Wed, Jan 7, 2026
[Archive]
Volume 10, Issue 1 (Winter 2024)
JCCNC 2024, 10(1): 25-34 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abrahams Simbeye J, Sharifi F, Navab E, Bahramnezhad F. Investigating Nurses’ Knowledge, Attitude, and Performance Regarding Pain Management of Non-verbal Critically-Ill Patients in Tanzania Intensive Care Units. JCCNC 2024; 10 (1) :25-34
URL: http://jccnc.iums.ac.ir/article-1-433-en.html
URL: http://jccnc.iums.ac.ir/article-1-433-en.html
1- Critical Care Nursing Department, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
2- Elderly Health Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
3- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran. ,bahramnezhad.f@gmail.com
2- Elderly Health Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
3- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 569 kb]
(906 Downloads)
| Abstract (HTML) (2674 Views)
● Pain control of non-verbal patients in the intensive care unit is often neglected by the medical staff, especially nurses.
● The attitude, knowledge, and performance of nurses toward pain control of non-verbal patients in intensive care units are poor.
● Nurses in Tanzania and other nurses with low knowledge, negative attitudes, and poor performance in pain management of non-verbal critically ill patients need appropriate in-service training to prevent harm to patients.
● The attitude, knowledge, and performance of nurses toward pain control of non-verbal patients in intensive care units are poor.
● Nurses in Tanzania and other nurses with low knowledge, negative attitudes, and poor performance in pain management of non-verbal critically ill patients need appropriate in-service training to prevent harm to patients.
Plain Language Summary
The pain of non-verbal patients in intensive care units may go unnoticed and even change the patient’s treatment. To assess and manage the pain of these patients, there is a need for special tools and special knowledge. In this study, we assessed the knowledge, attitude, and performance of nurses working in the intensive care units of hospitals in a city in Tanzania, and the findings showed that the nurses of these departments have poor knowledge, attitude, and performance concerning the pain management of these patients. It is recommended that nurses apply appropriate tools to assess the pain of these patients and use correct communication strategies to manage the pain of non-verbal critically ill patients in intensive care units. Holding continuous in-service training regarding pain management of non-verbal critically ill patients is also recommended.
Full-Text: (762 Views)
Introduction
Pain is a common and distressing symptom among non-verbal critically ill patients hospitalized in intensive care units (ICUs). Critically ill patients experience pain because of their illness or injury, invasive or surgical procedures, and many times it can be due to unpleasant stimuli followed by ICU routine interventions (Ayasrah, 2019). Nearly 50% of patients admitted to ICU report moderate to severe pain intensity (Karamjeet, 2017). Untreated pain can lead to unpleasant outcomes in ICU patients. These include poor daily performance, stress, depression, long-term hospitalization, and reduced quality of life and well-being (Issa et al., 2017). In addition, inadequate pain assessment and management have been associated with increased morbidity and mortality in intensive care settings (Issa et al., 2017). Inadequate pain management delays weaning from intubation and mechanical ventilation because pain reduces the number of effective coughs and leads to decreased respiratory ventilation, thereby increasing the incidence of ventilator-associated pneumonia (Payen et al., 2009; Chanques et al., 2006). Meanwhile, liberating the patient from mechanical ventilation should be done as soon as possible to prevent ventilator-associated pneumonia (Shaikh et al., 2018). Also, the use of narcotic drugs without proper evaluation of pain in patients who are dependent on mechanical ventilation can increase the duration of mechanical ventilation, suppress the cough reflex, increase oral secretions, and expose the patient to the risk of ventilator-dependent pneumonia (Morris et al., 2011). These patients are subject to excessive use of painkillers and sedatives, which the excessive use is associated with a longer period of mechanical ventilation (Liu et al., 2017). Prolonged mechanical ventilation, in addition to aspiration and cough reflex suppression, increases the risk of ventilator-associated pneumonia (Craven et al., 2013). Meanwhile, stopping or reducing the sedative can accelerate the removal of the tracheal tube, reduce the leakage of secretions behind the cuff, and the occurrence of ventilator-dependent pneumonia (Ayasrah, 2019). Accordingly, it is necessary to correctly measure the amount of pain in patients under mechanical ventilation who are unable to express their pain to reduce the duration of mechanical ventilation and the length of stay in the ICU. Intensive care nurses play an important role in the pain management of non-verbal critically ill patients. The findings of previous research show the importance of nursing knowledge, attitude, and practice regarding pain management for integration into the clinical environment to improve the quality of pain management of critically ill patients (Issa et al., 2017). A study in Zimbabwe showed that registered nurses had low levels of knowledge and poor attitudes about pain management in adult patients, particularly as most nurses relied on blood pressure and pulse rate measurements to assess patients’ pain intensity (Manwere et al., 2015). Nurses underestimate the severity of pain in non-verbal patients in 35% to 55% of cases due to the lack of knowledge and appropriate tools for pain assessment (Regina, 2013). Various studies have highlighted the challenges of non-verbal patients’ pain management in ICUs, including the lack of knowledge of nurses about pain management and the complications of inadequate pain management. The diagnosis of pain in non-verbal patients remains a major challenge in the ICU. This study adds that deterioration in the level of consciousness among ICU patients especially due to head trauma, routine use of sedation, and other physiological changes are the major causes that delay the pain assessment of non-verbal clients in the ICU (Asadi-Noghabi et al., 2015). Although the authors introduced the use of the critical-care pain observation tool as an effective tool for pain management in non-verbal patients in the ICU, they believe that this tool still has not brought favorable results. For this reason, they concluded that the lack of knowledge and incorrect attitudes among ICU nurses are among the main reasons for insufficient pain management of non-verbal patients in these units (Asadi-Noghabi et al., 2015).
Assessing pain in patients who cannot communicate in ICUs is a major challenge. This study also emphasized the use of behavioral pain scales and critical-care pain observation tools for pain assessment to produce the desired level of outcomes. It concluded that assessing pain in non-verbal adult patients in the ICU must rely on the observation of behavioral indicators of pain, such as moaning, motor restlessness, aggression, distorted expression, crying, and increased confusion (Shaikh et al., 2018). According to a study, pain assessment in non-verbal patients in the ICU is not easy because it requires experience as well as familiarity with the social, emotional, and cultural contexts of pain relief. Most of the patients who are in critical condition cannot verbalize because of being sedated, mechanically ventilated, and the severity of the disease. This study adds that it is important to consider specific behaviors and symptoms, such as facial expression and client posture to assess the severity of pain in this group of non-verbal patients (Regina, 2013).
There is still no clear protocol for pain management of nonverbal and intubated patients in the ICUs in Tanzania. Self-reports and abnormal vital signs are frequently used for pain assessment in ICUs. Critically ill patients are kept on routine analgesics (8-hourly) particularly opioids and intravenous paracetamol. In patients with severe pain especially post-operative patients or those with wounds, opioids are administered intravenously whenever necessary, or PRN which includes fentanyl, morphine, and pethidine (Malima & Khadija, 2014; Samwel & Boniface, 2019). ICUs’ services in Tanzania healthcare settings are not widely initiated. Only a few Tanzania referral hospitals have standard ICUs. Most of the ICUs are not structurally organized to care for patients who are in critical condition. This is due to the lack of financial resources, insufficient technology, and also inadequate training, and scarcity of critical care nurses. The majority of nurses working in the ICUs of Tanzania do not have specific training or specialization in the ICU (Malima & Khadija, 2014; Sawe et al., 2014). Accordingly, this study was conducted to determine the critical care nurses’ knowledge, attitude, and performance toward pain management of non-verbal critically ill adult patients admitted to the ICU.
Materials and Methods
Design, setting, and sample
This was a descriptive cross-sectional study that was conducted from February to May 2020 in four national referral hospitals in Dar es Salaam, Tanzania. The study population comprised nurses working in the ICUs of these hospitals. The study sample was 200 nurses with more than six months of experience in caring for critically ill patients in the ICU.
Participation in the study was voluntary. If the nurse was previously trained in pain management, they were excluded from the study. Also, student nurses, health attendants, and nurses who did not wish to participate in the study were excluded. Due to the small number of nurses, sampling was done through census and 170 nurses participated in the study.
Measurement instruments
The data were collected using a demographic characteristics questionnaire which included questions on sex, age, education level, duration of employment in the ICU, and the type of ICU, along with the knowledge and attitudes survey regarding pain scale and a performance tool by EunKyoung, 2012.
The knowledge and attitudes survey regarding the pain scale was developed by Ferrell and McCaffery (1987) and modified with permission by Al-Shaer et al. (2011). It was used to assess nurses’ knowledge and attitudes. The tool is composed of 39 items, including 21 true or false questions and 18 multiple choice questions, and evaluates four subscales of knowledge, attitude, barriers, and opiophobia. The total score ranges from 0 to 39, where scores less than 50% indicate poor knowledge and attitude, 50% to 75% is considered fair, and more than 75% is indicative of good knowledge and attitude. In data analysis using this tool, distinguishing items as measures of either knowledge or attitude should be avoided (Ferrel & McCaffery, 2012). In this study, the total score was considered and the Cronbach α of the scale was obtained at 0.85.
The performance tool by Eunkyoung was developed by the National Research Foundation of Korea and has been used in previous research to assess nurses’ performance toward pain management (EunKyoung, 2012). The tool consists of 34 items and five subscales, including pain assessment (17 items), patient and family education (5 items), pharmacologic management (5 items), non-pharmacologic management (5 items), and pain evaluation (2 items). Responses to the items are scored based on a 5-point Likert scale (from 5=always perform to 1=do not perform at all). The highest mean of this tool is 5 and higher scores are indicative of better performance. The validity of the tool has been confirmed by the pain experts from the Registered Nurses Association of Ontario (EunKyoung, 2012). In the current study, the Cronbach α of the tool was reported at 0.90.
The data were collected at four national referral hospitals in Tanzania from February 1 to May 20, 2020. A total of 170 questionnaires were collected and used for data analysis out of 202 which were distributed to eligible participants in all ICUs.
Data analysis
The data were analyzed using percentage and frequency distribution, Mean±SD. The one sample t-test was used to assess the relationship between the main variables and demographic characteristics. The Pearson correlation coefficient was used to examine the correlation between nurses’ knowledge, attitude, and performance. The significance level was set at P<0.05.
Results
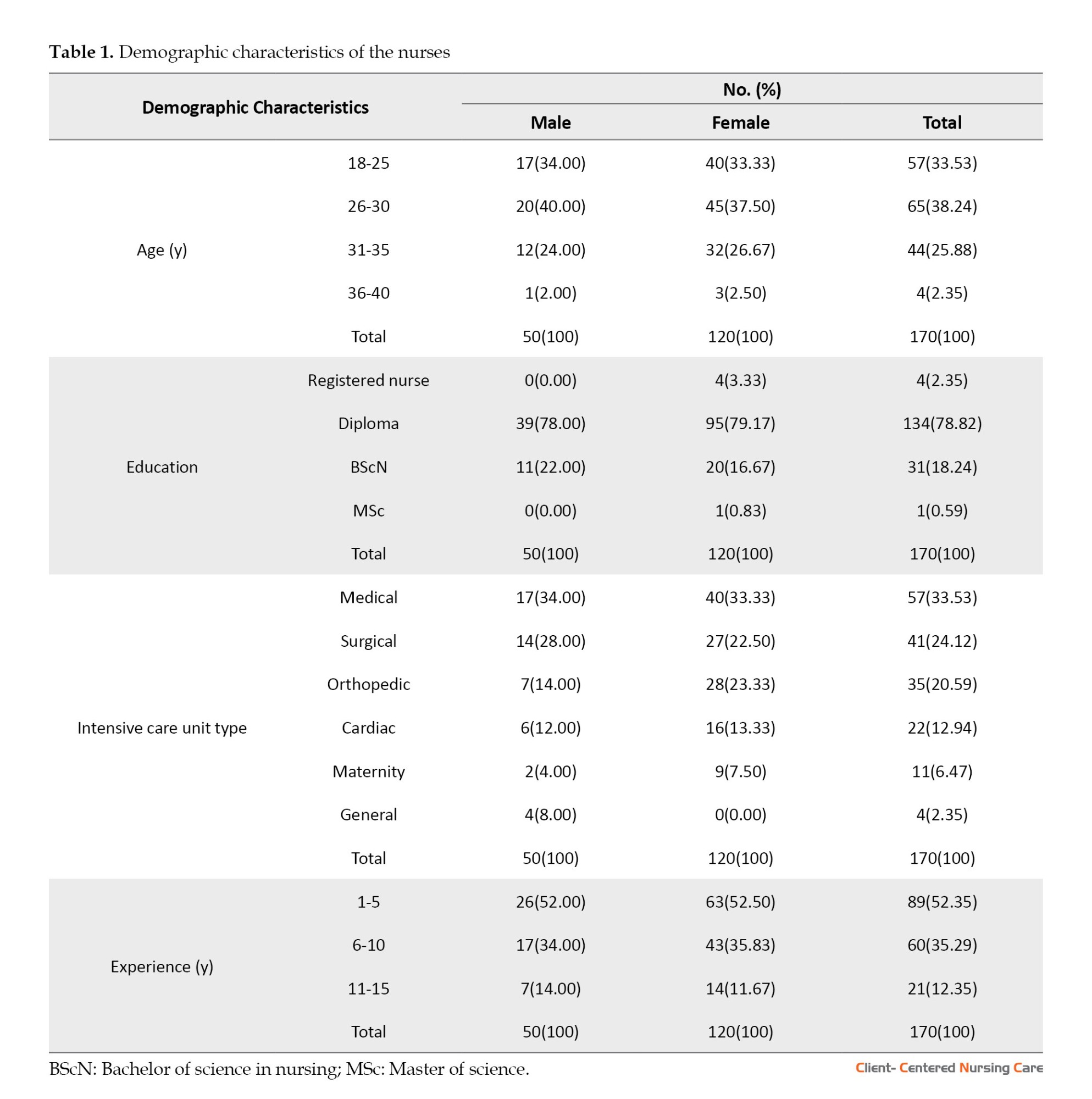
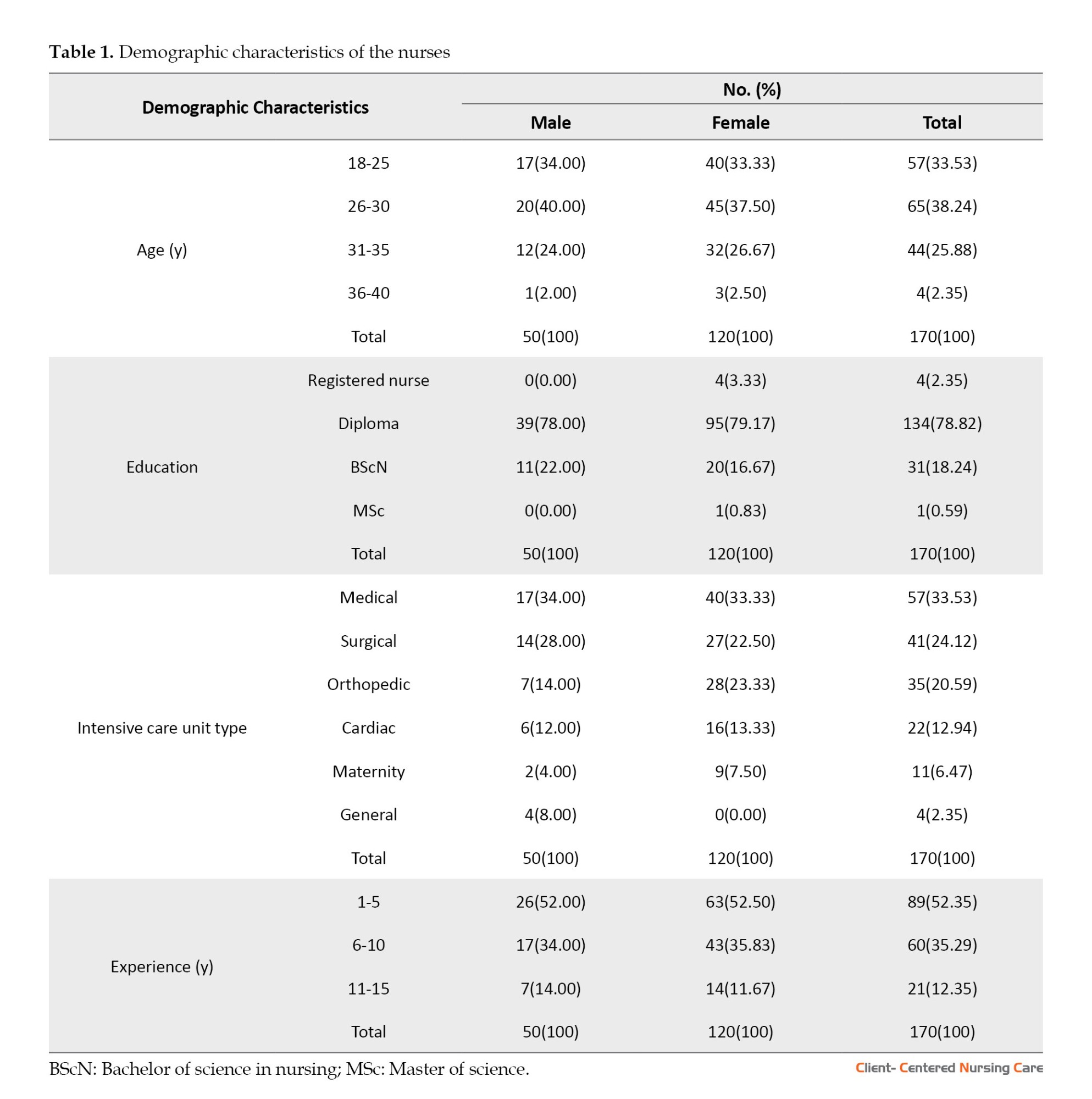
A total of 170 ICU nurses completed the questionnaires, making the overall response rate of 84.2%. The mean age of the subjects was 44.03±18.65 years. The majority of the nurses’ age (38.24%) were between 26-30 years. The mean experience of the study subjects in the ICU was 8.03±2.02 years. Most nurses (78.82%) had a diploma in nursing. Meanwhile, the majority of the nurses (33.53%) worked in the medical ICU. Most nurses’ experience (52.35%) was between 1 to 5 years. Other demographic characteristics are listed in Table 1.
