Tue, Jul 16, 2024
[Archive]
Volume 9, Issue 4 (Autumn 2023)
JCCNC 2023, 9(4): 277-286 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Najafi Ghezeljeh T, Jaber Muhaibes F, Haghani S, Kifah Mubdir A. Nurses’ Knowledge and Ability to Diagnose Delirium in Intensive Care Units of Iraq Teaching Hospitals. JCCNC 2023; 9 (4) :277-286
URL: http://jccnc.iums.ac.ir/article-1-449-en.html
URL: http://jccnc.iums.ac.ir/article-1-449-en.html
1- Nursing and Midwifery Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Nursing, Mustaqbel College University, Babylon, Iraq.
3- Nursing Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,abbaskefah123@gmail.com
2- Department of Nursing, Mustaqbel College University, Babylon, Iraq.
3- Nursing Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 574 kb]
(238 Downloads)
| Abstract (HTML) (850 Views)
Delirium, a common and serious clinical problem in ICUs, is associated with an increased risk of morbidity, mortality, and healthcare costs.
• The nurses’ knowledge of delirium and ability to recognize it were low.
• The lowest average of knowledge pertained to delirium’s incidence, signs, and symptoms, and the highest average to delirium’s risk factors and causes.
• Knowledge about delirium was significantly associated with undertaking delirium training courses and working experiences in ICUs.
Plain Language Summary
The incidence and prevalence of delirium in intensive care units (ICUs) are very high, imposing burdens on nurses and places a significant financial burden on national healthcare systems every year. This study aimed to investigate whether ICU nurses in Iraq are knowledgeable about delirium and capable of recognizing it. The results showed that the nurses’ knowledge of delirium and ability to recognize it were low. In addition, participation in delirium courses and increased work experience in ICUs may increase the nurses’ knowledge about delirium.
• The nurses’ knowledge of delirium and ability to recognize it were low.
• The lowest average of knowledge pertained to delirium’s incidence, signs, and symptoms, and the highest average to delirium’s risk factors and causes.
• Knowledge about delirium was significantly associated with undertaking delirium training courses and working experiences in ICUs.
Plain Language Summary
The incidence and prevalence of delirium in intensive care units (ICUs) are very high, imposing burdens on nurses and places a significant financial burden on national healthcare systems every year. This study aimed to investigate whether ICU nurses in Iraq are knowledgeable about delirium and capable of recognizing it. The results showed that the nurses’ knowledge of delirium and ability to recognize it were low. In addition, participation in delirium courses and increased work experience in ICUs may increase the nurses’ knowledge about delirium.
Full-Text: (113 Views)
1. Introduction
elirium is an acute, transient disruption of awareness characterized by various symptoms. The incidence of this disorder in intensive care units (ICUs) is very high, placing a lot of strain on nurses, leading to many adverse consequences for the patients. Ultimately, it imposes enormous costs on countries’ healthcare systems every year. If the complications of delirium are properly addressed, the recovery time will be faster (Erber, 2012). Delirium is a common disorder among critically ill patients, a fatal condition with few effective treatments (Reznik & Slooter, 2019). Between 25% and 80% of patients in ICUs experience delirium, with mechanically ventilated patients exhibiting a higher frequency. Delirium is associated with longer stays in the ICUs, a higher 6-month mortality, and elevated morbidity rates (Collet et al., 2018; Slooter et al., 2017). On average, delirium affects 29% during an ICU stay (Rood et al., 2018). It is associated with a poor, stressful prognosis for patients and their families (Slooter et al., 2017). Besides its complications, it results in expensive medical care, and less favorable outcomes. Healthcare costs related to delirium are estimated at more than $164 billion annually. The risk of death from delirium is 2 to 4 times higher in ICUs, increases the risk of death over 6 months by 70% in patients presenting to the emergency department (Hshieh et al., 2020).
Delirium can be further classified into three subcategories based on the motor activity profiles: Mixed, hypoactive, and hyperactive. These different subgroups vary in physiology, incidence rates, the length of the delirium event, treatment, and patient outcomes (Morandi et al., 2017). Patients with a hypoactive subtype show lethargy, little spontaneous movements, and delayed response to questions, which might be misconstrued as grief or dementia. Patients with hyperactive delirium are physically aggressive, agitated, and restless. They also frequently experience delusions and hallucinations. Furthermore, individuals with mixed delirium show signs of both hypoactive and hyperactive categories (Oh et al., 2017). A multi-professional team consultation is crucial to deal with delirium as it is a clinical emergency significantly affecting ICU patients’ survival (Ribeiro et al., 2015).
Early recognition of delirium is essential, and ICU staff should monitor its occurrence, while focusing on managing and preventing it (Park et al., 2019). Nurses and doctors should rely on their collective experience and the latest available data to determine the best course for managing ICU delirious patients (Collet et al., 2019).
Furthermore, delirium presents a dangerous condition that needs to be quickly diagnosed and treated in ICUs. The first step in preventing delirium is recognizing and comprehending the risk factors and triggering variables. Nurses must have the required education, skills, and experience to participate in diagnosing and treating delirium actively. ICU nursing is a complex and challenging job, where many patients are involved in this complex situation, an insight following the researcher’s experience as an ICU nurse.
The prevention and management of delirium is essential in the ICU, and nurses’ knowledge and ability will play a prominent role in following delirium prevention and treatment guidelines. However, the Iraqi health sector, like other sectors, is affected by the political, social, and cultural changes, the current security situation, and infrastructure destruction. Based on the researcher’s experience as an ICU nurse member, ICU nursing personnel operate in a complex and challenging area. In Iraq’s healthcare system, baccalaureate, technical, and skilled nurses all fall under the “graduate-trained nurses” category and work together.
Based on the literature review, no study was found regarding the knowledge and recognition ability of ICU Iraqi nurses about delirium. Accordingly, this study was carried out to determine the Iraqi nurses’ knowledge and recognition ability of delirium in the ICUs of this country.
2. Materials and Methods
This descriptive, cross-sectional study was carried out in Iraq in 2022. Hospital ICUs in Babylon, Al-Diwaniyah, and Karbala were the study settings. The participating hospitals included Imam Al-Sadiq Hospital, Al-Hilla General Teaching Hospital, Imam Al-Hussein Medical City, Al-Hindiya General Hospital, and Al-Diwaniyah Teaching Hospital. Except for the Al-Hindiya General Hospital, located in the easternmost governorate of Karbala, the other hospitals, each of which has one ICU, are located in the governorates’ centers in the cities of Babylon, Al-Diwaniyah, and Karbala. The inclusion criteria were having a university degree in nursing, giving direct care (clinical bedside) to the patients in the ICU, and consenting to participate in the study. Accordingly, all nurses with bachelor’s degrees working in the ICUs of the previously mentioned teaching hospitals represented the research sample. The subjects were recruited by census; ultimately, 154 nurses agreed to participate in the study.
The study data were gathered from August to September 2022, using a demographic information questionnaire created by the researcher, the delirium knowledge questionnaire (DKQ), and a case vignette to identify delirium.
The demographic information questionnaire included the nurses’ age, gender, marital status, type of shift, years of experience in the ICU, and education level history of taking delirium-related training within the previous 5 years.
The DKQ was devised by Detroyer et al. (2016) based on a questionnaire by Hare et al. (2008). It serves to evaluate all aspects of delirium knowledge. This 35-item true/false tool has 3 domains: 1) Knowledge related to the appearance, symptoms, and consequences of delirium (10 items), 2) Its underlying and risk factors (11 items), and 3) Delirium prevention and management approaches (14 items). Each question receives a score of 1 for a correct response and 0 for a wrong response, or “I don’t know.” The sum of the correct responses determines the final grade for delirium knowledge, ranging from 0 to 35, with a higher score indicating a deeper understanding of delirium.
The questionnaire was first subjected to forward translation from English to Arabic. Then, back translation was done from Arabic to English by a bilingual translator unaware of the original version. The translated text was then compared with the original one by three experienced Babylon University School of Nursing and Midwifery faculty members. After finalization, 20 nurses from another ICU were invited to complete the questionnaires. The Kuder Richardson 21 results for the dimensions and total DKQ were as follows: “Incidence, signs, symptoms, and consequences of delirium” (0.72); “risk factors and causes of delirium” (0.77); “management and prevention strategies” (0.81); and “total” (0.86). The results were acceptable, and no changes were needed.
The case vignette (case descriptions), developed by Fick et al. (2007), has been widely utilized in all research related to nurses’ recognition of various forms of delirium (Detroyer et al. 2016; Detroyer et al., 2018). This tool contains different cases of dementia patients; some indicate delirium coexists with preexisting dementia. In each case, the patient’s symptoms and medical history are thoroughly explained before a question is asked about the patient’s type of delirium. Every inquiry regarding what occurred with the patient has one proper response. Each scenario has choices for dementia, delirium, delirium with dementia, normal aging, depression, or none of the options. The sum of the correct responses, ranging from 0 to 5, determines the overall score for identifying delirium. A higher score indicates a higher capacity to detect and identify delirium. Its reliability has been assessed based on a kappa coefficient of 0.69 and a panel of specialists in the field of delirium who completed the case tool selection scenario questions (description of the case vignette) with 84% agreement (Fick et al., 2007).
The method of forward and back translation was similar to the previous questionnaire. After finalization, 20 nurses from another ICU were invited to complete the questionnaires. The internal consistency evaluation of the questionnaire was done using the Kuder-Richardson 21 coefficient, which yielded an acceptable level of internal consistency of 0.66.
Data analysis
Absolute and relative frequency, Mean±SD, and inferential statistics tests were used for data analysis. The relationship between the average values of the main variables and qualitative demographic variables was determined using the independent t-test. The relationship between main and quantitative demographic variables was investigated using the Pearson correlation coefficient. To compare different levels of knowledge among nurses, knowledge scores were presented based on a scale of 100. The data was analyzed using SPSS software, version 22. The significance level was set at P<0.05.
3. Results
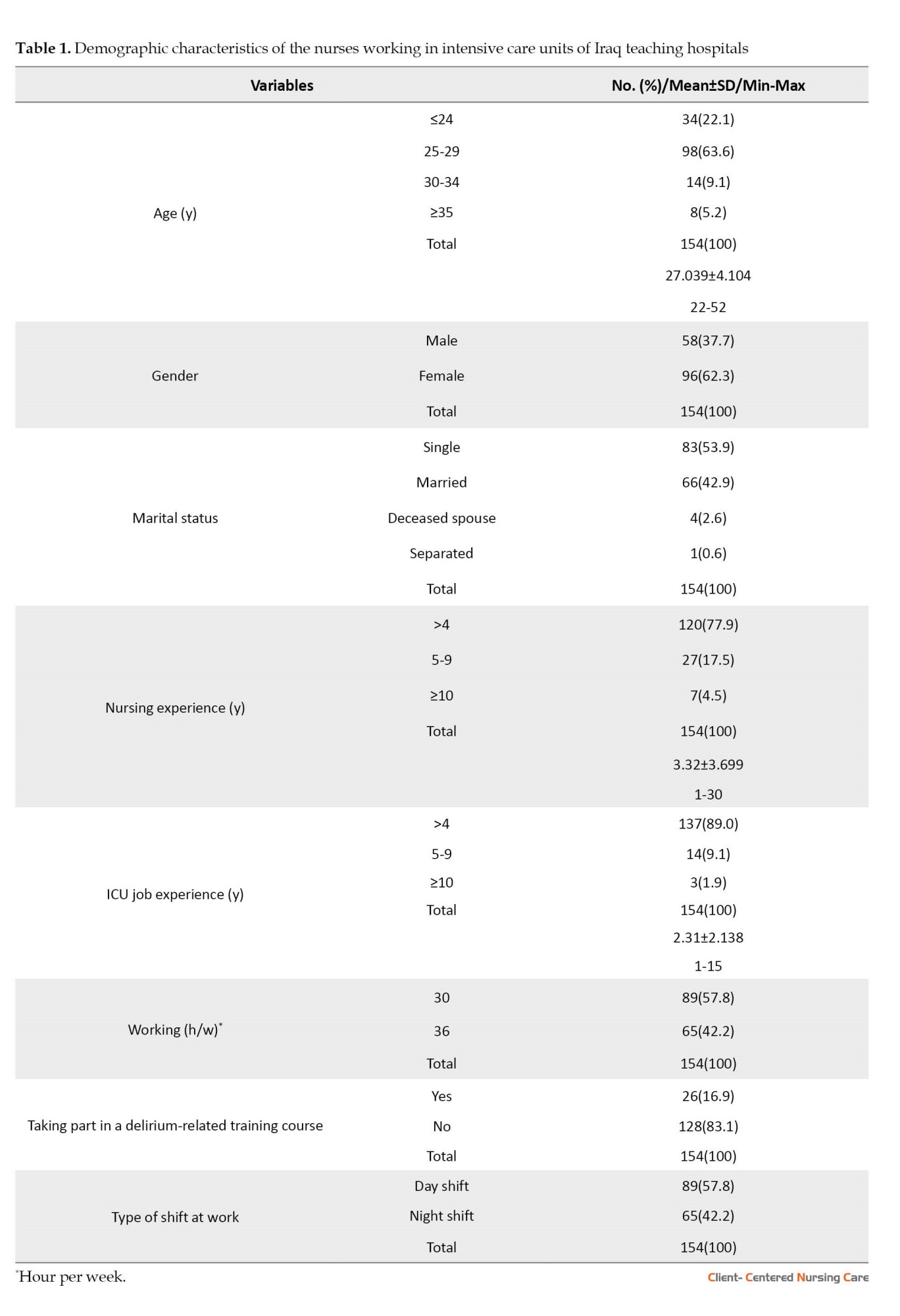
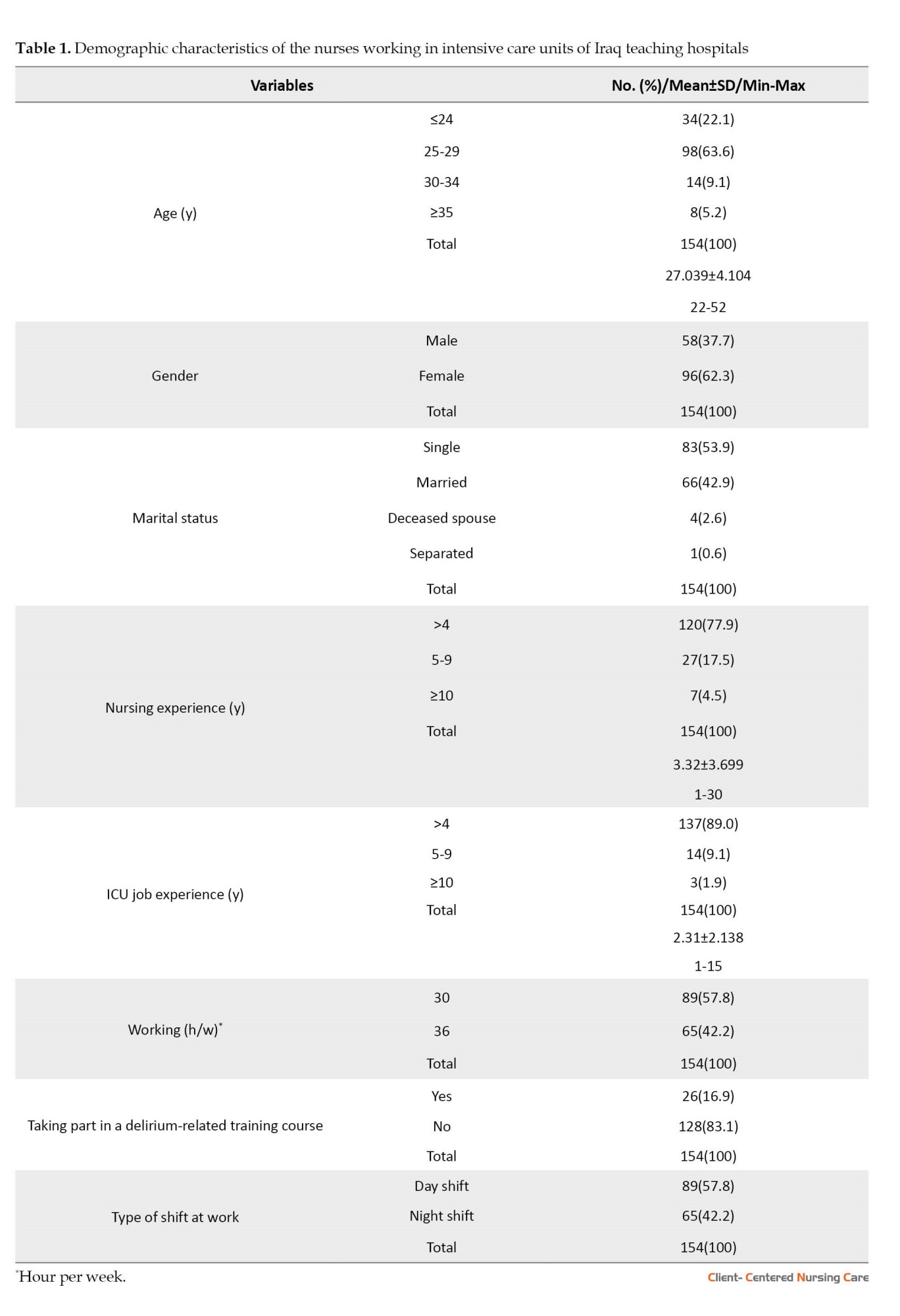
According to the results, most subjects (62.3%) were female, with the majority (63.6%) aged 25 and 29. More than half of the subjects (53.9%) were single. About 77.9% had 1-4 years of nursing experience, 89% had 1-4 years of experience in the ICU, and 57.8% worked 30 hours a week. Also, 83.1% had not taken any delirium-related training, and more than half (57.8%) worked the day shift (Table 1).
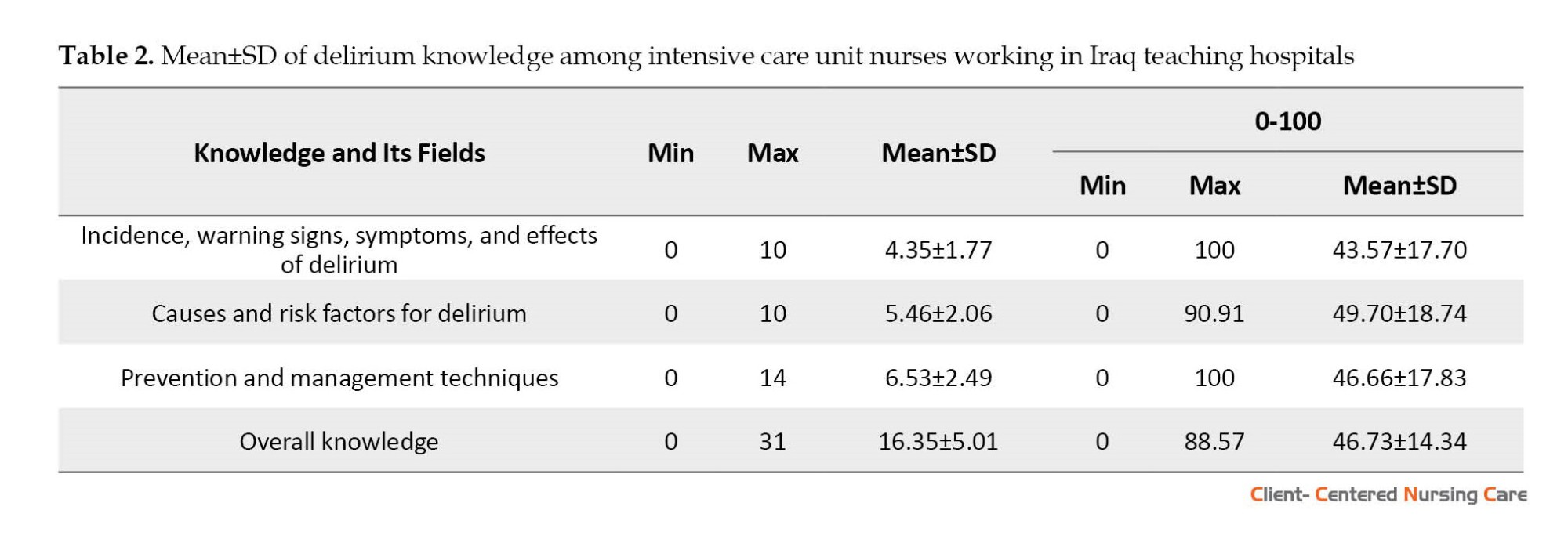
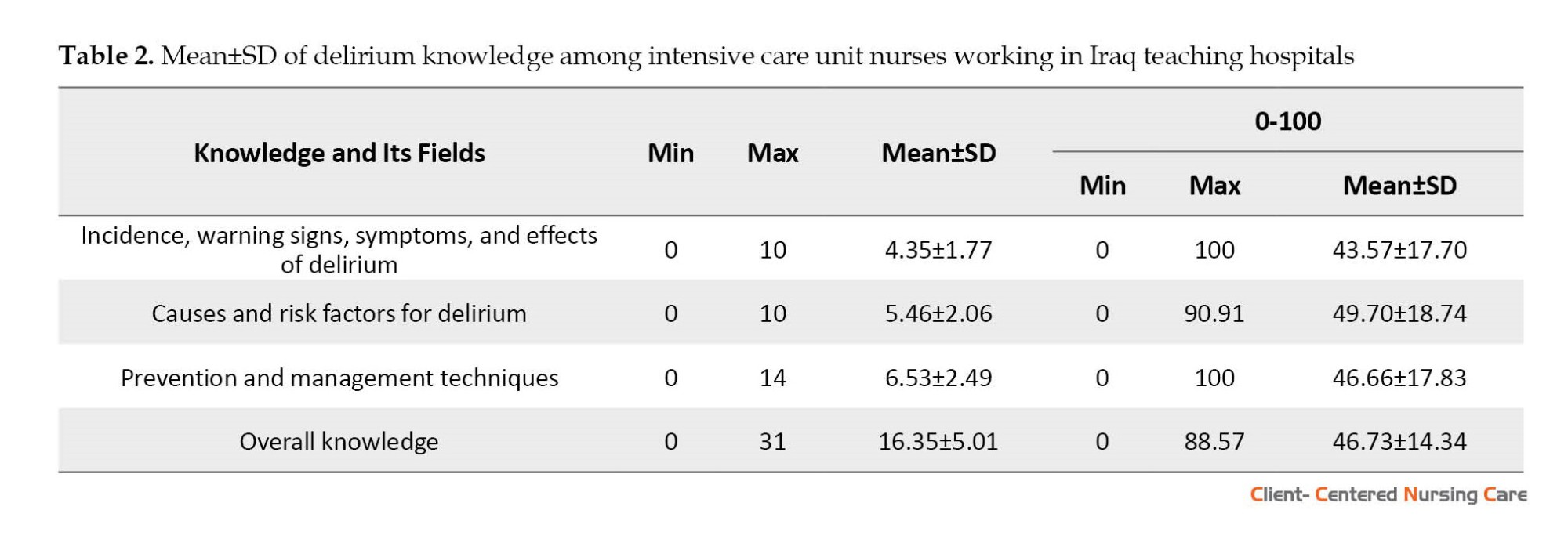
Knowledge of delirium incidence, signs, symptoms, and consequences had the lowest mean score (43.57±17.70), and knowledge of its risk factors and causes had the highest mean score (49.7±18.74). The general Mean±SD knowledge score was 46.73±14.34 (Table 2).
Among the items of DKQ, “fluctuation between orientation and disorientation is a typical feature of delirium” received the most wrong answers (83.1%). In contrast, the items “a patient with delirium is likely to be easily distracted and or have difficulty following a conversation” and “patients with delirium will often experience perceptual disturbances (e.g, visual and or auditory hallucinations)” had the lowest percentage of incorrect answers, about one-quarter of the present study sample (24.7%).
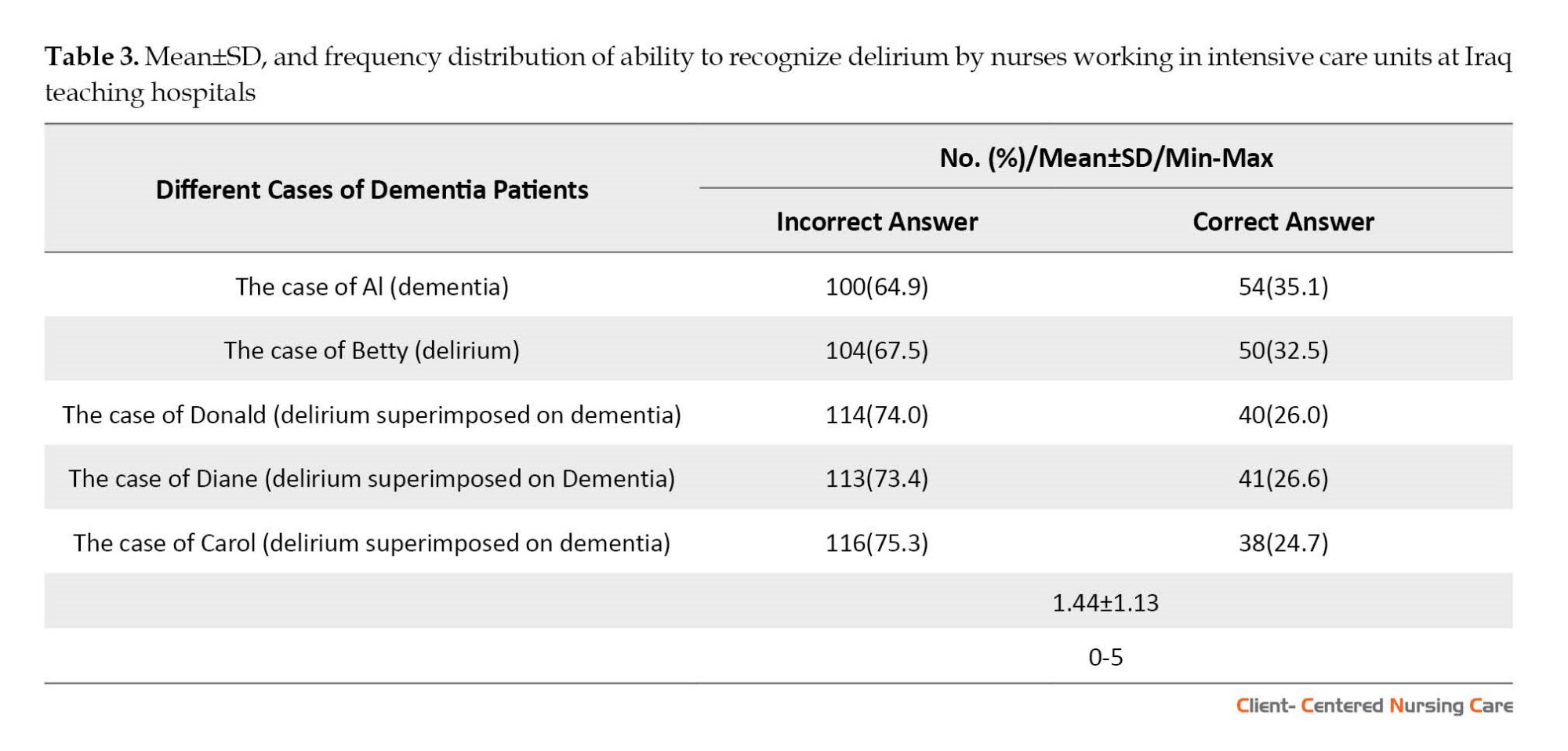
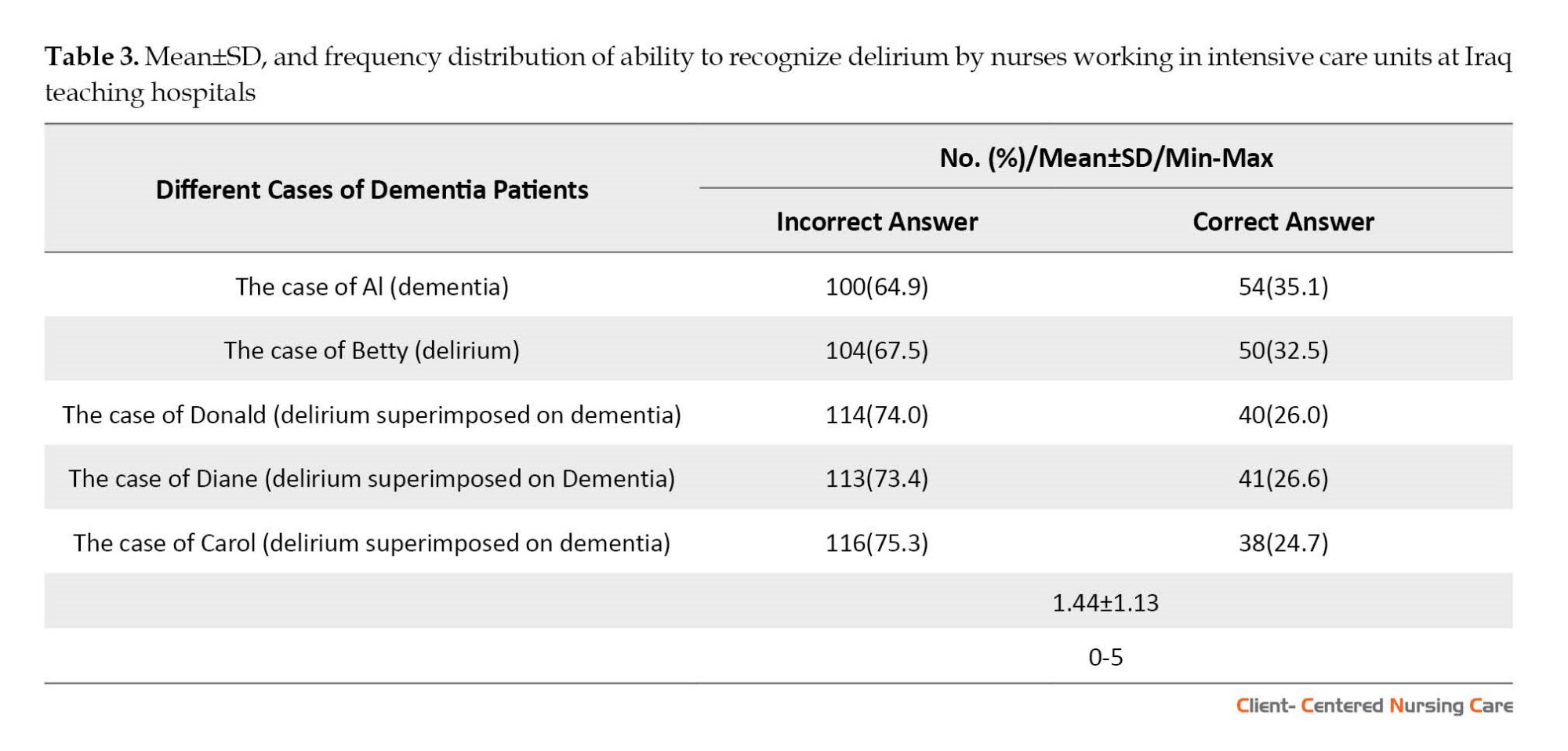
Based on Table 3, the findings revealed that while Al’s case had the lowest number of incorrect responses (64.9%), Carol’s case had the greatest percentage (75.3%) of incorrect responses. The percentage of incorrect answers was much higher than the correct ones. The Mean±SD score for recognizing delirium was 1.44±1.13.
According to Table 4, there was a significant relationship between delirium knowledge and having taken a delirium training course (P=0.008) and job experience in the ICU (P=0.046). However, no significant association was found between the ability to recognize delirium and the demographic characteristics of the subjects.

4. Discussion
The results indicated a low overall knowledge level among the subjects. The lowest knowledge was related to the incidence, signs, symptoms, and consequences of delirium, while the highest was related to the risk factors and causes of delirium. Additionally, a significant relationship was found between knowledge about delirium, participation in delirium training courses, and job experience in the ICU.
The low level of knowledge may be attributed to the lack of attention given to this issue in nursing education, training programs, and in-service training for nurses in Iraq. According to the findings, only those who attended a delirium training program acquired higher knowledge about it, indicating that education is vital for acquiring more knowledge and developing new skills. Moreover, the results suggested that increasing job experience in the ICU might enhance knowledge about delirium, but further research with a larger sample size is required to confirm this conclusion. The low level of knowledge can also be attributed to the nurses’ demanding work schedule and inability to attend face-to-face training programs. Surprisingly, more than half of the nurses in the study had not participated in any training program related to delirium. Since delirium is a critical issue in the care of at-risk patients, acquiring knowledge on this issue is imperative. Delirium is a patient safety issue, and healthcare center managers should plan and implement measures to empower their healthcare team, particularly nurses. Thus, educational programs to prevent delirium and care for those at risk are necessary.
The current study’s findings were consistent with those of a previous study conducted in Baghdad, indicating that most ICU nurses had a moderate level of knowledge regarding delirium, and most of them had not received any instructional programs about it (Ismail et al., 2021). Our findings are also consistent with those AbuRuz (2017) reported in Jordan, indicating that nurses lacked the fundamental knowledge to recognize delirium. In their study, nurses aged over 31 demonstrated significantly higher knowledge about delirium than their younger counterparts. Additionally, nurses with more expertise in the ICU exhibited better ability to recognize delirium. They believed that an inter-professional approach to delirium education could successfully improve the use of a delirium diagnostic instrument and awareness of the elements connected to this syndrome.
The ICU experience of nurses benefits their understanding of and attitude toward delirium. A study in the Netherlands shows that 61% of nurses answered the DKQ correctly, and only 40% of them had received in-service training in the last three years (Trogrlić et al., 2017). Another study in China indicates that the mean score of ICU nurses’ knowledge about subsyndromal delirium was low; 37.7% of the nurses thought their knowledge to be at the intermediate level, and 28.9% at the excellent level (Xing et al., 2022). Moreover, the study reveals that the nurses’ professional titles, ICU experience, marital status, ICU style, and delirium training are related to the nurses’ knowledge. The results of the current study are similar to those of the aforementioned studies.
In a study inconsistent with the recent research in the UK, Rowley-Conwy (2017) indicated that knowledge of the features, risk factors, and outcomes of delirium was mainly at a moderate level, perhaps reflecting the low levels of education on the topic. Also, Najafi Ghezeljeh et al. (2020) in Iran found that the pre-test mean score of delirium knowledge among ICU nurses in the experimental and control groups was moderate. The present study’s findings show that the nurses could barely diagnose delirium. Healthcare staff may significantly underestimate the incidence of delirium in different healthcare settings (Awad, 2019). Therefore, healthcare providers must improve their knowledge and ability to recognize delirium early, manage modifiable risk factors, and provide better care during the acute phase (Gnerre et al., 2016). Enhancing nurses’ knowledge and skills concerning delirium and its recognition is necessary to implement delirium screening successfully. Such training may also improve patient outcomes and prevent adverse effects (Blevins & DeGennaro, 2018).
The findings of the current study are consistent with those of previous research. A study by Rice et al. (2011) in the USA indicates that researchers identified delirium in 7% of patients, while nurses only recognized it 25% of the time. Similarly, in a study conducted in Thailand, nurses could not identify delirium in 29.6% of patients compared to researchers, who diagnosed delirium in 44.4% (Panitchote et al., 2015). Najafi Ghezeljeh et al. (2022) found that the delirium recognition ability among ICU nurses in the experimental and control groups was low. The study also revealed that interactive E-learning significantly improved critical care nurses’ delirium recognition abilities. Likewise, a study in Egypt by Mabrouk et al. (2022) found that more than half of the nurses had a moderate overall knowledge of delirium before the educational program. In China, Xing et al. (2022) found that ICU nurses’ performance in subsyndromal delirium was self-evaluated at the intermediate level, and 35.9% were at the excellent level. They also found that education level, ICU style, and training received were related to nurses’ performance.
Monfared et al. (2017) conducted a study in Iran to investigate the knowledge and attitudes of intensive care unit nurses regarding delirium. The findings showed that only 24.6% of nurses knew delirium well, and 76% had a positive attitude toward it. Most nurses had intermediate knowledge. In Poland, Krupa et al. (2022) concluded that nurses do not know the underlying causes of delirium and cannot communicate effectively with delirious patients. In Canada, nurses’ knowledge and attitudes toward delirium were positively correlated with their demographics. Most nurses had intermediate knowledge and reported positive attitudes toward delirium (Hickin et al., 2017). In a South Korean Q-methodology study, Jeong and Chang (2018) investigated nurses’ subjective recognition of delirium in older people. They observed four distinct perceptions of nurses’ ability to recognize delirium: prediction from the combined indicators, visible symptom-centered detection, detection of aberrant changes based on focused observation, and recognition based on diagnostic data. The study showed that nurses can successfully diagnose delirium using all the techniques disclosed by the four variables.
It is essential to note that the present study was conducted only in one region of Iraq, and the results cannot be generalized to other parts of the country. Similar research in this field is suggested in other regions. Regarding the study’s cross-sectional nature, the findings should be interpreted with caution.
5. Conclusion
The study shows the ICU nurses lack the proper knowledge and recognition abilities to diagnose delirium. To provide high-quality and safe nursing care, in-service programs should be provided to update the skill set of ICU nurses in Iraq. Routine assessments of nurses’ knowledge and recognition abilities should also be incorporated to identify areas for improvement. The study highlights the need for more education on delirium for nursing students. Future research should focus on identifying the reasons behind the low levels of knowledge, exploring factors that influence the effectiveness of in-service programs, investigating the potential benefits of technology-based training, and examining the impact of improved delirium recognition and management on patient outcomes and healthcare costs. The experiences and perspectives of patients and their families should also be explored to improve the quality of nursing care provided to patients with delirium in critical care settings.
Ethical Considerations
Compliance with ethical guidelines
The research process considered several ethical considerations, including obtaining permits from relevant health directorates and the Ethics Committee. Specifically, the Babylon, Al-Diwaniyah, and Karbala Health Directorates, as well as the Vice Chancellor for Research and the Ethics Committee of the Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.647). Informed written consent was also obtained from eligible participants, and they were informed about the study’s objectives and their voluntary participation in it.
Funding
This article extracted from a research project approved by the Research Department of the International Campus at the Iran University of Medical Sciences in 2022.
Authors' contributions
Conceptualization, supervision, and study design: Tahereh Ghezeljeh and Fakhria Jaber Muhaibes; Data collection and analysis: Shima Haghani and Abbas Kifah Mubdir; Critically revision of the manuscript and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the officials and personnel of the Imam Al-Sadiq Hospital, Al-Hilla General Teaching Hospital, Imam Al-Hussein Medical City, Al-Hindiya General Hospital, and Al-Diwaniyah Teaching Hospital and all the nurses who generously contributed their time and effort to participate in the study.
References
AbuRuz, M. E., 2017. Jordanian intensive care unit nurses’ knowledge of delirium recognition. Global Journal of Health Science, 9(4), pp. 182-9. [DOI:10.5539/gjhs.v9n4p182]
Awad, S. A., 2019. Critical care nurses’ knowledge, perception and barriers regarding delirium in adult critical care units. American Journal of Nursing Research, 7(2), pp. 193-8. [Link]
Blevins, C. S. & DeGennaro, R., 2018. Educational intervention to improve delirium recognition by nurses. American Journal of Critical Care, 27(4), pp. 270-8. [DOI:10.4037/ajcc2018851] [PMID]
Collet, M. O., Thomsen, T. & Egerod, I., 2019. Nurses’ and physicians’ approaches to delirium management in the intensive care unit: A focus group investigation. Australian Critical Care, 32(4), pp. 299-305. [DOI:10.1016/j.aucc.2018.07.001] [PMID]
Collet, M. O., et al., 2018. Prevalence and risk factors related to haloperidol use for delirium in adult intensive care patients: The multinational AID-ICU inception cohort study. Intensive Care Medicine, 44(7), pp. 1081–9. [DOI:10.1007/s00134-018-5204-y] [PMID]
Detroyer, E., et al., 2016. The effect of an interactive delirium e-learning tool on healthcare workers’ delirium recognition, knowledge and strain in caring for delirious patients: A pilot pretest/post-test study. BMC Medical Education, 16, pp. 17. [DOI:10.1186/s12909-016-0537-0] [PMID]
Detroyer, E., et al., 2018. Effect of an interactive E-learning tool for delirium on patient and nursing outcomes in a geriatric hospital setting: Findings of a before-after study. BMC Geriatrics, 18(1), pp. 19. [PMID]
Erber, J. T., 2012. Aging and older adulthood. New Jersey: Wiley. [Link]
Fick, D. M., et al., 2007. Recognizing delirium superimposed on dementia: Assessing nurses’ knowledge using case vignettes. Journal of Gerontological Nursing, 33(2), pp. 40-9. [DOI:10.3928/00989134-20070201-09] [PMID]
Gnerre, P., et al., 2016. Delirium: The invisible syndrome. Italian Journal of Medicine, 10(2), pp. 119-27. [DOI:10.4081/itjm.2016.626]
Hare, M., et al., 2008. A questionnaire to determine nurses' knowledge of delirium and its risk factors. Contemporary Nurse, 29(1), pp. 23–31.[DOI:10.5172/conu.673.29.1.23] [PMID]
Hickin, S. L., White, S. & Knopp-Sihota, J., 2017. Nurses’ knowledge and perception of delirium screening and assessment in the intensive care unit: Long-term effectiveness of an education-based knowledge translation intervention. Intensive and Critical Care Nursing, 41, pp. 43-9. [DOI:10.1016/j.iccn.2017.03.010] [PMID]
Hshieh, T. T., Inouye, S. K. & Oh, E. S., 2020. Delirium in the elderly. Clinics in Geriatric Medicine, 36(2), pp. 183–99.[DOI:10.1016/j.cger.2019.11.001] [PMID]
Ismail, M., Rahim, H. S., Abd Alwan, Y. H., Mahmoud, W. A., Salem, H. A., Reggio, H. K. and Abdullah, H. H. (2021) Assessment of Nurses’ knowledge Regarding Delirium at Adult Critical Care Units in Baghdad City. Al-Bayan Journal for Medical and Health Sciences, 1(1), pp. 9-20. [Link]
Jeong, E. & Chang, S. O., 2018. Exploring nurses’ recognition of delirium in the elderly by using Q-methodology. Japan Journal of Nursing Science, 15(4), pp. 298-308. [DOI:10.1111/jjns.12199] [PMID]
Krupa, S., et al., 2022. Nurses’ knowledge about Delirium in the group of intensive care units patients. International Journal of Environmental Research and Public Health, 19(5), pp. 2758. [DOI:10.3390/ijerph19052758] [PMID]
Mabrouk, S., et al., 2022. The effect of the training program on nursing staff knowledge regarding delirium in the elderly. Journal of Positive School Psychology, 6(7), pp. 5094-104. [Link]
Morandi, A., et al., 2017. Clinical features associated with delirium motor subtypes in older inpatients: results of a multicenter study. The American Journal of Geriatric Psychiatry, 25(10), pp. 1064-71. [DOI:10.1016/j.jagp.2017.05.003] [PMID]
Najafi Ghezeljeh, T., et al., 2020. [The effect of interactive e-learning on the knowledge of ICU Nurses regarding delirium (Persian)]. Iran Journal of Nursing, 33(123), pp. 47-61. [Link]
Najafi Ghezeljeh, T., et al., 2022. The effects of interactive E-learning on delirium recognition ability and delirium-related strain of care among critical care nurses. Journal of the Intensive Care Society, 23(1), pp. 44–52. [DOI:10.1177/1751143720972627] [PMID]
Oh, E. S., et al., 2017. Delirium in older persons: Advances in diagnosis and treatment. JAMA, 318(12), pp.1161-74. [DOI:10.1001/jama.2017.12067] [PMID]
Panitchote, A., et al., 2015. Under-recognition of delirium in older adults by nurses in the intensive care unit setting. Aging Clinical and Experimental Research, 27(5), pp. 735–40.[DOI:10.1007/s40520-015-0323-6] [PMID]
Park, S. Y. & Lee, H. B., 2019. Prevention and management of delirium in critically ill adult patients in the intensive care unit: A review based on the 2018 PADIS guidelines. Acute and Critical Care, 34(2), pp. 117-25. [DOI:10.4266/acc.2019.00451] [PMID]
Reznik, M. E. & Slooter, A. J., 2019. Delirium management in the ICU. Current Treatment Options in Neurology, 21(11), pp. 59. [DOI:10.1007/s11940-019-0599-5] [PMID]
Ribeiro, S. C. L., et al., 2015. Knowledge of nurses about delirium in critical patients: Collective subject discourse. 24(2), pp. 513-20. [DOI:10.1590/0104-07072015001702014]
Rice, K. L., et al., 2011. Nurses’ recognition of delirium in the hospitalized older adult. Clinical Nurse Specialist, 25(6), pp. 299-311. [DOI:10.1097/NUR.0b013e318234897b] [PMID]
Rood, P., et al., 2018. Effect of organisational factors on the variation in incidence of delirium in intensive care unit patients: A systematic review and meta-regression analysis. Australian Critical Care, 31(3), pp. 180-7. [DOI:10.1016/j.aucc.2018.02.002] [PMID]
Rowley-Conwy, G., 2017. Critical care nurses’ knowledge and practice of delirium assessment. British Journal of Nursing, 26(7), pp. 412-7. [DOI:10.12968/bjon.2017.26.7.412] [PMID]
Slooter, A. J., Van De Leur, R. R. & Zaal, I. J., 2017. Delirium in critically ill patients. Handbook of Clinical Neurology, 141, pp. 449-66. [DOI:10.1016/B978-0-444-63599-0.00025-9] [PMID]
Trogrlić, Z., et al., 2017. Attitudes, knowledge and practices concerning delirium: A survey among intensive care unit professionals. Nursing in Critical Care, 22(3), pp. 133-40. [DOI:10.1111/nicc.12239] [PMID]
Xing, H., et al., 2022. Knowledge, attitudes and practices of ICU nurses regarding subsyndromal delirium among 20 hospitals in China: A descriptive cross-sectional survey. BMJ Open, 12(9), pp. e063821. [DOI:10.1136/bmjopen-2022-063821] [PMID]
elirium is an acute, transient disruption of awareness characterized by various symptoms. The incidence of this disorder in intensive care units (ICUs) is very high, placing a lot of strain on nurses, leading to many adverse consequences for the patients. Ultimately, it imposes enormous costs on countries’ healthcare systems every year. If the complications of delirium are properly addressed, the recovery time will be faster (Erber, 2012). Delirium is a common disorder among critically ill patients, a fatal condition with few effective treatments (Reznik & Slooter, 2019). Between 25% and 80% of patients in ICUs experience delirium, with mechanically ventilated patients exhibiting a higher frequency. Delirium is associated with longer stays in the ICUs, a higher 6-month mortality, and elevated morbidity rates (Collet et al., 2018; Slooter et al., 2017). On average, delirium affects 29% during an ICU stay (Rood et al., 2018). It is associated with a poor, stressful prognosis for patients and their families (Slooter et al., 2017). Besides its complications, it results in expensive medical care, and less favorable outcomes. Healthcare costs related to delirium are estimated at more than $164 billion annually. The risk of death from delirium is 2 to 4 times higher in ICUs, increases the risk of death over 6 months by 70% in patients presenting to the emergency department (Hshieh et al., 2020).
Delirium can be further classified into three subcategories based on the motor activity profiles: Mixed, hypoactive, and hyperactive. These different subgroups vary in physiology, incidence rates, the length of the delirium event, treatment, and patient outcomes (Morandi et al., 2017). Patients with a hypoactive subtype show lethargy, little spontaneous movements, and delayed response to questions, which might be misconstrued as grief or dementia. Patients with hyperactive delirium are physically aggressive, agitated, and restless. They also frequently experience delusions and hallucinations. Furthermore, individuals with mixed delirium show signs of both hypoactive and hyperactive categories (Oh et al., 2017). A multi-professional team consultation is crucial to deal with delirium as it is a clinical emergency significantly affecting ICU patients’ survival (Ribeiro et al., 2015).
Early recognition of delirium is essential, and ICU staff should monitor its occurrence, while focusing on managing and preventing it (Park et al., 2019). Nurses and doctors should rely on their collective experience and the latest available data to determine the best course for managing ICU delirious patients (Collet et al., 2019).
Furthermore, delirium presents a dangerous condition that needs to be quickly diagnosed and treated in ICUs. The first step in preventing delirium is recognizing and comprehending the risk factors and triggering variables. Nurses must have the required education, skills, and experience to participate in diagnosing and treating delirium actively. ICU nursing is a complex and challenging job, where many patients are involved in this complex situation, an insight following the researcher’s experience as an ICU nurse.
The prevention and management of delirium is essential in the ICU, and nurses’ knowledge and ability will play a prominent role in following delirium prevention and treatment guidelines. However, the Iraqi health sector, like other sectors, is affected by the political, social, and cultural changes, the current security situation, and infrastructure destruction. Based on the researcher’s experience as an ICU nurse member, ICU nursing personnel operate in a complex and challenging area. In Iraq’s healthcare system, baccalaureate, technical, and skilled nurses all fall under the “graduate-trained nurses” category and work together.
Based on the literature review, no study was found regarding the knowledge and recognition ability of ICU Iraqi nurses about delirium. Accordingly, this study was carried out to determine the Iraqi nurses’ knowledge and recognition ability of delirium in the ICUs of this country.
2. Materials and Methods
This descriptive, cross-sectional study was carried out in Iraq in 2022. Hospital ICUs in Babylon, Al-Diwaniyah, and Karbala were the study settings. The participating hospitals included Imam Al-Sadiq Hospital, Al-Hilla General Teaching Hospital, Imam Al-Hussein Medical City, Al-Hindiya General Hospital, and Al-Diwaniyah Teaching Hospital. Except for the Al-Hindiya General Hospital, located in the easternmost governorate of Karbala, the other hospitals, each of which has one ICU, are located in the governorates’ centers in the cities of Babylon, Al-Diwaniyah, and Karbala. The inclusion criteria were having a university degree in nursing, giving direct care (clinical bedside) to the patients in the ICU, and consenting to participate in the study. Accordingly, all nurses with bachelor’s degrees working in the ICUs of the previously mentioned teaching hospitals represented the research sample. The subjects were recruited by census; ultimately, 154 nurses agreed to participate in the study.
The study data were gathered from August to September 2022, using a demographic information questionnaire created by the researcher, the delirium knowledge questionnaire (DKQ), and a case vignette to identify delirium.
The demographic information questionnaire included the nurses’ age, gender, marital status, type of shift, years of experience in the ICU, and education level history of taking delirium-related training within the previous 5 years.
The DKQ was devised by Detroyer et al. (2016) based on a questionnaire by Hare et al. (2008). It serves to evaluate all aspects of delirium knowledge. This 35-item true/false tool has 3 domains: 1) Knowledge related to the appearance, symptoms, and consequences of delirium (10 items), 2) Its underlying and risk factors (11 items), and 3) Delirium prevention and management approaches (14 items). Each question receives a score of 1 for a correct response and 0 for a wrong response, or “I don’t know.” The sum of the correct responses determines the final grade for delirium knowledge, ranging from 0 to 35, with a higher score indicating a deeper understanding of delirium.
The questionnaire was first subjected to forward translation from English to Arabic. Then, back translation was done from Arabic to English by a bilingual translator unaware of the original version. The translated text was then compared with the original one by three experienced Babylon University School of Nursing and Midwifery faculty members. After finalization, 20 nurses from another ICU were invited to complete the questionnaires. The Kuder Richardson 21 results for the dimensions and total DKQ were as follows: “Incidence, signs, symptoms, and consequences of delirium” (0.72); “risk factors and causes of delirium” (0.77); “management and prevention strategies” (0.81); and “total” (0.86). The results were acceptable, and no changes were needed.
The case vignette (case descriptions), developed by Fick et al. (2007), has been widely utilized in all research related to nurses’ recognition of various forms of delirium (Detroyer et al. 2016; Detroyer et al., 2018). This tool contains different cases of dementia patients; some indicate delirium coexists with preexisting dementia. In each case, the patient’s symptoms and medical history are thoroughly explained before a question is asked about the patient’s type of delirium. Every inquiry regarding what occurred with the patient has one proper response. Each scenario has choices for dementia, delirium, delirium with dementia, normal aging, depression, or none of the options. The sum of the correct responses, ranging from 0 to 5, determines the overall score for identifying delirium. A higher score indicates a higher capacity to detect and identify delirium. Its reliability has been assessed based on a kappa coefficient of 0.69 and a panel of specialists in the field of delirium who completed the case tool selection scenario questions (description of the case vignette) with 84% agreement (Fick et al., 2007).
The method of forward and back translation was similar to the previous questionnaire. After finalization, 20 nurses from another ICU were invited to complete the questionnaires. The internal consistency evaluation of the questionnaire was done using the Kuder-Richardson 21 coefficient, which yielded an acceptable level of internal consistency of 0.66.
Data analysis
Absolute and relative frequency, Mean±SD, and inferential statistics tests were used for data analysis. The relationship between the average values of the main variables and qualitative demographic variables was determined using the independent t-test. The relationship between main and quantitative demographic variables was investigated using the Pearson correlation coefficient. To compare different levels of knowledge among nurses, knowledge scores were presented based on a scale of 100. The data was analyzed using SPSS software, version 22. The significance level was set at P<0.05.
3. Results
According to the results, most subjects (62.3%) were female, with the majority (63.6%) aged 25 and 29. More than half of the subjects (53.9%) were single. About 77.9% had 1-4 years of nursing experience, 89% had 1-4 years of experience in the ICU, and 57.8% worked 30 hours a week. Also, 83.1% had not taken any delirium-related training, and more than half (57.8%) worked the day shift (Table 1).
Knowledge of delirium incidence, signs, symptoms, and consequences had the lowest mean score (43.57±17.70), and knowledge of its risk factors and causes had the highest mean score (49.7±18.74). The general Mean±SD knowledge score was 46.73±14.34 (Table 2).
Among the items of DKQ, “fluctuation between orientation and disorientation is a typical feature of delirium” received the most wrong answers (83.1%). In contrast, the items “a patient with delirium is likely to be easily distracted and or have difficulty following a conversation” and “patients with delirium will often experience perceptual disturbances (e.g, visual and or auditory hallucinations)” had the lowest percentage of incorrect answers, about one-quarter of the present study sample (24.7%).
Based on Table 3, the findings revealed that while Al’s case had the lowest number of incorrect responses (64.9%), Carol’s case had the greatest percentage (75.3%) of incorrect responses. The percentage of incorrect answers was much higher than the correct ones. The Mean±SD score for recognizing delirium was 1.44±1.13.
According to Table 4, there was a significant relationship between delirium knowledge and having taken a delirium training course (P=0.008) and job experience in the ICU (P=0.046). However, no significant association was found between the ability to recognize delirium and the demographic characteristics of the subjects.

4. Discussion
The results indicated a low overall knowledge level among the subjects. The lowest knowledge was related to the incidence, signs, symptoms, and consequences of delirium, while the highest was related to the risk factors and causes of delirium. Additionally, a significant relationship was found between knowledge about delirium, participation in delirium training courses, and job experience in the ICU.
The low level of knowledge may be attributed to the lack of attention given to this issue in nursing education, training programs, and in-service training for nurses in Iraq. According to the findings, only those who attended a delirium training program acquired higher knowledge about it, indicating that education is vital for acquiring more knowledge and developing new skills. Moreover, the results suggested that increasing job experience in the ICU might enhance knowledge about delirium, but further research with a larger sample size is required to confirm this conclusion. The low level of knowledge can also be attributed to the nurses’ demanding work schedule and inability to attend face-to-face training programs. Surprisingly, more than half of the nurses in the study had not participated in any training program related to delirium. Since delirium is a critical issue in the care of at-risk patients, acquiring knowledge on this issue is imperative. Delirium is a patient safety issue, and healthcare center managers should plan and implement measures to empower their healthcare team, particularly nurses. Thus, educational programs to prevent delirium and care for those at risk are necessary.
The current study’s findings were consistent with those of a previous study conducted in Baghdad, indicating that most ICU nurses had a moderate level of knowledge regarding delirium, and most of them had not received any instructional programs about it (Ismail et al., 2021). Our findings are also consistent with those AbuRuz (2017) reported in Jordan, indicating that nurses lacked the fundamental knowledge to recognize delirium. In their study, nurses aged over 31 demonstrated significantly higher knowledge about delirium than their younger counterparts. Additionally, nurses with more expertise in the ICU exhibited better ability to recognize delirium. They believed that an inter-professional approach to delirium education could successfully improve the use of a delirium diagnostic instrument and awareness of the elements connected to this syndrome.
The ICU experience of nurses benefits their understanding of and attitude toward delirium. A study in the Netherlands shows that 61% of nurses answered the DKQ correctly, and only 40% of them had received in-service training in the last three years (Trogrlić et al., 2017). Another study in China indicates that the mean score of ICU nurses’ knowledge about subsyndromal delirium was low; 37.7% of the nurses thought their knowledge to be at the intermediate level, and 28.9% at the excellent level (Xing et al., 2022). Moreover, the study reveals that the nurses’ professional titles, ICU experience, marital status, ICU style, and delirium training are related to the nurses’ knowledge. The results of the current study are similar to those of the aforementioned studies.
In a study inconsistent with the recent research in the UK, Rowley-Conwy (2017) indicated that knowledge of the features, risk factors, and outcomes of delirium was mainly at a moderate level, perhaps reflecting the low levels of education on the topic. Also, Najafi Ghezeljeh et al. (2020) in Iran found that the pre-test mean score of delirium knowledge among ICU nurses in the experimental and control groups was moderate. The present study’s findings show that the nurses could barely diagnose delirium. Healthcare staff may significantly underestimate the incidence of delirium in different healthcare settings (Awad, 2019). Therefore, healthcare providers must improve their knowledge and ability to recognize delirium early, manage modifiable risk factors, and provide better care during the acute phase (Gnerre et al., 2016). Enhancing nurses’ knowledge and skills concerning delirium and its recognition is necessary to implement delirium screening successfully. Such training may also improve patient outcomes and prevent adverse effects (Blevins & DeGennaro, 2018).
The findings of the current study are consistent with those of previous research. A study by Rice et al. (2011) in the USA indicates that researchers identified delirium in 7% of patients, while nurses only recognized it 25% of the time. Similarly, in a study conducted in Thailand, nurses could not identify delirium in 29.6% of patients compared to researchers, who diagnosed delirium in 44.4% (Panitchote et al., 2015). Najafi Ghezeljeh et al. (2022) found that the delirium recognition ability among ICU nurses in the experimental and control groups was low. The study also revealed that interactive E-learning significantly improved critical care nurses’ delirium recognition abilities. Likewise, a study in Egypt by Mabrouk et al. (2022) found that more than half of the nurses had a moderate overall knowledge of delirium before the educational program. In China, Xing et al. (2022) found that ICU nurses’ performance in subsyndromal delirium was self-evaluated at the intermediate level, and 35.9% were at the excellent level. They also found that education level, ICU style, and training received were related to nurses’ performance.
Monfared et al. (2017) conducted a study in Iran to investigate the knowledge and attitudes of intensive care unit nurses regarding delirium. The findings showed that only 24.6% of nurses knew delirium well, and 76% had a positive attitude toward it. Most nurses had intermediate knowledge. In Poland, Krupa et al. (2022) concluded that nurses do not know the underlying causes of delirium and cannot communicate effectively with delirious patients. In Canada, nurses’ knowledge and attitudes toward delirium were positively correlated with their demographics. Most nurses had intermediate knowledge and reported positive attitudes toward delirium (Hickin et al., 2017). In a South Korean Q-methodology study, Jeong and Chang (2018) investigated nurses’ subjective recognition of delirium in older people. They observed four distinct perceptions of nurses’ ability to recognize delirium: prediction from the combined indicators, visible symptom-centered detection, detection of aberrant changes based on focused observation, and recognition based on diagnostic data. The study showed that nurses can successfully diagnose delirium using all the techniques disclosed by the four variables.
It is essential to note that the present study was conducted only in one region of Iraq, and the results cannot be generalized to other parts of the country. Similar research in this field is suggested in other regions. Regarding the study’s cross-sectional nature, the findings should be interpreted with caution.
5. Conclusion
The study shows the ICU nurses lack the proper knowledge and recognition abilities to diagnose delirium. To provide high-quality and safe nursing care, in-service programs should be provided to update the skill set of ICU nurses in Iraq. Routine assessments of nurses’ knowledge and recognition abilities should also be incorporated to identify areas for improvement. The study highlights the need for more education on delirium for nursing students. Future research should focus on identifying the reasons behind the low levels of knowledge, exploring factors that influence the effectiveness of in-service programs, investigating the potential benefits of technology-based training, and examining the impact of improved delirium recognition and management on patient outcomes and healthcare costs. The experiences and perspectives of patients and their families should also be explored to improve the quality of nursing care provided to patients with delirium in critical care settings.
Ethical Considerations
Compliance with ethical guidelines
The research process considered several ethical considerations, including obtaining permits from relevant health directorates and the Ethics Committee. Specifically, the Babylon, Al-Diwaniyah, and Karbala Health Directorates, as well as the Vice Chancellor for Research and the Ethics Committee of the Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.647). Informed written consent was also obtained from eligible participants, and they were informed about the study’s objectives and their voluntary participation in it.
Funding
This article extracted from a research project approved by the Research Department of the International Campus at the Iran University of Medical Sciences in 2022.
Authors' contributions
Conceptualization, supervision, and study design: Tahereh Ghezeljeh and Fakhria Jaber Muhaibes; Data collection and analysis: Shima Haghani and Abbas Kifah Mubdir; Critically revision of the manuscript and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the officials and personnel of the Imam Al-Sadiq Hospital, Al-Hilla General Teaching Hospital, Imam Al-Hussein Medical City, Al-Hindiya General Hospital, and Al-Diwaniyah Teaching Hospital and all the nurses who generously contributed their time and effort to participate in the study.
References
AbuRuz, M. E., 2017. Jordanian intensive care unit nurses’ knowledge of delirium recognition. Global Journal of Health Science, 9(4), pp. 182-9. [DOI:10.5539/gjhs.v9n4p182]
Awad, S. A., 2019. Critical care nurses’ knowledge, perception and barriers regarding delirium in adult critical care units. American Journal of Nursing Research, 7(2), pp. 193-8. [Link]
Blevins, C. S. & DeGennaro, R., 2018. Educational intervention to improve delirium recognition by nurses. American Journal of Critical Care, 27(4), pp. 270-8. [DOI:10.4037/ajcc2018851] [PMID]
Collet, M. O., Thomsen, T. & Egerod, I., 2019. Nurses’ and physicians’ approaches to delirium management in the intensive care unit: A focus group investigation. Australian Critical Care, 32(4), pp. 299-305. [DOI:10.1016/j.aucc.2018.07.001] [PMID]
Collet, M. O., et al., 2018. Prevalence and risk factors related to haloperidol use for delirium in adult intensive care patients: The multinational AID-ICU inception cohort study. Intensive Care Medicine, 44(7), pp. 1081–9. [DOI:10.1007/s00134-018-5204-y] [PMID]
Detroyer, E., et al., 2016. The effect of an interactive delirium e-learning tool on healthcare workers’ delirium recognition, knowledge and strain in caring for delirious patients: A pilot pretest/post-test study. BMC Medical Education, 16, pp. 17. [DOI:10.1186/s12909-016-0537-0] [PMID]
Detroyer, E., et al., 2018. Effect of an interactive E-learning tool for delirium on patient and nursing outcomes in a geriatric hospital setting: Findings of a before-after study. BMC Geriatrics, 18(1), pp. 19. [PMID]
Erber, J. T., 2012. Aging and older adulthood. New Jersey: Wiley. [Link]
Fick, D. M., et al., 2007. Recognizing delirium superimposed on dementia: Assessing nurses’ knowledge using case vignettes. Journal of Gerontological Nursing, 33(2), pp. 40-9. [DOI:10.3928/00989134-20070201-09] [PMID]
Gnerre, P., et al., 2016. Delirium: The invisible syndrome. Italian Journal of Medicine, 10(2), pp. 119-27. [DOI:10.4081/itjm.2016.626]
Hare, M., et al., 2008. A questionnaire to determine nurses' knowledge of delirium and its risk factors. Contemporary Nurse, 29(1), pp. 23–31.[DOI:10.5172/conu.673.29.1.23] [PMID]
Hickin, S. L., White, S. & Knopp-Sihota, J., 2017. Nurses’ knowledge and perception of delirium screening and assessment in the intensive care unit: Long-term effectiveness of an education-based knowledge translation intervention. Intensive and Critical Care Nursing, 41, pp. 43-9. [DOI:10.1016/j.iccn.2017.03.010] [PMID]
Hshieh, T. T., Inouye, S. K. & Oh, E. S., 2020. Delirium in the elderly. Clinics in Geriatric Medicine, 36(2), pp. 183–99.[DOI:10.1016/j.cger.2019.11.001] [PMID]
Ismail, M., Rahim, H. S., Abd Alwan, Y. H., Mahmoud, W. A., Salem, H. A., Reggio, H. K. and Abdullah, H. H. (2021) Assessment of Nurses’ knowledge Regarding Delirium at Adult Critical Care Units in Baghdad City. Al-Bayan Journal for Medical and Health Sciences, 1(1), pp. 9-20. [Link]
Jeong, E. & Chang, S. O., 2018. Exploring nurses’ recognition of delirium in the elderly by using Q-methodology. Japan Journal of Nursing Science, 15(4), pp. 298-308. [DOI:10.1111/jjns.12199] [PMID]
Krupa, S., et al., 2022. Nurses’ knowledge about Delirium in the group of intensive care units patients. International Journal of Environmental Research and Public Health, 19(5), pp. 2758. [DOI:10.3390/ijerph19052758] [PMID]
Mabrouk, S., et al., 2022. The effect of the training program on nursing staff knowledge regarding delirium in the elderly. Journal of Positive School Psychology, 6(7), pp. 5094-104. [Link]
Morandi, A., et al., 2017. Clinical features associated with delirium motor subtypes in older inpatients: results of a multicenter study. The American Journal of Geriatric Psychiatry, 25(10), pp. 1064-71. [DOI:10.1016/j.jagp.2017.05.003] [PMID]
Najafi Ghezeljeh, T., et al., 2020. [The effect of interactive e-learning on the knowledge of ICU Nurses regarding delirium (Persian)]. Iran Journal of Nursing, 33(123), pp. 47-61. [Link]
Najafi Ghezeljeh, T., et al., 2022. The effects of interactive E-learning on delirium recognition ability and delirium-related strain of care among critical care nurses. Journal of the Intensive Care Society, 23(1), pp. 44–52. [DOI:10.1177/1751143720972627] [PMID]
Oh, E. S., et al., 2017. Delirium in older persons: Advances in diagnosis and treatment. JAMA, 318(12), pp.1161-74. [DOI:10.1001/jama.2017.12067] [PMID]
Panitchote, A., et al., 2015. Under-recognition of delirium in older adults by nurses in the intensive care unit setting. Aging Clinical and Experimental Research, 27(5), pp. 735–40.[DOI:10.1007/s40520-015-0323-6] [PMID]
Park, S. Y. & Lee, H. B., 2019. Prevention and management of delirium in critically ill adult patients in the intensive care unit: A review based on the 2018 PADIS guidelines. Acute and Critical Care, 34(2), pp. 117-25. [DOI:10.4266/acc.2019.00451] [PMID]
Reznik, M. E. & Slooter, A. J., 2019. Delirium management in the ICU. Current Treatment Options in Neurology, 21(11), pp. 59. [DOI:10.1007/s11940-019-0599-5] [PMID]
Ribeiro, S. C. L., et al., 2015. Knowledge of nurses about delirium in critical patients: Collective subject discourse. 24(2), pp. 513-20. [DOI:10.1590/0104-07072015001702014]
Rice, K. L., et al., 2011. Nurses’ recognition of delirium in the hospitalized older adult. Clinical Nurse Specialist, 25(6), pp. 299-311. [DOI:10.1097/NUR.0b013e318234897b] [PMID]
Rood, P., et al., 2018. Effect of organisational factors on the variation in incidence of delirium in intensive care unit patients: A systematic review and meta-regression analysis. Australian Critical Care, 31(3), pp. 180-7. [DOI:10.1016/j.aucc.2018.02.002] [PMID]
Rowley-Conwy, G., 2017. Critical care nurses’ knowledge and practice of delirium assessment. British Journal of Nursing, 26(7), pp. 412-7. [DOI:10.12968/bjon.2017.26.7.412] [PMID]
Slooter, A. J., Van De Leur, R. R. & Zaal, I. J., 2017. Delirium in critically ill patients. Handbook of Clinical Neurology, 141, pp. 449-66. [DOI:10.1016/B978-0-444-63599-0.00025-9] [PMID]
Trogrlić, Z., et al., 2017. Attitudes, knowledge and practices concerning delirium: A survey among intensive care unit professionals. Nursing in Critical Care, 22(3), pp. 133-40. [DOI:10.1111/nicc.12239] [PMID]
Xing, H., et al., 2022. Knowledge, attitudes and practices of ICU nurses regarding subsyndromal delirium among 20 hospitals in China: A descriptive cross-sectional survey. BMJ Open, 12(9), pp. e063821. [DOI:10.1136/bmjopen-2022-063821] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2023/01/1 | Accepted: 2023/05/23 | Published: 2023/11/1
Received: 2023/01/1 | Accepted: 2023/05/23 | Published: 2023/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |