Fri, Oct 18, 2024
[Archive]
Volume 10, Issue 1 (Winter 2024)
JCCNC 2024, 10(1): 35-44 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hakimi H, Afsaneh Abadi P, Momeni M. Association Between Fear of Hypoglycemia and Treatment Satisfaction Among Patients With Diabetes Mellitus. JCCNC 2024; 10 (1) :35-44
URL: http://jccnc.iums.ac.ir/article-1-489-en.html
URL: http://jccnc.iums.ac.ir/article-1-489-en.html
1- Metabolic Diseases Research Center, Research Institute for Prevention of Non-communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran.
2- School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran.
3- Metabolic Diseases Research Center, Research Institute for Prevention of Non-communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran. ,momeni65@gmail.com
2- School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran.
3- Metabolic Diseases Research Center, Research Institute for Prevention of Non-communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran. ,
Full-Text [PDF 628 kb]
(236 Downloads)
| Abstract (HTML) (1068 Views)
• Treatment satisfaction is one of the critical factors of care quality in patients with diabetes mellitus.
• One of the main side effects of treatment with antidiabetic drugs in patients with type 2 diabetes is hypoglycemia, which may cause fear of hypoglycemia in these patients.
• Treatment satisfaction was significantly associated with fear of hypoglycemia in this study.
• Being female, diabetes complications, low education level, and severe or very severe hypoglycemia were associated with lower satisfaction with treatment in patients with type 2 diabetes taking oral antidiabetic drugs.
• One of the main side effects of treatment with antidiabetic drugs in patients with type 2 diabetes is hypoglycemia, which may cause fear of hypoglycemia in these patients.
• Treatment satisfaction was significantly associated with fear of hypoglycemia in this study.
• Being female, diabetes complications, low education level, and severe or very severe hypoglycemia were associated with lower satisfaction with treatment in patients with type 2 diabetes taking oral antidiabetic drugs.
Plain Language Summary
Treatment of diabetes mellitus is a complex process. One of the most important concerns in the treatment of diabetes is maintaining an appropriate level of blood sugar along with preventing hypoglycemic episodes. Following the experience of hypoglycemia, patients may develop a fear of hypoglycemia and, thus, non-adherence to treatment. The findings of the present study indicated that the fear of hypoglycemia is related to a decrease in patients’ satisfaction with treatment. Therefore, the determination of patients at risk of fear of hypoglycemia by health care workers can be effective in improving treatment satisfaction and quality of life of these patients.
Full-Text: (116 Views)
Introduction
Diabetes mellitus is one of the prevalent non-communicable and metabolic diseases with debilitating effects. Meanwhile, rapid economic growth and urbanization have increased its prevalence worldwide (Onyango & Onyango, 2018). It is estimated that the number of diabetes will increase to 600 million people by 2035, more than 80% of whom live in developing countries (Bakker et al., 2016). It was reported that 85.5% of Iranians suffer from type 2 diabetes mellitus (T2DM) (Esteghamati et al., 2017).
Treating T2DM involves a complex and multidisciplinary process (Williams et al., 2012). Glycemic control without hypoglycemia is one of the main challenges in diabetes treatment (Stargardt et al., 2009). Despite various antidiabetic treatments, most T2DM patients do not achieve optimal glycemic control (Avramopoulos et al., 2015). Severe and recurrent hypoglycemia may lead to fear of hypoglycemia in patients with T2DM (Sheu et al., 2012) and adverse effects on diabetes management (Erol & Enc, 2011). Fear of hypoglycemia is associated with negative feelings such as psychological distress and anxiety in patients with diabetes. It is also considered a barrier to glycemic control, which negatively affects the self-management, quality of life, and mental health of patients with diabetes (Hapunda et al., 2020; Huang et al., 2022).
Treatment satisfaction is an essential indicator of the quality of care (Othman et al., 2015). It is defined as the “confirmation of expectations” for a patient, that is, the agreement between the patient’s expectations from the treatment and the results obtained (Alcubierre et al., 2014). To achieve treatment satisfaction, it is essential to understand the patient’s perspective on the current medication (Khdour et al., 2020). The patient’s negative attitude toward the effectiveness of the treatment is an important obstacle to adherence to treatment (Farhat et al., 2019). Many antidiabetic treatments lead to hypoglycemia and are therefore perceived by the patient as unpleasant and life-threatening, which may affect treatment adherence (Walz et al., 2014). Fear of hypoglycemia can lead to inadequate blood sugar control and blood sugar-increasing behaviors such as high carbohydrate intake, avoiding exercise, and reducing the dose of antihyperglycemic medications (Mitchell et al., 2013).
Considering that treatment satisfaction can increase the effectiveness of treatment and adherence to it, as well as blood sugar control (Chang et al., 2023), it seems necessary to investigate treatment satisfaction in patients with T2DM and its related factors. According to our search, no study has specifically focused on the relationship between fear of hypoglycemia and satisfaction with treatment in these patients. Therefore, the present study was carried out to assess the relationship between fear of hypoglycemia and satisfaction with treatment in Iranian patients with T2DM.
Materials and Methods
This cross-sectional study was conducted in the outpatient clinic of Velayat Hospital in Qazvin Province, Iran, in 2021. A total of 390 patients with T2DM treated with oral antidiabetic drugs were recruited by convenience sampling. The inclusion criteria were as follows: Being 18 years old or older, suffering from T2DM as diagnosed by the hospital doctor, and taking antihyperglycemic medication for at least 6 months. Patients with type 1 diabetes, pregnant women, and those treated with insulin were excluded from the study.
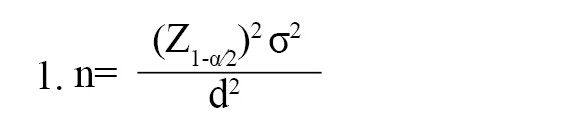
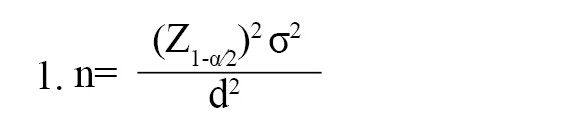
Considering a type I error of 0.05, a standard deviation of the fear of hypoglycemia in patients with T2DM as 8.6 (Yeke Fallah, 2019), a precision of 0.9, and a probability of 10 % missing data, the sample size was estimated to be 390 based on the Equation 1:
The data were collected using demographic and clinical characteristics questionnaires, diabetes medication satisfaction (DiabMedSat), and hypoglycemia fear survey-II (HFS).
The first part of the questionnaire included demographics (age, gender, education level, employment, marital status) and clinical characteristics (family history of diabetes, name and number of oral antihyperglycemic drugs, diabetes complications, hypoglycemia experience, and severity of hypoglycemia) of the patients. Complications of diabetes were assessed by asking patients and referring to their medical records. Answers to the question, “Have you ever felt symptoms of hypoglycemia?” (such as sweating, confusion/feeling disoriented, shakiness, clumsy or jerky movements, dizziness, sudden moodiness or behavior changes, hunger, tingling sensations around the mouth, difficulty concentrating, headache, and pale skin color) were used to evaluate patients’ reports of hypoglycemia symptoms in the past 6 months. According to recommendations of the American Diabetes Association Hypoglycemia Workgroup, the patients with hypoglycemia rated their hypoglycemia severity by selecting one of the following choices: 1) Mild (little or no interruption of activities and no assistance needed to manage symptoms), 2) Moderate (some interruption of activities and no assistance needed to manage symptoms), 3) Severe (needed the assistance of others to manage symptoms e.g. to bring food or drink, and 4) Very severe (requires medical attention including calling an ambulance, going to the emergency room or hospital, or seeing a doctor or nurse) (Marrett et al., 2011).
