Fri, Sep 19, 2025
[Archive]
Volume 10, Issue 1 (Winter 2024)
JCCNC 2024, 10(1): 65-74 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Muqdad Idan M, Khudhair A K S, Haghani S, Najafi Ghezeljeh T. Investigating the Knowledge, Attitude, and Practice of Iraqi Intensive Care Nursing Staff Regarding Hand Hygiene. JCCNC 2024; 10 (1) :65-74
URL: http://jccnc.iums.ac.ir/article-1-464-en.html
URL: http://jccnc.iums.ac.ir/article-1-464-en.html
1- School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- College of Nursing, University of Basrah, Basrah, Iraq.
3- Nursing and Midwifery Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- Cardiovascular Nursing Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran.
2- College of Nursing, University of Basrah, Basrah, Iraq.
3- Nursing and Midwifery Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- Cardiovascular Nursing Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 589 kb]
(604 Downloads)
| Abstract (HTML) (2598 Views)
● Hand hygiene serves as a critical first line of defense in reducing hospital-acquired infections.
● A lack of knowledge and an unfavorable level of attitude and practice about hand hygiene were observed among the ICU nurses.
● Female nurses demonstrated higher knowledge compared to male nurses.
● Nurses with a bachelor’s degree in nursing exhibited more positive attitudes and practices about hand hygiene compared to those with school nursing degrees and diplomas.
● A significant association was found between nurses’ attitudes and practices about hand hygiene and their years of practical experience in the ICU.
● A lack of knowledge and an unfavorable level of attitude and practice about hand hygiene were observed among the ICU nurses.
● Female nurses demonstrated higher knowledge compared to male nurses.
● Nurses with a bachelor’s degree in nursing exhibited more positive attitudes and practices about hand hygiene compared to those with school nursing degrees and diplomas.
● A significant association was found between nurses’ attitudes and practices about hand hygiene and their years of practical experience in the ICU.
Plain Language Summary
Hand hygiene serves as a critical first line of defense in reducing hospital-acquired infections and is paramount for infection control. This study determined the knowledge, attitudes, and practices of nurses in the ICUs of Basrah Hospital and Dhi Qar Hospital in Iraq regarding hand hygiene. The findings indicated that ICU nurses exhibit a deficiency in knowledge, an unfavorable attitude, and poor adherence to hand hygiene practices.
Full-Text: (779 Views)
Introduction
Hospital-acquired infections pose a significant concern for patients’ health and safety (Clack et al., 2017). They rank among the most common adverse events in healthcare, placing considerable strain on the core priorities of each hospital (Goodarzi et al., 2020). These infections represent a critical global public health issue (Sarani et al., 2016). According to the World Health Organization (WHO) estimates, approximately 15% of hospitalized patients are affected by such infections (WHO, 2010). The incidence rates vary, with high-income countries experiencing rates from 3.5% to 12%, and middle to low-income countries witnessing rates between 5.7% and 19.1% (Wang et al., 2018). Hospital-acquired infections have serious implications, leading to prolonged hospitalizations, increased antibiotic resistance, higher mortality rates, and escalated treatment expenses for patients and the healthcare system (Kwon et al., 2015). Intensive care units (ICUs) have a higher prevalence of hospital-acquired infections compared to other hospital settings (Albughbish et al., 2016). Healthcare workers play a critical role in supporting high-risk patients in ICUs to reduce their risk of such infections (Alsubaie et al., 2013). Hand hygiene is a fundamental factor in preventing the spread of healthcare-associated infectious diseases, as microorganisms are primarily transmitted in the hospital environment through the hands of healthcare workers (Wetzker et al., 2016); accordingly, proper hand hygiene is the most effective method to prevent hospital-acquired infections in healthcare settings (Hosseinialhashemi et al., 2015).
Nurses are in direct contact with patients; therefore, they may inadvertently transmit infections through daily care activities and the use of medical tools (Khan, 2021). Several factors contribute to nurses’ inconsistent hand-washing practices, including the characteristics of ICU patients, heavy workloads, nursing shortages, and inadequate resources (Fouad & Elther, 2020). Various issues, such as the lack of hand-washing sinks, limited time for hand hygiene, patients’ underlying conditions, and inadequate knowledge of hand hygiene standards result in low adherence to proper hand hygiene (Tan et al., 2020). Some nurses prefer using gloves rather than washing their hands, leading to potential cross-contamination when gloves are improperly discarded after use (Gunasekara et al., 2009).
Evaluating nurses’ hand hygiene knowledge, attitude, and practice is crucial to improving infection control. Previous studies among ICU nurses in Iran and Saudi Arabia showed varying levels of knowledge and positive perceptions of hand hygiene (Aledeilah et al., 2018). However, limited research has been conducted in Iraq on this topic, and existing studies have used instruments that lack adequate validity and reliability for assessment (Abduawahid & Mahmood, 2020). ICU nursing staff operate in a demanding and intricate sector of nursing. In Iraq’s healthcare system, baccalaureate, technical, and skilled nurses are all considered graduate-trained nurses and work collaboratively. Evaluating the knowledge, attitude, and practice of nursing staff regarding hand hygiene is crucial as it plays a pivotal role in preventing nosocomial infections. To improve nurses’ knowledge, attitude, and practice in hand hygiene, it is essential to assess the current situation and develop an effective plan. This study aimed to determine the knowledge, attitude, and practice of nursing personnel in ICUs of the hospitals in Basrah and Dhi-Qar in Iraq, where limited research has been conducted. This study can serve as a valuable foundation for future research endeavors, aimed at enhancing the knowledge, attitude, and practice of intensive care nurses in the field of hand hygiene.
Materials and Methods
Study design, setting, and sample
This was a descriptive cross-sectional study. In this study, knowledge, attitudes, and practice regarding hand hygiene among ICU nursing staff in governmental (teaching and non-teaching) hospitals of Al-Basra and Dhi-Qar cities in Iraq were investigated. In this study, all ICU nursing staff in governmental hospitals (teaching and non-teaching) of both cities were recruited through census, and all nursing staff working in the ICUs affiliated with Basra Hospital (Al-Basra Teaching Hospital, Al-Sadr Teaching Hospital, Al-Mawani Teaching Hospital, Al-Fayha Teaching Hospital, Al-Qurna General Hospital, Al-Mudaina General Hospital) and Nasiriyah hospitals (Nasiriyah Teaching Hospital, Nasiriyah Heart Center) participated in the study. In total, 231 nurses were included in the study. All nursing staff who were willing to participate in the research and were directly involved in patient care in the mentioned governmental hospitals of Al-Basra and Dhi-Qar cities, Iraq, were recruited for participation. However, head nurses who did not provide direct care for patients were excluded.
The data were collected from August to September 2022, employing various questionnaires, including a demographic form, nurses’ hand hygiene knowledge questionnaire, nurses’ hand hygiene attitude questionnaire, and nurses’ hand hygiene practice questionnaire. The data collection process utilized online electronic questionnaires created through Google Forms and distributed via social media, specifically WhatsApp. The researchers obtained the nurses’ cell phone numbers and formed WhatsApp groups for effective communication. The online electronic questionnaires were disseminated through WhatsApp groups, attracting participation from all eligible participants. The researcher further clarified the study’s procedure and objectives in person to ensure clarity and understanding among the participants.
Study instruments
Demographic form
The demographic form included various items, encompassing age, gender, marital status, level of education, nursing work experience, work experience in the ICU, working hours per week, and history of participation in an in-service training program related to controlling nosocomial infections within the past year.
Nurses’ hand hygiene knowledge questionnaire
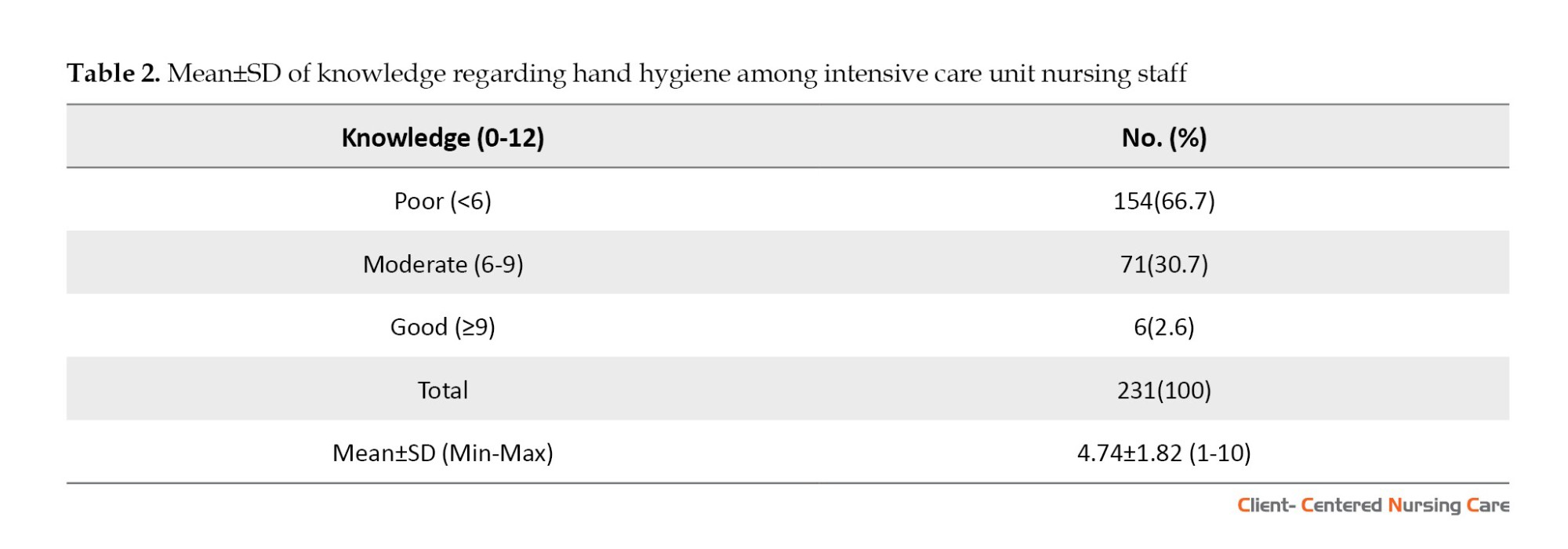
The questionnaire was developed by Van de Mortel in 2009. It evaluates nurses’ knowledge about hand hygiene through 12 four-choice questions. Each correct answer was given a score of one, while incorrect answers received a score of zero, resulting in a knowledge score range of 0 to 12. A higher score indicated a greater level of knowledge among nurses regarding hand hygiene. The Cronbach α coefficient is reported at 0.83, demonstrating acceptable internal consistency (Van de Mortel in 2009). Nursing staff determined their knowledge about hand hygiene by choosing the appropriate options. A score of more than 75% was considered good knowledge, 50%-74% was rendered moderate, and less than 50% was poor knowledge.
To translate the nurses’ hand hygiene knowledge questionnaire, the translation-retranslation method was employed. Initially, a translator familiar with medical concepts translated the text into Arabic. Subsequently, another translator, a bilingual specialist, translated the text from Arabic to English without the knowledge of the original questionnaire. Subsequently, the researcher and their supervisor compared the translated Arabic and English texts with the main questionnaire to ensure the accuracy of concepts and wording. The content validity of this translated questionnaire was reviewed by a panel of experts comprising three faculty members from the School of Nursing and Midwifery of University of Basrah, Iraq. In the present study, the Kuder Richardson 21 method was used to calculate the internal consistency of the questionnaire, yielding a value of 0.72.
Nurses’ hand hygiene attitude questionnaire
The attitude questionnaire regarding hand hygiene comprised 22 items. Nurses indicated their attitude toward hand hygiene using a 5-point Likert scale (I strongly disagree=1, I disagree=2, I am not sure=3, I agree=4, I strongly agree=5). The scores ranged from 22 to 110, with higher mean scores indicating a more favorable attitude toward hand hygiene. For specific items (5, 8, 10, 16, 17, 18, 19, and 20) in the nurses’ hand hygiene attitude questionnaire, the scoring is inverse, meaning a grade of 5 is considered complete disagreement and a score of 1 is intended for agreeing. A score of more than 75% is considered positive and indicative of a favorable attitude. The Cronbach α coefficient was reported at 0.87, indicating that the internal consistency of the questionnaire was appropriate (Van de Mortel in 2009).
To translate the nurses’ hand hygiene attitude questionnaire, the translation-back translation method was used. Initially, a translator familiar with the medical concepts translated the text into Arabic. Subsequently, another translator (a bilingual specialist) translated the text from Arabic to English without the knowledge of the original version. The researchers compared the translated Arabic and English texts with the main questionnaire to ensure the accuracy of concepts and wording. The content validity of the Arabic version of the questionnaire was assessed by a panel of experts comprising three faculty members from University of Basrah’s School of Nursing and Midwifery. The Cronbach α coefficient was calculated for the studied samples to determine the internal consistency of the questionnaire, yielding a value of 0.79.
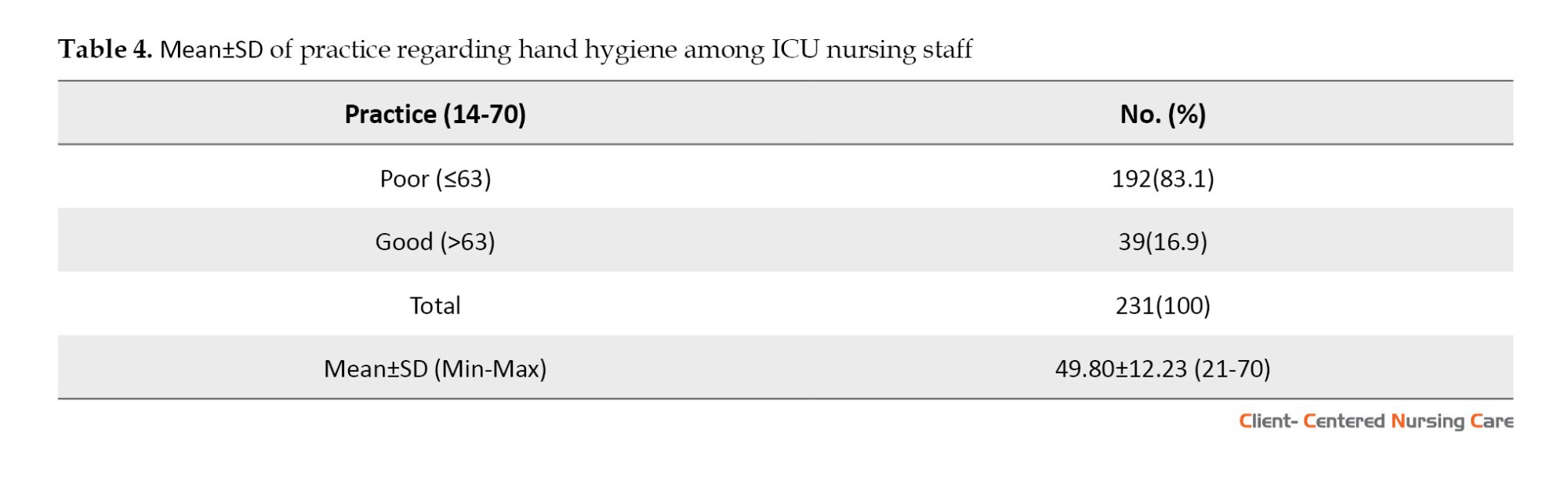
Nurses’ hand hygiene practice questionnaire
The practice questionnaire consisted of 14 items, and the nurses showed their practice on hand hygiene on a 5-point Likert scale (never=1, sometimes=2, half of the time=3, most of the time=4, always=5). The scores ranged from 14 to 70, and higher mean scores indicated better practice of hand hygiene (Van de Mortel in 2009). In this study, the translation-retranslation method was used to translate the transliteration practice questionnaire. To describe the samples, it was considered sufficient and desirable for nurses and staff to have answered 90% or more of the questions correctly. In a study on nursing staff, the Cronbach α coefficient was reported at 0.91 (Van de Mortel in 2009). The nursing staff was asked to complete the questionnaire. For this purpose, at first, a translator who was familiar with medical concepts translated the text into Arabic. Another translator (a bilingual specialist) then translated the text from Arabic to English. This translator was unaware of the original questionnaire. The translated Arabic and English texts were compared with the text of the main questionnaire and finalized for validity evaluation. The content validity of this questionnaire was reviewed by a panel of experts, consisting of three faculty members of the School of Nursing and Midwifery of University of Basrah. In the present study, the Cronbach α coefficient was calculated for the studied samples to determine the internal consistency of the questionnaire, yielding a value of 0.92.
Study procedure
The questionnaires were administered using Google Forms, which were distributed on social media platforms. Before data collection, all study subjects provided written informed consent. They were thoroughly briefed on the data collection method and study procedures during an in-person meeting. Subsequently, the nurses’ cell phone numbers were obtained to form a WhatsApp group, facilitating efficient communication. The questionnaires were delivered through this WhatsApp group, and regular weekly reminders were sent to prompt the nurses to complete them. The data collection process spanned four months.
After collecting the data from Google Forms, the information was exported to Excel software, and then transferred to SPSS software, version 22 for analysis. Descriptive statistics (absolute and relative frequency, Mean±SD) were used to summarize the data. Furthermore, inferential statistics (independent t-test, chi-square test, and Fisher test) were applied to achieve the research objectives. The Kolmogorov-Smirnov test was utilized to assess the normality of variables. Data analysis was conducted using the SPSS software, version 22. A significance level of <0.05 was considered for all statistical tests.
Results
In this study, 231 questionnaires were distributed in 8 selected hospitals in Al-Basra and Dhi-Qar cities. Table 1 shows that the age of the majority of participants (66.7%) was <30 years. Concerning gender, more than half of the sample (52.8%) was female, and more than half of them (50.2%) were married. More than half of the samples (59.3%) had a bachelor’s degree, and 52.5% of them had <5 years of practical experience in nursing. Meanwhile, more than half of the samples (72.7%) had practical experience in ICU. The results revealed that 88.8% of the participants worked 50 h or less per week. Finally, Table 1 shows that 54.1% of the samples participated in an in-service training program. In addition, Table 1 shows a significant relationship between hand hygiene knowledge and gender. Female nurses’ knowledge (4.98±1.92) was higher compared to males (4.48±1.68) (P=0.03). Also, there was a significant association between nurses’ attitudes and practices regarding hand hygiene and education level (P<0.001). Attitudes and practices regarding hand hygiene were higher among nurses who had a bachelor’s degree in nursing compared to others (P<0.001). There was a significant association between nurses’ attitudes toward hand hygiene and years of practical experience in the ICU (P=0.006). The mean score of attitude toward hand hygiene was lower among nurses with 5 to 10 years of experience in the ICU compared to those with less than 5 years of practical experience (P=0.015). Moreover, a significant association was found between nurses’ hand hygiene practices and their years of practical experience in the ICU (P=0.03). The results indicated that the mean score of hand hygiene practice was lower among nurses with more than 10 years of experience in the ICU than those with less than 5 years of practical experience (P=0.028) (Table 1).

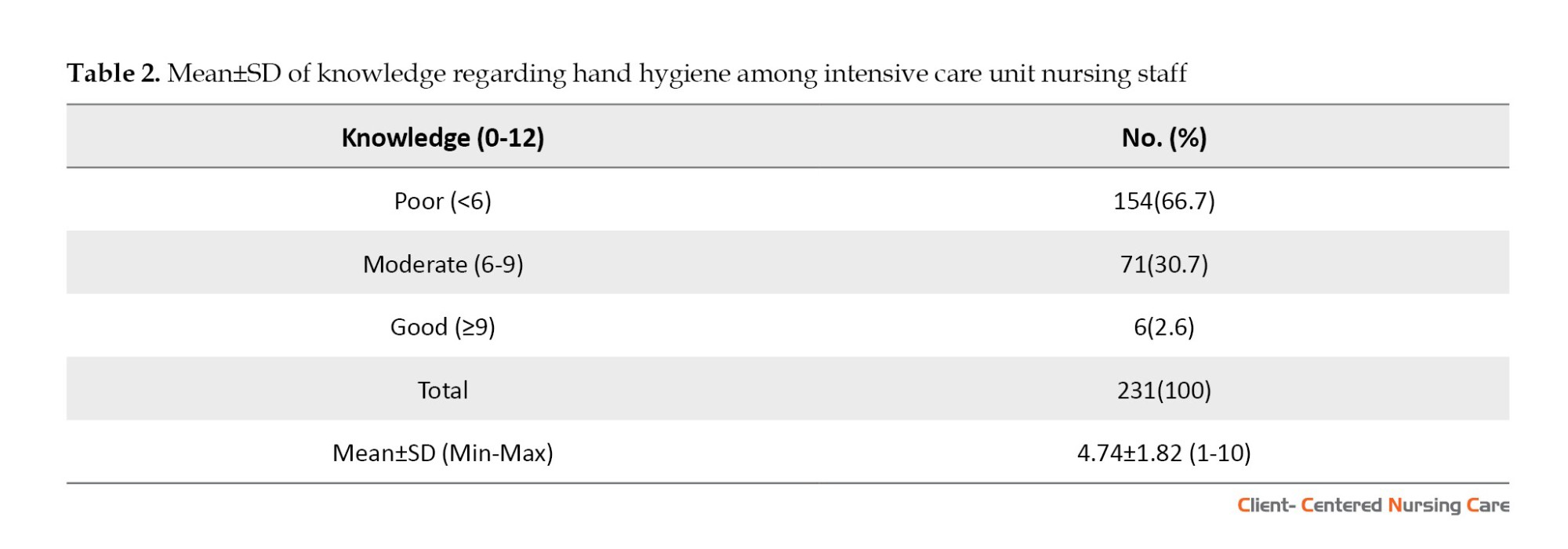
Table 2 illustrates that most nurses (66.7%) had poor knowledge.
According to Table 3, most nurses (74%) had unfavorable attitudes.
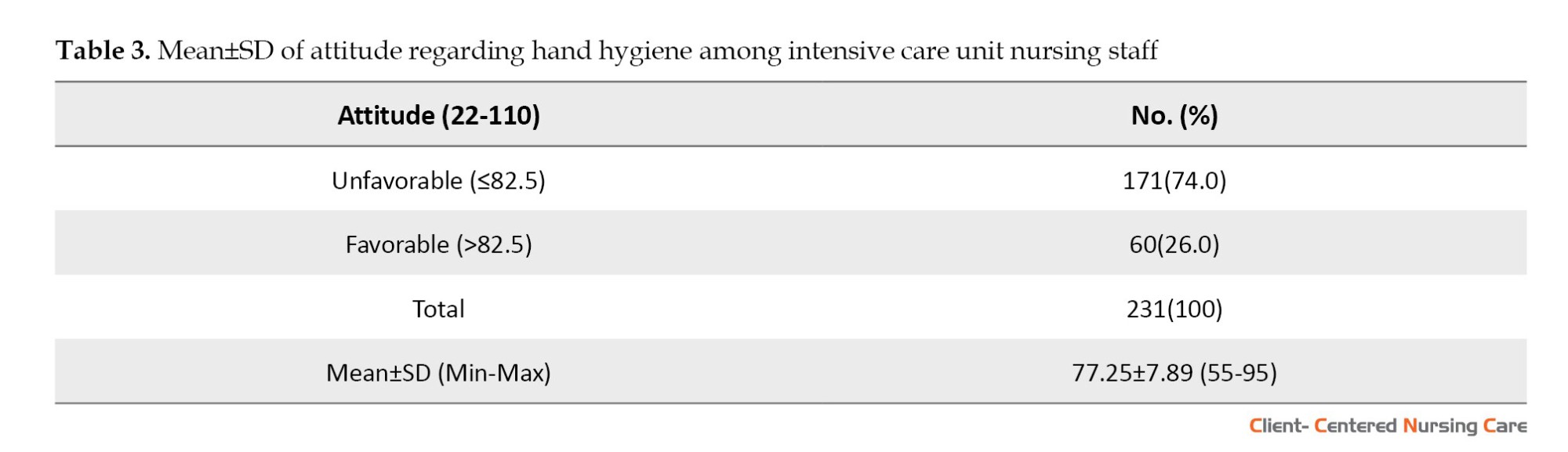
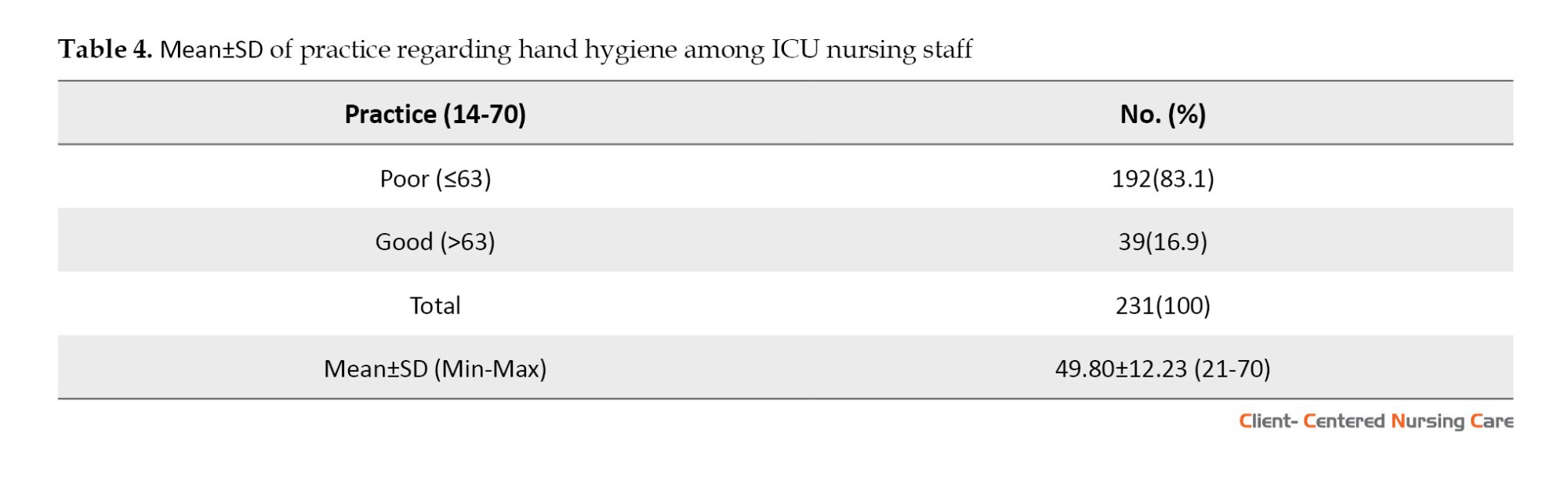
Table 4 indicated that most nurses (83.1%) had poor practice.
Discussion
The study was conducted to determine the knowledge, attitudes, and behaviors of ICU nursing staff in hospitals of Basrah City and Dhi- Qar City, in Iraq.
The results showed that the overall knowledge of the majority of the subjects about hand hygiene was low. The lack of previous training on hand hygiene for almost half of the subjects may explain the poor knowledge levels. Additionally, hospitals in Iraq lack educational interventions on hand hygiene, contributing to the issue. The study highlighted that more than half of the nurses had not received any training programs on hand hygiene, and even those who attended had low scores, due to inadequate quality, frequency, and time intervals between their in-service training. The authorities should prioritize providing in-service education about hand hygiene and nosocomial infections, focusing on the quality and methods of education and the frequency of updating nurses’ knowledge. Infection supervisors can also play a vital role in training, assessing, and evaluating nurses’ knowledge in this area. Frequent infection rounds and evaluations can help enhance nurses’ awareness and knowledge about hand hygiene.
These findings are in line with previous research conducted by Najafi Ghezeljeh et al. (2015) in Iran, which also explored nurses’ knowledge of hand hygiene. In a study conducted in Pakistan by Zil-E-Ali et al. (2017), it was found that less than half of the respondents had an acceptable level of knowledge about hand hygiene, a result similar to the study of Dutta et al. (2020), who reported that half of the participants had poor knowledge about hand hygiene, with nearly half of them lacking any hand hygiene training. In contrast to the findings of the present study, Ango et al. (2017), Aledeilah et al., (2018), Deepak et al. (2020), and Arthi et al. (2016) found that the majority of the participants had a high level of knowledge of hand hygiene. Also, in a study, almost all employees were aware of the seven steps to proper hand washing (Hammerschmidt & Manser, 2019).
Moreover, the current study reveals that female nurses possess better hand hygiene knowledge compared to their male counterparts. This gender-based difference in hand hygiene knowledge among Iraqi nurses calls for further investigation to identify its possible underlying causes. This could be attributed to cultural norms or a more targeted and focused education approach for female nurses within the Iraqi context. These results echo the findings of Zil-E-Ali et al. (2017), who also reported significant gender differences in nursing knowledge about hand hygiene, with female nurses demonstrating greater knowledge in this area. This emphasizes the need for continued research and attention to improve hand hygiene practices among all nurses, while also researching to clarify the potential gender-specific differences in knowledge about hand hygiene.
According to the findings, a significant number of Iraqi ICU nurses displayed an unfavorable attitude toward hand hygiene. This unfavorable attitude can be attributed to their low knowledge about hand hygiene, which leads to a lack of awareness regarding its importance in preventing infections in hospitals. Consequently, this lack of awareness appears to have a direct impact on their attitudes. However, nurses must recognize hand hygiene as a critical patient safety indicator. This result is consistent with a descriptive cross-sectional study conducted by Arthi et al. (2016) in India, which also indicated unfavorable attitudes toward hand hygiene among general nursing staff. Furthermore, similar findings were reported in a study conducted among nursing staff in hospitals in Kuwait by Al-Wazzan et al. (2011), which also identified weaknesses in attitudes toward hand hygiene. In contrast, the current finding contradicts the results of Ango et al. (2017), Aledeilah et al., (2018), and Hammerschmidt & Manser, (2019), whose studies found that the majority of healthcare providers exhibited a positive attitude toward hand hygiene.
The study revealed a significant relationship between the educational level and nursing attitudes toward hand hygiene, with nurses holding a bachelor’s degree displaying a more favorable attitude. Additionally, the results demonstrated that nurses with less than 5 years of practical experience in the ICU exhibited a more favorable attitude toward hand hygiene compared to those with 5-10 years of experience. These findings underscore the importance of university education, as well as high-quality and effective in-service education, in fostering and maintaining favorable attitudes toward hand hygiene among ICU nurses. However, the observed differences in hand hygiene attitudes based on practical experiences in the ICU among Iraqi nurses call for further investigation. It is essential to explore the factors contributing to this variation to gain a deeper understanding of how practical experience in the ICU may influence nurses’ attitudes toward hand hygiene.
According to the findings, ICU nurses’ practice of hand hygiene was poor, which can be attributed to their low knowledge and unfavorable attitude toward hand hygiene. Several factors contribute to this poor practice, including the demanding nature of their work, such as high workload and time constraints. Additionally, inadequate in-service training, lack of proper infrastructure for hand hygiene implementation, and insufficient or inefficient surveillance systems and nursing leadership also play a role. As nurses, protecting patients from harm is one of their ethical and professional obligations (Zil-E-Ali et al. 2017).
These results align with previous studies, such as those conducted by Arthi et al. (2016) and Deepak et al. (2020), which also reported the majority of nurses exhibiting poor hand hygiene practices. However, Aledeilah et al., (2018) reported a moderate level of hand hygiene practice among participants in their study.
The study’s findings revealed that nurses with a bachelor’s degree in nursing demonstrated better hand hygiene practices. This suggests that university education plays a significant role in influencing nursing practices regarding hand hygiene, leading to improved adherence to hand hygiene protocols. Furthermore, the results indicated that nurses with 5 years of experience had better hand hygiene practices compared to those with more than 10 years of experience in the ICU. This difference warrants further investigation to identify the reasons behind the higher hand hygiene practices among the 5-year experience group compared to the other groups. The overall findings underscore the importance of university education and the implementation of high-quality and efficient in-service education for promoting and maintaining appropriate hand hygiene practices among ICU nurses in Iraq. These educational initiatives are crucial in fostering a culture of effective hand hygiene, which ultimately contributes to better patient care and safety.
Conclusion
Based on the results, the nursing staff in this study had a lack of knowledge and an unfavorable level of attitude and practice. The study’s findings highlight the need for interventions to improve knowledge and awareness about hand hygiene among ICU nurses in Iraq, which could ultimately lead to more favorable attitudes and better adherence to hand hygiene practices, consequently enhancing patient safety in hospitals. Nurses’ knowledge and current skill sets in critical care units should be updated through high-quality and efficient in-service programs. To provide high-quality and safe nursing care, knowledge, attitude and practice of hand hygiene should be considered as part of the routine evaluation of ICU nurses. It is also suggested to consider more education time at nursing schools to train nursing staff about this important subject, in addition to evaluating and revising the educational programs for other nursing staff.
The findings of this study cannot be universally applied to all of Iraq due to its restriction to a specific section of the country. Consequently, further research of a similar nature is necessary in other regions to draw more comprehensive conclusions.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Iran University of Medical Sciences (IUMS) (Code: IR.IUMS.REC.1401.649). The required permissions were obtained from the Faculty of Nursing and Midwifery of IUMS the Director of Basrah a Dhi-Qar and the Health Department. The study’s objectives and voluntary participation of subjects were explained to all participants. All participants provided written informed consent.
Funding
This article is part of the research project approved by the Research Department of the International Campus at IUMS, Tehran-Iran in 2022.
Authors' contributions
Study design and data analysis: Tahereh Najafi Ghezeljeh, Maha Muqdad Idan, Shima Haghani; Initial draft: Tahereh Najafi Ghezeljeh, Maha Muqdad Idan, Abdul Kareem Salman Khudhair; Figures and tables: Tahereh Najafi Ghezeljeh, Maha Muqdad Idan; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers express their gratitude to the officials and nurses of Al-Sadr Teaching Hospital, Basrah General Hospital, Al-Mawani Teaching Hospital, Al-Fayhaa Teaching Hospital, Al-Madinah Hospital, Qurna Hospital, Nasiriyah Teaching Hospital, and Nasiriyah Heart Center.
References
Mahmood, N. R., Abdul, M. K. & Hassan, A. J., 2020. Awareness, knowledge, and attitude of hand hygiene practices among healthcare workers in Kirkuk pediatric hospital. Middle East Journal of Family Medicine, 18(2), pp. 42-6. [DOI:10.5742/MEWFM.2020.93765]
Albughbish, M., Nisi, A. & Borvayeh, H., 2016. [Hand hygiene compliance among ICU health workers in Golestan hospital in 2013 (Persian)]. Jundishapur Scientific Medical Journal, 15(3), pp. 355-62. [Link]
Aledeilah, R. D. I., et al., 2018. Assessment of knowledge, attitude, and practice of hand hygiene among health care workers in Arar City, Saudi Arabia. The Egyptian Journal of Hospital Medicine, 70(3), pp. 491-8. [DOI:10.12816/0043494]
Al-Wazzan, B., et al., 2011 Hand hygiene practices among nursing staff in public secondary care hospitals in Kuwait: Self-report and direct observation. Medical Principles and Practice, 20(4), pp. 326-31. [DOI:10.1159/000324545] [PMID]
Alsubaie, S., et al., 2019. Middle east respiratory syndrome coronavirus epidemic impact on healthcare workers’ risk perceptions, work, and personal lives. Journal of Infection in Developing Countries, 13(10), pp. 920–6. [DOI:10.3855/jidc.11753] [PMID]
Ango, U. M., et al., 2017. Knowledge, attitude and practice of hand hygiene among healthcare providers in semi-urban communities of Sokoto State, Nigeria. International Journal of Tropical Disease& Health, 26(2), pp. 1-9. [Link]
Arthi, G., Park, J. H. & Jung, H. Y., 2016. Existence and exponential stability for neutral stochastic integrodifferential equations with impulses driven by a fractional Brownian motion. Communications in Nonlinear Science and Numerical Simulation, 32, pp. 145-57. [DOI:10.1016/j.cnsns.2015.08.014]
Clack, L., et al., 2017. “First-person view” of pathogen transmission and hand hygiene-use of new head-mounted video capture and coding tool. Antimicrobial Resistance & Infection Control, 6, pp. 108. [DOI:10.1186/s13756-017-0267-z] [PMID]
Deepak, S. S. F., et al., 2020. Hand hygiene knowledge, attitude, practice, and hand microflora analysis of staff nurses in a Rural Tertiary care hospital. Journal of Family Medicine and Primary Care, 9(9), pp. 4969–73. [DOI:10.4103/jfmpc.jfmpc_773_20] [PMID]
Dutta, G., Singh, T. G. & Kumar, T., 2020. Knowledge and practice of hand hygiene among undergraduate students and junior doctors in the Regional Institute of Medical Sciences, Imphal. Journal of Family Medicine and Primary Care, 9(9), pp. 4741–6. [DOI:10.4103/jfmpc.jfmpc_794_20] [PMID]
Fouad, M. & Eltaher, S., 2020. Hand hygiene initiative: A comparative study of pre-and post-intervention outcomes. Eastern Mediterranean Health Journal, 26(2), pp. 198–205. [DOI:10.26719/2020.26.2.198] [PMID]
Goodarzi, Z., et al., 2020. Investigating the knowledge, attitude, and perception of hand hygiene of nursing employees working in Intensive Care Units of Iran University of Medical Sciences, 2018-2019. Medica, 15(2), pp. 230–7. [PMID]
Gunasekara, T., et al., 2009. Bacterial contamination of anesthetists’ hands, personal mobile phones, and wristwatches used during theatre sessions. Sri Lankan Journal of Anaesthesiology, 17(1), pp. 11-5. [Link]
Hammerschmidt, J. & Manser, T., 2019. Nurses’ knowledge, behaviour and compliance concerning hand hygiene in nursing homes: A cross-sectional mixed-methods study. BMC Health Services Research, 19(1), pp. 547. [DOI:10.1186/s12913-019-4347-z] [PMID]
Hosseinialhashemi, M., et al. 2015. Knowledge, attitudes, and practices of health care personnel concerning hand hygiene in Shiraz University of Medical Sciences hospitals, 2013-2014. American Journal of Infection Control, 43(9), pp. 1009–11.[DOI:10.1016/j.ajic.2015.05.002] [PMID]
Khan, M. H., et al., 2021. Knowledge, attitude, and practice toward handwashing among undergraduate nursing students in Lahore. Saudi Journal of Nursing and Health Care, 4, pp. 158-63. [Link]
Kwon, J. H., Olsen, M. A. & Dubberke, E. R., 2015. The morbidity, mortality, and costs associated with Clostridium difficile infection. Infectious Disease Clinics of North America, 29(1), pp. 123–34. [DOI:10.1016/j.idc.2014.11.003] [PMID]
Najafi Ghezeljeh, T., et al., 2015. [Nurses’ knowledge, beliefs, and practices towards hand hygiene (Persian)]. Hayat Journal, 21(1), pp. 79-93. [Link]
World Health Organization., 2010. The burden of healthcare-associated infection worldwide. Geneva: World Health Organization. [Link]
Sarani, H., et al., 2015. Knowledge, attitude, and practice of nurses about standard precautions for hospital-acquired infection in teaching hospitals affiliated to Zabol University of Medical Sciences (2014). Global Journal of Health Science, 8(3), pp. 193–8. [DOI:10.5539/gjhs.v8n3p193] [PMID]
Tan, J. B. X., et al., 2020. Hand rubbing with sprayed alcohol-based hand rub: An alternative method for effective hand hygiene. The Journal of Hospital Infection, 104(4), pp. 430–4.[DOI:10.1016/j.jhin.2020.02.008] [PMID]
Wang, J., et al., 2018. The prevalence of healthcare-associated infections in Mainland China: A systematic review and meta-analysis. Infection Control & Hospital Epidemiology, 39(6), pp. 701–9.[DOI:10.1017/ice.2018.60] [PMID]
Van De Mortel T., 2009. Development of a questionnaire to assess health care students’ hand hygiene knowledge, beliefs and practices. Australian Journal of Advanced Nursing, 26(3), pp. 9-16. [Link]
Wetzker, W., et al., 2016. Compliance with hand hygiene : Reference data from the national hand hygiene campaign in Germany. The Journal of Hospital Infection, 92(4), pp. 328–31. [DOI:10.1016/j.jhin.2016.01.022] [PMID]
Zil-E-Ali, A., et al., 2017. A survey of handwashing knowledge and attitudes among the healthcare professionals in Lahore, Pakistan. Cureus, 9(3), pp. e1089. [DOI:10.7759/cureus.1089]
Hospital-acquired infections pose a significant concern for patients’ health and safety (Clack et al., 2017). They rank among the most common adverse events in healthcare, placing considerable strain on the core priorities of each hospital (Goodarzi et al., 2020). These infections represent a critical global public health issue (Sarani et al., 2016). According to the World Health Organization (WHO) estimates, approximately 15% of hospitalized patients are affected by such infections (WHO, 2010). The incidence rates vary, with high-income countries experiencing rates from 3.5% to 12%, and middle to low-income countries witnessing rates between 5.7% and 19.1% (Wang et al., 2018). Hospital-acquired infections have serious implications, leading to prolonged hospitalizations, increased antibiotic resistance, higher mortality rates, and escalated treatment expenses for patients and the healthcare system (Kwon et al., 2015). Intensive care units (ICUs) have a higher prevalence of hospital-acquired infections compared to other hospital settings (Albughbish et al., 2016). Healthcare workers play a critical role in supporting high-risk patients in ICUs to reduce their risk of such infections (Alsubaie et al., 2013). Hand hygiene is a fundamental factor in preventing the spread of healthcare-associated infectious diseases, as microorganisms are primarily transmitted in the hospital environment through the hands of healthcare workers (Wetzker et al., 2016); accordingly, proper hand hygiene is the most effective method to prevent hospital-acquired infections in healthcare settings (Hosseinialhashemi et al., 2015).
Nurses are in direct contact with patients; therefore, they may inadvertently transmit infections through daily care activities and the use of medical tools (Khan, 2021). Several factors contribute to nurses’ inconsistent hand-washing practices, including the characteristics of ICU patients, heavy workloads, nursing shortages, and inadequate resources (Fouad & Elther, 2020). Various issues, such as the lack of hand-washing sinks, limited time for hand hygiene, patients’ underlying conditions, and inadequate knowledge of hand hygiene standards result in low adherence to proper hand hygiene (Tan et al., 2020). Some nurses prefer using gloves rather than washing their hands, leading to potential cross-contamination when gloves are improperly discarded after use (Gunasekara et al., 2009).
Evaluating nurses’ hand hygiene knowledge, attitude, and practice is crucial to improving infection control. Previous studies among ICU nurses in Iran and Saudi Arabia showed varying levels of knowledge and positive perceptions of hand hygiene (Aledeilah et al., 2018). However, limited research has been conducted in Iraq on this topic, and existing studies have used instruments that lack adequate validity and reliability for assessment (Abduawahid & Mahmood, 2020). ICU nursing staff operate in a demanding and intricate sector of nursing. In Iraq’s healthcare system, baccalaureate, technical, and skilled nurses are all considered graduate-trained nurses and work collaboratively. Evaluating the knowledge, attitude, and practice of nursing staff regarding hand hygiene is crucial as it plays a pivotal role in preventing nosocomial infections. To improve nurses’ knowledge, attitude, and practice in hand hygiene, it is essential to assess the current situation and develop an effective plan. This study aimed to determine the knowledge, attitude, and practice of nursing personnel in ICUs of the hospitals in Basrah and Dhi-Qar in Iraq, where limited research has been conducted. This study can serve as a valuable foundation for future research endeavors, aimed at enhancing the knowledge, attitude, and practice of intensive care nurses in the field of hand hygiene.
Materials and Methods
Study design, setting, and sample
This was a descriptive cross-sectional study. In this study, knowledge, attitudes, and practice regarding hand hygiene among ICU nursing staff in governmental (teaching and non-teaching) hospitals of Al-Basra and Dhi-Qar cities in Iraq were investigated. In this study, all ICU nursing staff in governmental hospitals (teaching and non-teaching) of both cities were recruited through census, and all nursing staff working in the ICUs affiliated with Basra Hospital (Al-Basra Teaching Hospital, Al-Sadr Teaching Hospital, Al-Mawani Teaching Hospital, Al-Fayha Teaching Hospital, Al-Qurna General Hospital, Al-Mudaina General Hospital) and Nasiriyah hospitals (Nasiriyah Teaching Hospital, Nasiriyah Heart Center) participated in the study. In total, 231 nurses were included in the study. All nursing staff who were willing to participate in the research and were directly involved in patient care in the mentioned governmental hospitals of Al-Basra and Dhi-Qar cities, Iraq, were recruited for participation. However, head nurses who did not provide direct care for patients were excluded.
The data were collected from August to September 2022, employing various questionnaires, including a demographic form, nurses’ hand hygiene knowledge questionnaire, nurses’ hand hygiene attitude questionnaire, and nurses’ hand hygiene practice questionnaire. The data collection process utilized online electronic questionnaires created through Google Forms and distributed via social media, specifically WhatsApp. The researchers obtained the nurses’ cell phone numbers and formed WhatsApp groups for effective communication. The online electronic questionnaires were disseminated through WhatsApp groups, attracting participation from all eligible participants. The researcher further clarified the study’s procedure and objectives in person to ensure clarity and understanding among the participants.
Study instruments
Demographic form
The demographic form included various items, encompassing age, gender, marital status, level of education, nursing work experience, work experience in the ICU, working hours per week, and history of participation in an in-service training program related to controlling nosocomial infections within the past year.
Nurses’ hand hygiene knowledge questionnaire
The questionnaire was developed by Van de Mortel in 2009. It evaluates nurses’ knowledge about hand hygiene through 12 four-choice questions. Each correct answer was given a score of one, while incorrect answers received a score of zero, resulting in a knowledge score range of 0 to 12. A higher score indicated a greater level of knowledge among nurses regarding hand hygiene. The Cronbach α coefficient is reported at 0.83, demonstrating acceptable internal consistency (Van de Mortel in 2009). Nursing staff determined their knowledge about hand hygiene by choosing the appropriate options. A score of more than 75% was considered good knowledge, 50%-74% was rendered moderate, and less than 50% was poor knowledge.
To translate the nurses’ hand hygiene knowledge questionnaire, the translation-retranslation method was employed. Initially, a translator familiar with medical concepts translated the text into Arabic. Subsequently, another translator, a bilingual specialist, translated the text from Arabic to English without the knowledge of the original questionnaire. Subsequently, the researcher and their supervisor compared the translated Arabic and English texts with the main questionnaire to ensure the accuracy of concepts and wording. The content validity of this translated questionnaire was reviewed by a panel of experts comprising three faculty members from the School of Nursing and Midwifery of University of Basrah, Iraq. In the present study, the Kuder Richardson 21 method was used to calculate the internal consistency of the questionnaire, yielding a value of 0.72.
Nurses’ hand hygiene attitude questionnaire
The attitude questionnaire regarding hand hygiene comprised 22 items. Nurses indicated their attitude toward hand hygiene using a 5-point Likert scale (I strongly disagree=1, I disagree=2, I am not sure=3, I agree=4, I strongly agree=5). The scores ranged from 22 to 110, with higher mean scores indicating a more favorable attitude toward hand hygiene. For specific items (5, 8, 10, 16, 17, 18, 19, and 20) in the nurses’ hand hygiene attitude questionnaire, the scoring is inverse, meaning a grade of 5 is considered complete disagreement and a score of 1 is intended for agreeing. A score of more than 75% is considered positive and indicative of a favorable attitude. The Cronbach α coefficient was reported at 0.87, indicating that the internal consistency of the questionnaire was appropriate (Van de Mortel in 2009).
To translate the nurses’ hand hygiene attitude questionnaire, the translation-back translation method was used. Initially, a translator familiar with the medical concepts translated the text into Arabic. Subsequently, another translator (a bilingual specialist) translated the text from Arabic to English without the knowledge of the original version. The researchers compared the translated Arabic and English texts with the main questionnaire to ensure the accuracy of concepts and wording. The content validity of the Arabic version of the questionnaire was assessed by a panel of experts comprising three faculty members from University of Basrah’s School of Nursing and Midwifery. The Cronbach α coefficient was calculated for the studied samples to determine the internal consistency of the questionnaire, yielding a value of 0.79.
Nurses’ hand hygiene practice questionnaire
The practice questionnaire consisted of 14 items, and the nurses showed their practice on hand hygiene on a 5-point Likert scale (never=1, sometimes=2, half of the time=3, most of the time=4, always=5). The scores ranged from 14 to 70, and higher mean scores indicated better practice of hand hygiene (Van de Mortel in 2009). In this study, the translation-retranslation method was used to translate the transliteration practice questionnaire. To describe the samples, it was considered sufficient and desirable for nurses and staff to have answered 90% or more of the questions correctly. In a study on nursing staff, the Cronbach α coefficient was reported at 0.91 (Van de Mortel in 2009). The nursing staff was asked to complete the questionnaire. For this purpose, at first, a translator who was familiar with medical concepts translated the text into Arabic. Another translator (a bilingual specialist) then translated the text from Arabic to English. This translator was unaware of the original questionnaire. The translated Arabic and English texts were compared with the text of the main questionnaire and finalized for validity evaluation. The content validity of this questionnaire was reviewed by a panel of experts, consisting of three faculty members of the School of Nursing and Midwifery of University of Basrah. In the present study, the Cronbach α coefficient was calculated for the studied samples to determine the internal consistency of the questionnaire, yielding a value of 0.92.
Study procedure
The questionnaires were administered using Google Forms, which were distributed on social media platforms. Before data collection, all study subjects provided written informed consent. They were thoroughly briefed on the data collection method and study procedures during an in-person meeting. Subsequently, the nurses’ cell phone numbers were obtained to form a WhatsApp group, facilitating efficient communication. The questionnaires were delivered through this WhatsApp group, and regular weekly reminders were sent to prompt the nurses to complete them. The data collection process spanned four months.
After collecting the data from Google Forms, the information was exported to Excel software, and then transferred to SPSS software, version 22 for analysis. Descriptive statistics (absolute and relative frequency, Mean±SD) were used to summarize the data. Furthermore, inferential statistics (independent t-test, chi-square test, and Fisher test) were applied to achieve the research objectives. The Kolmogorov-Smirnov test was utilized to assess the normality of variables. Data analysis was conducted using the SPSS software, version 22. A significance level of <0.05 was considered for all statistical tests.
Results
In this study, 231 questionnaires were distributed in 8 selected hospitals in Al-Basra and Dhi-Qar cities. Table 1 shows that the age of the majority of participants (66.7%) was <30 years. Concerning gender, more than half of the sample (52.8%) was female, and more than half of them (50.2%) were married. More than half of the samples (59.3%) had a bachelor’s degree, and 52.5% of them had <5 years of practical experience in nursing. Meanwhile, more than half of the samples (72.7%) had practical experience in ICU. The results revealed that 88.8% of the participants worked 50 h or less per week. Finally, Table 1 shows that 54.1% of the samples participated in an in-service training program. In addition, Table 1 shows a significant relationship between hand hygiene knowledge and gender. Female nurses’ knowledge (4.98±1.92) was higher compared to males (4.48±1.68) (P=0.03). Also, there was a significant association between nurses’ attitudes and practices regarding hand hygiene and education level (P<0.001). Attitudes and practices regarding hand hygiene were higher among nurses who had a bachelor’s degree in nursing compared to others (P<0.001). There was a significant association between nurses’ attitudes toward hand hygiene and years of practical experience in the ICU (P=0.006). The mean score of attitude toward hand hygiene was lower among nurses with 5 to 10 years of experience in the ICU compared to those with less than 5 years of practical experience (P=0.015). Moreover, a significant association was found between nurses’ hand hygiene practices and their years of practical experience in the ICU (P=0.03). The results indicated that the mean score of hand hygiene practice was lower among nurses with more than 10 years of experience in the ICU than those with less than 5 years of practical experience (P=0.028) (Table 1).

Table 2 illustrates that most nurses (66.7%) had poor knowledge.
According to Table 3, most nurses (74%) had unfavorable attitudes.
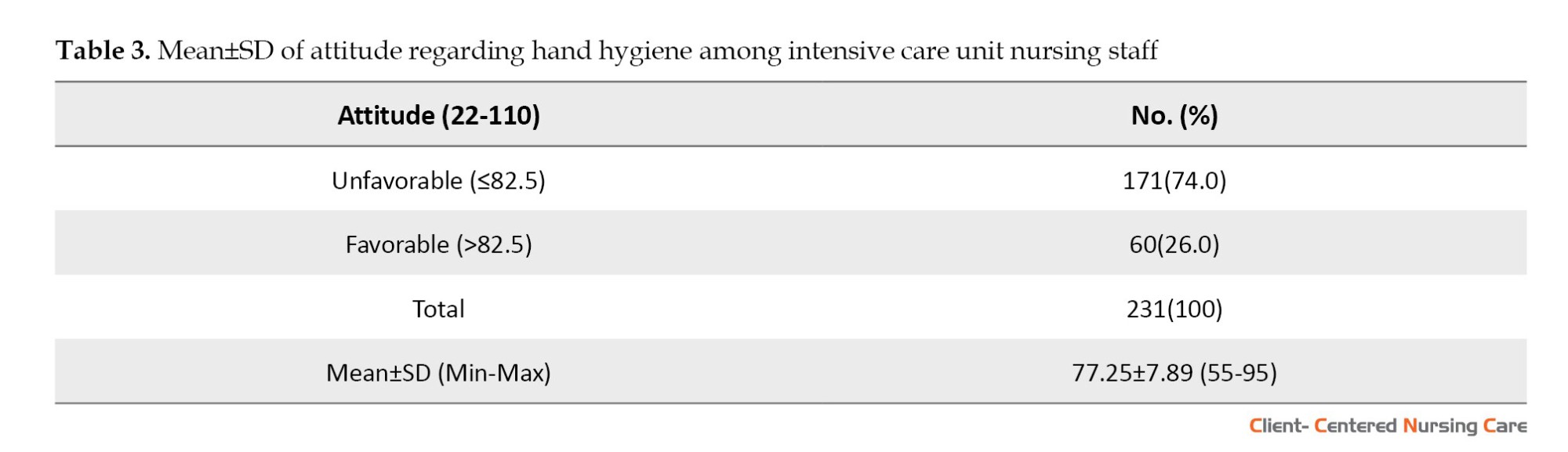
Table 4 indicated that most nurses (83.1%) had poor practice.
Discussion
The study was conducted to determine the knowledge, attitudes, and behaviors of ICU nursing staff in hospitals of Basrah City and Dhi- Qar City, in Iraq.
The results showed that the overall knowledge of the majority of the subjects about hand hygiene was low. The lack of previous training on hand hygiene for almost half of the subjects may explain the poor knowledge levels. Additionally, hospitals in Iraq lack educational interventions on hand hygiene, contributing to the issue. The study highlighted that more than half of the nurses had not received any training programs on hand hygiene, and even those who attended had low scores, due to inadequate quality, frequency, and time intervals between their in-service training. The authorities should prioritize providing in-service education about hand hygiene and nosocomial infections, focusing on the quality and methods of education and the frequency of updating nurses’ knowledge. Infection supervisors can also play a vital role in training, assessing, and evaluating nurses’ knowledge in this area. Frequent infection rounds and evaluations can help enhance nurses’ awareness and knowledge about hand hygiene.
These findings are in line with previous research conducted by Najafi Ghezeljeh et al. (2015) in Iran, which also explored nurses’ knowledge of hand hygiene. In a study conducted in Pakistan by Zil-E-Ali et al. (2017), it was found that less than half of the respondents had an acceptable level of knowledge about hand hygiene, a result similar to the study of Dutta et al. (2020), who reported that half of the participants had poor knowledge about hand hygiene, with nearly half of them lacking any hand hygiene training. In contrast to the findings of the present study, Ango et al. (2017), Aledeilah et al., (2018), Deepak et al. (2020), and Arthi et al. (2016) found that the majority of the participants had a high level of knowledge of hand hygiene. Also, in a study, almost all employees were aware of the seven steps to proper hand washing (Hammerschmidt & Manser, 2019).
Moreover, the current study reveals that female nurses possess better hand hygiene knowledge compared to their male counterparts. This gender-based difference in hand hygiene knowledge among Iraqi nurses calls for further investigation to identify its possible underlying causes. This could be attributed to cultural norms or a more targeted and focused education approach for female nurses within the Iraqi context. These results echo the findings of Zil-E-Ali et al. (2017), who also reported significant gender differences in nursing knowledge about hand hygiene, with female nurses demonstrating greater knowledge in this area. This emphasizes the need for continued research and attention to improve hand hygiene practices among all nurses, while also researching to clarify the potential gender-specific differences in knowledge about hand hygiene.
According to the findings, a significant number of Iraqi ICU nurses displayed an unfavorable attitude toward hand hygiene. This unfavorable attitude can be attributed to their low knowledge about hand hygiene, which leads to a lack of awareness regarding its importance in preventing infections in hospitals. Consequently, this lack of awareness appears to have a direct impact on their attitudes. However, nurses must recognize hand hygiene as a critical patient safety indicator. This result is consistent with a descriptive cross-sectional study conducted by Arthi et al. (2016) in India, which also indicated unfavorable attitudes toward hand hygiene among general nursing staff. Furthermore, similar findings were reported in a study conducted among nursing staff in hospitals in Kuwait by Al-Wazzan et al. (2011), which also identified weaknesses in attitudes toward hand hygiene. In contrast, the current finding contradicts the results of Ango et al. (2017), Aledeilah et al., (2018), and Hammerschmidt & Manser, (2019), whose studies found that the majority of healthcare providers exhibited a positive attitude toward hand hygiene.
The study revealed a significant relationship between the educational level and nursing attitudes toward hand hygiene, with nurses holding a bachelor’s degree displaying a more favorable attitude. Additionally, the results demonstrated that nurses with less than 5 years of practical experience in the ICU exhibited a more favorable attitude toward hand hygiene compared to those with 5-10 years of experience. These findings underscore the importance of university education, as well as high-quality and effective in-service education, in fostering and maintaining favorable attitudes toward hand hygiene among ICU nurses. However, the observed differences in hand hygiene attitudes based on practical experiences in the ICU among Iraqi nurses call for further investigation. It is essential to explore the factors contributing to this variation to gain a deeper understanding of how practical experience in the ICU may influence nurses’ attitudes toward hand hygiene.
According to the findings, ICU nurses’ practice of hand hygiene was poor, which can be attributed to their low knowledge and unfavorable attitude toward hand hygiene. Several factors contribute to this poor practice, including the demanding nature of their work, such as high workload and time constraints. Additionally, inadequate in-service training, lack of proper infrastructure for hand hygiene implementation, and insufficient or inefficient surveillance systems and nursing leadership also play a role. As nurses, protecting patients from harm is one of their ethical and professional obligations (Zil-E-Ali et al. 2017).
These results align with previous studies, such as those conducted by Arthi et al. (2016) and Deepak et al. (2020), which also reported the majority of nurses exhibiting poor hand hygiene practices. However, Aledeilah et al., (2018) reported a moderate level of hand hygiene practice among participants in their study.
The study’s findings revealed that nurses with a bachelor’s degree in nursing demonstrated better hand hygiene practices. This suggests that university education plays a significant role in influencing nursing practices regarding hand hygiene, leading to improved adherence to hand hygiene protocols. Furthermore, the results indicated that nurses with 5 years of experience had better hand hygiene practices compared to those with more than 10 years of experience in the ICU. This difference warrants further investigation to identify the reasons behind the higher hand hygiene practices among the 5-year experience group compared to the other groups. The overall findings underscore the importance of university education and the implementation of high-quality and efficient in-service education for promoting and maintaining appropriate hand hygiene practices among ICU nurses in Iraq. These educational initiatives are crucial in fostering a culture of effective hand hygiene, which ultimately contributes to better patient care and safety.
Conclusion
Based on the results, the nursing staff in this study had a lack of knowledge and an unfavorable level of attitude and practice. The study’s findings highlight the need for interventions to improve knowledge and awareness about hand hygiene among ICU nurses in Iraq, which could ultimately lead to more favorable attitudes and better adherence to hand hygiene practices, consequently enhancing patient safety in hospitals. Nurses’ knowledge and current skill sets in critical care units should be updated through high-quality and efficient in-service programs. To provide high-quality and safe nursing care, knowledge, attitude and practice of hand hygiene should be considered as part of the routine evaluation of ICU nurses. It is also suggested to consider more education time at nursing schools to train nursing staff about this important subject, in addition to evaluating and revising the educational programs for other nursing staff.
The findings of this study cannot be universally applied to all of Iraq due to its restriction to a specific section of the country. Consequently, further research of a similar nature is necessary in other regions to draw more comprehensive conclusions.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Iran University of Medical Sciences (IUMS) (Code: IR.IUMS.REC.1401.649). The required permissions were obtained from the Faculty of Nursing and Midwifery of IUMS the Director of Basrah a Dhi-Qar and the Health Department. The study’s objectives and voluntary participation of subjects were explained to all participants. All participants provided written informed consent.
Funding
This article is part of the research project approved by the Research Department of the International Campus at IUMS, Tehran-Iran in 2022.
Authors' contributions
Study design and data analysis: Tahereh Najafi Ghezeljeh, Maha Muqdad Idan, Shima Haghani; Initial draft: Tahereh Najafi Ghezeljeh, Maha Muqdad Idan, Abdul Kareem Salman Khudhair; Figures and tables: Tahereh Najafi Ghezeljeh, Maha Muqdad Idan; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers express their gratitude to the officials and nurses of Al-Sadr Teaching Hospital, Basrah General Hospital, Al-Mawani Teaching Hospital, Al-Fayhaa Teaching Hospital, Al-Madinah Hospital, Qurna Hospital, Nasiriyah Teaching Hospital, and Nasiriyah Heart Center.
References
Mahmood, N. R., Abdul, M. K. & Hassan, A. J., 2020. Awareness, knowledge, and attitude of hand hygiene practices among healthcare workers in Kirkuk pediatric hospital. Middle East Journal of Family Medicine, 18(2), pp. 42-6. [DOI:10.5742/MEWFM.2020.93765]
Albughbish, M., Nisi, A. & Borvayeh, H., 2016. [Hand hygiene compliance among ICU health workers in Golestan hospital in 2013 (Persian)]. Jundishapur Scientific Medical Journal, 15(3), pp. 355-62. [Link]
Aledeilah, R. D. I., et al., 2018. Assessment of knowledge, attitude, and practice of hand hygiene among health care workers in Arar City, Saudi Arabia. The Egyptian Journal of Hospital Medicine, 70(3), pp. 491-8. [DOI:10.12816/0043494]
Al-Wazzan, B., et al., 2011 Hand hygiene practices among nursing staff in public secondary care hospitals in Kuwait: Self-report and direct observation. Medical Principles and Practice, 20(4), pp. 326-31. [DOI:10.1159/000324545] [PMID]
Alsubaie, S., et al., 2019. Middle east respiratory syndrome coronavirus epidemic impact on healthcare workers’ risk perceptions, work, and personal lives. Journal of Infection in Developing Countries, 13(10), pp. 920–6. [DOI:10.3855/jidc.11753] [PMID]
Ango, U. M., et al., 2017. Knowledge, attitude and practice of hand hygiene among healthcare providers in semi-urban communities of Sokoto State, Nigeria. International Journal of Tropical Disease& Health, 26(2), pp. 1-9. [Link]
Arthi, G., Park, J. H. & Jung, H. Y., 2016. Existence and exponential stability for neutral stochastic integrodifferential equations with impulses driven by a fractional Brownian motion. Communications in Nonlinear Science and Numerical Simulation, 32, pp. 145-57. [DOI:10.1016/j.cnsns.2015.08.014]
Clack, L., et al., 2017. “First-person view” of pathogen transmission and hand hygiene-use of new head-mounted video capture and coding tool. Antimicrobial Resistance & Infection Control, 6, pp. 108. [DOI:10.1186/s13756-017-0267-z] [PMID]
Deepak, S. S. F., et al., 2020. Hand hygiene knowledge, attitude, practice, and hand microflora analysis of staff nurses in a Rural Tertiary care hospital. Journal of Family Medicine and Primary Care, 9(9), pp. 4969–73. [DOI:10.4103/jfmpc.jfmpc_773_20] [PMID]
Dutta, G., Singh, T. G. & Kumar, T., 2020. Knowledge and practice of hand hygiene among undergraduate students and junior doctors in the Regional Institute of Medical Sciences, Imphal. Journal of Family Medicine and Primary Care, 9(9), pp. 4741–6. [DOI:10.4103/jfmpc.jfmpc_794_20] [PMID]
Fouad, M. & Eltaher, S., 2020. Hand hygiene initiative: A comparative study of pre-and post-intervention outcomes. Eastern Mediterranean Health Journal, 26(2), pp. 198–205. [DOI:10.26719/2020.26.2.198] [PMID]
Goodarzi, Z., et al., 2020. Investigating the knowledge, attitude, and perception of hand hygiene of nursing employees working in Intensive Care Units of Iran University of Medical Sciences, 2018-2019. Medica, 15(2), pp. 230–7. [PMID]
Gunasekara, T., et al., 2009. Bacterial contamination of anesthetists’ hands, personal mobile phones, and wristwatches used during theatre sessions. Sri Lankan Journal of Anaesthesiology, 17(1), pp. 11-5. [Link]
Hammerschmidt, J. & Manser, T., 2019. Nurses’ knowledge, behaviour and compliance concerning hand hygiene in nursing homes: A cross-sectional mixed-methods study. BMC Health Services Research, 19(1), pp. 547. [DOI:10.1186/s12913-019-4347-z] [PMID]
Hosseinialhashemi, M., et al. 2015. Knowledge, attitudes, and practices of health care personnel concerning hand hygiene in Shiraz University of Medical Sciences hospitals, 2013-2014. American Journal of Infection Control, 43(9), pp. 1009–11.[DOI:10.1016/j.ajic.2015.05.002] [PMID]
Khan, M. H., et al., 2021. Knowledge, attitude, and practice toward handwashing among undergraduate nursing students in Lahore. Saudi Journal of Nursing and Health Care, 4, pp. 158-63. [Link]
Kwon, J. H., Olsen, M. A. & Dubberke, E. R., 2015. The morbidity, mortality, and costs associated with Clostridium difficile infection. Infectious Disease Clinics of North America, 29(1), pp. 123–34. [DOI:10.1016/j.idc.2014.11.003] [PMID]
Najafi Ghezeljeh, T., et al., 2015. [Nurses’ knowledge, beliefs, and practices towards hand hygiene (Persian)]. Hayat Journal, 21(1), pp. 79-93. [Link]
World Health Organization., 2010. The burden of healthcare-associated infection worldwide. Geneva: World Health Organization. [Link]
Sarani, H., et al., 2015. Knowledge, attitude, and practice of nurses about standard precautions for hospital-acquired infection in teaching hospitals affiliated to Zabol University of Medical Sciences (2014). Global Journal of Health Science, 8(3), pp. 193–8. [DOI:10.5539/gjhs.v8n3p193] [PMID]
Tan, J. B. X., et al., 2020. Hand rubbing with sprayed alcohol-based hand rub: An alternative method for effective hand hygiene. The Journal of Hospital Infection, 104(4), pp. 430–4.[DOI:10.1016/j.jhin.2020.02.008] [PMID]
Wang, J., et al., 2018. The prevalence of healthcare-associated infections in Mainland China: A systematic review and meta-analysis. Infection Control & Hospital Epidemiology, 39(6), pp. 701–9.[DOI:10.1017/ice.2018.60] [PMID]
Van De Mortel T., 2009. Development of a questionnaire to assess health care students’ hand hygiene knowledge, beliefs and practices. Australian Journal of Advanced Nursing, 26(3), pp. 9-16. [Link]
Wetzker, W., et al., 2016. Compliance with hand hygiene : Reference data from the national hand hygiene campaign in Germany. The Journal of Hospital Infection, 92(4), pp. 328–31. [DOI:10.1016/j.jhin.2016.01.022] [PMID]
Zil-E-Ali, A., et al., 2017. A survey of handwashing knowledge and attitudes among the healthcare professionals in Lahore, Pakistan. Cureus, 9(3), pp. e1089. [DOI:10.7759/cureus.1089]
Type of Study: Research |
Subject:
Special
Received: 2023/02/9 | Accepted: 2023/09/12 | Published: 2024/01/10
Received: 2023/02/9 | Accepted: 2023/09/12 | Published: 2024/01/10
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |