Sun, Jul 13, 2025
[Archive]
Volume 9, Issue 3 (Summer 2023)
JCCNC 2023, 9(3): 207-214 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hassan Shahi R, Hosseini F, Akbari A, Reza Sayadi A, Shahabi Nedjad M. The Effects of Music Intervention on Respiratory Comfort, Anxiety, and Depression During Noninvasive Mechanical Ventilation Among Patients With COVID-19. JCCNC 2023; 9 (3) :207-214
URL: http://jccnc.iums.ac.ir/article-1-448-en.html
URL: http://jccnc.iums.ac.ir/article-1-448-en.html
Reyhaneh Hassan Shahi1 

 , Fatemeh Hosseini *2
, Fatemeh Hosseini *2 

 , Ali Akbari1
, Ali Akbari1 

 , Ahmadreza Reza Sayadi3
, Ahmadreza Reza Sayadi3 

 , Maryam Shahabi Nedjad1
, Maryam Shahabi Nedjad1 




 , Fatemeh Hosseini *2
, Fatemeh Hosseini *2 

 , Ali Akbari1
, Ali Akbari1 

 , Ahmadreza Reza Sayadi3
, Ahmadreza Reza Sayadi3 

 , Maryam Shahabi Nedjad1
, Maryam Shahabi Nedjad1 


1- Department of Medical Surgical Nursing, Social Determinants of Health Research Center, School of Nursing and Midwifery, Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
2- Department of Community Health Nursing, Social Determinants of Health Research Center, School of Nursing and Midwifery, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. ,hossini1389@yahoo.com
3- Department of Psychiatric Nursing, Social Determinants of Health Research Center, School of Nursing and Midwifery, Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
2- Department of Community Health Nursing, Social Determinants of Health Research Center, School of Nursing and Midwifery, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. ,
3- Department of Psychiatric Nursing, Social Determinants of Health Research Center, School of Nursing and Midwifery, Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
Full-Text [PDF 624 kb]
(725 Downloads)
| Abstract (HTML) (2018 Views)
Full-Text: (401 Views)
1. Introduction
he novel coronavirus disease 2019 (COVID-19) is a great healthcare challenge worldwide. It appeared in December 2019 and rapidly became a pandemic and serious international healthcare concern in January 2020 (Lai et al., 2020). The prevalence of COVID-19 was 526 million confirmed cases, and over 6 million deaths have been reported globally by May 2022 (Kim & Yeniova, 2022). Despite great efforts to manage the disease through worldwide vaccination, the prevalence and mortality rates are still high (Lai et al., 2020). The most prevalent symptoms of COVID-19 are high fever, cough, exhaustion, myalgia, and dyspnea (Guo et al., 2020). In severe cases, COVID-19 can progress to respiratory distress and cause acute respiratory distress syndrome (ARDS) (Guo et al., 2020). This syndrome is associated with severe respiratory shunt and hypoxia which are not manageable through simple oxygen therapy; thus, mechanical ventilation (MV) will be required (Yang et al., 2020).
Noninvasive ventilation (NIV) is a technique for ARDS management. NIV creates a continuous or intermittent positive pressure in the airways to keep alveoli open during inspiration and prevent their collapse during expiration (Grieco et al., 2021). MV reduces the workload of the respiratory muscles, improves gas exchange, and reduces respiratory effort. During NIV, patients should be conscious of expelling secretions. However, consciousness during NIV may reduce the patient’s ability to cope with MV and lead to MV intolerance. The symptoms of MV intolerance are respiratory discomfort and anxiety, which may increase the need for endotracheal intubation and invasive MV (Okba et al., 2020).
There are different pharmacological and non-pharmacological techniques to reduce MV intolerance among conscious patients. Pharmacological techniques include the use of mild sedative agents. However, these techniques are usually associated with respiratory depression and impaired patient collaboration (Carron et al., 2013). Non-pharmacological techniques such as distraction, heat or cold therapy, and music therapy are mostly noninvasive, safer, and less expensive than pharmacological methods (Hashemy & Zakerimoghadam, 2013). They do not alter patients’ consciousness and collaboration. These techniques can effectively reduce anxiety, fear, pain, and discomfort and improve MV parameters and MV tolerance (Zakeri-Moghadam et al., 2016).
Music therapy (MT) is one of the non-pharmacological techniques with potentially positive effects on anxiety, fever, and calmness (Head et al., 2022). MT is an accessible and applicable noninvasive technique widely used worldwide for anxiety management (Thoma et al., 2013). It reduces the level of stress hormones by affecting the amygdala but increases the level of endorphins (Messika et al., 2016), thereby decreasing heart rate and improving general health, well-being, and respiratory rhythm and depth (Barber, 2021). Previous studies reported that MT positively affects mood, emotions, and cardiovascular, endocrine, and respiratory systems and, thereby, reduces anxiety (Hole et al., 2015), depression (Burrai et al., 2020), blood pressure, respiratory rate, heart rate, and MV-associated discomfort and problems (Barber, 2021).
Despite the known positive effects of MT on different health-related outcomes, limited information is available about its applicability to MV tolerance in patients with COVID-19. Therefore, this study aimed to evaluate the effects of MT on respiratory comfort, anxiety, and depression among patients with COVID-19 under NIV.
2. Materials and Methods
This randomized control trial was conducted in 2021. The research has a pre-test & post-test design with a control group. The subjects were 66 patients selected from the COVID-19 intensive care unit (ICU) of Ali Ibn Abi Talib Hospital, Rafsanjan City, Iran. The inclusion criteria were as follows: Age of 20–65 years, NIV for the first time, full consciousness, informed consent for participation, no problem hearing or listening to music, previous history of psychological problems, no record of taking psychiatric medications, and no history of acute emotional stress in the last 6 months. The exclusion criteria were discontinuing participation in the study, early discharge from ICU, any problem interfering with the qualification to receive the study intervention, and death during the study.
The sample size was calculated by the Equation 1:
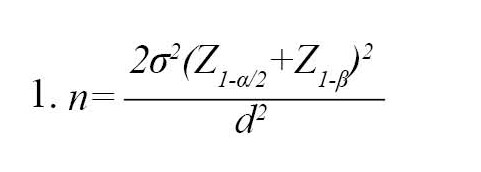
as 32 subjects per group, considering a standard deviation of 3.6, a confidence level of 0.95, a power of 0.85, and a d of 2.4 (Figure 1) (Mohammadi et al., 2014). Thus, 66 patients were recruited and divided into two groups of 33 people.

The subjects were assigned to either intervention or control study arms through the minimization method (a biased coin). Minimization has been suggested as the manner of choice for smaller trials to achieve equivalency in several prognostic factors (Anderson et al., 2008).
In this way, there was no significant difference between the studied arms regarding sociodemographic variables such as gender and age.
Data collection instruments
Data collection instruments were a demographic questionnaire, the hospital anxiety and depression scale (Zigmond & Snaith, 1983), and a visual analog scale (VAS).
The hospital anxiety and depression scale is a valid and reliable self-report 14-item scale for evaluating a patient’s anxiety and depression during the last week. It has a 7-item anxiety subscale and a 7-item depression subscale. Its items are scored on a 0–3 rating scale, and thereby, possible subscale scores are 0–21, which are interpreted as follows: Scores 0–7: Normal condition; 8–10: Mild problem; 11–14: Moderate problem; and 15–21: Severe problem. The response time of this scale is 5 minutes. A previous study in Iran reported this scale’s acceptable validity and reliability with a Cronbach α of 0.87 (Montazeri et al., 2003).
Respiratory comfort was assessed using a VAS (Messika et al., 2019; Price et al., 1983) developed this scale. The scale has been used to measure patients’ comfort in recent years. It is a 10-cm horizontal or vertical line with two ends representing the minimum and maximum scores for comfort (0-10 cm line) (Gift, 1989). In this scale, comfort has been defined as the lake of physical discomfort. Comfort scores of patients are documented by the researcher. The Iranian version of VAS has already been validated with good internal consistency.
Study intervention
The study intervention was 30 minutes of daily MT for 4 consecutive days implemented using the peace in dreamwork of Dr Arnd Stein (Messika et al., 2016). This work has a monotonous light theme without rhythmic and melodic stimuli (Zakeri-Moghadam et al., 2016). The first researcher implemented the MT intervention for each participant in the morning working shifts using an MP3 player and a JBL headphone (MBR-XB100VT). This headphone effectively reduces environmental noises. Participants in the control group received the same intervention while the MP3 player was turned off and headphones were in to reduce ambient noise. The headphone was disinfected after each use to reduce the risk of infection transmission. The levels of participants’ respiratory comfort, anxiety, and depression were assessed on the first day of NIV before and 4 days after the intervention. It is worth mentioning that the statistical analyst was unaware of the data of the intervention and control groups.
Data analysis
The SPSS software, version 16 was used for data analysis. The data were described using descriptive statistics, i.e. Mean±SD and frequency. The Kolmogorov-Smirnov test revealed the normal distribution of the study variables. Between-group comparisons were performed through the chi-square and independent samples t-tests, and within-group comparisons were performed using the paired-samples t-test. The level of significance was set at P<0.05.
3. Results
A total of 66 patients were recruited for the study. One participant from the control group was excluded due to developing critical conditions, and one from the intervention group due to early discharge from the ICU. Finally, the study was completed with 32 participants in each group (Figure 1).
The mean age of the subjects was 58.21±6.12 years in the control group and 57.02±6.41 years in the intervention group, and most participants were female in both groups (56.3%). There were no significant differences between the groups in terms of participants’ age, gender, level of education, occupation, history of COVID-19 affliction, history of other diseases, body mass index, history of drug abuse, and the results of COVID-19 PCR test (P>0.05, Table 1).

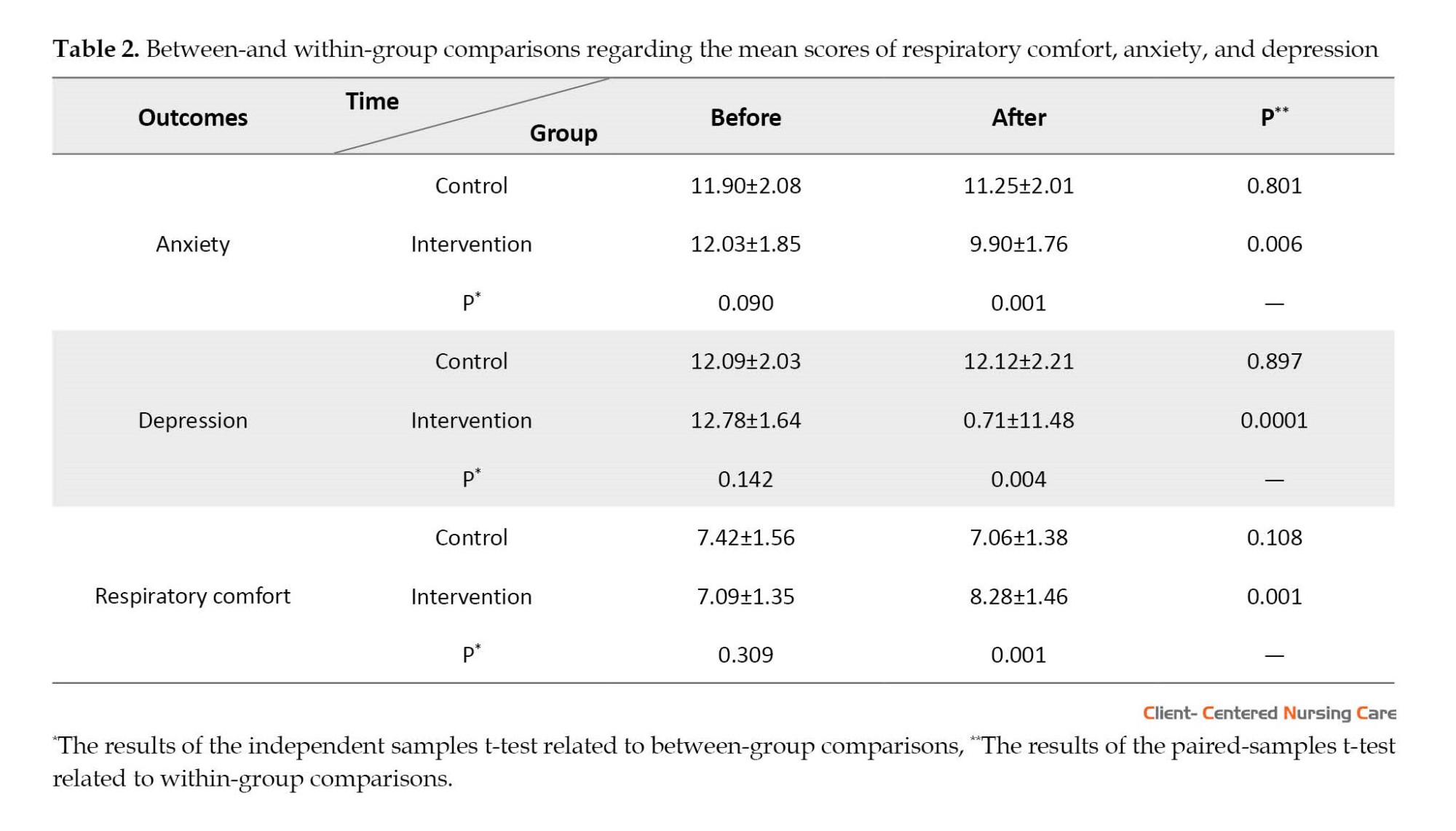
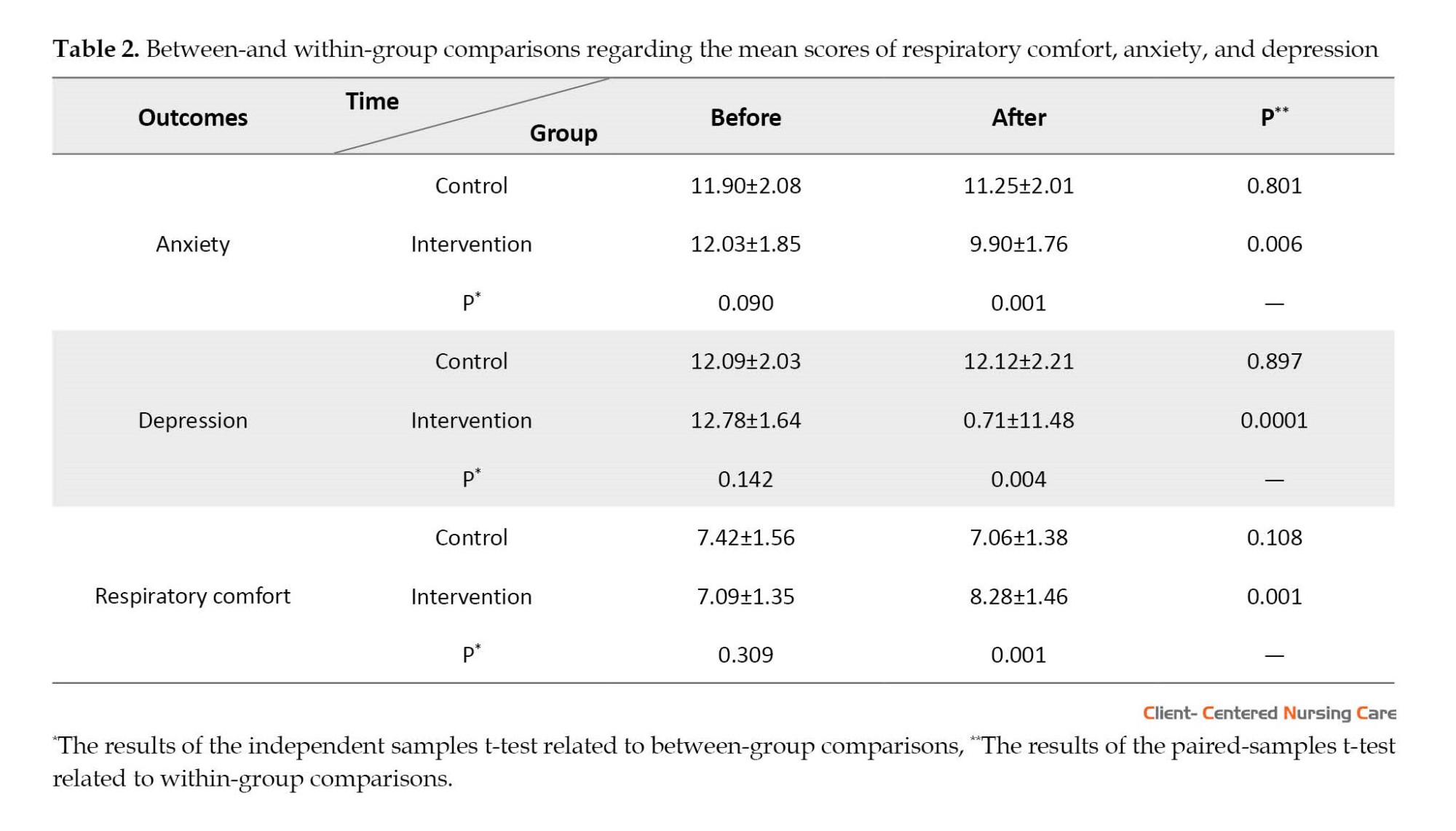
The study groups did not significantly differ from each other regarding the pre-test mean scores of respiratory comfort (P=0.309), anxiety (P=0.090), and depression (P=0.142). After the intervention, the level of anxiety (P=0.001) and depression (P=0.004) in the experimental group was significantly lower than in the control group. Moreover, the results of the paired-samples t-test revealed that, compared with baseline readings, the level of anxiety (P=0.006) and depression (P=0.0001) in the experimental group significantly decreased after the intervention. However, the level of anxiety (P=0.108) and depression (P=0.897) did not reduce significantly at the end of the study in the control group (Table 2). The independent t-test showed a significant difference (P=0.001) between the scores of the two groups after the intervention. Moreover, compared with the control group, the post-test mean scores of respiratory comfort were higher in the intervention group. But, the level of respiratory comfort in the control group did not decrease significantly at the end of the study (P=0.108). After the intervention, the average score of respiratory comfort increased (8.28±1.46).
