Sun, Jul 6, 2025
[Archive]
Volume 9, Issue 3 (Summer 2023)
JCCNC 2023, 9(3): 223-230 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aghamohammadi F, Saed O, Dinmohammadi M. Factors Affecting the Resilience of Iranian Nurses During the COVID-19 Pandemic. JCCNC 2023; 9 (3) :223-230
URL: http://jccnc.iums.ac.ir/article-1-451-en.html
URL: http://jccnc.iums.ac.ir/article-1-451-en.html
1- Department of Critical Care Nursing, Nursing and Midwifery School, Zanjan University of Medical Sciences, Zanjan, Iran.
2- Department of Clinical Psychology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran.
3- Social Determinants of Health Research Center, Zanjan University of Medical Sciences, Zanjan, Iran. ,mdinmohammadi@zums.ac.ir
2- Department of Clinical Psychology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran.
3- Social Determinants of Health Research Center, Zanjan University of Medical Sciences, Zanjan, Iran. ,
Full-Text [PDF 589 kb]
(505 Downloads)
| Abstract (HTML) (1723 Views)
Full-Text: (407 Views)
1. Introduction
In December 2019, a viral outbreak was reported in Wuhan, China. This disease was caused by a newly created and genetically modified coronavirus called SARS-CoV2, also known as COVID-19 (Zhu, Wei &Niu, 2020). The World Health Organization (WHO) announced the outbreak of a novel coronavirus in January 2020 and declared it an epidemic and public health concern in March 2020 (Zhou et al., 2020; Hasanzadeh et al., 2022).
Healthcare providers (HCWs) are regarded as the first to be exposed to the COVID-19 virus, leading the fight against the disease (Bao et al., 2020; Sood, 2020; Dinmohammadi et al., 2022). The prevalence of psychological disorders among healthcare personnel during pandemics has ranged between 50% and 75% (Lai et al., 2020; Pothiawala, 2020; Wu et al., 2009).
At the onset of the pandemic, the initial focus was on discovering new cases and preventing the spread of the disease, and its psychological effects were given less consideration (Xiang et al., 2020). The first studies on the psychological performance of humans in the face of a pandemic were undertaken by Chinese researchers (Lai et al., 2020). Direct interaction with COVID-19-infected patients exposes nurses to more traumatic situations, such as witnessing their suffering and death, heightening their fear and anxiety (Pappa et al., 2020). There has been a rise in posttraumatic stress disorder, anxiety, and insomnia among healthcare workers and patients (Bozdağ & Ergün, 2020). The prevalence of anxiety among healthcare professionals (HCPs) ranges from 22.6% to 36.3%. This rate is much higher than the general population’s rate of anxiety (Huang et al., 2020c). As a result, maintaining the mental health of frontline actors will become a critical global health concern in the months and possibly years to come (Kluge, 2020).
Promoting resilience among healthcare workers and organizations starts with understanding what resilience is (and is not). Historical psychology and the social sciences have conceptualized resilience as a trait (e.g. hardiness), a process (e.g. adaptation), or an outcome (e.g. the absence of posttraumatic stress or the presence of posttraumatic growth after particular adversity). Modern psychology and social science define resilience as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress” (Southwick et al., 2014). Resilience can play an adaptive role in alleviating stress and anxiety brought on by the COVID-19 crisis (Lupe et al., 2020; Polizzi et al., 2020).
Earlier studies have shown that nurses and other HCPs experience profound challenges during the recent pandemic, which may have affected their physical and emotional health and, subsequently, their professional performance (Foster et al., 2019). Due to the COVID-19 outbreak, HCPs must work under the most challenging circumstances (Greenberg et al., 2020). If HCPs and nurses lack the necessary resilience, not only will they be unable to recover, but the cumulative effects of negative emotions may also lead to psychological disorders (Huang et al., 2020b). To survive the COVID-19 pandemic, it is essential to support healthcare professionals’ mental health and resilience, particularly nurses (Huang et al., 2020a).
Also, it has been demonstrated that personal (e.g. gender, age, marital status), occupational (e.g. experience, working shift, employment status), and personality characteristics (e.g. optimism, perseverance, and cooperation) contribute to the development of resilience in HCPs (Iflaifel et al., 2020; Lisi et al., 2020).
Access to key medical, laboratory, and pharmaceutical equipment for hospitalized patient care has become significantly more difficult and unbearable due to the persistence of harsh sanctions against Iran. Unlike other countries, these issues may jeopardize Iranian nurses’ mental health and resilience (Takian et al., 2020). There is limited data available on the resilience of Iranian nurses and its determinants, particularly in light of the recent pandemic. This study aimed to identify the factors affecting Iranian nurses’ resilience in hospitals nationwide.
2. Materials and Methods
This cross-sectional web-based survey was conducted using the Google Forms platform during the pandemic. The Iranian nurses working in public and private hospitals were invited to participate in the survey via social networks like Telegram and WhatsApp. The inclusion criteria were willingness to participate in the study, a bachelor’s degree or higher in nursing, and at least 6 months of active employment. Incomplete surveys were the exclusion criterion.
The information was gathered from November 7 to November 29, 2020, using an online questionnaire. Participants had a maximum of 10 minutes to complete the questionnaires and were required to answer all the questions. Each individual was only permitted to complete the questionnaire once. To increase the response rate, reminder messages were sent to nurses’ social networks through the network administrator during the study course. A total of 1045 questionnaires were submitted by nurses who participated in the study. Twenty instances of surveys with missing information were omitted from the analysis. In the end, 1025 questionnaires were examined.
The study instrument was a two-part online questionnaire, with the first part pertaining to individual and occupational factors (age, gender, role, marital status, education level, work experience, employment status, type of ward, working in the COVID-19 ward, getting COVID-19, and working shift), and the second part comprising the 25-item Connor-Davidson resilience scale (CD-RISC). The questionnaire is rated on a 5-point Likert scale (completely incorrect=0 to completely correct=4). The minimum and maximum scores on this scale are 0 and 100, respectively, and higher scores indicate greater resilience (Connor & Davidson, 2003). The Persian version of this scale has been psychometrically tested, and its validity and reliability have been confirmed (Khoshouei, 2009; Samani et al., 2007). In this study, the Cronbach α reliability of the instrument was determined to be 0.87.
Data analysis
The frequency, Mean±SD were the indicators to describe the personal and occupational characteristics of the nurses. The distribution of data related to resilience was normal. The multiple linear regression (enter model) was used to investigate the influence of personal and occupational factors in predicting the nurses’ resilience. The assumptions of multiple linear regression analysis were established. The data were analyzed using SPSS software, version 22. The significance level was P<0.05.
3. Results
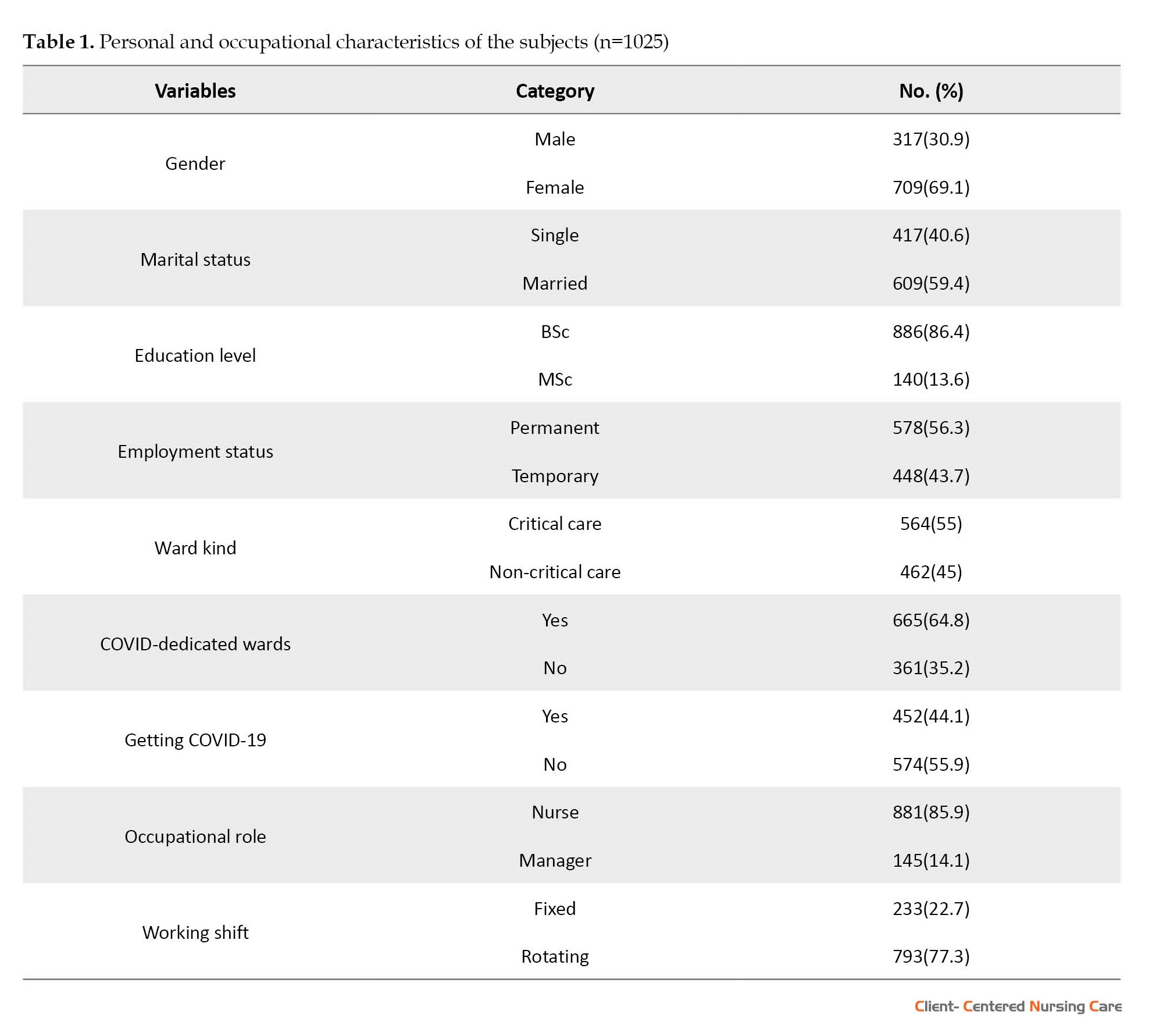
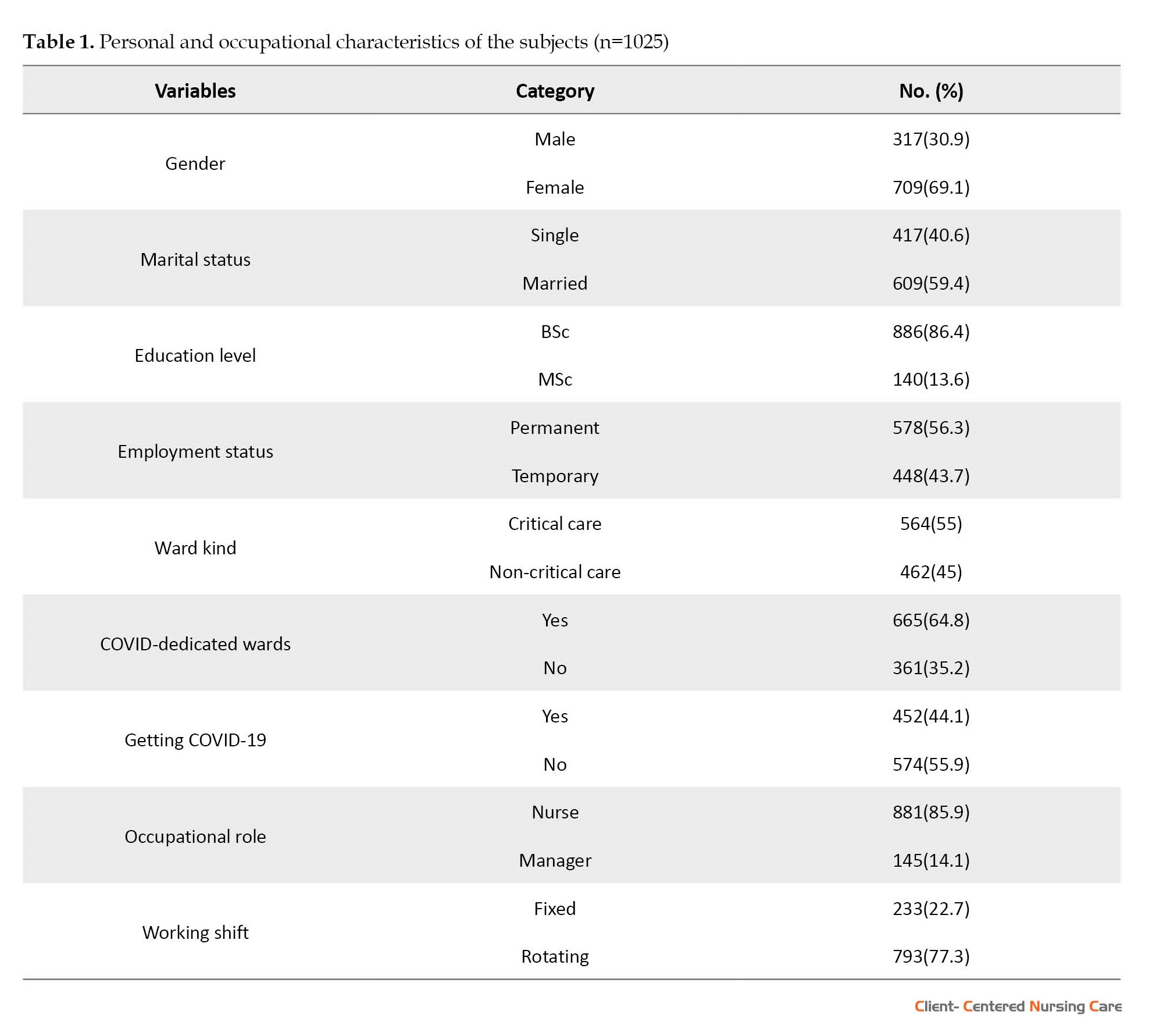
Among the 1045 surveys received, 1025 were valid and analyzable. The Mean±SD age of the nurses was 33.79±6.98 years, and their work experience was 9.61±6.62 years (Table 1).
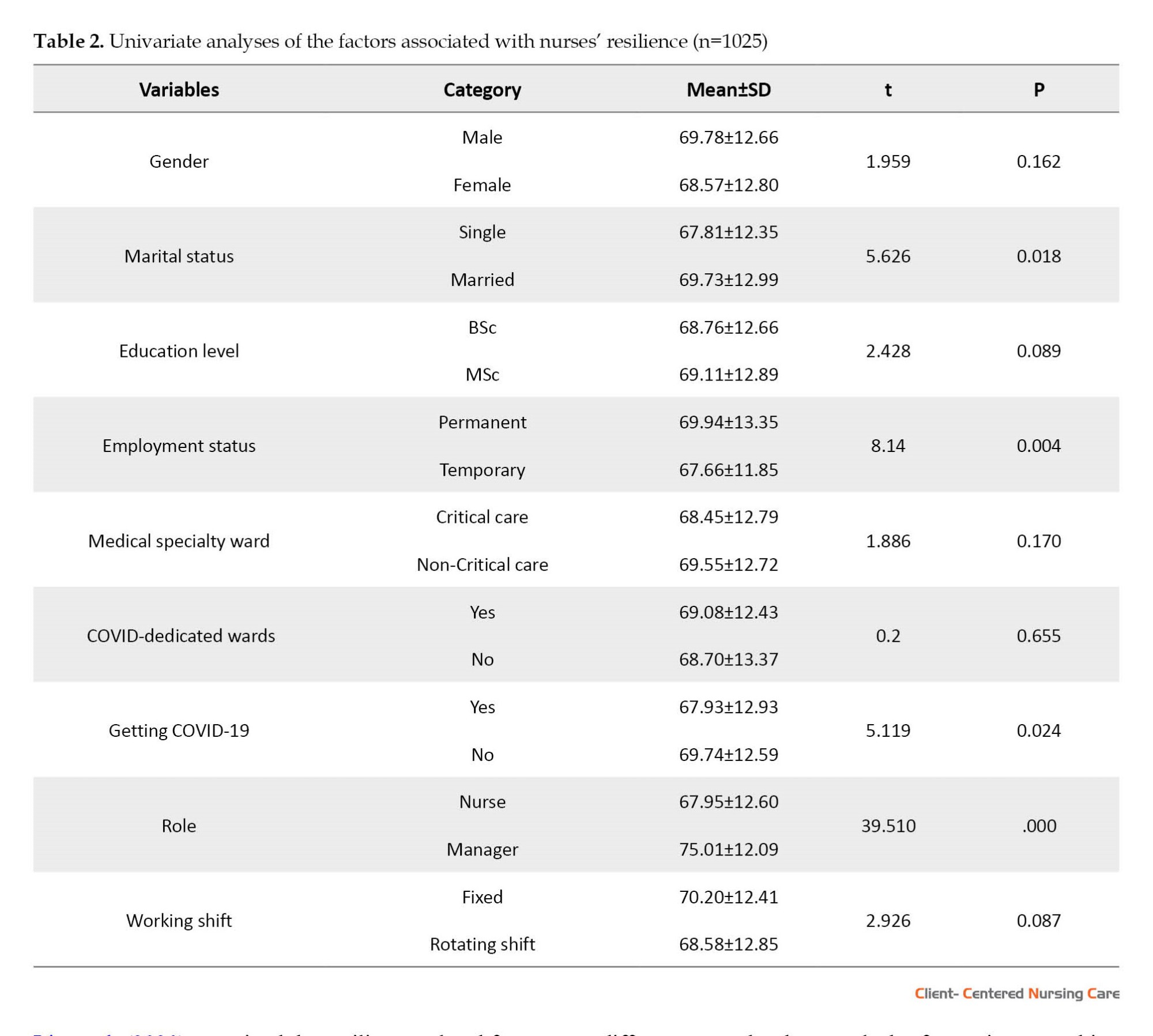
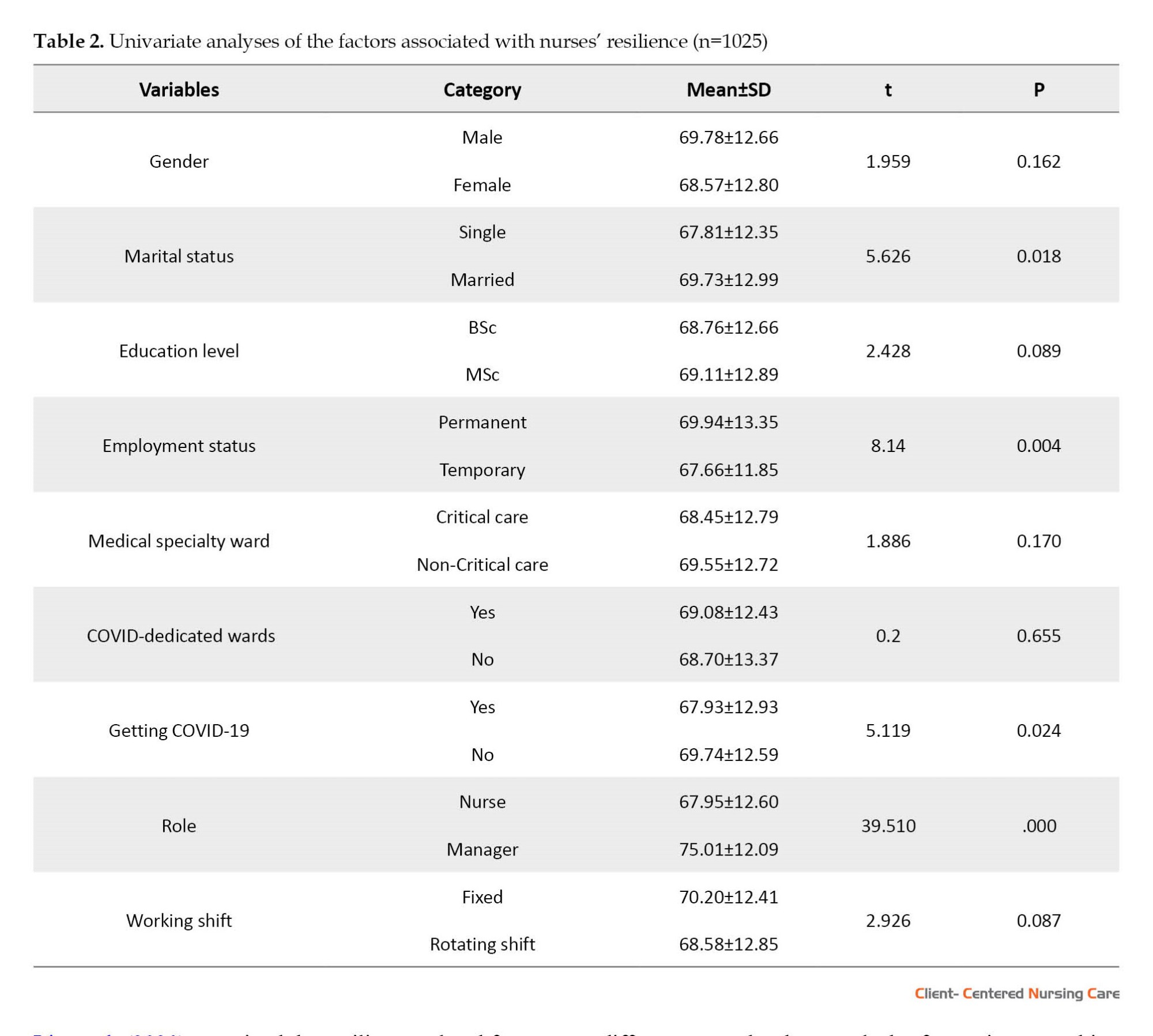
The nurses’ total Mean±SD resilience score was 68.95±12.76. According to the results of the t-test for independent groups, nurses who were married (P<0.001), permanently employed (P=0.004), and not infected with COVID-19 (P=0.024) were more resilient than others. Also, nurses in managerial roles (P<0.001) were more resilient than clinical nurses. Other variables were not significant (Table 2).
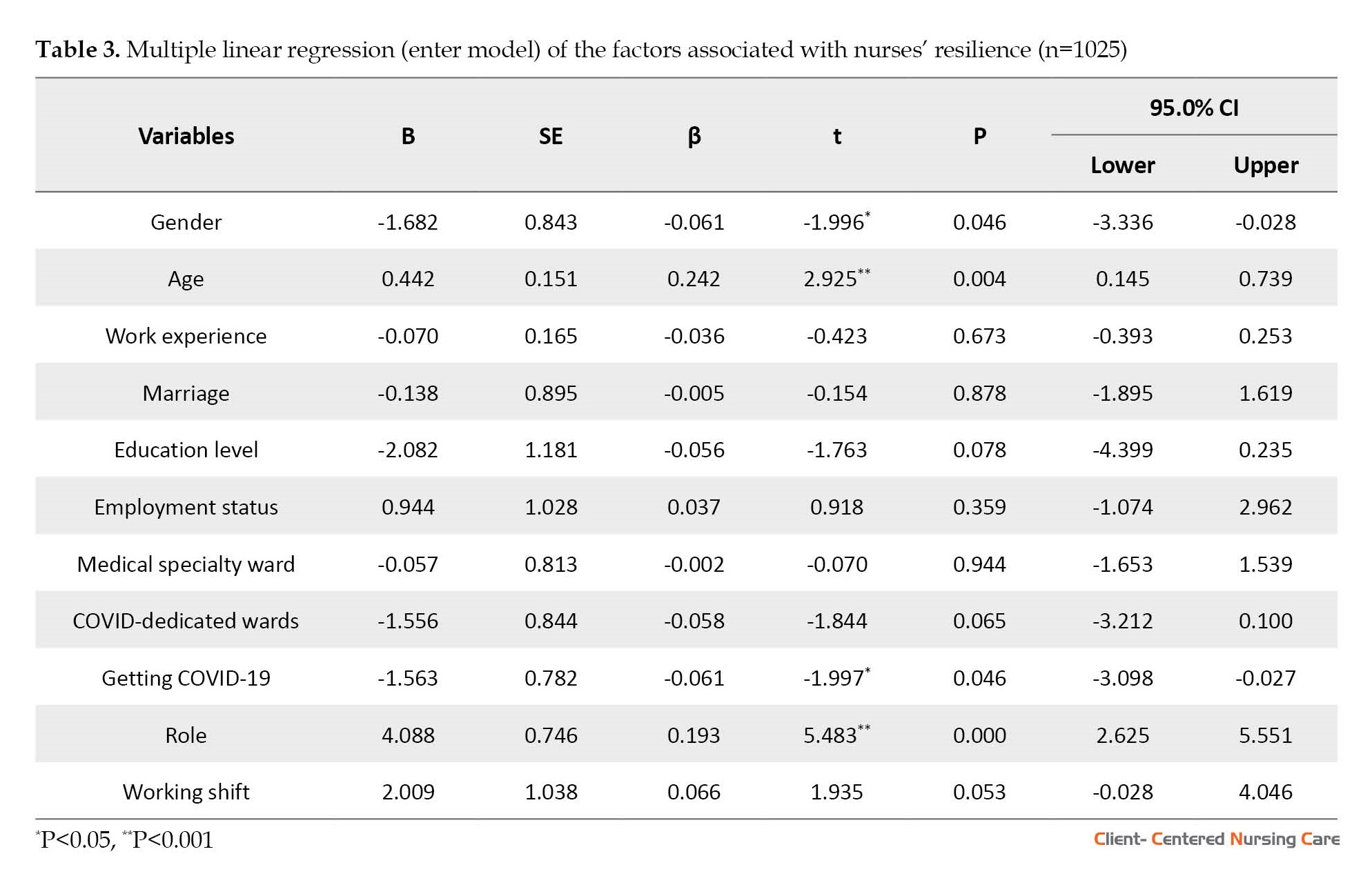
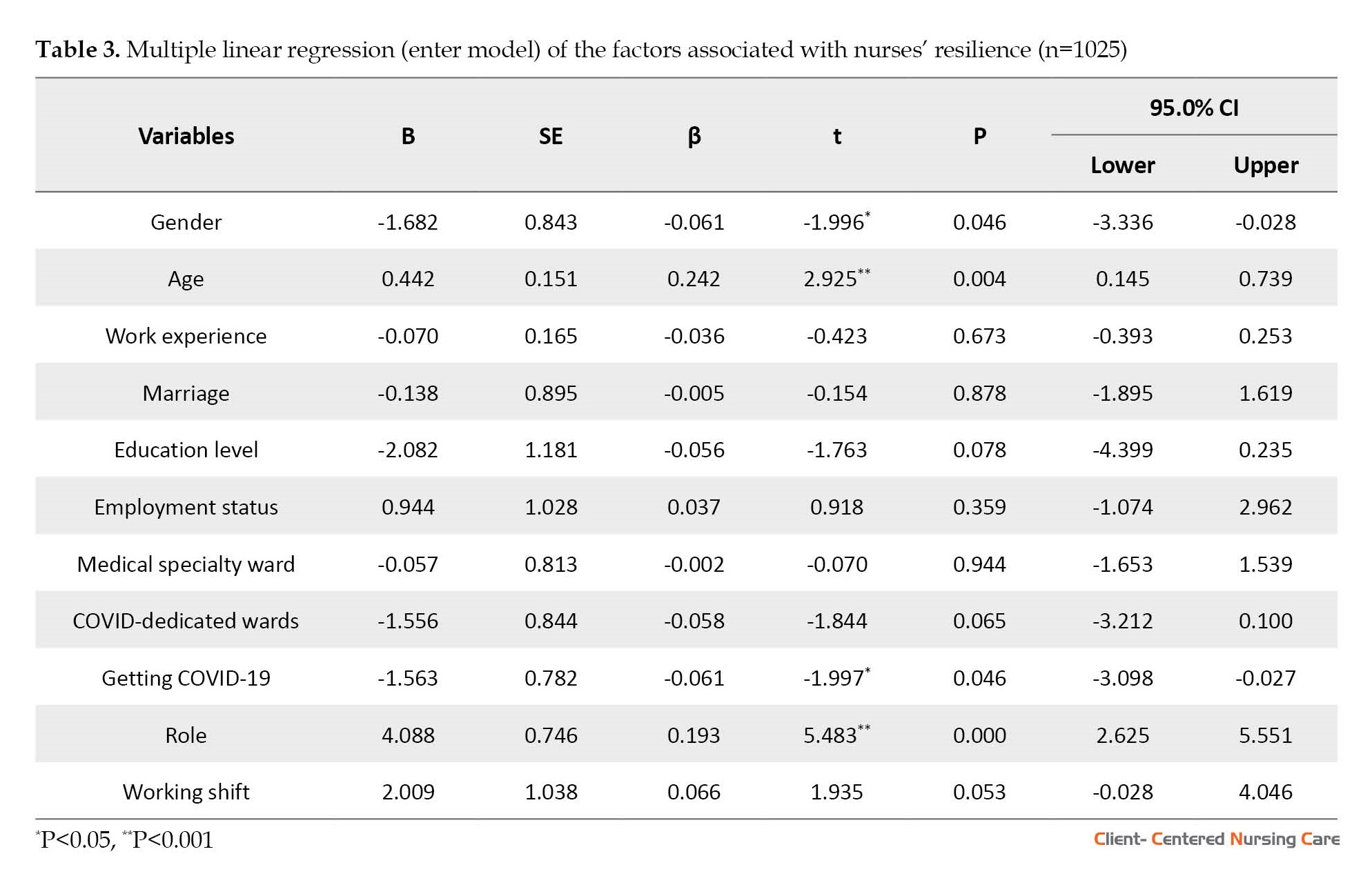
Eleven independent variables (age, gender, role, marital status, education level, work experience, employment status, type of ward, working in the COVID-19 ward, getting COVID-19, and working shift) were incorporated into the regression model with the resilience score as the dependent variable. According to multiple linear regression analysis, variables of age (β=0.242, P=0.004), gender (β=-0.061, P=0.046), role (β=0.193, P<0.001), and getting COVID-19 (β=-0.061, P=0.046) as independent variables could predict the nurses’ resilience. In other words, the resilience score of older nurses, male or in managerial positions who were not infected with COVID-19 during the pandemic, was higher than that of other nurses. Other personal and occupational variables failed to predict the nurses’ resilience (Table 3).
4. Discussion
In this study, the subjects’ overall resilience Mean±SD score was 68.95±12.76, and age, gender, role, and contracting COVID-19 were significant predictors of nurses’ resilience.
In the US general population, resilience averaged 80.4(12.8) (Connor & Davidson, 2003). Mean resilience scores were reported to be lower in Chinese, Japanese, Korean, and Iranian samples than in the general population of the US, although ethnicity and nationality have not been determining factors in the resilience of individuals in most studies (Khoshouei, 2009; Yu & Zhang, 2007). While most of these studies were conducted on the general population before the pandemic, the current study was conducted on a group of nurses with unique working circumstances during the COVID-19 pandemic. Thus, the stressful, exhausting, threatening, and unclear settings for nurses may be partly related to the variations in resilience scores between the general population and the nurses involved with the pandemic. A few studies have reported higher mean resilience of nurses (range: 75-82) (Gillespie et al., 2009; Tajanlangit, 2014). This discrepancy can be related to the usual conditions of nurses’ working environment before the COVID-19 pandemic. Since the present study has been carried out in the context of the COVID-19 pandemic, the resilience status of Iranian nurses seems to be relatively good.
Studies undertaken during the COVID-19 pandemic on the resiliency of nurses worldwide have frequently shown results comparable to those of the present study. Roberts et al. (2021) found that 65% of COVID-19-related respiratory disorders ward nurses scored moderate to high on the resilience scale (Roberts et al., 2021). Lin et al. (2020) examined the resilience-related factors in non-Chinese medical professionals during the COVID-19 pandemic and reported a Mean±SD resilience value of 67.03±13.22.
The multiple linear regression analysis identified just 4 variables (age, gender, contracting COVID-19, and role) out of 11 personal and occupational variables of nurses as effective predictors of nurse resilience. Male, older nurses, those in management roles, and those who did not get COVID-19 had significantly higher mean resilience scores than other nurses. Numerous studies have reported an association between age and resilience (Barzilay et al., 2020; Gillespie et al., 2009; Lisi et al., 2020; Luceño-Moreno et al., 2020). As healthcare workers age, they become more capable of handling crises. Professionals with more experience are more adept at handling bad events and appear to have greater psychological resilience (Bozdağ & Ergün, 2020). Younger workers have higher levels of posttraumatic stress and anxiety. This difference may be due to a lack of experience working in stressful environments (Luceño-Moreno et al., 2020). Sull et al. (2015) have shown that resilience increases with age and as employment ties strengthen. Another study also found that age groups and years of experience in nursing have significant associations with resilience (Ang et al., 2018).
Our study revealed that male nurses have greater resilience. This finding is comparable with the results of studies conducted in various countries around the world on HCPs, including nurses, during the COVID-19 pandemic (Barzilay et al., 2020; Bozdağ & Ergün, 2020; Huang et al., 2020c; Lisi et al., 2020; Luceño-Moreno et al., 2020). This issue can be traced to the differences between male and female responses to environmental pressures in the home and workplace.
A significant number of the nurses who participated in the study had COVID-19 within the previous 8 months. The mean resilience scores of these individuals were lower than those of other nurses. Given the immediate treatment in wards dedicated to COVID-19 patients and other wards not dedicated to COVID-19, nurses are experiencing extreme physical and psychological distress. They are at the forefront of the pandemic fight (Lai et al., 2020). Caring for COVID-19-infected patients exposes nurses to increased danger, and the likelihood of disease transmission to others and family members raises their anxiety and stress (Barzilay et al., 2020).
Also, in this study, nurses with managerial responsibilities, such as head nurses, supervisors, and matrons, showed greater resilience than nurses who provided direct care. Although both groups of nurses operated in the same work environment and faced relatively similar challenges during the pandemic, nurses with direct patient care responsibilities faced additional challenges, such as the risk of infection to themselves and their families, the stress caused by a lack of personal protective equipment, labor shortages, exposure to critically ill patients, and witnessing the death of patients. These factors could have more detrimental effects on their resilience. Numerous studies have demonstrated the impact of these variables on the mental health and resiliency of nurses and other HCPs during the COVID-19 pandemic (Barzilay et al., 2020; Huang et al., 2020c; Lai et al., 2020; Luceño-Moreno et al., 2020).
The mean resilience score of nurses with rotational shift work was lower than those with regular and fixed shifts. Although this factor was not detected as a predictor in the linear regression analysis, studies have shown that healthcare workers with rotational or irregular work schedules are more likely to develop psychological problems, and as a result, their resiliency may be compromised (Adams & Walls, 2020; Lee et al., 2017; Luceño-Moreno et al., 2020).
The COVID-19 pandemic spread rapidly and unexpectedly over most of the world, triggering a health crisis in industrialized and developing nations. The failure of countries to provide the essential human resources and equipment in a timely manner for the successful management of this crisis has caused several implications and challenges. As frontline actors in this crisis, HCPs endured greater pressure than others. Due to unfair economic sanctions, some countries, like Iran, were deprived of appropriate access to medical, laboratory, and pharmaceutical facilities and equipment to manage this crisis, resulting in greater damage than others.
This study was limited by its cross-sectional nature and co-occurrence with the country’s second wave of the COVID-19 outbreak. Thus, it may not accurately estimate the nurses’ true resilience. In addition, the study data were collected through social media platforms; hence, participants who were unfamiliar with or lacked access to these platforms were omitted. It is proposed that future studies address these limitations.
5. Conclusion
The current study indicated that the resilience status of Iranian nurses working in hospitals across the country is reasonably favorable. Female and younger nurses infected with COVID-19 are at greater risk.
Administrators and managers can use educational and supportive interventions to improve the resilience of healthcare workers, particularly young and female nurses, by offering organizational support resources, enhancing working conditions, and providing appropriate human resources.
Like other past crises, this crisis will have short- and long-term consequences that need further study. In the context of the psychological effects and consequences of the pandemic on people and healthcare personnel, longitudinal studies are required to evaluate how long this resilience will endure and be able to maintain mental health in the coming months and years.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Zanjan University of Medical Sciences (Code: IR.ZUMS.REC.1399.251). We explained the study objectives, the voluntary nature of participation, the confidentiality of their information, and the right to withdraw from the study for the participants. They provided verbal informed consent to participate in the study.
Funding
This article was extracted from MSc thesis of Fatemeh Aghamohammadi, approved by Department of Critical Care Nursing, Zanjan University of Medical Sciences and financially supported by Zanjan University of Medical Sciences.
Authors' contributions
Conceptualization, methodology, and data collection: Mohammadreza Dinmohammadi and Fatemeh Aghamohammadi; Writing, review, editing, funding acquisition, and resources: Mohammadreza Dinmohammadi; Data analysis and writing the original draft: Mohammadreza Dinmohammadi, Fatemeh Aghamohammadi, and Omid Saed; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate the participation of all nurses in this study.
References
Adams, J. G. & Walls, R. M., 2020. Supporting the health care workforce during the COVID-19 global epidemic. JAMA, 323(15), pp. 1439–40. [DOI:10.1001/jama.2020.3972] [PMID]
Ang, S. Y., et al., 2018. Association between demographics and resilience-a cross‐sectional study among nurses in Singapore. International Nursing Review, 65(3), pp. 459–66. [DOI:10.1111/inr.12441] [PMID]
Bao, Y., et al., 2020. 2019-nCoV epidemic: Address mental health care to empower society. Lancet, 395(10224), pp. e37–8.[DOI:10.1016/S0140-6736(20)30309-3] [PMID]
Barzilay, R., et al., 2020. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Translational Psychiatry, 10(1), pp. 291. [DOI:10.1038/s41398-020-00982-4] [PMID] [PMCID]
Bozdağ, F. & Ergün, N., 2021. Psychological resilience of healthcare professionals during COVID-19 pandemic. Psychological Reports, 124(6), pp. 2567–86. [DOI:10.1177/0033294120965477] [PMID] [PMCID]
Connor, K. M. & Davidson, J. R., 2003. Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), pp. 76–82. [DOI:10.1002/da.10113] [PMID]
Dinmohammadi, M., et al., 2022. Factors contributing to coronavirus disease 2019 vaccine hesitancy among healthcare workers in Iran: A descriptive-analytical study. Clinical Epidemiology and Global Health, 18, pp. 101182. [DOI:10.1016/j.cegh.2022.101182] [PMID] [PMCID]
Foster, K., et al., 2019. Resilience and mental health nursing: An integrative review of international literature. International Journal of Mental Health Nursing, 28, pp. 71-85. [DOI:10.1111/inm.12548] [PMID]
Gillespie, B. M., Chaboyer, W. & Wallis, M., 2009. The influence of personal characteristics on the resilience of operating room nurses: A predictor study. International Journal of Nursing Studies, 46(7), pp. 968–76. [DOI:10.1016/j.ijnurstu.2007.08.006] [PMID]
Greenberg, N., et al., 2020. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ, 368, pp. m1211. [DOI:10.1136/bmj.m1211] [PMID]
Hasanzadeh F, Aghajanloo, A. & Dinmohammadi M., 2022. [Factors affecting the acceptance of personal protection measures among patients before having COVID-19 (Persian)]. Journal of Payavard Salamat, 16(4), pp. 286-95. [Link]
Huang, J., et al., 2020. Care for the psychological status of frontline medical staff fighting against coronavirus disease 2019 (COVID-19). Clinical Infectious Diseases, 71(12), pp. 3268–9. [DOI:10.1093/cid/ciaa385] [PMID] [PMCID]
Huang, J. Z., et al., 2020. [Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19 (Chinese)]. Chinese Journal of Industrial Hygiene and Occupational Diseases, 38(3), pp. 192–5. [PMID]
Huang, L., et al., 2020. Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 novel coronavirus disease (COVID-19): A cross-sectional study. Medical Science Monitor, 26, pp. e925669. [DOI:10.12659/MSM.925669] [PMID] [PMCID]
Iflaifel, M., et al., 2020. Resilient health care: A systematic review of conceptualisations, study methods and factors that develop resilience. BMC Health Services Research, 20(1), pp. 324.[DOI:10.1186/s12913-020-05208-3] [PMID] [PMCID]
Khoshouei, M. S., 2009. Psychometric evaluation of the Connor-Davidson resilience scale (CD-RISC) using Iranian students. International Journal of Testing, 9(1), pp. 60-6.[DOI:10.1080/15305050902733471]
Kluge, H., 2020. Statement-physical and mental health key to resilience during COVID-19 pandemic. Geneva: World Health Organization. [Link]
Lai, J., et al., 2020. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), pp. e203976.[DOI:10.1001/jamanetworkopen.2020.3976] [PMID] [PMCID]
Lee, A., et al., 2017. Night shift work and risk of depression: Meta-analysis of observational studies. Journal of Korean Medical Science, 32(7), pp. 1091–6. [DOI:10.3346/jkms.2017.32.7.1091] [PMID] [PMCID]
Lin, J., et al., 2020. Factors associated with resilience among non-local medical workers sent to Wuhan, China during the COVID-19 outbreak. BMC Psychiatry, 20(1), pp. 417. [DOI:10.1186/s12888-020-02821-8] [PMID] [PMCID]
Lisi, L., et al., 2020. Levels and factors associated with resilience in italian healthcare professionals during the COVID-19 pandemic: A web-based survey. Behavioral Sciences, 10(12), pp. 183. [DOI:10.3390/bs10120183] [PMID] [PMCID]
Luceño-Moreno, L., et al., 2020. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in spanish health personnel during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 17(15), pp. 5514. [DOI:10.3390/ijerph17155514] [PMID] [PMCID]
Lupe, S. E., Keefer, L. & Szigethy, E., 2020. Gaining resilience and reducing stress in the age of COVID-19. Current Opinion in Gastroenterology, 36(4), pp. 295–303. [DOI:10.1097/MOG.0000000000000646] [PMID]
Pappa, S., et al., 2020. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 88, pp. 901-7. [DOI:10.1016/j.bbi.2020.05.026] [PMID] [PMCID]
Polizzi, C., Lynn, S. J. & Perry, A., 2020. Stress and coping in the time of COVID-19: Pathways to resilience and recovery. Clinical Neuropsychiatry, 17(2), pp. 59–62. [PMID]
Pothiawala, S., 2020. Psychological impact of the COVID-19 on health care workers in the emergency department. Frontiers in Emergency Medicine, 4(2s), pp. e58. [Link]
Roberts, N. J., et al., 2021. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respiratory Medicine, 176, pp. 106219. [DOI:10.1016/j.rmed.2020.106219] [PMID] [PMCID]
Samani, S., Jokar, B. & Sahragard, N., 2007. [Effects of resilience on mental health and life satisfaction (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology, 13 (3), pp. 290-5. [Link]
Sood, S., 2020. Psychological effects of the Coronavirus disease-2019 pandemic. Research and Humanities in Medical Education, 7, pp. 23–26. [Link]
Southwick, S. M., et al., 2014. Resilience definitions, theory, and challenges: interdisciplinary perspectives. European Journal of Psychotraumatology, 5, pp. 10.3402/ejpt.v5.25338. [DOI:10.3402/ejpt.v5.25338] [PMID] [PMCID]
Sull, A., Harland, N. & Moore, A., 2015. Resilience of healthcare workers in the UK; A cross-sectional survey. Journal of Occupational Medicine and Toxicology, 10, pp. 20. [DOI:10.1186/s12995-015-0061-x] [PMID] [PMCID]
Tajanlangit, A. L. N., 2014. Demographics, resilience, ethical climate, and burnout among selected Filipino mental health nurses. Manila: University of Santo Tomas Graduate School. [Link]
Takian, A., Raoofi, A. & Kazempour-Ardebili, S., 2020. COVID-19 battle during the toughest sanctions against Iran. Lancet, 395(10229), pp. 1035–6. [DOI:10.1016/S0140-6736(20)30668-1] [PMID]
Wu, P., et al., 2009. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 54(5), pp. 302–11. [DOI:10.1177/070674370905400504] [PMID] [PMCID]
Xiang, Y. T., et al., 2020. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry, 7(3), pp. 228–9. [DOI:10.1016/S2215-0366(20)30046-8] [PMID]
Yu, X. & Zhang, J., 2007. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behavior and Personality: An International Journal, 35(1), pp. 19-30. [DOI:10.2224/sbp.2007.35.1.19]
Zhou, P., et al., 2020. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), pp. 270–3. [DOI:10.1038/s41586-020-2012-7] [PMID] [PMCID]
Zhu, H., Wei, L. & Niu, P., 2020. The novel coronavirus outbreak in Wuhan, China. Global Health Research and Policy, 5, pp. 6. [DOI:10.1186/s41256-020-00135-6] [PMID] [PMCID]
In December 2019, a viral outbreak was reported in Wuhan, China. This disease was caused by a newly created and genetically modified coronavirus called SARS-CoV2, also known as COVID-19 (Zhu, Wei &Niu, 2020). The World Health Organization (WHO) announced the outbreak of a novel coronavirus in January 2020 and declared it an epidemic and public health concern in March 2020 (Zhou et al., 2020; Hasanzadeh et al., 2022).
Healthcare providers (HCWs) are regarded as the first to be exposed to the COVID-19 virus, leading the fight against the disease (Bao et al., 2020; Sood, 2020; Dinmohammadi et al., 2022). The prevalence of psychological disorders among healthcare personnel during pandemics has ranged between 50% and 75% (Lai et al., 2020; Pothiawala, 2020; Wu et al., 2009).
At the onset of the pandemic, the initial focus was on discovering new cases and preventing the spread of the disease, and its psychological effects were given less consideration (Xiang et al., 2020). The first studies on the psychological performance of humans in the face of a pandemic were undertaken by Chinese researchers (Lai et al., 2020). Direct interaction with COVID-19-infected patients exposes nurses to more traumatic situations, such as witnessing their suffering and death, heightening their fear and anxiety (Pappa et al., 2020). There has been a rise in posttraumatic stress disorder, anxiety, and insomnia among healthcare workers and patients (Bozdağ & Ergün, 2020). The prevalence of anxiety among healthcare professionals (HCPs) ranges from 22.6% to 36.3%. This rate is much higher than the general population’s rate of anxiety (Huang et al., 2020c). As a result, maintaining the mental health of frontline actors will become a critical global health concern in the months and possibly years to come (Kluge, 2020).
Promoting resilience among healthcare workers and organizations starts with understanding what resilience is (and is not). Historical psychology and the social sciences have conceptualized resilience as a trait (e.g. hardiness), a process (e.g. adaptation), or an outcome (e.g. the absence of posttraumatic stress or the presence of posttraumatic growth after particular adversity). Modern psychology and social science define resilience as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress” (Southwick et al., 2014). Resilience can play an adaptive role in alleviating stress and anxiety brought on by the COVID-19 crisis (Lupe et al., 2020; Polizzi et al., 2020).
Earlier studies have shown that nurses and other HCPs experience profound challenges during the recent pandemic, which may have affected their physical and emotional health and, subsequently, their professional performance (Foster et al., 2019). Due to the COVID-19 outbreak, HCPs must work under the most challenging circumstances (Greenberg et al., 2020). If HCPs and nurses lack the necessary resilience, not only will they be unable to recover, but the cumulative effects of negative emotions may also lead to psychological disorders (Huang et al., 2020b). To survive the COVID-19 pandemic, it is essential to support healthcare professionals’ mental health and resilience, particularly nurses (Huang et al., 2020a).
Also, it has been demonstrated that personal (e.g. gender, age, marital status), occupational (e.g. experience, working shift, employment status), and personality characteristics (e.g. optimism, perseverance, and cooperation) contribute to the development of resilience in HCPs (Iflaifel et al., 2020; Lisi et al., 2020).
Access to key medical, laboratory, and pharmaceutical equipment for hospitalized patient care has become significantly more difficult and unbearable due to the persistence of harsh sanctions against Iran. Unlike other countries, these issues may jeopardize Iranian nurses’ mental health and resilience (Takian et al., 2020). There is limited data available on the resilience of Iranian nurses and its determinants, particularly in light of the recent pandemic. This study aimed to identify the factors affecting Iranian nurses’ resilience in hospitals nationwide.
2. Materials and Methods
This cross-sectional web-based survey was conducted using the Google Forms platform during the pandemic. The Iranian nurses working in public and private hospitals were invited to participate in the survey via social networks like Telegram and WhatsApp. The inclusion criteria were willingness to participate in the study, a bachelor’s degree or higher in nursing, and at least 6 months of active employment. Incomplete surveys were the exclusion criterion.
The information was gathered from November 7 to November 29, 2020, using an online questionnaire. Participants had a maximum of 10 minutes to complete the questionnaires and were required to answer all the questions. Each individual was only permitted to complete the questionnaire once. To increase the response rate, reminder messages were sent to nurses’ social networks through the network administrator during the study course. A total of 1045 questionnaires were submitted by nurses who participated in the study. Twenty instances of surveys with missing information were omitted from the analysis. In the end, 1025 questionnaires were examined.
The study instrument was a two-part online questionnaire, with the first part pertaining to individual and occupational factors (age, gender, role, marital status, education level, work experience, employment status, type of ward, working in the COVID-19 ward, getting COVID-19, and working shift), and the second part comprising the 25-item Connor-Davidson resilience scale (CD-RISC). The questionnaire is rated on a 5-point Likert scale (completely incorrect=0 to completely correct=4). The minimum and maximum scores on this scale are 0 and 100, respectively, and higher scores indicate greater resilience (Connor & Davidson, 2003). The Persian version of this scale has been psychometrically tested, and its validity and reliability have been confirmed (Khoshouei, 2009; Samani et al., 2007). In this study, the Cronbach α reliability of the instrument was determined to be 0.87.
Data analysis
The frequency, Mean±SD were the indicators to describe the personal and occupational characteristics of the nurses. The distribution of data related to resilience was normal. The multiple linear regression (enter model) was used to investigate the influence of personal and occupational factors in predicting the nurses’ resilience. The assumptions of multiple linear regression analysis were established. The data were analyzed using SPSS software, version 22. The significance level was P<0.05.
3. Results
Among the 1045 surveys received, 1025 were valid and analyzable. The Mean±SD age of the nurses was 33.79±6.98 years, and their work experience was 9.61±6.62 years (Table 1).
The nurses’ total Mean±SD resilience score was 68.95±12.76. According to the results of the t-test for independent groups, nurses who were married (P<0.001), permanently employed (P=0.004), and not infected with COVID-19 (P=0.024) were more resilient than others. Also, nurses in managerial roles (P<0.001) were more resilient than clinical nurses. Other variables were not significant (Table 2).
Eleven independent variables (age, gender, role, marital status, education level, work experience, employment status, type of ward, working in the COVID-19 ward, getting COVID-19, and working shift) were incorporated into the regression model with the resilience score as the dependent variable. According to multiple linear regression analysis, variables of age (β=0.242, P=0.004), gender (β=-0.061, P=0.046), role (β=0.193, P<0.001), and getting COVID-19 (β=-0.061, P=0.046) as independent variables could predict the nurses’ resilience. In other words, the resilience score of older nurses, male or in managerial positions who were not infected with COVID-19 during the pandemic, was higher than that of other nurses. Other personal and occupational variables failed to predict the nurses’ resilience (Table 3).
4. Discussion
In this study, the subjects’ overall resilience Mean±SD score was 68.95±12.76, and age, gender, role, and contracting COVID-19 were significant predictors of nurses’ resilience.
In the US general population, resilience averaged 80.4(12.8) (Connor & Davidson, 2003). Mean resilience scores were reported to be lower in Chinese, Japanese, Korean, and Iranian samples than in the general population of the US, although ethnicity and nationality have not been determining factors in the resilience of individuals in most studies (Khoshouei, 2009; Yu & Zhang, 2007). While most of these studies were conducted on the general population before the pandemic, the current study was conducted on a group of nurses with unique working circumstances during the COVID-19 pandemic. Thus, the stressful, exhausting, threatening, and unclear settings for nurses may be partly related to the variations in resilience scores between the general population and the nurses involved with the pandemic. A few studies have reported higher mean resilience of nurses (range: 75-82) (Gillespie et al., 2009; Tajanlangit, 2014). This discrepancy can be related to the usual conditions of nurses’ working environment before the COVID-19 pandemic. Since the present study has been carried out in the context of the COVID-19 pandemic, the resilience status of Iranian nurses seems to be relatively good.
Studies undertaken during the COVID-19 pandemic on the resiliency of nurses worldwide have frequently shown results comparable to those of the present study. Roberts et al. (2021) found that 65% of COVID-19-related respiratory disorders ward nurses scored moderate to high on the resilience scale (Roberts et al., 2021). Lin et al. (2020) examined the resilience-related factors in non-Chinese medical professionals during the COVID-19 pandemic and reported a Mean±SD resilience value of 67.03±13.22.
The multiple linear regression analysis identified just 4 variables (age, gender, contracting COVID-19, and role) out of 11 personal and occupational variables of nurses as effective predictors of nurse resilience. Male, older nurses, those in management roles, and those who did not get COVID-19 had significantly higher mean resilience scores than other nurses. Numerous studies have reported an association between age and resilience (Barzilay et al., 2020; Gillespie et al., 2009; Lisi et al., 2020; Luceño-Moreno et al., 2020). As healthcare workers age, they become more capable of handling crises. Professionals with more experience are more adept at handling bad events and appear to have greater psychological resilience (Bozdağ & Ergün, 2020). Younger workers have higher levels of posttraumatic stress and anxiety. This difference may be due to a lack of experience working in stressful environments (Luceño-Moreno et al., 2020). Sull et al. (2015) have shown that resilience increases with age and as employment ties strengthen. Another study also found that age groups and years of experience in nursing have significant associations with resilience (Ang et al., 2018).
Our study revealed that male nurses have greater resilience. This finding is comparable with the results of studies conducted in various countries around the world on HCPs, including nurses, during the COVID-19 pandemic (Barzilay et al., 2020; Bozdağ & Ergün, 2020; Huang et al., 2020c; Lisi et al., 2020; Luceño-Moreno et al., 2020). This issue can be traced to the differences between male and female responses to environmental pressures in the home and workplace.
A significant number of the nurses who participated in the study had COVID-19 within the previous 8 months. The mean resilience scores of these individuals were lower than those of other nurses. Given the immediate treatment in wards dedicated to COVID-19 patients and other wards not dedicated to COVID-19, nurses are experiencing extreme physical and psychological distress. They are at the forefront of the pandemic fight (Lai et al., 2020). Caring for COVID-19-infected patients exposes nurses to increased danger, and the likelihood of disease transmission to others and family members raises their anxiety and stress (Barzilay et al., 2020).
Also, in this study, nurses with managerial responsibilities, such as head nurses, supervisors, and matrons, showed greater resilience than nurses who provided direct care. Although both groups of nurses operated in the same work environment and faced relatively similar challenges during the pandemic, nurses with direct patient care responsibilities faced additional challenges, such as the risk of infection to themselves and their families, the stress caused by a lack of personal protective equipment, labor shortages, exposure to critically ill patients, and witnessing the death of patients. These factors could have more detrimental effects on their resilience. Numerous studies have demonstrated the impact of these variables on the mental health and resiliency of nurses and other HCPs during the COVID-19 pandemic (Barzilay et al., 2020; Huang et al., 2020c; Lai et al., 2020; Luceño-Moreno et al., 2020).
The mean resilience score of nurses with rotational shift work was lower than those with regular and fixed shifts. Although this factor was not detected as a predictor in the linear regression analysis, studies have shown that healthcare workers with rotational or irregular work schedules are more likely to develop psychological problems, and as a result, their resiliency may be compromised (Adams & Walls, 2020; Lee et al., 2017; Luceño-Moreno et al., 2020).
The COVID-19 pandemic spread rapidly and unexpectedly over most of the world, triggering a health crisis in industrialized and developing nations. The failure of countries to provide the essential human resources and equipment in a timely manner for the successful management of this crisis has caused several implications and challenges. As frontline actors in this crisis, HCPs endured greater pressure than others. Due to unfair economic sanctions, some countries, like Iran, were deprived of appropriate access to medical, laboratory, and pharmaceutical facilities and equipment to manage this crisis, resulting in greater damage than others.
This study was limited by its cross-sectional nature and co-occurrence with the country’s second wave of the COVID-19 outbreak. Thus, it may not accurately estimate the nurses’ true resilience. In addition, the study data were collected through social media platforms; hence, participants who were unfamiliar with or lacked access to these platforms were omitted. It is proposed that future studies address these limitations.
5. Conclusion
The current study indicated that the resilience status of Iranian nurses working in hospitals across the country is reasonably favorable. Female and younger nurses infected with COVID-19 are at greater risk.
Administrators and managers can use educational and supportive interventions to improve the resilience of healthcare workers, particularly young and female nurses, by offering organizational support resources, enhancing working conditions, and providing appropriate human resources.
Like other past crises, this crisis will have short- and long-term consequences that need further study. In the context of the psychological effects and consequences of the pandemic on people and healthcare personnel, longitudinal studies are required to evaluate how long this resilience will endure and be able to maintain mental health in the coming months and years.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Zanjan University of Medical Sciences (Code: IR.ZUMS.REC.1399.251). We explained the study objectives, the voluntary nature of participation, the confidentiality of their information, and the right to withdraw from the study for the participants. They provided verbal informed consent to participate in the study.
Funding
This article was extracted from MSc thesis of Fatemeh Aghamohammadi, approved by Department of Critical Care Nursing, Zanjan University of Medical Sciences and financially supported by Zanjan University of Medical Sciences.
Authors' contributions
Conceptualization, methodology, and data collection: Mohammadreza Dinmohammadi and Fatemeh Aghamohammadi; Writing, review, editing, funding acquisition, and resources: Mohammadreza Dinmohammadi; Data analysis and writing the original draft: Mohammadreza Dinmohammadi, Fatemeh Aghamohammadi, and Omid Saed; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate the participation of all nurses in this study.
References
Adams, J. G. & Walls, R. M., 2020. Supporting the health care workforce during the COVID-19 global epidemic. JAMA, 323(15), pp. 1439–40. [DOI:10.1001/jama.2020.3972] [PMID]
Ang, S. Y., et al., 2018. Association between demographics and resilience-a cross‐sectional study among nurses in Singapore. International Nursing Review, 65(3), pp. 459–66. [DOI:10.1111/inr.12441] [PMID]
Bao, Y., et al., 2020. 2019-nCoV epidemic: Address mental health care to empower society. Lancet, 395(10224), pp. e37–8.[DOI:10.1016/S0140-6736(20)30309-3] [PMID]
Barzilay, R., et al., 2020. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Translational Psychiatry, 10(1), pp. 291. [DOI:10.1038/s41398-020-00982-4] [PMID] [PMCID]
Bozdağ, F. & Ergün, N., 2021. Psychological resilience of healthcare professionals during COVID-19 pandemic. Psychological Reports, 124(6), pp. 2567–86. [DOI:10.1177/0033294120965477] [PMID] [PMCID]
Connor, K. M. & Davidson, J. R., 2003. Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), pp. 76–82. [DOI:10.1002/da.10113] [PMID]
Dinmohammadi, M., et al., 2022. Factors contributing to coronavirus disease 2019 vaccine hesitancy among healthcare workers in Iran: A descriptive-analytical study. Clinical Epidemiology and Global Health, 18, pp. 101182. [DOI:10.1016/j.cegh.2022.101182] [PMID] [PMCID]
Foster, K., et al., 2019. Resilience and mental health nursing: An integrative review of international literature. International Journal of Mental Health Nursing, 28, pp. 71-85. [DOI:10.1111/inm.12548] [PMID]
Gillespie, B. M., Chaboyer, W. & Wallis, M., 2009. The influence of personal characteristics on the resilience of operating room nurses: A predictor study. International Journal of Nursing Studies, 46(7), pp. 968–76. [DOI:10.1016/j.ijnurstu.2007.08.006] [PMID]
Greenberg, N., et al., 2020. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ, 368, pp. m1211. [DOI:10.1136/bmj.m1211] [PMID]
Hasanzadeh F, Aghajanloo, A. & Dinmohammadi M., 2022. [Factors affecting the acceptance of personal protection measures among patients before having COVID-19 (Persian)]. Journal of Payavard Salamat, 16(4), pp. 286-95. [Link]
Huang, J., et al., 2020. Care for the psychological status of frontline medical staff fighting against coronavirus disease 2019 (COVID-19). Clinical Infectious Diseases, 71(12), pp. 3268–9. [DOI:10.1093/cid/ciaa385] [PMID] [PMCID]
Huang, J. Z., et al., 2020. [Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19 (Chinese)]. Chinese Journal of Industrial Hygiene and Occupational Diseases, 38(3), pp. 192–5. [PMID]
Huang, L., et al., 2020. Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 novel coronavirus disease (COVID-19): A cross-sectional study. Medical Science Monitor, 26, pp. e925669. [DOI:10.12659/MSM.925669] [PMID] [PMCID]
Iflaifel, M., et al., 2020. Resilient health care: A systematic review of conceptualisations, study methods and factors that develop resilience. BMC Health Services Research, 20(1), pp. 324.[DOI:10.1186/s12913-020-05208-3] [PMID] [PMCID]
Khoshouei, M. S., 2009. Psychometric evaluation of the Connor-Davidson resilience scale (CD-RISC) using Iranian students. International Journal of Testing, 9(1), pp. 60-6.[DOI:10.1080/15305050902733471]
Kluge, H., 2020. Statement-physical and mental health key to resilience during COVID-19 pandemic. Geneva: World Health Organization. [Link]
Lai, J., et al., 2020. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), pp. e203976.[DOI:10.1001/jamanetworkopen.2020.3976] [PMID] [PMCID]
Lee, A., et al., 2017. Night shift work and risk of depression: Meta-analysis of observational studies. Journal of Korean Medical Science, 32(7), pp. 1091–6. [DOI:10.3346/jkms.2017.32.7.1091] [PMID] [PMCID]
Lin, J., et al., 2020. Factors associated with resilience among non-local medical workers sent to Wuhan, China during the COVID-19 outbreak. BMC Psychiatry, 20(1), pp. 417. [DOI:10.1186/s12888-020-02821-8] [PMID] [PMCID]
Lisi, L., et al., 2020. Levels and factors associated with resilience in italian healthcare professionals during the COVID-19 pandemic: A web-based survey. Behavioral Sciences, 10(12), pp. 183. [DOI:10.3390/bs10120183] [PMID] [PMCID]
Luceño-Moreno, L., et al., 2020. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in spanish health personnel during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 17(15), pp. 5514. [DOI:10.3390/ijerph17155514] [PMID] [PMCID]
Lupe, S. E., Keefer, L. & Szigethy, E., 2020. Gaining resilience and reducing stress in the age of COVID-19. Current Opinion in Gastroenterology, 36(4), pp. 295–303. [DOI:10.1097/MOG.0000000000000646] [PMID]
Pappa, S., et al., 2020. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 88, pp. 901-7. [DOI:10.1016/j.bbi.2020.05.026] [PMID] [PMCID]
Polizzi, C., Lynn, S. J. & Perry, A., 2020. Stress and coping in the time of COVID-19: Pathways to resilience and recovery. Clinical Neuropsychiatry, 17(2), pp. 59–62. [PMID]
Pothiawala, S., 2020. Psychological impact of the COVID-19 on health care workers in the emergency department. Frontiers in Emergency Medicine, 4(2s), pp. e58. [Link]
Roberts, N. J., et al., 2021. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respiratory Medicine, 176, pp. 106219. [DOI:10.1016/j.rmed.2020.106219] [PMID] [PMCID]
Samani, S., Jokar, B. & Sahragard, N., 2007. [Effects of resilience on mental health and life satisfaction (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology, 13 (3), pp. 290-5. [Link]
Sood, S., 2020. Psychological effects of the Coronavirus disease-2019 pandemic. Research and Humanities in Medical Education, 7, pp. 23–26. [Link]
Southwick, S. M., et al., 2014. Resilience definitions, theory, and challenges: interdisciplinary perspectives. European Journal of Psychotraumatology, 5, pp. 10.3402/ejpt.v5.25338. [DOI:10.3402/ejpt.v5.25338] [PMID] [PMCID]
Sull, A., Harland, N. & Moore, A., 2015. Resilience of healthcare workers in the UK; A cross-sectional survey. Journal of Occupational Medicine and Toxicology, 10, pp. 20. [DOI:10.1186/s12995-015-0061-x] [PMID] [PMCID]
Tajanlangit, A. L. N., 2014. Demographics, resilience, ethical climate, and burnout among selected Filipino mental health nurses. Manila: University of Santo Tomas Graduate School. [Link]
Takian, A., Raoofi, A. & Kazempour-Ardebili, S., 2020. COVID-19 battle during the toughest sanctions against Iran. Lancet, 395(10229), pp. 1035–6. [DOI:10.1016/S0140-6736(20)30668-1] [PMID]
Wu, P., et al., 2009. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 54(5), pp. 302–11. [DOI:10.1177/070674370905400504] [PMID] [PMCID]
Xiang, Y. T., et al., 2020. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry, 7(3), pp. 228–9. [DOI:10.1016/S2215-0366(20)30046-8] [PMID]
Yu, X. & Zhang, J., 2007. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behavior and Personality: An International Journal, 35(1), pp. 19-30. [DOI:10.2224/sbp.2007.35.1.19]
Zhou, P., et al., 2020. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), pp. 270–3. [DOI:10.1038/s41586-020-2012-7] [PMID] [PMCID]
Zhu, H., Wei, L. & Niu, P., 2020. The novel coronavirus outbreak in Wuhan, China. Global Health Research and Policy, 5, pp. 6. [DOI:10.1186/s41256-020-00135-6] [PMID] [PMCID]
Type of Study: Research |
Subject:
General
Received: 2023/01/5 | Accepted: 2023/04/17 | Published: 2023/08/24
Received: 2023/01/5 | Accepted: 2023/04/17 | Published: 2023/08/24
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






