Fri, Aug 8, 2025
[Archive]
Volume 9, Issue 3 (Summer 2023)
JCCNC 2023, 9(3): 215-222 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yodang Y, Nuridah N. Characteristics and Palliative Care Needs of Older Indonesian Adults With Chronic Hypertension. JCCNC 2023; 9 (3) :215-222
URL: http://jccnc.iums.ac.ir/article-1-450-en.html
URL: http://jccnc.iums.ac.ir/article-1-450-en.html
1- Department of Nursing, Faculty of Science and Technology, Universitas Sembilanbelas November Kolaka, Kolaka, Indonesia. , yodang.usnkolaka@gmail.com
2- Department of Nursing, Faculty of Science and Technology, Universitas Sembilanbelas November Kolaka, Kolaka, Indonesia.
2- Department of Nursing, Faculty of Science and Technology, Universitas Sembilanbelas November Kolaka, Kolaka, Indonesia.
Full-Text [PDF 513 kb]
(555 Downloads)
| Abstract (HTML) (1912 Views)
Full-Text: (350 Views)
1. Introduction
Hypertension is the main risk factor for cardiovascular diseases and is the most common health-related problem in the general population that poses a health and economic problem worldwide (Oliveros et al., 2020; Uchmanowicz et al., 2018). Furthermore, hypertension significantly impacts cardiovascular outcomes such as heart failure, myocardial infarction, and stroke (Oliveros et al., 2020). Although high blood pressure is identified as a main cause of health-related issues globally, it is preventable and curable at low cost, and medications are available at all levels of healthcare facilities, from primary to tertiary ones (Hickey et al., 2022).
Hypertension contributes to the death rate of around 80% of the population globally, and its prevalence continues to increase, especially in developing countries such as Indonesia (Yodang & Nuridah, 2019). According to the Basic Health Research reports, the prevalence of hypertension in Indonesia differs in each province, ranging from 55.23% to 69.53% (Kemenkes, 2019). Further, Benetos et al. point out that the prevalence of hypertension is constantly growing due to the aging population, particularly those over 80 years old. Shifting demographic patterns elucidate that while the number of individuals at high risk of hypertension has slightly declined, the absolute number of individuals with hypertension is constantly growing (Benetos et al., 2019). Another study reports that blood pressure increases steadily with age, and consequently, the prevalence of hypertension is higher in older age groups (Anker et al., 2018).
There has been no consensus on the definition of chronic hypertension. The researchers have different points of view in defining chronic hypertension, but they generally agree that it has been developed over the years (Bateman et al., 2012). However, other researchers suggest its occurrence needs more than 3 months (Hickey et al., 2022). In addition, confirmation of chronic hypertension must be based on a record documenting hypertension and previous or current antihypertensive treatment, including lifestyle measures (Tita et al., 2022). As a chronic disease, hypertension is responsible for the cause of death in 45% of heart diseases, 51% of strokes, and 6% of adult death worldwide (Kurt & Gurdogan, 2022). The progression of chronic hypertension may cause complications, such as brain damage, cognitive impairment, and cardiovascular and neurological dysfunctions like atherosclerotic or remodeling of cerebral autoregulation. Other complications are progressive increases in the blood flow of cerebral vessels (González-Marrero et al., 2022), renal disease, and damage to the retina (Nam et al., 2022). Besides physical complications, hypertension can cause psychological, social, and economic complications over time as a chronic disease. It also affects individuals’ independence and increases patient care needs (Kurt & Gurdogan, 2022). In addition, like other serious chronic diseases, chronic hypertension requires long-term home treatment as well as institutional care due to cognitive, mental, and functional deterioration, frailty, multi-morbidities, poly-pharmacies, and loss of self-support partially or completely (Benetos et al., 2019). It also leads to treatment expenses exceeding the disposable income of the household, which has been an important reason for the return of borderline-poor families to poverty (Xu & Yang, 2022), Of 56.7 million people who needed palliative care (PC) in 2020, only 12%, or about 7 million, could access and receive the palliative service worldwide (Kagarmanova et al., 2022). Notably, 76% of people who need PC globally live in low- and middle-income countries, including Indonesia (Esteban-Burgos et al., 2021). PC is an integrated approach that focuses on improving the quality of life of patients and their families, especially patients with life-limiting or -threatening illnesses. PC prevents and alleviates the suffering of patients and families through early identification, evaluation, and flawless treatment of pain and other problems, whether physical, psychological, social, or spiritual issues (WHO, 2020). To meet the essential care demands, it is recommended that PC services be integrated into existing healthcare systems, such as primary healthcare services. The PC service is useful and remains suitable for elderly patients with untreatable and incurable diseases requiring effective management for suffering symptoms. The service aims to improve older patients’ comfort and performance and meet their physical, psychological, spiritual, and social needs, including financial issues (Esteban-Burgos et al., 2021). This study assessed older patients’ characteristics, such as sociodemographic data, and determined their PC needs. Considering the complexity and variable nature of the disease course of elderly patients, it is necessary to use objective indicators to evaluate and identify PC needs among elderly people who live with chronic disease, especially hypertension (Esteban-Burgos et al., 2021). There is little evidence about indicators of PC needs among older adults with chronic hypertension in the Indonesian context. Accordingly, this study aims to identify the characteristics and determinants of PC needs among elderly Indonesian patients with chronic hypertension.
2. Materials and Methods
It was a cross-sectional study conducted in a primary healthcare setting in Kolaka, Sulawesi Tenggara, Indonesia, capital regency, from July to August 2022. The study population was all elderly patients diagnosed with chronic hypertension recruited using the census method. A total of 142 patients met the inclusion criteria of the study. The inclusion criteria were as follows: Being diagnosed with hypertension for more than 6 months, attending the outpatient department, receiving antihypertensive drugs, aged 55 years and older, and intend to participate in the study. The subjects with acute disease, communicable disease, and dementia were excluded from the study.