DiabMedSat contains 21 items divided into three domains: The burden domain (11 items) measures any bothersome aspect of treatment, the efficacy domain (5 items) measures satisfaction with any physical or emotional effects of treatment, and the symptoms domain (5 items) evaluates symptoms that may have occurred as a result of the treatment. Each item is rated on a 7-point Likert scale ranging from 1 (never/not at all/not at all bothered/extremely dissatisfied) to 7 (all the time/extremely/extremely bothered/extremely satisfied) by the subjects. The range of raw scores of the subscales and the whole questionnaire is as follows: Burden, 11-57; efficacy, 5-33; symptom, 5-30; total (DiabMedSat), 120. The scores are then transformed from 0 to 100. The total score of each domain will be the result of the mean score of the items in that domain. The mean of the three domain scores determines the total score. Total and domain scores range from 0 to 100. A higher score indicates greater levels of treatment satisfaction. Items 1 (a-d), 2 (a-e), 5 (a-d), and 6 (a-c) are scored reversely. The DiabMedSat has acceptable internal consistency with an alpha coefficient=0.9 (Brod et al., 2006).
There are two subscales in the HFS-II: Behavioral and worry (Gonder-Frederick et al., 2011). Both subscales of the survey can be analyzed separately (Przezak, Bielka, & Molęda, 2022). This study evaluated patients’ concerns about hypoglycemia episodes using the HFS-worry subscale (HFS-W) alone (Atallah et al., 2020; Marrett et al., 2011; Sheu et al., 2012; Wild et al., 2007; Yeke Fallah et al., 2019). The HFS-W is composed of 18 items rated on a 5-point Likert scale ranging from 0 (never) to 4 (always) and is scored from 0 to 72 (most worry) (Gonder-Frederick et al., 2011). The HFS-W has high internal consistency (α=0.94) (Gonder‐Frederick et al., 2013).
The above instruments were translated into Persian by a PhD candidate in translation studies who then back-translated them into English. The content validity of the instruments was confirmed by 10 faculty members of the Nursing Department of Qazvin University of Medical Sciences. Content validity index (CVI) and content validity ratio (CVR) were calculated for the Persian version of the HFS-W subscale and the Persian version of DiabMedSat, and the results were (CVR=0.74, CVI=0.86) and (CVR=0.78, CVI=0.89), respectively. The reliability of the questionnaires was tested on 20 patients with T2DM before the final versions of the instruments were considered ready to use. The internal consistency reliability (α) for the Persian version of HFS-W was 0.96 and for the Persian version of DiabMedSat was 0.81. All the questionnaires were completed through face-to-face interviews with the subjects by the second author.
Data analysis
Continuous variables were presented by Mean±SD, whereas categorical variables as frequency and percentage. Univariate analysis (using the independent t-test, one-way analysis of variance, and Pearson correlations) was initially conducted to assess relationships between the independent variables and treatment satisfaction. A multiple linear regression with a backward elimination method was performed to determine potential factors that might affect the treatment satisfaction of patients with T2DM so that the dependent variable was treatment satisfaction, and the factors with P<0.05 in the univariate analysis were considered the independent variables. P<0.05 was considered statistically significant. The SPSS software, version 26 statistical software was used for data analysis.
Results
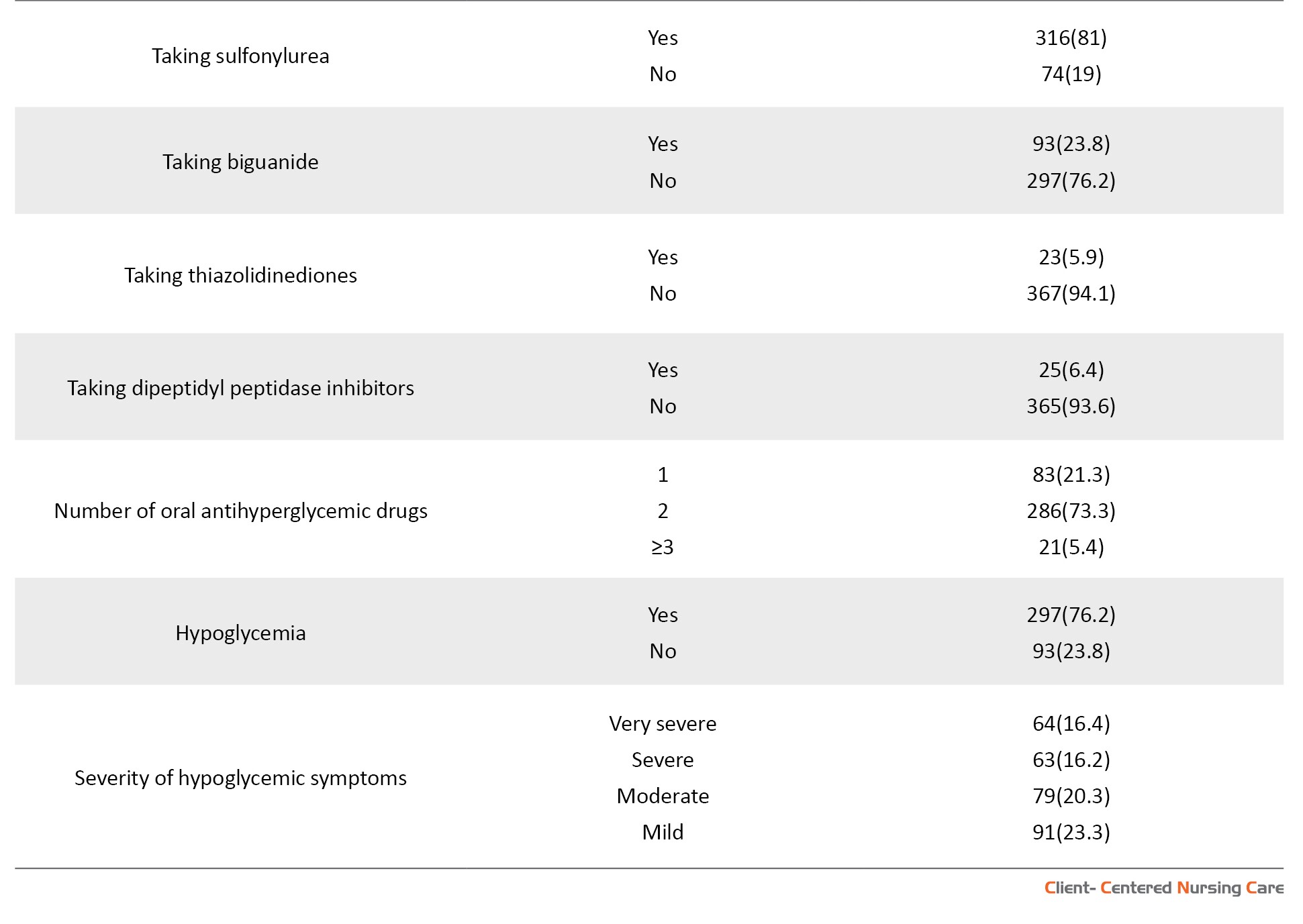
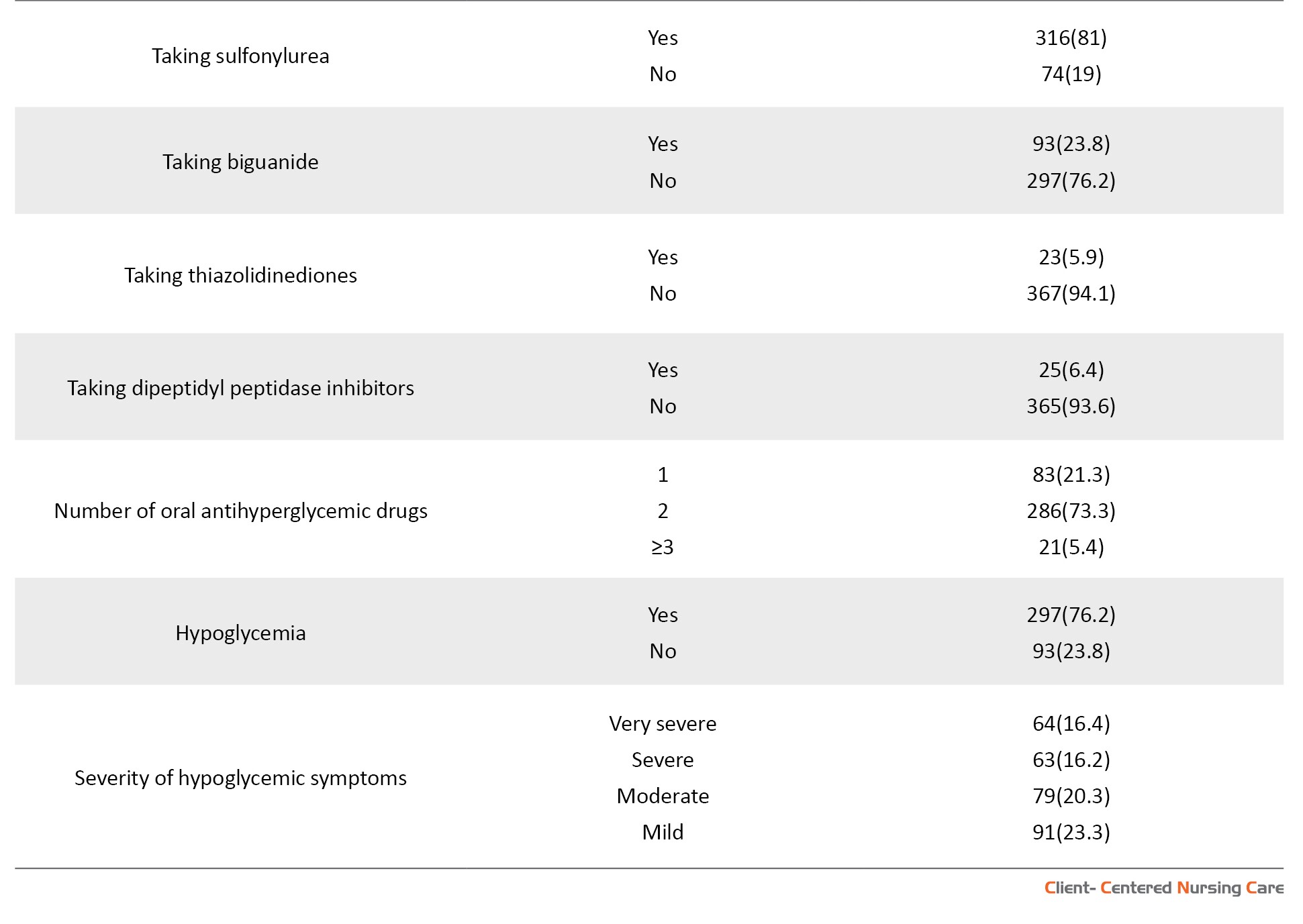
Demographic and clinical characteristics are summarized in Table 1. The Mean±SD age of the subjects was 53.49±11.49 years. Most patients were female (57.4%) (Table 1).

The mean scores of treatment satisfaction and fear of hypoglycemia are presented in Table 2.

Univariate analysis using the Pearson correlation test indicated that fear of hypoglycemia is negatively correlated with treatment satisfaction (r=-0.504, P<0.001). Treatment satisfaction is negatively associated with age (r=-0.248, P<0.001) and diabetes duration (r=-0.343, P<0.001). The univariate relationships of diabetes treatment satisfaction and categorical variables are shown in Table 3.

In multivariate linear regression analysis, treatment satisfaction scores were lower in females (β=-0.12, P<0.007) and patients with diabetes complications (β=-0.138, P<0.005). Patients with college (β=0.173, P<0.001) or secondary education (β=0.115, P<0.023) experienced higher treatment satisfaction than those with primary education. Patients with very severe (β=-0.29, P<0.001) or severe hypoglycemia (β=-0.157, P<0.034) experienced lower treatment satisfaction than those with mild hypoglycemia. Fear of hypoglycemia was associated with lower treatment satisfaction scores (β=-0.39, P<0.001). The regression model explained (27.7%) of the variance of treatment satisfaction (Table 4).

Discussion
The purpose of this study was to assess patients’ concerns about hypoglycemia episodes using the HFS-W.
In the current study, fear of hypoglycemia was significantly associated with lower treatment satisfaction. To the best of our knowledge, this study is one of the first of its kind to address the relationship between fear of hypoglycemia and treatment satisfaction in Iranian diabetic patients. It has been shown that the fear of hypoglycemia is related to the anxiety domain of the quality of life. At the same time, anxiety itself has been associated with lower satisfaction with treatment (Khdour et al., 2020). The fear of hypoglycemia is common among patients with diabetes. Anxiety, emotional stress, and insecurity associated with excessive fear can reduce one’s quality of life (Przezak et al., 2022).
Hypoglycemic events in patients with T2DM treated with antihyperglycemic drugs subject them to fear of hypoglycemia (Bradley et al., 2018; Sheu et al., 2012; Simon et al., 2015; Vexiau et al., 2008). The current study demonstrated that severity of hypoglycemic episodes is significantly associated with treatment satisfaction so that patients with severe hypoglycemia reported lower treatment satisfaction. This finding is consistent with previous studies showing that patients with hypoglycemic symptoms experienced non-adherence to medications and were less satisfied with treatment (Guisasola et al., 2008; Simon et al., 2015; Walz et al., 2014).
Hypoglycemia and fear of hypoglycemia may have detrimental effects on treatment satisfaction and glycemic control (Simon et al., 2015; Wang et al., 2020). To prevent hypoglycemia, patients who fear hypoglycemia tend to maintain high glucose levels. Hence, assessing patients’ fear of hypoglycemia in clinical practice and participation in individual and group psychotherapy sessions can promote the quality of diabetes care (Przezak et al., 2022). As well, patients’ satisfaction with treatment can be improved by teaching them the symptoms of hypoglycemia and how to prevent it. In line with previous studies, our study also showed that female gender is associated with lower treatment satisfaction (Nicolucci et al., 2009; Suzuki et al., 2021). According to Przezak et al., (2022), women with diabetes experience a greater fear of hypoglycemia, which can have adverse effects on their beliefs about the effectiveness of treatment. According to the findings of the present study, several studies showed that treatment satisfaction has an inverse relationship with diabetes complications in addition to being inversely related to the female gender (Atallah et al., 2020; Nicolucci et al., 2009; Zhou et al., 2019). Having complications of diabetes increases comorbidities and lowers quality of life, which can reduce satisfaction with treatment.
In contrast to the results of the current study, another study showed that patients with macrovascular complications had higher treatment satisfaction. They explained that healthcare providers probably pay more attention to patients with diabetes complications, which leads to higher treatment satisfaction. Also, they attributed the discrepancy in results to the different definitions and classifications of diabetes complications in various studies (Boels et al., 2017). In the present study, patients with higher education levels had higher treatment satisfaction. This finding was similar to other studies (Farhat et al., 2019; Zhou et al., 2019). Another study found that treatment satisfaction was positively associated with receiving diabetes education and medication counseling (Suzuki et al., 2021). Our study emphasizes the necessity of increasing patients’ awareness of diabetes and its potential complications and the importance of screening for diabetes complications.
Conclusion
Most patients with T2DM treated with oral antihyperglycemic drugs experience hypoglycemia, and the exposure of patients to hypoglycemic symptoms increases their fear of hypoglycemia. The present study showed that fear of hypoglycemia is associated with decreased satisfaction with treatment. Considering the importance of treatment satisfaction in blood sugar control and patients’ quality of life, screening patients for fear of hypoglycemia is recommended. In addition, it seems necessary to plan psychological interventions to reduce the fear of hypoglycemia in patients with T2DM.
This study has some limitations. First, the study’s cross-sectional nature allowed us to describe treatment satisfaction and fear of hypoglycemia at only one point in time. It is suggested that future studies design and implement interventions to increase treatment satisfaction with an emphasis on reducing the fear of hypoglycemia in patients with T2DM. The samples of this study were recruited from one hospital in Qazvin City, which can reduce the generalizability of the findings. Therefore, it is suggested that multicenter studies be conducted in the future to obtain more reliable evidence.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Qazvin University of Medical Sciences (IR.QUMS.REC.1399.101). The study objectives were explained to the patients, and they were assured of the confidentiality of their information. Written informed consent was obtained from all subjects.
Funding
This research received financial support from Qazvin University of Medical Sciences (Project No.: 99000233).
Authors' contributions
Conceptualization, methodology, statistical analysis, supervision, writing the original draft: Maryam Momeni and Hamideh Hakimi; Data collection: Pegah Afsaneh Abadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their special thanks to the study participants and the staff and the administrators of Velayat Hospital who helped to do this study.
References
Alcubierre, N., et al., 2014. A prospective cross-sectional study on quality of life and treatment satisfaction in type 2 diabetic patients with retinopathy without other major late diabetic complications. Health and Quality of Life Outcomes, 12(1), pp. 1-12. [DOI:10.1186/s12955-014-0131-2] [PMID]
Atallah, P., et al., 2020. Diabetes management, quality of life and treatment satisfaction in adult population in Jordan and Lebanon, observations from the SIMPLIFY study. Journal of Diabetes Mellitus, 10(02), pp. 73-87. [DOI:10.4236/jdm.2020.102007]
Avramopoulos, I., Moulis, A. & Nikas, N., 2015. Glycaemic control, treatment satisfaction and quality of life in type 2 diabetes patients in Greece: The PANORAMA study Greek results. World Journal of Diabetes, 6(1), pp. 208-16. [DOI:10.4239/wjd.v6.i1.208] [PMID]
Bakker, K., et al., 2016. The 2015 IWGDF guidance documents on prevention and management of foot problems in diabetes: Development of an evidence‐based global consensus. Diabetes/Metabolism Research and Reviews, 32 (Suppl 1), pp. 2–6. [DOI:10.1002/dmrr.2694] [PMID]
Boels, A. M., et al., 2017. What determines treatment satisfaction of patients with type 2 diabetes on insulin therapy? An observational study in eight European countries. BMJ Open, 7(7), pp. e016180. [DOI:10.1136/bmjopen-2017-016180] [PMID]
Bradley, C., et al., 2018. Predictors of quality of life and other patient-reported outcomes in the PANORAMA multinational study of people with type 2 diabetes. Diabetes Care, 41(2), pp. 267-76. [DOI:10.2337/dc16-2655] [PMID]
Brod, M., Skovlund, S. E. & Wittrup-Jensen, K. U., 2006. Measuring the impact of diabetes through patient report of treatment satisfaction, productivity and symptom experience. Quality of Life Research, 15(3), pp. 481-91. [DOI:10.1007/s11136-005-1624-6] [PMID]
Chang, Y. W., Shen, F. C. & Chen, C. Y., 2023. Investigation of treatment satisfaction and health-related quality of life after add-on to metformin-based therapy in patients with type 2 diabetes. Frontiers in Public Health, 11, pp. 1152284. [PMID]
Erol, O. & Enc, N., 2011. Hypoglycemia fear and self-efficacy of Turkish patients receiving insulin therapy. Asian Nursing Research, 5(4), pp. 222-8. [DOI:10.1016/j.anr.2011.12.001] [PMID]
Esteghamati, A., et al., 2017. Diabetes in Iran: Prospective analysis from first nationwide diabetes report of National Program for Prevention and Control of Diabetes (NPPCD-2016). Scientific Reports, 7(1), pp. 13461. [DOI:10.1038/s41598-017-13379-z] [PMID]
Farhat, R., et al., 2019. Adherence to oral glucose lowering drugs, quality of life, treatment satisfaction and illness perception: A cross-sectional study in patients with type 2 diabetes. Saudi Pharmaceutical Journal, 27(1), pp. 126-32. [DOI:10.1016/j.jsps.2018.09.005] [PMID]
Gonder-Frederick, L. A., et al., 2011. Psychometric properties of the hypoglycemia fear survey-ii for adults with type 1 diabetes. Diabetes Care, 34(4), pp. 801-6. [DOI:10.2337/dc10-1343] [PMID]
Gonder-Frederick, L. A., et al., 2013. Examining the behaviour subscale of the hypoglycaemia fear survey: An international study. Diabetic Medicine, 30(5), pp. 603-9. [DOI:10.1111/dme.12129] [PMID]
Guisasola, F. A., et al., 2008. Hypoglycaemic symptoms, treatment satisfaction, adherence and their associations with glycaemic goal in patients with type 2 diabetes mellitus: findings from the Real‐Life Effectiveness and Care Patterns of Diabetes Management (RECAP‐DM) Study. Diabetes, Obesity and Metabolism, 10 (Suppl 1), pp. 25–32. [PMID]
Hapunda, G., et al., 2020. Correlates of fear of hypoglycemia among patients with type 1 and 2 diabetes mellitus in outpatient hospitals in Zambia. International Journal of Diabetes in Developing Countries, 40, pp. 619-26. [DOI:10.1007/s13410-020-00835-2]
Huang, J., et al., 2022. Fear of hypoglycemia and associated factors in hospitalized patients with type 2 diabetes: A crosssectional study. Scientific Reports, 12(1), pp. 20338. [DOI:10.1038/s41598-022-24822-1] [PMID]
Khdour, M. R., Awadallah, H. B. & Al-Hamed, D. H., 2020. Treatment satisfaction and quality of life among type 2 diabetes patients: A cross-sectional study in west bank, Palestine. Journal of Diabetes Research, 2020, pp. 1834534. [DOI:10.1155/2020/1834534] [PMID]
Marrett, E., et al., 2011. Assessment of severity and frequency of self-reported hypoglycemia on quality of life in patients with type 2 diabetes treated with oral antihyperglycemic agents: A survey study. BMC Research Notes, 4, pp. 251. [DOI:10.1186/1756-0500-4-251] [PMID]
Mitchell, B. D., et al., 2013. Hypoglycaemic events in patients with type 2 diabetes in the United Kingdom: Associations with patient-reported outcomes and self-reported HbA1c. BMC Endocrine Disorders, 13, pp. 59. [DOI:10.1186/1472-6823-13-59] [PMID]
Nicolucci, A., et al., 2009. Clinical and socio-economic correlates of quality of life and treatment satisfaction in patients with type 2 diabetes. Nutrition, Metabolism and Cardiovascular Diseases, 19(1), pp. 45-53. [DOI:10.1016/j.numecd.2007.12.005] [PMID]
Onyango, E. M., & Onyango, B. M., 2018. The rise of noncommunicable diseases in Kenya: An examination of the time trends and contribution of the changes in diet and physical inactivity. Journal of Epidemiology and Global Health, 8(1-2), pp. 1-7. [DOI:10.2991/j.jegh.2017.11.004] [PMID]
Othman, Z., et al., 2015. Predictors of patient satisfaction among diabetic population attending primary health care centers at Dubai Health Authority. Quality in Primary Care, 23(4). [Link]
Przezak, A., Bielka, W. & Molęda, P., 2022. Fear of hypoglycemia-An underestimated problem. Brain and Behavior, 12(7), pp. e2633. [DOI:10.1002/brb3.2633] [PMID]
Sheu, W. H. H., et al., 2012. Hypoglycemia is associated with increased worry and lower quality of life among patients with type 2 diabetes treated with oral antihyperglycemic agents in the Asia-Pacific region. Diabetes Research and Clinical Practice, 96(2), pp. 141-8. [DOI:10.1016/j.diabres.2011.12.027] [PMID]
Simon, D., et al., 2015. Hypoglycaemic episodes in patients with type 2 diabetes-risk factors and associations with patient-reported outcomes: The PANORAMA Study. Diabetes & Metabolism, 41(6), pp. 470-9. [DOI:10.1016/j.diabet.2015.08.007] [PMID]
Stargardt, T., et al., 2009. Fear of hypoglycaemia: Defining a minimum clinically important difference in patients with type 2 diabetes. Health and Quality of Life Outcomes, 7, pp. 91. [DOI:10.1186/1477-7525-7-91] [PMID]
Suzuki, R., et al., 2021. Factors associated with treatment adherence and satisfaction in type 2 diabetes management in Japan: Results from a web-based questionnaire survey. Diabetes Therapy, 12(9), pp. 2343–58. [DOI:10.1007/s13300-021-01100-3] [PMID]
Vexiau, P., et al., 2008. Hypoglycaemia in patients with type 2 diabetes treated with a combination of metformin and sulphonylurea therapy in France. Diabetes, Obesity and Metabolism, 10 (Suppl 1), pp. 16–24. [DOI:10.1111/j.1463-1326.2008.00883.x] [PMID]
Walz, L., et al., 2014. Impact of symptomatic hypoglycemia on medication adherence, patient satisfaction with treatment, and glycemic control in patients with type 2 diabetes. Patient Preference and Adherence, 8, pp. 593–601. [DOI:10.2147/PPA.S58781] [PMID]
Wang, J. S., et al., 2020. Associations of fear of hypoglycemia with second‐line use of insulin secretagogues or insulin and subsequent glycemic control in patients with type 2 diabetes: An analysis using data from the DISCOVER study. International Journal of Clinical Practice, 74(6), pp. e13485. [DOI:10.1111/ijcp.13485] [PMID]
Wild, D., et al., 2007. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Education and Counseling, 68(1), pp. 10-5. [DOI:10.1016/j.pec.2007.05.003] [PMID]
Williams, S. A., et al., 2012. The burden of hypoglycemia on healthcare utilization, costs, and quality of life among type 2 diabetes mellitus patients. Journal of Diabetes and its Complications, 26(5), pp. 399-406. [DOI:10.1016/j.jdiacomp.2012.05.002] [PMID]
Yeke Fallah, L., et al., 2019. [Factors affecting hypoglycemia fear in patients with type 2 diabetes (Persian)]. The Journal of Qazvin University of Medical Sciences, 23(2), pp. 104-14. [Link]
Zhou, Z., et al., 2019. Association between the medication adherence and treatment satisfaction among patients with type 2 diabetes in Guangdong Province, China. Proceedings of the 2019 International Conference on Modeling, Simulation, Optimization and Numerical Techniques (SMONT 2019), 165, pp. 253-7. [DOI:10.2991/smont-19.2019.56]
Diabetes mellitus is one of the prevalent non-communicable and metabolic diseases with debilitating effects. Meanwhile, rapid economic growth and urbanization have increased its prevalence worldwide (Onyango & Onyango, 2018). It is estimated that the number of diabetes will increase to 600 million people by 2035, more than 80% of whom live in developing countries (Bakker et al., 2016). It was reported that 85.5% of Iranians suffer from type 2 diabetes mellitus (T2DM) (Esteghamati et al., 2017).
Treating T2DM involves a complex and multidisciplinary process (Williams et al., 2012). Glycemic control without hypoglycemia is one of the main challenges in diabetes treatment (Stargardt et al., 2009). Despite various antidiabetic treatments, most T2DM patients do not achieve optimal glycemic control (Avramopoulos et al., 2015). Severe and recurrent hypoglycemia may lead to fear of hypoglycemia in patients with T2DM (Sheu et al., 2012) and adverse effects on diabetes management (Erol & Enc, 2011). Fear of hypoglycemia is associated with negative feelings such as psychological distress and anxiety in patients with diabetes. It is also considered a barrier to glycemic control, which negatively affects the self-management, quality of life, and mental health of patients with diabetes (Hapunda et al., 2020; Huang et al., 2022).
Treatment satisfaction is an essential indicator of the quality of care (Othman et al., 2015). It is defined as the “confirmation of expectations” for a patient, that is, the agreement between the patient’s expectations from the treatment and the results obtained (Alcubierre et al., 2014). To achieve treatment satisfaction, it is essential to understand the patient’s perspective on the current medication (Khdour et al., 2020). The patient’s negative attitude toward the effectiveness of the treatment is an important obstacle to adherence to treatment (Farhat et al., 2019). Many antidiabetic treatments lead to hypoglycemia and are therefore perceived by the patient as unpleasant and life-threatening, which may affect treatment adherence (Walz et al., 2014). Fear of hypoglycemia can lead to inadequate blood sugar control and blood sugar-increasing behaviors such as high carbohydrate intake, avoiding exercise, and reducing the dose of antihyperglycemic medications (Mitchell et al., 2013).
Considering that treatment satisfaction can increase the effectiveness of treatment and adherence to it, as well as blood sugar control (Chang et al., 2023), it seems necessary to investigate treatment satisfaction in patients with T2DM and its related factors. According to our search, no study has specifically focused on the relationship between fear of hypoglycemia and satisfaction with treatment in these patients. Therefore, the present study was carried out to assess the relationship between fear of hypoglycemia and satisfaction with treatment in Iranian patients with T2DM.
Materials and Methods
This cross-sectional study was conducted in the outpatient clinic of Velayat Hospital in Qazvin Province, Iran, in 2021. A total of 390 patients with T2DM treated with oral antidiabetic drugs were recruited by convenience sampling. The inclusion criteria were as follows: Being 18 years old or older, suffering from T2DM as diagnosed by the hospital doctor, and taking antihyperglycemic medication for at least 6 months. Patients with type 1 diabetes, pregnant women, and those treated with insulin were excluded from the study.
Considering a type I error of 0.05, a standard deviation of the fear of hypoglycemia in patients with T2DM as 8.6 (Yeke Fallah, 2019), a precision of 0.9, and a probability of 10 % missing data, the sample size was estimated to be 390 based on the Equation 1:
The data were collected using demographic and clinical characteristics questionnaires, diabetes medication satisfaction (DiabMedSat), and hypoglycemia fear survey-II (HFS).
The first part of the questionnaire included demographics (age, gender, education level, employment, marital status) and clinical characteristics (family history of diabetes, name and number of oral antihyperglycemic drugs, diabetes complications, hypoglycemia experience, and severity of hypoglycemia) of the patients. Complications of diabetes were assessed by asking patients and referring to their medical records. Answers to the question, “Have you ever felt symptoms of hypoglycemia?” (such as sweating, confusion/feeling disoriented, shakiness, clumsy or jerky movements, dizziness, sudden moodiness or behavior changes, hunger, tingling sensations around the mouth, difficulty concentrating, headache, and pale skin color) were used to evaluate patients’ reports of hypoglycemia symptoms in the past 6 months. According to recommendations of the American Diabetes Association Hypoglycemia Workgroup, the patients with hypoglycemia rated their hypoglycemia severity by selecting one of the following choices: 1) Mild (little or no interruption of activities and no assistance needed to manage symptoms), 2) Moderate (some interruption of activities and no assistance needed to manage symptoms), 3) Severe (needed the assistance of others to manage symptoms e.g. to bring food or drink, and 4) Very severe (requires medical attention including calling an ambulance, going to the emergency room or hospital, or seeing a doctor or nurse) (Marrett et al., 2011).
DiabMedSat contains 21 items divided into three domains: The burden domain (11 items) measures any bothersome aspect of treatment, the efficacy domain (5 items) measures satisfaction with any physical or emotional effects of treatment, and the symptoms domain (5 items) evaluates symptoms that may have occurred as a result of the treatment. Each item is rated on a 7-point Likert scale ranging from 1 (never/not at all/not at all bothered/extremely dissatisfied) to 7 (all the time/extremely/extremely bothered/extremely satisfied) by the subjects. The range of raw scores of the subscales and the whole questionnaire is as follows: Burden, 11-57; efficacy, 5-33; symptom, 5-30; total (DiabMedSat), 120. The scores are then transformed from 0 to 100. The total score of each domain will be the result of the mean score of the items in that domain. The mean of the three domain scores determines the total score. Total and domain scores range from 0 to 100. A higher score indicates greater levels of treatment satisfaction. Items 1 (a-d), 2 (a-e), 5 (a-d), and 6 (a-c) are scored reversely. The DiabMedSat has acceptable internal consistency with an alpha coefficient=0.9 (Brod et al., 2006).
There are two subscales in the HFS-II: Behavioral and worry (Gonder-Frederick et al., 2011). Both subscales of the survey can be analyzed separately (Przezak, Bielka, & Molęda, 2022). This study evaluated patients’ concerns about hypoglycemia episodes using the HFS-worry subscale (HFS-W) alone (Atallah et al., 2020; Marrett et al., 2011; Sheu et al., 2012; Wild et al., 2007; Yeke Fallah et al., 2019). The HFS-W is composed of 18 items rated on a 5-point Likert scale ranging from 0 (never) to 4 (always) and is scored from 0 to 72 (most worry) (Gonder-Frederick et al., 2011). The HFS-W has high internal consistency (α=0.94) (Gonder‐Frederick et al., 2013).
The above instruments were translated into Persian by a PhD candidate in translation studies who then back-translated them into English. The content validity of the instruments was confirmed by 10 faculty members of the Nursing Department of Qazvin University of Medical Sciences. Content validity index (CVI) and content validity ratio (CVR) were calculated for the Persian version of the HFS-W subscale and the Persian version of DiabMedSat, and the results were (CVR=0.74, CVI=0.86) and (CVR=0.78, CVI=0.89), respectively. The reliability of the questionnaires was tested on 20 patients with T2DM before the final versions of the instruments were considered ready to use. The internal consistency reliability (α) for the Persian version of HFS-W was 0.96 and for the Persian version of DiabMedSat was 0.81. All the questionnaires were completed through face-to-face interviews with the subjects by the second author.
Data analysis
Continuous variables were presented by Mean±SD, whereas categorical variables as frequency and percentage. Univariate analysis (using the independent t-test, one-way analysis of variance, and Pearson correlations) was initially conducted to assess relationships between the independent variables and treatment satisfaction. A multiple linear regression with a backward elimination method was performed to determine potential factors that might affect the treatment satisfaction of patients with T2DM so that the dependent variable was treatment satisfaction, and the factors with P<0.05 in the univariate analysis were considered the independent variables. P<0.05 was considered statistically significant. The SPSS software, version 26 statistical software was used for data analysis.
Results
Demographic and clinical characteristics are summarized in Table 1. The Mean±SD age of the subjects was 53.49±11.49 years. Most patients were female (57.4%) (Table 1).

The mean scores of treatment satisfaction and fear of hypoglycemia are presented in Table 2.

Univariate analysis using the Pearson correlation test indicated that fear of hypoglycemia is negatively correlated with treatment satisfaction (r=-0.504, P<0.001). Treatment satisfaction is negatively associated with age (r=-0.248, P<0.001) and diabetes duration (r=-0.343, P<0.001). The univariate relationships of diabetes treatment satisfaction and categorical variables are shown in Table 3.

In multivariate linear regression analysis, treatment satisfaction scores were lower in females (β=-0.12, P<0.007) and patients with diabetes complications (β=-0.138, P<0.005). Patients with college (β=0.173, P<0.001) or secondary education (β=0.115, P<0.023) experienced higher treatment satisfaction than those with primary education. Patients with very severe (β=-0.29, P<0.001) or severe hypoglycemia (β=-0.157, P<0.034) experienced lower treatment satisfaction than those with mild hypoglycemia. Fear of hypoglycemia was associated with lower treatment satisfaction scores (β=-0.39, P<0.001). The regression model explained (27.7%) of the variance of treatment satisfaction (Table 4).

Discussion
The purpose of this study was to assess patients’ concerns about hypoglycemia episodes using the HFS-W.
In the current study, fear of hypoglycemia was significantly associated with lower treatment satisfaction. To the best of our knowledge, this study is one of the first of its kind to address the relationship between fear of hypoglycemia and treatment satisfaction in Iranian diabetic patients. It has been shown that the fear of hypoglycemia is related to the anxiety domain of the quality of life. At the same time, anxiety itself has been associated with lower satisfaction with treatment (Khdour et al., 2020). The fear of hypoglycemia is common among patients with diabetes. Anxiety, emotional stress, and insecurity associated with excessive fear can reduce one’s quality of life (Przezak et al., 2022).
Hypoglycemic events in patients with T2DM treated with antihyperglycemic drugs subject them to fear of hypoglycemia (Bradley et al., 2018; Sheu et al., 2012; Simon et al., 2015; Vexiau et al., 2008). The current study demonstrated that severity of hypoglycemic episodes is significantly associated with treatment satisfaction so that patients with severe hypoglycemia reported lower treatment satisfaction. This finding is consistent with previous studies showing that patients with hypoglycemic symptoms experienced non-adherence to medications and were less satisfied with treatment (Guisasola et al., 2008; Simon et al., 2015; Walz et al., 2014).
Hypoglycemia and fear of hypoglycemia may have detrimental effects on treatment satisfaction and glycemic control (Simon et al., 2015; Wang et al., 2020). To prevent hypoglycemia, patients who fear hypoglycemia tend to maintain high glucose levels. Hence, assessing patients’ fear of hypoglycemia in clinical practice and participation in individual and group psychotherapy sessions can promote the quality of diabetes care (Przezak et al., 2022). As well, patients’ satisfaction with treatment can be improved by teaching them the symptoms of hypoglycemia and how to prevent it. In line with previous studies, our study also showed that female gender is associated with lower treatment satisfaction (Nicolucci et al., 2009; Suzuki et al., 2021). According to Przezak et al., (2022), women with diabetes experience a greater fear of hypoglycemia, which can have adverse effects on their beliefs about the effectiveness of treatment. According to the findings of the present study, several studies showed that treatment satisfaction has an inverse relationship with diabetes complications in addition to being inversely related to the female gender (Atallah et al., 2020; Nicolucci et al., 2009; Zhou et al., 2019). Having complications of diabetes increases comorbidities and lowers quality of life, which can reduce satisfaction with treatment.
In contrast to the results of the current study, another study showed that patients with macrovascular complications had higher treatment satisfaction. They explained that healthcare providers probably pay more attention to patients with diabetes complications, which leads to higher treatment satisfaction. Also, they attributed the discrepancy in results to the different definitions and classifications of diabetes complications in various studies (Boels et al., 2017). In the present study, patients with higher education levels had higher treatment satisfaction. This finding was similar to other studies (Farhat et al., 2019; Zhou et al., 2019). Another study found that treatment satisfaction was positively associated with receiving diabetes education and medication counseling (Suzuki et al., 2021). Our study emphasizes the necessity of increasing patients’ awareness of diabetes and its potential complications and the importance of screening for diabetes complications.
Conclusion
Most patients with T2DM treated with oral antihyperglycemic drugs experience hypoglycemia, and the exposure of patients to hypoglycemic symptoms increases their fear of hypoglycemia. The present study showed that fear of hypoglycemia is associated with decreased satisfaction with treatment. Considering the importance of treatment satisfaction in blood sugar control and patients’ quality of life, screening patients for fear of hypoglycemia is recommended. In addition, it seems necessary to plan psychological interventions to reduce the fear of hypoglycemia in patients with T2DM.
This study has some limitations. First, the study’s cross-sectional nature allowed us to describe treatment satisfaction and fear of hypoglycemia at only one point in time. It is suggested that future studies design and implement interventions to increase treatment satisfaction with an emphasis on reducing the fear of hypoglycemia in patients with T2DM. The samples of this study were recruited from one hospital in Qazvin City, which can reduce the generalizability of the findings. Therefore, it is suggested that multicenter studies be conducted in the future to obtain more reliable evidence.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Qazvin University of Medical Sciences (IR.QUMS.REC.1399.101). The study objectives were explained to the patients, and they were assured of the confidentiality of their information. Written informed consent was obtained from all subjects.
Funding
This research received financial support from Qazvin University of Medical Sciences (Project No.: 99000233).
Authors' contributions
Conceptualization, methodology, statistical analysis, supervision, writing the original draft: Maryam Momeni and Hamideh Hakimi; Data collection: Pegah Afsaneh Abadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their special thanks to the study participants and the staff and the administrators of Velayat Hospital who helped to do this study.
References
Alcubierre, N., et al., 2014. A prospective cross-sectional study on quality of life and treatment satisfaction in type 2 diabetic patients with retinopathy without other major late diabetic complications. Health and Quality of Life Outcomes, 12(1), pp. 1-12. [DOI:10.1186/s12955-014-0131-2] [PMID]
Atallah, P., et al., 2020. Diabetes management, quality of life and treatment satisfaction in adult population in Jordan and Lebanon, observations from the SIMPLIFY study. Journal of Diabetes Mellitus, 10(02), pp. 73-87. [DOI:10.4236/jdm.2020.102007]
Avramopoulos, I., Moulis, A. & Nikas, N., 2015. Glycaemic control, treatment satisfaction and quality of life in type 2 diabetes patients in Greece: The PANORAMA study Greek results. World Journal of Diabetes, 6(1), pp. 208-16. [DOI:10.4239/wjd.v6.i1.208] [PMID]
Bakker, K., et al., 2016. The 2015 IWGDF guidance documents on prevention and management of foot problems in diabetes: Development of an evidence‐based global consensus. Diabetes/Metabolism Research and Reviews, 32 (Suppl 1), pp. 2–6. [DOI:10.1002/dmrr.2694] [PMID]
Boels, A. M., et al., 2017. What determines treatment satisfaction of patients with type 2 diabetes on insulin therapy? An observational study in eight European countries. BMJ Open, 7(7), pp. e016180. [DOI:10.1136/bmjopen-2017-016180] [PMID]
Bradley, C., et al., 2018. Predictors of quality of life and other patient-reported outcomes in the PANORAMA multinational study of people with type 2 diabetes. Diabetes Care, 41(2), pp. 267-76. [DOI:10.2337/dc16-2655] [PMID]
Brod, M., Skovlund, S. E. & Wittrup-Jensen, K. U., 2006. Measuring the impact of diabetes through patient report of treatment satisfaction, productivity and symptom experience. Quality of Life Research, 15(3), pp. 481-91. [DOI:10.1007/s11136-005-1624-6] [PMID]
Chang, Y. W., Shen, F. C. & Chen, C. Y., 2023. Investigation of treatment satisfaction and health-related quality of life after add-on to metformin-based therapy in patients with type 2 diabetes. Frontiers in Public Health, 11, pp. 1152284. [PMID]
Erol, O. & Enc, N., 2011. Hypoglycemia fear and self-efficacy of Turkish patients receiving insulin therapy. Asian Nursing Research, 5(4), pp. 222-8. [DOI:10.1016/j.anr.2011.12.001] [PMID]
Esteghamati, A., et al., 2017. Diabetes in Iran: Prospective analysis from first nationwide diabetes report of National Program for Prevention and Control of Diabetes (NPPCD-2016). Scientific Reports, 7(1), pp. 13461. [DOI:10.1038/s41598-017-13379-z] [PMID]
Farhat, R., et al., 2019. Adherence to oral glucose lowering drugs, quality of life, treatment satisfaction and illness perception: A cross-sectional study in patients with type 2 diabetes. Saudi Pharmaceutical Journal, 27(1), pp. 126-32. [DOI:10.1016/j.jsps.2018.09.005] [PMID]
Gonder-Frederick, L. A., et al., 2011. Psychometric properties of the hypoglycemia fear survey-ii for adults with type 1 diabetes. Diabetes Care, 34(4), pp. 801-6. [DOI:10.2337/dc10-1343] [PMID]
Gonder-Frederick, L. A., et al., 2013. Examining the behaviour subscale of the hypoglycaemia fear survey: An international study. Diabetic Medicine, 30(5), pp. 603-9. [DOI:10.1111/dme.12129] [PMID]
Guisasola, F. A., et al., 2008. Hypoglycaemic symptoms, treatment satisfaction, adherence and their associations with glycaemic goal in patients with type 2 diabetes mellitus: findings from the Real‐Life Effectiveness and Care Patterns of Diabetes Management (RECAP‐DM) Study. Diabetes, Obesity and Metabolism, 10 (Suppl 1), pp. 25–32. [PMID]
Hapunda, G., et al., 2020. Correlates of fear of hypoglycemia among patients with type 1 and 2 diabetes mellitus in outpatient hospitals in Zambia. International Journal of Diabetes in Developing Countries, 40, pp. 619-26. [DOI:10.1007/s13410-020-00835-2]
Huang, J., et al., 2022. Fear of hypoglycemia and associated factors in hospitalized patients with type 2 diabetes: A crosssectional study. Scientific Reports, 12(1), pp. 20338. [DOI:10.1038/s41598-022-24822-1] [PMID]
Khdour, M. R., Awadallah, H. B. & Al-Hamed, D. H., 2020. Treatment satisfaction and quality of life among type 2 diabetes patients: A cross-sectional study in west bank, Palestine. Journal of Diabetes Research, 2020, pp. 1834534. [DOI:10.1155/2020/1834534] [PMID]
Marrett, E., et al., 2011. Assessment of severity and frequency of self-reported hypoglycemia on quality of life in patients with type 2 diabetes treated with oral antihyperglycemic agents: A survey study. BMC Research Notes, 4, pp. 251. [DOI:10.1186/1756-0500-4-251] [PMID]
Mitchell, B. D., et al., 2013. Hypoglycaemic events in patients with type 2 diabetes in the United Kingdom: Associations with patient-reported outcomes and self-reported HbA1c. BMC Endocrine Disorders, 13, pp. 59. [DOI:10.1186/1472-6823-13-59] [PMID]
Nicolucci, A., et al., 2009. Clinical and socio-economic correlates of quality of life and treatment satisfaction in patients with type 2 diabetes. Nutrition, Metabolism and Cardiovascular Diseases, 19(1), pp. 45-53. [DOI:10.1016/j.numecd.2007.12.005] [PMID]
Onyango, E. M., & Onyango, B. M., 2018. The rise of noncommunicable diseases in Kenya: An examination of the time trends and contribution of the changes in diet and physical inactivity. Journal of Epidemiology and Global Health, 8(1-2), pp. 1-7. [DOI:10.2991/j.jegh.2017.11.004] [PMID]
Othman, Z., et al., 2015. Predictors of patient satisfaction among diabetic population attending primary health care centers at Dubai Health Authority. Quality in Primary Care, 23(4). [Link]
Przezak, A., Bielka, W. & Molęda, P., 2022. Fear of hypoglycemia-An underestimated problem. Brain and Behavior, 12(7), pp. e2633. [DOI:10.1002/brb3.2633] [PMID]
Sheu, W. H. H., et al., 2012. Hypoglycemia is associated with increased worry and lower quality of life among patients with type 2 diabetes treated with oral antihyperglycemic agents in the Asia-Pacific region. Diabetes Research and Clinical Practice, 96(2), pp. 141-8. [DOI:10.1016/j.diabres.2011.12.027] [PMID]
Simon, D., et al., 2015. Hypoglycaemic episodes in patients with type 2 diabetes-risk factors and associations with patient-reported outcomes: The PANORAMA Study. Diabetes & Metabolism, 41(6), pp. 470-9. [DOI:10.1016/j.diabet.2015.08.007] [PMID]
Stargardt, T., et al., 2009. Fear of hypoglycaemia: Defining a minimum clinically important difference in patients with type 2 diabetes. Health and Quality of Life Outcomes, 7, pp. 91. [DOI:10.1186/1477-7525-7-91] [PMID]
Suzuki, R., et al., 2021. Factors associated with treatment adherence and satisfaction in type 2 diabetes management in Japan: Results from a web-based questionnaire survey. Diabetes Therapy, 12(9), pp. 2343–58. [DOI:10.1007/s13300-021-01100-3] [PMID]
Vexiau, P., et al., 2008. Hypoglycaemia in patients with type 2 diabetes treated with a combination of metformin and sulphonylurea therapy in France. Diabetes, Obesity and Metabolism, 10 (Suppl 1), pp. 16–24. [DOI:10.1111/j.1463-1326.2008.00883.x] [PMID]
Walz, L., et al., 2014. Impact of symptomatic hypoglycemia on medication adherence, patient satisfaction with treatment, and glycemic control in patients with type 2 diabetes. Patient Preference and Adherence, 8, pp. 593–601. [DOI:10.2147/PPA.S58781] [PMID]
Wang, J. S., et al., 2020. Associations of fear of hypoglycemia with second‐line use of insulin secretagogues or insulin and subsequent glycemic control in patients with type 2 diabetes: An analysis using data from the DISCOVER study. International Journal of Clinical Practice, 74(6), pp. e13485. [DOI:10.1111/ijcp.13485] [PMID]
Wild, D., et al., 2007. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Education and Counseling, 68(1), pp. 10-5. [DOI:10.1016/j.pec.2007.05.003] [PMID]
Williams, S. A., et al., 2012. The burden of hypoglycemia on healthcare utilization, costs, and quality of life among type 2 diabetes mellitus patients. Journal of Diabetes and its Complications, 26(5), pp. 399-406. [DOI:10.1016/j.jdiacomp.2012.05.002] [PMID]
Yeke Fallah, L., et al., 2019. [Factors affecting hypoglycemia fear in patients with type 2 diabetes (Persian)]. The Journal of Qazvin University of Medical Sciences, 23(2), pp. 104-14. [Link]
Zhou, Z., et al., 2019. Association between the medication adherence and treatment satisfaction among patients with type 2 diabetes in Guangdong Province, China. Proceedings of the 2019 International Conference on Modeling, Simulation, Optimization and Numerical Techniques (SMONT 2019), 165, pp. 253-7. [DOI:10.2991/smont-19.2019.56]
Type of Study: Research |
Subject:
Special
Received: 2023/05/26 | Accepted: 2023/09/25 | Published: 2024/01/10
Received: 2023/05/26 | Accepted: 2023/09/25 | Published: 2024/01/10
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






