the NICU, lacking experience of a dead neonate, and passed at least 3 days of neonate admission to NICU. The exclusion criteria were having a positive PCR test, cognitive impairment, having severe gynecologic problems before, during, or after delivery, drug abuse, and the use of antidepressants. Convenience sampling was used to select the eligible subjects. For this purpose, the researcher visited one of the hospitals every day and invited the mothers who met the inclusion criteria to the study until the sample size was achieved.
The data were collected using a sociodemographic questionnaire, the Coronavirus anxiety scale (CAS), the fear of COVID-19 scale, and the maternal role adaptation scale in NICUs.
The sociodemographic questionnaire consisted of the mother’s characteristics, including age, occupation, education level, economic status, and neonatal characteristics, including neonate’s sex, gestational age, corrected age, and neonatal birth weight that the researcher completed.
CAS scale was designed by Lee (2020). This scale has five items that measure distinct behavioral, cognitive, emotional, and physiological responses to COVID-19 anxiety. Each item of the CAS is rated on a 5-point Likert scale from 0 (not at all) to 4 (nearly every day) based on experiences over the past two weeks. A CAS total score ≥9 indicates probable dysfunctional Coronavirus-related anxiety. This scale has high reliability (α=0.93) (Lee, 2020). Abasi et al. evaluated the psychometric properties of CAS in Iran. The results demonstrated that the Persian version of the scale (P-CAS) had a good internal consistency (α=0.80) (Abasi et al., 2021). The Cronbach α coefficient of the scale in this study was 0.911.
Fear of COVID-19 scale was developed to complement the clinical efforts in preventing the spread of and treating COVID-19 cases (Ahorsu et al., 2020). This scale has 7 items, and respondents express their opinion using a five-point Likert scale. Each item was rated from 1 to 5, and the total would be from 7 to 35. A higher score indicates a greater fear of the Coronavirus. The internal consistency (α=0.82) and test-retest reliability (by intraclass correlation coefficient) (ICC=0.72) of the scale were satisfactory (Ahorsu et al., 2020). The robust psychometric properties of this instrument were also confirmed in Portugal with composite reliability (CR=0.88) and internal consistency (Cronbach α coefficient=0.82). They showed it is a valid and reliable tool to assess the fear of COVID-19 among the general population (Magano et al., 2021). Psychometric properties of the Persian version of the scale were confirmed, and its Cronbach α coefficient was reported as 0.87 (Dadfar et al., 2021). The Cronbach α coefficient for this scale in the present study was 0.84.
The maternal role adaptation scale in NICUs was designed by Heydarpour et al. (2016) and contained 32 items and 6 dimensions: Participation in care (14 items), self-efficacy (6 items), distant mothering (3 items), uncertainty (4 items), interaction (3 items), and growth and development (2 items). They are scored on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The total score is calculated by the sum of the dimensions’ scores ranging from 32 to 160, and the higher scores indicate better maternal role attainment. The scale’s reliability has been approved with Cronbach α and intraclass correlation coefficient as 0.77 and 0.81, respectively. This tool is relatively simple, and mothers of preterm babies can complete it within 10 minutes (Heydarpour et al., 2016). The present study obtained a Cronbach α coefficient of 0.801 for the maternal role adaptation scale, confirming its reliability.
After receiving the letter of introduction from IUMS, the data were collected in different shift works according to the predetermined schedule. The mothers had enough time to complete the questionnaires through self-reporting. Data were collected in a relaxed and safe place without compromising the care of the baby. SPSS software, version 23 was used for all statistical analyses. Descriptive statistics were used to assess the frequency (percentage) and Mean±SD of participants’ characteristics. The Kolmogorov-Smirnov test was used to determine data distribution, indicating all the data have a normal distribution. Accordingly, the parametric inferential statistics consisting of the independent samples t-test, one-way ANOVA, and the Pearson correlation coefficient were used to assess the relationship between demographic variables and anxiety, fear, and maternal role attainment. The Pearson correlation coefficient test evaluated the associations between anxiety, fear, and maternal role attainment.
3. Results
In this study, 211 mothers with preterm neonates participated. Most mothers had secondary education (66.82%), were second para (41.2%), had a history of Coronavirus infection (76.8%), had received the COVID-19 vaccine (65.9%), had not any abortion (65.8%), and were housewives (83.4%). The characteristics of the mothers and their neonates are presented in Table 1.

There were statistically significant relationships between para (P=0.006), children’s number (P<0.001), neonate’s birth weight (P<0.001), neonatal gestational age (P=0.009), and maternal role attainment. Also, none of the demographic variables had a significant relationship with anxiety and fear (P>0.05).
The mean score of the mothers’ anxiety was 11.44±3.19, and 59.2% had not experienced Coronavirus-related anxiety. The mean fear and maternal role attainment score was 26.49±5.92 and 57.61±11.95, respectively (Table 2).

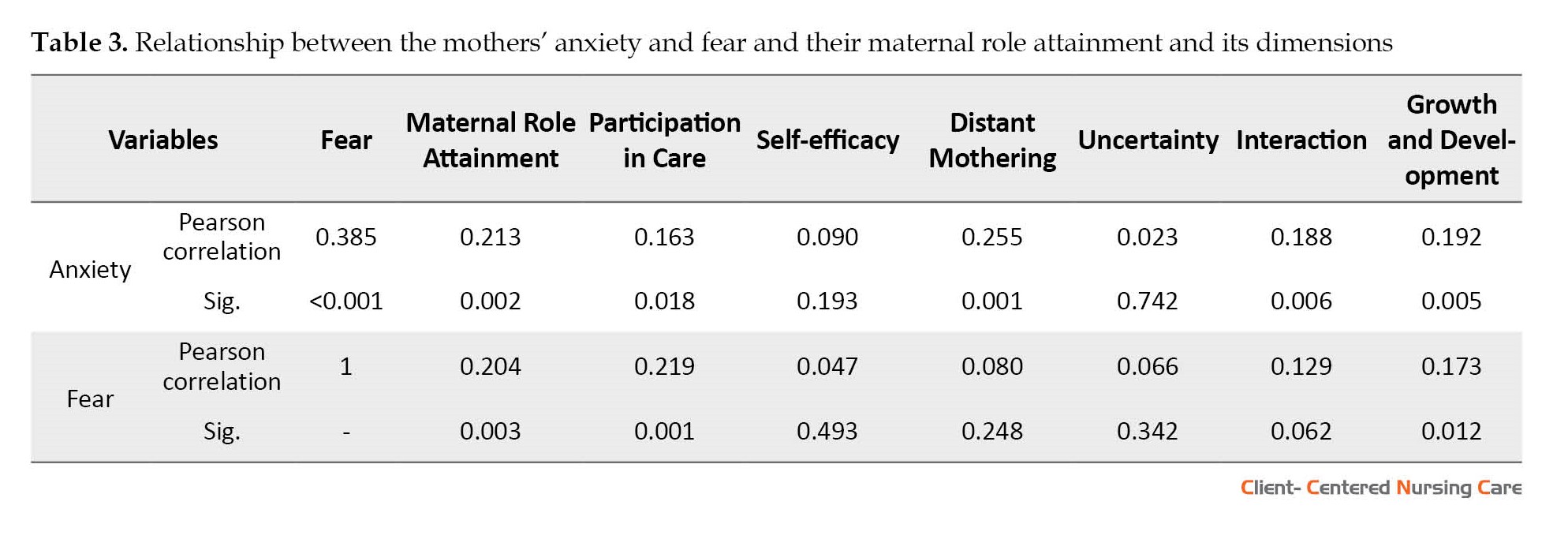
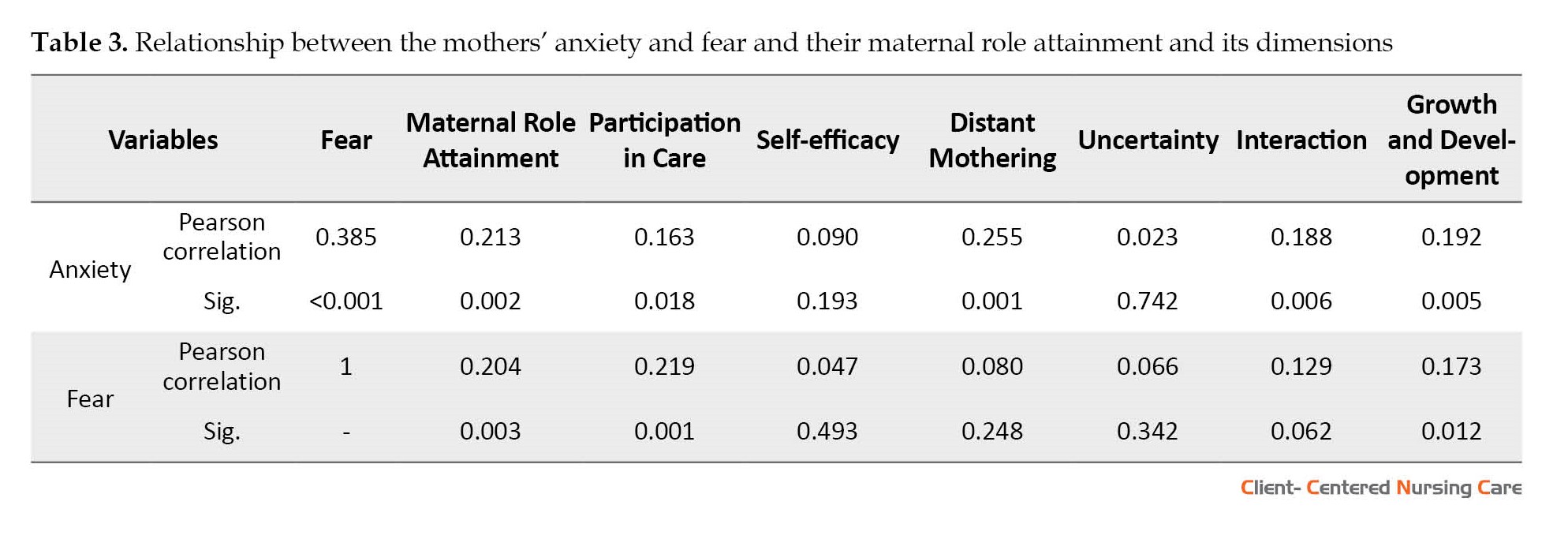
The Pearson correlation coefficient was used to assess the linear relationship between the variables, and the results indicated a positive and significant relationship between anxiety and fear (r=0.385, P<0.001). Also, there were positive and significant relationships between anxiety and maternal role attainment (r=0.213, P=0.002), and dimensions of participation in care (r=0.163, P=0.018), distant mothering (r=0.255, P=0.001), interaction (r=0.188, P=0.006), and growth and development (r=0.192, P=0.005). There were also positive and significant relationships between fear and maternal role attainment (r=0.204, P=0.003) and the dimensions of participation in care (r=0.219, P=0.001) and growth and development (r=0.173, P=0.012) (Table 3).