The research instrument consisted of sociodemographics and the supportive and palliative care indicators tool (SPICT). The sociodemographic variables included age (in years), gender, primary health care (PHC) location, and comorbidities. The PHC location was categorized into “rural” and “semi-urban.” Comorbidities were classified into “with comorbidities” and “without comorbidities.” The PC needs of the participants were assessed by using the SPICT.
Originally, the SPICT was developed and introduced by a scholar and research group at one of the universities in Scotland, UK. The tool could help multidisciplinary teams investigate patients who deteriorate from chronic disease and end of life in all care settings. The instrument comprises general and clinical indicators and a review of current care and care planning. The general indicators have 7 items, and the clinical indicators have 23 items and 8 life-limiting conditions. While the last part provides essential recommendations for reviewing and care planning. Patients with at least two common indicators of the SPICT indicated that the patients require PC services (Effendy et al., 2022).
A study conducted by Effendy et al. (2022) was the first Indonesian study on the SPICT translation. The study found that the instrument in the Indonesian version is valid and reliable for screening patients who need palliative care.
3. Results
The subjects were 142 elderlies with chronic hypertension. The age of the subjects ranged from 55 to 91 years; their Mean±SD age was 65.42±6.412 years with a standard error mean of 0.538. Most of them were female (55.6%), lived in rural areas (54.9%), had comorbidities (77.5%), and had one comorbid at least (66.9%). The details of the sociodemographics of the respondents are presented in Table 1.

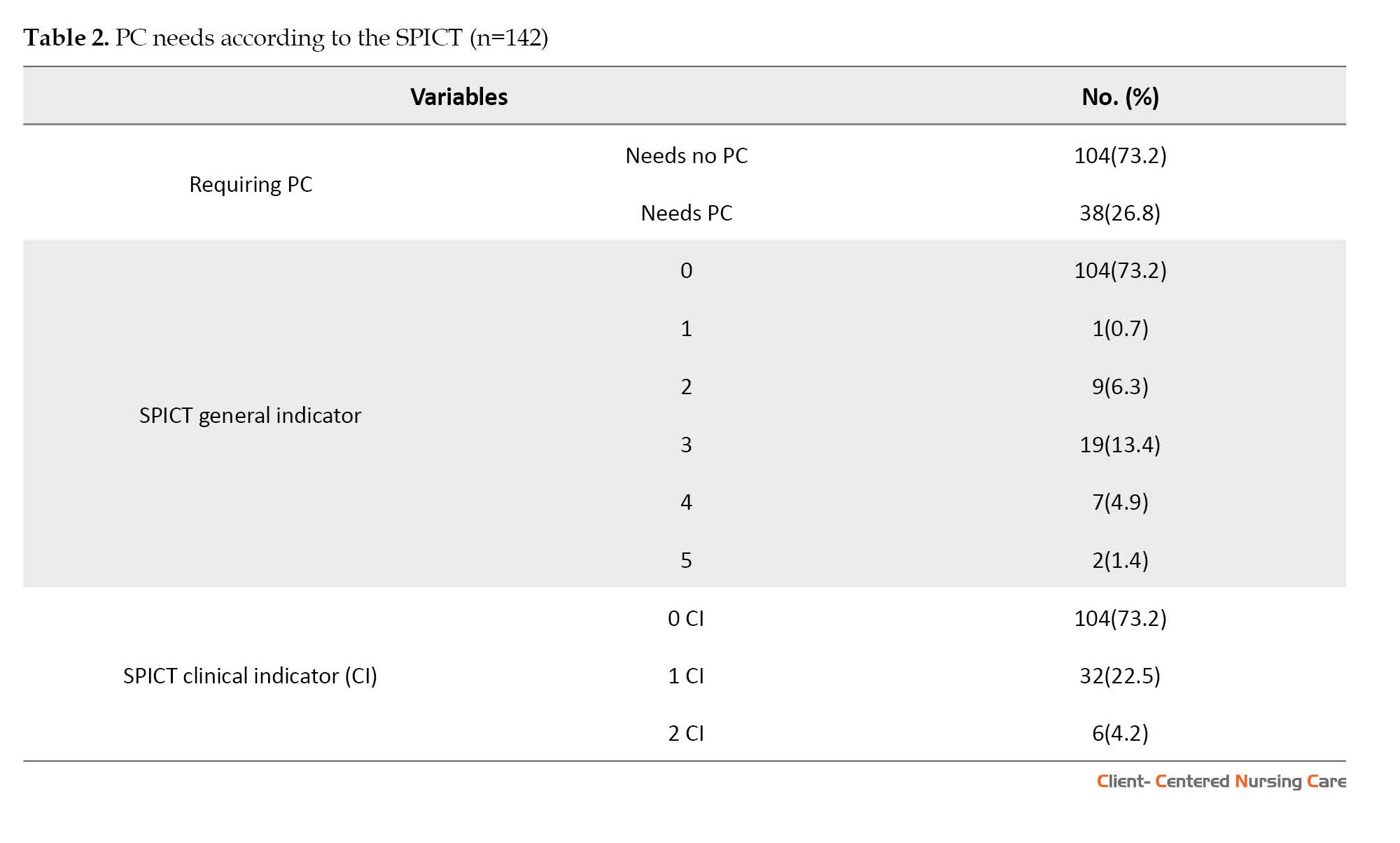
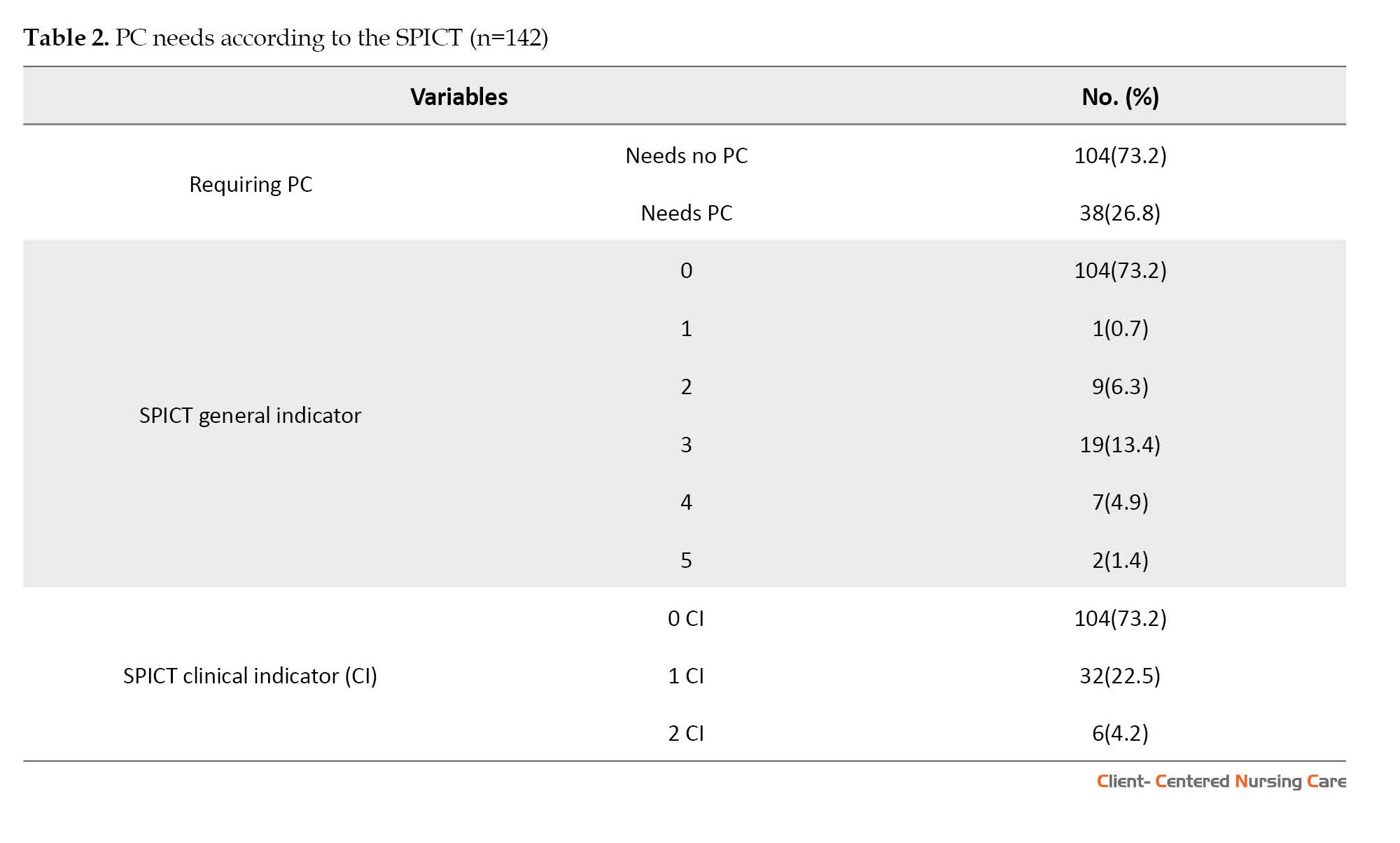
Based on the results, 26.8% of older adults needed PC (A patient is identified as a person in need of PC services when at least one indicator is found in the general and clinical indicators of the SPICT). Additionally, some subjects had 3 out of 6 general indicators, while others had 5 general indicators. For the clinical indicator, most subjects had one indicator. The detail of PC needs is presented in Table 2.
The detail of crosstab data analysis for the characteristics of the subjects and their PC needs is presented in Table 3.
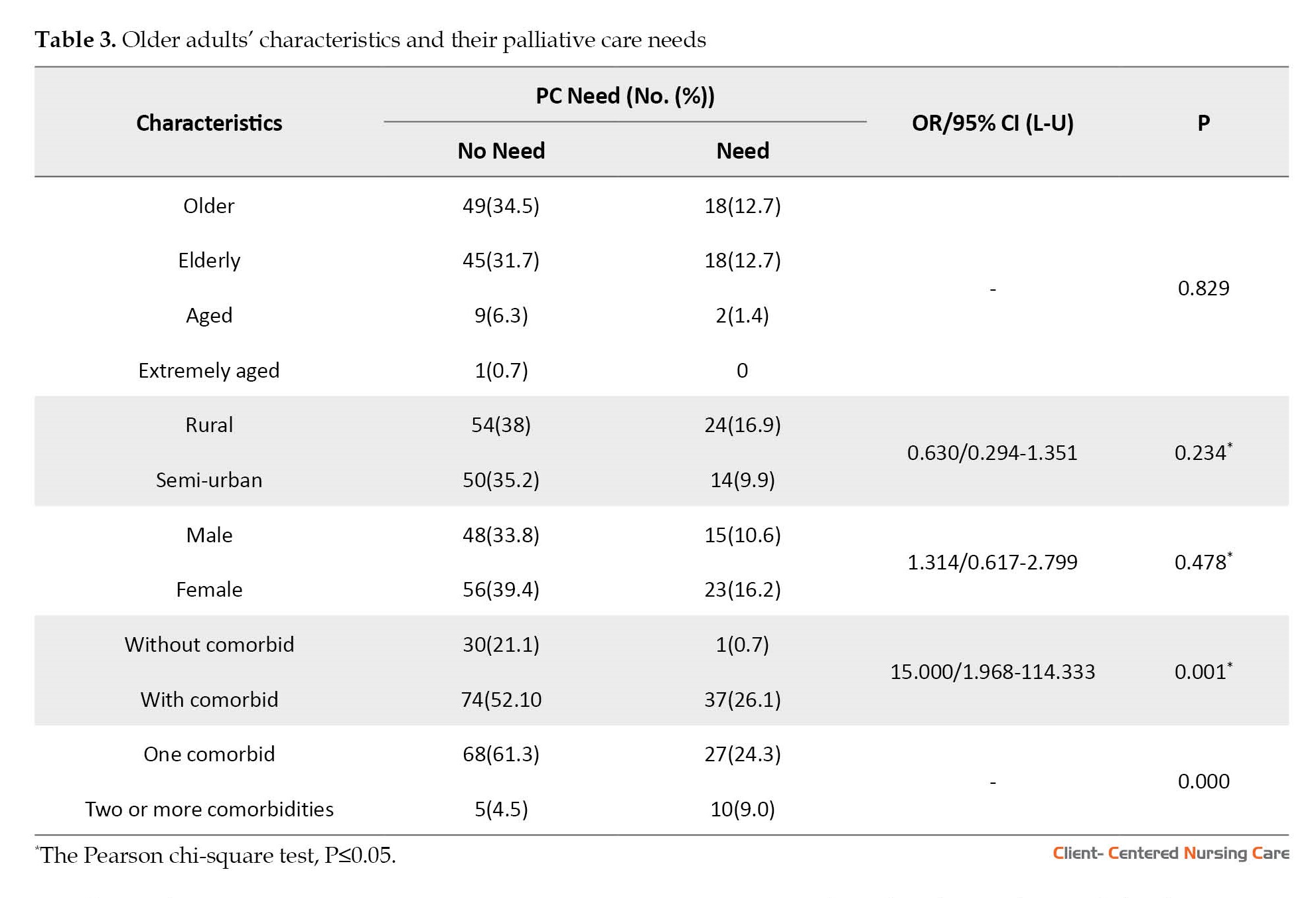
Based on the Pearson chi-square test for having comorbidities (P=0.001; 95% CI, 1.968%-114.333%), there is a significant relationship between comorbidities and PC needs among the subjects. Compared to patients without comorbidity, the odds ratio for comorbidity is 15.00 for PC needs. Further, according to the test results for the number of comorbidities (P=0.000), the number of comorbidities also has a significant relationship with requiring PC in older adults with chronic hypertension.
4. Discussion
To the best of our knowledge, this study, which focuses on chronic hypertension among older adults, and the assessment and identification of elderly patients with general PC needs, is the first to be conducted in Indonesia. According to the World Health Organization (WHO), PC should be available to all patients with special needs resulting from advanced and life-threatening to life-limiting illnesses, including older patients (Romanò et al., 2022).
Physicians, general practitioners, nurses, midwives, public health professionals, nutritionists and dieticians, and environmental health professionals have recently offered healthcare services in Indonesian primary care facilities. However, only physicians and nurses are responsible for monitoring patients’ clinical conditions, making connections, or organizing consultations when necessary (Marcucci et al., 2016). To improve access to palliative care, we must first investigate and understand the population’s needs (Etkind et al., 2017).
Based on the age groups, this study’s findings were consistent with a previous study conducted in a large city in a hospital setting in Indonesia. The study reported that 33.9% of respondents were between 56 and 65 (Effendy et al., 2022). In the same way, in our study, the age range of most participants (47.2%) was between 55-65 years.
In terms of gender, those who needed PC were predominantly females. However, there was no significant association between gender and PC needs among the participants. In contrast, another study reported that the severity and course of hypertension increase remarkably with aging advancement in women (Reddy et al., 2018). Furthermore, there are many challenges in geriatric cardiology, especially when making clinical decisions, because of not only the age of the patient but the overall medical, physical, social, and mental characteristics. Thus, each person should take place for personalized care (Oliveros et al., 2020).
A total of 77.5% of the respondents had comorbidities, and nearly 11% suffered two or more two comorbidities, while around 67% had one comorbidity. The reason for this finding in some cases may be a delayed diagnosis, and when they were recruited in this study, most of them suffered from hypertension for more than 6 months and even years. It means that comorbidities progression might have occurred during their disease course. Further, some studies have already reported that hypertension is the main risk factor for most morbidities in the elderly, such as cardiovascular and cerebrovascular diseases. Furthermore, it also causes poor quality of life and activities of daily living (Reddy et al., 2018). A study conducted in Thailand found that hypertension was the most common comorbidity in cancer and non-cancer patients. The study concluded that the low functional status and low survival in both cancer and non-cancer patients were more likely a reason for the patient needing PC and being admitted to the PC unit (Prompantakorn et al., 2021). Moreover, in line with our study, it has been found that patients with psychiatric comorbidity and serious disease are at high risk of poor quality of life and high symptom affliction, and psychiatric comorbidity is also related to increased use of PC (Sadowska et al., 2023).
Our study was conducted in one primary healthcare setting in Indonesia, and the sample size was small, thus limiting the generalizability of the findings. Furthermore, we did not include some characteristics of the respondents, such as the age when they were first diagnosed as hypertensive patients, medication adherence, and access to primary healthcare or healthcare facilities. Finally, the cross-sectional nature of the study limits its generalizability.
5. Conclusion
A total of 26.8% of the patients with chronic hypertension needed palliative care. According to the results, PC needs had a significant relationship with comorbidities. Also, older patients with more than one comorbidity had a higher demand for PC than those with only one. Medical professionals are suggested to pay more attention to comorbidities in patients with chronic hypertension. To provide stronger evidence, research with a larger sample size is recommended. Moreover, to strengthen the evidence related to PC needs among the elderly living with chronic hypertension, more sociodemographic characteristics like functional status, survival, and survival time are considered.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Health Research of Association of Indonesian Public Health Experts (Code: 547/UN4.6.4.5.31/PP36/2020). The study followed the Strengthening the reporting of observational studies in epidemiology (STROBE) guidelines, and the subjects signed an informed consent to participate in this study.
Funding
This research received a grant from the Indonesian Government (Grant No.: 073/SPK/D4/PPK.01.APTV/2022).
Authors' contributions
The authors equally contributed in preparation of this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Ministry of Education, Culture, and Research and Higher Education for the research grant under the Penelitian Dosen Pemula (PDP) scheme and the budget provided in 2022.
References
Anker, D., et al., 2018. Screening and treatment of hypertension in older adults: Less is more? Public Health Reviews, 39, pp. 26. [DOI:10.1186/s40985-018-0101-z] [PMID] [PMCID]
Bateman, B. T., et al., 2012. Prevalence, trends, and outcomes of chronic hypertension: A nationwide sample of delivery admissions. American Journal of Obstetrics and Gynecology, 206(2), pp. 134-e1. [DOI:10.1016/j.ajog.2011.10.878] [PMID] [PMCID]
Benetos, A., Petrovic, M. & Strandberg, T., 2019. Hypertension management in older and frail older patients. Circulation Research, 124(7), pp. 1045-60. [DOI:10.1161/CIRCRESAHA.118.313236] [PMID]
Efendy, C., Silva, J. F. D. S. & Padmawati, R. S., 2022. Identifying palliative care needs of patients with non-communicable disease in Indonesia using the SPICT tool: A descriptive cross- sectional study. BMC Palliative Care, 21(1), pp. 19. [PMID] [PMCID]
Esteban-Burgos, A. A., et al., 2021. A new approach to the identification of palliative care needs and advanced chronic patients among nursing home residents. International Journal of Environmental Research and Public Health, 18(6), pp. 3171. [DOI:10.3390/ijerph18063171] [PMID] [PMCID]
Etkind, S. N., et al., 2017. How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC Medicine, 15(1), pp. 102. [DOI:10.1186/s12916-017-0860-2] [PMID] [PMCID]
González-Marrero, I., et al., 2022. Altered Expression of AQP1 and AQP4 in brain barriers and cerebrospinal fluid may affect cerebral water balance during chronic hypertension. International Journal of Molecular Sciences, 23(20), pp. 12277. [DOI:10.3390/ijms232012277] [PMID] [PMCID]
Hickey, M. D., et al., 2022. Effect of a one-time financial incentive on linkage to chronic hypertension care in Kenya and Uganda: A randomized controlled trial. Plos One, 17(11), pp. e0277312. [DOI:10.1371/journal.pone.0277312] [PMID] [PMCID]
Kagarmanova, A., et al., 2022. Palliative care in Uganda: Quantitative descriptive study of key palliative care indicators 2018-2020. BMC Palliative Care, 21(1), pp. 55. [DOI:10.1186/s12904-022-00930-7] [PMID] [PMCID]
Kemenkes., 2019. Laporan Nasional Riskesdas 2018/Badan Penelitian dan Pengembangan Kesehatan. Jakarta: Lembaga Penerbit Badan Penelitian dan Pengembangan Kesehatan.
Kurt, D. & Gurdogan, E. P., 2022. The effect of self-management support on knowledge level, treatment compliance and selfcare management in patients with hypertension. Australian Journal of Advanced Nursing, 39(3), pp. 14-23. [DOI:10.37464/2020.393.543]
Marcucci, F. C., et al., 2016. Identification and characteristics of patients with palliative care needs in Brazilian primary care. BMC Palliative Care, 15, pp. 51. [DOI:10.1186/s12904-016-0125-4] [PMID] [PMCID]
Nam, K. Y., et al., 2022. Different characteristics of retinal damage between chronic hypertension and hypertensive retinopathy. Scientific Reports, 12(1), pp. 18902. [DOI:10.1038/s41598-022-23756-y] [PMID] [PMCID]
Oliveros, E., et al., 2020. Hypertension in older adults: Assessment, management, and challenges. Clinical Cardiology, 43(2), pp. 99-107. [DOI:10.1002/clc.23303] [PMID] [PMCID]
Prompantakorn, P., et al., 2021. Palliative Performance Scale and survival in patients with cancer and non-cancer diagnoses needing a palliative care consultation: A retrospective cohort study. BMC Palliative Care, 20(1), pp. 74. [DOI:10.1186/s12904-021-00773-8] [PMID] [PMCID]
Reddy, B. M., Ganguly, E. & Sharma, P. K., 2018. Hypertension and its correlates in the oldest old population aged 80 years and above in urban South India. Journal of Gerontology & Geriatric Research, 7(3), pp. 472. [DOI:10.4172/2167-7182.1000472] [PMID] [PMCID]
Romanò, M., et al., 2022. Palliative care for patients with end-stage, non-oncologic diseases-a retrospective study in three public palliative care departments in Northern Italy. Healthcare, 10(6), pp. 1031. [DOI:10.3390/healthcare10061031] [PMID] [PMCID]
Sadowska, K., et al., 2023. Psychiatric comorbidities and outcomes in palliative and end-of-life care: A systematic review. Journal of Pain and Symptom Management, 66(1), pp. e129–51. [DOI:10.1016/j.jpainsymman.2023.03.007] [PMID]
Hypertension is the main risk factor for cardiovascular diseases and is the most common health-related problem in the general population that poses a health and economic problem worldwide (Oliveros et al., 2020; Uchmanowicz et al., 2018). Furthermore, hypertension significantly impacts cardiovascular outcomes such as heart failure, myocardial infarction, and stroke (Oliveros et al., 2020). Although high blood pressure is identified as a main cause of health-related issues globally, it is preventable and curable at low cost, and medications are available at all levels of healthcare facilities, from primary to tertiary ones (Hickey et al., 2022).
Hypertension contributes to the death rate of around 80% of the population globally, and its prevalence continues to increase, especially in developing countries such as Indonesia (Yodang & Nuridah, 2019). According to the Basic Health Research reports, the prevalence of hypertension in Indonesia differs in each province, ranging from 55.23% to 69.53% (Kemenkes, 2019). Further, Benetos et al. point out that the prevalence of hypertension is constantly growing due to the aging population, particularly those over 80 years old. Shifting demographic patterns elucidate that while the number of individuals at high risk of hypertension has slightly declined, the absolute number of individuals with hypertension is constantly growing (Benetos et al., 2019). Another study reports that blood pressure increases steadily with age, and consequently, the prevalence of hypertension is higher in older age groups (Anker et al., 2018).
There has been no consensus on the definition of chronic hypertension. The researchers have different points of view in defining chronic hypertension, but they generally agree that it has been developed over the years (Bateman et al., 2012). However, other researchers suggest its occurrence needs more than 3 months (Hickey et al., 2022). In addition, confirmation of chronic hypertension must be based on a record documenting hypertension and previous or current antihypertensive treatment, including lifestyle measures (Tita et al., 2022). As a chronic disease, hypertension is responsible for the cause of death in 45% of heart diseases, 51% of strokes, and 6% of adult death worldwide (Kurt & Gurdogan, 2022). The progression of chronic hypertension may cause complications, such as brain damage, cognitive impairment, and cardiovascular and neurological dysfunctions like atherosclerotic or remodeling of cerebral autoregulation. Other complications are progressive increases in the blood flow of cerebral vessels (González-Marrero et al., 2022), renal disease, and damage to the retina (Nam et al., 2022). Besides physical complications, hypertension can cause psychological, social, and economic complications over time as a chronic disease. It also affects individuals’ independence and increases patient care needs (Kurt & Gurdogan, 2022). In addition, like other serious chronic diseases, chronic hypertension requires long-term home treatment as well as institutional care due to cognitive, mental, and functional deterioration, frailty, multi-morbidities, poly-pharmacies, and loss of self-support partially or completely (Benetos et al., 2019). It also leads to treatment expenses exceeding the disposable income of the household, which has been an important reason for the return of borderline-poor families to poverty (Xu & Yang, 2022), Of 56.7 million people who needed palliative care (PC) in 2020, only 12%, or about 7 million, could access and receive the palliative service worldwide (Kagarmanova et al., 2022). Notably, 76% of people who need PC globally live in low- and middle-income countries, including Indonesia (Esteban-Burgos et al., 2021). PC is an integrated approach that focuses on improving the quality of life of patients and their families, especially patients with life-limiting or -threatening illnesses. PC prevents and alleviates the suffering of patients and families through early identification, evaluation, and flawless treatment of pain and other problems, whether physical, psychological, social, or spiritual issues (WHO, 2020). To meet the essential care demands, it is recommended that PC services be integrated into existing healthcare systems, such as primary healthcare services. The PC service is useful and remains suitable for elderly patients with untreatable and incurable diseases requiring effective management for suffering symptoms. The service aims to improve older patients’ comfort and performance and meet their physical, psychological, spiritual, and social needs, including financial issues (Esteban-Burgos et al., 2021). This study assessed older patients’ characteristics, such as sociodemographic data, and determined their PC needs. Considering the complexity and variable nature of the disease course of elderly patients, it is necessary to use objective indicators to evaluate and identify PC needs among elderly people who live with chronic disease, especially hypertension (Esteban-Burgos et al., 2021). There is little evidence about indicators of PC needs among older adults with chronic hypertension in the Indonesian context. Accordingly, this study aims to identify the characteristics and determinants of PC needs among elderly Indonesian patients with chronic hypertension.
2. Materials and Methods
It was a cross-sectional study conducted in a primary healthcare setting in Kolaka, Sulawesi Tenggara, Indonesia, capital regency, from July to August 2022. The study population was all elderly patients diagnosed with chronic hypertension recruited using the census method. A total of 142 patients met the inclusion criteria of the study. The inclusion criteria were as follows: Being diagnosed with hypertension for more than 6 months, attending the outpatient department, receiving antihypertensive drugs, aged 55 years and older, and intend to participate in the study. The subjects with acute disease, communicable disease, and dementia were excluded from the study.
The research instrument consisted of sociodemographics and the supportive and palliative care indicators tool (SPICT). The sociodemographic variables included age (in years), gender, primary health care (PHC) location, and comorbidities. The PHC location was categorized into “rural” and “semi-urban.” Comorbidities were classified into “with comorbidities” and “without comorbidities.” The PC needs of the participants were assessed by using the SPICT.
Originally, the SPICT was developed and introduced by a scholar and research group at one of the universities in Scotland, UK. The tool could help multidisciplinary teams investigate patients who deteriorate from chronic disease and end of life in all care settings. The instrument comprises general and clinical indicators and a review of current care and care planning. The general indicators have 7 items, and the clinical indicators have 23 items and 8 life-limiting conditions. While the last part provides essential recommendations for reviewing and care planning. Patients with at least two common indicators of the SPICT indicated that the patients require PC services (Effendy et al., 2022).
A study conducted by Effendy et al. (2022) was the first Indonesian study on the SPICT translation. The study found that the instrument in the Indonesian version is valid and reliable for screening patients who need palliative care.
3. Results
The subjects were 142 elderlies with chronic hypertension. The age of the subjects ranged from 55 to 91 years; their Mean±SD age was 65.42±6.412 years with a standard error mean of 0.538. Most of them were female (55.6%), lived in rural areas (54.9%), had comorbidities (77.5%), and had one comorbid at least (66.9%). The details of the sociodemographics of the respondents are presented in Table 1.

Based on the results, 26.8% of older adults needed PC (A patient is identified as a person in need of PC services when at least one indicator is found in the general and clinical indicators of the SPICT). Additionally, some subjects had 3 out of 6 general indicators, while others had 5 general indicators. For the clinical indicator, most subjects had one indicator. The detail of PC needs is presented in Table 2.
The detail of crosstab data analysis for the characteristics of the subjects and their PC needs is presented in Table 3.
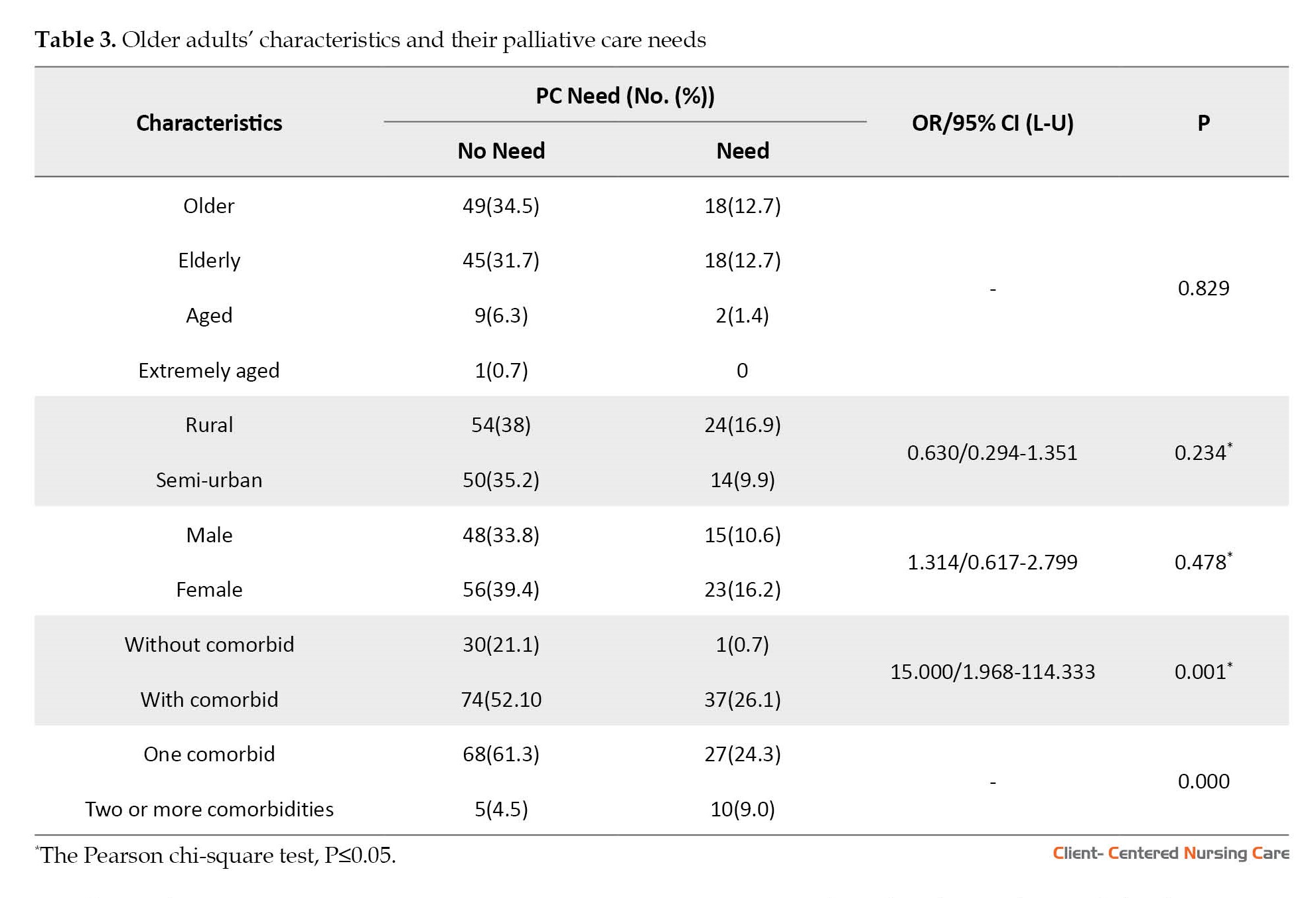
Based on the Pearson chi-square test for having comorbidities (P=0.001; 95% CI, 1.968%-114.333%), there is a significant relationship between comorbidities and PC needs among the subjects. Compared to patients without comorbidity, the odds ratio for comorbidity is 15.00 for PC needs. Further, according to the test results for the number of comorbidities (P=0.000), the number of comorbidities also has a significant relationship with requiring PC in older adults with chronic hypertension.
4. Discussion
To the best of our knowledge, this study, which focuses on chronic hypertension among older adults, and the assessment and identification of elderly patients with general PC needs, is the first to be conducted in Indonesia. According to the World Health Organization (WHO), PC should be available to all patients with special needs resulting from advanced and life-threatening to life-limiting illnesses, including older patients (Romanò et al., 2022).
Physicians, general practitioners, nurses, midwives, public health professionals, nutritionists and dieticians, and environmental health professionals have recently offered healthcare services in Indonesian primary care facilities. However, only physicians and nurses are responsible for monitoring patients’ clinical conditions, making connections, or organizing consultations when necessary (Marcucci et al., 2016). To improve access to palliative care, we must first investigate and understand the population’s needs (Etkind et al., 2017).
Based on the age groups, this study’s findings were consistent with a previous study conducted in a large city in a hospital setting in Indonesia. The study reported that 33.9% of respondents were between 56 and 65 (Effendy et al., 2022). In the same way, in our study, the age range of most participants (47.2%) was between 55-65 years.
In terms of gender, those who needed PC were predominantly females. However, there was no significant association between gender and PC needs among the participants. In contrast, another study reported that the severity and course of hypertension increase remarkably with aging advancement in women (Reddy et al., 2018). Furthermore, there are many challenges in geriatric cardiology, especially when making clinical decisions, because of not only the age of the patient but the overall medical, physical, social, and mental characteristics. Thus, each person should take place for personalized care (Oliveros et al., 2020).
A total of 77.5% of the respondents had comorbidities, and nearly 11% suffered two or more two comorbidities, while around 67% had one comorbidity. The reason for this finding in some cases may be a delayed diagnosis, and when they were recruited in this study, most of them suffered from hypertension for more than 6 months and even years. It means that comorbidities progression might have occurred during their disease course. Further, some studies have already reported that hypertension is the main risk factor for most morbidities in the elderly, such as cardiovascular and cerebrovascular diseases. Furthermore, it also causes poor quality of life and activities of daily living (Reddy et al., 2018). A study conducted in Thailand found that hypertension was the most common comorbidity in cancer and non-cancer patients. The study concluded that the low functional status and low survival in both cancer and non-cancer patients were more likely a reason for the patient needing PC and being admitted to the PC unit (Prompantakorn et al., 2021). Moreover, in line with our study, it has been found that patients with psychiatric comorbidity and serious disease are at high risk of poor quality of life and high symptom affliction, and psychiatric comorbidity is also related to increased use of PC (Sadowska et al., 2023).
Our study was conducted in one primary healthcare setting in Indonesia, and the sample size was small, thus limiting the generalizability of the findings. Furthermore, we did not include some characteristics of the respondents, such as the age when they were first diagnosed as hypertensive patients, medication adherence, and access to primary healthcare or healthcare facilities. Finally, the cross-sectional nature of the study limits its generalizability.
5. Conclusion
A total of 26.8% of the patients with chronic hypertension needed palliative care. According to the results, PC needs had a significant relationship with comorbidities. Also, older patients with more than one comorbidity had a higher demand for PC than those with only one. Medical professionals are suggested to pay more attention to comorbidities in patients with chronic hypertension. To provide stronger evidence, research with a larger sample size is recommended. Moreover, to strengthen the evidence related to PC needs among the elderly living with chronic hypertension, more sociodemographic characteristics like functional status, survival, and survival time are considered.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Health Research of Association of Indonesian Public Health Experts (Code: 547/UN4.6.4.5.31/PP36/2020). The study followed the Strengthening the reporting of observational studies in epidemiology (STROBE) guidelines, and the subjects signed an informed consent to participate in this study.
Funding
This research received a grant from the Indonesian Government (Grant No.: 073/SPK/D4/PPK.01.APTV/2022).
Authors' contributions
The authors equally contributed in preparation of this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Ministry of Education, Culture, and Research and Higher Education for the research grant under the Penelitian Dosen Pemula (PDP) scheme and the budget provided in 2022.
References
Anker, D., et al., 2018. Screening and treatment of hypertension in older adults: Less is more? Public Health Reviews, 39, pp. 26. [DOI:10.1186/s40985-018-0101-z] [PMID] [PMCID]
Bateman, B. T., et al., 2012. Prevalence, trends, and outcomes of chronic hypertension: A nationwide sample of delivery admissions. American Journal of Obstetrics and Gynecology, 206(2), pp. 134-e1. [DOI:10.1016/j.ajog.2011.10.878] [PMID] [PMCID]
Benetos, A., Petrovic, M. & Strandberg, T., 2019. Hypertension management in older and frail older patients. Circulation Research, 124(7), pp. 1045-60. [DOI:10.1161/CIRCRESAHA.118.313236] [PMID]
Efendy, C., Silva, J. F. D. S. & Padmawati, R. S., 2022. Identifying palliative care needs of patients with non-communicable disease in Indonesia using the SPICT tool: A descriptive cross- sectional study. BMC Palliative Care, 21(1), pp. 19. [PMID] [PMCID]
Esteban-Burgos, A. A., et al., 2021. A new approach to the identification of palliative care needs and advanced chronic patients among nursing home residents. International Journal of Environmental Research and Public Health, 18(6), pp. 3171. [DOI:10.3390/ijerph18063171] [PMID] [PMCID]
Etkind, S. N., et al., 2017. How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC Medicine, 15(1), pp. 102. [DOI:10.1186/s12916-017-0860-2] [PMID] [PMCID]
González-Marrero, I., et al., 2022. Altered Expression of AQP1 and AQP4 in brain barriers and cerebrospinal fluid may affect cerebral water balance during chronic hypertension. International Journal of Molecular Sciences, 23(20), pp. 12277. [DOI:10.3390/ijms232012277] [PMID] [PMCID]
Hickey, M. D., et al., 2022. Effect of a one-time financial incentive on linkage to chronic hypertension care in Kenya and Uganda: A randomized controlled trial. Plos One, 17(11), pp. e0277312. [DOI:10.1371/journal.pone.0277312] [PMID] [PMCID]
Kagarmanova, A., et al., 2022. Palliative care in Uganda: Quantitative descriptive study of key palliative care indicators 2018-2020. BMC Palliative Care, 21(1), pp. 55. [DOI:10.1186/s12904-022-00930-7] [PMID] [PMCID]
Kemenkes., 2019. Laporan Nasional Riskesdas 2018/Badan Penelitian dan Pengembangan Kesehatan. Jakarta: Lembaga Penerbit Badan Penelitian dan Pengembangan Kesehatan.
Kurt, D. & Gurdogan, E. P., 2022. The effect of self-management support on knowledge level, treatment compliance and selfcare management in patients with hypertension. Australian Journal of Advanced Nursing, 39(3), pp. 14-23. [DOI:10.37464/2020.393.543]
Marcucci, F. C., et al., 2016. Identification and characteristics of patients with palliative care needs in Brazilian primary care. BMC Palliative Care, 15, pp. 51. [DOI:10.1186/s12904-016-0125-4] [PMID] [PMCID]
Nam, K. Y., et al., 2022. Different characteristics of retinal damage between chronic hypertension and hypertensive retinopathy. Scientific Reports, 12(1), pp. 18902. [DOI:10.1038/s41598-022-23756-y] [PMID] [PMCID]
Oliveros, E., et al., 2020. Hypertension in older adults: Assessment, management, and challenges. Clinical Cardiology, 43(2), pp. 99-107. [DOI:10.1002/clc.23303] [PMID] [PMCID]
Prompantakorn, P., et al., 2021. Palliative Performance Scale and survival in patients with cancer and non-cancer diagnoses needing a palliative care consultation: A retrospective cohort study. BMC Palliative Care, 20(1), pp. 74. [DOI:10.1186/s12904-021-00773-8] [PMID] [PMCID]
Reddy, B. M., Ganguly, E. & Sharma, P. K., 2018. Hypertension and its correlates in the oldest old population aged 80 years and above in urban South India. Journal of Gerontology & Geriatric Research, 7(3), pp. 472. [DOI:10.4172/2167-7182.1000472] [PMID] [PMCID]
Romanò, M., et al., 2022. Palliative care for patients with end-stage, non-oncologic diseases-a retrospective study in three public palliative care departments in Northern Italy. Healthcare, 10(6), pp. 1031. [DOI:10.3390/healthcare10061031] [PMID] [PMCID]
Sadowska, K., et al., 2023. Psychiatric comorbidities and outcomes in palliative and end-of-life care: A systematic review. Journal of Pain and Symptom Management, 66(1), pp. e129–51. [DOI:10.1016/j.jpainsymman.2023.03.007] [PMID]
Type of Study: Research |
Subject:
General
Received: 2023/01/4 | Accepted: 2023/04/24 | Published: 2023/08/24
Received: 2023/01/4 | Accepted: 2023/04/24 | Published: 2023/08/24
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