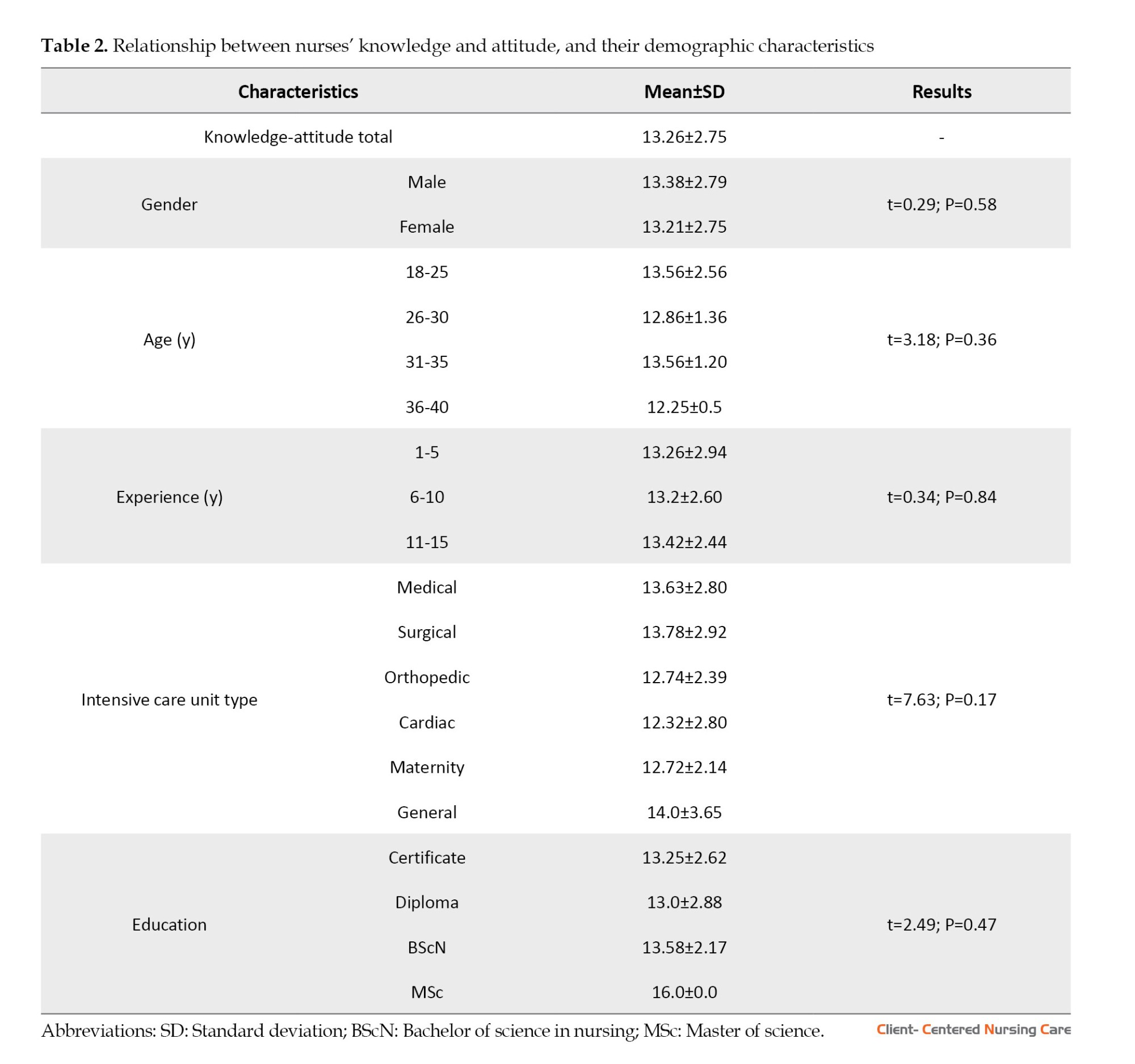
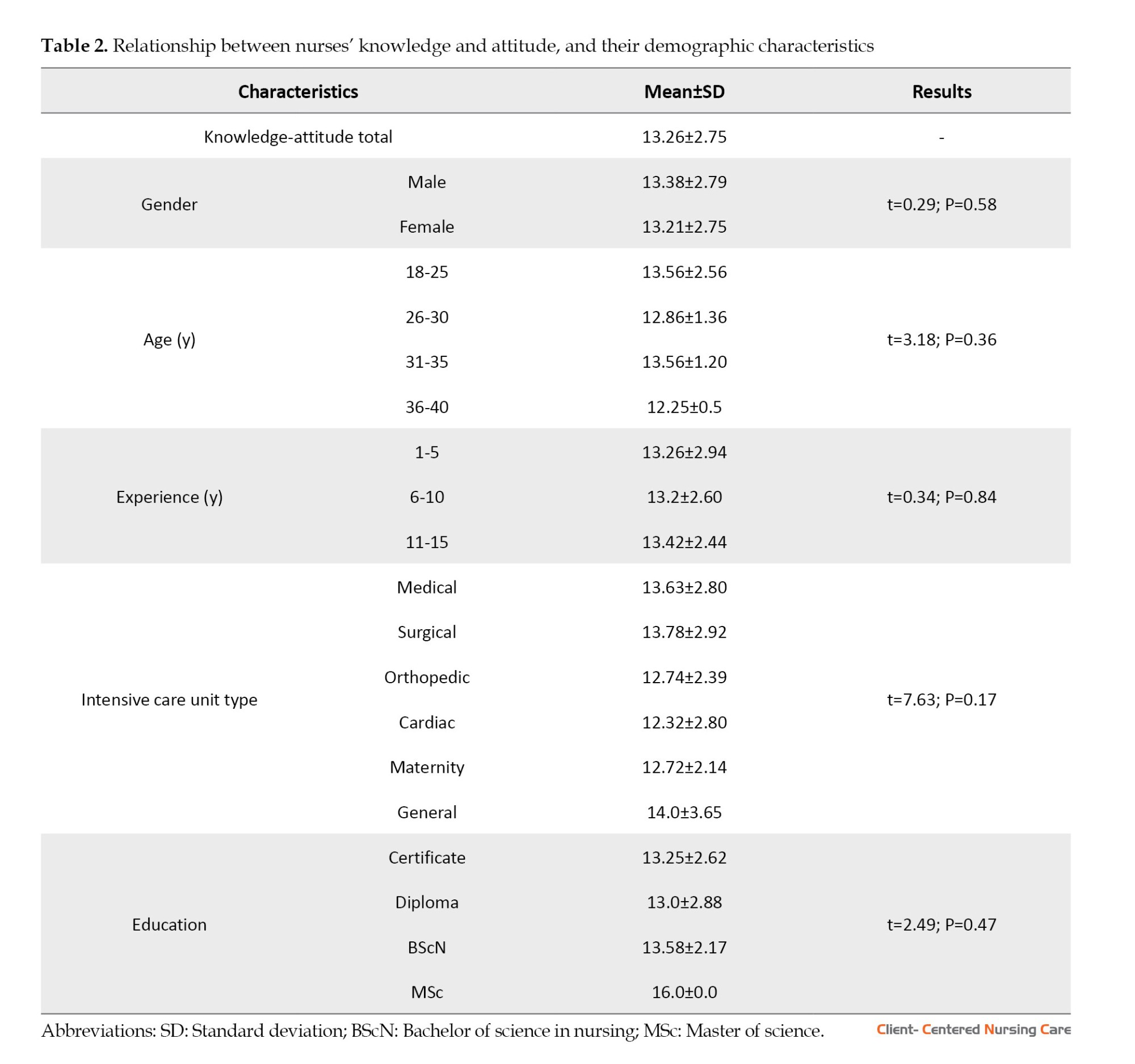
Nurses’ mean knowledge and attitude score was 13.26±2.75, indicating inadequate knowledge and negative attitude. The mean performance score was 2.08±0.16, indicating low performance. There was no significant relationship between nurses’ knowledge and attitude and their demographic characteristics (Table 2).