4. Discussion
Many mothers experience psychological symptoms such as acute stress, anxiety, depression, and fear while their babies are admitted to NICU (Rogers et al., 2013; Treyvaud et al., 2014). These problems have recently called for increased psychological support for families with neonates admitted to NICUs (Treyvaud et al., 2019). The COVID-19 pandemic is acting as a great new environmental stressor, adding to the pre-existing psychological distress of these mothers (Erdei & Liu, 2020). This study investigated the relationship between maternal fear and anxiety about COVID-19 and maternal role attainment in Iranian mothers with preterm neonates admitted to NICUs.
The findings of this study indicated that the mean scores of COVID-19 anxiety and fear in mothers with preterm neonates were at a high level. Some studies on pregnant women have reported the same levels of COVID-19 anxiety (Karimi et al., 2021; Abedzadeh-Kalahroudi et al., 2021; Moyer et al., 2020). Pregnancy, childbirth, postpartum, and the period of adjustment with mothering are the most sensitive times for mothers physically and mentally. Therefore, there may be a risk of mental disorders in these episodes. The negative view and uncertainty about the baby’s health caused by the COVID-19 pandemic increase the mother’s fear and anxiety (Mertens et al., 2020). A study of mothers with neonates admitted to the NICU found that concerns related to COVID-19 were strongly associated with mental health symptoms in this population (Lemmon et al., 2020). A study investigating the psychological effect of COVID-19 on mothers with premature babies reported that the average overall score for COVID-19 anxiety was mild (Eghbali Babadi et al., 2021). A study conducted during the COVID-19 outbreak found that over half of parents whose babies were admitted to the NICU scored higher than the cut-off point on anxiety (Polloni et al., 2021).
As shown in previous pandemics, outbreaks of infectious diseases increased fear in society (Su et al., 2007; Zhu et al., 2008). Fear is an adaptive defense mechanism in humans that is essential for survival and involves several biological processes preparing to respond to potentially dangerous events. However, when it is chronic or disproportionate, it can cause psychiatric disorders (Su et al., 2007). The fear is increased among women during the COVID-19 outbreak because of concern about their children’s health (Pearson et al., 2021). Studies on maternal fear of COVID-19 are limited. In a study by Uzun et al. which examined postpartum COVID-19 fear and its association with breastfeeding, mothers scored high on COVID-19 fear (Uzun et al., 2021). Prolonged separation from the infant leads to impairment in the parent/child relationship, a substantial neurological factor for the infant’s health and development (Tandberg et al., 2019; Erdei & Liu, 2020).
Conversely, the interaction between parents and their neonate lead to infant development, while separation may cause distress and fear in both (Bergman et al., 2019). It is shown that worry about the baby contracting COVID-19, along with the social restrictions caused by preventive measures, negatively affects the thoughts and feelings of mothers and increases psychological symptoms such as anxiety, depression, and distress (Zanardo et al., 2020; Liu et al., 2021). The research results also showed a direct and significant relationship between anxiety and fear of COVID-19 and maternal role attainment. To situate motherhood in the global COVID-19 pandemic context, one must first consider motherhood in a broader social context (Hillier & Greig, 2020). It seems that due to the effects of poverty and social inequality on the pandemic in Iran and the world (Asaadi & Daliri, 2021), as well as mothers’ perception of the uncontrollability of the pandemic, these mothers have experienced more fear and anxiety and therefore put a lot of effort into taking care of their babies. According to the results, the mother’s participation in childcare has the highest score, while the growth and development dimension has the lowest score. The results of another study on the determinants of a mother’s role adaptation in mothers with premature babies also showed that participation in the childcare dimension has the highest score (Khalesi et al., 2021). The mother’s presence and the repeated hugging of the baby can make a stronger parent-child attachment and become the basis for subsequent interactions that provide the possibility of further child development. In addition, it strengthens the feeling of motherhood and leads to greater achievement of maternal role (Sullivan et al., 2011). Another study shows that mothers with a passive role in caring for their infants, whose participation is low, are less adapted to maternal roles) (Taubman-Ben-Ari et al., 2009). It has been shown that most mothers of normal babies and those hospitalized in NICU have reported the negative impact of this pandemic on social and family relationships and the motherhood role, and this negative impact was more prominent among mothers with babies hospitalized in NICU (Bin-Nun et al., 2021). The presence and active participation of parents in the care of infants are essential for the infant’s health and wellbeing of the parents. Such aspects of care should always be considered, and adequate psychological support should be provided to parents if restrictions must be re-imposed (Bembich et al., 2020; Carter et al., 2021).
The results of the present study indicated that maternal role attainment improves with higher parity rates. Consistent with this result, it has been shown that most primiparous women are not ready to face maternal role (Ruchala & James, 1997). A positive correlation between maternal confidence and parity was observed in the Liu study (Liu et al., 2012b). Knowledge and skill are requirements of maternal role attainment. Mothers should know infants’ normal growth and development and have information regarding their child’s unique crying patterns, sleeping, feeding, and other behaviors. The multipara mothers experience these issues, and the inexperienced primiparas have more concerns about maternal attainment (Hung, 2007).
The findings showed that maternal role attainment improves with more children. The experiences of first-time mothers are generally different from the experiences of mothers with more children (Black et al., 2009). These mothers are not adjusted to their new maternal role in the early postpartum period and need constant learning and adaptation (Shrestha et al., 2019). Prior experience caring for babies is reported to affect maternal confidence (Maehara et al., 2016). It seems that increasing the children number will improve maternal role attainment related to increasing experiences, competency, and confidence. The present study indicated that maternal role attainment was enhanced with increased gestational age. Consistent with this result, Ahmadpour et al. study also shows that maternal role adaptation and gestational age have a significant relationship (Ahmadpour et al., 2022). The findings also show that maternal role attainment improves with the increase in the neonate’s birth weight. Traditional methods of caring for preterm infants in the incubator led to the separation of infants from their mothers and defect in maternal role identity (Badiee et al., 2014). Consistent with this result, another study shows a positive relationship between maternal role adaptation and neonatal birth weight (Rajabi et al., 2018).
The cross-sectional design and convenience sampling are among the limitations of the current study, which reduce the generalizability of the findings. Therefore, it is better to conduct future studies using longitudinal designs that separate the possible stress and anxiety caused by the admission of a newborn in NICU from psychological problems caused by exposure to the Coronavirus and also by using random sampling. Also, fear and anxiety are subjective concepts, and evaluating them objectively has shortcomings. The self-report method has restrictions to reject the possibility that participants respond under the influence of social desirability factors.
5. Conclusion
This study determined the relationship between maternal fear and anxiety of COVID-19 and maternal role attainment in Iranian mothers whose preterm neonates were admitted to the NICU; the results indicated that the mother’s anxiety and fear were at a high level and there were weak significant positive relationships between maternal role attainment and the mentioned variables. The results highlight the strong need to evaluate the mental health of these mothers during the COVID-19 pandemic. Healthcare providers should always be aware of effective interventions as much as possible and utilize strategies to support mothers with preterm infants in this pandemic and potential future health crises.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Institutional Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.285). The research aims and the confidentiality of the data were explained, and written informed consent was obtained from participants.
Funding
This study was funded and supported by Iran University of Medical Sciences (Grant No.: 1400-2-3-21570).
Authors' contributions
Conceptualization, writing the initial draft, review, and editing: Mona Alinejad-Naeini and Farshad Heidari-Beni; Methodology and data analysis: Farshad Heidari-Beni; Data collection: Mona Alinejad-Naeini and Parvaneh Zamani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate Iran University of Medical Sciences's financial support and the mothers who participated in this study.
References
Abasi, I., et al., 2021. Psychometric Properties of Coronavirus Anxiety Scale in Iranian population. Iranian Journal of Psychiatry and Behavioral Sciences, 15(4), pp. e112707. [DOI:10.5812/ijpbs.112707]
Abedzadeh-Kalahroudi, M., et al., 2021. [Anxiety and perceived stress of pregnant women towards COVID-19 disease and its related factors in Kashan (2020) (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility, 24(5), pp. 8-18. [Link]
Ahmadpour, P., et al., 2022. Predictors of maternal role adaptation in Iranian women: A cross-sectional study. BMC Pregnancy and Childbirth, 22(1), pp. 367. [DOI:10.1186/s12884-022-04702-2] [PMID] [PMCID]
Ahorsu, D. K., et al., 2022. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 20(3), pp. 1537–45. [PMID]
Alfaraj, S. H., Al-Tawfiq, J. A. & Memish, Z. A., 2019. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: Report of two cases & review of the literature. Journal of Microbiology, Immunology and Infection, 52(3), pp. 501-3. [DOI:10.1016/j.jmii.2018.04.005]
Asaadi, M. & Daliri, H., 2021. [Evaluating the effect of poverty and economic inequality on the corona pandemic in Iran and the world (Persian)]. Journal of Health Administration, 24(2), pp. 20-32. [Link]
Badiee, Z., Faramarzi, S. & MiriZadeh, T., 2014. The effect of kangaroo mother care on mental health of mothers with low birth weight infants. Advanced Biomedical Research, 3, pp. 214.[DOI:10.4103/2277-9175.143262] [PMID] [PMCID]
Bassetti, M., Vena, A. & Giacobbe, D. R., 2020. The novel Chinese coronavirus (2019‐nCoV) infections: Challenges for fighting the storm. European Journal of Clinical Investigation, 50(3), pp. e13209. [DOI:10.1111/eci.13209]
Bembich, S., et al., 2020. Parents experiencing NICU visit restrictions due to COVID‐19 pandemic. Acta Paediatrica (Oslo, Norway: 1992), 110(3), pp. 940–1. [DOI:10.1111/apa.15620] [PMID] [PMCID]
Bergman, N. J., etal., 2019. Nurturescience versus neuroscience: A case for rethinking perinatal mother-infant behaviors and relationship. Birth Defects Research, 111(15), pp. 1110–27.[DOI:10.1002/bdr2.1529] [PMID]
Bin-Nun, A., et al., 2021. Infant delivery and maternal stress during the COVID-19 pandemic: A comparison of the well-baby versus neonatal intensive care environments. Journal of Perinatology, 41(11), pp. 2614–20. [DOI:10.1038/s41372-021-01016-7] [PMID] [PMCID]
Black, B. P., Holditch-Davis, D. & Miles, M. S., 2009. Life course theory as a framework to examine becoming a mother of a medically fragile preterm infant. Research in Nursing & Health, 32(1), pp. 38-49. [DOI:10.1002/nur.20298] [PMID] [PMCID]
Brooks, S. K., et al., 2020. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227),pp. 912–20. [DOI:10.1016/S0140-6736(20)30460-8] [PMID]
Buekens, P., et al., 2020. A call for action for COVID-19 surveillance and research during pregnancy. The Lancet. Global Health, 8(7), pp. e877–8. [DOI:10.1016/S2214-109X(20)30206-0] [PMID]
Carter, B. S., Willis, T. & Knackstedt, A., 2021. Neonatal family-centered care in a pandemic. Journal of Perinatology, 41(5), pp. 1177–9. [DOI:10.1038/s41372-021-00976-0] [PMID] [PMCID]
Cavicchiolo, M. E., et al., 2020. Managing a tertiary‐level NICU in the time of COVID‐19: Lessons learned from a high‐risk zone. Pediatric Pulmonology, 55(6), pp. 1308–10. [DOI:10.1002/ppul.24788] [PMID] [PMCID]
Cucinotta, D. & Vanelli, M., 2020. WHO declares COVID-19 a pandemic. Acta Bio-Medica: Atenei Parmensis, 91(1), pp. 157–60. [PMID]
Dadfar, M., Mahoghegh, F. & Eslami, M., 2021. The Fear of COVID-19 Scale (FCV-19S): A study of Iranian University Students. Mankind Quarterly, 61(3). [DOI:10.46469/mq.2021.61.3.19]
Dekel, S., et al., 2019. Is childbirth-induced PTSD associated with low maternal attachment? Archives of Women’s Mental Health, 22(1), pp. 119–22. [DOI:10.1007/s00737-018-0853-y] [PMID]
Eghbali Babadi, S., Namnabati, M. & Hosseini, S. M., 2021. The psychological impact of COVID-19 on mothers with premature infants. Evidence Based Care, 11(3), pp. 60-7. [DOI:10.22038/EBCJ.2021.61349.2598]
Erdei, C. & Liu, C. H., 2020. The downstream effects of COVID-19: A call for supporting family wellbeing in the NICU. Journal of Perinatology, 40(9), pp. 1283–5. [DOI:10.1038/s41372-020-0745-7] [PMID] [PMCID]
Fallon, V., et al., 2021. Postpartum-specific anxiety and maternal bonding: further evidence to support the use of childbearing specific mood tools. Journal of Reproductive and Infant Psychology, 39(2), pp. 114–24. [DOI:10.1080/02646838.2019.1680960] [PMID]
Fouquier, K. F., 2013. State of the science: Does the theory of maternal role attainment apply to African American motherhood? Journal of Midwifery & Women’s Health, 58(2), pp. 203–10. [DOI:10.1111/j.1542-2011.2012.00206.x] [PMID]
Heydarpour, S., et al., 2016. Developing and measuring psychometric properties of “maternal role adaptation instrument in mothers of preterm infants admitted to the neonatal intensive care unit. Journal of Clinical Research in Paramedical Sciences, 5(3), pp. e81495. [Link]
Hillier, K. M. & Greig, C. J., 2020. Motherhood and mothering during COVID-19: A gendered intersectional analysis of caregiving during the global pandemic within a Canadian context. Journal of Mother Studies, 5(1). [Link]
Hung, C. H., 2007. The psychosocial consequences for primiparas and multiparas. The Kaohsiung Journal of Medical Sciences, 23(7), pp. 352-360. [DOI:10.1016/S1607-551X(09)70421-8]
Jungari, S., 2020. Maternal mental health in India during COVID-19. Public Health, 185, pp. 97-8. [DOI:10.1016/j.puhe.2020.05.062] [PMID] [PMCID]
Karimi, L., et al., 2021. [Relationship between social support and anxiety caused by COVID-19 in pregnant women (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility, 23(10), pp. 9-17. [DOI:10.22038/IJOGI.2020.17482]
Khalesi, Z. B., et al., 2021. Determinants of maternal role adaptation in mothers with preterm neonates. JBRA Assisted Reproduction, 25(3), pp. 434–8. [DOI:10.5935/1518-0557.20200108] [PMID] [PMCID]
Kordi, M., et al., 2017. The effect of maternal role training program on role attainment and maternal role satisfaction in nulliparous women with unplanned pregnancy. Journal of Education and Health Promotion, 6, pp. 61. [PMID]
Lee, S. A., 2020. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death studies, 44(7), pp. 393–401. [DOI:10.1080/07481187.2020.1748481] [PMID]
Lemmon, M. E., et al., 2020. Beyond the first wave: Consequences of COVID-19 on high-risk infants and families. American Journal of Perinatology, 37(12), pp. 1283–8. [DOI:10.1055/s-0040-1715839] [PMID] [PMCID]
Liu, C. C., et al., 2012. Effects of maternal confidence and competence on maternal parenting stress in newborn care. Journal of Advanced Nursing, 68(4), pp. 908-18. [PMID]
Liu, C. H., Erdei, C. & Mittal, L., 2021. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Research, 295, pp. 113552. [DOI:10.1016/j.psychres.2020.113552] [PMID] [PMCID]
Liu, X., et al., 2012. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry, 53(1), pp. 15-23. [PMID] [PMCID]
Maehara, K., et al., 2016. Factors affecting maternal confidence among older and younger Japanese primiparae at one month post-partum. Japan Journal of Nursing Science, 13(4), pp. 424-36. [DOI:10.1111/jjns.12123]