4. Discussion
This study aimed to evaluate the effects of MT on respiratory comfort, anxiety, and depression among COVID-19 patients under NIV. The findings revealed the significant positive impact of MT on respiratory comfort, anxiety, and depression among these patients.
We found that MT significantly improved respiratory comfort. In agreement with this finding, a previous study showed that MT significantly has improved respiratory comfort and adherence to continuous positive airway pressure treatment among adult individuals with sleep apnea (Barber, 2021). Another study showed that MT improved respiratory comfort among children in pediatric ICU (Liu et al., 2019). Moreover, a survey of the effect of music on the difficulty of dyspnea, anxiety, and hemodynamic parameters in patients with dyspnea found that MT has significantly reduced the patients’ dyspnea severity and improved their hemodynamic parameters (Ergin et al., 2018). However, a study reported the inconsiderable effect of MT on respiratory comfort (Mateu‐Capell et al., 2019).
This contradiction may be due to the differences between the studies regarding their intervention goal to assess the effect of sound isolation versus music on the comfort of mechanically ventilated patients admitted. The mean of the subjects’ ages was 69 years in the above study.
The effects of MT depend on the type and characteristics of music and participants’ interest in listening to music (Yung et al., 2001).
We also found that MT has significantly reduced anxiety and depression among patients with COVID-19 under NIV. This finding is in line with the result of many previous studies reporting the significant positive effects of MT on anxiety (Dai et al., 2020; Nilsson, 2009; Packiam et al., 2018) and depression (Dai et al., 2020; Nilsson, 2009). Music probably reduces anxiety and depression and improves calmness by reducing negative emotions, regulating internal bodily processes, stimulating a neuro-vegetative response, and reducing stress (Rabiee et al., 2007). Contrary to our findings, a study showed that MT had no significant effects on anxiety and sedative exposure during weaning from MV (Hetland et al., 2017). An explanation for this contradiction is that our study was conducted on patients with COVID-19 under NIV, while that study was conducted during weaning from invasive MV. Many factors affect successful weaning, and it is a complex process. Moreover, patients under invasive MV receive sedatives that alter their consciousness and affect MT outcomes.
It is worth mentioning that the patient’s characteristics, the music therapist’s white uniform, and the patient’s focus and interest in the music might have affected the results.
5. Conclusion
This study shows the effectiveness of MT in improving respiratory comfort and reducing anxiety and depression among patients with COVID-19 under NIV. Given MT’s safety, simplicity, affordability, and easy applicability, nurses can use it to improve MV tolerance, care outcomes, and recovery among patients under MV. As there is no consensus over the best MT techniques, more studies are recommended to compare the effects of various MT interventions.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Rafsanjan University of Medical Sciences (Code: IR.RUMS.REC.1400.076). Besides, the study was registered as a clinical trial in the Iranian Registry of Clinical Trials (Code: IRCT20171002036498N5).
Funding
This article was extracted from MSc thesis of Reyhaneh Hassan Shahi, approved by Department of Medical Surgical Nursing, Rafsanjan University of Medical Science (Code: IR.RUMS.REC.1400.076).
Authors' contributions
Conceptualization, study design and administration: Ali Akbari; Data collection: Reyhana Hassan Shahi; Data analysis: Fatemeh Hosseini; Data analysis: Ahmad Reza Sayadi; Writing the initial draft: Maryam Shahabi Nedjad; Reviewed the results and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We want to thank all patients who participated in this study.
References
Andersen, B. L., et al., 2008. Psychologic intervention improves survival for breast cancer patients: A randomized clinical trial. Cancer, 113(12), pp. 3450-8. [DOI:10.1002/cncr.23969] [PMID] [PMCID]
Barber, T., 2021. Effectiveness of music on comfort and adherence to continuous positive airway pressure therapy in an adult population with obstructive sleep apnea [BSc. thesis]. Florida: Jacksonville University. [Link]
Burrai, F., et al., 2020. Beneficial effects of listening to classical music in patients with heart failure: A randomized controlled trial. Journal of Cardiac Failure, 26(7), pp. 541-9. [PMID]
Carron, M., et al., 2013. Complications of non-invasive ventilation techniques: A comprehensive qualitative review of randomized trials. British Journal of Anaesthesia, 110(6), pp. 896-914 [DOI:10.1093/bja/aet070] [PMID]
Dai, W. S., et al., 2020. The effect of music therapy on pain, anxiety and depression in patients after coronary artery bypass grafting. Journal of Cardiothoracic Surgery, 15(1), pp. 81. [PMID] [PMCID]
Ergin, E., Sagkal Midilli, T. & Baysal, E., 2018. The effect of music on dyspnea severity, anxiety, and hemodynamic parameters in patients with dyspnea. Journal of Hospice & Palliative Nursing, 20(1), pp. 81-7. [DOI:10.1097/NJH.0000000000000403] [PMID]
Gift, A. G., 1989. Visual analogue scales: Measurement of subjective phenomena. Nursing Research, 38(5), pp. 286-8. [DOI:10.1097/00006199-198909000-00006] [PMID]
Grieco, D. L., et al., 2021. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Medicine, 47(8), pp. 851–66. [DOI:10.1007/s00134-021-06459-2] [PMID] [PMCID]
Guo, L., et al., 2020. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19). Clinical Infectious Diseases, 71(15), pp. 778-85. [DOI:10.1093/cid/ciaa310] [PMID] [PMCID]
Hashemy, S. & Zakerimoghadam, M., 2013. [Comparative study of the effect of muscle relaxation and music therapy on anxiety level in patients waiting for cardiac catheterization (Persian)]. Iranian Journal of Cardiovascular Nursing, 1(4), pp. 22-30. [Link]
Head, J., et al., 2022. Positive Stimulation for Medically Sedated Patients (PSMSP): A music therapy intervention to treat sedation-related delirium in critical care. Chest, 162(2), pp. 367–74. [DOI:10.1016/j.chest.2022.02.011] [PMID]
Hetland, B., et al., 2017. Predictive associations of music, anxiety, and sedative exposure on mechanical ventilation weaning trials. American Journal of Critical Care, 26(3), pp. 210-20. [DOI:10.4037/ajcc2017468] [PMID] [PMCID]
Hole, J., et al., 2015. Music as an aid for postoperative recovery in adults: A systematic review and meta-analysis. The Lancet, 386(10004), pp. 1659-71. [PMID]
Kim, J. W., 2021. Regional and chronological variation of chemosensory dysfunction in COVID-19: A meta-analysis. Journal of Korean Medical Science, 36(4), pp. e40. [PMID]
Lai, C. C., et al., 2020. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents, 55(3), pp. 105924. [PMID]
Liu, M. H., et al., 2019. Effect of personalized music intervention in mechanically ventilated children in pediatric ICU: A pilot study. Pediatric Critical Care Medicine, 21(1), pp. e8–e14. [DOI:10.1097/PCC.0000000000002159] [PMID]
Mateu‐Capell, M., et al., 2019. Sound isolation and music on the comfort of mechanically ventilated critical patients. Nursing in Critical Care, 24(5), pp. 290-8. [DOI:10.1111/nicc.12407] [PMID]
Messika, J., et al., 2016. Effect of a musical intervention on tolerance and efficacy of noninvasive ventilation in the ICU: Study protocol for a randomized controlled trial (MUSique pour l’Insuffisance Respiratoire Aigue-Mus-IRA). Trials, 17(1), pp. 450. [PMID] [PMCID]
Messika, J., et al., 2019. A musical intervention for respiratory comfort during noninvasive ventilation in the ICU. European Respiratory Journal, 53(1), pp. 1801873. [DOI:10.1183/13993003.01873-2018] [PMID]
Mohammadi, A., et al., 2014. Effects of music listening on preoperative state anxiety and physiological parameters in patients undergoing general surgery: A randomized quasi-experimental trail. Central European Journal of Nursing and Midwifery, 5(4), pp. 156-60. [DOI:10.15452/CEJNM.2014.05.0011]
Montazeri, A., et al., 2003. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health and Quality of Life Outcomes, 1, pp. 14. [PMID] [PMCID]
Nilsson, U., 2009. Soothing music can increase oxytocin levels during bed rest after open‐heart surgery: A randomised control trial. Journal of Clinical Nursing, 18(15), pp. 2153-61. [PMID]
Okba, N., et al., 2020. Severe acute respiratory syndrome coronavirus 2− specific antibody responses in coronavirus disease patients. Emerging Infectious Diseases, 26(7), pp. 1478–88.[DOI:10.3201/eid2607.200841] [PMID] [PMCID]
Packiam, V. T., et al., 2018. No effect of music on anxiety and pain during transrectal prostate biopsies: A randomized trial. Urology, 117, pp. 31-5. [PMID]
Price, D. D., et al., 1983. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain, 17(1), pp. 45-56. [DOI:10.1016/0304-3959(83)90126-4] [PMID]
Rabiee, M., et al., 2007. [The effect of music on the rate of anxiety among hospitalized children (Persian)]. Journal of Gorgan University of Medical Sciences, 9(3), pp. 59-64 . [Link]
Thoma, M. V., et al., 2013. The effect of music on the human stress response. PloS One, 8(8), e70156. [DOI:10.1371/journal.pone.0070156] [PMID] [PMCID]
Yang, X., et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. The Lancet Respiratory Medicine, 8(5), pp. 475-81. [PMID]
Yung, P., French, P. & Leung, B., 2001. Relaxation training as complementary therapy for mild hypertension control and the implications of evidence-based medicine. Complementary Therapies in Nursing and Midwifery, 7(2), pp. 59-65. [DOI:10.1054/ctnm.2000.0523] [PMID]
Zakeri-Moghadam, M., et al., 2016. [The effect of music therapy on ventilation criteria in patients undergoing mechanical ventilation (Persian)]. Iranian Journal of Cardiovascular Nursing, 5(2), 30-7. [Link]
Zigmond, A. S. & Snaith, R. P., 1983. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), pp. 361-70. [DOI:10.1111/j.1600-0447.1983.tb09716.x] [PMID]
he novel coronavirus disease 2019 (COVID-19) is a great healthcare challenge worldwide. It appeared in December 2019 and rapidly became a pandemic and serious international healthcare concern in January 2020 (Lai et al., 2020). The prevalence of COVID-19 was 526 million confirmed cases, and over 6 million deaths have been reported globally by May 2022 (Kim & Yeniova, 2022). Despite great efforts to manage the disease through worldwide vaccination, the prevalence and mortality rates are still high (Lai et al., 2020). The most prevalent symptoms of COVID-19 are high fever, cough, exhaustion, myalgia, and dyspnea (Guo et al., 2020). In severe cases, COVID-19 can progress to respiratory distress and cause acute respiratory distress syndrome (ARDS) (Guo et al., 2020). This syndrome is associated with severe respiratory shunt and hypoxia which are not manageable through simple oxygen therapy; thus, mechanical ventilation (MV) will be required (Yang et al., 2020).
Noninvasive ventilation (NIV) is a technique for ARDS management. NIV creates a continuous or intermittent positive pressure in the airways to keep alveoli open during inspiration and prevent their collapse during expiration (Grieco et al., 2021). MV reduces the workload of the respiratory muscles, improves gas exchange, and reduces respiratory effort. During NIV, patients should be conscious of expelling secretions. However, consciousness during NIV may reduce the patient’s ability to cope with MV and lead to MV intolerance. The symptoms of MV intolerance are respiratory discomfort and anxiety, which may increase the need for endotracheal intubation and invasive MV (Okba et al., 2020).
There are different pharmacological and non-pharmacological techniques to reduce MV intolerance among conscious patients. Pharmacological techniques include the use of mild sedative agents. However, these techniques are usually associated with respiratory depression and impaired patient collaboration (Carron et al., 2013). Non-pharmacological techniques such as distraction, heat or cold therapy, and music therapy are mostly noninvasive, safer, and less expensive than pharmacological methods (Hashemy & Zakerimoghadam, 2013). They do not alter patients’ consciousness and collaboration. These techniques can effectively reduce anxiety, fear, pain, and discomfort and improve MV parameters and MV tolerance (Zakeri-Moghadam et al., 2016).
Music therapy (MT) is one of the non-pharmacological techniques with potentially positive effects on anxiety, fever, and calmness (Head et al., 2022). MT is an accessible and applicable noninvasive technique widely used worldwide for anxiety management (Thoma et al., 2013). It reduces the level of stress hormones by affecting the amygdala but increases the level of endorphins (Messika et al., 2016), thereby decreasing heart rate and improving general health, well-being, and respiratory rhythm and depth (Barber, 2021). Previous studies reported that MT positively affects mood, emotions, and cardiovascular, endocrine, and respiratory systems and, thereby, reduces anxiety (Hole et al., 2015), depression (Burrai et al., 2020), blood pressure, respiratory rate, heart rate, and MV-associated discomfort and problems (Barber, 2021).
Despite the known positive effects of MT on different health-related outcomes, limited information is available about its applicability to MV tolerance in patients with COVID-19. Therefore, this study aimed to evaluate the effects of MT on respiratory comfort, anxiety, and depression among patients with COVID-19 under NIV.
2. Materials and Methods
This randomized control trial was conducted in 2021. The research has a pre-test & post-test design with a control group. The subjects were 66 patients selected from the COVID-19 intensive care unit (ICU) of Ali Ibn Abi Talib Hospital, Rafsanjan City, Iran. The inclusion criteria were as follows: Age of 20–65 years, NIV for the first time, full consciousness, informed consent for participation, no problem hearing or listening to music, previous history of psychological problems, no record of taking psychiatric medications, and no history of acute emotional stress in the last 6 months. The exclusion criteria were discontinuing participation in the study, early discharge from ICU, any problem interfering with the qualification to receive the study intervention, and death during the study.
The sample size was calculated by the Equation 1:
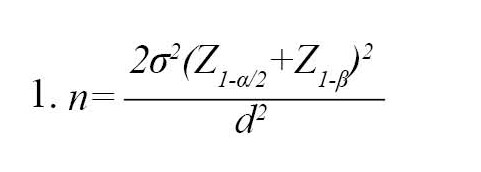
as 32 subjects per group, considering a standard deviation of 3.6, a confidence level of 0.95, a power of 0.85, and a d of 2.4 (Figure 1) (Mohammadi et al., 2014). Thus, 66 patients were recruited and divided into two groups of 33 people.

The subjects were assigned to either intervention or control study arms through the minimization method (a biased coin). Minimization has been suggested as the manner of choice for smaller trials to achieve equivalency in several prognostic factors (Anderson et al., 2008).
In this way, there was no significant difference between the studied arms regarding sociodemographic variables such as gender and age.
Data collection instruments
Data collection instruments were a demographic questionnaire, the hospital anxiety and depression scale (Zigmond & Snaith, 1983), and a visual analog scale (VAS).
The hospital anxiety and depression scale is a valid and reliable self-report 14-item scale for evaluating a patient’s anxiety and depression during the last week. It has a 7-item anxiety subscale and a 7-item depression subscale. Its items are scored on a 0–3 rating scale, and thereby, possible subscale scores are 0–21, which are interpreted as follows: Scores 0–7: Normal condition; 8–10: Mild problem; 11–14: Moderate problem; and 15–21: Severe problem. The response time of this scale is 5 minutes. A previous study in Iran reported this scale’s acceptable validity and reliability with a Cronbach α of 0.87 (Montazeri et al., 2003).
Respiratory comfort was assessed using a VAS (Messika et al., 2019; Price et al., 1983) developed this scale. The scale has been used to measure patients’ comfort in recent years. It is a 10-cm horizontal or vertical line with two ends representing the minimum and maximum scores for comfort (0-10 cm line) (Gift, 1989). In this scale, comfort has been defined as the lake of physical discomfort. Comfort scores of patients are documented by the researcher. The Iranian version of VAS has already been validated with good internal consistency.
Study intervention
The study intervention was 30 minutes of daily MT for 4 consecutive days implemented using the peace in dreamwork of Dr Arnd Stein (Messika et al., 2016). This work has a monotonous light theme without rhythmic and melodic stimuli (Zakeri-Moghadam et al., 2016). The first researcher implemented the MT intervention for each participant in the morning working shifts using an MP3 player and a JBL headphone (MBR-XB100VT). This headphone effectively reduces environmental noises. Participants in the control group received the same intervention while the MP3 player was turned off and headphones were in to reduce ambient noise. The headphone was disinfected after each use to reduce the risk of infection transmission. The levels of participants’ respiratory comfort, anxiety, and depression were assessed on the first day of NIV before and 4 days after the intervention. It is worth mentioning that the statistical analyst was unaware of the data of the intervention and control groups.
Data analysis
The SPSS software, version 16 was used for data analysis. The data were described using descriptive statistics, i.e. Mean±SD and frequency. The Kolmogorov-Smirnov test revealed the normal distribution of the study variables. Between-group comparisons were performed through the chi-square and independent samples t-tests, and within-group comparisons were performed using the paired-samples t-test. The level of significance was set at P<0.05.
3. Results
A total of 66 patients were recruited for the study. One participant from the control group was excluded due to developing critical conditions, and one from the intervention group due to early discharge from the ICU. Finally, the study was completed with 32 participants in each group (Figure 1).
The mean age of the subjects was 58.21±6.12 years in the control group and 57.02±6.41 years in the intervention group, and most participants were female in both groups (56.3%). There were no significant differences between the groups in terms of participants’ age, gender, level of education, occupation, history of COVID-19 affliction, history of other diseases, body mass index, history of drug abuse, and the results of COVID-19 PCR test (P>0.05, Table 1).

The study groups did not significantly differ from each other regarding the pre-test mean scores of respiratory comfort (P=0.309), anxiety (P=0.090), and depression (P=0.142). After the intervention, the level of anxiety (P=0.001) and depression (P=0.004) in the experimental group was significantly lower than in the control group. Moreover, the results of the paired-samples t-test revealed that, compared with baseline readings, the level of anxiety (P=0.006) and depression (P=0.0001) in the experimental group significantly decreased after the intervention. However, the level of anxiety (P=0.108) and depression (P=0.897) did not reduce significantly at the end of the study in the control group (Table 2). The independent t-test showed a significant difference (P=0.001) between the scores of the two groups after the intervention. Moreover, compared with the control group, the post-test mean scores of respiratory comfort were higher in the intervention group. But, the level of respiratory comfort in the control group did not decrease significantly at the end of the study (P=0.108). After the intervention, the average score of respiratory comfort increased (8.28±1.46).
4. Discussion
This study aimed to evaluate the effects of MT on respiratory comfort, anxiety, and depression among COVID-19 patients under NIV. The findings revealed the significant positive impact of MT on respiratory comfort, anxiety, and depression among these patients.
We found that MT significantly improved respiratory comfort. In agreement with this finding, a previous study showed that MT significantly has improved respiratory comfort and adherence to continuous positive airway pressure treatment among adult individuals with sleep apnea (Barber, 2021). Another study showed that MT improved respiratory comfort among children in pediatric ICU (Liu et al., 2019). Moreover, a survey of the effect of music on the difficulty of dyspnea, anxiety, and hemodynamic parameters in patients with dyspnea found that MT has significantly reduced the patients’ dyspnea severity and improved their hemodynamic parameters (Ergin et al., 2018). However, a study reported the inconsiderable effect of MT on respiratory comfort (Mateu‐Capell et al., 2019).
This contradiction may be due to the differences between the studies regarding their intervention goal to assess the effect of sound isolation versus music on the comfort of mechanically ventilated patients admitted. The mean of the subjects’ ages was 69 years in the above study.
The effects of MT depend on the type and characteristics of music and participants’ interest in listening to music (Yung et al., 2001).
We also found that MT has significantly reduced anxiety and depression among patients with COVID-19 under NIV. This finding is in line with the result of many previous studies reporting the significant positive effects of MT on anxiety (Dai et al., 2020; Nilsson, 2009; Packiam et al., 2018) and depression (Dai et al., 2020; Nilsson, 2009). Music probably reduces anxiety and depression and improves calmness by reducing negative emotions, regulating internal bodily processes, stimulating a neuro-vegetative response, and reducing stress (Rabiee et al., 2007). Contrary to our findings, a study showed that MT had no significant effects on anxiety and sedative exposure during weaning from MV (Hetland et al., 2017). An explanation for this contradiction is that our study was conducted on patients with COVID-19 under NIV, while that study was conducted during weaning from invasive MV. Many factors affect successful weaning, and it is a complex process. Moreover, patients under invasive MV receive sedatives that alter their consciousness and affect MT outcomes.
It is worth mentioning that the patient’s characteristics, the music therapist’s white uniform, and the patient’s focus and interest in the music might have affected the results.
5. Conclusion
This study shows the effectiveness of MT in improving respiratory comfort and reducing anxiety and depression among patients with COVID-19 under NIV. Given MT’s safety, simplicity, affordability, and easy applicability, nurses can use it to improve MV tolerance, care outcomes, and recovery among patients under MV. As there is no consensus over the best MT techniques, more studies are recommended to compare the effects of various MT interventions.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Rafsanjan University of Medical Sciences (Code: IR.RUMS.REC.1400.076). Besides, the study was registered as a clinical trial in the Iranian Registry of Clinical Trials (Code: IRCT20171002036498N5).
Funding
This article was extracted from MSc thesis of Reyhaneh Hassan Shahi, approved by Department of Medical Surgical Nursing, Rafsanjan University of Medical Science (Code: IR.RUMS.REC.1400.076).
Authors' contributions
Conceptualization, study design and administration: Ali Akbari; Data collection: Reyhana Hassan Shahi; Data analysis: Fatemeh Hosseini; Data analysis: Ahmad Reza Sayadi; Writing the initial draft: Maryam Shahabi Nedjad; Reviewed the results and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We want to thank all patients who participated in this study.
References
Andersen, B. L., et al., 2008. Psychologic intervention improves survival for breast cancer patients: A randomized clinical trial. Cancer, 113(12), pp. 3450-8. [DOI:10.1002/cncr.23969] [PMID] [PMCID]
Barber, T., 2021. Effectiveness of music on comfort and adherence to continuous positive airway pressure therapy in an adult population with obstructive sleep apnea [BSc. thesis]. Florida: Jacksonville University. [Link]
Burrai, F., et al., 2020. Beneficial effects of listening to classical music in patients with heart failure: A randomized controlled trial. Journal of Cardiac Failure, 26(7), pp. 541-9. [PMID]
Carron, M., et al., 2013. Complications of non-invasive ventilation techniques: A comprehensive qualitative review of randomized trials. British Journal of Anaesthesia, 110(6), pp. 896-914 [DOI:10.1093/bja/aet070] [PMID]
Dai, W. S., et al., 2020. The effect of music therapy on pain, anxiety and depression in patients after coronary artery bypass grafting. Journal of Cardiothoracic Surgery, 15(1), pp. 81. [PMID] [PMCID]
Ergin, E., Sagkal Midilli, T. & Baysal, E., 2018. The effect of music on dyspnea severity, anxiety, and hemodynamic parameters in patients with dyspnea. Journal of Hospice & Palliative Nursing, 20(1), pp. 81-7. [DOI:10.1097/NJH.0000000000000403] [PMID]
Gift, A. G., 1989. Visual analogue scales: Measurement of subjective phenomena. Nursing Research, 38(5), pp. 286-8. [DOI:10.1097/00006199-198909000-00006] [PMID]
Grieco, D. L., et al., 2021. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Medicine, 47(8), pp. 851–66. [DOI:10.1007/s00134-021-06459-2] [PMID] [PMCID]
Guo, L., et al., 2020. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19). Clinical Infectious Diseases, 71(15), pp. 778-85. [DOI:10.1093/cid/ciaa310] [PMID] [PMCID]
Hashemy, S. & Zakerimoghadam, M., 2013. [Comparative study of the effect of muscle relaxation and music therapy on anxiety level in patients waiting for cardiac catheterization (Persian)]. Iranian Journal of Cardiovascular Nursing, 1(4), pp. 22-30. [Link]
Head, J., et al., 2022. Positive Stimulation for Medically Sedated Patients (PSMSP): A music therapy intervention to treat sedation-related delirium in critical care. Chest, 162(2), pp. 367–74. [DOI:10.1016/j.chest.2022.02.011] [PMID]
Hetland, B., et al., 2017. Predictive associations of music, anxiety, and sedative exposure on mechanical ventilation weaning trials. American Journal of Critical Care, 26(3), pp. 210-20. [DOI:10.4037/ajcc2017468] [PMID] [PMCID]
Hole, J., et al., 2015. Music as an aid for postoperative recovery in adults: A systematic review and meta-analysis. The Lancet, 386(10004), pp. 1659-71. [PMID]
Kim, J. W., 2021. Regional and chronological variation of chemosensory dysfunction in COVID-19: A meta-analysis. Journal of Korean Medical Science, 36(4), pp. e40. [PMID]
Lai, C. C., et al., 2020. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents, 55(3), pp. 105924. [PMID]
Liu, M. H., et al., 2019. Effect of personalized music intervention in mechanically ventilated children in pediatric ICU: A pilot study. Pediatric Critical Care Medicine, 21(1), pp. e8–e14. [DOI:10.1097/PCC.0000000000002159] [PMID]
Mateu‐Capell, M., et al., 2019. Sound isolation and music on the comfort of mechanically ventilated critical patients. Nursing in Critical Care, 24(5), pp. 290-8. [DOI:10.1111/nicc.12407] [PMID]
Messika, J., et al., 2016. Effect of a musical intervention on tolerance and efficacy of noninvasive ventilation in the ICU: Study protocol for a randomized controlled trial (MUSique pour l’Insuffisance Respiratoire Aigue-Mus-IRA). Trials, 17(1), pp. 450. [PMID] [PMCID]
Messika, J., et al., 2019. A musical intervention for respiratory comfort during noninvasive ventilation in the ICU. European Respiratory Journal, 53(1), pp. 1801873. [DOI:10.1183/13993003.01873-2018] [PMID]
Mohammadi, A., et al., 2014. Effects of music listening on preoperative state anxiety and physiological parameters in patients undergoing general surgery: A randomized quasi-experimental trail. Central European Journal of Nursing and Midwifery, 5(4), pp. 156-60. [DOI:10.15452/CEJNM.2014.05.0011]
Montazeri, A., et al., 2003. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health and Quality of Life Outcomes, 1, pp. 14. [PMID] [PMCID]
Nilsson, U., 2009. Soothing music can increase oxytocin levels during bed rest after open‐heart surgery: A randomised control trial. Journal of Clinical Nursing, 18(15), pp. 2153-61. [PMID]
Okba, N., et al., 2020. Severe acute respiratory syndrome coronavirus 2− specific antibody responses in coronavirus disease patients. Emerging Infectious Diseases, 26(7), pp. 1478–88.[DOI:10.3201/eid2607.200841] [PMID] [PMCID]
Packiam, V. T., et al., 2018. No effect of music on anxiety and pain during transrectal prostate biopsies: A randomized trial. Urology, 117, pp. 31-5. [PMID]
Price, D. D., et al., 1983. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain, 17(1), pp. 45-56. [DOI:10.1016/0304-3959(83)90126-4] [PMID]
Rabiee, M., et al., 2007. [The effect of music on the rate of anxiety among hospitalized children (Persian)]. Journal of Gorgan University of Medical Sciences, 9(3), pp. 59-64 . [Link]
Thoma, M. V., et al., 2013. The effect of music on the human stress response. PloS One, 8(8), e70156. [DOI:10.1371/journal.pone.0070156] [PMID] [PMCID]
Yang, X., et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. The Lancet Respiratory Medicine, 8(5), pp. 475-81. [PMID]
Yung, P., French, P. & Leung, B., 2001. Relaxation training as complementary therapy for mild hypertension control and the implications of evidence-based medicine. Complementary Therapies in Nursing and Midwifery, 7(2), pp. 59-65. [DOI:10.1054/ctnm.2000.0523] [PMID]
Zakeri-Moghadam, M., et al., 2016. [The effect of music therapy on ventilation criteria in patients undergoing mechanical ventilation (Persian)]. Iranian Journal of Cardiovascular Nursing, 5(2), 30-7. [Link]
Zigmond, A. S. & Snaith, R. P., 1983. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), pp. 361-70. [DOI:10.1111/j.1600-0447.1983.tb09716.x] [PMID]
Type of Study: Research |
Subject:
General
Received: 2022/12/28 | Accepted: 2023/04/16 | Published: 2023/08/24
Received: 2022/12/28 | Accepted: 2023/04/16 | Published: 2023/08/24
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |