Tue, Jul 16, 2024
[Archive]
Volume 9, Issue 4 (Autumn 2023)
JCCNC 2023, 9(4): 243-254 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Karami B, Khodabakhshi-Koolaee A, Heidari H, Davoodi H. The Effectiveness of Solution-focused Narrative Therapy and Mindfulness-based Stress Reduction on the Level of Expressed Emotion in Mothers of Boys With Gross Motor Disabilities. JCCNC 2023; 9 (4) :243-254
URL: http://jccnc.iums.ac.ir/article-1-468-en.html
URL: http://jccnc.iums.ac.ir/article-1-468-en.html
1- Department of Counseling, Faculty of Humanities, Khomein Branch, Islamic Azad University, Khomein, Iran.
2- Department of Psychology & Educational Sciences, Faculty of Humanities, Khatam University, Tehran, Iran. ,a.khodabakhshid@khatam.ac.ir
2- Department of Psychology & Educational Sciences, Faculty of Humanities, Khatam University, Tehran, Iran. ,
Full-Text [PDF 712 kb]
(361 Downloads)
| Abstract (HTML) (1572 Views)
Mothers of children with gross motor disabilities experience objective and subjective care burdens, leading to highly expressed and negative emotions, such as hostility, severe criticism, and intolerance toward their children.
• Psychological interventions could reduce the intensely expressed emotion of mothers toward their children.
• This study examined the effects of solution-focused narrative therapy (SFNT) and mindfulness-based stress reduction on the expressed emotions of mothers of male children with gross motor disabilities.
• The results revealed that both treatments were effective, but SFNT was more effective in reducing the expressed emotions.
• It seems that SFNT and the efforts of mothers to redefine their life stories give them more strength and power to control their life conditions, explaining the superiority of SFNT.
Plain Language Summary
Mothers with highly expressed negative emotions, such as hostility and criticism toward their disabled children, experience higher psychological distress and lower quality of child-mother interactions. The present study determined that solution-focused narrative therapy (SFNT) and mindfulness-based stress reduction (MBSR) could decrease the expressed emotions of these mothers. However, SFNT had a greater effect than MBSR in reducing expressed emotion in mothers.
• Psychological interventions could reduce the intensely expressed emotion of mothers toward their children.
• This study examined the effects of solution-focused narrative therapy (SFNT) and mindfulness-based stress reduction on the expressed emotions of mothers of male children with gross motor disabilities.
• The results revealed that both treatments were effective, but SFNT was more effective in reducing the expressed emotions.
• It seems that SFNT and the efforts of mothers to redefine their life stories give them more strength and power to control their life conditions, explaining the superiority of SFNT.
Plain Language Summary
Mothers with highly expressed negative emotions, such as hostility and criticism toward their disabled children, experience higher psychological distress and lower quality of child-mother interactions. The present study determined that solution-focused narrative therapy (SFNT) and mindfulness-based stress reduction (MBSR) could decrease the expressed emotions of these mothers. However, SFNT had a greater effect than MBSR in reducing expressed emotion in mothers.
Full-Text: (133 Views)
1. Introduction
Caring for a disabled child in the family creates stress and disrupts the physical and mental health of the parents, especially mothers. Compared to fathers, mothers spend a substantial amount of time with their children and assume leadership roles in the family (Khodabakhshi-Koolaee & Derakhshandeh, 2015). Motor disabilities in children can lead to problems in doing daily activities. They face severe disabilities, such as poor eye-hand coordination. Thus, they often bump into things while moving, constantly fall, and have problems coordinating muscles to do their tasks. These problems hinder their progress in school assignments and disruption in daily activities. Gross motor disabilities develop due to genetic reasons, such as Down syndrome, neuromuscular disorders (e.g. muscular dystrophy or cerebral palsy); developmental reasons, such as autism; and hormonal causes, such as hypothyroidism (Morris & Bartlett, 2004).
Caregivers of disabled children, especially mothers, experience negative emotions and intense emotional conflicts with their disabled children. Vaughn & Leff (1976) introduced the expressed emotion (EE) scale. They found that close caregivers of patients with mental disorders, especially mothers, express negative emotions, such as violence and severe criticism towards the sick member of the family (Khoshgoftar et al., 2022). Hastings et al. (2006) reported that mothers of children with intellectual disabilities have negative emotions, such as criticism towards their children. These mothers experience depression and distress while caring for their children. Coleman (2010) showed that the emotions expressed by mothers of children with fragile X syndrome are accompanied by emotional involvement, hostility, and criticism toward their children.
Although mothers with disabled children experience intense stress and low quality of life, few psychological programs and interventions address their needs. Some psychological interventions for the family include cognitive-behavioral therapy interventions and psychological training (Romero-Gonzalez et al., 2018). Mindfulness-based stress reduction (MBSR) emerges as a practical approach for these parents to improving their physical and mental health (Benn et al., 2012). A study documented that the MBSR program can effectively reduce stress and improve the psychological well-being of parents of children with developmental disabilities (Bazzano et al., 2015).
The MBSR program was proposed by Kabat-Zinn (1990) at the University of Massachusetts Chan Medical School. MBSR, a client-centered therapy, employs structured intensive psychological training in many clinical environments, hospitals, and schools. Mindfulness techniques help people observe their consciousness impartially and without judgment, reducing stress and regulating emotions (Petcharat, 2018). A meta-analysis study concluded that mindfulness intervention could reduce parenting stress and be an effective treatment option to help parents (Burgdorf et al., 2019). Because of its flexibility, mindfulness-based therapy can be combined with other treatments. For example, a mindfulness yoga program (MiYoga) could help reduce the stress of parents of children with cerebral palsy (Mak et al., 2019).
Narrative therapy is a new solution-focused treatment combining narrative and solution-focused treatments. Solution-focused narrative therapy (SFNT) can help people with psychological stress cope with their problems. As the name suggests, narrative therapy means telling the story of our identity and its related meanings. Narrative therapy helps clients develop a new way of telling their story, different from the problematic path. The new story involves one’s hopes, values, and commitments. The therapist helps the client extensively draw paths, narratives, life events, opportunities, and possibilities (White & Morgan, 2006; Metcalf, 2017; Metcalf, 2021). Instead of focusing on the problems, the clients create a distance between themselves and the problems by highlighting the possible effects of the problems in their lives. Narrative therapy tries to separate the nature of the client from their problems. In this way, clients can discover their positive abilities and get a better and more straightforward narrative of the nature of their lives and themselves (Riley & Malchiodi, 2003; Chang & Nylund, 2013). SFNT aims to participate clients effectively and meaningfully in their life choices (Metcalf, 2017). It can give people the independence to redefine their lives and engage in their decisions. SFNT is a holistic model derived from two language-based therapies with a postmodern perspective. The therapist and client collaborate in creating a solution-focused narrative framework for rewriting the client’s life (Riley & Malchiodi, 2003; Chang & Nylund, 2013).
Previous studies have shown the effectiveness of SFNT for other clinical groups, including the quality of life of cancer patients (Perry, 2020) and the life of couples after marital infidelity (Saunders, 2020). Schwellnus et al. (2020) used solution-focused therapy to help children and adolescents with cerebral palsy disabilities set life goals. Their results show that, after completing the intervention, the participants can determine their life goals. Another study examined the impact of narrative therapy on children with developmental disabilities and their parents in India. The results support that parents and their children welcome the opportunities created to change and rewrite their life stories. The study also shows how narrative therapy can make a difference in the lives of children, their families, and the wider community (Baldiwala & Kanakia, 2022).
Mothers with disabled children experience many psychological and physical stresses due to long-term care of their children (Khodabakhshi-Koolaee et al., 2019). These stresses lead to psychological problems and decrease parent-child interaction quality due to negative emotions, such as criticism and violence. As detailed above, SFNT has been employed in other clinical groups, but its effectiveness has not been explored in mothers of boys with gross motor disabilities. This therapy is necessary because, during the treatment process, mothers modify their internalized stories, expect more about their destinies, and ultimately have better control over their lives (White & Morgan, 2006). Moreover, considering the higher prevalence and risk factors of developmental and gross motor delay among boys than girls (Soleimani et al., 2018; Veldman et al., 2020), it is crucial to compare the effectiveness of SFNT and MBSR on the level of EE in mothers of male children with gross motor disabilities.
2. Materials and Methods
Design, setting, and sample
This quasi-experimental study employed a pre-test-post-test design with a control group.
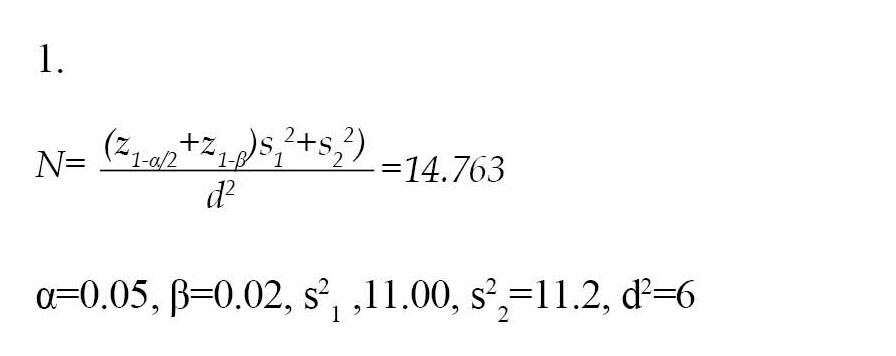
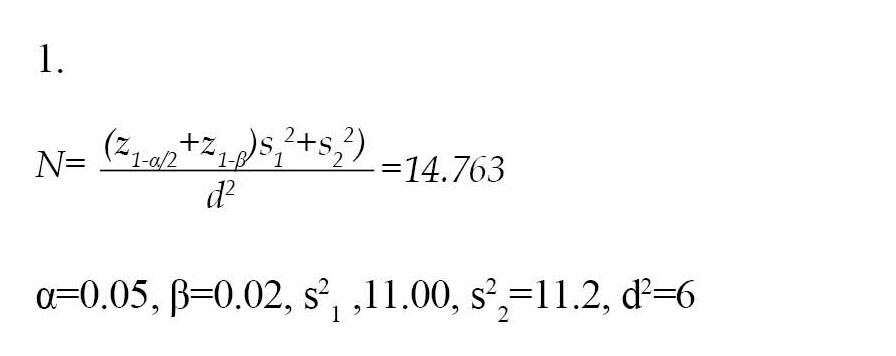
The sample size was estimated at 45 mothers based on the Equation 1:
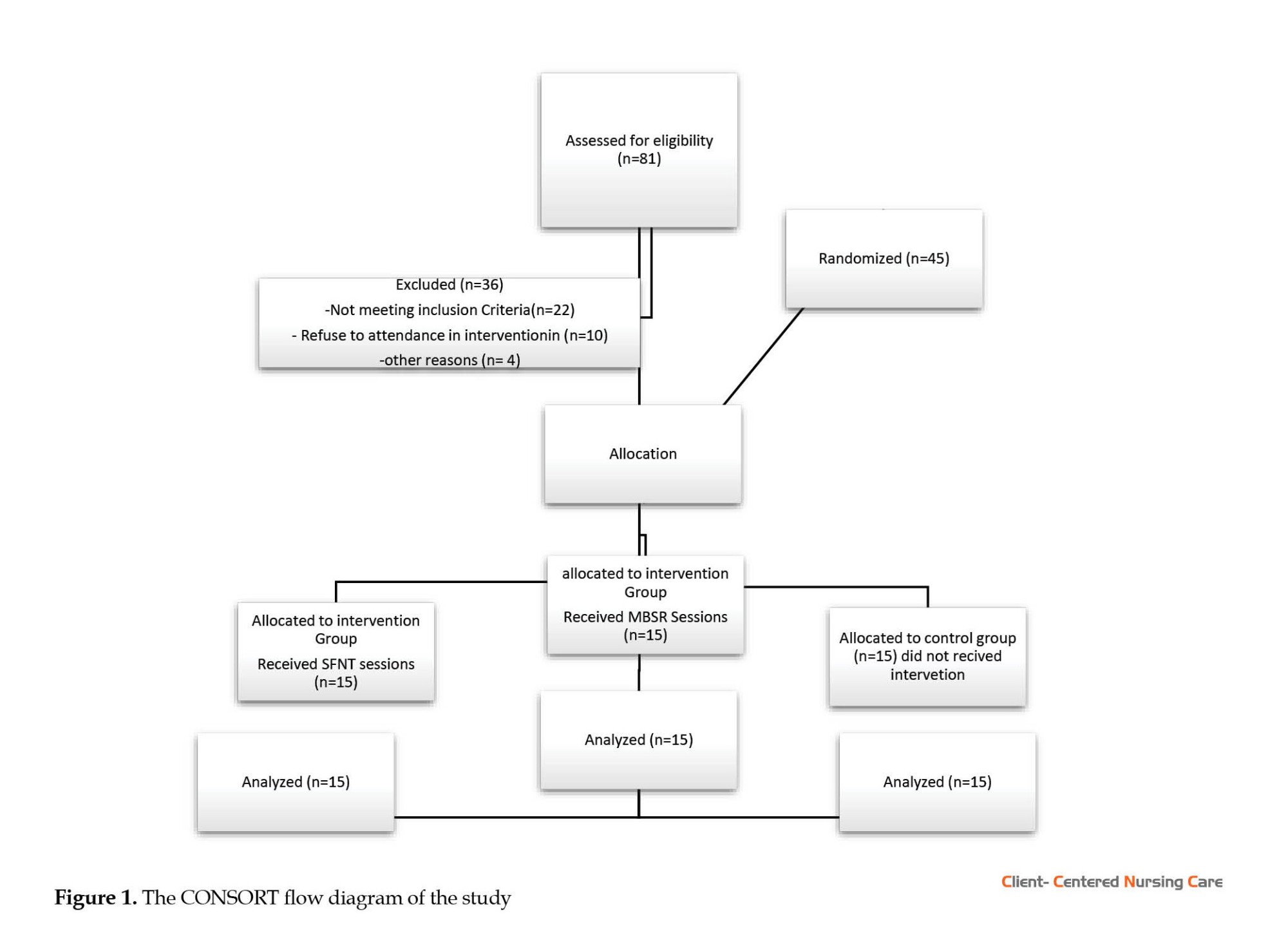
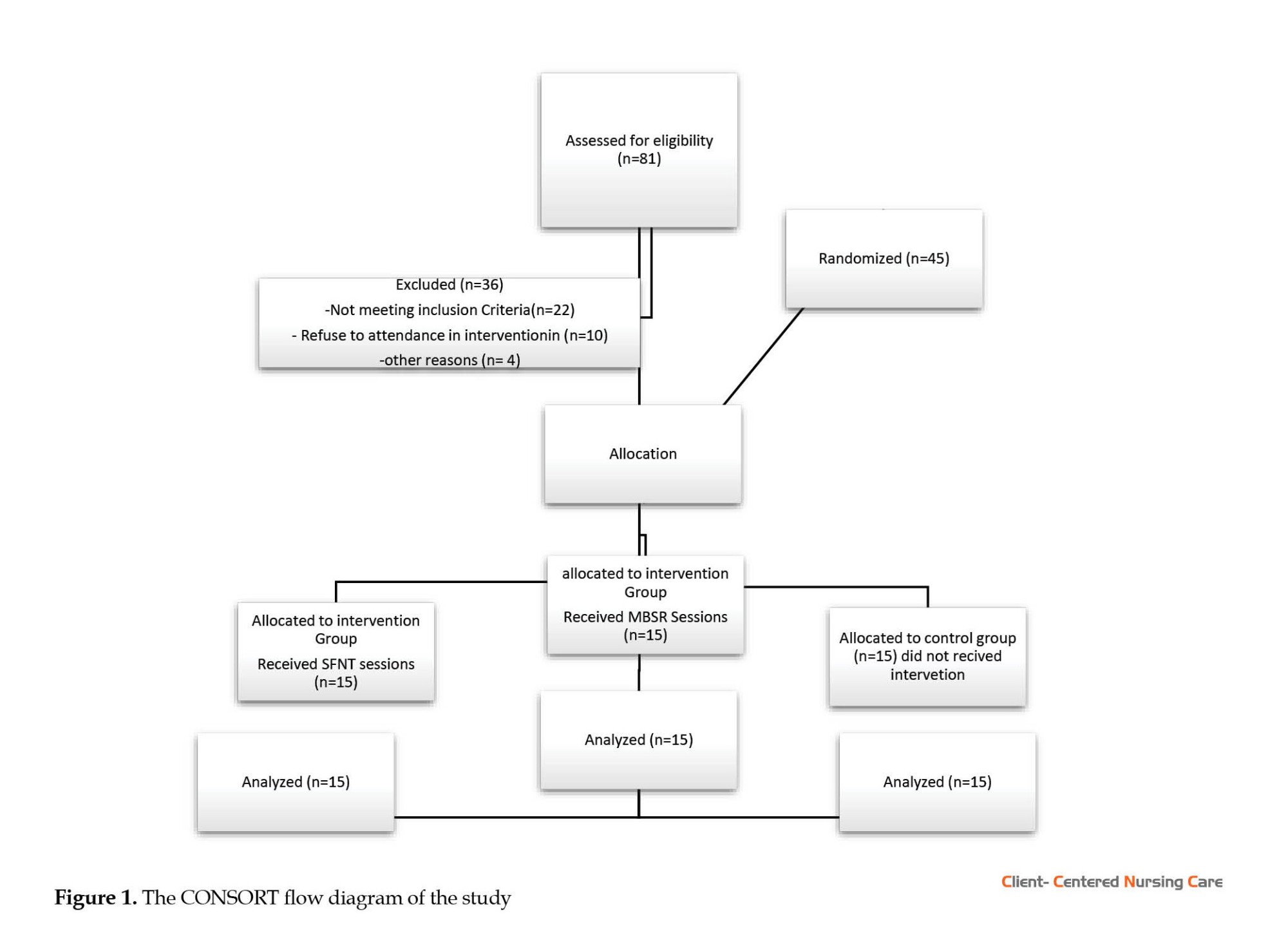
To recruit participants, 81 mothers were initially assessed for eligibility. Then, 36 subjects were excluded due to not meeting inclusion criteria (n=22), reluctance to participate in the intervention (n=10), and other reasons (n=4) (Figure 1). In the next step, 45 mothers were randomly assigned to 2 intervention groups and 1 control group by drawing lots to minimize confounders and eliminate systematic bias.
The inclusion criteria were having a son with one of the gross motor disabilities, not being divorced (due to life problems for female heads of the family), and literacy for reading and writing. The exclusion criteria were absence in more than two therapy sessions and simultaneous participation in other psychotherapy programs.
Study instruments
The study instruments were as follows.
The demographic form included the mother’s age, education level, and child’s age.
The level of expressed emotion (LEE) scale was used to evaluate the quality of mothers’ EE. The scale was developed by Cole & Kazarian (1988) to investigate the perceived emotional climate in a person’s influential relationships. This scale has 60 items and 4 subscales: Intrusiveness, emotional response, attitude toward illness, and tolerance/expectations. Each item is scored from 1 to 4 (1=untrue, 2=somewhat untrue, 3=somewhat true, and 4=true). The total scores ranged from 60 to 240, with higher scores indicating more intense emotional involvement. The Cronbach α values for intrusiveness, emotional response, attitude toward illness, and tolerance/expectations are 0.667, 0.89, 0.84, and 0.78, respectively. In addition, The Cronbach α for the whole scale is 0.94 (Cole & Kazarian, 1988). This questionnaire was first translated into Persian by Dehghani (2003), and its reliability was reported by calculating the Cronbach α as 0.93. In this study, the Cronbach α of this scale was calculated as 0.91. This scale was completed through self-reporting by mothers participating in the research in the pre-test and post-test stages.
Study procedure
A total of 45 mothers with male children suffering from gross motor disabilities were selected and randomly assigned to three equal groups, each comprising 15 persons. Each therapy intervention (SFNT and MBSR) was conducted 2 days per week. To this end, the SFNT sessions were held on Saturdays from 10-12 AM for 9 consecutive weeks. Each session took 90 minutes (White & Morgan, 2006; Metcalf, 2017), and the MBSR sessions were held on Tuesdays from 10-12 AM for 8 consecutive weeks. Each session took 90 minutes (Petcharat, 2018; Reibel & McCown, 2019). All sessions were held in person at the “Success Counselling Center” in Tehran Province, Iran. All the sessions were conducted in groups and by psychoeducation (e.g. giving information verbally, written materials and handouts, exercise or homework to encourage the mothers to discover information for themselves), question and answer, and dialogue between the therapist and the mother. The therapist was a PhD student in Family Counseling. One week after the end of the intervention sessions, a post-test was taken from all three groups.
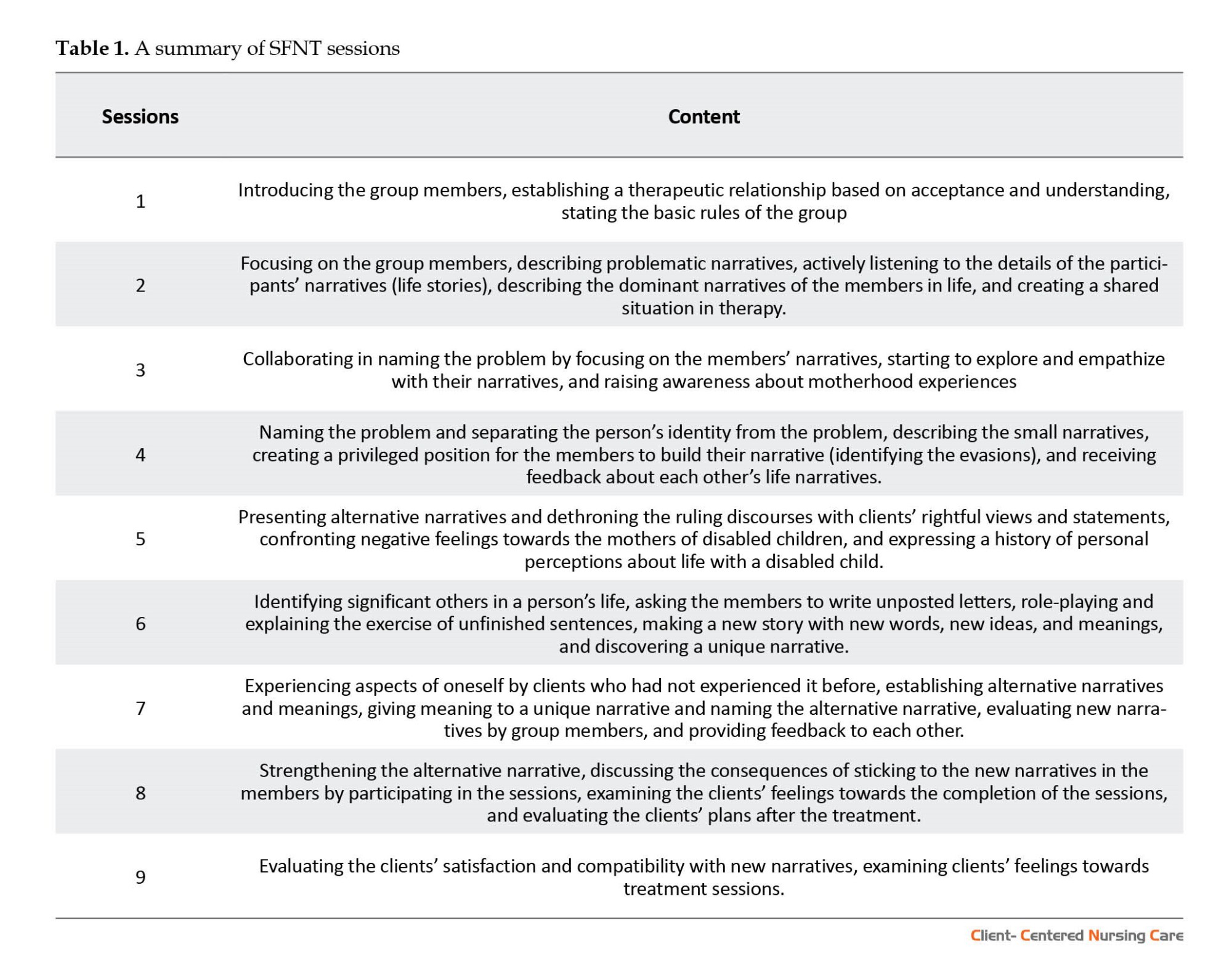
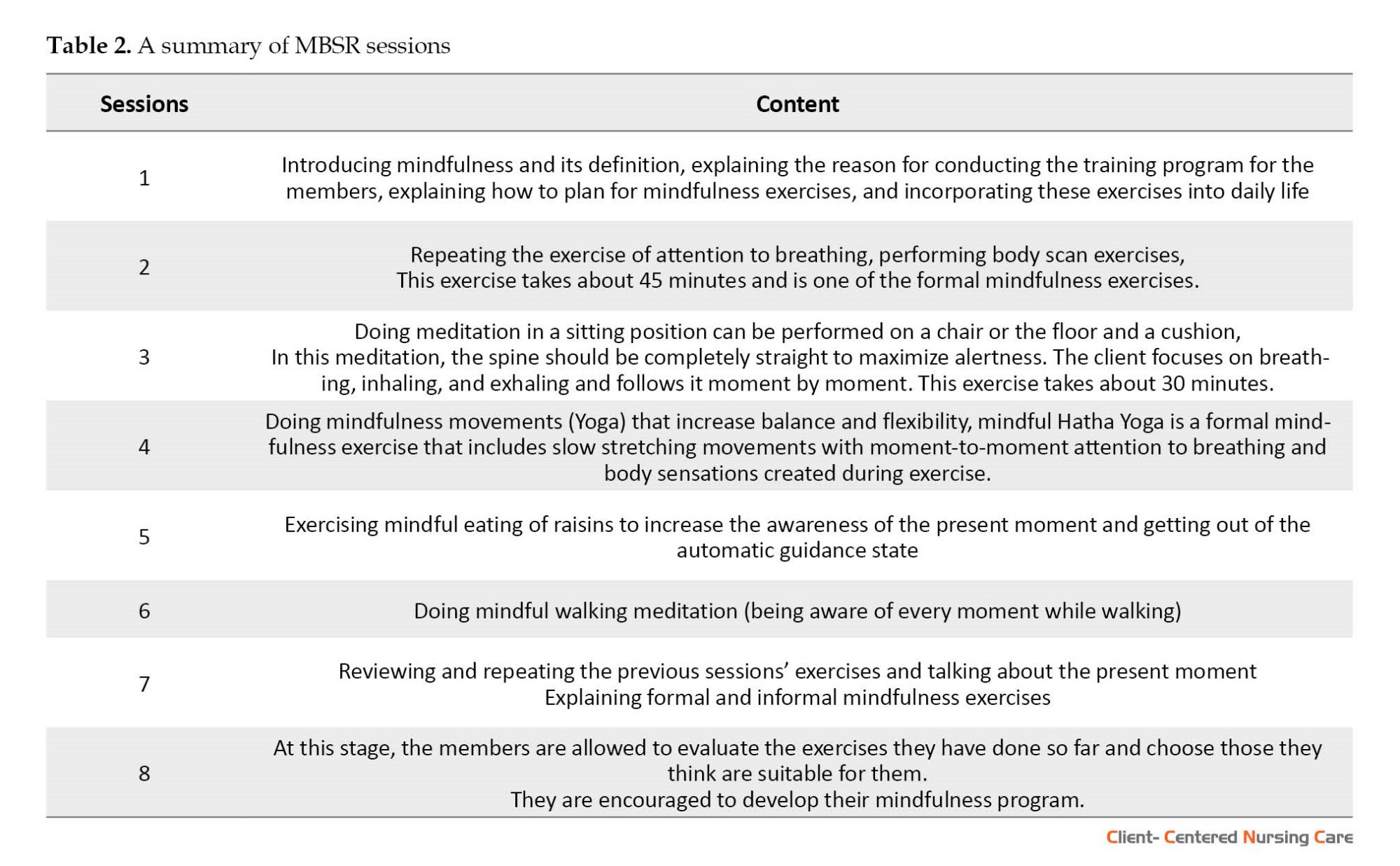
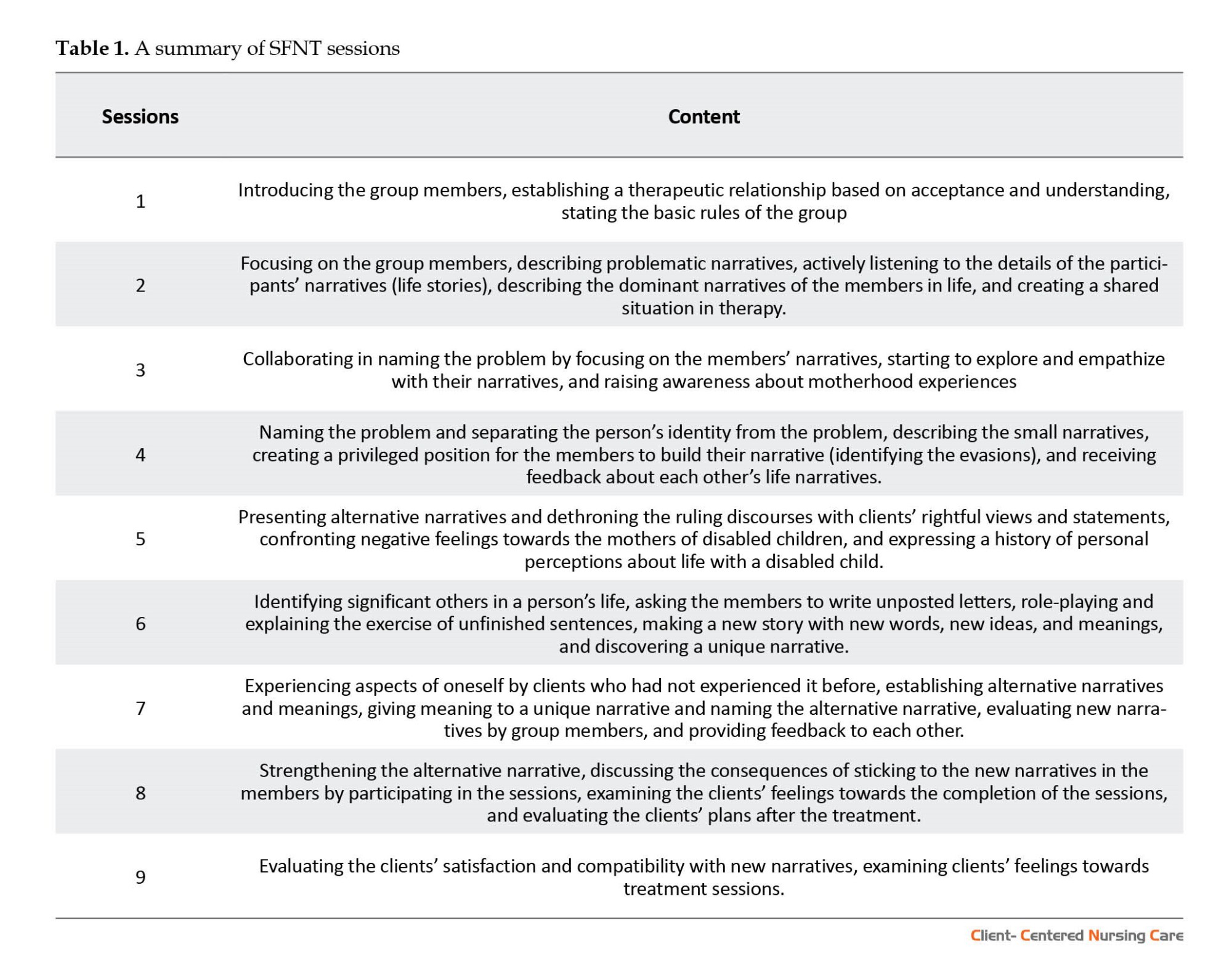
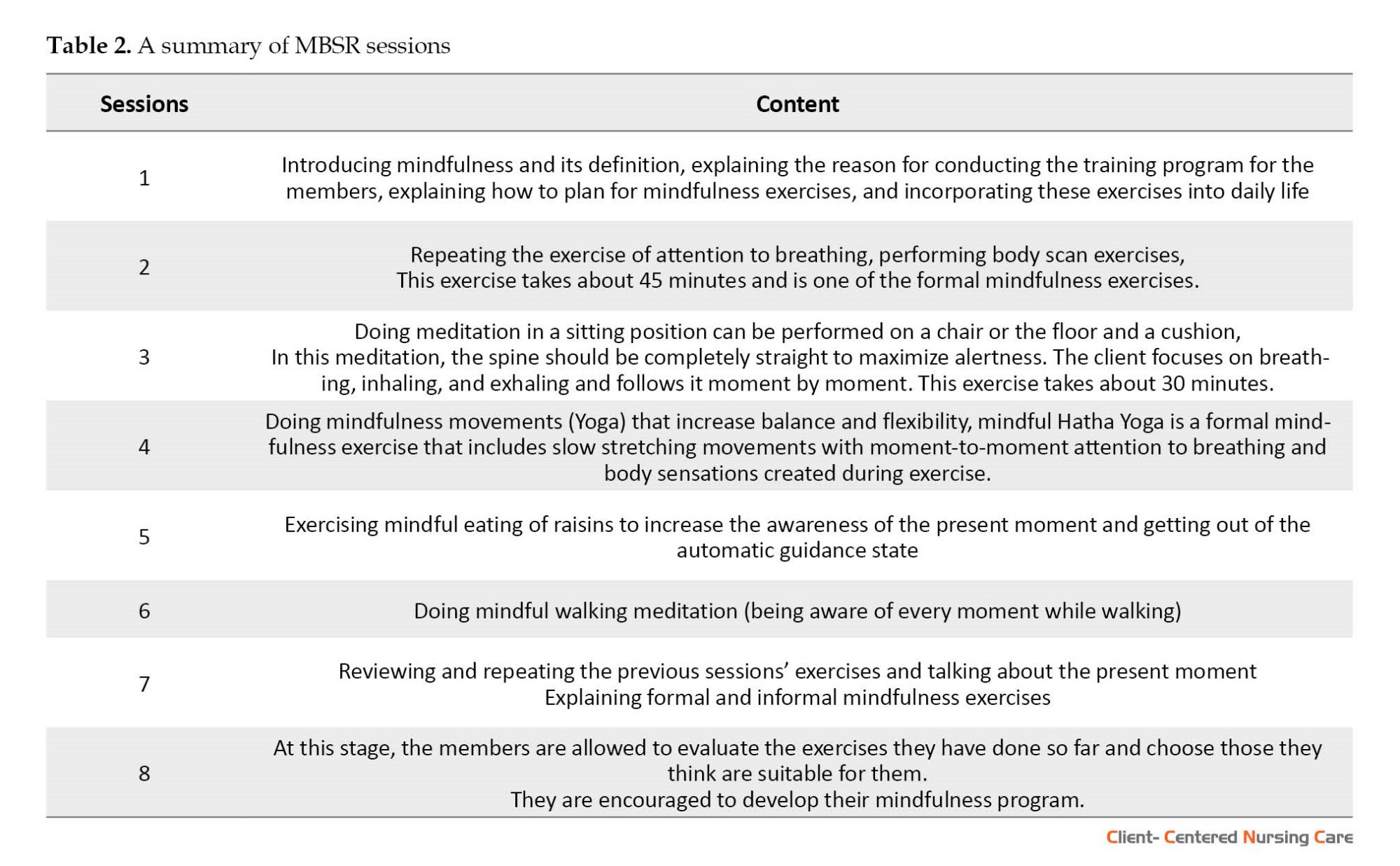
Tables 1 and 2 show a summary of the content of the SFNT and MBSR sessions.
Data analysis
The collected data were analyzed using descriptive statistics, such as frequency, percentage, Mean±SD. In addition, the multivariate analysis of variance (MANOVA) and least significant difference (LSD) post hoc test were used to compare the groups. The data were analyzed using SPSS software, version 26. The significance level was set at P<0.05.
3. Results
The average age of the mothers participating in this study was 40.02±3.4 years, and the mean age of their children was 9.06±2.8 years. The personal characteristics of the subjects are presented in Table 3.
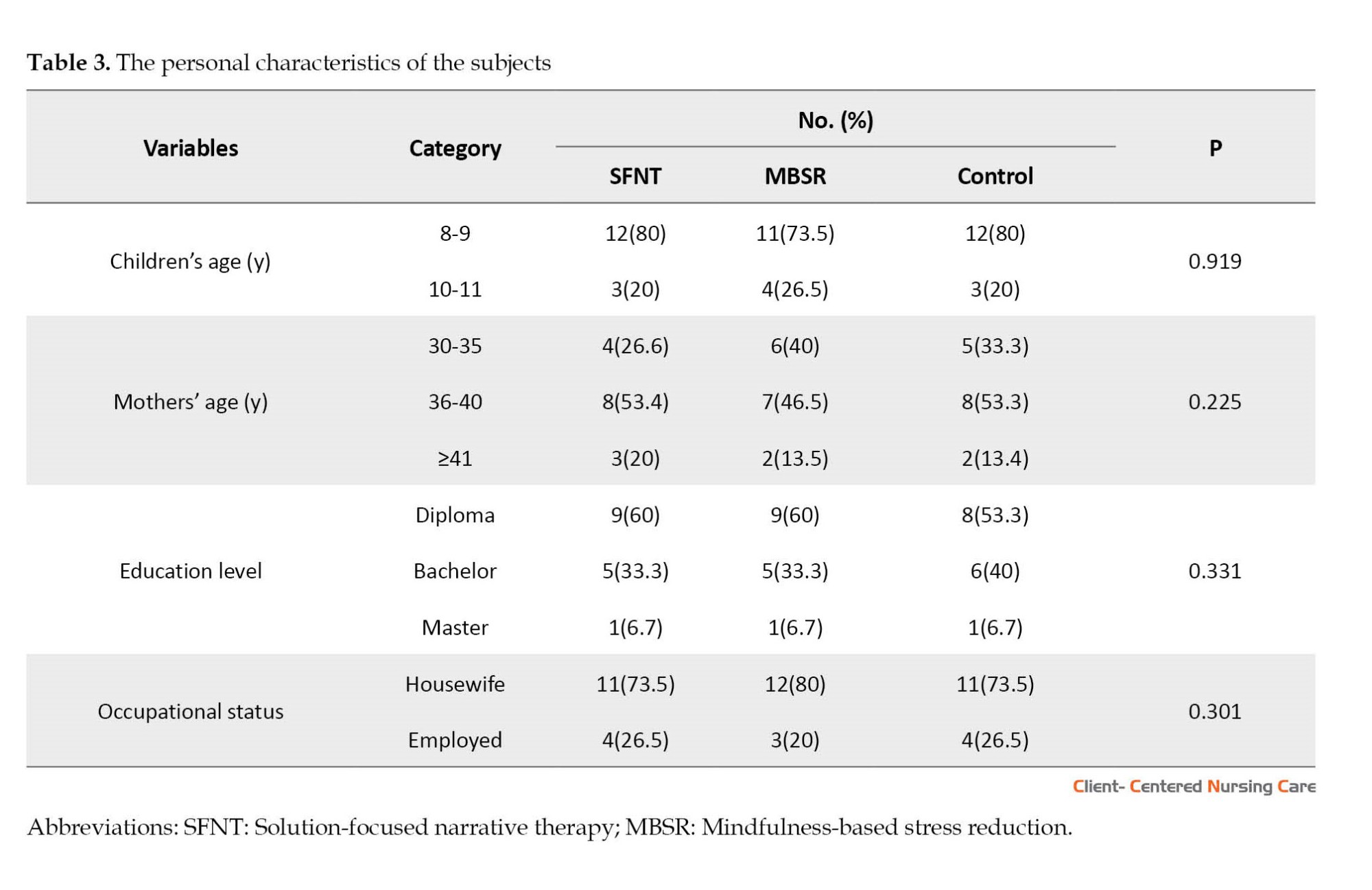
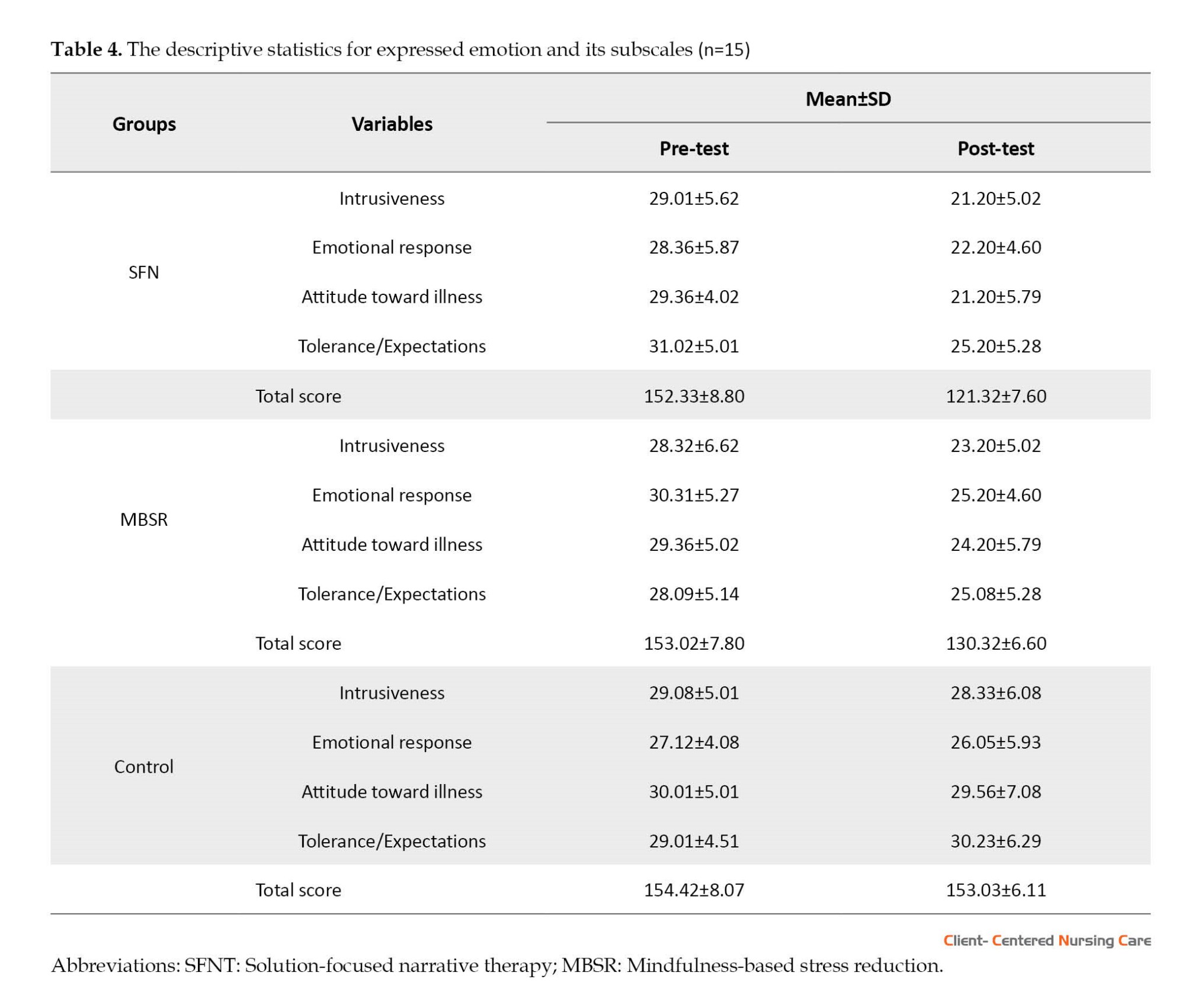
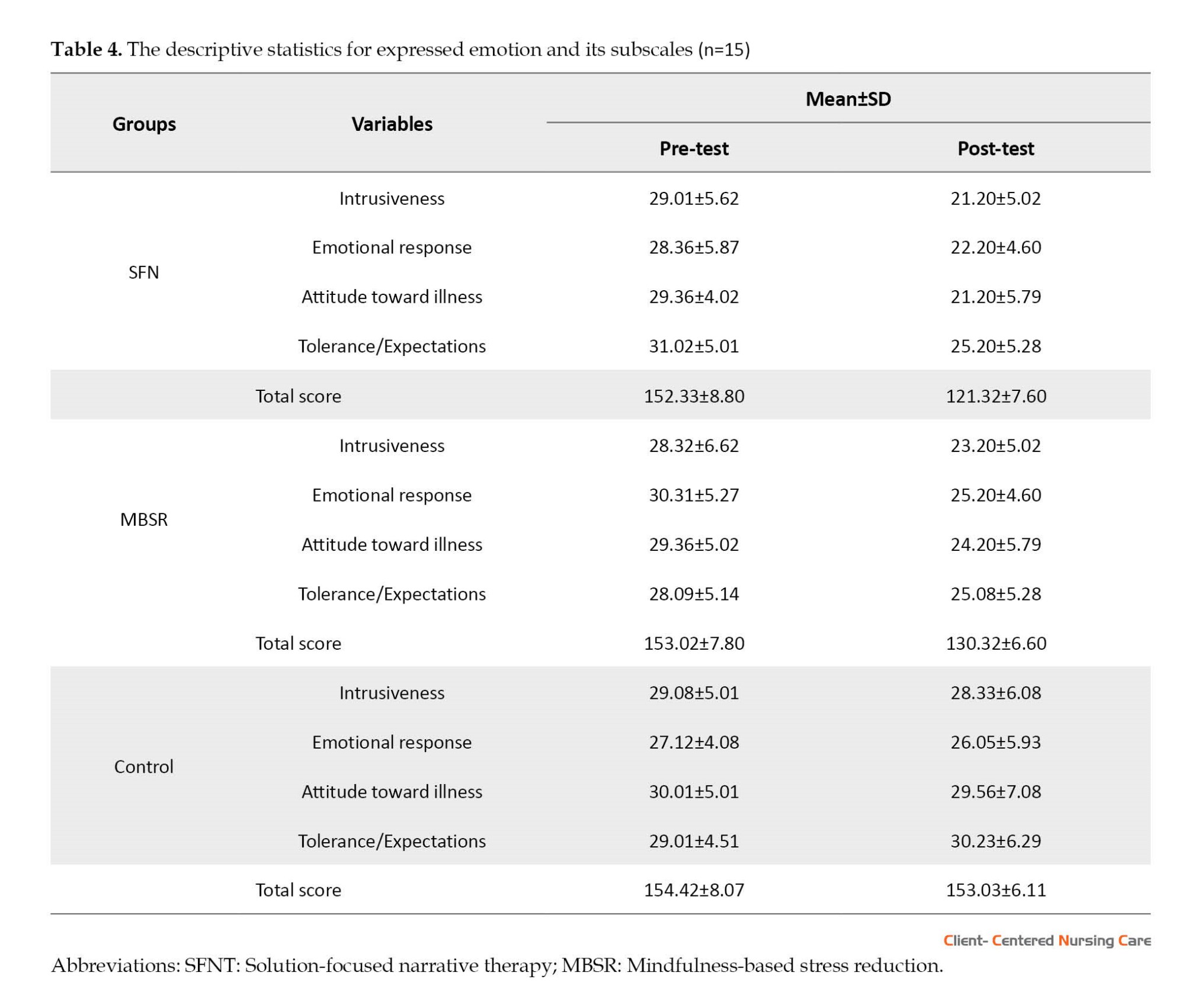
Table 4 details the descriptive statistics for EE and its subscales in the intervention and control groups in the pre-test and post-test phases.
Analysis of covariance (ANCOVA) was run to compare the group means. Prior to ANCOVA, the assumptions of this test were first checked using Levene’s and Box’s M tests. Because the results were not significant (P>0.05), ANCOVA was subsequently performed.
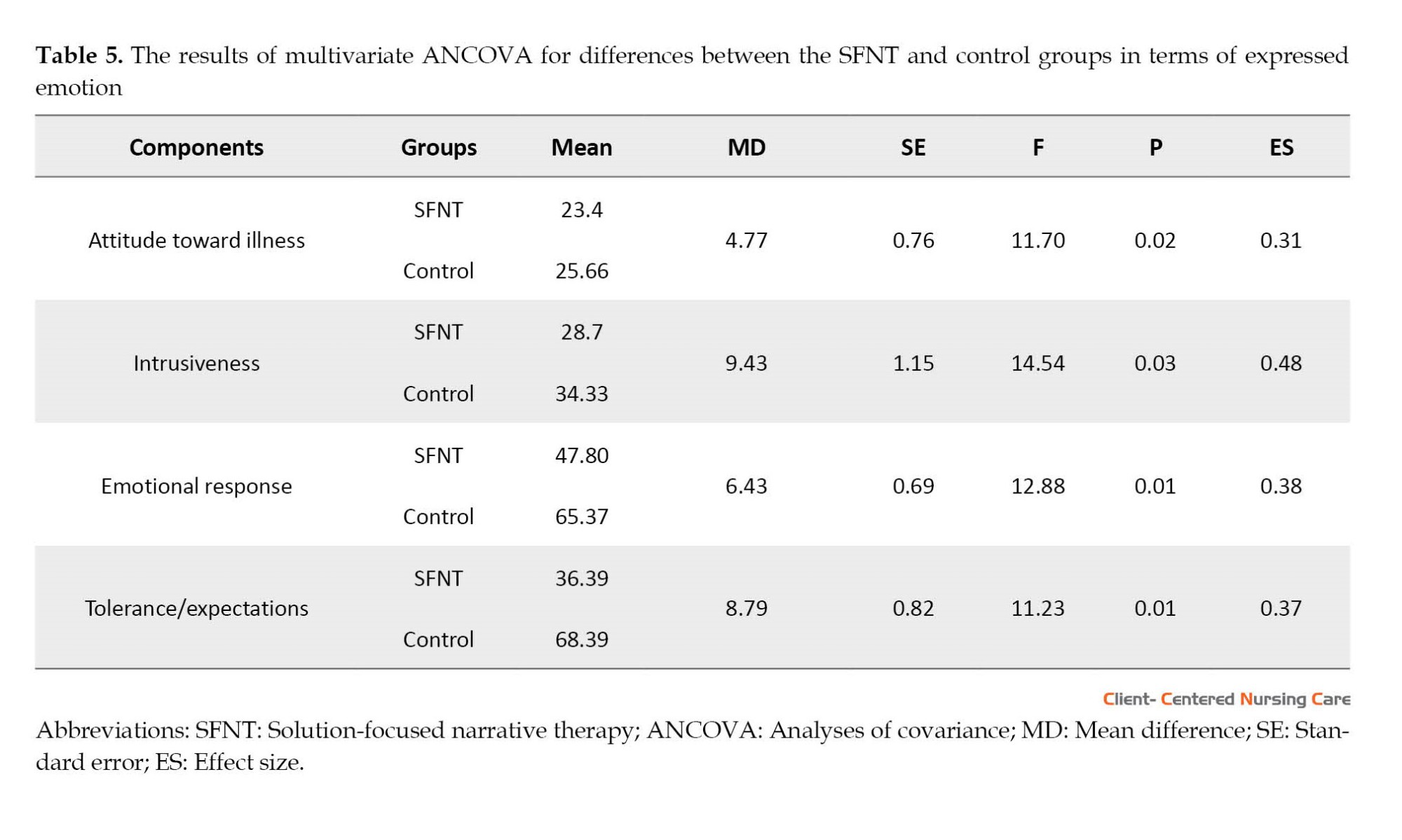
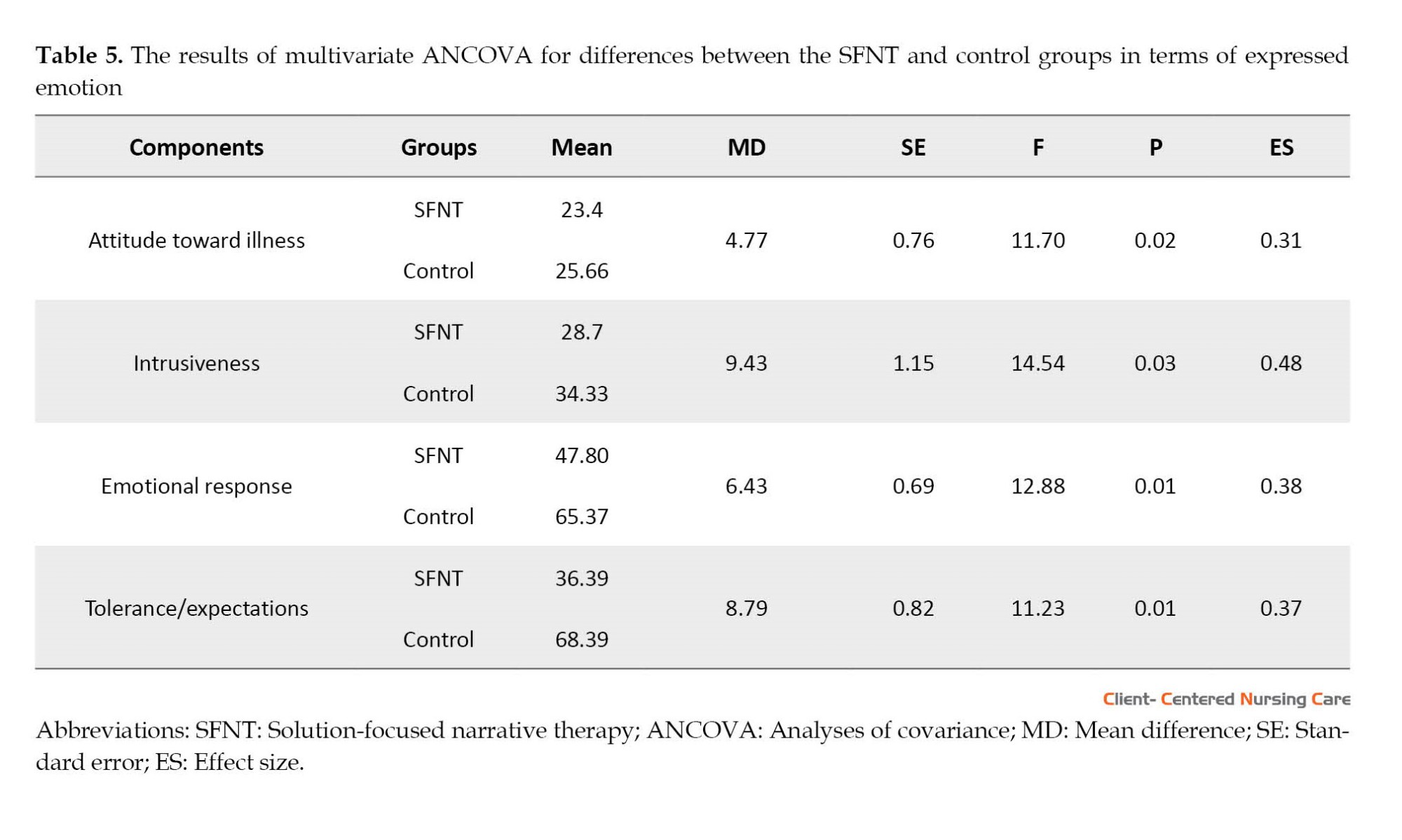
As can be seen in Table 5, the F values for the components of negative attitude towards illness (F=11.70, P=0.02), intrusiveness (F=14.54, P=0.03), emotional response (F=12.88, P=0.01), and tolerance/expectations (F=11.23, P=0.01) were significant, indicating significant between-group differences in terms of the mentioned variables. A comparison of the group means also suggested that the mean values were greater for the SFNT group than the control group. This finding indicates that SFNT is effective in the level of EE of mothers of children with gross motor disabilities.
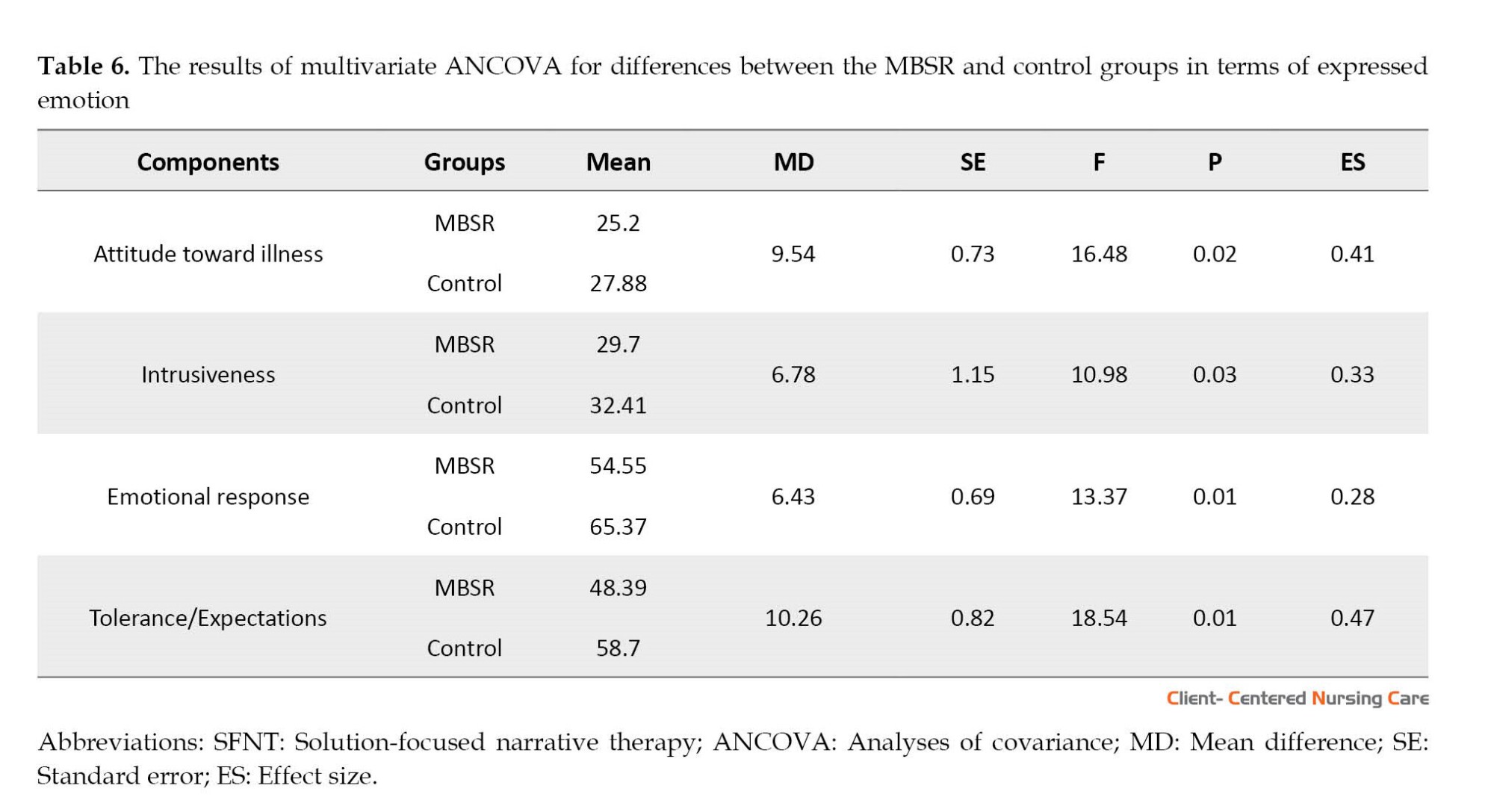
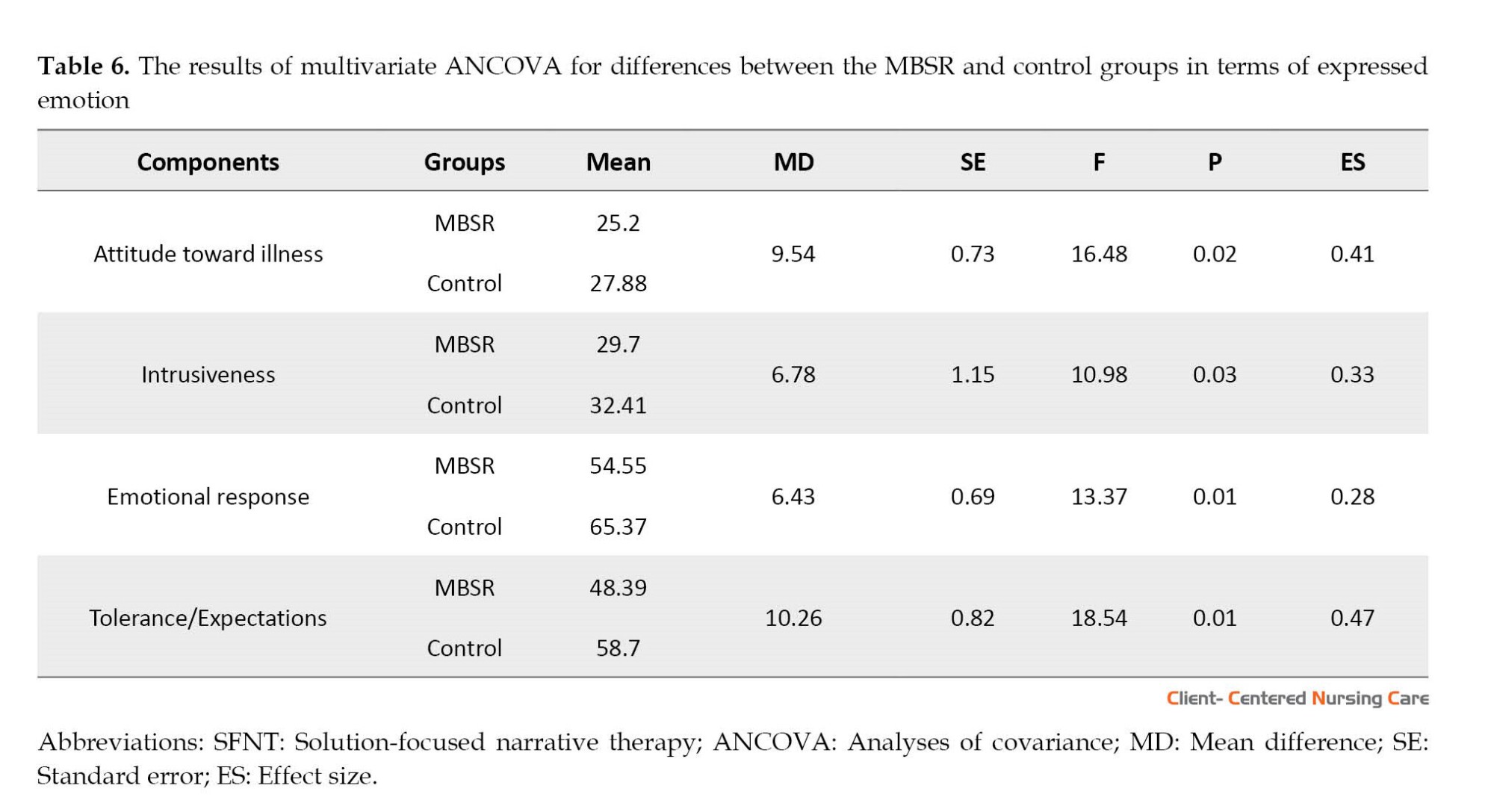
As can be seen in Table 6, the F values for the components of negative attitude towards illness (F=16.48, P=0.02), intrusiveness (F=10.98, P=0.03), emotional response (F=13.37, P=0.01), and tolerance/expectations (F=18.54, P=0.01) were significant, indicating significant between-group differences in terms of the mentioned variables. A comparison of the group means also suggested that the mean values were greater for the MBSR group than the control group. This finding indicates that MBSR is effective in the level of EE of mothers of children with gross motor disabilities.
The results of multivariate ANCOVA by taking the pre-test scores as control variables are shown in Table 7. Wilks’ lambda test results indicated significant differences between the three groups in the post-test scores (F=2.521, P<0.01).
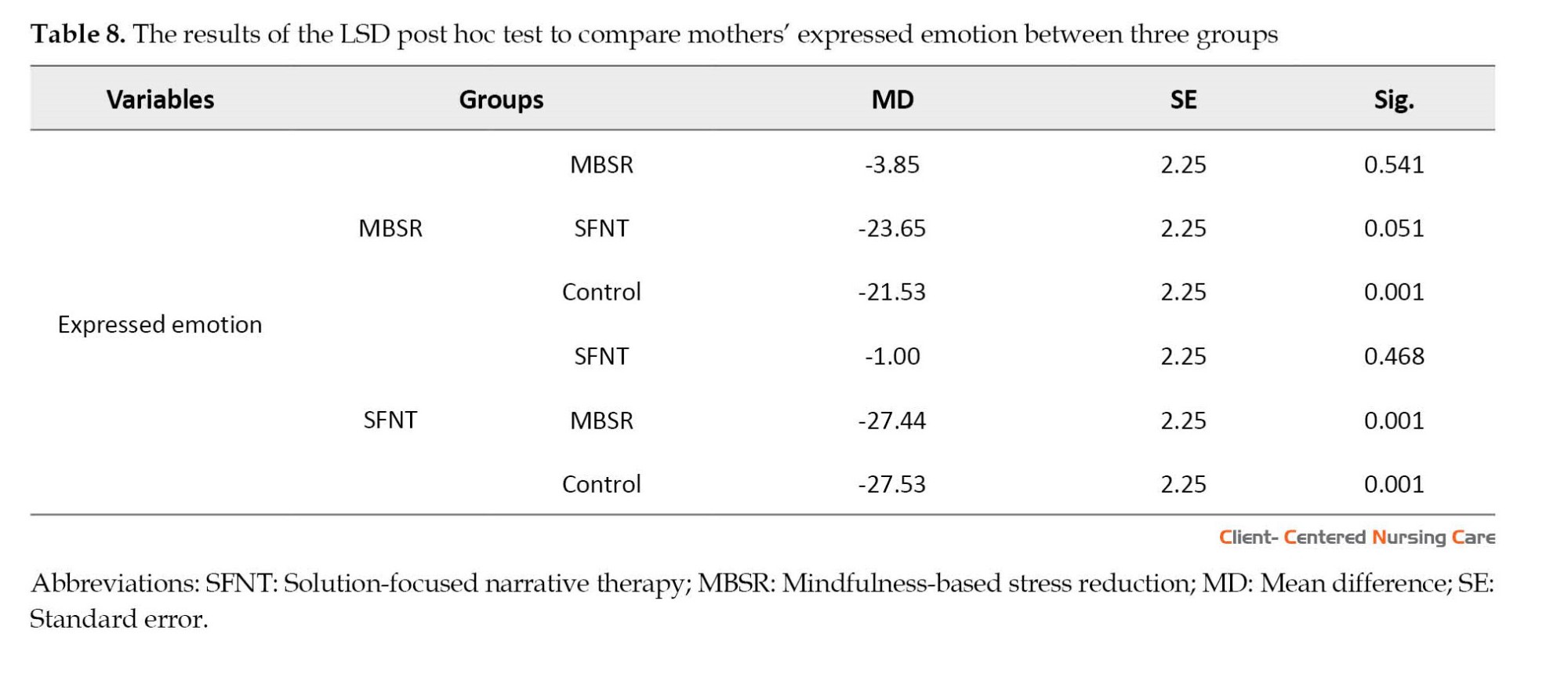
.jpg)
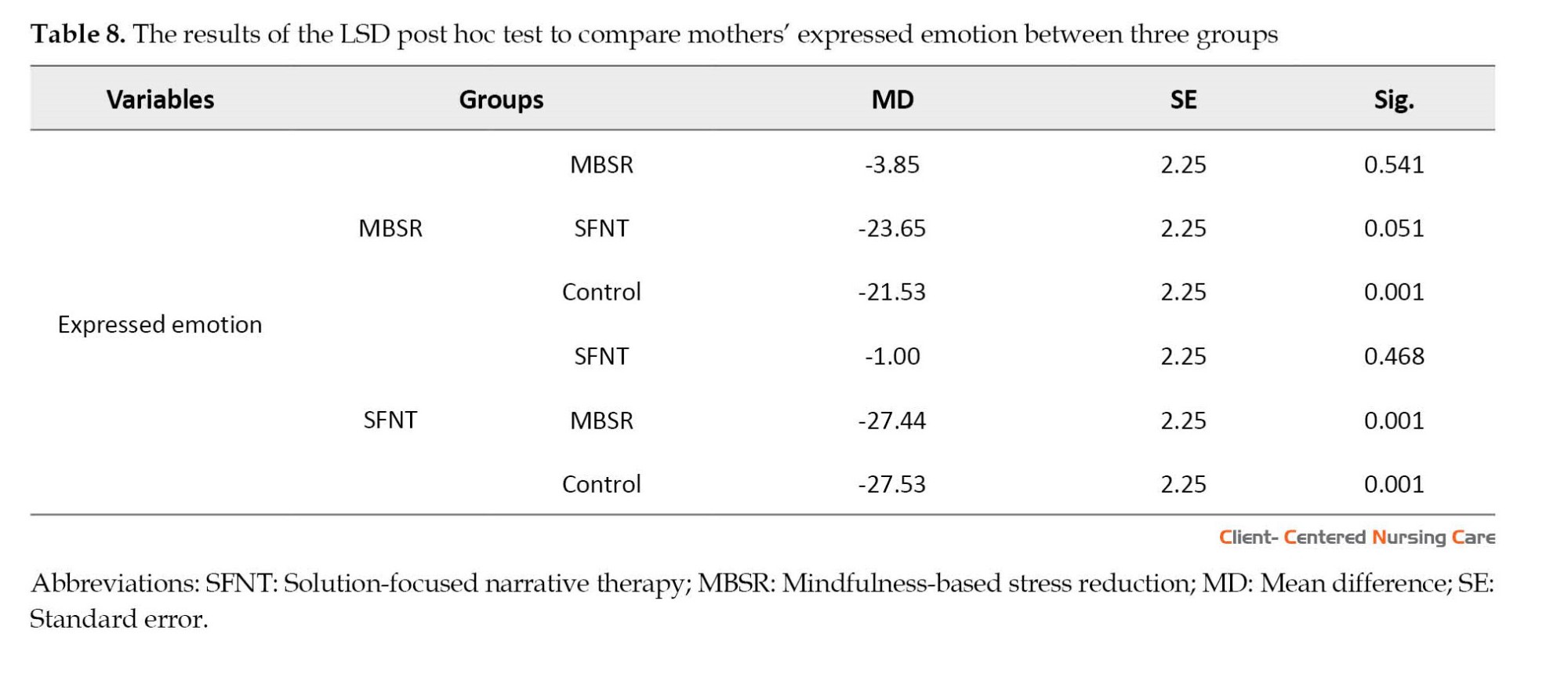
Pairwise comparisons using the LSD post hoc test (Table 8) showed that the two intervention groups had significant differences in mothers’ EE (P<0.05), indicating that SFNT was more effective than (MBSR therapy in reducing mothers’ EE (P<0.01).
4. Discussion
The present study compared the effectiveness of SFNT and MBSR on the level of EE in mothers of male children with gross motor disabilities. The results showed that both therapies significantly reduced the expression of the mothers’ negative emotions, such as aggression and criticism. Parents with disabled children express strong negative feelings through aggression and criticism towards their children with developmental disabilities (Thompson et al., 2018; Stiles-Shields et al., 2022). However, in this study, the demographic characteristics of mothers were controlled across all groups, and there was no significant difference between them. Still, it is acknowledged that the mother’s stress level and emotional expression could be partly related to socio-demographic variables. For example, a study found that unemployed mothers and those with lower education exhibited higher levels of parental distress than employed mothers (Fucà et al., 2022).
The data in this study showed that MBSR intervention can help reduce the expressed negative emotions of mothers. Mothers with disabled children endure high levels of stress, expressed through aggression, criticism, or emotional over-involvement due to repeated failures in dealing with their child’s physical problems and other people’s behavior. A study used mindfulness-based positive behavior support training for 3 months to reduce the stress of mothers of adolescents with autism spectrum disorder, and the results showed that teaching mothers was accompanied by an increase in their children’s compliance behaviors and ultimately led to a reduction in parenting stress level (Singh et al., 2014).
MBSR is a non-judgmental therapy that helps people consciously increase their awareness of the present moment because they perform guided mindfulness practices that cover many aspects of daily life, such as breathing, bodily sensations, movement, and eating (Semple & Hatt, 2012; Epstein, 2010). In another study, Crawley et al. (2022) used mindfulness-based music and songwriting to help reduce the psychological distress and problems of mothers of children with disabilities. After 4 weeks, they observed a significant reduction in mothers’ psychological problems. It is believed that the effectiveness of MBSR is more prominent in reducing the parenting stress of mothers with disabled children (Sing et al., 2014; Burgdorf et al., 2019). For example, a meta-analysis study by Chua and Shorey revealed that mindfulness- and acceptance commitment therapy (ACT)-based interventions effectively reduced stress, anxiety, and depression of parents of children with developmental disabilities. Nevertheless, these interventions were not effective in raising parents’ mindfulness. These conflicting results could be attributed to the religious and cultural differences between Eastern and Western societies and how people perceive the world. Compared to other religions and Western cultures, Muslims and Buddhists believe in the effectiveness of mindfulness-based therapy in reducing stress as they have already experienced moments of mindfulness in their prayers and worship (Chua & Shorey, 2021). Therefore, cultural and religious factors could have strengthened the effect of MBSR intervention on the reduction of expressed emotions of Iranian mothers.
Studies have revealed that SFNT increases social participation and informed decisions of people with cerebral palsy Schwellnus et al. (2020) and reduces psychological distress in mothers with disabled children (Baldiwala & Kanakia, 2022). This therapy has also been effective in other children’s problems in the family. However, previous studies have not directly reported reduced negative emotional expression in mothers of children with motor disabilities. For example, D’Abate used the SFNT intervention to resolve conflicts related to child custody rights in conflicting couples, and the results indicated a reduction in the psychological stress of children and their parents and the creation of alternative solutions to help the family (D’Abate, 2016). Besides, Myers and colleagues (2006) used SFNT in a case study to treat a boy who experienced sexual abuse. The results showed that SFNT helped the child have a new life narrative and overcome his problems with conscious decisions.
A comparison of the effectiveness of these two therapies showed that SFNT was more effective than MBSR. This difference could be attributed to the nature of these therapies. Mindfulness therapies focus on meditation techniques, relaxation, and mindfulness of a person’s life moment by moment, while SFNT is a postmodern therapy that requires more exploration and meditation on narratives, how people make decisions in life, and their greater participation in their life events (Ricks et al., 2014). Thus, SFNT can be effective in the mother’s EE, which is more influenced by the change of life story, the creation of new narratives, and ultimately, the feeling of more control over life. In narrative therapy, mothers could talk freely about their feelings, thoughts, and life experiences that they previously had difficulty expressing. They face an opportunity to talk about their bitter experiences and internalized stigma and try to find new and creative solutions with the therapist’s help. Mothers in the group rewrote their life stories, and rewriting the life story led to their creativity and finally discovering new aspects of their lives.
This study was conducted with some limitations. First, it examined only the mothers from one counseling center in Tehran. Second, due to procedural problems, it was impossible to follow up on the effectiveness of the two therapies in the long term. The third limitation of this study was the random allocation of groups by drawing lots, which did not guarantee the possibility of removing the complete influence of the confounders. Therefore, it is recommended to conduct a similar study in more centers, follow up on the durability of the interventions, and randomly assign groups using more reliable methods.
5. Conclusion
The results showed that both therapies can reduce the expression of negative emotions in the mothers of children with gross motor disabilities. However, SFNT had a more significant effect on lowering negatively expressed feelings. Due to psychological pressures and burdens on mothers or their lack of familiarity with the complex concepts of child management behavior treatments, they cannot strictly implement therapeutic instructions. Therefore, providing opportunities for training and group counseling, discussion, and question and answer sessions gives mothers more possibilities to help care for themselves and their children. In future research, it is suggested that the newer MBSR methods, Yoga and meditation, be used to reduce the psychological stress of mothers. Also, SFNT therapeutic intervention should be done by emphasizing the redefined narrative of the mother and father (parents) about the child’s disability and their EE.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the North Tehran Branch, Islamic Azad University (Code: IR.IAU.TNB.REC.1401.055) and Informed written consent was obtained from all the subjects. To comply with ethical guidelines, 6 training sessions were held for the control group after completing the interventions.
Funding
This study was extracted from PhD dissertation of Behnaz Karami, approved by Department of Counseling, North Tehran Branch, Islamic Azad University.
Authors' contributions
Conducting research, data gathering and analysis: Behnaz Karami; Conceptualization, study design, and drafting of the initial version: Anahita Khodabakhshi-Koolaee; Data analysis: Hassan Heidari and Hossein Davoodi; Supervision: Anahita Khodabakhshi-Koolaee, Hassan Heidari and Hossein Davoodi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants who contributed to conducting this research project.
References
Baldiwala, J. & Kanakia, T., 2022. Using narrative therapy with children experiencing developmental disabilities and their families in India: A qualitative study. Journal of Child Health Care, 26(2), pp. 307-18. [DOI:10.1177/13674935211014739] [PMID]
Bazzano, A., et al., 2015. Mindfulness-based stress reduction (MBSR) for parents and caregivers of individuals with developmental disabilities: A community-based approach. Journal of Child and Family Studies, 24, pp. 298-308. [DOI:10.1007/s10826-013-9836-9]
Benn, R., et al., 2012. Mindfulness training effects for parents and educators of children with special needs. Developmental Psychology, 48(5), pp. 1476-87. [DOI:10.1037/a0027537] [PMID]
Burgdorf, V., Szabó, M. & Abbott, M. J., 2019. The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: A systematic review and meta-analysis. Frontiers in Psychology, 10, pp. 1336. [DOI:10.3389/fpsyg.2019.01336] [PMID]
Chang, J. & Nylund, D., 2013. Narrative and solution-focused therapies: A twenty-year retrospective. Journal of Systemic Therapies, 32(2), pp. 72-88. [DOI:10.1521/jsyt.2013.32.2.72]
Chua, J. Y. X. & Shorey, S., 2022. The effect of mindfulness-based and acceptance commitment therapy-based interventions to improve the mental well-being among parents of children with developmental disabilities: A systematic review and meta-analysis. Journal of Autism and Developmental Disorders, 52(6), pp. 2770-83. [DOI:10.1007/s10803-021-04893-1] [PMID]
Cole, J. D. & Kazarian, S. S., 1988. The level of expressed emotion scale: A new measure of expressed emotion. Journal of Clinical Psychology, 44(3), pp. 392-7. [DOI:10.1002/1097-4679(198805)44:33.0.CO;2-3] [PMID]
Coleman, J. M., 2010. The expressed emotion of mothers of children with fragile X syndrome [PhD dissertation]. Denver: University of Denver. [Link]
Crawley, Z., 2022. Mindfulness-based music and songwriting: Pilot data from a novel telehealth intervention for parents of children with disabilities [PhD dissertation]. Nashville: Vanderbilt University. [Link]
D’Abate, D. A., 2016. Use of solution-focused and family narrative approaches in working with high conflict families: Strategies and techniques that can be utilized in parenting coordination and co-parenting coaching. Journal of Child Custody, 13(4), pp. 269-88. [DOI:10.1080/15379418.2016.1247308]
Dehghani, S. H., 2003. [Expressed emotion and sexuality (Persian)]. Journal of Fundamental Mental Health, 5(19-20), pp. 84-91. [Link]
Hastings, R. P., et al., 2006. Maternal distress and expressed emotion: Cross-sectional and longitudinal relationships with behavior problems of children with intellectual disabilities. American Journal on Mental Retardation, 111(1), pp. 48-61. [DOI:10.1352/0895-8017(2006)111[48:MDAEEC]2.0.CO;2]
Epstein, B. J., 2010. Effects of a mindfulness-based stress reduction program on fathers of children with a developmental disability [PhD dissertation]. New York: Hofstra University. [Link]
Fucà, E., et al., 2022. Parenting stress in mothers of children and adolescents with down syndrome. Journal of Clinical Medicine, 11(5), pp. 1188. [DOI:10.3390/jcm11051188] [PMID]
Kabat-Zinn J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing. [Link]
Khodabakhshi-Koolaee, A., Koshki, M. A. & Kalhor, N., 2019. [Analysis of the experiences of mothers in caring for a disabled child: A phenomenological Study (Persian)]. Iranian Journal of Pediatric Nursing, 6(2), pp. 68-75. [Link]
Khodabakhshi Koolaee, A. & Derakhshandeh M., 2015. [Effectiveness of hope-oriented group therapy on life meaning and resilience in mothers with physical-motor disabled children (Persian)]. Journal of Pediatric Nursing, 1(3), pp. 15-25.
Khoshgoftar, M., Khodabakhshi-Koolaee, A. & Sheikhi, M. R., 2022. Analysis of the early mother-child relationship in schizophrenic patients. International Journal of Social Psychiatry, 68(3), pp. 548-54. [DOI:10.1177/0020764021991186] [PMID]
Mak, C. K., Whittingham, K. & Boyd, R. N., 2019. Experiences of children and parents in MiYoga, an embodied mindfulness yoga program for cerebral palsy: A mixed method study. Complementary Therapies in Clinical Practice, 34, pp. 208-16. [DOI:10.1016/j.ctcp.2018.12.006.] [PMID]
Metcalf, L., 2017. Solution-focused narrative therapy. New York: Springer Publishing Company. [DOI:10.1891/9780826131775]
Metcalf, L., 2021. Counseling toward solutions: A practical, solution-focused program for working with students, teachers, and parents. New York: Routledge. [DOI:10.4324/9781003122128]
Morris, C. & Bartlett, D., 2004. Gross motor function classification system: Impact and utility. Developmental Medicine and Child Neurology, 46(1), pp. 60-5. [DOI:10.1017/S0012162204000118] [PMID]
Perry, V., 2020. A solution-focused narrative therapeutic approach to improving quality of life with cancer patients participating in group therapy [PhD dissertation]. Texas: Texas Wesleyan University. [Link]
Petcharat, M., 2018. The effects of a brief culturally tailored Thai mindfulness intervention on stress, anxiety, and mindfulness in Thai parents of children with developmental disabilities [PhD dissertation]. Boca Raton: Florida Atlantic University. [Link]
Reibel, D. & McCown, D., 2019. Mindfulness-based stress reduction: Theory, practice and evidence base. In: I. Ivtzan (ed), Handbook of mindfulness-based programmes (pp. 29-41). London: Routledge. [DOI:10.4324/9781315265438-4]
Ricks, L., et al., 2014. My story: The use of narrative therapy in individual and group counseling. Journal of Creativity in Mental Health, 9(1), pp. 99-110. [DOI:10.1080/15401383.2013.870947]
Riley, S. & Malchiodi, C. A., 2003. Solution-focused and narrative approaches. In: C. A. Malchiodi (ed), Handbook of art therapy ( pp. 82-92). New York: The Guilford Press. [Link]
Romero-Gonzalez, M., Chandler, S. & Simonoff, E., 2018. The relationship of parental expressed emotion to co-occurring psychopathology in individuals with autism spectrum disorder: A systematic review. Research in Developmental Disabilities, 72, pp. 152-65. [DOI:10.1016/j.ridd.2017.10.022] [PMID]
Saunders, L. M., 2020. A solution-focused narrative therapeutic approach to restoring couple relationships after infidelity [PhD dissertation]. Texas: Texas Wesleyan University. [Link]
Schwellnus, H., et al., 2020. A solution-focused coaching intervention with children and youth with cerebral palsy to achieve participation-oriented goals. Physical & Occupational Therapy in Pediatrics, 40(4), pp. 423-40. [DOI:10.1080/01942638.2020.1711841] [PMID]
Semple, R. J. & Hatt, S. P., 2012. Translation of Eastern meditative disciplines into Western psychotherapy. In: L. J. Miller (ed), The Oxford handbook of psychology and spirituality. Oxford: Oxford University Press. [DOI:10.1093/oxfordhb/9780199729920.013.0021]
Singh, N. N., et al., 2014. Mindfulness-based positive behavior support (MBPBS) for mothers of adolescents with autism spectrum disorder: Effects on adolescents’ behavior and parental stress. Mindfulness, 5, pp. 646-57. [DOI:10.1007/s12671-014-0321-3]
Soleimani, F., et al., 2018. [Relationship between gender and development status in children (Persian)]. Archives of Rehabilitation, 18(4), pp. 338-45. [DOI:10.21859/jrehab.18.4.8]
Stiles-Shields, C., et al., 2023. Caregiver expressed emotion in families of youth with spina bifida: Demographic, medical, and family correlates. Journal of Pediatric Psychology, 48(2), pp. 144-55. [DOI:10.1093/jpepsy/jsac073] [PMID]
Thompson, T., Coleman, J. & Olmos, A., 2018. The expressed emotion of parents of children with developmental disabilities: A meta-analysis. Life Span and Disability, 21(2), pp. 177-89. [PMID]
Vaughn, C. & Leff, J., 1976. The measurement of expressed emotion in the families of psychiatric patients. British Journal of Social and Clinical Psychology, 15(2), pp. 157-65. [DOI:10.1111/j.2044-8260.1976.tb00021.x] [PMID]
Veldman, S. L., et al., 2020. Prevalence and risk factors of gross motor delay in pre-schoolers. Journal of Paediatrics and Child Health, 56(4), pp. 571-6. [DOI:10.1111/jpc.14684] [PMID]
White, M. K. & Morgan, A., 2006. Narrative therapy with children and their families. Adelaide: Dulwich Centre Publications. [Link]
Caring for a disabled child in the family creates stress and disrupts the physical and mental health of the parents, especially mothers. Compared to fathers, mothers spend a substantial amount of time with their children and assume leadership roles in the family (Khodabakhshi-Koolaee & Derakhshandeh, 2015). Motor disabilities in children can lead to problems in doing daily activities. They face severe disabilities, such as poor eye-hand coordination. Thus, they often bump into things while moving, constantly fall, and have problems coordinating muscles to do their tasks. These problems hinder their progress in school assignments and disruption in daily activities. Gross motor disabilities develop due to genetic reasons, such as Down syndrome, neuromuscular disorders (e.g. muscular dystrophy or cerebral palsy); developmental reasons, such as autism; and hormonal causes, such as hypothyroidism (Morris & Bartlett, 2004).
Caregivers of disabled children, especially mothers, experience negative emotions and intense emotional conflicts with their disabled children. Vaughn & Leff (1976) introduced the expressed emotion (EE) scale. They found that close caregivers of patients with mental disorders, especially mothers, express negative emotions, such as violence and severe criticism towards the sick member of the family (Khoshgoftar et al., 2022). Hastings et al. (2006) reported that mothers of children with intellectual disabilities have negative emotions, such as criticism towards their children. These mothers experience depression and distress while caring for their children. Coleman (2010) showed that the emotions expressed by mothers of children with fragile X syndrome are accompanied by emotional involvement, hostility, and criticism toward their children.
Although mothers with disabled children experience intense stress and low quality of life, few psychological programs and interventions address their needs. Some psychological interventions for the family include cognitive-behavioral therapy interventions and psychological training (Romero-Gonzalez et al., 2018). Mindfulness-based stress reduction (MBSR) emerges as a practical approach for these parents to improving their physical and mental health (Benn et al., 2012). A study documented that the MBSR program can effectively reduce stress and improve the psychological well-being of parents of children with developmental disabilities (Bazzano et al., 2015).
The MBSR program was proposed by Kabat-Zinn (1990) at the University of Massachusetts Chan Medical School. MBSR, a client-centered therapy, employs structured intensive psychological training in many clinical environments, hospitals, and schools. Mindfulness techniques help people observe their consciousness impartially and without judgment, reducing stress and regulating emotions (Petcharat, 2018). A meta-analysis study concluded that mindfulness intervention could reduce parenting stress and be an effective treatment option to help parents (Burgdorf et al., 2019). Because of its flexibility, mindfulness-based therapy can be combined with other treatments. For example, a mindfulness yoga program (MiYoga) could help reduce the stress of parents of children with cerebral palsy (Mak et al., 2019).
Narrative therapy is a new solution-focused treatment combining narrative and solution-focused treatments. Solution-focused narrative therapy (SFNT) can help people with psychological stress cope with their problems. As the name suggests, narrative therapy means telling the story of our identity and its related meanings. Narrative therapy helps clients develop a new way of telling their story, different from the problematic path. The new story involves one’s hopes, values, and commitments. The therapist helps the client extensively draw paths, narratives, life events, opportunities, and possibilities (White & Morgan, 2006; Metcalf, 2017; Metcalf, 2021). Instead of focusing on the problems, the clients create a distance between themselves and the problems by highlighting the possible effects of the problems in their lives. Narrative therapy tries to separate the nature of the client from their problems. In this way, clients can discover their positive abilities and get a better and more straightforward narrative of the nature of their lives and themselves (Riley & Malchiodi, 2003; Chang & Nylund, 2013). SFNT aims to participate clients effectively and meaningfully in their life choices (Metcalf, 2017). It can give people the independence to redefine their lives and engage in their decisions. SFNT is a holistic model derived from two language-based therapies with a postmodern perspective. The therapist and client collaborate in creating a solution-focused narrative framework for rewriting the client’s life (Riley & Malchiodi, 2003; Chang & Nylund, 2013).
Previous studies have shown the effectiveness of SFNT for other clinical groups, including the quality of life of cancer patients (Perry, 2020) and the life of couples after marital infidelity (Saunders, 2020). Schwellnus et al. (2020) used solution-focused therapy to help children and adolescents with cerebral palsy disabilities set life goals. Their results show that, after completing the intervention, the participants can determine their life goals. Another study examined the impact of narrative therapy on children with developmental disabilities and their parents in India. The results support that parents and their children welcome the opportunities created to change and rewrite their life stories. The study also shows how narrative therapy can make a difference in the lives of children, their families, and the wider community (Baldiwala & Kanakia, 2022).
Mothers with disabled children experience many psychological and physical stresses due to long-term care of their children (Khodabakhshi-Koolaee et al., 2019). These stresses lead to psychological problems and decrease parent-child interaction quality due to negative emotions, such as criticism and violence. As detailed above, SFNT has been employed in other clinical groups, but its effectiveness has not been explored in mothers of boys with gross motor disabilities. This therapy is necessary because, during the treatment process, mothers modify their internalized stories, expect more about their destinies, and ultimately have better control over their lives (White & Morgan, 2006). Moreover, considering the higher prevalence and risk factors of developmental and gross motor delay among boys than girls (Soleimani et al., 2018; Veldman et al., 2020), it is crucial to compare the effectiveness of SFNT and MBSR on the level of EE in mothers of male children with gross motor disabilities.
2. Materials and Methods
Design, setting, and sample
This quasi-experimental study employed a pre-test-post-test design with a control group.
The sample size was estimated at 45 mothers based on the Equation 1:
To recruit participants, 81 mothers were initially assessed for eligibility. Then, 36 subjects were excluded due to not meeting inclusion criteria (n=22), reluctance to participate in the intervention (n=10), and other reasons (n=4) (Figure 1). In the next step, 45 mothers were randomly assigned to 2 intervention groups and 1 control group by drawing lots to minimize confounders and eliminate systematic bias.
The inclusion criteria were having a son with one of the gross motor disabilities, not being divorced (due to life problems for female heads of the family), and literacy for reading and writing. The exclusion criteria were absence in more than two therapy sessions and simultaneous participation in other psychotherapy programs.
Study instruments
The study instruments were as follows.
The demographic form included the mother’s age, education level, and child’s age.
The level of expressed emotion (LEE) scale was used to evaluate the quality of mothers’ EE. The scale was developed by Cole & Kazarian (1988) to investigate the perceived emotional climate in a person’s influential relationships. This scale has 60 items and 4 subscales: Intrusiveness, emotional response, attitude toward illness, and tolerance/expectations. Each item is scored from 1 to 4 (1=untrue, 2=somewhat untrue, 3=somewhat true, and 4=true). The total scores ranged from 60 to 240, with higher scores indicating more intense emotional involvement. The Cronbach α values for intrusiveness, emotional response, attitude toward illness, and tolerance/expectations are 0.667, 0.89, 0.84, and 0.78, respectively. In addition, The Cronbach α for the whole scale is 0.94 (Cole & Kazarian, 1988). This questionnaire was first translated into Persian by Dehghani (2003), and its reliability was reported by calculating the Cronbach α as 0.93. In this study, the Cronbach α of this scale was calculated as 0.91. This scale was completed through self-reporting by mothers participating in the research in the pre-test and post-test stages.
Study procedure
A total of 45 mothers with male children suffering from gross motor disabilities were selected and randomly assigned to three equal groups, each comprising 15 persons. Each therapy intervention (SFNT and MBSR) was conducted 2 days per week. To this end, the SFNT sessions were held on Saturdays from 10-12 AM for 9 consecutive weeks. Each session took 90 minutes (White & Morgan, 2006; Metcalf, 2017), and the MBSR sessions were held on Tuesdays from 10-12 AM for 8 consecutive weeks. Each session took 90 minutes (Petcharat, 2018; Reibel & McCown, 2019). All sessions were held in person at the “Success Counselling Center” in Tehran Province, Iran. All the sessions were conducted in groups and by psychoeducation (e.g. giving information verbally, written materials and handouts, exercise or homework to encourage the mothers to discover information for themselves), question and answer, and dialogue between the therapist and the mother. The therapist was a PhD student in Family Counseling. One week after the end of the intervention sessions, a post-test was taken from all three groups.
Tables 1 and 2 show a summary of the content of the SFNT and MBSR sessions.
Data analysis
The collected data were analyzed using descriptive statistics, such as frequency, percentage, Mean±SD. In addition, the multivariate analysis of variance (MANOVA) and least significant difference (LSD) post hoc test were used to compare the groups. The data were analyzed using SPSS software, version 26. The significance level was set at P<0.05.
3. Results
The average age of the mothers participating in this study was 40.02±3.4 years, and the mean age of their children was 9.06±2.8 years. The personal characteristics of the subjects are presented in Table 3.
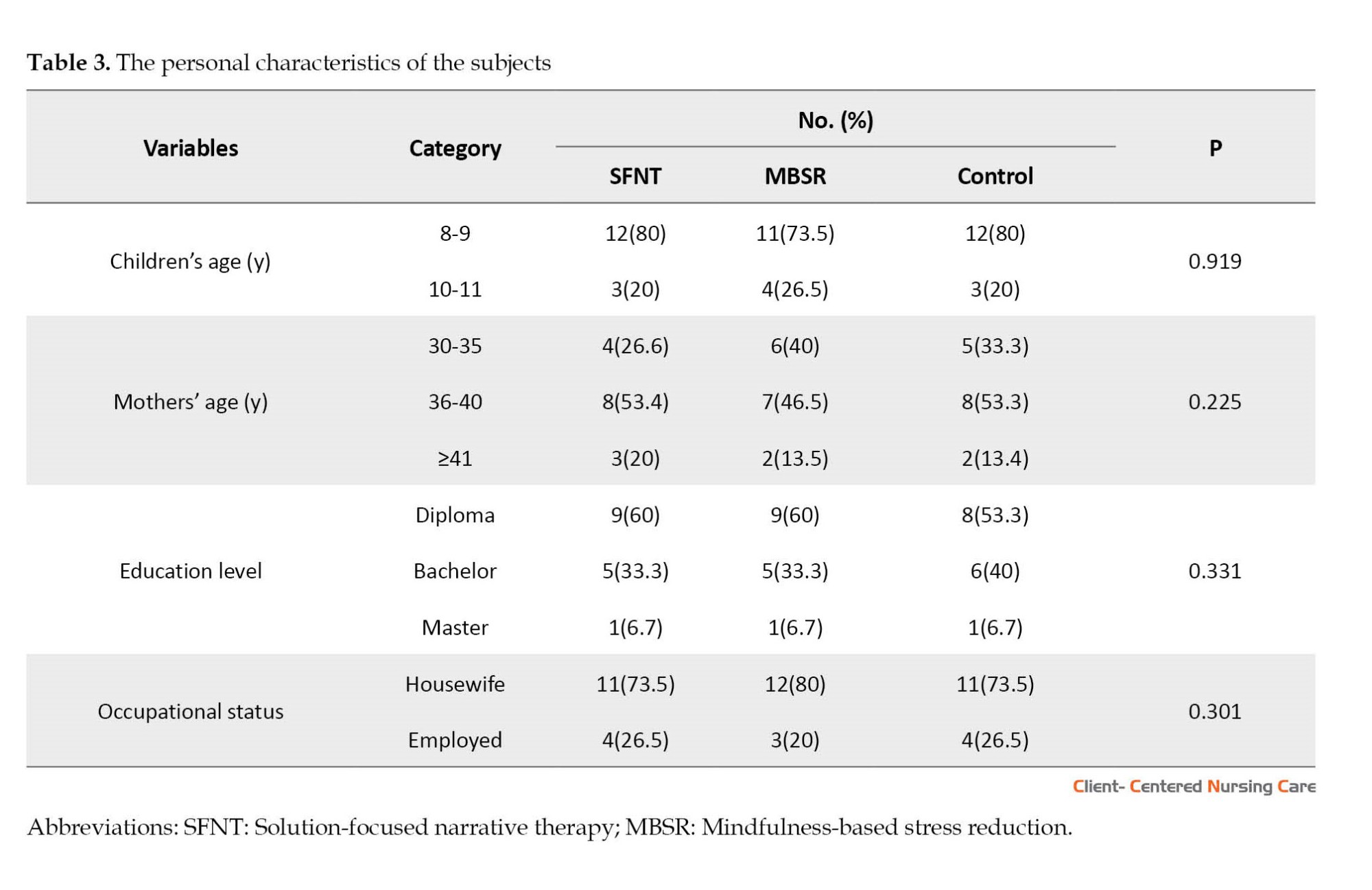
Table 4 details the descriptive statistics for EE and its subscales in the intervention and control groups in the pre-test and post-test phases.
Analysis of covariance (ANCOVA) was run to compare the group means. Prior to ANCOVA, the assumptions of this test were first checked using Levene’s and Box’s M tests. Because the results were not significant (P>0.05), ANCOVA was subsequently performed.
As can be seen in Table 5, the F values for the components of negative attitude towards illness (F=11.70, P=0.02), intrusiveness (F=14.54, P=0.03), emotional response (F=12.88, P=0.01), and tolerance/expectations (F=11.23, P=0.01) were significant, indicating significant between-group differences in terms of the mentioned variables. A comparison of the group means also suggested that the mean values were greater for the SFNT group than the control group. This finding indicates that SFNT is effective in the level of EE of mothers of children with gross motor disabilities.
As can be seen in Table 6, the F values for the components of negative attitude towards illness (F=16.48, P=0.02), intrusiveness (F=10.98, P=0.03), emotional response (F=13.37, P=0.01), and tolerance/expectations (F=18.54, P=0.01) were significant, indicating significant between-group differences in terms of the mentioned variables. A comparison of the group means also suggested that the mean values were greater for the MBSR group than the control group. This finding indicates that MBSR is effective in the level of EE of mothers of children with gross motor disabilities.
The results of multivariate ANCOVA by taking the pre-test scores as control variables are shown in Table 7. Wilks’ lambda test results indicated significant differences between the three groups in the post-test scores (F=2.521, P<0.01).
.jpg)
Pairwise comparisons using the LSD post hoc test (Table 8) showed that the two intervention groups had significant differences in mothers’ EE (P<0.05), indicating that SFNT was more effective than (MBSR therapy in reducing mothers’ EE (P<0.01).
4. Discussion
The present study compared the effectiveness of SFNT and MBSR on the level of EE in mothers of male children with gross motor disabilities. The results showed that both therapies significantly reduced the expression of the mothers’ negative emotions, such as aggression and criticism. Parents with disabled children express strong negative feelings through aggression and criticism towards their children with developmental disabilities (Thompson et al., 2018; Stiles-Shields et al., 2022). However, in this study, the demographic characteristics of mothers were controlled across all groups, and there was no significant difference between them. Still, it is acknowledged that the mother’s stress level and emotional expression could be partly related to socio-demographic variables. For example, a study found that unemployed mothers and those with lower education exhibited higher levels of parental distress than employed mothers (Fucà et al., 2022).
The data in this study showed that MBSR intervention can help reduce the expressed negative emotions of mothers. Mothers with disabled children endure high levels of stress, expressed through aggression, criticism, or emotional over-involvement due to repeated failures in dealing with their child’s physical problems and other people’s behavior. A study used mindfulness-based positive behavior support training for 3 months to reduce the stress of mothers of adolescents with autism spectrum disorder, and the results showed that teaching mothers was accompanied by an increase in their children’s compliance behaviors and ultimately led to a reduction in parenting stress level (Singh et al., 2014).
MBSR is a non-judgmental therapy that helps people consciously increase their awareness of the present moment because they perform guided mindfulness practices that cover many aspects of daily life, such as breathing, bodily sensations, movement, and eating (Semple & Hatt, 2012; Epstein, 2010). In another study, Crawley et al. (2022) used mindfulness-based music and songwriting to help reduce the psychological distress and problems of mothers of children with disabilities. After 4 weeks, they observed a significant reduction in mothers’ psychological problems. It is believed that the effectiveness of MBSR is more prominent in reducing the parenting stress of mothers with disabled children (Sing et al., 2014; Burgdorf et al., 2019). For example, a meta-analysis study by Chua and Shorey revealed that mindfulness- and acceptance commitment therapy (ACT)-based interventions effectively reduced stress, anxiety, and depression of parents of children with developmental disabilities. Nevertheless, these interventions were not effective in raising parents’ mindfulness. These conflicting results could be attributed to the religious and cultural differences between Eastern and Western societies and how people perceive the world. Compared to other religions and Western cultures, Muslims and Buddhists believe in the effectiveness of mindfulness-based therapy in reducing stress as they have already experienced moments of mindfulness in their prayers and worship (Chua & Shorey, 2021). Therefore, cultural and religious factors could have strengthened the effect of MBSR intervention on the reduction of expressed emotions of Iranian mothers.
Studies have revealed that SFNT increases social participation and informed decisions of people with cerebral palsy Schwellnus et al. (2020) and reduces psychological distress in mothers with disabled children (Baldiwala & Kanakia, 2022). This therapy has also been effective in other children’s problems in the family. However, previous studies have not directly reported reduced negative emotional expression in mothers of children with motor disabilities. For example, D’Abate used the SFNT intervention to resolve conflicts related to child custody rights in conflicting couples, and the results indicated a reduction in the psychological stress of children and their parents and the creation of alternative solutions to help the family (D’Abate, 2016). Besides, Myers and colleagues (2006) used SFNT in a case study to treat a boy who experienced sexual abuse. The results showed that SFNT helped the child have a new life narrative and overcome his problems with conscious decisions.
A comparison of the effectiveness of these two therapies showed that SFNT was more effective than MBSR. This difference could be attributed to the nature of these therapies. Mindfulness therapies focus on meditation techniques, relaxation, and mindfulness of a person’s life moment by moment, while SFNT is a postmodern therapy that requires more exploration and meditation on narratives, how people make decisions in life, and their greater participation in their life events (Ricks et al., 2014). Thus, SFNT can be effective in the mother’s EE, which is more influenced by the change of life story, the creation of new narratives, and ultimately, the feeling of more control over life. In narrative therapy, mothers could talk freely about their feelings, thoughts, and life experiences that they previously had difficulty expressing. They face an opportunity to talk about their bitter experiences and internalized stigma and try to find new and creative solutions with the therapist’s help. Mothers in the group rewrote their life stories, and rewriting the life story led to their creativity and finally discovering new aspects of their lives.
This study was conducted with some limitations. First, it examined only the mothers from one counseling center in Tehran. Second, due to procedural problems, it was impossible to follow up on the effectiveness of the two therapies in the long term. The third limitation of this study was the random allocation of groups by drawing lots, which did not guarantee the possibility of removing the complete influence of the confounders. Therefore, it is recommended to conduct a similar study in more centers, follow up on the durability of the interventions, and randomly assign groups using more reliable methods.
5. Conclusion
The results showed that both therapies can reduce the expression of negative emotions in the mothers of children with gross motor disabilities. However, SFNT had a more significant effect on lowering negatively expressed feelings. Due to psychological pressures and burdens on mothers or their lack of familiarity with the complex concepts of child management behavior treatments, they cannot strictly implement therapeutic instructions. Therefore, providing opportunities for training and group counseling, discussion, and question and answer sessions gives mothers more possibilities to help care for themselves and their children. In future research, it is suggested that the newer MBSR methods, Yoga and meditation, be used to reduce the psychological stress of mothers. Also, SFNT therapeutic intervention should be done by emphasizing the redefined narrative of the mother and father (parents) about the child’s disability and their EE.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the North Tehran Branch, Islamic Azad University (Code: IR.IAU.TNB.REC.1401.055) and Informed written consent was obtained from all the subjects. To comply with ethical guidelines, 6 training sessions were held for the control group after completing the interventions.
Funding
This study was extracted from PhD dissertation of Behnaz Karami, approved by Department of Counseling, North Tehran Branch, Islamic Azad University.
Authors' contributions
Conducting research, data gathering and analysis: Behnaz Karami; Conceptualization, study design, and drafting of the initial version: Anahita Khodabakhshi-Koolaee; Data analysis: Hassan Heidari and Hossein Davoodi; Supervision: Anahita Khodabakhshi-Koolaee, Hassan Heidari and Hossein Davoodi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants who contributed to conducting this research project.
References
Baldiwala, J. & Kanakia, T., 2022. Using narrative therapy with children experiencing developmental disabilities and their families in India: A qualitative study. Journal of Child Health Care, 26(2), pp. 307-18. [DOI:10.1177/13674935211014739] [PMID]
Bazzano, A., et al., 2015. Mindfulness-based stress reduction (MBSR) for parents and caregivers of individuals with developmental disabilities: A community-based approach. Journal of Child and Family Studies, 24, pp. 298-308. [DOI:10.1007/s10826-013-9836-9]
Benn, R., et al., 2012. Mindfulness training effects for parents and educators of children with special needs. Developmental Psychology, 48(5), pp. 1476-87. [DOI:10.1037/a0027537] [PMID]
Burgdorf, V., Szabó, M. & Abbott, M. J., 2019. The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: A systematic review and meta-analysis. Frontiers in Psychology, 10, pp. 1336. [DOI:10.3389/fpsyg.2019.01336] [PMID]
Chang, J. & Nylund, D., 2013. Narrative and solution-focused therapies: A twenty-year retrospective. Journal of Systemic Therapies, 32(2), pp. 72-88. [DOI:10.1521/jsyt.2013.32.2.72]
Chua, J. Y. X. & Shorey, S., 2022. The effect of mindfulness-based and acceptance commitment therapy-based interventions to improve the mental well-being among parents of children with developmental disabilities: A systematic review and meta-analysis. Journal of Autism and Developmental Disorders, 52(6), pp. 2770-83. [DOI:10.1007/s10803-021-04893-1] [PMID]
Cole, J. D. & Kazarian, S. S., 1988. The level of expressed emotion scale: A new measure of expressed emotion. Journal of Clinical Psychology, 44(3), pp. 392-7. [DOI:10.1002/1097-4679(198805)44:33.0.CO;2-3] [PMID]
Coleman, J. M., 2010. The expressed emotion of mothers of children with fragile X syndrome [PhD dissertation]. Denver: University of Denver. [Link]
Crawley, Z., 2022. Mindfulness-based music and songwriting: Pilot data from a novel telehealth intervention for parents of children with disabilities [PhD dissertation]. Nashville: Vanderbilt University. [Link]
D’Abate, D. A., 2016. Use of solution-focused and family narrative approaches in working with high conflict families: Strategies and techniques that can be utilized in parenting coordination and co-parenting coaching. Journal of Child Custody, 13(4), pp. 269-88. [DOI:10.1080/15379418.2016.1247308]
Dehghani, S. H., 2003. [Expressed emotion and sexuality (Persian)]. Journal of Fundamental Mental Health, 5(19-20), pp. 84-91. [Link]
Hastings, R. P., et al., 2006. Maternal distress and expressed emotion: Cross-sectional and longitudinal relationships with behavior problems of children with intellectual disabilities. American Journal on Mental Retardation, 111(1), pp. 48-61. [DOI:10.1352/0895-8017(2006)111[48:MDAEEC]2.0.CO;2]
Epstein, B. J., 2010. Effects of a mindfulness-based stress reduction program on fathers of children with a developmental disability [PhD dissertation]. New York: Hofstra University. [Link]
Fucà, E., et al., 2022. Parenting stress in mothers of children and adolescents with down syndrome. Journal of Clinical Medicine, 11(5), pp. 1188. [DOI:10.3390/jcm11051188] [PMID]
Kabat-Zinn J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing. [Link]
Khodabakhshi-Koolaee, A., Koshki, M. A. & Kalhor, N., 2019. [Analysis of the experiences of mothers in caring for a disabled child: A phenomenological Study (Persian)]. Iranian Journal of Pediatric Nursing, 6(2), pp. 68-75. [Link]
Khodabakhshi Koolaee, A. & Derakhshandeh M., 2015. [Effectiveness of hope-oriented group therapy on life meaning and resilience in mothers with physical-motor disabled children (Persian)]. Journal of Pediatric Nursing, 1(3), pp. 15-25.
Khoshgoftar, M., Khodabakhshi-Koolaee, A. & Sheikhi, M. R., 2022. Analysis of the early mother-child relationship in schizophrenic patients. International Journal of Social Psychiatry, 68(3), pp. 548-54. [DOI:10.1177/0020764021991186] [PMID]
Mak, C. K., Whittingham, K. & Boyd, R. N., 2019. Experiences of children and parents in MiYoga, an embodied mindfulness yoga program for cerebral palsy: A mixed method study. Complementary Therapies in Clinical Practice, 34, pp. 208-16. [DOI:10.1016/j.ctcp.2018.12.006.] [PMID]
Metcalf, L., 2017. Solution-focused narrative therapy. New York: Springer Publishing Company. [DOI:10.1891/9780826131775]
Metcalf, L., 2021. Counseling toward solutions: A practical, solution-focused program for working with students, teachers, and parents. New York: Routledge. [DOI:10.4324/9781003122128]
Morris, C. & Bartlett, D., 2004. Gross motor function classification system: Impact and utility. Developmental Medicine and Child Neurology, 46(1), pp. 60-5. [DOI:10.1017/S0012162204000118] [PMID]
Perry, V., 2020. A solution-focused narrative therapeutic approach to improving quality of life with cancer patients participating in group therapy [PhD dissertation]. Texas: Texas Wesleyan University. [Link]
Petcharat, M., 2018. The effects of a brief culturally tailored Thai mindfulness intervention on stress, anxiety, and mindfulness in Thai parents of children with developmental disabilities [PhD dissertation]. Boca Raton: Florida Atlantic University. [Link]
Reibel, D. & McCown, D., 2019. Mindfulness-based stress reduction: Theory, practice and evidence base. In: I. Ivtzan (ed), Handbook of mindfulness-based programmes (pp. 29-41). London: Routledge. [DOI:10.4324/9781315265438-4]
Ricks, L., et al., 2014. My story: The use of narrative therapy in individual and group counseling. Journal of Creativity in Mental Health, 9(1), pp. 99-110. [DOI:10.1080/15401383.2013.870947]
Riley, S. & Malchiodi, C. A., 2003. Solution-focused and narrative approaches. In: C. A. Malchiodi (ed), Handbook of art therapy ( pp. 82-92). New York: The Guilford Press. [Link]
Romero-Gonzalez, M., Chandler, S. & Simonoff, E., 2018. The relationship of parental expressed emotion to co-occurring psychopathology in individuals with autism spectrum disorder: A systematic review. Research in Developmental Disabilities, 72, pp. 152-65. [DOI:10.1016/j.ridd.2017.10.022] [PMID]
Saunders, L. M., 2020. A solution-focused narrative therapeutic approach to restoring couple relationships after infidelity [PhD dissertation]. Texas: Texas Wesleyan University. [Link]
Schwellnus, H., et al., 2020. A solution-focused coaching intervention with children and youth with cerebral palsy to achieve participation-oriented goals. Physical & Occupational Therapy in Pediatrics, 40(4), pp. 423-40. [DOI:10.1080/01942638.2020.1711841] [PMID]
Semple, R. J. & Hatt, S. P., 2012. Translation of Eastern meditative disciplines into Western psychotherapy. In: L. J. Miller (ed), The Oxford handbook of psychology and spirituality. Oxford: Oxford University Press. [DOI:10.1093/oxfordhb/9780199729920.013.0021]
Singh, N. N., et al., 2014. Mindfulness-based positive behavior support (MBPBS) for mothers of adolescents with autism spectrum disorder: Effects on adolescents’ behavior and parental stress. Mindfulness, 5, pp. 646-57. [DOI:10.1007/s12671-014-0321-3]
Soleimani, F., et al., 2018. [Relationship between gender and development status in children (Persian)]. Archives of Rehabilitation, 18(4), pp. 338-45. [DOI:10.21859/jrehab.18.4.8]
Stiles-Shields, C., et al., 2023. Caregiver expressed emotion in families of youth with spina bifida: Demographic, medical, and family correlates. Journal of Pediatric Psychology, 48(2), pp. 144-55. [DOI:10.1093/jpepsy/jsac073] [PMID]
Thompson, T., Coleman, J. & Olmos, A., 2018. The expressed emotion of parents of children with developmental disabilities: A meta-analysis. Life Span and Disability, 21(2), pp. 177-89. [PMID]
Vaughn, C. & Leff, J., 1976. The measurement of expressed emotion in the families of psychiatric patients. British Journal of Social and Clinical Psychology, 15(2), pp. 157-65. [DOI:10.1111/j.2044-8260.1976.tb00021.x] [PMID]
Veldman, S. L., et al., 2020. Prevalence and risk factors of gross motor delay in pre-schoolers. Journal of Paediatrics and Child Health, 56(4), pp. 571-6. [DOI:10.1111/jpc.14684] [PMID]
White, M. K. & Morgan, A., 2006. Narrative therapy with children and their families. Adelaide: Dulwich Centre Publications. [Link]
Type of Study: Research |
Subject:
Special
Received: 2023/03/3 | Accepted: 2023/06/24 | Published: 2023/11/1
Received: 2023/03/3 | Accepted: 2023/06/24 | Published: 2023/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