Magano, J., et al., 2021. Validation and psychometric properties of the Portuguese version of the Coronavirus Anxiety Scale (CAS) and fear of COVID-19 Scale (FCV-19S) and associations with travel, tourism and hospitality. International Journal of Environmental Research and Public Health, 18(2), pp. 427.[DOI:10.3390/ijerph18020427] [PMID] [PMCID]
Mayopoulos, G. A., et al., 2021. COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. Journal of Affective Disorders, 282, pp. 122-5. [DOI:10.1016/j.jad.2020.12.101] [PMID] [PMCID]
McIntosh, K., Hirsch, M. S. & Bloom, A., 2020. Coronavirus disease 2019 (COVID-19). UpToDate Hirsch MS Bloom, 5(1), pp. 873. [Link]
Mertens, G., et al., 2020. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74, pp. 102258. [DOI:10.1016/j.janxdis.2020.102258] [PMID] [PMCID]
Moyer, C. A., et al., 2020. Pregnancy-related anxiety during COVID-19: A nationwide survey of 2740 pregnant women. Archives of Women’s Mental Health, 23(6), pp. 757–65. [DOI:10.1007/s00737-020-01073-5] [PMID] [PMCID]
Nolvi, S., et al., 2016. Maternal postnatal psychiatric symptoms and infant temperament affect early mother-infant bonding. Infant Behavior and Development, 43, pp. 13-23 [DOI:10.1016/j.infbeh.2016.03.003] [PMID]
Pearson, C., et al., 2022. Understanding the impact of COVID-19 on physician moms. Disaster Medicine and Public Health Preparedness, 16(5), pp. 2049–55. [DOI:10.1017/dmp.2021.49] [PMID] [PMCID]
Polloni, L., et al., 2021. Psychological wellbeing of parents with infants admitted to the neonatal intensive care unit during SARS-CoV-2 pandemic. Children, 8(9), pp. 755. [DOI:10.3390/children8090755] [PMID] [PMCID]
Rajabi, A., et al., 2018. Evaluation of maternal role adaptation in mothers with late-preterm infants and its related factors. Preventive Care in Nursing & Midwifery Journal, 8(1), pp. 1-10. [Link]
Rogers, C. E., et al., 2013. Identifying mothers of very preterm infants at-risk for postpartum depression and anxiety before discharge. Journal of Perinatology, 33(3), pp. 171–6. [DOI:10.1038/jp.2012.75] [PMID] [PMCID]
Rothe, C., et al., 2020. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. The New England Journal of Medicine, 382(10), pp. 970–1. [DOI:10.1056/NEJMc2001468] [PMID] [PMCID]
Ruchala, P. L. & James, D. C., 1997. Social support knowledge of infant development, and maternal confidence among adolescent and adult mothers. Journal of Obstetric, Gynecologic & Neonatal Nursing, 26(6), pp. 685-9. [DOI:10.1111/j.1552-6909.1997.tb02743.x] [PMID]
Saccone, G., et al., 2020. Psychological impact of coronavirus disease 2019 in pregnant women. American Journal of Obstetrics & Gynecology, 223(2), pp. 293–5. [DOI:10.1016/j.ajog.2020.05.003] [PMID] [PMCID]
Salimi, R., Gomar, R. & Heshmati, B., 2020. The COVID-19 outbreak in Iran. Journal of Global Health, 10(1), pp. 010365. [DOI:10.7189/jogh.10.010365] [PMID] [PMCID]
Sansom, L., 2010. Confident parenting-A book proposal [MA thesis]. Pennsylvania: University of Pennsylvania. [Link]
Schwartz, D. A. & Graham, A. L., 2020. Potential maternal and infant outcomes from coronavirus 2019-nCoV (SARS-CoV-2) infecting pregnant women: Lessons from SARS, MERS, and other human coronavirus infections. Viruses, 12(2), pp. 194.[DOI:10.3390/v12020194] [PMID] [PMCID]
Shrestha, S., et al., 2019. Maternal role: A concept analysis. Journal of Midwifery and Reproductive Health, 7(3), pp. 1732-41. [Link]
Su, T. P., et al., 2007. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. Journal of Psychiatric Research, 41(1-2), pp. 119–30. [DOI:10.1016/j.jpsychires.2005.12.006] [PMID] [PMCID]
Sullivan, R., et al., 2011. Infant bonding and attachment to the caregiver: Insights from basic and clinical science. Clinics in Perinatology, 38(4), pp. 643–55. [DOI:10.1016/j.clp.2011.08.011] [PMID] [PMCID]
Suzuki, S., 2022. Psychological status of postpartum women under the COVID-19 pandemic in Japan. The Journal of Maternal-Fetal & Neonatal Medicine, 35(9), pp. 1798–800. [DOI:10.1080/14767058.2020.1763949] [PMID]
Tandberg, B. S., et al., 2019. Parent psychological wellbeing in a single-family room versus an open bay neonatal intensive care unit. PloS one, 14(11), pp. e0224488. [DOI:10.1371/journal.pone.0224488] [PMID] [PMCID]
Taubman-Ben-Ari, O., et al., 2009. The transition to motherhood-A time for growth. Journal of Social and Clinical Psychology, 28(8), pp. 943-70. [DOI:10.1521/jscp.2009.28.8.943]
Thapa, S. B., et al., 2020. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstetricia et Gynecologica Scandinavica, 99(7), pp. 817–8. [DOI:10.1111/aogs.13894] [PMID] [PMCID]
Tolja, R., Nakić Radoš, S. & Anđelinović, M., 2020. The role of maternal mental health, infant temperament, and couple’s relationship quality for mother-infant bonding. Journal of Reproductive and Infant Psychology, 38(4), pp. 395-407. [DOI:10.1080/02646838.2020.1733503] [PMID]
Treyvaud, K., et al., 2014. Very preterm birth influences parental mental health and family outcomes seven years after birth. The Journal of Pediatrics, 164(3), pp. 515–21. [DOI:10.1016/j.jpeds.2013.11.001] [PMID] [PMCID]
Treyvaud, K., et al., 2019. A multilayered approach is needed in the NICU to support parents after the preterm birth of their infant. Early Human Development, 139, pp. 104838. [DOI:10.1016/j.earlhumdev.2019.104838] [PMID]
Uzun, A., et al., 2021. Investigating of fear of COVID-19 after pregnancy and association with breastfeeding. Journal of Ideas in Health, 4(1), pp. 327-33. [DOI:10.47108/jidhealth.Vol4.Iss1.98]
Verma, S., et al., 2020. Neonatal intensive care unit preparedness for the Novel Coronavirus Disease-2019 pandemic: A New York City hospital perspective. Current Problems in Pediatric and Adolescent Health Care, 50(4), pp. 100795. [DOI:10.1016/j.cppeds.2020.100795] [PMID] [PMCID]
Wachs, T. D., Black, M. M. & Engle, P. L., 2009. Maternal depression: A global threat to children’s health, development, and behavior and to human rights. Child Development Perspectives, 3(1), pp. 51-9. [DOI:10.1111/j.1750-8606.2008.00077.x]
Zanardo, V., et al., 2020. Psychological impact of COVID‐19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. International Journal of Gynecology & Obstetrics, 150(2), pp. 184–8. [DOI:10.1002/ijgo.13249] [PMID] [PMCID]
Zeng, L., et al., 2020. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatrics, 174(7), pp. 722–5. [PMID]
Zhu, X., et al., 2008. Changes in emotion of the Chinese public in regard to the SARS period. Social Behavior and Personality: An International Journal, 36(4), pp. 447-54. [DOI:10.2224/sbp.2008.36.4.447]
The novel Coronavirus 2019 (COVID-19) outbreak started in China in 2019 and quickly became a menace to global health. The World Health Organization (WHO) has introduced COVID-19 as an international public health emergency (Cucinotta & Vanelli, 2020; Wachs et al., 2009). COVID-19 pandemic is a serious public health emergency, especially in populations that health systems are vulnerable to crisis (Rothe et al., 2020; Mcintosh et al., 2020). The official announcement of the disease outbreak in Iran also caused panic and public concern (Salimi et al., 2020). Mothers are concerned about their children being infected with this virus. Preterm neonates have an immature immune system, which puts them at greater risk for severe infections. Cases of neonatal pneumonia were identified in newborns whose mothers were infected with COVID-19 (Zeng et al., 2020). While mothers and their neonates were not initially identified as high-risk populations, evidence from previous viral outbreaks suggests a risk of adverse outcomes for both mother and infant (Alfaraj et al., 2019). This possibility has given rise to pandemic policies, such as observing social distancing and preventing vertical infection, as well as establishing special considerations to protect the health of mothers and babies and the need to consider unwanted consequences for them (Buekens et al., 2020). The neonatal intensive care unit (NICU) environment appears to facilitate the transmission of the COVID-19 virus, and given the role of asymptomatic persons in the spread of the virus, these dangers cannot be undervalued (Cavicchiolo et al., 2020). Studies on different types of transmission, clinical spectrum, and duration of virus excretion in COVID-19 patients are ongoing. In the absence of sufficient evidence, it is recommended that a cautious approach be taken to close contact between an asymptomatic, suspected, or established COVID-19 mother and her infant (Verma et al., 2020).
The COVID-19 pandemic will negatively affect maternal psychological health, highlighting the need for intervention (Saccone et al., 2020). Several studies have been conducted on the effects of quarantine on maternal psychological health, which have stated a high prevalence of emotional symptoms (Brooks et al., 2020; Liu et al., 2012a). Women are more psychologically affected by the same pandemics, such as severe acute respiratory syndrome and middle eastern respiratory syndrome (Schwartz & Graham, 2020). Concerns related to contracting COVID-19 start from the first hours of birth and continue until the days after delivery, making mothers an emotionally susceptible group (Thapa et al., 2020). Recently, several studies have indicated the negative effect of COVID-19 on maternal psychological health (Zanardo et al., 2020; Suzuki, 2020). Maternal psychological wellbeing difficulties are believed to be related to short-term and long-term risks to the mother-newborn relationship, especially the mother-newborn attachment (Nolvi et al., 2016; Fallon et al., 2021; Tolja et al., 2020). According to the mentioned reasons, healthcare providers must pay more attention to the psychological health of mothers after childbirth (Bassetti et al., 2020). Mothers with premature babies must cope with the unknown stresses of the postpartum period and endure the pressures caused by the pandemic during the critical care period for their children (Dekel et al., 2019). Mothers may also face broader challenges that undermine their ability to care for high-risk infants. Disruption of the social support structure due to the need for social distance may increase the mother’s sense of isolation and symptoms of anxiety and depression (Lemmon et al., 2020). Some studies about Coronavirus pandemic indicated fear, anxiety, depression and the symptoms caused by them through self-reporting and clinical evaluations in the postpartum period (Saccone et al., 2020; Jungari, 2020).
The term “maternal role attainment” is part of the transition process that leads to acquiring maternal role identity. During this period, the mother can fulfill her maternal role and behave appropriately for the determined maternal role (Fouquier, 2013). Achieving the maternal role is one of mothers’ greatest fundamental and significant roles (Sansom, 2010). Mother, neonate, and environment are variables associated with the maternal role. Maternal variables such as marital status, maternal age, maternal confidence, birth experience, stress, and emotional state influence maternal role attainment (Kordi et al., 2017). However, the effects of COVID-19 on maternal stress due to childbirth and subsequent maternal complications are unknown (Mayopoulos et al., 2021). Despite the vulnerability of mothers with preterm infants during the COVID-19 pandemic, no study has been conducted on the fear and anxiety of mothers with preterm newborns admitted to NICU in Iran. Also, the effect of COVID-19 disease on mother-infant relationships and maternal role attainment is unclear. Accordingly, our study will determine the relationship of maternal fear and anxiety about COVID-19 with maternal role development in Iranian mothers with premature neonates admitted to NICUs.
2. Materials and Methods
This descriptive correlational study was conducted in three level-III NICUs affiliated with the Iran University of Medical Sciences (IUMS) in Tehran City, Iran, from June 2021 to July 2022. NICUs in Iran comprise two sections: NICU and post-NICU. Preterm newborns after birth are admitted to the NICU due to dangerous health situations and the need for intensive medical care. Preterm newborns are transported to the post-NICU for continuation of care after recovering and stabilizing their condition. In both areas, access is restricted to prevent transmission of infection, and only parents of preterm neonates can visit their children whenever they wish. The basic principles and policies are the same in both areas.
Sampling was performed from both NICU and post-NICU. This study sample was mothers with their premature neonate in the NICU who were recruited via convenience sampling. The sample size was calculated to be 211 at a 95% confidence interval and 80% test power. Also, for the relationship between maternal role, fear, and anxiety of COVID-19 to be considered statistically significant (considering the absence of a similar study), the amount of the correlation coefficient was considered equal to 0.2. After inserting the values in Equations 1 and 2, the sample size was estimated as follows:

The inclusion criteria were being mothers of neonates admitted to NICU, having a neonate with 28–37 weeks gestational age, having the ability to read and write in Persian, having no previous experience in the NICU, lacking experience of a dead neonate, and passed at least 3 days of neonate admission to NICU. The exclusion criteria were having a positive PCR test, cognitive impairment, having severe gynecologic problems before, during, or after delivery, drug abuse, and the use of antidepressants. Convenience sampling was used to select the eligible subjects. For this purpose, the researcher visited one of the hospitals every day and invited the mothers who met the inclusion criteria to the study until the sample size was achieved.
The data were collected using a sociodemographic questionnaire, the Coronavirus anxiety scale (CAS), the fear of COVID-19 scale, and the maternal role adaptation scale in NICUs.
The sociodemographic questionnaire consisted of the mother’s characteristics, including age, occupation, education level, economic status, and neonatal characteristics, including neonate’s sex, gestational age, corrected age, and neonatal birth weight that the researcher completed.
CAS scale was designed by Lee (2020). This scale has five items that measure distinct behavioral, cognitive, emotional, and physiological responses to COVID-19 anxiety. Each item of the CAS is rated on a 5-point Likert scale from 0 (not at all) to 4 (nearly every day) based on experiences over the past two weeks. A CAS total score ≥9 indicates probable dysfunctional Coronavirus-related anxiety. This scale has high reliability (α=0.93) (Lee, 2020). Abasi et al. evaluated the psychometric properties of CAS in Iran. The results demonstrated that the Persian version of the scale (P-CAS) had a good internal consistency (α=0.80) (Abasi et al., 2021). The Cronbach α coefficient of the scale in this study was 0.911.
Fear of COVID-19 scale was developed to complement the clinical efforts in preventing the spread of and treating COVID-19 cases (Ahorsu et al., 2020). This scale has 7 items, and respondents express their opinion using a five-point Likert scale. Each item was rated from 1 to 5, and the total would be from 7 to 35. A higher score indicates a greater fear of the Coronavirus. The internal consistency (α=0.82) and test-retest reliability (by intraclass correlation coefficient) (ICC=0.72) of the scale were satisfactory (Ahorsu et al., 2020). The robust psychometric properties of this instrument were also confirmed in Portugal with composite reliability (CR=0.88) and internal consistency (Cronbach α coefficient=0.82). They showed it is a valid and reliable tool to assess the fear of COVID-19 among the general population (Magano et al., 2021). Psychometric properties of the Persian version of the scale were confirmed, and its Cronbach α coefficient was reported as 0.87 (Dadfar et al., 2021). The Cronbach α coefficient for this scale in the present study was 0.84.
The maternal role adaptation scale in NICUs was designed by Heydarpour et al. (2016) and contained 32 items and 6 dimensions: Participation in care (14 items), self-efficacy (6 items), distant mothering (3 items), uncertainty (4 items), interaction (3 items), and growth and development (2 items). They are scored on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The total score is calculated by the sum of the dimensions’ scores ranging from 32 to 160, and the higher scores indicate better maternal role attainment. The scale’s reliability has been approved with Cronbach α and intraclass correlation coefficient as 0.77 and 0.81, respectively. This tool is relatively simple, and mothers of preterm babies can complete it within 10 minutes (Heydarpour et al., 2016). The present study obtained a Cronbach α coefficient of 0.801 for the maternal role adaptation scale, confirming its reliability.
After receiving the letter of introduction from IUMS, the data were collected in different shift works according to the predetermined schedule. The mothers had enough time to complete the questionnaires through self-reporting. Data were collected in a relaxed and safe place without compromising the care of the baby. SPSS software, version 23 was used for all statistical analyses. Descriptive statistics were used to assess the frequency (percentage) and Mean±SD of participants’ characteristics. The Kolmogorov-Smirnov test was used to determine data distribution, indicating all the data have a normal distribution. Accordingly, the parametric inferential statistics consisting of the independent samples t-test, one-way ANOVA, and the Pearson correlation coefficient were used to assess the relationship between demographic variables and anxiety, fear, and maternal role attainment. The Pearson correlation coefficient test evaluated the associations between anxiety, fear, and maternal role attainment.
3. Results
In this study, 211 mothers with preterm neonates participated. Most mothers had secondary education (66.82%), were second para (41.2%), had a history of Coronavirus infection (76.8%), had received the COVID-19 vaccine (65.9%), had not any abortion (65.8%), and were housewives (83.4%). The characteristics of the mothers and their neonates are presented in Table 1.

There were statistically significant relationships between para (P=0.006), children’s number (P<0.001), neonate’s birth weight (P<0.001), neonatal gestational age (P=0.009), and maternal role attainment. Also, none of the demographic variables had a significant relationship with anxiety and fear (P>0.05).
The mean score of the mothers’ anxiety was 11.44±3.19, and 59.2% had not experienced Coronavirus-related anxiety. The mean fear and maternal role attainment score was 26.49±5.92 and 57.61±11.95, respectively (Table 2).

The Pearson correlation coefficient was used to assess the linear relationship between the variables, and the results indicated a positive and significant relationship between anxiety and fear (r=0.385, P<0.001). Also, there were positive and significant relationships between anxiety and maternal role attainment (r=0.213, P=0.002), and dimensions of participation in care (r=0.163, P=0.018), distant mothering (r=0.255, P=0.001), interaction (r=0.188, P=0.006), and growth and development (r=0.192, P=0.005). There were also positive and significant relationships between fear and maternal role attainment (r=0.204, P=0.003) and the dimensions of participation in care (r=0.219, P=0.001) and growth and development (r=0.173, P=0.012) (Table 3).
4. Discussion
Many mothers experience psychological symptoms such as acute stress, anxiety, depression, and fear while their babies are admitted to NICU (Rogers et al., 2013; Treyvaud et al., 2014). These problems have recently called for increased psychological support for families with neonates admitted to NICUs (Treyvaud et al., 2019). The COVID-19 pandemic is acting as a great new environmental stressor, adding to the pre-existing psychological distress of these mothers (Erdei & Liu, 2020). This study investigated the relationship between maternal fear and anxiety about COVID-19 and maternal role attainment in Iranian mothers with preterm neonates admitted to NICUs.
The findings of this study indicated that the mean scores of COVID-19 anxiety and fear in mothers with preterm neonates were at a high level. Some studies on pregnant women have reported the same levels of COVID-19 anxiety (Karimi et al., 2021; Abedzadeh-Kalahroudi et al., 2021; Moyer et al., 2020). Pregnancy, childbirth, postpartum, and the period of adjustment with mothering are the most sensitive times for mothers physically and mentally. Therefore, there may be a risk of mental disorders in these episodes. The negative view and uncertainty about the baby’s health caused by the COVID-19 pandemic increase the mother’s fear and anxiety (Mertens et al., 2020). A study of mothers with neonates admitted to the NICU found that concerns related to COVID-19 were strongly associated with mental health symptoms in this population (Lemmon et al., 2020). A study investigating the psychological effect of COVID-19 on mothers with premature babies reported that the average overall score for COVID-19 anxiety was mild (Eghbali Babadi et al., 2021). A study conducted during the COVID-19 outbreak found that over half of parents whose babies were admitted to the NICU scored higher than the cut-off point on anxiety (Polloni et al., 2021).
As shown in previous pandemics, outbreaks of infectious diseases increased fear in society (Su et al., 2007; Zhu et al., 2008). Fear is an adaptive defense mechanism in humans that is essential for survival and involves several biological processes preparing to respond to potentially dangerous events. However, when it is chronic or disproportionate, it can cause psychiatric disorders (Su et al., 2007). The fear is increased among women during the COVID-19 outbreak because of concern about their children’s health (Pearson et al., 2021). Studies on maternal fear of COVID-19 are limited. In a study by Uzun et al. which examined postpartum COVID-19 fear and its association with breastfeeding, mothers scored high on COVID-19 fear (Uzun et al., 2021). Prolonged separation from the infant leads to impairment in the parent/child relationship, a substantial neurological factor for the infant’s health and development (Tandberg et al., 2019; Erdei & Liu, 2020).
Conversely, the interaction between parents and their neonate lead to infant development, while separation may cause distress and fear in both (Bergman et al., 2019). It is shown that worry about the baby contracting COVID-19, along with the social restrictions caused by preventive measures, negatively affects the thoughts and feelings of mothers and increases psychological symptoms such as anxiety, depression, and distress (Zanardo et al., 2020; Liu et al., 2021). The research results also showed a direct and significant relationship between anxiety and fear of COVID-19 and maternal role attainment. To situate motherhood in the global COVID-19 pandemic context, one must first consider motherhood in a broader social context (Hillier & Greig, 2020). It seems that due to the effects of poverty and social inequality on the pandemic in Iran and the world (Asaadi & Daliri, 2021), as well as mothers’ perception of the uncontrollability of the pandemic, these mothers have experienced more fear and anxiety and therefore put a lot of effort into taking care of their babies. According to the results, the mother’s participation in childcare has the highest score, while the growth and development dimension has the lowest score. The results of another study on the determinants of a mother’s role adaptation in mothers with premature babies also showed that participation in the childcare dimension has the highest score (Khalesi et al., 2021). The mother’s presence and the repeated hugging of the baby can make a stronger parent-child attachment and become the basis for subsequent interactions that provide the possibility of further child development. In addition, it strengthens the feeling of motherhood and leads to greater achievement of maternal role (Sullivan et al., 2011). Another study shows that mothers with a passive role in caring for their infants, whose participation is low, are less adapted to maternal roles) (Taubman-Ben-Ari et al., 2009). It has been shown that most mothers of normal babies and those hospitalized in NICU have reported the negative impact of this pandemic on social and family relationships and the motherhood role, and this negative impact was more prominent among mothers with babies hospitalized in NICU (Bin-Nun et al., 2021). The presence and active participation of parents in the care of infants are essential for the infant’s health and wellbeing of the parents. Such aspects of care should always be considered, and adequate psychological support should be provided to parents if restrictions must be re-imposed (Bembich et al., 2020; Carter et al., 2021).
The results of the present study indicated that maternal role attainment improves with higher parity rates. Consistent with this result, it has been shown that most primiparous women are not ready to face maternal role (Ruchala & James, 1997). A positive correlation between maternal confidence and parity was observed in the Liu study (Liu et al., 2012b). Knowledge and skill are requirements of maternal role attainment. Mothers should know infants’ normal growth and development and have information regarding their child’s unique crying patterns, sleeping, feeding, and other behaviors. The multipara mothers experience these issues, and the inexperienced primiparas have more concerns about maternal attainment (Hung, 2007).
The findings showed that maternal role attainment improves with more children. The experiences of first-time mothers are generally different from the experiences of mothers with more children (Black et al., 2009). These mothers are not adjusted to their new maternal role in the early postpartum period and need constant learning and adaptation (Shrestha et al., 2019). Prior experience caring for babies is reported to affect maternal confidence (Maehara et al., 2016). It seems that increasing the children number will improve maternal role attainment related to increasing experiences, competency, and confidence. The present study indicated that maternal role attainment was enhanced with increased gestational age. Consistent with this result, Ahmadpour et al. study also shows that maternal role adaptation and gestational age have a significant relationship (Ahmadpour et al., 2022). The findings also show that maternal role attainment improves with the increase in the neonate’s birth weight. Traditional methods of caring for preterm infants in the incubator led to the separation of infants from their mothers and defect in maternal role identity (Badiee et al., 2014). Consistent with this result, another study shows a positive relationship between maternal role adaptation and neonatal birth weight (Rajabi et al., 2018).
The cross-sectional design and convenience sampling are among the limitations of the current study, which reduce the generalizability of the findings. Therefore, it is better to conduct future studies using longitudinal designs that separate the possible stress and anxiety caused by the admission of a newborn in NICU from psychological problems caused by exposure to the Coronavirus and also by using random sampling. Also, fear and anxiety are subjective concepts, and evaluating them objectively has shortcomings. The self-report method has restrictions to reject the possibility that participants respond under the influence of social desirability factors.
5. Conclusion
This study determined the relationship between maternal fear and anxiety of COVID-19 and maternal role attainment in Iranian mothers whose preterm neonates were admitted to the NICU; the results indicated that the mother’s anxiety and fear were at a high level and there were weak significant positive relationships between maternal role attainment and the mentioned variables. The results highlight the strong need to evaluate the mental health of these mothers during the COVID-19 pandemic. Healthcare providers should always be aware of effective interventions as much as possible and utilize strategies to support mothers with preterm infants in this pandemic and potential future health crises.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Institutional Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.285). The research aims and the confidentiality of the data were explained, and written informed consent was obtained from participants.
Funding
This study was funded and supported by Iran University of Medical Sciences (Grant No.: 1400-2-3-21570).
Authors' contributions
Conceptualization, writing the initial draft, review, and editing: Mona Alinejad-Naeini and Farshad Heidari-Beni; Methodology and data analysis: Farshad Heidari-Beni; Data collection: Mona Alinejad-Naeini and Parvaneh Zamani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate Iran University of Medical Sciences's financial support and the mothers who participated in this study.
References
Abasi, I., et al., 2021. Psychometric Properties of Coronavirus Anxiety Scale in Iranian population. Iranian Journal of Psychiatry and Behavioral Sciences, 15(4), pp. e112707. [DOI:10.5812/ijpbs.112707]
Abedzadeh-Kalahroudi, M., et al., 2021. [Anxiety and perceived stress of pregnant women towards COVID-19 disease and its related factors in Kashan (2020) (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility, 24(5), pp. 8-18. [Link]
Ahmadpour, P., et al., 2022. Predictors of maternal role adaptation in Iranian women: A cross-sectional study. BMC Pregnancy and Childbirth, 22(1), pp. 367. [DOI:10.1186/s12884-022-04702-2] [PMID] [PMCID]
Ahorsu, D. K., et al., 2022. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 20(3), pp. 1537–45. [PMID]
Alfaraj, S. H., Al-Tawfiq, J. A. & Memish, Z. A., 2019. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: Report of two cases & review of the literature. Journal of Microbiology, Immunology and Infection, 52(3), pp. 501-3. [DOI:10.1016/j.jmii.2018.04.005]
Asaadi, M. & Daliri, H., 2021. [Evaluating the effect of poverty and economic inequality on the corona pandemic in Iran and the world (Persian)]. Journal of Health Administration, 24(2), pp. 20-32. [Link]
Badiee, Z., Faramarzi, S. & MiriZadeh, T., 2014. The effect of kangaroo mother care on mental health of mothers with low birth weight infants. Advanced Biomedical Research, 3, pp. 214.[DOI:10.4103/2277-9175.143262] [PMID] [PMCID]
Bassetti, M., Vena, A. & Giacobbe, D. R., 2020. The novel Chinese coronavirus (2019‐nCoV) infections: Challenges for fighting the storm. European Journal of Clinical Investigation, 50(3), pp. e13209. [DOI:10.1111/eci.13209]
Bembich, S., et al., 2020. Parents experiencing NICU visit restrictions due to COVID‐19 pandemic. Acta Paediatrica (Oslo, Norway: 1992), 110(3), pp. 940–1. [DOI:10.1111/apa.15620] [PMID] [PMCID]
Bergman, N. J., etal., 2019. Nurturescience versus neuroscience: A case for rethinking perinatal mother-infant behaviors and relationship. Birth Defects Research, 111(15), pp. 1110–27.[DOI:10.1002/bdr2.1529] [PMID]
Bin-Nun, A., et al., 2021. Infant delivery and maternal stress during the COVID-19 pandemic: A comparison of the well-baby versus neonatal intensive care environments. Journal of Perinatology, 41(11), pp. 2614–20. [DOI:10.1038/s41372-021-01016-7] [PMID] [PMCID]
Black, B. P., Holditch-Davis, D. & Miles, M. S., 2009. Life course theory as a framework to examine becoming a mother of a medically fragile preterm infant. Research in Nursing & Health, 32(1), pp. 38-49. [DOI:10.1002/nur.20298] [PMID] [PMCID]
Brooks, S. K., et al., 2020. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227),pp. 912–20. [DOI:10.1016/S0140-6736(20)30460-8] [PMID]
Buekens, P., et al., 2020. A call for action for COVID-19 surveillance and research during pregnancy. The Lancet. Global Health, 8(7), pp. e877–8. [DOI:10.1016/S2214-109X(20)30206-0] [PMID]
Carter, B. S., Willis, T. & Knackstedt, A., 2021. Neonatal family-centered care in a pandemic. Journal of Perinatology, 41(5), pp. 1177–9. [DOI:10.1038/s41372-021-00976-0] [PMID] [PMCID]
Cavicchiolo, M. E., et al., 2020. Managing a tertiary‐level NICU in the time of COVID‐19: Lessons learned from a high‐risk zone. Pediatric Pulmonology, 55(6), pp. 1308–10. [DOI:10.1002/ppul.24788] [PMID] [PMCID]
Cucinotta, D. & Vanelli, M., 2020. WHO declares COVID-19 a pandemic. Acta Bio-Medica: Atenei Parmensis, 91(1), pp. 157–60. [PMID]
Dadfar, M., Mahoghegh, F. & Eslami, M., 2021. The Fear of COVID-19 Scale (FCV-19S): A study of Iranian University Students. Mankind Quarterly, 61(3). [DOI:10.46469/mq.2021.61.3.19]
Dekel, S., et al., 2019. Is childbirth-induced PTSD associated with low maternal attachment? Archives of Women’s Mental Health, 22(1), pp. 119–22. [DOI:10.1007/s00737-018-0853-y] [PMID]
Eghbali Babadi, S., Namnabati, M. & Hosseini, S. M., 2021. The psychological impact of COVID-19 on mothers with premature infants. Evidence Based Care, 11(3), pp. 60-7. [DOI:10.22038/EBCJ.2021.61349.2598]
Erdei, C. & Liu, C. H., 2020. The downstream effects of COVID-19: A call for supporting family wellbeing in the NICU. Journal of Perinatology, 40(9), pp. 1283–5. [DOI:10.1038/s41372-020-0745-7] [PMID] [PMCID]
Fallon, V., et al., 2021. Postpartum-specific anxiety and maternal bonding: further evidence to support the use of childbearing specific mood tools. Journal of Reproductive and Infant Psychology, 39(2), pp. 114–24. [DOI:10.1080/02646838.2019.1680960] [PMID]
Fouquier, K. F., 2013. State of the science: Does the theory of maternal role attainment apply to African American motherhood? Journal of Midwifery & Women’s Health, 58(2), pp. 203–10. [DOI:10.1111/j.1542-2011.2012.00206.x] [PMID]
Heydarpour, S., et al., 2016. Developing and measuring psychometric properties of “maternal role adaptation instrument in mothers of preterm infants admitted to the neonatal intensive care unit. Journal of Clinical Research in Paramedical Sciences, 5(3), pp. e81495. [Link]
Hillier, K. M. & Greig, C. J., 2020. Motherhood and mothering during COVID-19: A gendered intersectional analysis of caregiving during the global pandemic within a Canadian context. Journal of Mother Studies, 5(1). [Link]
Hung, C. H., 2007. The psychosocial consequences for primiparas and multiparas. The Kaohsiung Journal of Medical Sciences, 23(7), pp. 352-360. [DOI:10.1016/S1607-551X(09)70421-8]
Jungari, S., 2020. Maternal mental health in India during COVID-19. Public Health, 185, pp. 97-8. [DOI:10.1016/j.puhe.2020.05.062] [PMID] [PMCID]
Karimi, L., et al., 2021. [Relationship between social support and anxiety caused by COVID-19 in pregnant women (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility, 23(10), pp. 9-17. [DOI:10.22038/IJOGI.2020.17482]
Khalesi, Z. B., et al., 2021. Determinants of maternal role adaptation in mothers with preterm neonates. JBRA Assisted Reproduction, 25(3), pp. 434–8. [DOI:10.5935/1518-0557.20200108] [PMID] [PMCID]
Kordi, M., et al., 2017. The effect of maternal role training program on role attainment and maternal role satisfaction in nulliparous women with unplanned pregnancy. Journal of Education and Health Promotion, 6, pp. 61. [PMID]
Lee, S. A., 2020. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death studies, 44(7), pp. 393–401. [DOI:10.1080/07481187.2020.1748481] [PMID]
Lemmon, M. E., et al., 2020. Beyond the first wave: Consequences of COVID-19 on high-risk infants and families. American Journal of Perinatology, 37(12), pp. 1283–8. [DOI:10.1055/s-0040-1715839] [PMID] [PMCID]
Liu, C. C., et al., 2012. Effects of maternal confidence and competence on maternal parenting stress in newborn care. Journal of Advanced Nursing, 68(4), pp. 908-18. [PMID]
Liu, C. H., Erdei, C. & Mittal, L., 2021. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Research, 295, pp. 113552. [DOI:10.1016/j.psychres.2020.113552] [PMID] [PMCID]
Liu, X., et al., 2012. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry, 53(1), pp. 15-23. [PMID] [PMCID]
Maehara, K., et al., 2016. Factors affecting maternal confidence among older and younger Japanese primiparae at one month post-partum. Japan Journal of Nursing Science, 13(4), pp. 424-36. [DOI:10.1111/jjns.12123]
Magano, J., et al., 2021. Validation and psychometric properties of the Portuguese version of the Coronavirus Anxiety Scale (CAS) and fear of COVID-19 Scale (FCV-19S) and associations with travel, tourism and hospitality. International Journal of Environmental Research and Public Health, 18(2), pp. 427.[DOI:10.3390/ijerph18020427] [PMID] [PMCID]
Mayopoulos, G. A., et al., 2021. COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. Journal of Affective Disorders, 282, pp. 122-5. [DOI:10.1016/j.jad.2020.12.101] [PMID] [PMCID]
McIntosh, K., Hirsch, M. S. & Bloom, A., 2020. Coronavirus disease 2019 (COVID-19). UpToDate Hirsch MS Bloom, 5(1), pp. 873. [Link]
Mertens, G., et al., 2020. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74, pp. 102258. [DOI:10.1016/j.janxdis.2020.102258] [PMID] [PMCID]
Moyer, C. A., et al., 2020. Pregnancy-related anxiety during COVID-19: A nationwide survey of 2740 pregnant women. Archives of Women’s Mental Health, 23(6), pp. 757–65. [DOI:10.1007/s00737-020-01073-5] [PMID] [PMCID]
Nolvi, S., et al., 2016. Maternal postnatal psychiatric symptoms and infant temperament affect early mother-infant bonding. Infant Behavior and Development, 43, pp. 13-23 [DOI:10.1016/j.infbeh.2016.03.003] [PMID]
Pearson, C., et al., 2022. Understanding the impact of COVID-19 on physician moms. Disaster Medicine and Public Health Preparedness, 16(5), pp. 2049–55. [DOI:10.1017/dmp.2021.49] [PMID] [PMCID]
Polloni, L., et al., 2021. Psychological wellbeing of parents with infants admitted to the neonatal intensive care unit during SARS-CoV-2 pandemic. Children, 8(9), pp. 755. [DOI:10.3390/children8090755] [PMID] [PMCID]
Rajabi, A., et al., 2018. Evaluation of maternal role adaptation in mothers with late-preterm infants and its related factors. Preventive Care in Nursing & Midwifery Journal, 8(1), pp. 1-10. [Link]
Rogers, C. E., et al., 2013. Identifying mothers of very preterm infants at-risk for postpartum depression and anxiety before discharge. Journal of Perinatology, 33(3), pp. 171–6. [DOI:10.1038/jp.2012.75] [PMID] [PMCID]
Rothe, C., et al., 2020. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. The New England Journal of Medicine, 382(10), pp. 970–1. [DOI:10.1056/NEJMc2001468] [PMID] [PMCID]
Ruchala, P. L. & James, D. C., 1997. Social support knowledge of infant development, and maternal confidence among adolescent and adult mothers. Journal of Obstetric, Gynecologic & Neonatal Nursing, 26(6), pp. 685-9. [DOI:10.1111/j.1552-6909.1997.tb02743.x] [PMID]
Saccone, G., et al., 2020. Psychological impact of coronavirus disease 2019 in pregnant women. American Journal of Obstetrics & Gynecology, 223(2), pp. 293–5. [DOI:10.1016/j.ajog.2020.05.003] [PMID] [PMCID]
Salimi, R., Gomar, R. & Heshmati, B., 2020. The COVID-19 outbreak in Iran. Journal of Global Health, 10(1), pp. 010365. [DOI:10.7189/jogh.10.010365] [PMID] [PMCID]
Sansom, L., 2010. Confident parenting-A book proposal [MA thesis]. Pennsylvania: University of Pennsylvania. [Link]
Schwartz, D. A. & Graham, A. L., 2020. Potential maternal and infant outcomes from coronavirus 2019-nCoV (SARS-CoV-2) infecting pregnant women: Lessons from SARS, MERS, and other human coronavirus infections. Viruses, 12(2), pp. 194.[DOI:10.3390/v12020194] [PMID] [PMCID]
Shrestha, S., et al., 2019. Maternal role: A concept analysis. Journal of Midwifery and Reproductive Health, 7(3), pp. 1732-41. [Link]
Su, T. P., et al., 2007. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. Journal of Psychiatric Research, 41(1-2), pp. 119–30. [DOI:10.1016/j.jpsychires.2005.12.006] [PMID] [PMCID]
Sullivan, R., et al., 2011. Infant bonding and attachment to the caregiver: Insights from basic and clinical science. Clinics in Perinatology, 38(4), pp. 643–55. [DOI:10.1016/j.clp.2011.08.011] [PMID] [PMCID]
Suzuki, S., 2022. Psychological status of postpartum women under the COVID-19 pandemic in Japan. The Journal of Maternal-Fetal & Neonatal Medicine, 35(9), pp. 1798–800. [DOI:10.1080/14767058.2020.1763949] [PMID]
Tandberg, B. S., et al., 2019. Parent psychological wellbeing in a single-family room versus an open bay neonatal intensive care unit. PloS one, 14(11), pp. e0224488. [DOI:10.1371/journal.pone.0224488] [PMID] [PMCID]
Taubman-Ben-Ari, O., et al., 2009. The transition to motherhood-A time for growth. Journal of Social and Clinical Psychology, 28(8), pp. 943-70. [DOI:10.1521/jscp.2009.28.8.943]
Thapa, S. B., et al., 2020. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstetricia et Gynecologica Scandinavica, 99(7), pp. 817–8. [DOI:10.1111/aogs.13894] [PMID] [PMCID]
Tolja, R., Nakić Radoš, S. & Anđelinović, M., 2020. The role of maternal mental health, infant temperament, and couple’s relationship quality for mother-infant bonding. Journal of Reproductive and Infant Psychology, 38(4), pp. 395-407. [DOI:10.1080/02646838.2020.1733503] [PMID]
Treyvaud, K., et al., 2014. Very preterm birth influences parental mental health and family outcomes seven years after birth. The Journal of Pediatrics, 164(3), pp. 515–21. [DOI:10.1016/j.jpeds.2013.11.001] [PMID] [PMCID]
Treyvaud, K., et al., 2019. A multilayered approach is needed in the NICU to support parents after the preterm birth of their infant. Early Human Development, 139, pp. 104838. [DOI:10.1016/j.earlhumdev.2019.104838] [PMID]
Uzun, A., et al., 2021. Investigating of fear of COVID-19 after pregnancy and association with breastfeeding. Journal of Ideas in Health, 4(1), pp. 327-33. [DOI:10.47108/jidhealth.Vol4.Iss1.98]
Verma, S., et al., 2020. Neonatal intensive care unit preparedness for the Novel Coronavirus Disease-2019 pandemic: A New York City hospital perspective. Current Problems in Pediatric and Adolescent Health Care, 50(4), pp. 100795. [DOI:10.1016/j.cppeds.2020.100795] [PMID] [PMCID]
Wachs, T. D., Black, M. M. & Engle, P. L., 2009. Maternal depression: A global threat to children’s health, development, and behavior and to human rights. Child Development Perspectives, 3(1), pp. 51-9. [DOI:10.1111/j.1750-8606.2008.00077.x]
Zanardo, V., et al., 2020. Psychological impact of COVID‐19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. International Journal of Gynecology & Obstetrics, 150(2), pp. 184–8. [DOI:10.1002/ijgo.13249] [PMID] [PMCID]
Zeng, L., et al., 2020. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatrics, 174(7), pp. 722–5. [PMID]
Zhu, X., et al., 2008. Changes in emotion of the Chinese public in regard to the SARS period. Social Behavior and Personality: An International Journal, 36(4), pp. 447-54. [DOI:10.2224/sbp.2008.36.4.447]
Type of Study: Research |
Subject:
Special
Received: 2022/10/13 | Accepted: 2023/02/12 | Published: 2023/08/24
Received: 2022/10/13 | Accepted: 2023/02/12 | Published: 2023/08/24
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