Meanwhile, no significant relationship was found between the nurses’ performance on pain assessment and their demographic characteristics (Table 3).

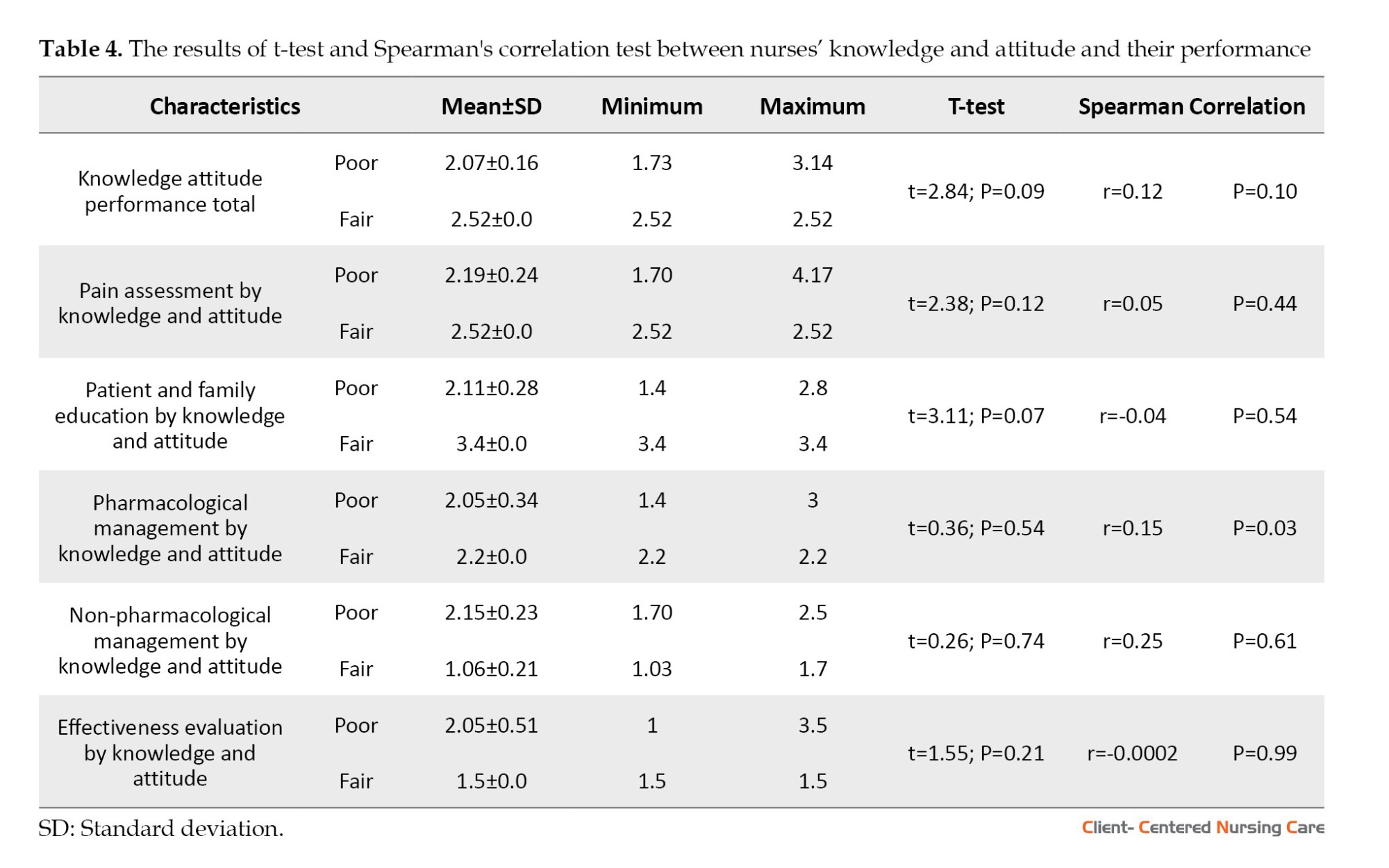
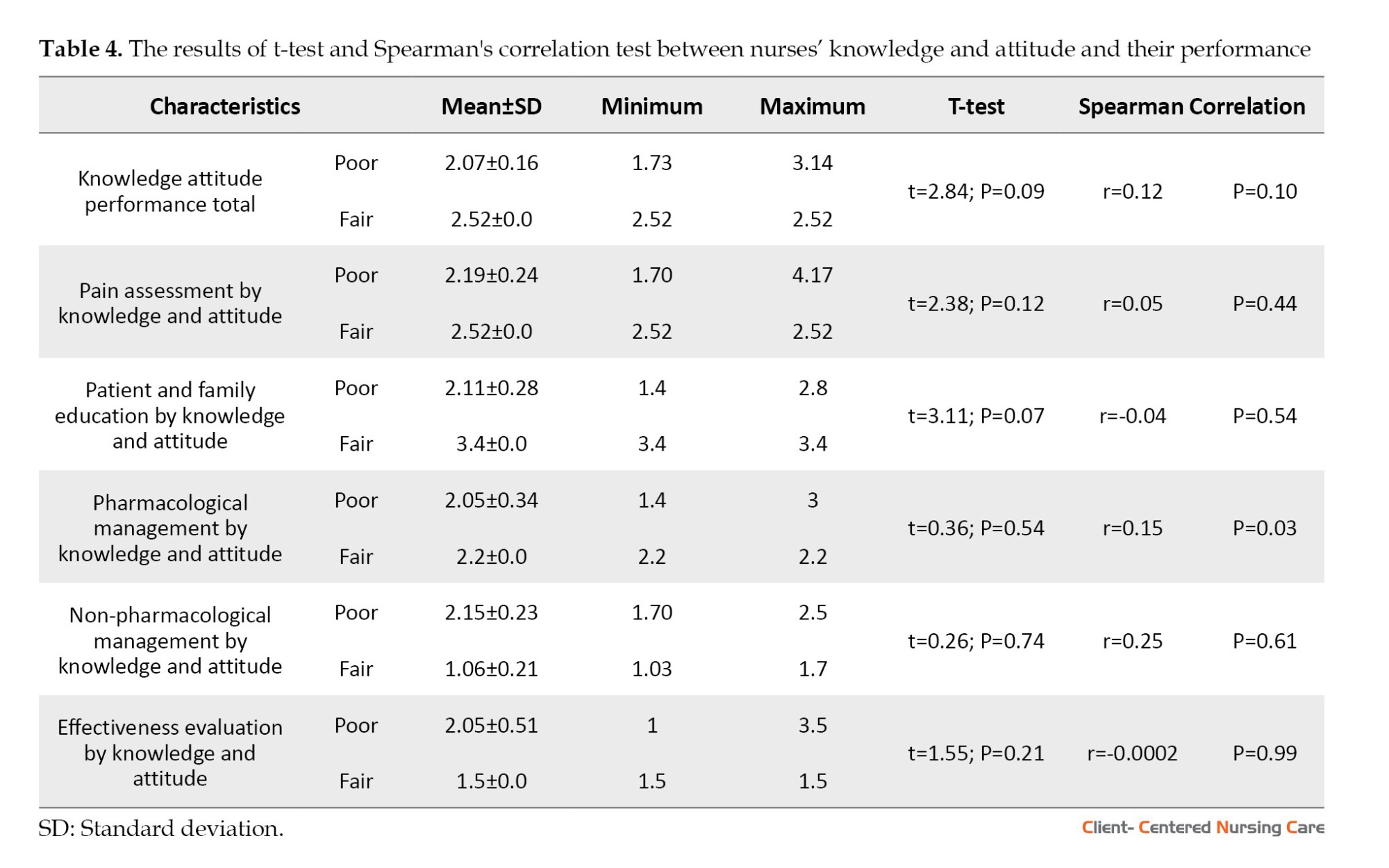
The t-test showed no significant relationship between nurses’ knowledge and attitude and total performance. No significant relationship was found between nurses’ knowledge and attitude and the performance subscales (Table 4).
