Sat, Dec 13, 2025
[Archive]
Volume 9, Issue 3 (Summer 2023)
JCCNC 2023, 9(3): 199-206 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bastani F, Amirijavid A. Sleep Quality in the Survivors of COVID-19. JCCNC 2023; 9 (3) :199-206
URL: http://jccnc.iums.ac.ir/article-1-447-en.html
URL: http://jccnc.iums.ac.ir/article-1-447-en.html
1- Nursing and Midwifery Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Community Health and Geriatric Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,aidaamirijavid77@gmail.com
2- Department of Community Health and Geriatric Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 581 kb]
(723 Downloads)
| Abstract (HTML) (1922 Views)
Full-Text: (538 Views)
1. Introduction
Sleep, as one of the basic physiological needs of humans, is regulated by the brain. Sleep is one of the three basic elements (apart from healthy eating and regular exercise) of good health. Sleep quality is a multidimensional and complex concept associated with various diseases, unwanted injuries, reduced quality of life, reduced daily performance, and inappropriate cognitive performance. It is essential for maintaining the body’s physiological function and is very important in everyday life (Vibha & Sushil, 2020). According to a report, nearly 50% of survivors hospitalized due to COVID-19 had poor sleep quality 7 months after discharge from the hospital (Fernández-de-Las-Peñas, 2021).
A new strain of severe acute respiratory syndrome, recently identified as an infectious disease (COVID-19), was caused by SARS-CoV-2 in Chinese patients with severe pneumonia (Islam & Iqbal, 2020). According to the guidelines of the National Health System (NHS) in England regarding the needs of those recovering from COVID-19, it is predicted that a large burden of physical, neurological, and psychological conditions of patients after discharge will be imposed on this system. This issue requires thorough and comprehensive assessments to address these challenges (England NHS, 2020).
The general population has experienced a high level of physical problems and significant psychological stress during the COVID-19 pandemic, which can probably affect the quantity and quality of people’s sleep) Rajkumar, 2020. In this sleep disorder, there is a type of rapid eye movement along with sleep apnea and an increase in the apnea-hypopnea index, which is considered a kind of fatigue syndrome after surviving the COVID-19 infection and is an unfortunate experience for many patients. One theory suggests that sleep apnea leads to the patient waking up at night with the feeling of suffocation and burning in the lungs, and as a result, the quality of sleep decreases (Koczulla et al., 2021). A study has shown that sleep disturbance may increase in patients with acute respiratory distress after recovery compared to the general population. In some recovered patients, acute respiratory distress syndrome exists several months after discharge from the hospital, and the possibility of disturbed sleep quality in people with COVID-19 increases (Dimitrievski et al., 2021). The post-COVID-19 syndrome, also called prolonged COVID-19, should be paid attention to. This syndrome refers to symptoms that persist for more than 3 weeks after the diagnosis and treatment of cases of COVID-19 that have specific clinical manifestations. The incidence of post-COVID-19 syndrome is estimated to be between 10% and 35%. Fatigue is the most commonly reported symptom, followed by shortness of breath that remains in the patient. Psychological problems, chest pain, smell and taste disorders, and sleep disorders are other symptoms that affect patients. Therefore, primary healthcare professionals and healthcare teams, such as community health nurses, play a key role in evaluating, identifying, and managing the symptoms of patients with post-COVID-19 syndrome. This issue necessitates wider research in this field (Pavli et al., 2021). In this disease, sleep patterns, sleep quality, and the diagnosis and management of sleep disorders are all profoundly and somewhat unexpectedly affected, so research on sleep disorders in patients with COVID-19 is still ongoing in both acute and chronic stages of the disease (Jahrami et al., 2021).
Accordingly, this study determined the sleep quality of those who recovered from COVID-19. The study was done at the Imam Khomeini Sarab Medical Research Center in East Azerbaijan Province, Iran.
2. Materials and Methods
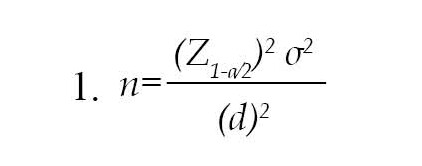
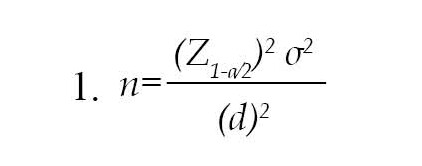
This research is a descriptive cross-sectional study on the sleep quality of the survivors of COVID-19 discharged from Imam Khomeini Sarab Hospital. The sample size is 217, at a confidence level of 95%, accuracy of 0.5 points (relative to the range of scores from 0 to 21), the standard deviation of sleep quality as 4.43, and d=1 in the Equations 1.
Given the possibility of sample drop, 222 patients were considered to participate in the study. The eligible subjects were recruited by consecutive sampling. After coordinating with the head and hospital, the list of discharged patients with COVID-19 was received from the medical records department, and their phone numbers were provided to the researcher. Then, the eligible people were contacted through the government telephone of the hospital, and the people who were willing to participate answered the questions of the questionnaires by reading the research over the phone. Information about the disease was also extracted from the patient’s records. The inclusion criteria were the ability to answer the questionnaire items, no history of taking sleeping pills or sleep disorders before contracting COVID-19, availability of phone numbers, age of 18 years or older, and at least one month passed since discharge. The data were collected from July to September 2022 after providing a complete explanation of the study and its objectives, emphasizing the voluntary nature of participation, confidentiality of the information, and obtaining oral informed consent. The research tools included a demographic and disease characteristics questionnaire and the Pittsburgh sleep quality index (PSQI).
Demographic and disease characteristics questionnaire
This questionnaire included age, gender, education level, marital status, employment status, underlying diseases, economic status, self-assessment of health, number of months since contracting COVID-19 and its vaccination, and number of COVID-19 vaccinations.
Pittsburgh sleep quality index (PSQI)
Pittsburgh sleep quality index (PSQI) is a self-report questionnaire for assessing sleep quality over one month. This measure has 18 items, creating 7 components producing one global score, and takes 5–10 minutes to complete (Buysse et al., 1989). PSQI was used to assess sleep status not only because of its simplicity, high reliability, and validity but also because of its comprehensive evaluation of sleep status from several dimensions. In the original version, acceptable measures of internal homogeneity, consistency (test re-test reliability), and validity were obtained. PSQI global score >5 has a diagnostic sensitivity of 89.6% and a specificity of 86.5% (kappa=0.75, P≤0.001) in distinguishing between good and poor sleep. Seven components of this index are the subjective quality of sleep, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep medications, and daytime dysfunction. Each dimension is scored between 0 and 3 (0=none, 1=weak, 2=moderate, 3=severe), with a total score ranging from 0 to 21. A score of more than 5 indicated a poor sleeper, while others were recognized as good. The validity and reliability of this questionnaire were estimated by Zhang (2020) with a Cronbach α of 0.78. The reliability of this tool in Iran was reported by Nasiriziba, et al. (2020) with a Cronbach α of 0.89. The validity of this questionnaire was checked and confirmed by the content validity method in the same study by three members of the academic staff of the Faculty of Nursing and Midwifery of Iran University of Medical Sciences (Nasiriziba, et al., 2020).
The data were analyzed by statistical methods such as frequency distribution tables, central and dispersion indicators, and inferential statistics in SPSS software, version 20. The independent t-test was used to determine the association between gender, employment status, marital status, associated diseases, and health self-assessment with sleep quality. ANOVA and Scheffé post hoc test were used for the variables of age, education, and economic status. The level of significance was set at P≥0.05.
3. Results
The results showed that 94 subjects (42.3%) were men and 128(57.7%) were women. Mean age of the subjects was 50.32±16.75 years. According to Table 1, the subjects’ mean sleep quality score was 9.19±3.68, indicating poor sleep quality.

Table 2 shows the scores of the 7 components of sleep quality, their minimum, maximum and Mean±SD.
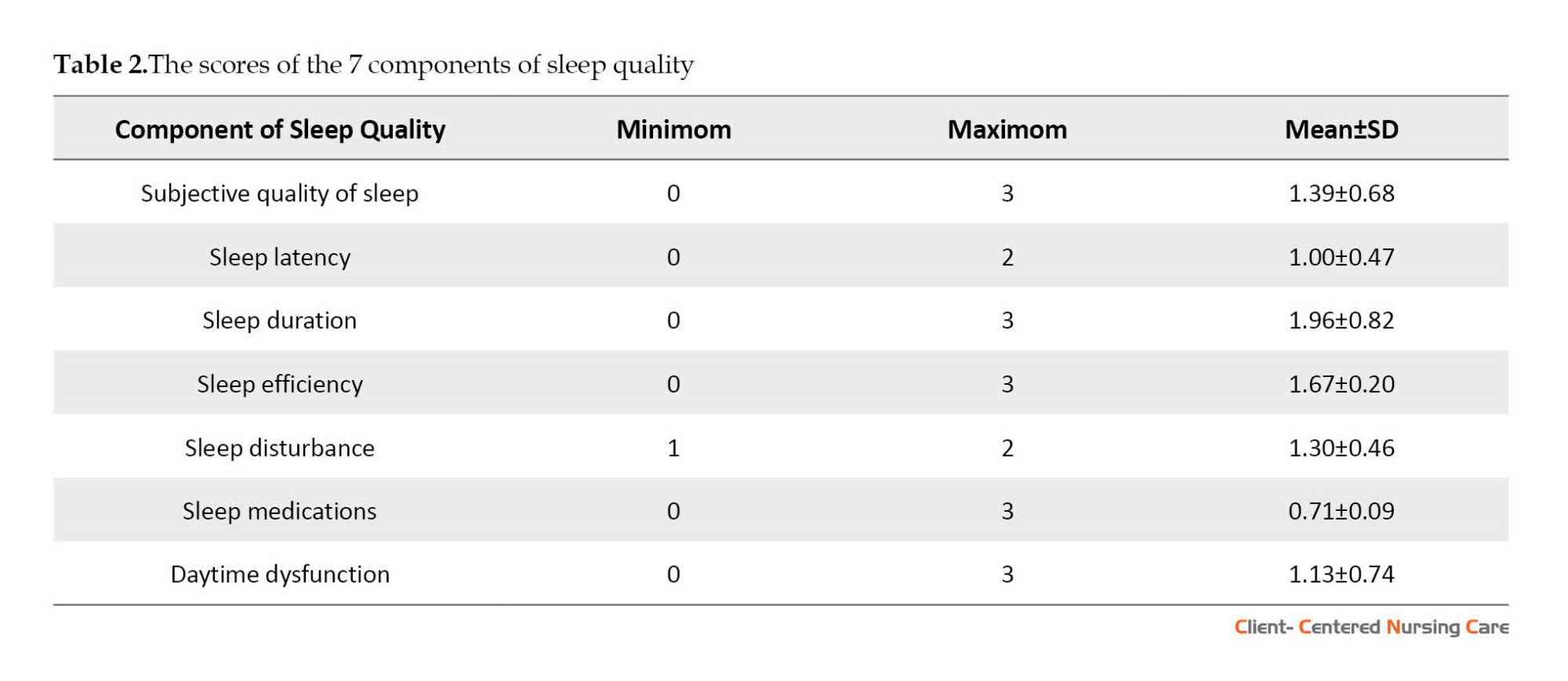
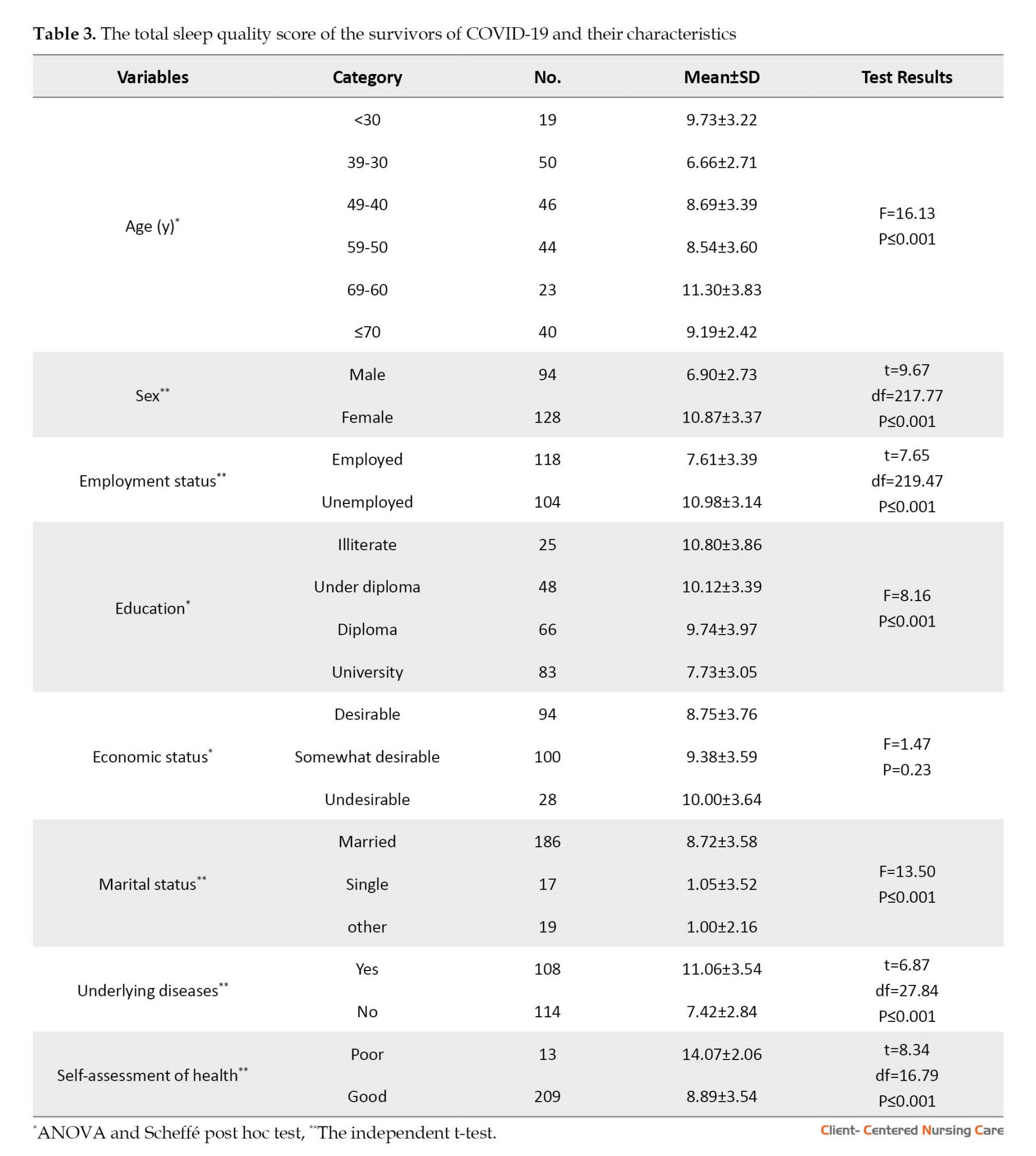
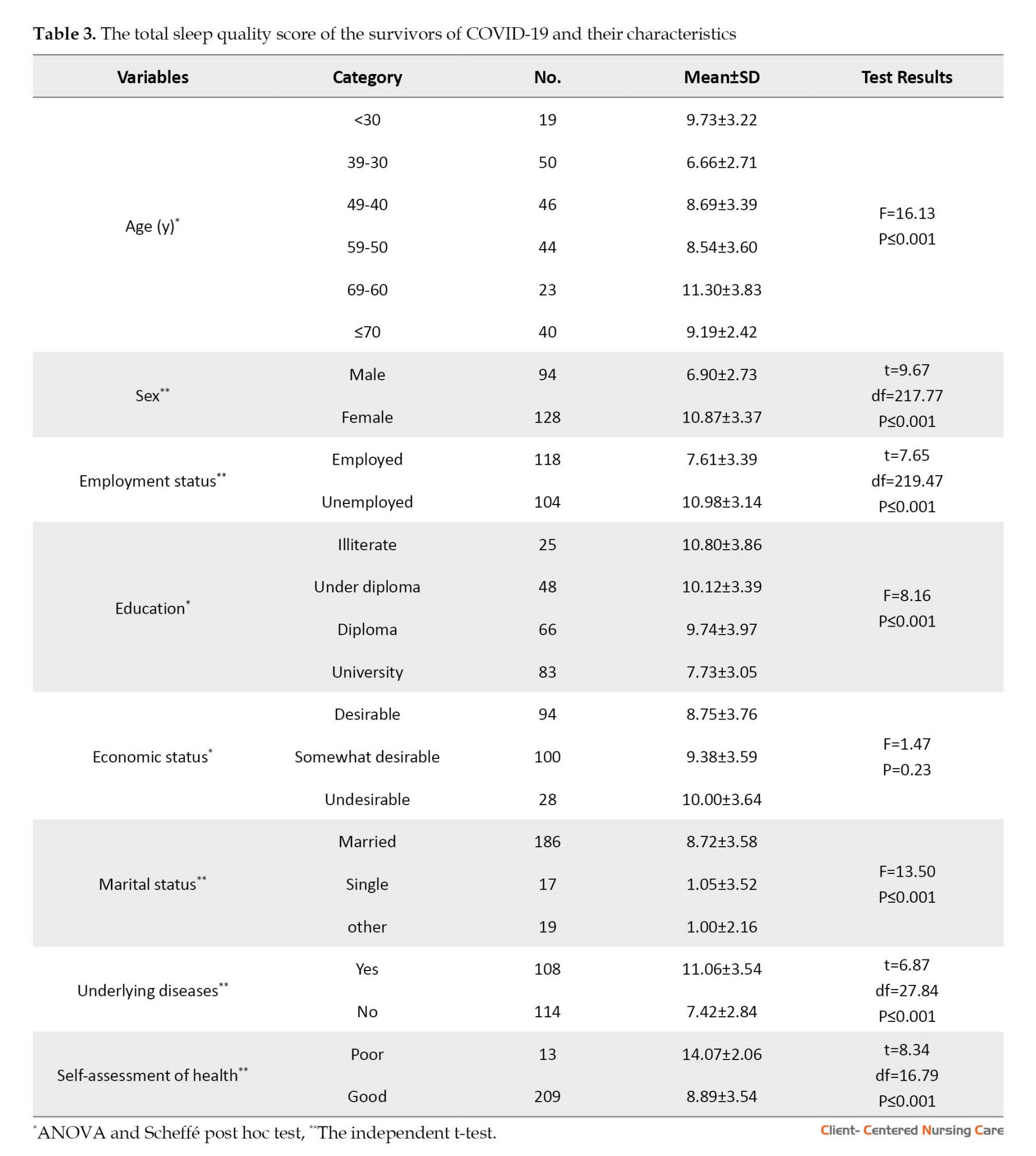
Table 3 shows the relationship between the total sleep quality score of the discharged COVID-19 patients and their demographic characteristics.
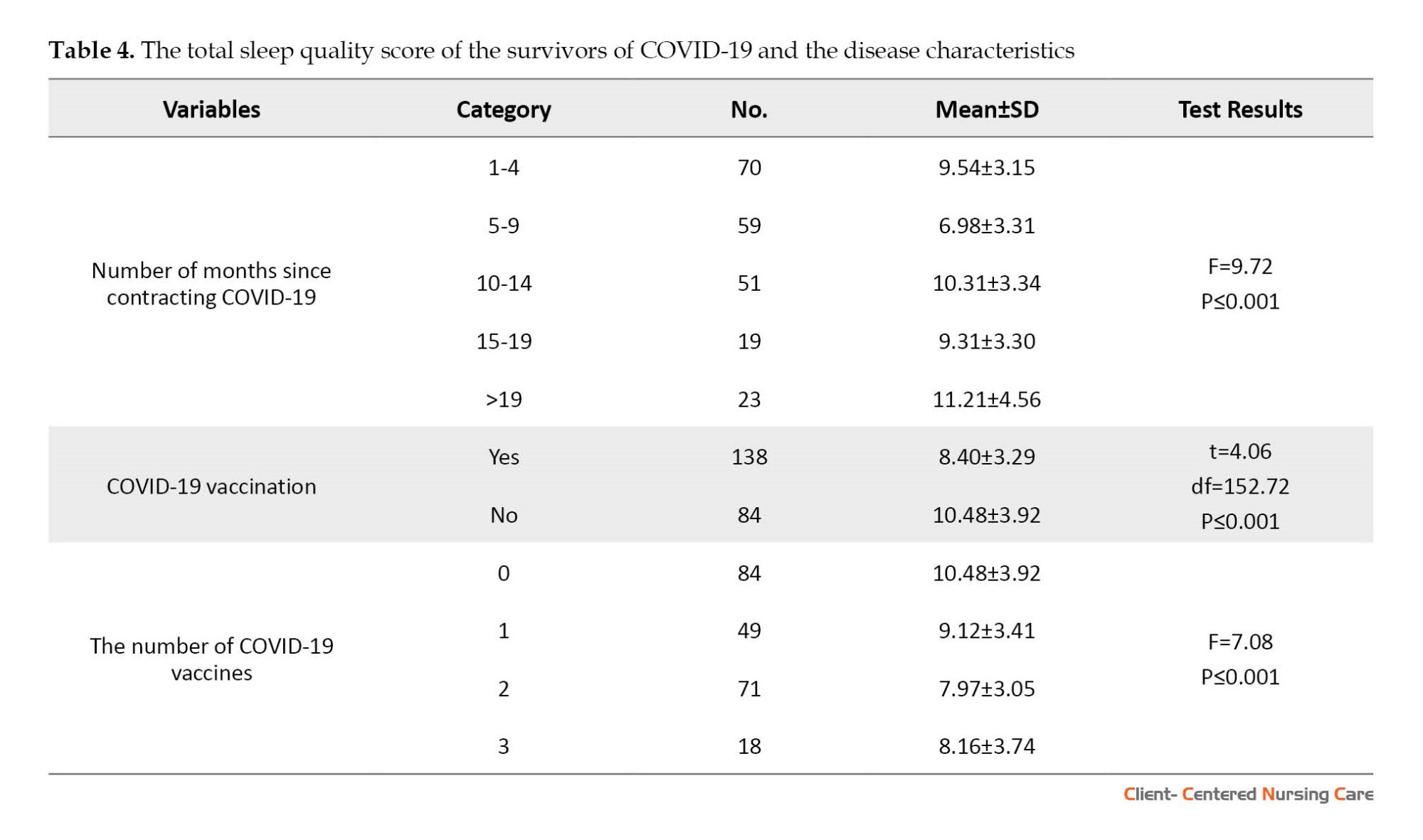
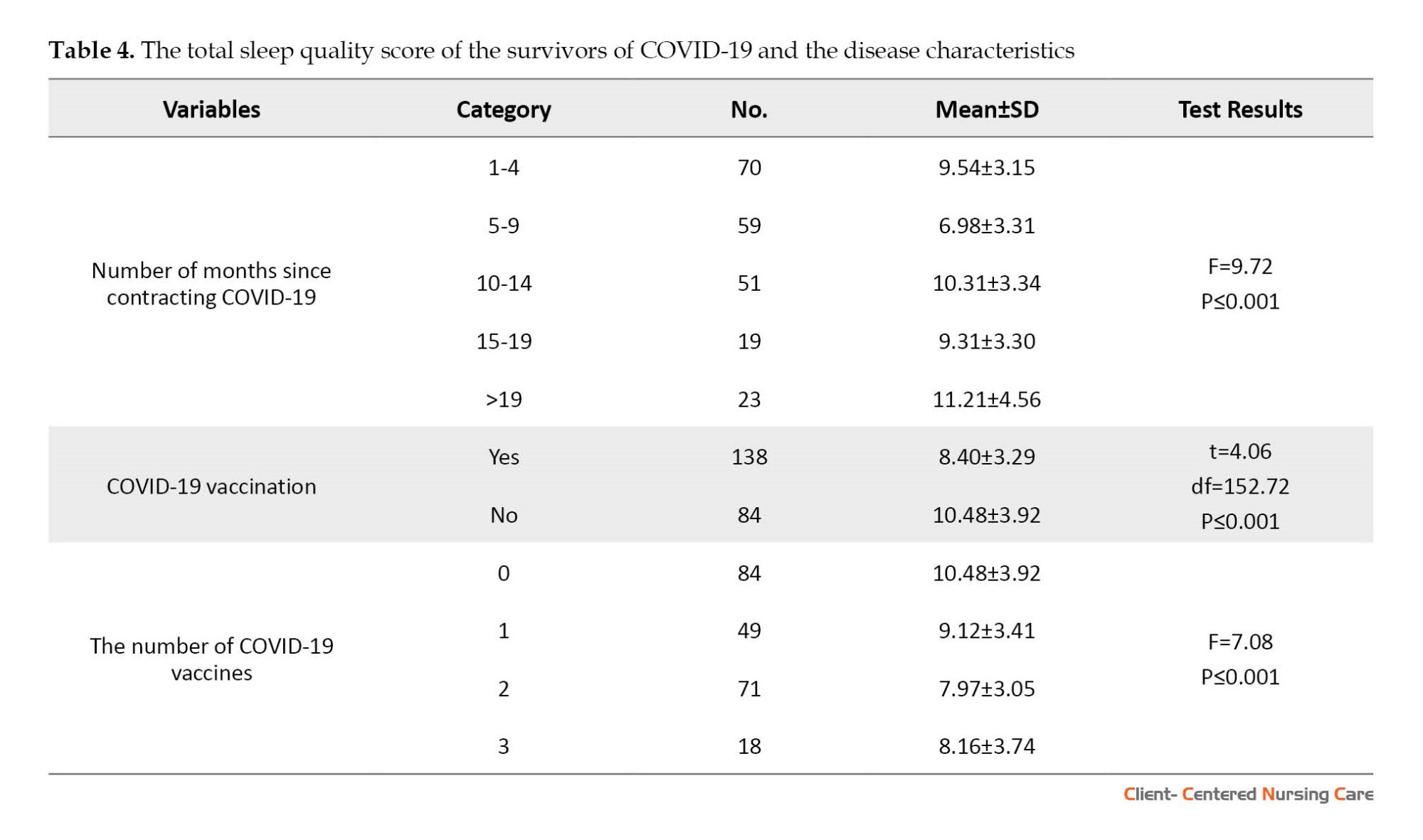
In Table 4, the relationship between the total sleep quality score of the discharged COVID-19 patients and the characteristics related to the disease is shown.
4. Discussion
This study was conducted to determine the sleep quality of COVID-19 survivors discharged from the hospital for at least one month. The results showed that about 84.4%(187 people) of the subjects had poor sleep quality, which is somewhat consistent with the results of the study by Campo-Arias et al. (2022) on the recovered patients of COVID-19, and based on its results about 60% of the participants reported insomnia. Also, Huang et al. study in China to determine complications after COVID-19 shows that sleep disorders are among the most common complications after recovery from COVID-19. The mentioned study used a researcher-made, self-report symptom questionnaire different from the instrument used in our research (PSQI) (Huang et al., 2021).
The findings showed that all 7 components of sleep quality were disturbed and decreased. The results of the study by El Sayed et al. (2021) to determine the sleep status in the post-COVID-19 period and its impact on various aspects of people’s quality of life showed that the quality of the 7 components of sleep is impaired and decreased, which is in line with the results of our study. Also, our study’s findings align with the findings of Benítez et al. (2022) study, which showed that the quality of the 7 components of sleep is impaired in those who have recovered from COVID-19.
Our findings showed the most demographic and disease characteristics related to the sleep quality of those who have recovered from COVID-19. In this way, unemployed people had poorer sleep quality than employed people. As age increases, the quality of sleep becomes lower. The people who did not receive the vaccine had a more unfavorable sleep quality than the vaccinated people, and the sleep quality of married people was higher than other marital status groups. Also, illiterate people’s sleep quality was poorer than other groups. These results are consistent with the results of several previous studies. In the study of Fu et al. (2022), there was a significant relationship between the quality of sleep of those who recovered from COVID-19 and age, so older people had poorer sleep quality. In a study by Jiang et al. (2021) conducted on patients who recovered from COVID-19, it was found that older adults have reported more sleep problems. In the study of Notarte et al. (2022), it was found that the development of prolonged COVID, which s the long-term presence of symptoms after recovery from COVID-19, quality of sleep is better in vaccinated people. Also, Alqahtani et al. (2022) study showed that unmarried people have poorer sleep quality. El Sayed et al. (2021) found that unmarried people also have a lower sleep quality.
However, our study’s results were inconsistent with the results of some previous studies. We found that unemployed people had poorer sleep quality than their employed counterparts. However, Fu et al. (2022) found that full-time employees reported the lowest sleep quality. We found that the people who did not receive the vaccine had a more unfavorable sleep quality than those vaccinated. Still, Fernández-de-Las-Peñas et al. (2022) found no difference between the vaccinated and non-vaccinated groups regarding the investigated variables, including sleep quality.
The findings of our study showed that the sleep quality of married people was higher than other marital groups. Still, Akıncı and Basar (2021) reported no significant relationship between the sleep quality of those who recovered from COVID-19 and their marital status. We also found that illiterate people’s sleep quality was poorer than other groups. Still, in the study of Akıncı and Bassar (2021), there was no significant difference between the subjects with different education levels.
Due to not completing the questionnaires in person, some questions were unclear to the respondents. If the research samples raised a question, the researcher fully explained it to overcome this limitation. In this study, the CT (cycle threshold) criterion, which is especially used to measure the severity of the COVID-19 disease, was unfortunately not performed at the Imam Khomeini Sarab Hospital. People’s perceptions and tolerances regarding the phenomenon of sleep and the components of sleep quality are different, which may be caused by individual differences related to ethnicity, cultural, social factors, and economic status, which was beyond the researcher’s control. Also, the study’s cross-sectional nature is one of its limitations, which requires cautious use of the results.
5. Conclusion
According to the results, the quality of sleep of the survivors of COVID-19 discharged from the Imam Khomeini Sarab Medical Research Training Center was poor. Because poor sleep quality can negatively affect many aspects of life, it is very important to follow up on the sleep quality of those who have recovered from COVID-19 and think of measures to improve it. Considering the vulnerability of this group of people, it is suggested that their sleep quality be monitored in the post-discharge period, and educational-counseling interventions be provided to improve their sleep quality. Since the present study was conducted only in one center with many referrals in Sarab City, it is recommended that the next studies be conducted in multicenter and larger hospitals. Prospective and longitudinal studies are also suggested.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Iran University of Medical Sciences (Code: IR.IUMS.REC.1400.854). We explained the study objectives, the voluntary nature of participation, the confidentiality of their information, and the right to withdraw from the study for the participants. They provided verbal informed consent to participate in the study.
Funding
The article was extracted from the MSc thesis of Aida Amirijavid, approved by Department of Community Health and Geriatric Nursing, Iran University of Medical Sciences.
Authors' contributions
All authors equally contributed in preparation of this paper.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their appreciation to financial support of the Iran University of Medical Sciences, study participants and the Imam Khomeini Research and Training Center, in Sarab, Iran, for their collaboration.
References
Akıncı, T. & Melek Başar, H., 2021. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep Medicine, 80, pp. 167-70. [DOI:10.1016/j.sleep.2021.01.034] [PMID] [PMCID]
Alqahtani, A. S., 2022. Impact of the loss of smell on the sleep quality and fatigue level in COVID 19 survivors. European Archives of Oto-Rhino-Laryngology, 279(9), PP. 4443–9. [DOI:10.1007/s00405-022-07381-z] [PMID] [PMCID]
Benítez, I. D., et al., 2022. Sleep and circadian health of critical COVID-19 survivors 3 months after hospital discharge. Critical Care Medicine, 50(6), pp. 945-54. [DOI:10.1097/CCM.0000000000005476] [PMID] [PMCID]
Buysse, D. J., et al., 1989. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), pp. 193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
Campo-Arias, A., Pedrozo-Pupo, J. C. & Caballero-Domínguez, C. C., 2022. Relation of perceived discrimination with depression, insomnia and post-traumatic stress in COVID-19 survivors. Psychiatry Research, 307, pp. 114337. [DOI:10.1016/j.psychres.2021.114337] [PMID] [PMCID]
Dimitrievski, A., et al., 2021. Towards detecting pneumonia progression in COVID-19 patients by monitoring sleep disturbance using data streams of non-invasive sensor networks. Sensors, 21(9), pp. 3030. [DOI:10.3390/s21093030] [PMID] [PMCID]
El Sayed, S., et al., 2021. Sleep in post-COVID-19 recovery period and its impact on different domains of quality of life. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery, 57(1), pp. 172 [DOI:10.1186/s41983-021-00429-7] [PMID] [PMCID]
NHS., 2020. After-care needs of inpatients recovering from COVID-19. London: NHS. [Link]
Fernández-de-Las-Peñas, C., et al., 2021. Anxiety, depression and poor sleep quality as long-term post-COVID sequelae in previously hospitalized patients: A multicenter study. The Journal of Infection, 83(4), pp. 496–522. [DOI:10.1016/j.jinf.2021.06.022] [PMID] [PMCID]
Fernández-de-Las-Peñas, C., et al., 2022. Differences in long-COVID symptoms between vaccinated and non-vaccinated (BNT162b2 Vaccine) hospitalized COVID-19 survivors infected with the delta variant. Vaccines, 10(9), pp. 1481. [DOI:10.3390/vaccines10091481] [PMID] [PMCID]
Fu, L., et al., 2022. Associations between COVID-19 related stigma and sleep quality among COVID-19 survivors six months after hospital discharge. Sleep Medicine, 91, pp. 273-81. [DOI:10.1016/j.sleep.2021.10.020] [PMID] [PMCID]
The Johns Hopkins University., 2022. What Is Coronavirus? Retrieved from: [Link]
Huang, C., et al., 2021. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet, 397(10270), pp. 220-32. [DOI:10.1016/S0140-6736(20)32656-8] [PMID]
Islam, K. U. & Iqbal, J., 2020. An update on molecular diagnostics for COVID-19. Frontiers in Cellular and Infection Microbiology, 10, pp. 560616. [DOI:10.3389/fcimb.2020.560616] [PMID] [PMCID]
Jahrami, H., et al., 2021. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. Journal of Clinical Sleep Medicine, 17(2), pp. 299-313. [DOI:10.5664/jcsm.8930] [PMID] [PMCID]
Jiang, Z., et al., 2021. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. Journal of Psychiatric Research, 136, pp. 595-602. [DOI:10.1016/j.jpsychires.2020.10.034] [PMID] [PMCID]
Koczulla, A. R., et al., 2021. Newly detected rapid eye movement associated sleep apnea after coronavirus disease 2019 as a possible cause for chronic fatigue: Two case reports. Journal of Medical Case Reports, 15(1), pp. 211. [DOI:10.1186/s13256-021-02819-0] [PMID] [PMCID]
Nasiri Ziba, F., Veisimiankali, M. & Haghani, H., 2020. [Association between demographic characteristics and sleep quality of elderly patients with coronary artery disease hospitalized in Imam Ali Hospital during 2018 (Persian)]. Journal of Ilam University of Medical Sciences, 28(1), pp. 1-11. [DOI:10.29252/sjimu.28.1.1]
Notarte, K. I., et al., 2022. Impact of COVID-19 vaccination on the risk of developing long-COVID and on existing long-COVID symptoms: A systematic review. EClinicalMedicine, 53, pp. 101624. [DOI:10.1016/j.eclinm.2022.101624] [PMID] [PMCID]
Pavli, A., Theodoridou, M. & Maltezou, H. C., 2021. Post-COVID syndrome: Incidence, clinical spectrum, and challenges for primary healthcare professionals. Archives of Medical Research, 52(6), pp. 575–81. [DOI:10.1016/j.arcmed.2021.03.010] [PMID] [PMCID]
Rajkumar, R. P., 2020. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, pp. 102066. [DOI:10.1016/j.ajp.2020.102066] [PMID] [PMCID]
Jha, V. M. & Jha, S. K., 2020. Sleep: Evolution and functions. Singapore: Springer. [Link]
Zhang, J., 2020. Mental disorders, fatigue, perceived event impact, and coping in post-illness patients with COVID-19 within 1 month after discharge: A case-controlled study. The Lancet, pp. 1-20. [Unpublished].
Sleep, as one of the basic physiological needs of humans, is regulated by the brain. Sleep is one of the three basic elements (apart from healthy eating and regular exercise) of good health. Sleep quality is a multidimensional and complex concept associated with various diseases, unwanted injuries, reduced quality of life, reduced daily performance, and inappropriate cognitive performance. It is essential for maintaining the body’s physiological function and is very important in everyday life (Vibha & Sushil, 2020). According to a report, nearly 50% of survivors hospitalized due to COVID-19 had poor sleep quality 7 months after discharge from the hospital (Fernández-de-Las-Peñas, 2021).
A new strain of severe acute respiratory syndrome, recently identified as an infectious disease (COVID-19), was caused by SARS-CoV-2 in Chinese patients with severe pneumonia (Islam & Iqbal, 2020). According to the guidelines of the National Health System (NHS) in England regarding the needs of those recovering from COVID-19, it is predicted that a large burden of physical, neurological, and psychological conditions of patients after discharge will be imposed on this system. This issue requires thorough and comprehensive assessments to address these challenges (England NHS, 2020).
The general population has experienced a high level of physical problems and significant psychological stress during the COVID-19 pandemic, which can probably affect the quantity and quality of people’s sleep) Rajkumar, 2020. In this sleep disorder, there is a type of rapid eye movement along with sleep apnea and an increase in the apnea-hypopnea index, which is considered a kind of fatigue syndrome after surviving the COVID-19 infection and is an unfortunate experience for many patients. One theory suggests that sleep apnea leads to the patient waking up at night with the feeling of suffocation and burning in the lungs, and as a result, the quality of sleep decreases (Koczulla et al., 2021). A study has shown that sleep disturbance may increase in patients with acute respiratory distress after recovery compared to the general population. In some recovered patients, acute respiratory distress syndrome exists several months after discharge from the hospital, and the possibility of disturbed sleep quality in people with COVID-19 increases (Dimitrievski et al., 2021). The post-COVID-19 syndrome, also called prolonged COVID-19, should be paid attention to. This syndrome refers to symptoms that persist for more than 3 weeks after the diagnosis and treatment of cases of COVID-19 that have specific clinical manifestations. The incidence of post-COVID-19 syndrome is estimated to be between 10% and 35%. Fatigue is the most commonly reported symptom, followed by shortness of breath that remains in the patient. Psychological problems, chest pain, smell and taste disorders, and sleep disorders are other symptoms that affect patients. Therefore, primary healthcare professionals and healthcare teams, such as community health nurses, play a key role in evaluating, identifying, and managing the symptoms of patients with post-COVID-19 syndrome. This issue necessitates wider research in this field (Pavli et al., 2021). In this disease, sleep patterns, sleep quality, and the diagnosis and management of sleep disorders are all profoundly and somewhat unexpectedly affected, so research on sleep disorders in patients with COVID-19 is still ongoing in both acute and chronic stages of the disease (Jahrami et al., 2021).
Accordingly, this study determined the sleep quality of those who recovered from COVID-19. The study was done at the Imam Khomeini Sarab Medical Research Center in East Azerbaijan Province, Iran.
2. Materials and Methods
This research is a descriptive cross-sectional study on the sleep quality of the survivors of COVID-19 discharged from Imam Khomeini Sarab Hospital. The sample size is 217, at a confidence level of 95%, accuracy of 0.5 points (relative to the range of scores from 0 to 21), the standard deviation of sleep quality as 4.43, and d=1 in the Equations 1.
Given the possibility of sample drop, 222 patients were considered to participate in the study. The eligible subjects were recruited by consecutive sampling. After coordinating with the head and hospital, the list of discharged patients with COVID-19 was received from the medical records department, and their phone numbers were provided to the researcher. Then, the eligible people were contacted through the government telephone of the hospital, and the people who were willing to participate answered the questions of the questionnaires by reading the research over the phone. Information about the disease was also extracted from the patient’s records. The inclusion criteria were the ability to answer the questionnaire items, no history of taking sleeping pills or sleep disorders before contracting COVID-19, availability of phone numbers, age of 18 years or older, and at least one month passed since discharge. The data were collected from July to September 2022 after providing a complete explanation of the study and its objectives, emphasizing the voluntary nature of participation, confidentiality of the information, and obtaining oral informed consent. The research tools included a demographic and disease characteristics questionnaire and the Pittsburgh sleep quality index (PSQI).
Demographic and disease characteristics questionnaire
This questionnaire included age, gender, education level, marital status, employment status, underlying diseases, economic status, self-assessment of health, number of months since contracting COVID-19 and its vaccination, and number of COVID-19 vaccinations.
Pittsburgh sleep quality index (PSQI)
Pittsburgh sleep quality index (PSQI) is a self-report questionnaire for assessing sleep quality over one month. This measure has 18 items, creating 7 components producing one global score, and takes 5–10 minutes to complete (Buysse et al., 1989). PSQI was used to assess sleep status not only because of its simplicity, high reliability, and validity but also because of its comprehensive evaluation of sleep status from several dimensions. In the original version, acceptable measures of internal homogeneity, consistency (test re-test reliability), and validity were obtained. PSQI global score >5 has a diagnostic sensitivity of 89.6% and a specificity of 86.5% (kappa=0.75, P≤0.001) in distinguishing between good and poor sleep. Seven components of this index are the subjective quality of sleep, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep medications, and daytime dysfunction. Each dimension is scored between 0 and 3 (0=none, 1=weak, 2=moderate, 3=severe), with a total score ranging from 0 to 21. A score of more than 5 indicated a poor sleeper, while others were recognized as good. The validity and reliability of this questionnaire were estimated by Zhang (2020) with a Cronbach α of 0.78. The reliability of this tool in Iran was reported by Nasiriziba, et al. (2020) with a Cronbach α of 0.89. The validity of this questionnaire was checked and confirmed by the content validity method in the same study by three members of the academic staff of the Faculty of Nursing and Midwifery of Iran University of Medical Sciences (Nasiriziba, et al., 2020).
The data were analyzed by statistical methods such as frequency distribution tables, central and dispersion indicators, and inferential statistics in SPSS software, version 20. The independent t-test was used to determine the association between gender, employment status, marital status, associated diseases, and health self-assessment with sleep quality. ANOVA and Scheffé post hoc test were used for the variables of age, education, and economic status. The level of significance was set at P≥0.05.
3. Results
The results showed that 94 subjects (42.3%) were men and 128(57.7%) were women. Mean age of the subjects was 50.32±16.75 years. According to Table 1, the subjects’ mean sleep quality score was 9.19±3.68, indicating poor sleep quality.

Table 2 shows the scores of the 7 components of sleep quality, their minimum, maximum and Mean±SD.
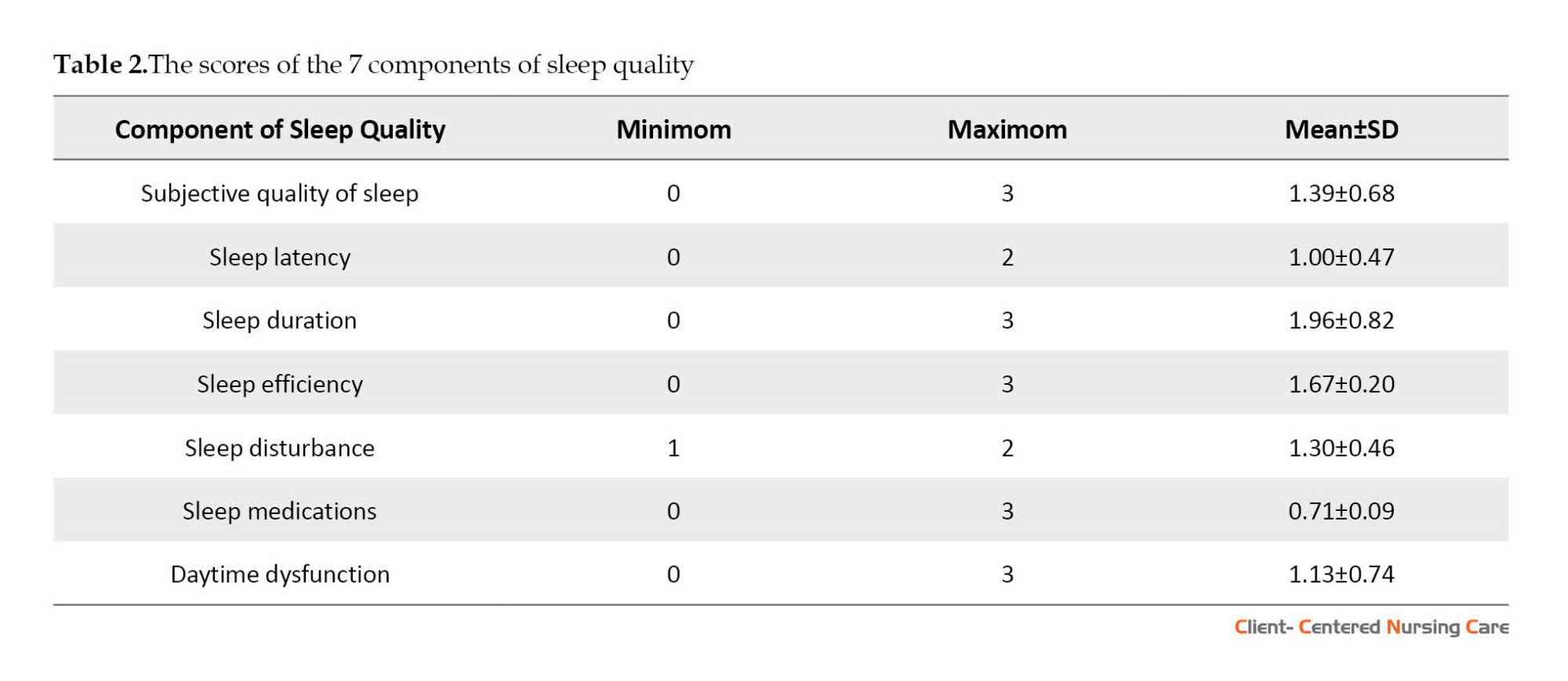
Table 3 shows the relationship between the total sleep quality score of the discharged COVID-19 patients and their demographic characteristics.
In Table 4, the relationship between the total sleep quality score of the discharged COVID-19 patients and the characteristics related to the disease is shown.
4. Discussion
This study was conducted to determine the sleep quality of COVID-19 survivors discharged from the hospital for at least one month. The results showed that about 84.4%(187 people) of the subjects had poor sleep quality, which is somewhat consistent with the results of the study by Campo-Arias et al. (2022) on the recovered patients of COVID-19, and based on its results about 60% of the participants reported insomnia. Also, Huang et al. study in China to determine complications after COVID-19 shows that sleep disorders are among the most common complications after recovery from COVID-19. The mentioned study used a researcher-made, self-report symptom questionnaire different from the instrument used in our research (PSQI) (Huang et al., 2021).
The findings showed that all 7 components of sleep quality were disturbed and decreased. The results of the study by El Sayed et al. (2021) to determine the sleep status in the post-COVID-19 period and its impact on various aspects of people’s quality of life showed that the quality of the 7 components of sleep is impaired and decreased, which is in line with the results of our study. Also, our study’s findings align with the findings of Benítez et al. (2022) study, which showed that the quality of the 7 components of sleep is impaired in those who have recovered from COVID-19.
Our findings showed the most demographic and disease characteristics related to the sleep quality of those who have recovered from COVID-19. In this way, unemployed people had poorer sleep quality than employed people. As age increases, the quality of sleep becomes lower. The people who did not receive the vaccine had a more unfavorable sleep quality than the vaccinated people, and the sleep quality of married people was higher than other marital status groups. Also, illiterate people’s sleep quality was poorer than other groups. These results are consistent with the results of several previous studies. In the study of Fu et al. (2022), there was a significant relationship between the quality of sleep of those who recovered from COVID-19 and age, so older people had poorer sleep quality. In a study by Jiang et al. (2021) conducted on patients who recovered from COVID-19, it was found that older adults have reported more sleep problems. In the study of Notarte et al. (2022), it was found that the development of prolonged COVID, which s the long-term presence of symptoms after recovery from COVID-19, quality of sleep is better in vaccinated people. Also, Alqahtani et al. (2022) study showed that unmarried people have poorer sleep quality. El Sayed et al. (2021) found that unmarried people also have a lower sleep quality.
However, our study’s results were inconsistent with the results of some previous studies. We found that unemployed people had poorer sleep quality than their employed counterparts. However, Fu et al. (2022) found that full-time employees reported the lowest sleep quality. We found that the people who did not receive the vaccine had a more unfavorable sleep quality than those vaccinated. Still, Fernández-de-Las-Peñas et al. (2022) found no difference between the vaccinated and non-vaccinated groups regarding the investigated variables, including sleep quality.
The findings of our study showed that the sleep quality of married people was higher than other marital groups. Still, Akıncı and Basar (2021) reported no significant relationship between the sleep quality of those who recovered from COVID-19 and their marital status. We also found that illiterate people’s sleep quality was poorer than other groups. Still, in the study of Akıncı and Bassar (2021), there was no significant difference between the subjects with different education levels.
Due to not completing the questionnaires in person, some questions were unclear to the respondents. If the research samples raised a question, the researcher fully explained it to overcome this limitation. In this study, the CT (cycle threshold) criterion, which is especially used to measure the severity of the COVID-19 disease, was unfortunately not performed at the Imam Khomeini Sarab Hospital. People’s perceptions and tolerances regarding the phenomenon of sleep and the components of sleep quality are different, which may be caused by individual differences related to ethnicity, cultural, social factors, and economic status, which was beyond the researcher’s control. Also, the study’s cross-sectional nature is one of its limitations, which requires cautious use of the results.
5. Conclusion
According to the results, the quality of sleep of the survivors of COVID-19 discharged from the Imam Khomeini Sarab Medical Research Training Center was poor. Because poor sleep quality can negatively affect many aspects of life, it is very important to follow up on the sleep quality of those who have recovered from COVID-19 and think of measures to improve it. Considering the vulnerability of this group of people, it is suggested that their sleep quality be monitored in the post-discharge period, and educational-counseling interventions be provided to improve their sleep quality. Since the present study was conducted only in one center with many referrals in Sarab City, it is recommended that the next studies be conducted in multicenter and larger hospitals. Prospective and longitudinal studies are also suggested.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Iran University of Medical Sciences (Code: IR.IUMS.REC.1400.854). We explained the study objectives, the voluntary nature of participation, the confidentiality of their information, and the right to withdraw from the study for the participants. They provided verbal informed consent to participate in the study.
Funding
The article was extracted from the MSc thesis of Aida Amirijavid, approved by Department of Community Health and Geriatric Nursing, Iran University of Medical Sciences.
Authors' contributions
All authors equally contributed in preparation of this paper.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their appreciation to financial support of the Iran University of Medical Sciences, study participants and the Imam Khomeini Research and Training Center, in Sarab, Iran, for their collaboration.
References
Akıncı, T. & Melek Başar, H., 2021. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep Medicine, 80, pp. 167-70. [DOI:10.1016/j.sleep.2021.01.034] [PMID] [PMCID]
Alqahtani, A. S., 2022. Impact of the loss of smell on the sleep quality and fatigue level in COVID 19 survivors. European Archives of Oto-Rhino-Laryngology, 279(9), PP. 4443–9. [DOI:10.1007/s00405-022-07381-z] [PMID] [PMCID]
Benítez, I. D., et al., 2022. Sleep and circadian health of critical COVID-19 survivors 3 months after hospital discharge. Critical Care Medicine, 50(6), pp. 945-54. [DOI:10.1097/CCM.0000000000005476] [PMID] [PMCID]
Buysse, D. J., et al., 1989. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), pp. 193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
Campo-Arias, A., Pedrozo-Pupo, J. C. & Caballero-Domínguez, C. C., 2022. Relation of perceived discrimination with depression, insomnia and post-traumatic stress in COVID-19 survivors. Psychiatry Research, 307, pp. 114337. [DOI:10.1016/j.psychres.2021.114337] [PMID] [PMCID]
Dimitrievski, A., et al., 2021. Towards detecting pneumonia progression in COVID-19 patients by monitoring sleep disturbance using data streams of non-invasive sensor networks. Sensors, 21(9), pp. 3030. [DOI:10.3390/s21093030] [PMID] [PMCID]
El Sayed, S., et al., 2021. Sleep in post-COVID-19 recovery period and its impact on different domains of quality of life. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery, 57(1), pp. 172 [DOI:10.1186/s41983-021-00429-7] [PMID] [PMCID]
NHS., 2020. After-care needs of inpatients recovering from COVID-19. London: NHS. [Link]
Fernández-de-Las-Peñas, C., et al., 2021. Anxiety, depression and poor sleep quality as long-term post-COVID sequelae in previously hospitalized patients: A multicenter study. The Journal of Infection, 83(4), pp. 496–522. [DOI:10.1016/j.jinf.2021.06.022] [PMID] [PMCID]
Fernández-de-Las-Peñas, C., et al., 2022. Differences in long-COVID symptoms between vaccinated and non-vaccinated (BNT162b2 Vaccine) hospitalized COVID-19 survivors infected with the delta variant. Vaccines, 10(9), pp. 1481. [DOI:10.3390/vaccines10091481] [PMID] [PMCID]
Fu, L., et al., 2022. Associations between COVID-19 related stigma and sleep quality among COVID-19 survivors six months after hospital discharge. Sleep Medicine, 91, pp. 273-81. [DOI:10.1016/j.sleep.2021.10.020] [PMID] [PMCID]
The Johns Hopkins University., 2022. What Is Coronavirus? Retrieved from: [Link]
Huang, C., et al., 2021. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet, 397(10270), pp. 220-32. [DOI:10.1016/S0140-6736(20)32656-8] [PMID]
Islam, K. U. & Iqbal, J., 2020. An update on molecular diagnostics for COVID-19. Frontiers in Cellular and Infection Microbiology, 10, pp. 560616. [DOI:10.3389/fcimb.2020.560616] [PMID] [PMCID]
Jahrami, H., et al., 2021. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. Journal of Clinical Sleep Medicine, 17(2), pp. 299-313. [DOI:10.5664/jcsm.8930] [PMID] [PMCID]
Jiang, Z., et al., 2021. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. Journal of Psychiatric Research, 136, pp. 595-602. [DOI:10.1016/j.jpsychires.2020.10.034] [PMID] [PMCID]
Koczulla, A. R., et al., 2021. Newly detected rapid eye movement associated sleep apnea after coronavirus disease 2019 as a possible cause for chronic fatigue: Two case reports. Journal of Medical Case Reports, 15(1), pp. 211. [DOI:10.1186/s13256-021-02819-0] [PMID] [PMCID]
Nasiri Ziba, F., Veisimiankali, M. & Haghani, H., 2020. [Association between demographic characteristics and sleep quality of elderly patients with coronary artery disease hospitalized in Imam Ali Hospital during 2018 (Persian)]. Journal of Ilam University of Medical Sciences, 28(1), pp. 1-11. [DOI:10.29252/sjimu.28.1.1]
Notarte, K. I., et al., 2022. Impact of COVID-19 vaccination on the risk of developing long-COVID and on existing long-COVID symptoms: A systematic review. EClinicalMedicine, 53, pp. 101624. [DOI:10.1016/j.eclinm.2022.101624] [PMID] [PMCID]
Pavli, A., Theodoridou, M. & Maltezou, H. C., 2021. Post-COVID syndrome: Incidence, clinical spectrum, and challenges for primary healthcare professionals. Archives of Medical Research, 52(6), pp. 575–81. [DOI:10.1016/j.arcmed.2021.03.010] [PMID] [PMCID]
Rajkumar, R. P., 2020. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, pp. 102066. [DOI:10.1016/j.ajp.2020.102066] [PMID] [PMCID]
Jha, V. M. & Jha, S. K., 2020. Sleep: Evolution and functions. Singapore: Springer. [Link]
Zhang, J., 2020. Mental disorders, fatigue, perceived event impact, and coping in post-illness patients with COVID-19 within 1 month after discharge: A case-controlled study. The Lancet, pp. 1-20. [Unpublished].
Type of Study: Research |
Subject:
Special
Received: 2022/12/28 | Accepted: 2023/04/11 | Published: 2023/08/24
Received: 2022/12/28 | Accepted: 2023/04/11 | Published: 2023/08/24
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |