Sun, Sep 7, 2025
[Archive]
Volume 10, Issue 2 (Spring 2024)
JCCNC 2024, 10(2): 125-134 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Moghadas M, Mohammadpour A, Ghasemi R, Ajamzibad H. The Effect of Training With and Without Follow-up Through Telenursing on the Management of Stage 1 Hypertension in Older People. JCCNC 2024; 10 (2) :125-134
URL: http://jccnc.iums.ac.ir/article-1-510-en.html
URL: http://jccnc.iums.ac.ir/article-1-510-en.html
1- Student Research Committee, Gonabad University of Medical Sciences, Gonabad, Iran.
2- Department of Medical Surgical Nursing, Faculty of Nursing, Gonabad University of Medical Sciences, Gonabad, Iran.
3- Department of Cardiology, School of Medicine, Torbat Heydariyeh University of Medical Sciences, Torbat Heydariyeh, Iran.
4- Department of Aging Health, Social Development & Health Promotion Research Center, Faculty of Nursing, Gonabad University of Medical Sciences, Gonabad, Iran. ,ajam.h@gmu.ac.ir
2- Department of Medical Surgical Nursing, Faculty of Nursing, Gonabad University of Medical Sciences, Gonabad, Iran.
3- Department of Cardiology, School of Medicine, Torbat Heydariyeh University of Medical Sciences, Torbat Heydariyeh, Iran.
4- Department of Aging Health, Social Development & Health Promotion Research Center, Faculty of Nursing, Gonabad University of Medical Sciences, Gonabad, Iran. ,
Full-Text [PDF 641 kb]
(550 Downloads)
| Abstract (HTML) (2132 Views)
● Hypertension is a controllable risk factor for heart and blood vessel diseases.
● According to the American Heart Association (AHA) and the American College of Cardiology (ACC) clinical practice guideline for controlling hypertension and its follow-up through telenursing, educating older patients are efficient in handling hypertension.
● The experimental group’s systolic and diastolic blood pressure and pulse pressure decreased significantly compared to the control group after the intervention.
● According to the American Heart Association (AHA) and the American College of Cardiology (ACC) clinical practice guideline for controlling hypertension and its follow-up through telenursing, educating older patients are efficient in handling hypertension.
● The experimental group’s systolic and diastolic blood pressure and pulse pressure decreased significantly compared to the control group after the intervention.
Plain Language Summary
Although high blood pressure is a main risk factor for cardiovascular diseases, a considerable percentage of hypertensive patients are unable to manage their hypertension due to a lack of knowledge. Even after teaching and receiving information, patients often need follow-up on care and program implementation. Telenursing, through telecommunications technology, provides this follow-up from remote areas. Accordingly, the present study was designed to examine the impact of training based on the American Heart Association (AHA) and the American College of Cardiology (ACC) clinical practice guideline with and without follow-up through telenursing on stage 1 hypertension among older adult patients with stable angina pectoris. Based on the results, follow-up training given to patients through telenursing efficiently handles their high blood pressure.
Full-Text: (506 Views)
Introduction
Hypertension (HTN) is a main risk factor for heart and blood vessel diseases, such as angina pectoris (Kringeland et al., 2022). It is also a preventable cause of mortality, incapability, and hospitalization among older adults (Carey et al., 2018). Systolic hypertension is one of the most powerful indicators of HTN among older adults. Its prevalence among older adults above 65 years of age has been reported as 61.7%-67.7% (Kim et al., 2019). Globally, over 1 billion people suffer from HTN (Zhou et al., 2021). Many patients cannot control their diseases (Izadirad et al., 2014). Angina pectoris is the most common cardiac ischemic disease, which causes repeated hospitalization in intensive care units and can seriously affect the life and work of patients and families. Age, gender, familial history, race, cigarette smoking, animal fats, HTN, and stress are among the factors that contribute to angina pectoris. Therefore, controlling high blood pressure can be essential to preventing cardiovascular diseases, especially angina pectoris (Sarrafzadegan & Mohammmadifard., 2019; Kloner et al., 2017).
There are various clinical guidelines for the prevention and control of HTN; one of them is the American College of Cardiology (ACC) and the American Heart Association (AHA) clinical practice guideline (ACC/AHA guideline, 2017). It has been prepared based on scientific evidence and the practical experience of the specialists. According to ACC/AHA guidelines, in order to prevent and treat hypertension (HTN), blood pressure (BP) should be categorized as normal, high, or stage 1 or 2 HTN. Normal BP is defined as <120/<80 mm Hg, while high BP is 120-129/<80 mm Hg. Stage 1 HTN is when the systolic BP is 130-139 or diastolic BP is 80-89 mm Hg, and stage 2 HTN is a systolic BP of ≥140 or diastolic BP of ≥90 mm Hg (Whelton et al., 2017). Also, based on this guideline, training is required to make lifestyle changes (including regular physical activity, balanced nutrition, no smoking, no drinking alcohol, appropriate handling of stress, and losing weight) (Carey et al., 2018). Compared to some guidelines, one of the advantages of the AHA/ACC guideline is its emphasis on lifestyle and diet modification in treating stage 1 HTN and does not recommend medication for them (Whelton et al., 2017).
Receiving proper education is one of the essential needs of patients, and having complete information about the course of the disease and its treatment is one of their most important rights. Patient education is one of the crucial responsibilities and roles of caring nurses, which helps to recover patients and promote their health. Further, patient education may help increase patient compliance and lifestyle changes (Ghoulami-Shilsari & Esmaeilpour Bandboni, 2019; Elbialy et al., 2022). Today, many patients are discharged from the hospital after a short period of hospitalization, and a major part of their recovery period is spent at home without benefiting from continuous medical or nursing care. Based on this, the necessary information and training should be given to patients and their families before leaving the hospital. This training should be continued after leaving the hospital so that patients can care for themselves at home based on what they have learned (Dinh et al., 2016).
There are various educational methods, including need-based learning, telenursing, follow-up care plans, and other educational methods for helping patients after discharge from the hospital (Morris, 2022; Friedman et al., 2011). Telenursing/telehealth nursing utilizes technology to deliver nursing services via computers, mobile phones, and other instruments. Telenursing is a cost-effective and efficient method to evaluate patients’ care requirements and follow-up on their education (Ghoulami-Shilsari & Esmaeilpour Bandboni, 2019). Telenursing is a suitable means of fulfilling the needs of older adult patients. This method is ideal for older adult patients and all patients who require monitoring, such as hypertensive patients (Ghai & Kalyan, 2017). It also enhances the relationship between clients and caregiver staff and removes the time and place obstacles. In addition, telenursing effectively reduces costs and facilitates access to healthcare (Nazer Mozafari et al., 2017). Telenursing may be used as a suitable approach to provide training to hypertensive patients. Especially since elderly patients with HTN need more education and continuous checking, follow-up through telenursing can be an effective tool (Talebi et al., 2023). Adherence to recommendations is critical in managing HTN and preventing its side effects (Cho et al., 2018). Telenursing follow-up of what the patient has learned may affect adherence to recommendations in older adults.
In light of what was said, HTN is a significant risk factor for cardiovascular illnesses, and the ACC/AHA has provided appropriate guideline for lifestyle modification to control stage 1 hypertension. On the other hand, follow-up training given to patients through telenursing can effectively manage heart and blood vessel diseases in the elderly. In addition, no studies were found in this field. Therefore, the present study was designed to assess the impact of training with and without follow-up via telenursing on managing HTN in older people with stable angina pectoris.
Materials and Methods
Design, setting, and sample
This quasi-experimental research employs a pre-test and post-test design with a control group. It assessed the effectiveness of training based on ACC/AHA guideline for HTN with and without follow-up through telenursing on stage 1 HTN among older adults in 2021. The study setting was Ahmadieh Clinic, affiliated with the Torbat Heydarieh University of Medical Sciences, Torbat Heydarieh City, Iran. This clinic is an outpatient department that services cardiac and hypertensive patients. Every day, cardiologists attend this clinic to visit 150 to 200 patients. In addition, patients receive routine education about their disease by nurses and other staff.
Using comparing two means formula and based on Najafi Ghezeljeh et al.’s research (2017), with a test power of 90% and a confidence level of 99%, a sample size of 25 was calculated per group. Finally, 30 subjects were assigned for each group (60 older adults), considering a possible sample attrition rate of 20%.

Among 140 available older patients with HTN, 60 stage 1 HTN patients were selected purposively according to inclusion criteria. The criteria for entering the study were willingness to participate in the study, age 60-75 years, stage 1 HTN, atherosclerotic cardiovascular disease (ASCVD) index of lower than 10%, having a cellphone, ability to answer phone calls, no speaking or hearing disorders, not receiving medication for controlling HTN, and no cognitive disorders based on the abbreviated mental test score (AMTS). Acquiring a score of seven and above indicated no cognitive disorder. The exclusion criteria were unwillingness to continue participation, twice or more not answering phone calls, migration or long travel, and changes in the hypertension stage.
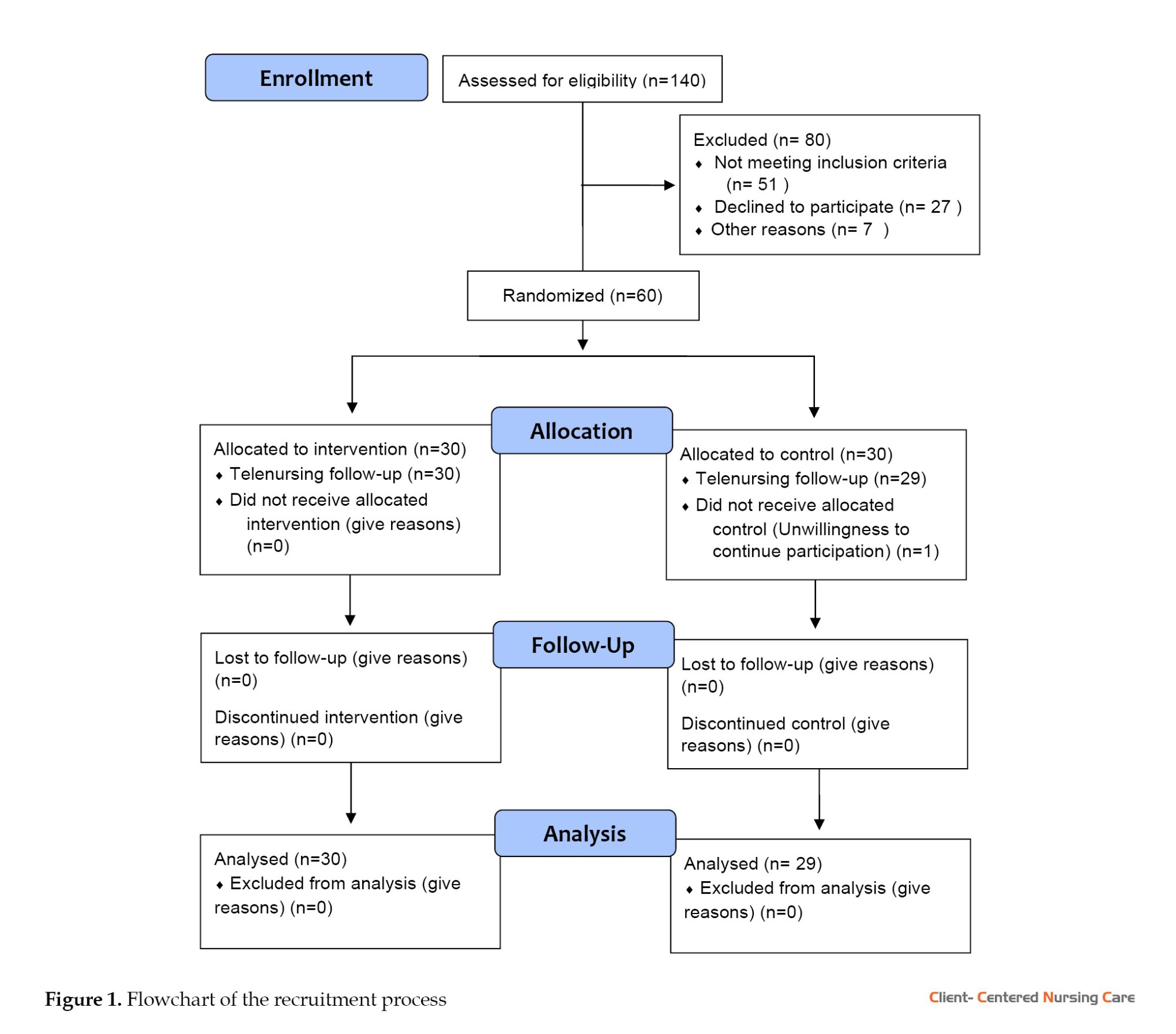
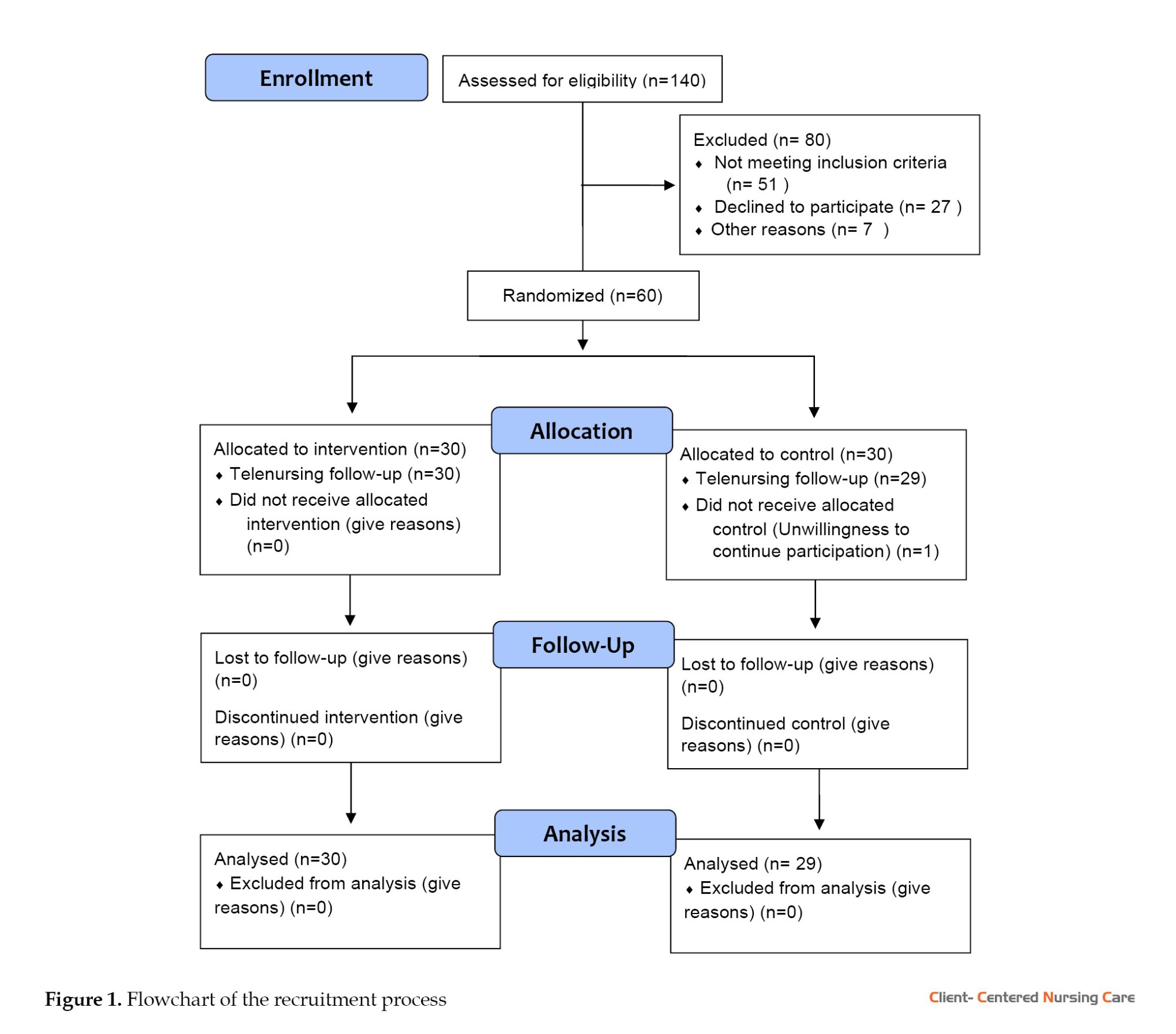
Randomization
The subjects were equally allocated to the two study groups at a proportion of 1:1. Allocation into intervention and control groups was done using the balanced block randomization method with four permutation blocks. To perform this, the letters X and Y were considered for the intervention and control groups, respectively. Conceivable modes within this way include XXYY, YYXX, XYXY, XYYX, YXXY, and YXYX. Each mode was written on a sheet. All of them are numbered from 1 to 6. A number is then chosen by rolling a dice. According to the selected mode, participants were assigned into two groups. This procedure continued until the sample study was completed. Later on, one subject from the control group dropped out because of unwillingness to continue (Figure 1).
Face-to-face training sessions were held individually for each patient in the clinic. To understand the content better, lecture sessions were accompanied by the retraining method and PowerPoint slides. The duration of sessions for each patient was 45 minutes, and a total of 59 face-to-face training sessions were held. The principal investigator taught lifestyle modification, and based on ACC/AHA guideline for HTN, patients’ questions were answered. Training according to the ACC/AHA guidelines for HTN includes non-pharmacological actions to decrease BP, such as losing weight for overweight people, using a proper diet that limits supplement salts (such as sodium and potassium) in the nutritional regimen, and increasing activities with a regular exercise plan. The patients were asked to apply these pieces of training to their daily schedules. After the training session, the first author performed telenursing in the intervention group. The first author contacted the patients weekly for three months to ensure the instructions were followed. Phone calls were often made between 16:00 and 19:00, and each phone call lasted at least 10 or at most 20 minutes. During the phone calls, the patient was reminded of the educational points, and if needed, the necessary guidance was provided again. In each telenursing call, the patients were asked about following a healthy diet, including regular exercise in their daily schedule, and quitting or reducing smoking, and the patients’ questions were answered. The control group received the cardiovascular center services after receiving the educational content according to the ACC/AHA guideline for HTN. After collecting the data, both groups were given a training booklet containing the necessary tips and common questions.
Measurement
Before random allocation, the conscious intellectual activity status of the subjects was assessed using the AMTS. It is a 10-point scale quickly to evaluate the elderly for possible cognitive disorders. Hodkinson (1972) designed the AMTS in 1972, and Bakhtiyari et al. (2014) confirmed the validity and reliability of its Persian edition. Acquiring a score of seven or above indicates no cognitive disorder. The ASCVD index was also calculated for each patient. This index investigates the risk of cardiovascular disease over the next 10 years. It is calculated based on the relevant software by entering pertinent indicators, including age, gender, race, plasma lipid (cholesterol, high-density lipoprotein, low-density lipoprotein), history of taking aspirin, and history of consuming statins. Based on ACC/AHA guideline, lifestyle modification is the first-line treatment of stage 1 HTN in patients with ASCVD below 10% (Carey et al., 2018). All participants met this criterion, and no one was excluded from this stage.
The data were obtained using a set of questions about demographic characteristics and an aneroid sphygmomanometer. The set of questions included gender, age, weight, marital condition, occupation, education level, economic condition, medication (except antihypertensive agents), history of cardiac disease in first-degree relatives, as well as years past from the disease. An aneroid sphygmomanometer was used to measure BP. The interrater reliability method was used for precise monitoring and measurement by an aneroid sphygmomanometer. The first researcher, using an aneroid sphygmomanometer, took the BP of 10 patients, and another researcher tested the BP of those 10 patients using a Richter mercury sphygmomanometer. The Pearson test revealed a relationship between the results of two evaluators (r=0.89). The clinical medical engineer assessed the validity of the aneroid sphygmomanometer according to the constructor’s report and a blood pressure calibration kit. To check the accuracy of the aneroid sphygmomanometer during the data collection process, it was compared with a mercury sphygmomanometer every day. For this purpose, BP is measured from a person under standard conditions using both devices, and the results are compared. The BP of the patients was measured using a standard method and from the right hand in a sitting position in the morning.
In this study, the subjects were not aware of their placement in the groups. Three months before and three months after the end of the intervention, the BP of patients was measured by the first author. To this end, the patients were contacted and asked to come to the clinic. BP was measured twice at an interval of 5 minutes, and then the average of the two values was recorded.
Data analysis
To investigate the study data, first, the normal distribution of the variables was checked with the Kolmogorov-Smirnov test. The findings indicated that, except for height, other quantitative variables did not follow the normal distribution. The chi-square test and Fisher exact test were used to compare between the two groups the qualitative variables, including history of non-cardiac disease, history of medication other than antihypertensive, economic status, marital status, gender, job, education level, and history of heart disease in first-degree relatives. The Wilcoxon test was used to compare each group’s pulse pressure and systolic and diastolic BP before and after the intervention. The independent t-test and Mann-Whitney test were used to compare height, age, weight, duration of illness, and ASCVD index between the two groups. In addition, the Mann-Whitney test was used to compare pulse pressure and systolic and diastolic BP before and after the intervention between the two groups. Statistical tests were done in data analysis at a significance level of 0.05.
Results
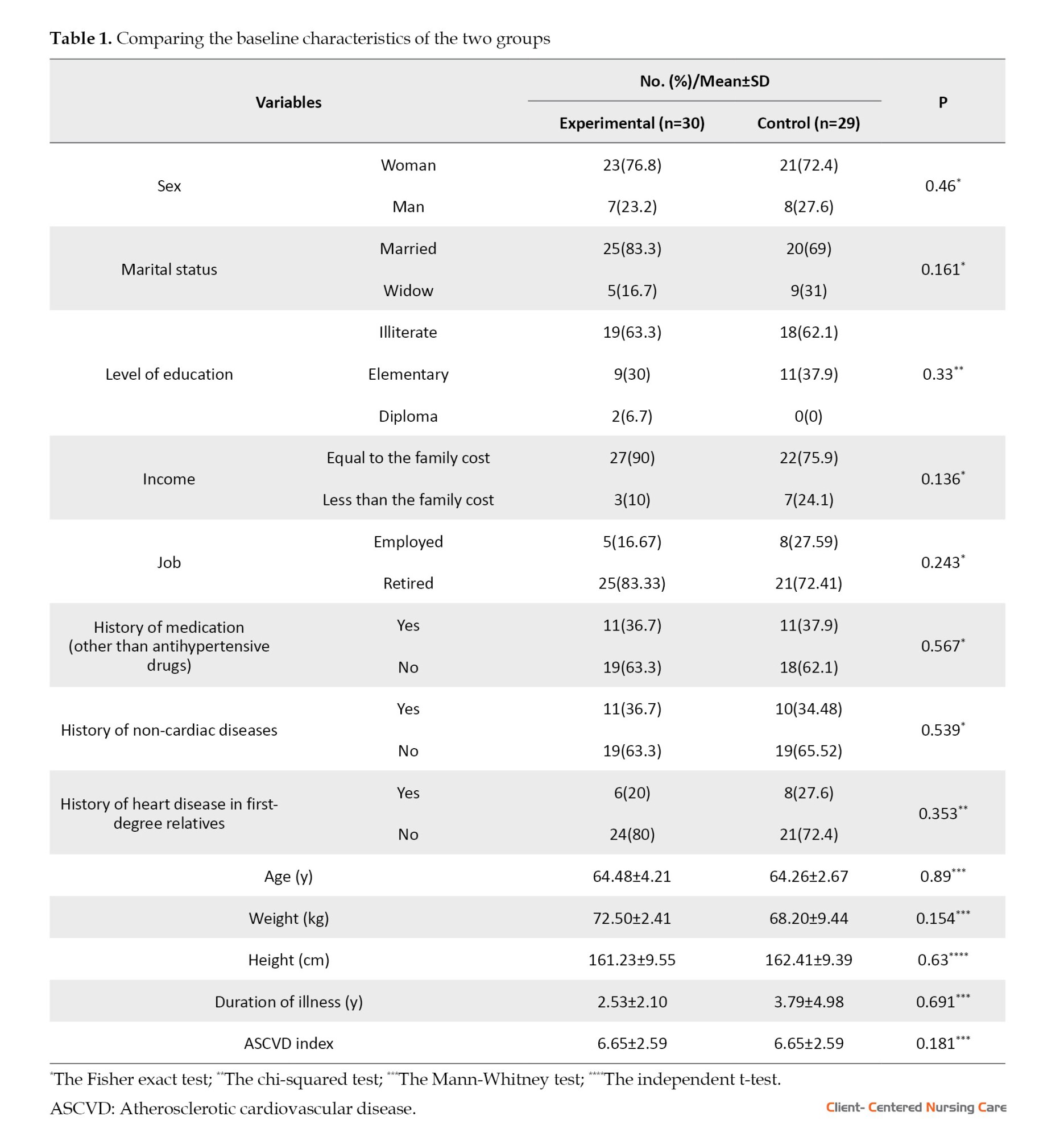
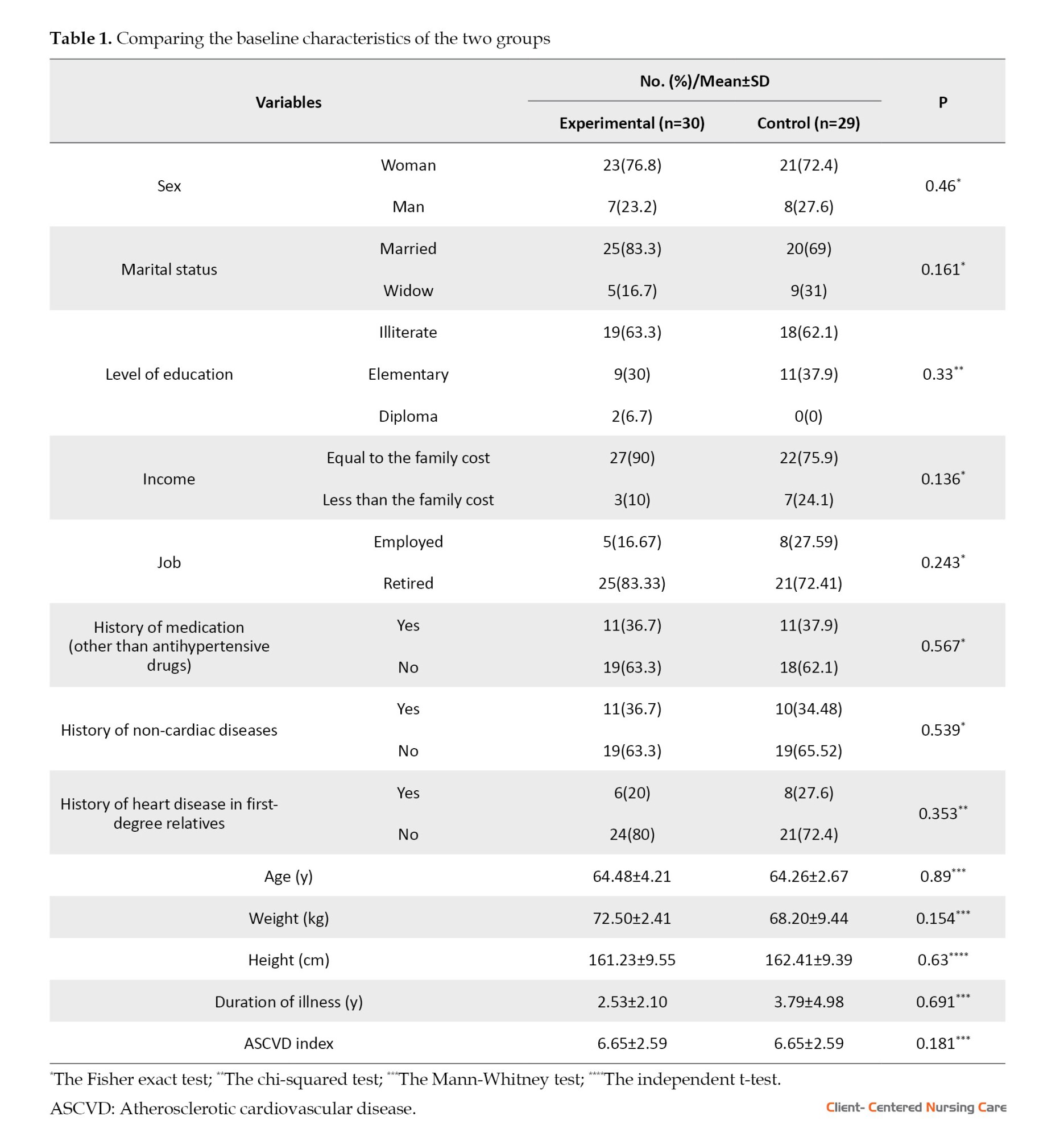
The results of statistical tests showed that the two study groups were homogenous in terms of baseline characteristics (Table 1).
Results of the Mann-Whitney test showed that the two study groups were comparable regarding systolic BP (P=0.11), diastolic BP (P=0.90), and pulse pressure (P=0.24) before the intervention (Table 2).

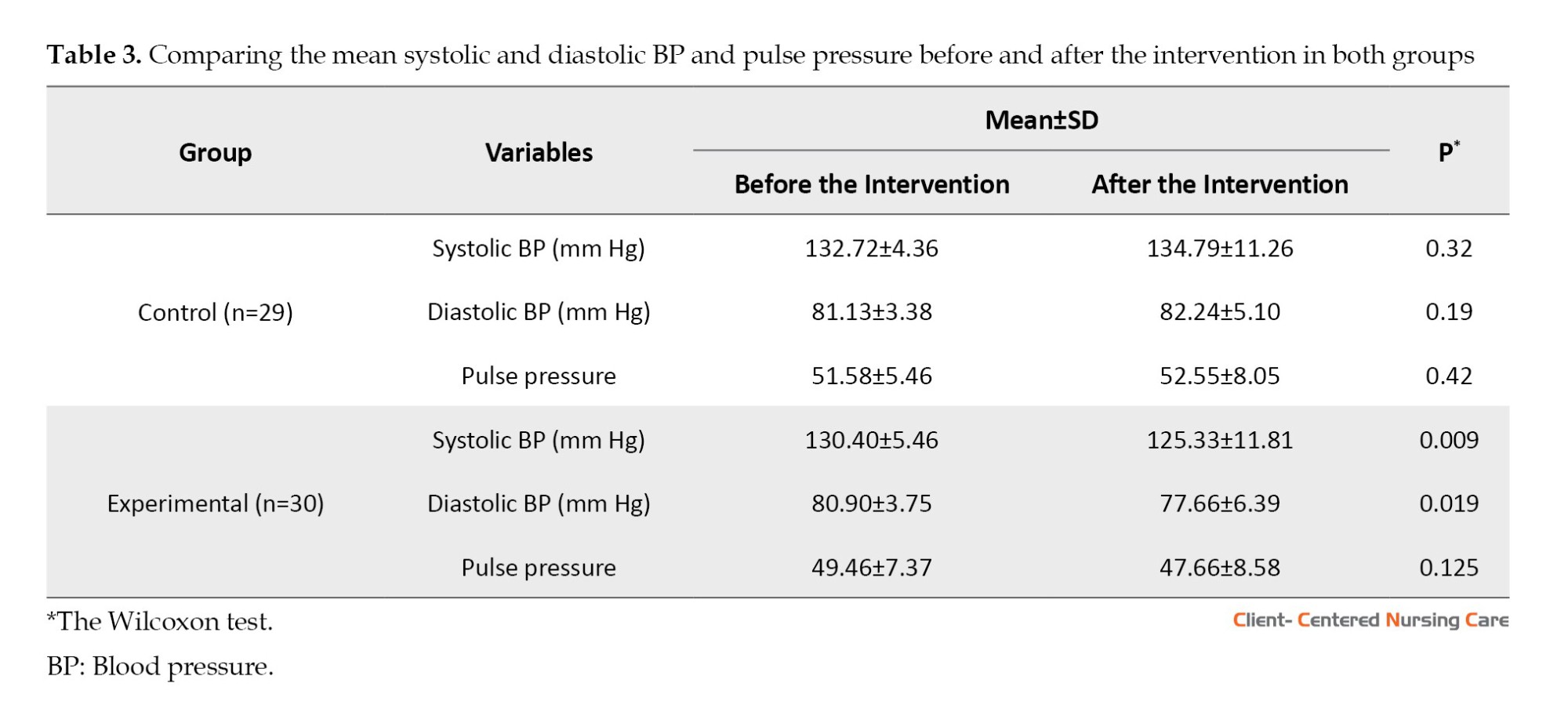
The results of the Wilcoxon test showed that the averages of systolic blood pressure (P=0.32), diastolic blood pressure (P=0.192), and pulse pressure (P=0.425) were not significantly different in the control group before and after the intervention (Table 3). However, the systolic BP (P=0.009) and diastolic BP (P=0.019) after the intervention were significantly lower than the baseline in the experimental group. Comparing the average pulse pressure (P=0.125) before and after the intervention in both groups revealed no significant difference (Table 3).
A comparison of systolic BP, diastolic BP, and pulse pressure of the two study groups after the intervention indicated a significant difference. Compared to the control group, systolic BP (P=0.001), diastolic BP (P=0.002), and pulse pressure (P=0.006) were significantly lower in the experimental group (Table 4).

Discussion
The current study aimed to compare the impacts of training based on ACC/AHA guideline with and without follow-up through telenursing in older people with stage 1 HTN.
A comparison of the mean systolic and diastolic BP in the intervention group showed a significant decrease post-intervention, while no notable difference was observed in the control group before and after the intervention. These findings align with the research conducted by Sadeghi-Gandomani et al. (2021) and Mohsen et al. (2020). Mohsen et al.’s study (2020) was conducted according to the World Health Organization (WHO) guidelines for controlling HTN, and Sadeghi-Gandomani et al. (2021) study used no specific educational guideline. However, follow-up through telenursing was the same in all these studies. This means that telenursing is effective as an intervention in managing HTN. Therefore, this method can manage stage 1 HTN in older people. Compared to the above studies, the advantages of the current study are three things: It was conducted on older people, the duration of the intervention was longer, and it was performed according to a well-known guideline.
Moreover, the results of the current study indicated that the systolic and diastolic BP significantly decreased in the experimental group after the intervention. These findings align with the research conducted by Sadeghi-Gandomani et al. (2021) and Mohsen et al. (2020); their goal was to evaluate the impact of telenursing on BP and body mass index of people with prehypertension. In addition, the results of a study conducted by Talebi et al. (2023) to determine the impacts of telenursing on the handling of self-care behaviors in people with chronic HTN showed that telenursing can improve the nutritional status and disease management of people with chronic HTN. The research results by Elbialy et al. (2022), and Ghoulami-Shilsari et al. (2019) showed that self-management hypertension training through telenursing increases patients’ knowledge and improves their lifestyle. Moreover, telenursing has improved self-care behaviors (Ghoulami-Shilsari et al., 2019) and increased self-efficacy (Keshavraz et al., 2020). In many cases, patients may not have understood the importance of the provided training. Based on this, it is appropriate to follow the training given by telenursing for better disease management. During these follow-ups, the care provider team discovers the patient’s problems. In addition, an opportunity arises in which the patients are guided about managing their diseases. All of these measures can be effective in managing and reducing BP. Based on Khosravi et al. (2012), the most common causes of uncontrolled HTN in the elderly are lack of knowledge, non-compliance with the diet, stress, smoking, and irregular medication intake. Meanwhile, follow-up through telenursing can reduce these defects and help improve the patient’s lifestyle. Mamashli et al. (2022) showed that telenursing reduces hospitalization, BP, and mortality and increases quality of life.
Conclusions
The current study specified that training based on the ACC/AHA clinical practice guideline and telenursing follow-up proves effective in managing stage 1 HTN in older adults. Therefore, it is proposed that telenursing be used to manage HTN in older people. Considering the ever-increasing growth of the elderly population and the high prevalence of HTN in these people, it is suggested that proper planning and policy should be made regarding the follow-up of the disease status of this group through telenursing. Nurses can train older adults through telenursing methods and improve the management of HTN in this group. Considering that there is no telenursing course in Iran, and this course is not offered as a specialty in nursing schools, it is suggested that nurses start a telehealth nursing course and receive specialized training. It is recommended that similar studies be conducted on patients with HTN at other stages to evaluate the effectiveness of follow-up through telenursing intervention.
The limitation of this research was that the sample consisted of patients with stage 1 HTN. Therefore, generalizing the findings to other HTN stages should be cautiously performed. The benefits of the present research encompass adherence to standard BP measurement conditions alongside the inclusion of a control group and an adequate sample size.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Gonabad University of Medical Sciences approved this study (Code: IR.GMU.REC.1399.057). The aim and procedure of the study were explained to the patients. Written informed consent was obtained from the subjects, and they were assured that their unwillingness to participate in the study would not prevent them from receiving the routine services at the center.
Funding
The present article was extracted from the master’s thesis of Maryam Moghadas, approved by the Social Development & Health Promotion Research Center, Gonabad University of Medical Sciences, Gonabad, Iran.
Authors' contributions
Researching, data gathering, and data analysis: Maryam Moghadas; Supervision, Conceptualizations, study design, and drafting of the initial version of the manuscript: Hosein Ajamzibad; Data analysis and co-advisor: Ali Mohammadpour and Reza Ghasemi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We sincerely appreciate the Vice-Chancellor for Education and Research of Gonabad University of Medical Sciences and the manager and staff of the Ahmaideh Heart Clinic, Torbat Heydarieh, Iran.
References
Elbialy, A. A., et al., 2022. Effect of implementing Tele-nursing versus Traditional nursing Program on knowledge, life style modification and blood pressure control for hypertensive patients. International Egyptian Journal of Nursing Sciences and Research, 3(1), pp. 484-515. [DOI:10.21608/ejnsr.2022.247231]
Bakhtiyari, F., et al., 2014. [Validation of the Persian version of Abbreviated Mental Test (AMT) in elderly residents of Kahrizak Charity Foundation (Persian)]. Iranian Journal of Diabetes and Metabolism, 13(6), pp. 487-94. [Link]
Carey, R. M., Whelton, P. K. & 2017 ACC/AHA Hypertension Guideline Writing Committee., 2018. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Annals of Internal Medicine, 168(5), pp. 351-8. [DOI:10.7326/M17-3203] [PMID]
Cho, M. H., et al., 2018. Association between cognitive impairment and poor antihypertensive medication adherence in elderly hypertensive patients without dementia. Scientific Reports, 8(1), pp. 11688. [DOI:10.1038/s41598-018-29974-7] [PMID]
Colantonio, Lisandro D et al. “2017 ACC/AHA Blood Pressure Treatment Guideline Recommendations and Cardiovascular Risk.” Journal of the American College of Cardiology vol. 72,11 (2018): 1187-1197. [DOI:10.1016/j.jacc.2018.05.074
Ha Dinh, T. T., et al., 2016. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14(1), pp. 210–47. [DOI:10.11124/jbisrir-2016-2296] [PMID]
Friedman, A. J., et al., 2011. Effective teaching strategies and methods of delivery for patient education: A systematic review and practice guideline recommendations. Journal of Cancer Education, 26(1), pp. 12–21. [DOI:10.1007/s13187-010-0183-x] [PMID]
Ghai, S., & Kalyan, G; 2017. Tele-nursing an emerging innovation in health sector [internet]. Retrieved from: [Link]
Ghoulami-Shilsari, F. & Bandboni, M. E., 2019. Tele-Nursing in chronic disease care: A systematic review. Jundishapur Journal of Chronic Disease Care, 8(2), pp. e84379. [DOI:10.5812/jjcdc.84379]
Hodkinson HM; 1972. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age and Ageing; 1: p. 233-238. [DOI:10.1093/ageing/1.4.233] [PMID]
Izadirad, H., et al., 2014. [Effectivness of an educational program based on BASNEF model on blood pressure in hypertension (Persian)]. Payesh (Health Monitor), 13(4), pp. 487-95. [Link]
Keshavarz, N., et al., 2020. Effect of telenursing on the self-efficacy of patients with myocardial infarction: A quasi-experimental study. Signa Vitae, 16(2), pp. 92-6. [Link]
Khosravi, A., et al., 2012. Causes of failure to control hypertension in people over 65 years of age. ARYA Atherosclerosis Journal, 7(Special Issue), pp. S42-6. [Link]
Kim, H. C., et al., 2019. 2018 Korean Society of Hypertension guidelines for the management of hypertension: Part I-epidemiology of hypertension. Clinical Hypertension, 25, pp, 16 [DOI:10.1186/s40885-019-0121-0] [PMID]
Kloner, R. A. & Chaitman, B., 2017. Angina and its management. Journal of Cardiovascular Pharmacology and Therapeutics, 22(3), pp. 199-209. [DOI:10.1177/1074248416679733] [PMID]
Kringeland, E., et al., 2022. Stage 1 hypertension, sex, and acute coronary syndromes during midlife: The Hordaland Health Study. European Journal of Preventive Cardiology, 29(1), pp. 147-154. [DOI:10.1093/eurjpc/zwab068] [PMID]
Mamashli, L., Bekmaz, K. & Mohammad pour, Y., 2022. [Telenursing in cardiovascular diseases: A critical review of systematic reviews of evidence (Persian)]. Iranian Journal of Systematic Review in Medical Sciences, 2(3), pp. 20-32. [Link]
Mohsen, M. M., et al., 2020. Tele-nursing versus routine outpatient teaching for improving arterial blood pressure and body mass index for hypertensive patients. American Journal of Nursing Research, 8(1), pp. 18-26. [Link]
Morris, G. 2022. 10 ways nurses and nurse leaders can improve patient education, Nurse Journal. Retrived from: [Link]
Najafi Ghezeljeh T, Nasr Esfahani M, & Sharifian S., 2017. [Comparing the effect of self-management training by mobile phone-based social network follow-up on blood pressure in people with hypertension (Persian)]. Iranian Journal of Cardiovascular Nursing, 6(1), pp. 22-31. [Link]
Nazer Mozafari, M., et al., 2017. [Effect of telephone follow-up (Tele-nursing) on nutritional self-efficacy & physical activity in patients with coronary artery bypass graft in Shiraz Namazi hospital in 2015 (Persian)]. Journal of Iranian Society Anaesthesiology and Intensive Care, 38(4), pp. 53-63. [Link]
Sadeghi-Gandomani, H., 2021. Impact of telenursing on blood pressure and body mass index of people with prehypertension: A randomized controlled clinical trial. Iranian Journal of Nursing and Midwifery Research, 26(6), pp. 544-9. [Link]
Sarrafzadegan, N. & Mohammmadifard, N., 2019. Cardiovascular disease in Iran in the last 40 years: Prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Archives of Iranian Medicine, 22(4), pp. 204-10. [Link]
Talebi, F., et al., 2023. Effects of telenursing on the management of self-care behaviors in patients with chronic hypertension. Journal of Research and Health, 13(4), pp. 273-80. [DOI:10.32598/JRH.13.4.2118.1]
Whelton, P. K., et al., 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology, 71(19), pp. e127–248. [DOI:10.1016/j.jacc.2017.11.006] [PMID]
NCD Risk Factor Collaboration (NCD-RisC)., 2021. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet, 398(10304), pp. 957-80. [DOI:10.1016/S0140-6736(21)01330-1] [PMID]
Hypertension (HTN) is a main risk factor for heart and blood vessel diseases, such as angina pectoris (Kringeland et al., 2022). It is also a preventable cause of mortality, incapability, and hospitalization among older adults (Carey et al., 2018). Systolic hypertension is one of the most powerful indicators of HTN among older adults. Its prevalence among older adults above 65 years of age has been reported as 61.7%-67.7% (Kim et al., 2019). Globally, over 1 billion people suffer from HTN (Zhou et al., 2021). Many patients cannot control their diseases (Izadirad et al., 2014). Angina pectoris is the most common cardiac ischemic disease, which causes repeated hospitalization in intensive care units and can seriously affect the life and work of patients and families. Age, gender, familial history, race, cigarette smoking, animal fats, HTN, and stress are among the factors that contribute to angina pectoris. Therefore, controlling high blood pressure can be essential to preventing cardiovascular diseases, especially angina pectoris (Sarrafzadegan & Mohammmadifard., 2019; Kloner et al., 2017).
There are various clinical guidelines for the prevention and control of HTN; one of them is the American College of Cardiology (ACC) and the American Heart Association (AHA) clinical practice guideline (ACC/AHA guideline, 2017). It has been prepared based on scientific evidence and the practical experience of the specialists. According to ACC/AHA guidelines, in order to prevent and treat hypertension (HTN), blood pressure (BP) should be categorized as normal, high, or stage 1 or 2 HTN. Normal BP is defined as <120/<80 mm Hg, while high BP is 120-129/<80 mm Hg. Stage 1 HTN is when the systolic BP is 130-139 or diastolic BP is 80-89 mm Hg, and stage 2 HTN is a systolic BP of ≥140 or diastolic BP of ≥90 mm Hg (Whelton et al., 2017). Also, based on this guideline, training is required to make lifestyle changes (including regular physical activity, balanced nutrition, no smoking, no drinking alcohol, appropriate handling of stress, and losing weight) (Carey et al., 2018). Compared to some guidelines, one of the advantages of the AHA/ACC guideline is its emphasis on lifestyle and diet modification in treating stage 1 HTN and does not recommend medication for them (Whelton et al., 2017).
Receiving proper education is one of the essential needs of patients, and having complete information about the course of the disease and its treatment is one of their most important rights. Patient education is one of the crucial responsibilities and roles of caring nurses, which helps to recover patients and promote their health. Further, patient education may help increase patient compliance and lifestyle changes (Ghoulami-Shilsari & Esmaeilpour Bandboni, 2019; Elbialy et al., 2022). Today, many patients are discharged from the hospital after a short period of hospitalization, and a major part of their recovery period is spent at home without benefiting from continuous medical or nursing care. Based on this, the necessary information and training should be given to patients and their families before leaving the hospital. This training should be continued after leaving the hospital so that patients can care for themselves at home based on what they have learned (Dinh et al., 2016).
There are various educational methods, including need-based learning, telenursing, follow-up care plans, and other educational methods for helping patients after discharge from the hospital (Morris, 2022; Friedman et al., 2011). Telenursing/telehealth nursing utilizes technology to deliver nursing services via computers, mobile phones, and other instruments. Telenursing is a cost-effective and efficient method to evaluate patients’ care requirements and follow-up on their education (Ghoulami-Shilsari & Esmaeilpour Bandboni, 2019). Telenursing is a suitable means of fulfilling the needs of older adult patients. This method is ideal for older adult patients and all patients who require monitoring, such as hypertensive patients (Ghai & Kalyan, 2017). It also enhances the relationship between clients and caregiver staff and removes the time and place obstacles. In addition, telenursing effectively reduces costs and facilitates access to healthcare (Nazer Mozafari et al., 2017). Telenursing may be used as a suitable approach to provide training to hypertensive patients. Especially since elderly patients with HTN need more education and continuous checking, follow-up through telenursing can be an effective tool (Talebi et al., 2023). Adherence to recommendations is critical in managing HTN and preventing its side effects (Cho et al., 2018). Telenursing follow-up of what the patient has learned may affect adherence to recommendations in older adults.
In light of what was said, HTN is a significant risk factor for cardiovascular illnesses, and the ACC/AHA has provided appropriate guideline for lifestyle modification to control stage 1 hypertension. On the other hand, follow-up training given to patients through telenursing can effectively manage heart and blood vessel diseases in the elderly. In addition, no studies were found in this field. Therefore, the present study was designed to assess the impact of training with and without follow-up via telenursing on managing HTN in older people with stable angina pectoris.
Materials and Methods
Design, setting, and sample
This quasi-experimental research employs a pre-test and post-test design with a control group. It assessed the effectiveness of training based on ACC/AHA guideline for HTN with and without follow-up through telenursing on stage 1 HTN among older adults in 2021. The study setting was Ahmadieh Clinic, affiliated with the Torbat Heydarieh University of Medical Sciences, Torbat Heydarieh City, Iran. This clinic is an outpatient department that services cardiac and hypertensive patients. Every day, cardiologists attend this clinic to visit 150 to 200 patients. In addition, patients receive routine education about their disease by nurses and other staff.
Using comparing two means formula and based on Najafi Ghezeljeh et al.’s research (2017), with a test power of 90% and a confidence level of 99%, a sample size of 25 was calculated per group. Finally, 30 subjects were assigned for each group (60 older adults), considering a possible sample attrition rate of 20%.

Among 140 available older patients with HTN, 60 stage 1 HTN patients were selected purposively according to inclusion criteria. The criteria for entering the study were willingness to participate in the study, age 60-75 years, stage 1 HTN, atherosclerotic cardiovascular disease (ASCVD) index of lower than 10%, having a cellphone, ability to answer phone calls, no speaking or hearing disorders, not receiving medication for controlling HTN, and no cognitive disorders based on the abbreviated mental test score (AMTS). Acquiring a score of seven and above indicated no cognitive disorder. The exclusion criteria were unwillingness to continue participation, twice or more not answering phone calls, migration or long travel, and changes in the hypertension stage.
Randomization
The subjects were equally allocated to the two study groups at a proportion of 1:1. Allocation into intervention and control groups was done using the balanced block randomization method with four permutation blocks. To perform this, the letters X and Y were considered for the intervention and control groups, respectively. Conceivable modes within this way include XXYY, YYXX, XYXY, XYYX, YXXY, and YXYX. Each mode was written on a sheet. All of them are numbered from 1 to 6. A number is then chosen by rolling a dice. According to the selected mode, participants were assigned into two groups. This procedure continued until the sample study was completed. Later on, one subject from the control group dropped out because of unwillingness to continue (Figure 1).
Face-to-face training sessions were held individually for each patient in the clinic. To understand the content better, lecture sessions were accompanied by the retraining method and PowerPoint slides. The duration of sessions for each patient was 45 minutes, and a total of 59 face-to-face training sessions were held. The principal investigator taught lifestyle modification, and based on ACC/AHA guideline for HTN, patients’ questions were answered. Training according to the ACC/AHA guidelines for HTN includes non-pharmacological actions to decrease BP, such as losing weight for overweight people, using a proper diet that limits supplement salts (such as sodium and potassium) in the nutritional regimen, and increasing activities with a regular exercise plan. The patients were asked to apply these pieces of training to their daily schedules. After the training session, the first author performed telenursing in the intervention group. The first author contacted the patients weekly for three months to ensure the instructions were followed. Phone calls were often made between 16:00 and 19:00, and each phone call lasted at least 10 or at most 20 minutes. During the phone calls, the patient was reminded of the educational points, and if needed, the necessary guidance was provided again. In each telenursing call, the patients were asked about following a healthy diet, including regular exercise in their daily schedule, and quitting or reducing smoking, and the patients’ questions were answered. The control group received the cardiovascular center services after receiving the educational content according to the ACC/AHA guideline for HTN. After collecting the data, both groups were given a training booklet containing the necessary tips and common questions.
Measurement
Before random allocation, the conscious intellectual activity status of the subjects was assessed using the AMTS. It is a 10-point scale quickly to evaluate the elderly for possible cognitive disorders. Hodkinson (1972) designed the AMTS in 1972, and Bakhtiyari et al. (2014) confirmed the validity and reliability of its Persian edition. Acquiring a score of seven or above indicates no cognitive disorder. The ASCVD index was also calculated for each patient. This index investigates the risk of cardiovascular disease over the next 10 years. It is calculated based on the relevant software by entering pertinent indicators, including age, gender, race, plasma lipid (cholesterol, high-density lipoprotein, low-density lipoprotein), history of taking aspirin, and history of consuming statins. Based on ACC/AHA guideline, lifestyle modification is the first-line treatment of stage 1 HTN in patients with ASCVD below 10% (Carey et al., 2018). All participants met this criterion, and no one was excluded from this stage.
The data were obtained using a set of questions about demographic characteristics and an aneroid sphygmomanometer. The set of questions included gender, age, weight, marital condition, occupation, education level, economic condition, medication (except antihypertensive agents), history of cardiac disease in first-degree relatives, as well as years past from the disease. An aneroid sphygmomanometer was used to measure BP. The interrater reliability method was used for precise monitoring and measurement by an aneroid sphygmomanometer. The first researcher, using an aneroid sphygmomanometer, took the BP of 10 patients, and another researcher tested the BP of those 10 patients using a Richter mercury sphygmomanometer. The Pearson test revealed a relationship between the results of two evaluators (r=0.89). The clinical medical engineer assessed the validity of the aneroid sphygmomanometer according to the constructor’s report and a blood pressure calibration kit. To check the accuracy of the aneroid sphygmomanometer during the data collection process, it was compared with a mercury sphygmomanometer every day. For this purpose, BP is measured from a person under standard conditions using both devices, and the results are compared. The BP of the patients was measured using a standard method and from the right hand in a sitting position in the morning.
In this study, the subjects were not aware of their placement in the groups. Three months before and three months after the end of the intervention, the BP of patients was measured by the first author. To this end, the patients were contacted and asked to come to the clinic. BP was measured twice at an interval of 5 minutes, and then the average of the two values was recorded.
Data analysis
To investigate the study data, first, the normal distribution of the variables was checked with the Kolmogorov-Smirnov test. The findings indicated that, except for height, other quantitative variables did not follow the normal distribution. The chi-square test and Fisher exact test were used to compare between the two groups the qualitative variables, including history of non-cardiac disease, history of medication other than antihypertensive, economic status, marital status, gender, job, education level, and history of heart disease in first-degree relatives. The Wilcoxon test was used to compare each group’s pulse pressure and systolic and diastolic BP before and after the intervention. The independent t-test and Mann-Whitney test were used to compare height, age, weight, duration of illness, and ASCVD index between the two groups. In addition, the Mann-Whitney test was used to compare pulse pressure and systolic and diastolic BP before and after the intervention between the two groups. Statistical tests were done in data analysis at a significance level of 0.05.
Results
The results of statistical tests showed that the two study groups were homogenous in terms of baseline characteristics (Table 1).
Results of the Mann-Whitney test showed that the two study groups were comparable regarding systolic BP (P=0.11), diastolic BP (P=0.90), and pulse pressure (P=0.24) before the intervention (Table 2).

The results of the Wilcoxon test showed that the averages of systolic blood pressure (P=0.32), diastolic blood pressure (P=0.192), and pulse pressure (P=0.425) were not significantly different in the control group before and after the intervention (Table 3). However, the systolic BP (P=0.009) and diastolic BP (P=0.019) after the intervention were significantly lower than the baseline in the experimental group. Comparing the average pulse pressure (P=0.125) before and after the intervention in both groups revealed no significant difference (Table 3).
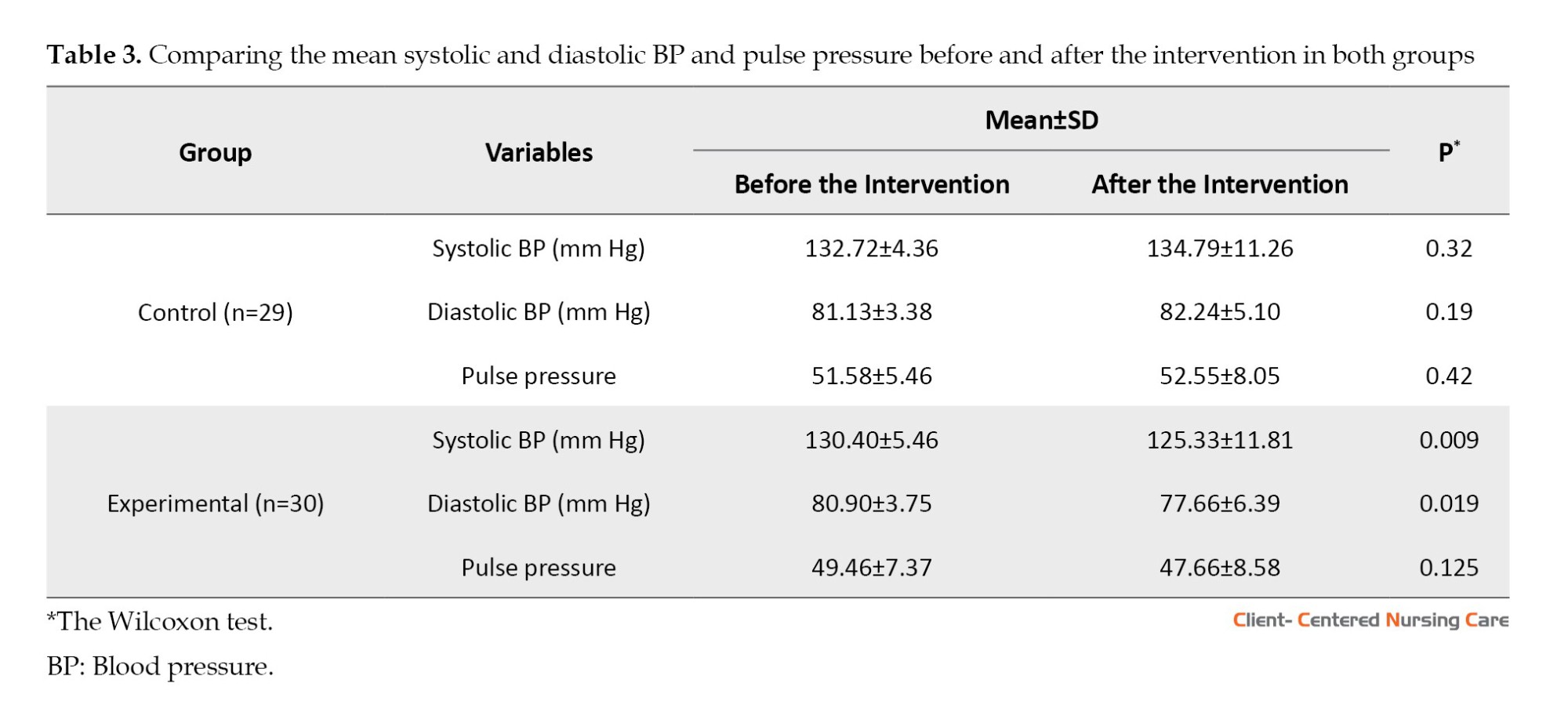
A comparison of systolic BP, diastolic BP, and pulse pressure of the two study groups after the intervention indicated a significant difference. Compared to the control group, systolic BP (P=0.001), diastolic BP (P=0.002), and pulse pressure (P=0.006) were significantly lower in the experimental group (Table 4).

Discussion
The current study aimed to compare the impacts of training based on ACC/AHA guideline with and without follow-up through telenursing in older people with stage 1 HTN.
A comparison of the mean systolic and diastolic BP in the intervention group showed a significant decrease post-intervention, while no notable difference was observed in the control group before and after the intervention. These findings align with the research conducted by Sadeghi-Gandomani et al. (2021) and Mohsen et al. (2020). Mohsen et al.’s study (2020) was conducted according to the World Health Organization (WHO) guidelines for controlling HTN, and Sadeghi-Gandomani et al. (2021) study used no specific educational guideline. However, follow-up through telenursing was the same in all these studies. This means that telenursing is effective as an intervention in managing HTN. Therefore, this method can manage stage 1 HTN in older people. Compared to the above studies, the advantages of the current study are three things: It was conducted on older people, the duration of the intervention was longer, and it was performed according to a well-known guideline.
Moreover, the results of the current study indicated that the systolic and diastolic BP significantly decreased in the experimental group after the intervention. These findings align with the research conducted by Sadeghi-Gandomani et al. (2021) and Mohsen et al. (2020); their goal was to evaluate the impact of telenursing on BP and body mass index of people with prehypertension. In addition, the results of a study conducted by Talebi et al. (2023) to determine the impacts of telenursing on the handling of self-care behaviors in people with chronic HTN showed that telenursing can improve the nutritional status and disease management of people with chronic HTN. The research results by Elbialy et al. (2022), and Ghoulami-Shilsari et al. (2019) showed that self-management hypertension training through telenursing increases patients’ knowledge and improves their lifestyle. Moreover, telenursing has improved self-care behaviors (Ghoulami-Shilsari et al., 2019) and increased self-efficacy (Keshavraz et al., 2020). In many cases, patients may not have understood the importance of the provided training. Based on this, it is appropriate to follow the training given by telenursing for better disease management. During these follow-ups, the care provider team discovers the patient’s problems. In addition, an opportunity arises in which the patients are guided about managing their diseases. All of these measures can be effective in managing and reducing BP. Based on Khosravi et al. (2012), the most common causes of uncontrolled HTN in the elderly are lack of knowledge, non-compliance with the diet, stress, smoking, and irregular medication intake. Meanwhile, follow-up through telenursing can reduce these defects and help improve the patient’s lifestyle. Mamashli et al. (2022) showed that telenursing reduces hospitalization, BP, and mortality and increases quality of life.
Conclusions
The current study specified that training based on the ACC/AHA clinical practice guideline and telenursing follow-up proves effective in managing stage 1 HTN in older adults. Therefore, it is proposed that telenursing be used to manage HTN in older people. Considering the ever-increasing growth of the elderly population and the high prevalence of HTN in these people, it is suggested that proper planning and policy should be made regarding the follow-up of the disease status of this group through telenursing. Nurses can train older adults through telenursing methods and improve the management of HTN in this group. Considering that there is no telenursing course in Iran, and this course is not offered as a specialty in nursing schools, it is suggested that nurses start a telehealth nursing course and receive specialized training. It is recommended that similar studies be conducted on patients with HTN at other stages to evaluate the effectiveness of follow-up through telenursing intervention.
The limitation of this research was that the sample consisted of patients with stage 1 HTN. Therefore, generalizing the findings to other HTN stages should be cautiously performed. The benefits of the present research encompass adherence to standard BP measurement conditions alongside the inclusion of a control group and an adequate sample size.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Gonabad University of Medical Sciences approved this study (Code: IR.GMU.REC.1399.057). The aim and procedure of the study were explained to the patients. Written informed consent was obtained from the subjects, and they were assured that their unwillingness to participate in the study would not prevent them from receiving the routine services at the center.
Funding
The present article was extracted from the master’s thesis of Maryam Moghadas, approved by the Social Development & Health Promotion Research Center, Gonabad University of Medical Sciences, Gonabad, Iran.
Authors' contributions
Researching, data gathering, and data analysis: Maryam Moghadas; Supervision, Conceptualizations, study design, and drafting of the initial version of the manuscript: Hosein Ajamzibad; Data analysis and co-advisor: Ali Mohammadpour and Reza Ghasemi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We sincerely appreciate the Vice-Chancellor for Education and Research of Gonabad University of Medical Sciences and the manager and staff of the Ahmaideh Heart Clinic, Torbat Heydarieh, Iran.
References
Elbialy, A. A., et al., 2022. Effect of implementing Tele-nursing versus Traditional nursing Program on knowledge, life style modification and blood pressure control for hypertensive patients. International Egyptian Journal of Nursing Sciences and Research, 3(1), pp. 484-515. [DOI:10.21608/ejnsr.2022.247231]
Bakhtiyari, F., et al., 2014. [Validation of the Persian version of Abbreviated Mental Test (AMT) in elderly residents of Kahrizak Charity Foundation (Persian)]. Iranian Journal of Diabetes and Metabolism, 13(6), pp. 487-94. [Link]
Carey, R. M., Whelton, P. K. & 2017 ACC/AHA Hypertension Guideline Writing Committee., 2018. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Annals of Internal Medicine, 168(5), pp. 351-8. [DOI:10.7326/M17-3203] [PMID]
Cho, M. H., et al., 2018. Association between cognitive impairment and poor antihypertensive medication adherence in elderly hypertensive patients without dementia. Scientific Reports, 8(1), pp. 11688. [DOI:10.1038/s41598-018-29974-7] [PMID]
Colantonio, Lisandro D et al. “2017 ACC/AHA Blood Pressure Treatment Guideline Recommendations and Cardiovascular Risk.” Journal of the American College of Cardiology vol. 72,11 (2018): 1187-1197. [DOI:10.1016/j.jacc.2018.05.074
Ha Dinh, T. T., et al., 2016. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14(1), pp. 210–47. [DOI:10.11124/jbisrir-2016-2296] [PMID]
Friedman, A. J., et al., 2011. Effective teaching strategies and methods of delivery for patient education: A systematic review and practice guideline recommendations. Journal of Cancer Education, 26(1), pp. 12–21. [DOI:10.1007/s13187-010-0183-x] [PMID]
Ghai, S., & Kalyan, G; 2017. Tele-nursing an emerging innovation in health sector [internet]. Retrieved from: [Link]
Ghoulami-Shilsari, F. & Bandboni, M. E., 2019. Tele-Nursing in chronic disease care: A systematic review. Jundishapur Journal of Chronic Disease Care, 8(2), pp. e84379. [DOI:10.5812/jjcdc.84379]
Hodkinson HM; 1972. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age and Ageing; 1: p. 233-238. [DOI:10.1093/ageing/1.4.233] [PMID]
Izadirad, H., et al., 2014. [Effectivness of an educational program based on BASNEF model on blood pressure in hypertension (Persian)]. Payesh (Health Monitor), 13(4), pp. 487-95. [Link]
Keshavarz, N., et al., 2020. Effect of telenursing on the self-efficacy of patients with myocardial infarction: A quasi-experimental study. Signa Vitae, 16(2), pp. 92-6. [Link]
Khosravi, A., et al., 2012. Causes of failure to control hypertension in people over 65 years of age. ARYA Atherosclerosis Journal, 7(Special Issue), pp. S42-6. [Link]
Kim, H. C., et al., 2019. 2018 Korean Society of Hypertension guidelines for the management of hypertension: Part I-epidemiology of hypertension. Clinical Hypertension, 25, pp, 16 [DOI:10.1186/s40885-019-0121-0] [PMID]
Kloner, R. A. & Chaitman, B., 2017. Angina and its management. Journal of Cardiovascular Pharmacology and Therapeutics, 22(3), pp. 199-209. [DOI:10.1177/1074248416679733] [PMID]
Kringeland, E., et al., 2022. Stage 1 hypertension, sex, and acute coronary syndromes during midlife: The Hordaland Health Study. European Journal of Preventive Cardiology, 29(1), pp. 147-154. [DOI:10.1093/eurjpc/zwab068] [PMID]
Mamashli, L., Bekmaz, K. & Mohammad pour, Y., 2022. [Telenursing in cardiovascular diseases: A critical review of systematic reviews of evidence (Persian)]. Iranian Journal of Systematic Review in Medical Sciences, 2(3), pp. 20-32. [Link]
Mohsen, M. M., et al., 2020. Tele-nursing versus routine outpatient teaching for improving arterial blood pressure and body mass index for hypertensive patients. American Journal of Nursing Research, 8(1), pp. 18-26. [Link]
Morris, G. 2022. 10 ways nurses and nurse leaders can improve patient education, Nurse Journal. Retrived from: [Link]
Najafi Ghezeljeh T, Nasr Esfahani M, & Sharifian S., 2017. [Comparing the effect of self-management training by mobile phone-based social network follow-up on blood pressure in people with hypertension (Persian)]. Iranian Journal of Cardiovascular Nursing, 6(1), pp. 22-31. [Link]
Nazer Mozafari, M., et al., 2017. [Effect of telephone follow-up (Tele-nursing) on nutritional self-efficacy & physical activity in patients with coronary artery bypass graft in Shiraz Namazi hospital in 2015 (Persian)]. Journal of Iranian Society Anaesthesiology and Intensive Care, 38(4), pp. 53-63. [Link]
Sadeghi-Gandomani, H., 2021. Impact of telenursing on blood pressure and body mass index of people with prehypertension: A randomized controlled clinical trial. Iranian Journal of Nursing and Midwifery Research, 26(6), pp. 544-9. [Link]
Sarrafzadegan, N. & Mohammmadifard, N., 2019. Cardiovascular disease in Iran in the last 40 years: Prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Archives of Iranian Medicine, 22(4), pp. 204-10. [Link]
Talebi, F., et al., 2023. Effects of telenursing on the management of self-care behaviors in patients with chronic hypertension. Journal of Research and Health, 13(4), pp. 273-80. [DOI:10.32598/JRH.13.4.2118.1]
Whelton, P. K., et al., 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology, 71(19), pp. e127–248. [DOI:10.1016/j.jacc.2017.11.006] [PMID]
NCD Risk Factor Collaboration (NCD-RisC)., 2021. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet, 398(10304), pp. 957-80. [DOI:10.1016/S0140-6736(21)01330-1] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2023/07/6 | Accepted: 2023/11/26 | Published: 2024/05/1
Received: 2023/07/6 | Accepted: 2023/11/26 | Published: 2024/05/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |