Tue, Jan 27, 2026
[Archive]
Volume 9, Issue 3 (Summer 2023)
JCCNC 2023, 9(3): 171-182 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Siagian H, Rusmimpong R, Sukurni S, Arimaswati A, Alifariki L O. Dysphagia Improvement Using Acupuncture Therapy: A Systematic Review. JCCNC 2023; 9 (3) :171-182
URL: http://jccnc.iums.ac.ir/article-1-455-en.html
URL: http://jccnc.iums.ac.ir/article-1-455-en.html
Heriviyatno.J Siagian1 

 , Rusmimpong Rusmimpong2
, Rusmimpong Rusmimpong2 

 , Sukurni Sukurni3
, Sukurni Sukurni3 

 , Arimaswati Arimaswati *4
, Arimaswati Arimaswati *4 

 , La Ode Alifariki5
, La Ode Alifariki5 




 , Rusmimpong Rusmimpong2
, Rusmimpong Rusmimpong2 

 , Sukurni Sukurni3
, Sukurni Sukurni3 

 , Arimaswati Arimaswati *4
, Arimaswati Arimaswati *4 

 , La Ode Alifariki5
, La Ode Alifariki5 


1- Medical Surgical Nursing Department, College of Science and Technology, Sembilanbelas November University, Kolaka, Indonesia.
2- Health Polytechnic of Jambi, Jambi, Indonesia.
3- Department of Nursing, Faculty of Medical, Haluoleo University, Kendari, Indonesia.
4- Department of Medical, Faculty of Medical, Haluoleo University, Kendari, Indonesia. ,arimaswati.uho@gmail.com
5- Department of Epidemiology, Faculty of Medical, Haluoleo University, Kendari, Indonesia.
2- Health Polytechnic of Jambi, Jambi, Indonesia.
3- Department of Nursing, Faculty of Medical, Haluoleo University, Kendari, Indonesia.
4- Department of Medical, Faculty of Medical, Haluoleo University, Kendari, Indonesia. ,
5- Department of Epidemiology, Faculty of Medical, Haluoleo University, Kendari, Indonesia.
Full-Text [PDF 1148 kb]
(1190 Downloads)
| Abstract (HTML) (2418 Views)
Full-Text: (853 Views)
1. Introduction
Dysphagia is prevalent in stroke survivors, with an incidence rate of 8.1% to 80%. Dysphagia was reported in 36.3% of post-stroke patients in Asia (Meng et al., 2020). Dysphagia worsens when swallowing liquids (Lancaster, 2015), causing major problems such as aspiration, pneumonia, and even death (Calandra-Buonaura et al., 2021; Waters et al., 2022). Furthermore, dysphagia is associated with social anxiety, withdrawal, and depression (MacDonald et al., 2018; Olesen et al., 2021). It may also impact daily activities, quality of life, and stroke prognosis. Repetitive transcranial magnetic stimulation, swallowing training (Huang et al., 2014; Wen et al., 2022), transcutaneous and retropharyngeal electrical stimulation, non-invasive brain stimulation strategies, transcranial direct current stimulation (Marin et al., 2018), speech and language therapy (Brady et al., 2016), expiratory muscle strength training (Guillén-Solà et al., 2017; Park et al., 2016a), behavioral interventions (Speyer et al., 2022), dietary modification (Teuschl et al., 2018), and neuromuscular electrical stimulation (Chen et al., 2016; Park et al., 2016b). As a result, managing patients with post-stroke dysphagia requires a multidisciplinary approach (Song et al., 2015; Park et al., 2016b).
Acupuncture is a traditional Chinese medicine procedure in which acupuncturists insert needles through the skin to balance life energy, known as “qi.” Over the past 1000 years, China has used acupuncture for stroke rehabilitation. Even the World Health Organization (WHO) has acknowledged acupunctures as an alternative and complementary technique for stroke therapy and care (Chavez et al., 2017). Traditional manual acupuncture (TA), electroacupuncture (EA) (Lim et al., 2014; Yu et al., 2018), moxibustion acupuncture (MA), and scalp acupuncture (SA) are available modes for treating dysphagia following a stroke (Zhang et al., 2014). A series of trials in humans and investigations in animals have revealed that the acupuncture mechanism for stroke primarily includes neurotransmitter release regulation, cerebral microcirculation regulation, anti-apoptosis, stimulation of neurogenesis and cell proliferation, and neuroplasticity regulation (Belskaya et al., 2020; Li & Wang, 2013).
Acupuncture’s physiological influence on dysphagia after stroke has not been well researched. Previous studies show that acupuncture affects regional brain activity (Deng et al., 2016; Jia et al., 2015; Demao et al., 2016; Feng et al., 2016; Meng et al., 2016; Yu et al., 2018). Furthermore, acupuncture can aid in repairing and reconstructing swallowing function by forming new synaptic connections and hastening the restoration and reconstruction of the swallowing reflex arc (Li et al., 2018; Wu et al., 2019). Given the possible benefits of acupuncture for treating dysphagia after stroke, its use in dysphagia intervention has grown in popularity in China and worldwide.
According to a previous systematic review, acupuncture can lessen clinical symptoms such as trouble swallowing and lower the prevalence of dysphagia (Geeganage et al., 2012). It can also enhance patients’ quality of life. Acupuncture has been included in the most recent Cochrane study on swallowing therapy, although it did not significantly affect the outcomes of dependency/disability, misaspiration rate, or death (Bath et al., 2018).
Acupuncture research for dysphagia or swallowing disorders has risen, although the outcomes have been inconsistent (Chan et al., 2012; Feng et al., 2016; Xia et al., 2016; Chan et al., 2020). In a few systematic reviews, acupuncture has been utilized to treat dysphagia in stroke patients (Cai et al., 2015; Jiang et al., 2022; Li et al., 2018; Ye et al., 2017). However, a satisfactory conclusion would not be possible without higher-quality research. As a result, the inclusion and exclusion criteria were developed after incorporating previous relevant reports, and the studies using a single-blind approach were pooled to be examined independently. Furthermore, there is currently a lack of conclusive proof. Given the growing number of RCTs using acupuncture for dysphagia caused by a swallowing issue, this review study explored the potential of acupuncture in treating dysphagia in stroke patients and the most promising acupuncture points for treating dysphagia.
2. Materials and Methods
Study protocol
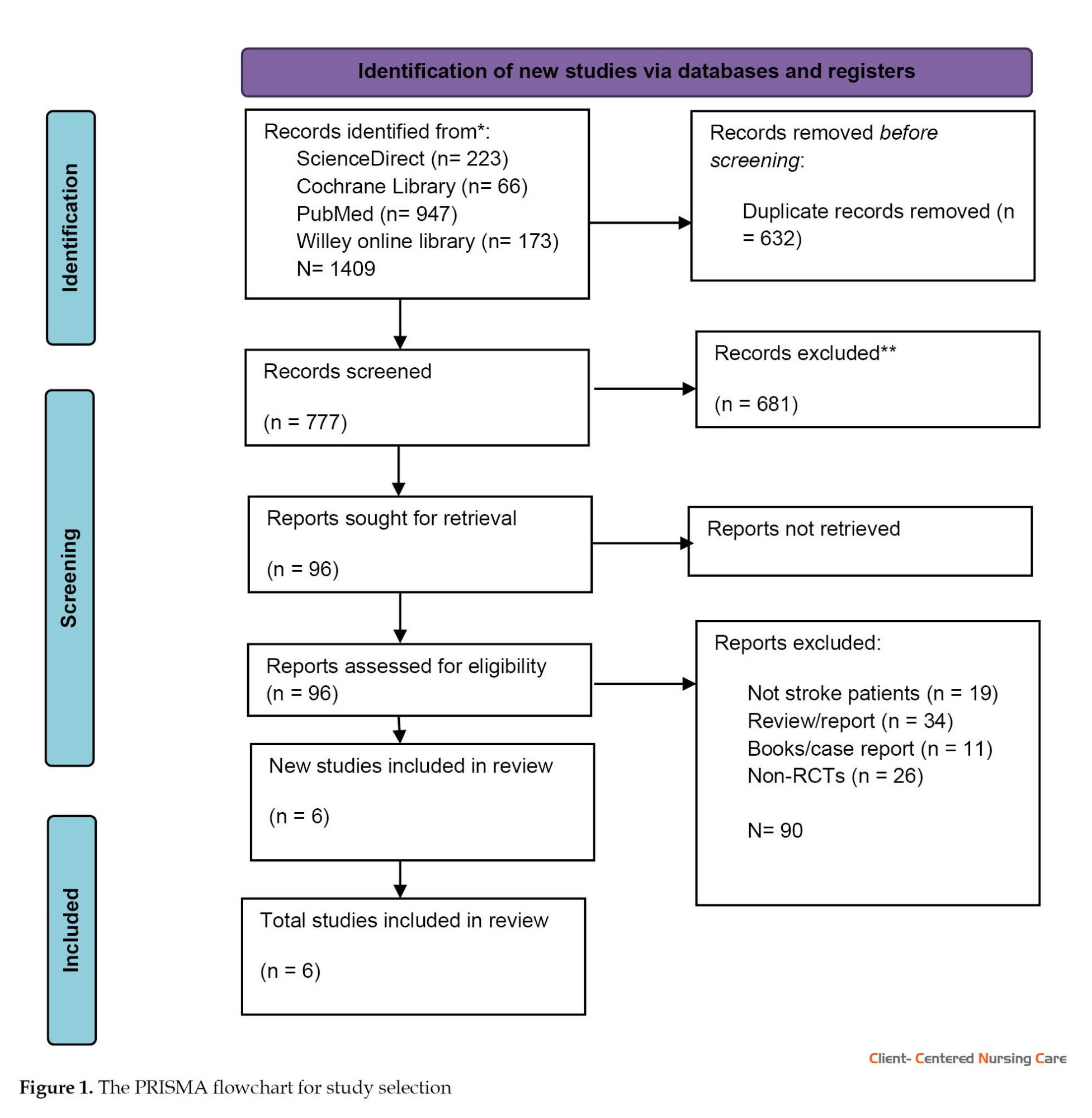
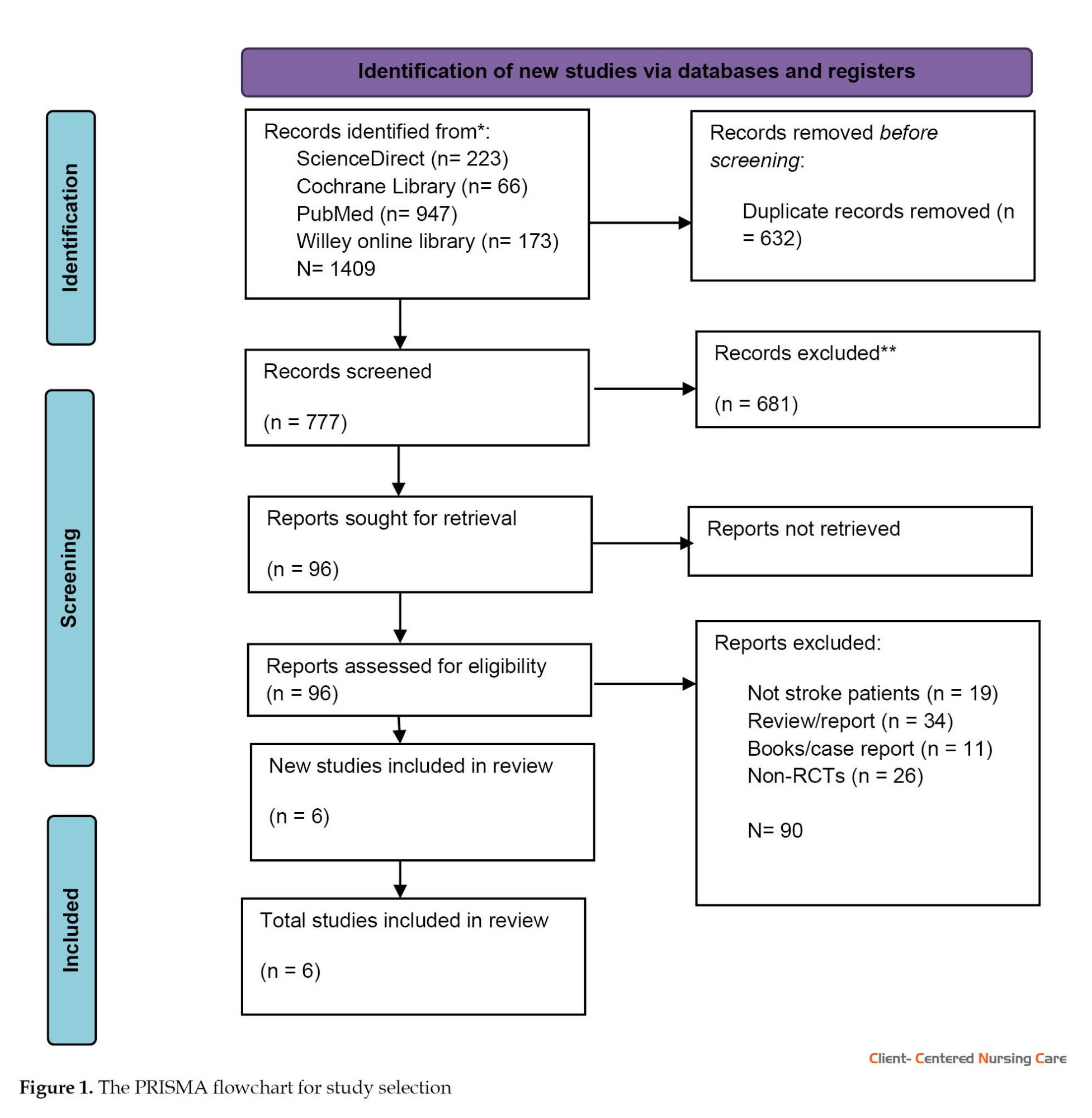
Following the preferred reporting items for systematic reviews and meta-analysis (PRISMA) 2020 recommendations (Page et al., 2021), we conducted a systematic evaluation of the literature comprising RCTs that documented the effectiveness of acupuncture therapy on dysphagia in post-stroke patients.
The population, intervention, comparison, outcome, and study design (PICOS) criteria outlined in Table 1 were used to select studies for inclusion in this review.

Eligibility criteria
We removed articles uploaded to RefWorks, a web-based reference management software, and duplicates. It was then disseminated to the team members and continued by assigning to a single reviewer’s initial review of the title and abstract. The next step was a full-text review executed by two reviewers. Additional reviewers were prepared for any disagreement to reach a consensus. Articles were included if the study subjects were >15 years old, >1 week post-stroke, the intervention of acupuncture or combined with other therapy, the study in a clinic or community, and the full text was available in English. Articles were excluded if the study was unavailable in English version, observational studies, theses, conference abstracts, commentaries, and editorials; poster presentations were also excluded.
Information source
A database search was conducted in May 2022 by a medical librarian for articles published within the past 12 years, from 2010 to 2022. The databases searched were PubMed, ScienceDirect, Wiley Online Library, and Cochrane Library.
Search strategy
The following search terms were used to build a comprehensive search strategy for each database: “Stroke,” “hemorrhagic stroke,” “cerebral hemorrhage,” “ischemic stroke,” “acupuncture,” “impaired swallowing,” AND “dysphagia” (Table 2). A review of references of all included studies was also performed.

Data extraction
Using the Cochrane data extraction and assessment form, two authors (HJS and LoA) independently extracted data from relevant studies. Disagreements between authors were resolved by consensus of all authors. The data extracted included the author(s), year of publication and country of origin, research design, sampling, assessment indicators, and main findings.
Quality assessment
The quality of the studies was assessed by two authors independently using the critical appraisal skills program (CASP) for the randomized controlled trial (critical appraisal skills program (CASP), 2022). This tool consists of 11 questions which are divided into three sections with the choices of “yes,” “no,” and “can’t tell” checklist columns. We categorize the quality of studies into high, medium, and low. In high-quality studies, the “yes” answers are 10–11; in medium-quality studies, the “yes” answers are 7–9; and in low-quality studies, the “yes” answers are ≤6.
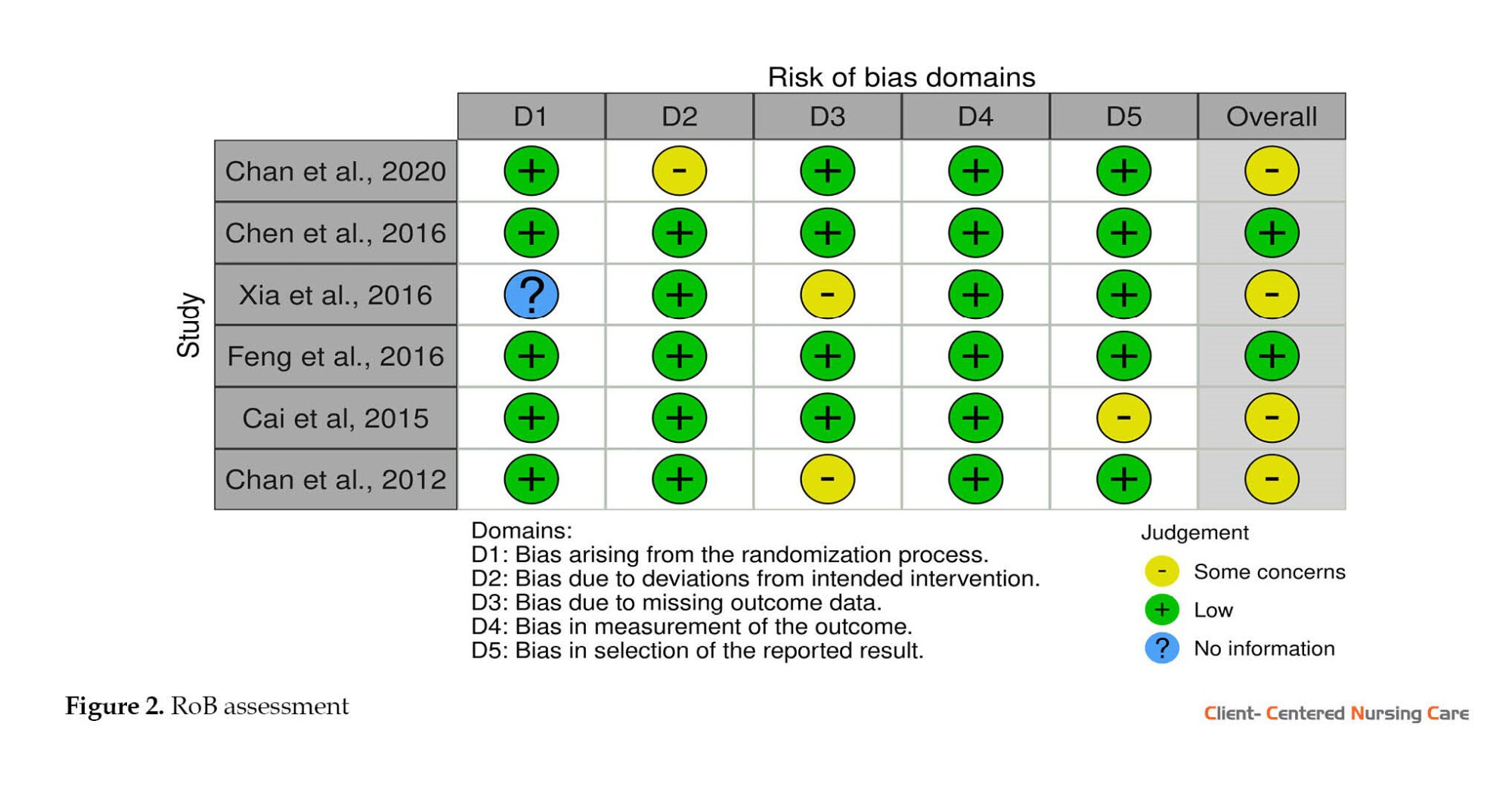
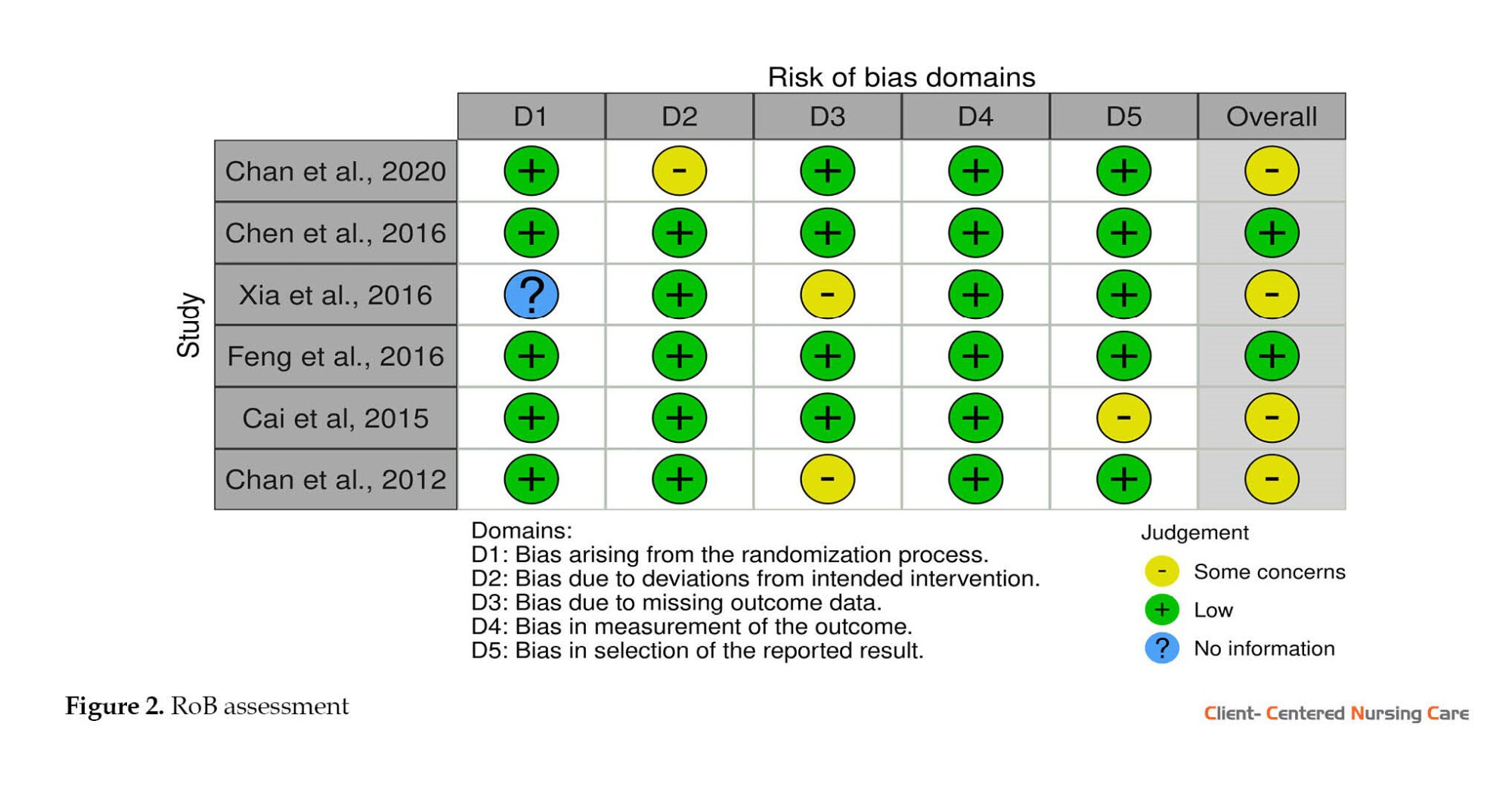
Risk of bias assessment
We assessed the risk of bias using the Cochrane RoB‑2 (by using RoB (risk-of-bias tool) software, version 2 (Sterne et al., 2019), which uses the following 5 domains: Randomization process, deviation from intended interventions, missing outcome data, outcome measurement, and selection of the reported result. The overall risk of bias rating is derived from the 5 individual ratings and determined by the RoB-2 algorithm. Each domain’s categorization of bias assessments includes high, moderate, and low. The bias assessment results are presented as a traffic light plot from the RoB visualization tool.
3. Results
Study selection
The literature search results identified 1409 publications through the forward and backward search of relevant papers from the databases used. A complete screening was carried out on 777 articles. It was determined that 681 articles failed to meet the eligibility criteria at the full-text screening stage. At the end of the stage, only 6 articles were finally eligible for further analysis. Data were analyzed thematically. The search results follow the PRISMA 2020 flowchart (Figure 1).
Results of study quality and bias assessment
Each study was screened against the 11 questions forming the CASP method. The screening result indicated that most eligible studies are high-quality, with "yes" answers between 10-11. Only one study was in the medium-quality category (8/11).
Based on the results of risk of bias analysis using the Cochrane RoB 2 tool (Sterne et al. 2019), 2 studies were found to be in the low risk of bias category, and the rest were in the status with some concerns (Figure 2).
Characterization of included studies
Table 3 summarizes the features of all included trials investigating the therapeutic impact of acupuncture in persons with dysphagia after stroke (6 studies with 740 participants). For all trials, the median duration of symptoms was 6 months. Most participants (n=95) were older adults with an average age of 64 years. The average duration of the interventions implemented was 26 days. All the examined trials employed either single acupuncture or acupuncture paired with rehabilitation. The rehabilitation treatment methods included a swallowing therapy program, physical stimulation, physiotherapy, occupational therapy, and swallowing training. Instruments used to evaluate the effect of interventions, including the Royal Brisbane Hospital outcome measure for swallowing (RBHOMS), standard swallowing function score (SSA), Dysphagia outcome severity scale (DOSS), videofluoroscopic swallow study (VFSS), and watian water swallow test (WWST).
.jpg)
Efficacy of acupuncture
Based on the collected studies’ results, the included studies showed great potential in improving the patient’s swallowing condition, which can be seen in the statistical significance of acupuncture therapy on changes in the patient’s swallowing score (P<0.001). The biggest changes occurred in studies that provided acupuncture therapy more than once daily for 30 minutes per session.
No single study reveals the unsuccessful use of acupuncture therapy for dysphagia. However, acupuncture therapy will be more effective when combined with other therapies, such as a swallowing therapy program, physical stimulation (Chan et al., 2020; Chen et al., 2016; Xia et al., 2016), normal limb posture, passive motion with hemiplegic side, bedside rehabilitation (Bobath technique, overturning movement, bridge movement), neuromuscular electrical stimulation (Chen et al., 2016), oral motor exercises, different swallowing techniques, positioning and diet modification (Chan et al., 2012).
Acupuncture points
There are different acupoints from the studies included in this review, including GB20 (Fengchi), EX-HN14 (Yiming), BL10 (Tianzhu), GV16 (Fengfu), Gongxue (1 cun below GB20-Cun is a traditional Chinese unit of length), and CV23 (Lianquan) (Chen et al., 2016), GB 12 (Wan Gu bilateral), GB20 (Feng Chi, bilateral), CV23 (Lian Quan), DU20 (Bai Hui), LI4 (He Gu, bilateral), HT5 (Tong Li, bilateral), Hang Sang, Shang Lian Quan (EX-HN20) (Chan et al., 2020), fengchi (GB 20, unilateral), jiaji (C2-C4) (EX-B2, bilateral), lianquan (CV23, unilateral), jiajianquan (left CV 23 and right CV 23, bilateral), and baihui (GV 20, unilateral) (Xia et al., 2016), Juanquan (EXHN10) (at the midpoint of dorsal raphe of the tongue) and Haiquan (EX-HN11) (Sublingual frenulum midpoint) (Cai et al., 2015). Acupoits on the body are Fengchi (GB20) and Neiguan (PC6) (Cai et al., 2015), angu (GB 12), Fengchi (GB 20) and Yifeng (SJ 17) (Chan et al., 2012).
4. Discussion
This systematic review evaluated 6 RCTs analyzing the efficacy of acupuncture compared with standard rehabilitation of dysphagia in stroke patients. Almost all relevant studies were conducted in China, given that acupuncture therapy is part of traditional Chinese medicine. There were few studies regarding acupuncture treatment for dysphagia in stroke patients that we could access; mainly, the available articles were in Chinese. In addition, the other studies were not RCTs, as we had defined them as inclusion criteria in the article search. Based on the accumulating evidence, acupuncture can significantly improve dysphagia in stroke cases. In addition, acupuncture combined with standard rehabilitation shows a better effect.
The study discovered that the therapeutic efficacy of acupuncture or acupuncture integrated with different interventions was superior to the control group. Meanwhile, the varied sources of instances may result in disparate statistical conclusions. Acupuncture, rehabilitation, and swallowing training were all linked to the practitioners’ professional skills, just like the efficacy evaluation.
Acupuncture, alone or combined with other interventions, is frequently used in China to treat dysphagia following a stroke. Some evidence backs up that acupuncture can help with dysphagia after a stroke. Although one report (Ye et al., 2017) states that acupuncture improves dysphagia after stroke, this study does not provide a positive conclusion. According to one study (Meng et al., 2016), acupuncture simultaneous with swallowing rehabilitation training offers some benefits. According to Long and Wu, (2012), acupuncture may be effective for dysphagia, but more research is needed. The current study uses multiple inclusion and exclusion standards to estimate the efficacy of acupuncture in treating dysphagia after stroke and re-examined this efficacy, resulting in more powerful evidence. Most studies use the WWST, SSA, and other dysphagia outcome indicators. Three investigations used VFSS as a scoring indicator (Cai et al., 2015; Feng et al., 2016; Chen et al., 2016). The WWST was proposed by Toshio Watian from Japan and is used as an initial screening for dysphagia.
Meanwhile, depending on the patient’s feelings and susceptibility level, it must be consistent with most clinical and laboratory examination results (Juan et al., 2016). However, everything is clearly labeled and easy to use. As a result, it has been used in numerous clinical studies (Zeng et al., 2015; Xia et al., 2016; Zhang et al., 2014). Hence, evaluating criteria in clinical trial design must be more rigorous and scientific. To improve dependability, high-level evaluators should be chosen to assess efficacy for dysphagia simultaneously. Acupoints, stimulation type, needle retention time, and treatment sessions were all different in the acupuncture therapy regimen. Although particular acupoints are more regularly employed, the intensity of acupuncture therapy varies substantially across included RCTs.
GB20 and CV23 are the acupoints that seem frequently in the studies. As a result, acupuncture at these two acupoints may aid in treating dysphagia following a stroke. The WHO conventional acupoints (WHO, 2007) place GB20 at the sub-occipital depression and the surrounding head clamp muscle, sternocleidomastoid muscle, trapezius muscle, and branches of the lesser occipital nerve. CV23 can be found in Adam’s tubercle, the anterior region of the cervical midline, and the depression of the superior margin of the hyoid bone. The suprahyoid muscle, hypoglossal, facial, glossopharyngeal, and vagus are among the surrounding anatomical tissues. According to studies, EA stimulation of CV23 triggered swallowing-related neurons in rats’ ventrolateral medulla (VLM) and boosted swallowing activity. 5-Hydroxytryptamine may be essential in this excitatory effect (Ye et al., 2019; You et al., 2018).
This systematic review provides evidence to consider acupuncture as an alternative treatment for dysphagia but preferably in combination with standard post-stroke medical treatment for routine therapy, especially in the international background of an increasing application of acupuncture therapy.
Some limitations in this review include the small number of studies analyzed due to language limitations and access to certain databases. For this reason, the results of this study must be mentioned with caution. Besides, most trials were implemented in China, and it was hard to determine the efficacy of acupuncture in different countries and ethnic groups. Finally, since there were some concerns related to bias in most included studies, the findings should be interpreted with caution.
5. Conclusion
To summarize, acupuncture for dysphagia after stroke demonstrates therapeutic efficacy and is safe and reliable within a certain range. More stringent evaluation criteria and high-quality RCT designs are required to further examine acupuncture for treating dysphagia following stroke. Since no side effects were found from this acupuncture therapy, the duration of the intervention should have been longer, at least up to one year. Improving circulation and the affected nervous system in areas related to chewing and swallowing requires a longer recovery time, especially for older people.
Ethical Considerations
Compliance with ethical guidelines
All the authors have contributed to the design and conduct of the study. Duplicate publications were removed. Data were extracted independently by two authors, and disagreement between them were resolved by consensus after consulting with other researchers. Decisions on which data to include are also agreed upon by all authors.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
conceptualization and drafting the manuscript: Heriviyatno. J Siagian and Arimaswati Arimaswati; Data curation: Rusmimpong Rusmimpong and Sukurni Sukurni; Data analysis and interpretation: Heriviyatno.J Siagian and La Ode Alifariki; Critical revision of the article: Arimaswati Arimaswati; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the head of the University Library of Sembilanbelas November Kolaka, and HaluOleo University, who have provided access to literature database search tools.
References
Bath, P. M., Lee, H. S. & Everton, L. F., 2018. Swallowing Therapy for Dysphagia in Acute and Subacute Stroke. Cochrane Database of Systematic Reviews, 10(10), pp. CD000323. [DOI:10.1002/14651858.CD000323.pub3] [PMID]
Belskaya, G. N., 2020. [Acupuncture in the prevention and treatment of stroke: A review of foreign studies (Russian)]. Voprosy Kurortologii, Fizioterapii, i Lechebnoi Fizicheskoi Kultury , 97(2), pp. 68-77. [DOI:10.17116/kurort20209702168] [PMID]
Brady, M. C., et al., 2016. Speech and language therapy for aphasia following stroke. The Cochrane Database of Systematic Reviews, 2016(6), pp. CD000425. [DOI:10.1002/14651858.CD000425.pub4] [PMID]
Cai, H., et al., 2015. Tongue acupuncture in treatment of post-stroke dysphagia. International Journal of Clinical and Experimental Medicine, 8(8), pp. 14090-4. [PMID]
Calandra-Buonaura, G., et al., 2021. Dysphagia in multiple system atrophy consensus statement on diagnosis, prognosis and treatment. Parkinsonism & Related Disorders, 86, pp. 124-32. [DOI:10.1016/j.parkreldis.2021.03.027] [PMID]
Chan, S. L., et al., 2012. Therapeutic effects of acupuncture for neurogenic dysphagia-a randomized controlled trial. Journal of Traditional Chinese Medicine, 32(1), pp. 25-30. [DOI:10.1016/S0254-6272(12)60027-2] [PMID]
Chan, Y. T., et al., 2020. Acupuncture for poststroke dysphagia: A pilot, nonrandomized, self-controlled trial. Evidence-Based Complementary and Alternative Medicine: eCAM, 2020, pp. 4689296. [DOI:10.1155/2020/4689296] [PMID] [PMCID]
Chavez, L. M., et al., 2017. Mechanisms of acupuncture therapy in ischemic stroke rehabilitation: A literature review of basic studies. International Journal of Molecular Sciences, 18(11), pp. 2270. [DOI:10.3390/ijms18112270] [PMID] [PMCID]
Chen, Y. W., et al., 2016. The effects of surface neuromuscular electrical stimulation on post-stroke dysphagia: A systemic review and meta-analysis. Clinical Rehabilitation, 30(1), pp. 24-35. [DOI:10.1177/0269215515571681] [PMID]
Deng, M., et al., 2016. Acupuncture for amnestic mild cognitive impairment: A meta-analysis of randomised controlled trials. Acupuncture in Medicine: Journal of the British Medical Acupuncture Society, 34(5), 342–348. [DOI:10.1136/acupmed-2015-010989] [PMID]
Deng, D., et al. 2016.“Changes in regional brain homogeneity induced by electro-acupuncture stimulation at the baihui acupoint in healthy subjects: A functional magnetic resonance imaging study.”Journal of Alternative and Complementary Medicine vol. 22,10 (2016): 794-799. [DOI:10.1089/acm.2015.0286] [PMID]
Feng, S., Cao, S., Du, S., Yin, T., Mai, F., Chen, X., & Su, X. (2016). [Acuuncture combined with swallowing training for post-stroke dysphagia: A randomized controlled trial (Chinease)]. Chinese Acupuncture & Moxibustion, 36(4), 347–350. [PMID]
Geeganage, C., et al., 2012. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database of Systematic Reviews, 10, pp. CD000323. [DOI:10.1002/14651858.CD000323.pub2] [PMID]
Guillén-Solà, A., et al., 2017. Respiratory muscle strength training and neuromuscular electrical stimulation in subacute dysphagic stroke patients: A randomized controlled trial. Clinical Rehabilitation, 31(6), pp. 761-71. [DOI:10.1177/0269215516652446] [PMID]
Huang, K. L., et al., 2014. Functional outcome in acute stroke patients with oropharyngeal dysphagia after swallowing therapy. Journal of Stroke and Cerebrovascular Diseases, 23(10), pp. 2547-53. [DOI:10.1016/j.jstrokecerebrovasdis.2014.05.031] [PMID]
Jia, B., et al., 2015. The effects of acupuncture at real or sham acupoints on the intrinsic brain activity in mild cognitive impairment patients. Evidence-Based Complementary and Alternative Medicine, 2015, pp. 529675. [DOI:10.1155/2015/529675] [PMID] [PMCID]
Jiang, H., et al., 2022. Manual acupuncture or combination of rehabilitation therapy to treat poststroke dysphagia: A systematic review and meta-analysis of randomized controlled trials. Evidence-Based Complementary and Alternative Medicine, 2022, pp. 8803507. [DOI:10.1155/2022/8803507] [PMID] [PMCID]
Juan, W., et al., 2016. Value of applying water swallowing test for patients with dysphagia after acute stroke. Journal of Shanghai Jiaotong, 36(07), pp. 1049. [DOI:10.3969/j.issn.1674-8115.2016.07.018]
Lancaster, J., 2015. Dysphagia: Its nature, assessment and management. British Journal of Community Nursing, Suppl Nutrition, pp. S28–32. [DOI:10.12968/bjcn.2015.20.Sup6a.S28] [PMID]
Li, L.X., et al., 2018. Acupuncture treatment for post-stroke dysphagia: An update meta-analysis of randomized controlled trials. Chinese Journal of Integrative Medicine, 24(9), pp. 686-95. [DOI:10.1007/s11655-018-3005-3] [PMID]
Li, X. & Wang, Q., 2013. Acupuncture therapy for stroke patients. International Review of Neurobiology, 111, pp. 159-79. [DOI:10.1016/B978-0-12-411545-3.00008-0] [PMID]
Lim, K.B., et al., 2014. Effect of low-frequency rTMS and NMES on subacute unilateral hemispheric stroke with dysphagia. Annals of Rehabilitation Medicine, 38(5), 592–602. [DOI:10.5535/arm.2014.38.5.592] [PMID] [PMCID]
Long, Y.B. & Wu, X.P., 2012. A meta-analysis of the efficacy of acupuncture in treating dysphagia in patients with a stroke. Acupuncture in Medicine, 30(4), pp. 291-7. [DOI:10.1136/acupmed-2012-010155] [PMID]
Marin, S., et al., 2018. Cost of oropharyngeal dysphagia after stroke: Protocol for a systematic review. BMJ Open, 8(12), pp. e022775. [DOI:10.1136/bmjopen-2018-022775] [PMID] [PMCID]
Meng, D., et al., 2016. Clinical literature study of acupuncture and moxibustion in the treatment of post stroke dysphagia based on meta-analysis. Chinese Medicine Modern Distance Education of China, 16(64), 148-153. [Link]
Meng, P. P., et al., 2020. The occurrence rate of swallowing disorders after stroke patients in Asia: A PRISMA-compliant systematic review and meta-analysis. Journal of Stroke and Cerebrovascular Diseases, 29(10), pp.105113. [DOI:10.1016/j.jstrokecerebrovasdis.2020.105113] [PMID]
Namasivayam-MacDonald, A.M. & Shune, S.E., 2018. The burden of dysphagia on family caregivers of the elderly: A systematic review. Geriatrics, 3(2), pp. 30. [DOI:10.3390/geriatrics3020030] [PMID] [PMCID]
Olesen, M. D., et al., 2021. Prevalence of signs of dysphagia and associated risk factors in geriatric patients admitted to an acute medical unit. Clinical Nutrition ESPEN, 41, pp. 208-16. [DOI:10.1016/j.clnesp.2020.12.020] [PMID]
Page, M. J., et al., 2021. The PRISMA 2020 Statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, pp. 105906. [PMID]
Park, J. S., et al., 2016. Effects of neuromuscular electrical stimulation combined with effortful swallowing on post-stroke oropharyngeal dysphagia: A randomised controlled trial. Journal of Oral Rehabilitation, 43(6), 426–434. [DOI:10.1111/joor.12390] [PMID]
Park, J. S., et al., 2016. Effects of expiratory muscle strength training on oropharyngeal dysphagia in subacute stroke patients: A randomised controlled trial. Journal of Oral Rehabilitation 43(5):364-72. [DOI:10.1111/joor.12382] [PMID]
Song, Y.P., Yang, W., Guo, H.M. and Han, Y.Y., 2006. [Clinical observation on acupuncture combined with medicine for treatment of infantile febrile convulsion (Chinese)]. Chinese Acupuncture & Moxibustion, 26(8), pp.561-562. [PMID]
Speyer, R., et al., 2022. Behavioural interventions in people with oropharyngeal dysphagia: A systematic review and meta-analysis of randomised clinical trials. Journal of Clinical Medicine, 11(3), pp. 685. [DOI:10.3390/jcm11030685] [PMID] [PMCID]
Sterne, J. A. C., et al., 2019. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed.), 366, pp. l4898. [DOI:10.1136/bmj.l4898] [PMID]
Teuschl, Y., et al., 2018. Systematic dysphagia screening and dietary modifications to reduce stroke-associated pneumonia rates in a stroke-unit. Plos One, 13(2), pp. e0192142. [DOI:10.1371/journal.pone.0192142] [PMID] [PMCID]
Waters, A. M., et al., 2022. Investigating dysphagia in adults: Symptoms and tests.” BMJ (Clinical research ed.), 379, pp. e067347. [DOI:10.1136/bmj-2021-067347] [PMID]
Wen, X., et al., 2023. The effect of repetitive transcranial magnetic stimulation in synchronization with effortful swallowing on post-stroke dysphagia. Dysphagia, 38(3), pp. 912–22. [DOI:10.1007/s00455-022-10515-4] [PMID]
World Health Organization. & Regional Office for the Western Pacific., 2007. WHO international standard terminologies on traditional medicine in the Western Pacific Region. Manila: WHO Regional Office for the Western Pacific. [Link]
Wu, W. B., 2019. Relieving throat and opening orifice acupuncture therapy for the post-stroke dysphagia. World Journal of Acupuncture-Moxibustion, 29(1), pp. 37-41. [DOI:10.1016/j.wjam.2019.04.004]
Xia, W., Zheng, C., Zhu, S., & Tang, Z. (2016). Does the addition of specific acupuncture to standard swallowing training improve outcomes in patients with dysphagia after stroke? a randomized controlled trial. Clinical Rehabilitation, 30(3), 237-246. [DOI:10.1177/0269215515578698]
Ye, Q., et al., 2019. Effect of electro-acupuncture on regulating the swallowing by activating the interneuron in ventrolateral medulla (VLM). Brain Research Bulletin, 144, pp. 132-9. [DOI:10.1016/j.brainresbull.2018.11.021] [PMID]
Ye, Q., et al., 2017. Systematic review on acupuncture for treatment of dysphagia after stroke. Evidence-Based Complementary and Alternative Medicine, 2017, pp. 6421852. [DOI:10.1155/2017/6421852] [PMID] [PMCID]
You, H., et al., 2018. Role of 5-HT1A in the nucleus of the solitary tract in the regulation of swallowing activities evoked by electroacupuncture in anesthetized rats. Neuroscience Letters, 687, 308-312. [DOI: 10.1016/j.neulet.2018.06.018]
Yu, H., et al., 2018. Modulation of spectral power and functional connectivity in human brain by acupuncture stimulation. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 26(5), pp. 977-86. [DOI:10.1109/TNSRE.2018.2828143] [PMID]
Zhang, J. H., Wang, D. & Liu, M., 2014. Overview of systematic reviews and meta-analyses of acupuncture for stroke. Neuroepidemiology, 42(1), pp. 50-8. [DOI:10.1159/000355435] [PMID]
Zeng, Y., Bao, Y., Zhu, M., Chen, S., & Fang, J. (2015). [Mild cognitive impairment of stroke at subacute stage treated with acupuncture: A randomized controlled trial (Chinease)]. Chinese Acupuncture & Moxibustion, 35(10), 979–982.
Dysphagia is prevalent in stroke survivors, with an incidence rate of 8.1% to 80%. Dysphagia was reported in 36.3% of post-stroke patients in Asia (Meng et al., 2020). Dysphagia worsens when swallowing liquids (Lancaster, 2015), causing major problems such as aspiration, pneumonia, and even death (Calandra-Buonaura et al., 2021; Waters et al., 2022). Furthermore, dysphagia is associated with social anxiety, withdrawal, and depression (MacDonald et al., 2018; Olesen et al., 2021). It may also impact daily activities, quality of life, and stroke prognosis. Repetitive transcranial magnetic stimulation, swallowing training (Huang et al., 2014; Wen et al., 2022), transcutaneous and retropharyngeal electrical stimulation, non-invasive brain stimulation strategies, transcranial direct current stimulation (Marin et al., 2018), speech and language therapy (Brady et al., 2016), expiratory muscle strength training (Guillén-Solà et al., 2017; Park et al., 2016a), behavioral interventions (Speyer et al., 2022), dietary modification (Teuschl et al., 2018), and neuromuscular electrical stimulation (Chen et al., 2016; Park et al., 2016b). As a result, managing patients with post-stroke dysphagia requires a multidisciplinary approach (Song et al., 2015; Park et al., 2016b).
Acupuncture is a traditional Chinese medicine procedure in which acupuncturists insert needles through the skin to balance life energy, known as “qi.” Over the past 1000 years, China has used acupuncture for stroke rehabilitation. Even the World Health Organization (WHO) has acknowledged acupunctures as an alternative and complementary technique for stroke therapy and care (Chavez et al., 2017). Traditional manual acupuncture (TA), electroacupuncture (EA) (Lim et al., 2014; Yu et al., 2018), moxibustion acupuncture (MA), and scalp acupuncture (SA) are available modes for treating dysphagia following a stroke (Zhang et al., 2014). A series of trials in humans and investigations in animals have revealed that the acupuncture mechanism for stroke primarily includes neurotransmitter release regulation, cerebral microcirculation regulation, anti-apoptosis, stimulation of neurogenesis and cell proliferation, and neuroplasticity regulation (Belskaya et al., 2020; Li & Wang, 2013).
Acupuncture’s physiological influence on dysphagia after stroke has not been well researched. Previous studies show that acupuncture affects regional brain activity (Deng et al., 2016; Jia et al., 2015; Demao et al., 2016; Feng et al., 2016; Meng et al., 2016; Yu et al., 2018). Furthermore, acupuncture can aid in repairing and reconstructing swallowing function by forming new synaptic connections and hastening the restoration and reconstruction of the swallowing reflex arc (Li et al., 2018; Wu et al., 2019). Given the possible benefits of acupuncture for treating dysphagia after stroke, its use in dysphagia intervention has grown in popularity in China and worldwide.
According to a previous systematic review, acupuncture can lessen clinical symptoms such as trouble swallowing and lower the prevalence of dysphagia (Geeganage et al., 2012). It can also enhance patients’ quality of life. Acupuncture has been included in the most recent Cochrane study on swallowing therapy, although it did not significantly affect the outcomes of dependency/disability, misaspiration rate, or death (Bath et al., 2018).
Acupuncture research for dysphagia or swallowing disorders has risen, although the outcomes have been inconsistent (Chan et al., 2012; Feng et al., 2016; Xia et al., 2016; Chan et al., 2020). In a few systematic reviews, acupuncture has been utilized to treat dysphagia in stroke patients (Cai et al., 2015; Jiang et al., 2022; Li et al., 2018; Ye et al., 2017). However, a satisfactory conclusion would not be possible without higher-quality research. As a result, the inclusion and exclusion criteria were developed after incorporating previous relevant reports, and the studies using a single-blind approach were pooled to be examined independently. Furthermore, there is currently a lack of conclusive proof. Given the growing number of RCTs using acupuncture for dysphagia caused by a swallowing issue, this review study explored the potential of acupuncture in treating dysphagia in stroke patients and the most promising acupuncture points for treating dysphagia.
2. Materials and Methods
Study protocol
Following the preferred reporting items for systematic reviews and meta-analysis (PRISMA) 2020 recommendations (Page et al., 2021), we conducted a systematic evaluation of the literature comprising RCTs that documented the effectiveness of acupuncture therapy on dysphagia in post-stroke patients.
The population, intervention, comparison, outcome, and study design (PICOS) criteria outlined in Table 1 were used to select studies for inclusion in this review.

Eligibility criteria
We removed articles uploaded to RefWorks, a web-based reference management software, and duplicates. It was then disseminated to the team members and continued by assigning to a single reviewer’s initial review of the title and abstract. The next step was a full-text review executed by two reviewers. Additional reviewers were prepared for any disagreement to reach a consensus. Articles were included if the study subjects were >15 years old, >1 week post-stroke, the intervention of acupuncture or combined with other therapy, the study in a clinic or community, and the full text was available in English. Articles were excluded if the study was unavailable in English version, observational studies, theses, conference abstracts, commentaries, and editorials; poster presentations were also excluded.
Information source
A database search was conducted in May 2022 by a medical librarian for articles published within the past 12 years, from 2010 to 2022. The databases searched were PubMed, ScienceDirect, Wiley Online Library, and Cochrane Library.
Search strategy
The following search terms were used to build a comprehensive search strategy for each database: “Stroke,” “hemorrhagic stroke,” “cerebral hemorrhage,” “ischemic stroke,” “acupuncture,” “impaired swallowing,” AND “dysphagia” (Table 2). A review of references of all included studies was also performed.

Data extraction
Using the Cochrane data extraction and assessment form, two authors (HJS and LoA) independently extracted data from relevant studies. Disagreements between authors were resolved by consensus of all authors. The data extracted included the author(s), year of publication and country of origin, research design, sampling, assessment indicators, and main findings.
Quality assessment
The quality of the studies was assessed by two authors independently using the critical appraisal skills program (CASP) for the randomized controlled trial (critical appraisal skills program (CASP), 2022). This tool consists of 11 questions which are divided into three sections with the choices of “yes,” “no,” and “can’t tell” checklist columns. We categorize the quality of studies into high, medium, and low. In high-quality studies, the “yes” answers are 10–11; in medium-quality studies, the “yes” answers are 7–9; and in low-quality studies, the “yes” answers are ≤6.
Risk of bias assessment
We assessed the risk of bias using the Cochrane RoB‑2 (by using RoB (risk-of-bias tool) software, version 2 (Sterne et al., 2019), which uses the following 5 domains: Randomization process, deviation from intended interventions, missing outcome data, outcome measurement, and selection of the reported result. The overall risk of bias rating is derived from the 5 individual ratings and determined by the RoB-2 algorithm. Each domain’s categorization of bias assessments includes high, moderate, and low. The bias assessment results are presented as a traffic light plot from the RoB visualization tool.
3. Results
Study selection
The literature search results identified 1409 publications through the forward and backward search of relevant papers from the databases used. A complete screening was carried out on 777 articles. It was determined that 681 articles failed to meet the eligibility criteria at the full-text screening stage. At the end of the stage, only 6 articles were finally eligible for further analysis. Data were analyzed thematically. The search results follow the PRISMA 2020 flowchart (Figure 1).
Results of study quality and bias assessment
Each study was screened against the 11 questions forming the CASP method. The screening result indicated that most eligible studies are high-quality, with "yes" answers between 10-11. Only one study was in the medium-quality category (8/11).
Based on the results of risk of bias analysis using the Cochrane RoB 2 tool (Sterne et al. 2019), 2 studies were found to be in the low risk of bias category, and the rest were in the status with some concerns (Figure 2).
Characterization of included studies
Table 3 summarizes the features of all included trials investigating the therapeutic impact of acupuncture in persons with dysphagia after stroke (6 studies with 740 participants). For all trials, the median duration of symptoms was 6 months. Most participants (n=95) were older adults with an average age of 64 years. The average duration of the interventions implemented was 26 days. All the examined trials employed either single acupuncture or acupuncture paired with rehabilitation. The rehabilitation treatment methods included a swallowing therapy program, physical stimulation, physiotherapy, occupational therapy, and swallowing training. Instruments used to evaluate the effect of interventions, including the Royal Brisbane Hospital outcome measure for swallowing (RBHOMS), standard swallowing function score (SSA), Dysphagia outcome severity scale (DOSS), videofluoroscopic swallow study (VFSS), and watian water swallow test (WWST).
.jpg)
Efficacy of acupuncture
Based on the collected studies’ results, the included studies showed great potential in improving the patient’s swallowing condition, which can be seen in the statistical significance of acupuncture therapy on changes in the patient’s swallowing score (P<0.001). The biggest changes occurred in studies that provided acupuncture therapy more than once daily for 30 minutes per session.
No single study reveals the unsuccessful use of acupuncture therapy for dysphagia. However, acupuncture therapy will be more effective when combined with other therapies, such as a swallowing therapy program, physical stimulation (Chan et al., 2020; Chen et al., 2016; Xia et al., 2016), normal limb posture, passive motion with hemiplegic side, bedside rehabilitation (Bobath technique, overturning movement, bridge movement), neuromuscular electrical stimulation (Chen et al., 2016), oral motor exercises, different swallowing techniques, positioning and diet modification (Chan et al., 2012).
Acupuncture points
There are different acupoints from the studies included in this review, including GB20 (Fengchi), EX-HN14 (Yiming), BL10 (Tianzhu), GV16 (Fengfu), Gongxue (1 cun below GB20-Cun is a traditional Chinese unit of length), and CV23 (Lianquan) (Chen et al., 2016), GB 12 (Wan Gu bilateral), GB20 (Feng Chi, bilateral), CV23 (Lian Quan), DU20 (Bai Hui), LI4 (He Gu, bilateral), HT5 (Tong Li, bilateral), Hang Sang, Shang Lian Quan (EX-HN20) (Chan et al., 2020), fengchi (GB 20, unilateral), jiaji (C2-C4) (EX-B2, bilateral), lianquan (CV23, unilateral), jiajianquan (left CV 23 and right CV 23, bilateral), and baihui (GV 20, unilateral) (Xia et al., 2016), Juanquan (EXHN10) (at the midpoint of dorsal raphe of the tongue) and Haiquan (EX-HN11) (Sublingual frenulum midpoint) (Cai et al., 2015). Acupoits on the body are Fengchi (GB20) and Neiguan (PC6) (Cai et al., 2015), angu (GB 12), Fengchi (GB 20) and Yifeng (SJ 17) (Chan et al., 2012).
4. Discussion
This systematic review evaluated 6 RCTs analyzing the efficacy of acupuncture compared with standard rehabilitation of dysphagia in stroke patients. Almost all relevant studies were conducted in China, given that acupuncture therapy is part of traditional Chinese medicine. There were few studies regarding acupuncture treatment for dysphagia in stroke patients that we could access; mainly, the available articles were in Chinese. In addition, the other studies were not RCTs, as we had defined them as inclusion criteria in the article search. Based on the accumulating evidence, acupuncture can significantly improve dysphagia in stroke cases. In addition, acupuncture combined with standard rehabilitation shows a better effect.
The study discovered that the therapeutic efficacy of acupuncture or acupuncture integrated with different interventions was superior to the control group. Meanwhile, the varied sources of instances may result in disparate statistical conclusions. Acupuncture, rehabilitation, and swallowing training were all linked to the practitioners’ professional skills, just like the efficacy evaluation.
Acupuncture, alone or combined with other interventions, is frequently used in China to treat dysphagia following a stroke. Some evidence backs up that acupuncture can help with dysphagia after a stroke. Although one report (Ye et al., 2017) states that acupuncture improves dysphagia after stroke, this study does not provide a positive conclusion. According to one study (Meng et al., 2016), acupuncture simultaneous with swallowing rehabilitation training offers some benefits. According to Long and Wu, (2012), acupuncture may be effective for dysphagia, but more research is needed. The current study uses multiple inclusion and exclusion standards to estimate the efficacy of acupuncture in treating dysphagia after stroke and re-examined this efficacy, resulting in more powerful evidence. Most studies use the WWST, SSA, and other dysphagia outcome indicators. Three investigations used VFSS as a scoring indicator (Cai et al., 2015; Feng et al., 2016; Chen et al., 2016). The WWST was proposed by Toshio Watian from Japan and is used as an initial screening for dysphagia.
Meanwhile, depending on the patient’s feelings and susceptibility level, it must be consistent with most clinical and laboratory examination results (Juan et al., 2016). However, everything is clearly labeled and easy to use. As a result, it has been used in numerous clinical studies (Zeng et al., 2015; Xia et al., 2016; Zhang et al., 2014). Hence, evaluating criteria in clinical trial design must be more rigorous and scientific. To improve dependability, high-level evaluators should be chosen to assess efficacy for dysphagia simultaneously. Acupoints, stimulation type, needle retention time, and treatment sessions were all different in the acupuncture therapy regimen. Although particular acupoints are more regularly employed, the intensity of acupuncture therapy varies substantially across included RCTs.
GB20 and CV23 are the acupoints that seem frequently in the studies. As a result, acupuncture at these two acupoints may aid in treating dysphagia following a stroke. The WHO conventional acupoints (WHO, 2007) place GB20 at the sub-occipital depression and the surrounding head clamp muscle, sternocleidomastoid muscle, trapezius muscle, and branches of the lesser occipital nerve. CV23 can be found in Adam’s tubercle, the anterior region of the cervical midline, and the depression of the superior margin of the hyoid bone. The suprahyoid muscle, hypoglossal, facial, glossopharyngeal, and vagus are among the surrounding anatomical tissues. According to studies, EA stimulation of CV23 triggered swallowing-related neurons in rats’ ventrolateral medulla (VLM) and boosted swallowing activity. 5-Hydroxytryptamine may be essential in this excitatory effect (Ye et al., 2019; You et al., 2018).
This systematic review provides evidence to consider acupuncture as an alternative treatment for dysphagia but preferably in combination with standard post-stroke medical treatment for routine therapy, especially in the international background of an increasing application of acupuncture therapy.
Some limitations in this review include the small number of studies analyzed due to language limitations and access to certain databases. For this reason, the results of this study must be mentioned with caution. Besides, most trials were implemented in China, and it was hard to determine the efficacy of acupuncture in different countries and ethnic groups. Finally, since there were some concerns related to bias in most included studies, the findings should be interpreted with caution.
5. Conclusion
To summarize, acupuncture for dysphagia after stroke demonstrates therapeutic efficacy and is safe and reliable within a certain range. More stringent evaluation criteria and high-quality RCT designs are required to further examine acupuncture for treating dysphagia following stroke. Since no side effects were found from this acupuncture therapy, the duration of the intervention should have been longer, at least up to one year. Improving circulation and the affected nervous system in areas related to chewing and swallowing requires a longer recovery time, especially for older people.
Ethical Considerations
Compliance with ethical guidelines
All the authors have contributed to the design and conduct of the study. Duplicate publications were removed. Data were extracted independently by two authors, and disagreement between them were resolved by consensus after consulting with other researchers. Decisions on which data to include are also agreed upon by all authors.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
conceptualization and drafting the manuscript: Heriviyatno. J Siagian and Arimaswati Arimaswati; Data curation: Rusmimpong Rusmimpong and Sukurni Sukurni; Data analysis and interpretation: Heriviyatno.J Siagian and La Ode Alifariki; Critical revision of the article: Arimaswati Arimaswati; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the head of the University Library of Sembilanbelas November Kolaka, and HaluOleo University, who have provided access to literature database search tools.
References
Bath, P. M., Lee, H. S. & Everton, L. F., 2018. Swallowing Therapy for Dysphagia in Acute and Subacute Stroke. Cochrane Database of Systematic Reviews, 10(10), pp. CD000323. [DOI:10.1002/14651858.CD000323.pub3] [PMID]
Belskaya, G. N., 2020. [Acupuncture in the prevention and treatment of stroke: A review of foreign studies (Russian)]. Voprosy Kurortologii, Fizioterapii, i Lechebnoi Fizicheskoi Kultury , 97(2), pp. 68-77. [DOI:10.17116/kurort20209702168] [PMID]
Brady, M. C., et al., 2016. Speech and language therapy for aphasia following stroke. The Cochrane Database of Systematic Reviews, 2016(6), pp. CD000425. [DOI:10.1002/14651858.CD000425.pub4] [PMID]
Cai, H., et al., 2015. Tongue acupuncture in treatment of post-stroke dysphagia. International Journal of Clinical and Experimental Medicine, 8(8), pp. 14090-4. [PMID]
Calandra-Buonaura, G., et al., 2021. Dysphagia in multiple system atrophy consensus statement on diagnosis, prognosis and treatment. Parkinsonism & Related Disorders, 86, pp. 124-32. [DOI:10.1016/j.parkreldis.2021.03.027] [PMID]
Chan, S. L., et al., 2012. Therapeutic effects of acupuncture for neurogenic dysphagia-a randomized controlled trial. Journal of Traditional Chinese Medicine, 32(1), pp. 25-30. [DOI:10.1016/S0254-6272(12)60027-2] [PMID]
Chan, Y. T., et al., 2020. Acupuncture for poststroke dysphagia: A pilot, nonrandomized, self-controlled trial. Evidence-Based Complementary and Alternative Medicine: eCAM, 2020, pp. 4689296. [DOI:10.1155/2020/4689296] [PMID] [PMCID]
Chavez, L. M., et al., 2017. Mechanisms of acupuncture therapy in ischemic stroke rehabilitation: A literature review of basic studies. International Journal of Molecular Sciences, 18(11), pp. 2270. [DOI:10.3390/ijms18112270] [PMID] [PMCID]
Chen, Y. W., et al., 2016. The effects of surface neuromuscular electrical stimulation on post-stroke dysphagia: A systemic review and meta-analysis. Clinical Rehabilitation, 30(1), pp. 24-35. [DOI:10.1177/0269215515571681] [PMID]
Deng, M., et al., 2016. Acupuncture for amnestic mild cognitive impairment: A meta-analysis of randomised controlled trials. Acupuncture in Medicine: Journal of the British Medical Acupuncture Society, 34(5), 342–348. [DOI:10.1136/acupmed-2015-010989] [PMID]
Deng, D., et al. 2016.“Changes in regional brain homogeneity induced by electro-acupuncture stimulation at the baihui acupoint in healthy subjects: A functional magnetic resonance imaging study.”Journal of Alternative and Complementary Medicine vol. 22,10 (2016): 794-799. [DOI:10.1089/acm.2015.0286] [PMID]
Feng, S., Cao, S., Du, S., Yin, T., Mai, F., Chen, X., & Su, X. (2016). [Acuuncture combined with swallowing training for post-stroke dysphagia: A randomized controlled trial (Chinease)]. Chinese Acupuncture & Moxibustion, 36(4), 347–350. [PMID]
Geeganage, C., et al., 2012. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database of Systematic Reviews, 10, pp. CD000323. [DOI:10.1002/14651858.CD000323.pub2] [PMID]
Guillén-Solà, A., et al., 2017. Respiratory muscle strength training and neuromuscular electrical stimulation in subacute dysphagic stroke patients: A randomized controlled trial. Clinical Rehabilitation, 31(6), pp. 761-71. [DOI:10.1177/0269215516652446] [PMID]
Huang, K. L., et al., 2014. Functional outcome in acute stroke patients with oropharyngeal dysphagia after swallowing therapy. Journal of Stroke and Cerebrovascular Diseases, 23(10), pp. 2547-53. [DOI:10.1016/j.jstrokecerebrovasdis.2014.05.031] [PMID]
Jia, B., et al., 2015. The effects of acupuncture at real or sham acupoints on the intrinsic brain activity in mild cognitive impairment patients. Evidence-Based Complementary and Alternative Medicine, 2015, pp. 529675. [DOI:10.1155/2015/529675] [PMID] [PMCID]
Jiang, H., et al., 2022. Manual acupuncture or combination of rehabilitation therapy to treat poststroke dysphagia: A systematic review and meta-analysis of randomized controlled trials. Evidence-Based Complementary and Alternative Medicine, 2022, pp. 8803507. [DOI:10.1155/2022/8803507] [PMID] [PMCID]
Juan, W., et al., 2016. Value of applying water swallowing test for patients with dysphagia after acute stroke. Journal of Shanghai Jiaotong, 36(07), pp. 1049. [DOI:10.3969/j.issn.1674-8115.2016.07.018]
Lancaster, J., 2015. Dysphagia: Its nature, assessment and management. British Journal of Community Nursing, Suppl Nutrition, pp. S28–32. [DOI:10.12968/bjcn.2015.20.Sup6a.S28] [PMID]
Li, L.X., et al., 2018. Acupuncture treatment for post-stroke dysphagia: An update meta-analysis of randomized controlled trials. Chinese Journal of Integrative Medicine, 24(9), pp. 686-95. [DOI:10.1007/s11655-018-3005-3] [PMID]
Li, X. & Wang, Q., 2013. Acupuncture therapy for stroke patients. International Review of Neurobiology, 111, pp. 159-79. [DOI:10.1016/B978-0-12-411545-3.00008-0] [PMID]
Lim, K.B., et al., 2014. Effect of low-frequency rTMS and NMES on subacute unilateral hemispheric stroke with dysphagia. Annals of Rehabilitation Medicine, 38(5), 592–602. [DOI:10.5535/arm.2014.38.5.592] [PMID] [PMCID]
Long, Y.B. & Wu, X.P., 2012. A meta-analysis of the efficacy of acupuncture in treating dysphagia in patients with a stroke. Acupuncture in Medicine, 30(4), pp. 291-7. [DOI:10.1136/acupmed-2012-010155] [PMID]
Marin, S., et al., 2018. Cost of oropharyngeal dysphagia after stroke: Protocol for a systematic review. BMJ Open, 8(12), pp. e022775. [DOI:10.1136/bmjopen-2018-022775] [PMID] [PMCID]
Meng, D., et al., 2016. Clinical literature study of acupuncture and moxibustion in the treatment of post stroke dysphagia based on meta-analysis. Chinese Medicine Modern Distance Education of China, 16(64), 148-153. [Link]
Meng, P. P., et al., 2020. The occurrence rate of swallowing disorders after stroke patients in Asia: A PRISMA-compliant systematic review and meta-analysis. Journal of Stroke and Cerebrovascular Diseases, 29(10), pp.105113. [DOI:10.1016/j.jstrokecerebrovasdis.2020.105113] [PMID]
Namasivayam-MacDonald, A.M. & Shune, S.E., 2018. The burden of dysphagia on family caregivers of the elderly: A systematic review. Geriatrics, 3(2), pp. 30. [DOI:10.3390/geriatrics3020030] [PMID] [PMCID]
Olesen, M. D., et al., 2021. Prevalence of signs of dysphagia and associated risk factors in geriatric patients admitted to an acute medical unit. Clinical Nutrition ESPEN, 41, pp. 208-16. [DOI:10.1016/j.clnesp.2020.12.020] [PMID]
Page, M. J., et al., 2021. The PRISMA 2020 Statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, pp. 105906. [PMID]
Park, J. S., et al., 2016. Effects of neuromuscular electrical stimulation combined with effortful swallowing on post-stroke oropharyngeal dysphagia: A randomised controlled trial. Journal of Oral Rehabilitation, 43(6), 426–434. [DOI:10.1111/joor.12390] [PMID]
Park, J. S., et al., 2016. Effects of expiratory muscle strength training on oropharyngeal dysphagia in subacute stroke patients: A randomised controlled trial. Journal of Oral Rehabilitation 43(5):364-72. [DOI:10.1111/joor.12382] [PMID]
Song, Y.P., Yang, W., Guo, H.M. and Han, Y.Y., 2006. [Clinical observation on acupuncture combined with medicine for treatment of infantile febrile convulsion (Chinese)]. Chinese Acupuncture & Moxibustion, 26(8), pp.561-562. [PMID]
Speyer, R., et al., 2022. Behavioural interventions in people with oropharyngeal dysphagia: A systematic review and meta-analysis of randomised clinical trials. Journal of Clinical Medicine, 11(3), pp. 685. [DOI:10.3390/jcm11030685] [PMID] [PMCID]
Sterne, J. A. C., et al., 2019. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed.), 366, pp. l4898. [DOI:10.1136/bmj.l4898] [PMID]
Teuschl, Y., et al., 2018. Systematic dysphagia screening and dietary modifications to reduce stroke-associated pneumonia rates in a stroke-unit. Plos One, 13(2), pp. e0192142. [DOI:10.1371/journal.pone.0192142] [PMID] [PMCID]
Waters, A. M., et al., 2022. Investigating dysphagia in adults: Symptoms and tests.” BMJ (Clinical research ed.), 379, pp. e067347. [DOI:10.1136/bmj-2021-067347] [PMID]
Wen, X., et al., 2023. The effect of repetitive transcranial magnetic stimulation in synchronization with effortful swallowing on post-stroke dysphagia. Dysphagia, 38(3), pp. 912–22. [DOI:10.1007/s00455-022-10515-4] [PMID]
World Health Organization. & Regional Office for the Western Pacific., 2007. WHO international standard terminologies on traditional medicine in the Western Pacific Region. Manila: WHO Regional Office for the Western Pacific. [Link]
Wu, W. B., 2019. Relieving throat and opening orifice acupuncture therapy for the post-stroke dysphagia. World Journal of Acupuncture-Moxibustion, 29(1), pp. 37-41. [DOI:10.1016/j.wjam.2019.04.004]
Xia, W., Zheng, C., Zhu, S., & Tang, Z. (2016). Does the addition of specific acupuncture to standard swallowing training improve outcomes in patients with dysphagia after stroke? a randomized controlled trial. Clinical Rehabilitation, 30(3), 237-246. [DOI:10.1177/0269215515578698]
Ye, Q., et al., 2019. Effect of electro-acupuncture on regulating the swallowing by activating the interneuron in ventrolateral medulla (VLM). Brain Research Bulletin, 144, pp. 132-9. [DOI:10.1016/j.brainresbull.2018.11.021] [PMID]
Ye, Q., et al., 2017. Systematic review on acupuncture for treatment of dysphagia after stroke. Evidence-Based Complementary and Alternative Medicine, 2017, pp. 6421852. [DOI:10.1155/2017/6421852] [PMID] [PMCID]
You, H., et al., 2018. Role of 5-HT1A in the nucleus of the solitary tract in the regulation of swallowing activities evoked by electroacupuncture in anesthetized rats. Neuroscience Letters, 687, 308-312. [DOI: 10.1016/j.neulet.2018.06.018]
Yu, H., et al., 2018. Modulation of spectral power and functional connectivity in human brain by acupuncture stimulation. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 26(5), pp. 977-86. [DOI:10.1109/TNSRE.2018.2828143] [PMID]
Zhang, J. H., Wang, D. & Liu, M., 2014. Overview of systematic reviews and meta-analyses of acupuncture for stroke. Neuroepidemiology, 42(1), pp. 50-8. [DOI:10.1159/000355435] [PMID]
Zeng, Y., Bao, Y., Zhu, M., Chen, S., & Fang, J. (2015). [Mild cognitive impairment of stroke at subacute stage treated with acupuncture: A randomized controlled trial (Chinease)]. Chinese Acupuncture & Moxibustion, 35(10), 979–982.
Type of Study: Research |
Subject:
General
Received: 2023/01/18 | Accepted: 2023/04/15 | Published: 2023/08/24
Received: 2023/01/18 | Accepted: 2023/04/15 | Published: 2023/08/24
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