Discussion
This study assessed the nurses’ knowledge, attitude, and performance regarding pain management of non-verbal critically ill adult patients admitted to ICUs in Tanzania.
Regarding the knowledge and attitude of nurses, our study showed that most nurses scored below 50% of the total average, indicating their lack of knowledge and negative attitude regarding pain management. This may be related to the lack of in-service training for pain management of non-verbal critically ill patients admitted to the ICU. This finding is consistent with a prior study that assessed nurses’ knowledge and attitudes using the same tool. The study found that Saudi nurses in Riyadh, Saudi Arabia, had inadequate pain management knowledge compared with nurses from other regions of the world. The researcher concluded that it is essential to include pain management of non-verbal critically ill patients in the undergraduate nursing curriculum and in-service training of nurses (Samarkandi, 2018). Issa et al., (2017) also found that the mean score for the entire knowledge and attitude was less than 50%, indicating insufficient knowledge and poor attitude toward pain management among ICU nurses. A total of 83.1% of nurses in this study had a bachelor’s degree; however, none of them had specific training on pain assessment and management of non-verbal patients (Issa et al., 2017).
Despite their academic education, ICU nurses still do not have sufficient knowledge regarding the pain management of non-verbal patients, especially in the field of application of research findings in pain management. This uniformity of findings shows that nurses working in ICUs need continuous in-service training in the field of pain management of non-verbal critically ill adult patients admitted to the ICU, regardless of their educational background (Medrzycka-Dabrowska, 2017).
The mean performance score of the nurses in our study was low. The results of a study in South Korea were consistent with the findings of the current research. The findings of this descriptive study showed that the performance of nurses in the field of pain management was not good. Accordingly, it is necessary to use new strategies to promote performance among nurses (Han et al., 2016). It is believed that the assessment of pain in non-communicative adult patients in the ICU should rely on the observation of behavioral indicators of pain. The selection of pain assessment tools in clinical practice should be done carefully. An assessment tool can only be shown to be valid for a specific purpose and a given group of respondents and context of care (Payen & Gélinas, 2014).
There was no relationship between knowledge, attitude, and performance of nurses in pain management in our study. Han et al., (2016) also stated that nurses with sufficient knowledge and attitude about pain management did not perform well in pain management, which also indicates the need for continuous in-service training for nurses in the ICU regarding pain management of non- verbal critically ill patients (Han et al., 2016).
Conclusion
In this study, we assessed critical care nurses’ knowledge, attitude, and performance regarding pain management of non-verbal critically ill adult patients admitted to the ICUs in Tanzania. The findings revealed that nurses had inadequate knowledge, negative attitudes, and insufficient performance toward pain management. Also, there was no significant relationship between the nurses’ knowledge and attitude and their performance in the pain management of these patients.
To improve the knowledge, attitude, and performance of nurses working in the ICUs of Tanzania and other developing countries with the same context, we recommend that critical care departments in all hospitals hold advanced in-service training courses on the pain management of non-verbal critically ill patients for nurses, regardless of their education background. Especially, nurses with bachelor’s degrees in nursing may proceed with master’s in critical care nursing to improve their knowledge and skill in pain management of non-verbal patients. The health administrators and policymakers in clinical settings are also recommended to utilize evidence-based pain management protocols and guidelines and make sure that ICUs use behavioral pain scales on pain assessment for patients who are mechanically ventilated and critical care pain observation tools for non-verbal patients who are not mechanically ventilated. In addition, critical care nurses should be trained to use pharmacological and non-pharmacological strategies of pain management to avoid dependence, addiction, and withdrawal effects which happen due to the frequent use of pharmacological treatment of pain. We recommend future research on the area of pain management to be conducted in developing countries, especially on exploring nurses’ knowledge, attitude, and performance regarding pain management in the ICU. This could help to create awareness and improve performance among critical care nurses who are playing a major role in diagnosing and managing pain in non-verbal critically ill patients admitted to the ICU. Finally, repeated studies, frequent in-service education, and continuous updates on evidence-based pain management guidelines are needed to improve nurses’ performance towards pain management of non-verbal critically ill patients.
The instrument used in our study contained closed questions, so participants who had no opinion or insufficient knowledge may have chosen an answer anyway. However, all respondents were asked to ensure that they answered the questionnaire honestly. In addition, the findings used in this study were based on self-report. Therefore, the participants may have reported a socially acceptable experience rather than their actual performance. Attempts were made to minimize this limitation by asking nurses to be honest when providing feedback.
Ethical Considerations
Compliance with ethical guidelines
This study was conducted after receiving ethical approval from the Nursing, Midwifery, and Rehabilitation Research Ethics Committee of Tehran University of Medical Sciences (Code: IR.TUMS.FNM.REC.1398.150). Permission to conduct the research was also obtained from the relevant ICU hospitals in Tanzania. By obtaining informed consent, the researchers respected the participants’ autonomy and ensured that they were not forced to participate against their will and that confidentiality was maintained.
Funding
The present article was extracted from the master's thesis of Joel Abrahams Simbeye, approved by Department of Critical Care Nursing, School of Nursing and Midwifery, International Campus of Tehran University of Medical Sciences.
Authors' contributions
Conceptualization, investigation, and writing the original draft: Fatemeh Bahramnezhad and Joel Abrahams Simbeye; Methodology, writing and editing: Farshad Sharifi; Supervision: Fatemeh Bahramnezhad; Final approval: All Authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the research vice-chancellor of Tehran University of Medical Sciences and the international vice-chancellor of this university. Also, the authors consider it necessary to acknowledge and thank the Tanzanian nurses for their participation in this study.
References
Al-Shaer, D., Hill, P. D. & Anderson, M. A., 2011. Nurses’ knowledge and attitudes regarding pain assessment and intervention. Medsurg Nursing, 20(1), pp 7-11. [Link]
Asadi-Noghabi, A. A., 2015. Nurses use of critical care pain observational tool in patients with low consciousness. Oman Medical Journal, 30(4), pp. 276-82. [DOI:10.5001/omj.2015.55] [PMID]
Ayasrah, S. M., 2019. Pain among non-verbal critically Ill mechanically ventilated patients: Prevalence, correlates and predictors. Journal of Critical Care, 49, pp. 14-20. [DOI:10.1016/j.jcrc.2018.10.002] [PMID]
Chanques, G., et al., 2006. Impact of systematic evaluation of pain and agitation in an intensive care unit. Critical Care Medicine, 34(6), pp. 1691–9. [DOI:10.1097/01.CCM.0000218416.62457.56] [PMID]
Craven, D. E., et al., 2013. Incidence and outcomes of ventilator-associated tracheobronchitis and pneumonia. The American Journal of Medicine, 126(6), pp. 542-9. [DOI:10.1016/j.amjmed.2012.12.012] [PMID]
Eunkyoung, K. & Myonghwa, P., 2012. Nurses’ awareness and performance about evidence based pain management in older adults. Korean Journal Adult Nursing, 24(1), pp. 20-30. [DOI:10.7475/kjan.2012.24.1.20]
Ferrel, B. & McCaffery, M., 2012. Knowledge and attitudes survey regarding pain. City of Hope Pain & Palliative Care Resource Center, 30(9), pp. 45-50.
Han, J., Park, H. & Jin, M., 2016. Nurses’ knowledge & performance of pain management at a general hospital. Journal of Korean Academy Fundamentals of Nursing, 23(1), pp. 7-12. [DOI:10.7739/jkafn.2016.23.1.6]
Issa, M., Awajeh, A. & Khraisat, F., 2017. Knowledge and attitude about pain and pain management among critical care nurses in a tertiary hospital. Journal of Intensive and Critical Care, 3(1), pp. 1-7. [Link]
Liu, D., et al., 2017. The influence of analgesic-based sedation protocols on delirium and outcomes in critically ill patients: A randomized controlled trial. PloS One, 12(9), pp. e0184310.[DOI:10.1371/journal.pone.0184310] [PMID]
Karamjeet, K., 2017. Knowledge and attitude regarding pain management among staff nurses. Nursing and Care Open Access Journal, 2(1), pp. 5-7. [DOI:10.15406/ncoaj.2017.02.00024]
Malima, Y. & Khadija, I. 2014. Scope of practice for nurses and midwives in Tanzania. Dar es salaam: TNMC. [Link]
Manwere, A., et al., 2015. Knowledge and attitudes of registered nurses towards pain management of adult medical patients: A case of Bindura hospital. Health Science Journal, 9 (4). pp. 1-6. [Link]
Mędrzycka-Dąbrowska, W., et al., 2017. Nurse’s knowledge and barriers regarding pain management. Journal of Perianesthesia Nursing: Official Journal of the American Society of PeriAnesthesia Nurses, 33(5), pp. 715–26. [DOI:10.1016/j.jopan.2017.03.005] [PMID]
Morris, P. E., et al., 2011. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. The American Journal of The Medical Sciences, 341(5), pp. 373–7. [DOI:10.1097/MAJ.0b013e31820ab4f6] [PMID]
Payen, J. F. & Gélinas, C., 2014. Measuring pain in non-verbal critically ill patients: Which pain instrument? Critical Care, 18(5), pp 554. [DOI:10.1186/s13054-014-0554-5] [PMID]
Payen, J. F., et al., 2009. Pain assessment is associated with decreased duration of mechanical ventilation in the intensive care unit: A post hocanalysis of the DOLOREA study. Anesthesiology, 111(6), pp. 1308-16. [DOI:10.1097/ALN.0b013e3181c0d4f0] [PMID]
Payen, J. F. & Chanques, G., 2012. Pain assessment in the ICU can improve outcome. Clinical Pulmonary Medicine, 19(1), pp. 21-6. [Link]
Regina, S., 2013. Nursing team knowledge on behavioural assessment of pain in critical care patients. Original Article, 34 (3), pp 55-63.
Souza, R. C. S., et al., 2013. Nursing team knowledge on behavioural assessment of pain in critical care patients. Revista Gaucha de Enfermagem, 34(3), pp. 55-63. [Link]
Samarkandi O. A., 2018. Knolwledge and attitudes of nurses toward pain management. Saudi Journal of Anaesthesia, 12 (2), pp. 220-6. [DOI:10.4103/sja.SJA_587_17] [PMID]
Samwel, R. & Boniface, R., 2019. Pain management and factors associated with its severity among post surgical patients admitted in the intensive care unit at Muhimbili National Hospital, Tanzania. Open Journal of Anaesthesiology, 9(2), pp. 10. [DOI:10.4236/ojanes.2019.92003]
Sawe, H. R., et al., 2014. Disease patterns and clinical outcomes of patients admitted in intensive care units of tertiary referral hospitals of Tanzania. BMC International Health and Human Rights, 14, pp. 26. [DOI:10.1186/1472-698X-14-26] [PMID]
Shaikh, N., et al., 2018. Acute pain management in intensive care patients: Facts and figures. In: N. A. Shallik (Ed), Pain Management in Special Circumstances ( pp.59-71). London: IntechOpen. [Link]
Pain is a common and distressing symptom among non-verbal critically ill patients hospitalized in intensive care units (ICUs). Critically ill patients experience pain because of their illness or injury, invasive or surgical procedures, and many times it can be due to unpleasant stimuli followed by ICU routine interventions (Ayasrah, 2019). Nearly 50% of patients admitted to ICU report moderate to severe pain intensity (Karamjeet, 2017). Untreated pain can lead to unpleasant outcomes in ICU patients. These include poor daily performance, stress, depression, long-term hospitalization, and reduced quality of life and well-being (Issa et al., 2017). In addition, inadequate pain assessment and management have been associated with increased morbidity and mortality in intensive care settings (Issa et al., 2017). Inadequate pain management delays weaning from intubation and mechanical ventilation because pain reduces the number of effective coughs and leads to decreased respiratory ventilation, thereby increasing the incidence of ventilator-associated pneumonia (Payen et al., 2009; Chanques et al., 2006). Meanwhile, liberating the patient from mechanical ventilation should be done as soon as possible to prevent ventilator-associated pneumonia (Shaikh et al., 2018). Also, the use of narcotic drugs without proper evaluation of pain in patients who are dependent on mechanical ventilation can increase the duration of mechanical ventilation, suppress the cough reflex, increase oral secretions, and expose the patient to the risk of ventilator-dependent pneumonia (Morris et al., 2011). These patients are subject to excessive use of painkillers and sedatives, which the excessive use is associated with a longer period of mechanical ventilation (Liu et al., 2017). Prolonged mechanical ventilation, in addition to aspiration and cough reflex suppression, increases the risk of ventilator-associated pneumonia (Craven et al., 2013). Meanwhile, stopping or reducing the sedative can accelerate the removal of the tracheal tube, reduce the leakage of secretions behind the cuff, and the occurrence of ventilator-dependent pneumonia (Ayasrah, 2019). Accordingly, it is necessary to correctly measure the amount of pain in patients under mechanical ventilation who are unable to express their pain to reduce the duration of mechanical ventilation and the length of stay in the ICU. Intensive care nurses play an important role in the pain management of non-verbal critically ill patients. The findings of previous research show the importance of nursing knowledge, attitude, and practice regarding pain management for integration into the clinical environment to improve the quality of pain management of critically ill patients (Issa et al., 2017). A study in Zimbabwe showed that registered nurses had low levels of knowledge and poor attitudes about pain management in adult patients, particularly as most nurses relied on blood pressure and pulse rate measurements to assess patients’ pain intensity (Manwere et al., 2015). Nurses underestimate the severity of pain in non-verbal patients in 35% to 55% of cases due to the lack of knowledge and appropriate tools for pain assessment (Regina, 2013). Various studies have highlighted the challenges of non-verbal patients’ pain management in ICUs, including the lack of knowledge of nurses about pain management and the complications of inadequate pain management. The diagnosis of pain in non-verbal patients remains a major challenge in the ICU. This study adds that deterioration in the level of consciousness among ICU patients especially due to head trauma, routine use of sedation, and other physiological changes are the major causes that delay the pain assessment of non-verbal clients in the ICU (Asadi-Noghabi et al., 2015). Although the authors introduced the use of the critical-care pain observation tool as an effective tool for pain management in non-verbal patients in the ICU, they believe that this tool still has not brought favorable results. For this reason, they concluded that the lack of knowledge and incorrect attitudes among ICU nurses are among the main reasons for insufficient pain management of non-verbal patients in these units (Asadi-Noghabi et al., 2015).
Assessing pain in patients who cannot communicate in ICUs is a major challenge. This study also emphasized the use of behavioral pain scales and critical-care pain observation tools for pain assessment to produce the desired level of outcomes. It concluded that assessing pain in non-verbal adult patients in the ICU must rely on the observation of behavioral indicators of pain, such as moaning, motor restlessness, aggression, distorted expression, crying, and increased confusion (Shaikh et al., 2018). According to a study, pain assessment in non-verbal patients in the ICU is not easy because it requires experience as well as familiarity with the social, emotional, and cultural contexts of pain relief. Most of the patients who are in critical condition cannot verbalize because of being sedated, mechanically ventilated, and the severity of the disease. This study adds that it is important to consider specific behaviors and symptoms, such as facial expression and client posture to assess the severity of pain in this group of non-verbal patients (Regina, 2013).
There is still no clear protocol for pain management of nonverbal and intubated patients in the ICUs in Tanzania. Self-reports and abnormal vital signs are frequently used for pain assessment in ICUs. Critically ill patients are kept on routine analgesics (8-hourly) particularly opioids and intravenous paracetamol. In patients with severe pain especially post-operative patients or those with wounds, opioids are administered intravenously whenever necessary, or PRN which includes fentanyl, morphine, and pethidine (Malima & Khadija, 2014; Samwel & Boniface, 2019). ICUs’ services in Tanzania healthcare settings are not widely initiated. Only a few Tanzania referral hospitals have standard ICUs. Most of the ICUs are not structurally organized to care for patients who are in critical condition. This is due to the lack of financial resources, insufficient technology, and also inadequate training, and scarcity of critical care nurses. The majority of nurses working in the ICUs of Tanzania do not have specific training or specialization in the ICU (Malima & Khadija, 2014; Sawe et al., 2014). Accordingly, this study was conducted to determine the critical care nurses’ knowledge, attitude, and performance toward pain management of non-verbal critically ill adult patients admitted to the ICU.
Materials and Methods
Design, setting, and sample
This was a descriptive cross-sectional study that was conducted from February to May 2020 in four national referral hospitals in Dar es Salaam, Tanzania. The study population comprised nurses working in the ICUs of these hospitals. The study sample was 200 nurses with more than six months of experience in caring for critically ill patients in the ICU.
Participation in the study was voluntary. If the nurse was previously trained in pain management, they were excluded from the study. Also, student nurses, health attendants, and nurses who did not wish to participate in the study were excluded. Due to the small number of nurses, sampling was done through census and 170 nurses participated in the study.
Measurement instruments
The data were collected using a demographic characteristics questionnaire which included questions on sex, age, education level, duration of employment in the ICU, and the type of ICU, along with the knowledge and attitudes survey regarding pain scale and a performance tool by EunKyoung, 2012.
The knowledge and attitudes survey regarding the pain scale was developed by Ferrell and McCaffery (1987) and modified with permission by Al-Shaer et al. (2011). It was used to assess nurses’ knowledge and attitudes. The tool is composed of 39 items, including 21 true or false questions and 18 multiple choice questions, and evaluates four subscales of knowledge, attitude, barriers, and opiophobia. The total score ranges from 0 to 39, where scores less than 50% indicate poor knowledge and attitude, 50% to 75% is considered fair, and more than 75% is indicative of good knowledge and attitude. In data analysis using this tool, distinguishing items as measures of either knowledge or attitude should be avoided (Ferrel & McCaffery, 2012). In this study, the total score was considered and the Cronbach α of the scale was obtained at 0.85.
The performance tool by Eunkyoung was developed by the National Research Foundation of Korea and has been used in previous research to assess nurses’ performance toward pain management (EunKyoung, 2012). The tool consists of 34 items and five subscales, including pain assessment (17 items), patient and family education (5 items), pharmacologic management (5 items), non-pharmacologic management (5 items), and pain evaluation (2 items). Responses to the items are scored based on a 5-point Likert scale (from 5=always perform to 1=do not perform at all). The highest mean of this tool is 5 and higher scores are indicative of better performance. The validity of the tool has been confirmed by the pain experts from the Registered Nurses Association of Ontario (EunKyoung, 2012). In the current study, the Cronbach α of the tool was reported at 0.90.
The data were collected at four national referral hospitals in Tanzania from February 1 to May 20, 2020. A total of 170 questionnaires were collected and used for data analysis out of 202 which were distributed to eligible participants in all ICUs.
Data analysis
The data were analyzed using percentage and frequency distribution, Mean±SD. The one sample t-test was used to assess the relationship between the main variables and demographic characteristics. The Pearson correlation coefficient was used to examine the correlation between nurses’ knowledge, attitude, and performance. The significance level was set at P<0.05.
Results
A total of 170 ICU nurses completed the questionnaires, making the overall response rate of 84.2%. The mean age of the subjects was 44.03±18.65 years. The majority of the nurses’ age (38.24%) were between 26-30 years. The mean experience of the study subjects in the ICU was 8.03±2.02 years. Most nurses (78.82%) had a diploma in nursing. Meanwhile, the majority of the nurses (33.53%) worked in the medical ICU. Most nurses’ experience (52.35%) was between 1 to 5 years. Other demographic characteristics are listed in Table 1.
Nurses’ mean knowledge and attitude score was 13.26±2.75, indicating inadequate knowledge and negative attitude. The mean performance score was 2.08±0.16, indicating low performance. There was no significant relationship between nurses’ knowledge and attitude and their demographic characteristics (Table 2).
Meanwhile, no significant relationship was found between the nurses’ performance on pain assessment and their demographic characteristics (Table 3).

The t-test showed no significant relationship between nurses’ knowledge and attitude and total performance. No significant relationship was found between nurses’ knowledge and attitude and the performance subscales (Table 4).
Discussion
This study assessed the nurses’ knowledge, attitude, and performance regarding pain management of non-verbal critically ill adult patients admitted to ICUs in Tanzania.
Regarding the knowledge and attitude of nurses, our study showed that most nurses scored below 50% of the total average, indicating their lack of knowledge and negative attitude regarding pain management. This may be related to the lack of in-service training for pain management of non-verbal critically ill patients admitted to the ICU. This finding is consistent with a prior study that assessed nurses’ knowledge and attitudes using the same tool. The study found that Saudi nurses in Riyadh, Saudi Arabia, had inadequate pain management knowledge compared with nurses from other regions of the world. The researcher concluded that it is essential to include pain management of non-verbal critically ill patients in the undergraduate nursing curriculum and in-service training of nurses (Samarkandi, 2018). Issa et al., (2017) also found that the mean score for the entire knowledge and attitude was less than 50%, indicating insufficient knowledge and poor attitude toward pain management among ICU nurses. A total of 83.1% of nurses in this study had a bachelor’s degree; however, none of them had specific training on pain assessment and management of non-verbal patients (Issa et al., 2017).
Despite their academic education, ICU nurses still do not have sufficient knowledge regarding the pain management of non-verbal patients, especially in the field of application of research findings in pain management. This uniformity of findings shows that nurses working in ICUs need continuous in-service training in the field of pain management of non-verbal critically ill adult patients admitted to the ICU, regardless of their educational background (Medrzycka-Dabrowska, 2017).
The mean performance score of the nurses in our study was low. The results of a study in South Korea were consistent with the findings of the current research. The findings of this descriptive study showed that the performance of nurses in the field of pain management was not good. Accordingly, it is necessary to use new strategies to promote performance among nurses (Han et al., 2016). It is believed that the assessment of pain in non-communicative adult patients in the ICU should rely on the observation of behavioral indicators of pain. The selection of pain assessment tools in clinical practice should be done carefully. An assessment tool can only be shown to be valid for a specific purpose and a given group of respondents and context of care (Payen & Gélinas, 2014).
There was no relationship between knowledge, attitude, and performance of nurses in pain management in our study. Han et al., (2016) also stated that nurses with sufficient knowledge and attitude about pain management did not perform well in pain management, which also indicates the need for continuous in-service training for nurses in the ICU regarding pain management of non- verbal critically ill patients (Han et al., 2016).
Conclusion
In this study, we assessed critical care nurses’ knowledge, attitude, and performance regarding pain management of non-verbal critically ill adult patients admitted to the ICUs in Tanzania. The findings revealed that nurses had inadequate knowledge, negative attitudes, and insufficient performance toward pain management. Also, there was no significant relationship between the nurses’ knowledge and attitude and their performance in the pain management of these patients.
To improve the knowledge, attitude, and performance of nurses working in the ICUs of Tanzania and other developing countries with the same context, we recommend that critical care departments in all hospitals hold advanced in-service training courses on the pain management of non-verbal critically ill patients for nurses, regardless of their education background. Especially, nurses with bachelor’s degrees in nursing may proceed with master’s in critical care nursing to improve their knowledge and skill in pain management of non-verbal patients. The health administrators and policymakers in clinical settings are also recommended to utilize evidence-based pain management protocols and guidelines and make sure that ICUs use behavioral pain scales on pain assessment for patients who are mechanically ventilated and critical care pain observation tools for non-verbal patients who are not mechanically ventilated. In addition, critical care nurses should be trained to use pharmacological and non-pharmacological strategies of pain management to avoid dependence, addiction, and withdrawal effects which happen due to the frequent use of pharmacological treatment of pain. We recommend future research on the area of pain management to be conducted in developing countries, especially on exploring nurses’ knowledge, attitude, and performance regarding pain management in the ICU. This could help to create awareness and improve performance among critical care nurses who are playing a major role in diagnosing and managing pain in non-verbal critically ill patients admitted to the ICU. Finally, repeated studies, frequent in-service education, and continuous updates on evidence-based pain management guidelines are needed to improve nurses’ performance towards pain management of non-verbal critically ill patients.
The instrument used in our study contained closed questions, so participants who had no opinion or insufficient knowledge may have chosen an answer anyway. However, all respondents were asked to ensure that they answered the questionnaire honestly. In addition, the findings used in this study were based on self-report. Therefore, the participants may have reported a socially acceptable experience rather than their actual performance. Attempts were made to minimize this limitation by asking nurses to be honest when providing feedback.
Ethical Considerations
Compliance with ethical guidelines
This study was conducted after receiving ethical approval from the Nursing, Midwifery, and Rehabilitation Research Ethics Committee of Tehran University of Medical Sciences (Code: IR.TUMS.FNM.REC.1398.150). Permission to conduct the research was also obtained from the relevant ICU hospitals in Tanzania. By obtaining informed consent, the researchers respected the participants’ autonomy and ensured that they were not forced to participate against their will and that confidentiality was maintained.
Funding
The present article was extracted from the master's thesis of Joel Abrahams Simbeye, approved by Department of Critical Care Nursing, School of Nursing and Midwifery, International Campus of Tehran University of Medical Sciences.
Authors' contributions
Conceptualization, investigation, and writing the original draft: Fatemeh Bahramnezhad and Joel Abrahams Simbeye; Methodology, writing and editing: Farshad Sharifi; Supervision: Fatemeh Bahramnezhad; Final approval: All Authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the research vice-chancellor of Tehran University of Medical Sciences and the international vice-chancellor of this university. Also, the authors consider it necessary to acknowledge and thank the Tanzanian nurses for their participation in this study.
References
Al-Shaer, D., Hill, P. D. & Anderson, M. A., 2011. Nurses’ knowledge and attitudes regarding pain assessment and intervention. Medsurg Nursing, 20(1), pp 7-11. [Link]
Asadi-Noghabi, A. A., 2015. Nurses use of critical care pain observational tool in patients with low consciousness. Oman Medical Journal, 30(4), pp. 276-82. [DOI:10.5001/omj.2015.55] [PMID]
Ayasrah, S. M., 2019. Pain among non-verbal critically Ill mechanically ventilated patients: Prevalence, correlates and predictors. Journal of Critical Care, 49, pp. 14-20. [DOI:10.1016/j.jcrc.2018.10.002] [PMID]
Chanques, G., et al., 2006. Impact of systematic evaluation of pain and agitation in an intensive care unit. Critical Care Medicine, 34(6), pp. 1691–9. [DOI:10.1097/01.CCM.0000218416.62457.56] [PMID]
Craven, D. E., et al., 2013. Incidence and outcomes of ventilator-associated tracheobronchitis and pneumonia. The American Journal of Medicine, 126(6), pp. 542-9. [DOI:10.1016/j.amjmed.2012.12.012] [PMID]
Eunkyoung, K. & Myonghwa, P., 2012. Nurses’ awareness and performance about evidence based pain management in older adults. Korean Journal Adult Nursing, 24(1), pp. 20-30. [DOI:10.7475/kjan.2012.24.1.20]
Ferrel, B. & McCaffery, M., 2012. Knowledge and attitudes survey regarding pain. City of Hope Pain & Palliative Care Resource Center, 30(9), pp. 45-50.
Han, J., Park, H. & Jin, M., 2016. Nurses’ knowledge & performance of pain management at a general hospital. Journal of Korean Academy Fundamentals of Nursing, 23(1), pp. 7-12. [DOI:10.7739/jkafn.2016.23.1.6]
Issa, M., Awajeh, A. & Khraisat, F., 2017. Knowledge and attitude about pain and pain management among critical care nurses in a tertiary hospital. Journal of Intensive and Critical Care, 3(1), pp. 1-7. [Link]
Liu, D., et al., 2017. The influence of analgesic-based sedation protocols on delirium and outcomes in critically ill patients: A randomized controlled trial. PloS One, 12(9), pp. e0184310.[DOI:10.1371/journal.pone.0184310] [PMID]
Karamjeet, K., 2017. Knowledge and attitude regarding pain management among staff nurses. Nursing and Care Open Access Journal, 2(1), pp. 5-7. [DOI:10.15406/ncoaj.2017.02.00024]
Malima, Y. & Khadija, I. 2014. Scope of practice for nurses and midwives in Tanzania. Dar es salaam: TNMC. [Link]
Manwere, A., et al., 2015. Knowledge and attitudes of registered nurses towards pain management of adult medical patients: A case of Bindura hospital. Health Science Journal, 9 (4). pp. 1-6. [Link]
Mędrzycka-Dąbrowska, W., et al., 2017. Nurse’s knowledge and barriers regarding pain management. Journal of Perianesthesia Nursing: Official Journal of the American Society of PeriAnesthesia Nurses, 33(5), pp. 715–26. [DOI:10.1016/j.jopan.2017.03.005] [PMID]
Morris, P. E., et al., 2011. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. The American Journal of The Medical Sciences, 341(5), pp. 373–7. [DOI:10.1097/MAJ.0b013e31820ab4f6] [PMID]
Payen, J. F. & Gélinas, C., 2014. Measuring pain in non-verbal critically ill patients: Which pain instrument? Critical Care, 18(5), pp 554. [DOI:10.1186/s13054-014-0554-5] [PMID]
Payen, J. F., et al., 2009. Pain assessment is associated with decreased duration of mechanical ventilation in the intensive care unit: A post hocanalysis of the DOLOREA study. Anesthesiology, 111(6), pp. 1308-16. [DOI:10.1097/ALN.0b013e3181c0d4f0] [PMID]
Payen, J. F. & Chanques, G., 2012. Pain assessment in the ICU can improve outcome. Clinical Pulmonary Medicine, 19(1), pp. 21-6. [Link]
Regina, S., 2013. Nursing team knowledge on behavioural assessment of pain in critical care patients. Original Article, 34 (3), pp 55-63.
Souza, R. C. S., et al., 2013. Nursing team knowledge on behavioural assessment of pain in critical care patients. Revista Gaucha de Enfermagem, 34(3), pp. 55-63. [Link]
Samarkandi O. A., 2018. Knolwledge and attitudes of nurses toward pain management. Saudi Journal of Anaesthesia, 12 (2), pp. 220-6. [DOI:10.4103/sja.SJA_587_17] [PMID]
Samwel, R. & Boniface, R., 2019. Pain management and factors associated with its severity among post surgical patients admitted in the intensive care unit at Muhimbili National Hospital, Tanzania. Open Journal of Anaesthesiology, 9(2), pp. 10. [DOI:10.4236/ojanes.2019.92003]
Sawe, H. R., et al., 2014. Disease patterns and clinical outcomes of patients admitted in intensive care units of tertiary referral hospitals of Tanzania. BMC International Health and Human Rights, 14, pp. 26. [DOI:10.1186/1472-698X-14-26] [PMID]
Shaikh, N., et al., 2018. Acute pain management in intensive care patients: Facts and figures. In: N. A. Shallik (Ed), Pain Management in Special Circumstances ( pp.59-71). London: IntechOpen. [Link]
Type of Study: Research |
Subject:
General
Received: 2022/10/30 | Accepted: 2023/08/29 | Published: 2024/01/10
Received: 2022/10/30 | Accepted: 2023/08/29 | Published: 2024/01/10
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






