Tue, Sep 17, 2024
[Archive]
Volume 10, Issue 1 (Winter 2024)
JCCNC 2024, 10(1): 55-64 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shashi P, Madhavi V, Shasthry S M. The Effect of a Teaching Program on Knowledge, Practice, and Response Time of Nurses Regarding the Management of Upper Gastrointestinal Bleeding. JCCNC 2024; 10 (1) :55-64
URL: http://jccnc.iums.ac.ir/article-1-512-en.html
URL: http://jccnc.iums.ac.ir/article-1-512-en.html
1- Department of Medical-Surgical Nursing, Govt College of Nursing, S. N. Medical College, Agra, India. , prakashshashipr@gmail.com
2- Department of Medical-Surgical Nursing, College of Nursing, Institute of Liver and Biliary Sciences, New Delhi, India.
3- Department of Hepatology, Institute of Liver and Biliary Sciences, New Delhi, India.
2- Department of Medical-Surgical Nursing, College of Nursing, Institute of Liver and Biliary Sciences, New Delhi, India.
3- Department of Hepatology, Institute of Liver and Biliary Sciences, New Delhi, India.
Keywords: Gastrointestinal diseases, Bleeding, Emergency care, Nurses performance evaluation, Medical education
Full-Text [PDF 1053 kb]
(733 Downloads)
| Abstract (HTML) (1877 Views)
● Upper gastrointestinal bleeding (UGIB) is a common medical emergency and includes self-limiting bleeding to life-threatening hemorrhagic emergencies.
● Emergency management of UGIB requires nurses’ knowledge and their effective and fast performance.
● Nurses’ response time regarding the management of UGIB reduced after the intervention.
● Nurses’ knowledge and practice regarding the management of UGIB improved after the intervention.
● Teaching programs about the management of UGIB improved nurses’ practice.
● Emergency management of UGIB requires nurses’ knowledge and their effective and fast performance.
● Nurses’ response time regarding the management of UGIB reduced after the intervention.
● Nurses’ knowledge and practice regarding the management of UGIB improved after the intervention.
● Teaching programs about the management of UGIB improved nurses’ practice.
Plain Language Summary
Nurses play an essential role in accurate assessment and performing appropriate and quick interventions in dealing with the immediate risk of upper gastrointestinal emergency bleeding. Therefore, they must have proper knowledge and performance levels in this field. The results of this study showed that the implementation of training by face-to-face lecture method improves nurses’ knowledge and performance and shortens their response time in managing upper gastrointestinal emergency bleeding. Regular evaluation of the knowledge and performance of emergency nurses in this field and the implementation of an appropriate training program to improve their response time is suggested.
Full-Text: (287 Views)
Introduction
Upper gastrointestinal bleeding (UGIB) is a potentially life-threatening abdominal emergency that remains a common cause of hospitalization. It is a hemorrhage involving the mouth to the duodenum proximal to the ligament of Treitz (Tielleman et al., 2015).
Although significant advances have been made in diagnosing, preventing, and treating nonvariceal bleeding in the upper gastrointestinal tract, it is still a serious problem in clinical practice (Siau et al., 2017). UGIB accounts for 75% of all acute gastrointestinal (GI) bleeding cases. It is a common condition with an annual incidence of approximately 80 to 150 per 100000 people, with estimated mortality rates between 2% and 15%. UGIB can manifest as hematemesis (bright red or coffee-ground emesis), hematochezia, or melena. Patients can also present with symptoms secondary to blood loss, such as syncopal episodes, fatigue, and weakness. UGIB can be acute, occult, or faint (Antunes & Copelin, 2023).
Nurses play an essential part in managing patients with UGIB. In the first instance, they assist a patient in hypovolemic shock; patient comfort can be maintained by assessing the need for analgesia. The nurse should also be an expert in ABC (airway, breathing, chest compressions) resuscitation and assess the patient’s fluid and electrolyte status (Bayumi, 2016; Smith, 2012).
Patients with UGIB need special nursing care. To ensure the quality of this care, it is important to use a special nursing training program that includes the knowledge and skills nurses require to effectively perform care, increase cost-effectiveness, reduce patient problems and complications, and improve patient clinical outcomes (Bayumi, 2016).
With their knowledge and expertise, professional nurses have a significant role in diagnosing, managing, and improving the condition of patients with UGIB. The nurse’s role ranges from assessing the patient’s condition, helping to perform diagnostic and therapeutic procedures, prescribing fluids and other treatments, evaluating implemented interventions, and conservative management (Khalifa, 2011).
Based on what was said, the current study was conducted to assess the effect of a teaching program on the knowledge, practice, and reduction of nurses’ response time regarding the management of UGIB.
Materials and Methods
Study design, setting, and sample
It was a quasi-experimental study with a pre-test and post-test design. The study setting was the Emergency Room of the Institute of Liver and Biliary Sciences (ILBS), New Delhi, India. All available nurses (20 nurses) providing care for patients with UGIB at the above-mentioned setting were recruited through a total enumeration sampling. Also, 70 events (35 events before and 35 after the intervention) were observed during the data collection period.
Nurses with at least three months of experience in the Emergency Room of ILBS and consent to participate in the study were included. There was no sample attrition until the end of the study.
Operational definitions
In this study, “practice” refers to the performance of requisite interventions by the nursing team to manage UGIB in patients with chronic liver disease visiting the Emergency Room. The nursing practice is assessed per the interventional activities performed by the nursing team and measured as practice scores using an observation checklist.
In this study, “response time” refers to the time spent by the nursing team implementing appropriate nursing intervention for managing a chronic liver disease patient with UGIB, from the patient’s entry to the emergency room to the patient’s transfer to the outside. An observational checklist evaluates the response time.
In this study, the “event” refers to the referral of a chronic liver disease patient with UGIB to the Emergency Room of ILBS during the data collection period. It includes the patient’s management from the time of entrance to the emergency room until the time of his/her transfer to the endoscopy room, intensive care unit (ICU), upper GI bleeding ward, and so on.
Instruments
The data were collected using a demographic questionnaire, a nurses’ knowledge assessment questionnaire, and an observation checklist.
Demographic characteristics of the nurses were collected using closed-ended questions about their age, gender, and marital status. Nurses’ knowledge assessment self-administrated questionnaire includes 30 true-false questions that were developed by the researcher based on reviewing relevant literature (Lewis et al., 2016; Urden et al., 2015; Dewit & Kumagai, 2013) to collect data related to two main aspects of UGIB. The first was nurses’ knowledge associated with UGIB, and the second was nurses’ knowledge about caring for patients with UGIB. Based upon the literature review and expert guidance, the items were constructed under five domains: General assessment, primary assessment, resuscitation and stabilization, history taking and health assessment, and supportive treatment. Each correct answer in this questionnaire was scored 1, and a wrong answer or “didn’t know” was scored 0. The total score of the questionnaire ranged from 0 to 30 (100%). The total knowledge score was classified as the following: Very good, 27-30 (>90%); good, 24-26 (80%-89%); average, 21-23 (70%-79%); and poor, 0-20 (<70%).
Observation checklist
The researchers developed an observation checklist based on available assets in the Emergency Room, the UGI bleed-nursing checklist of the institution, reviewing relevant literature, i.e. the National Institute for Health and Care Excellence (NICE) pathway of acute upper gastrointestinal bleeding guidelines (2016), American Journal of Gastroenterology (ACG), clinical guidelines of upper gastrointestinal and ulcer bleeding (Laine et al., 2021), the South East Sydney Local Health District (SESLHD), adult emergency nurse protocol of gastrointestinal bleeding.
The researchers also sought guidance from the experts, gastroenterologists, and hepatology team of ILBS to assess the practice score and response time of nurses in managing UGIB. This checklist consisted of 34 items, including primary assessment, resuscitation and stabilization, history collection and health assessment, supportive treatment, and transfer out (to GI bleed ward/endoscopy room/ICU). The researchers observed the nurses’ practice in each event. The performance of the nursing team was marked by the researcher in the ‘Done’ column if it had been performed. If the nursing team had not performed the activity or did it incorrectly, the observer recorded it in the ‘not done’ or ‘done incorrect/incomplete’ column. The performance of an activity was given a score of 1, and its non-implementation was given a score of 0. The maximum possible score was 34, and the minimum was 0. The level of practice was categorized as follows: Very good, 30-34 (>90%); good, 27-29 (80%-89%); average, 23-26 (70%-79%); and poor, 0-22 (<70%). The checklist also had two columns for the activity’s time and the response time. The researcher measured the response time in minutes using the same watch (Appendix 1).
Development of teaching program
A teaching program on UGIB was prepared based on the current and past, local and international recent related literature and different studies related to theoretical knowledge of the research and various aspects of this issue using books, articles, journals, and official databases as PubMed, eMedicineHealth, Medscape, Medline Plus and National Health Library of India. Some related documents were the NICE AUGIB guidelines (2016), ACG clinical guidelines of UGIB (2021), and the SESLHD adult emergency nurse protocol of UGIB.
The content of the teaching program was organized under some subheadings, including definition, classification, causes, initial evaluation, general management, risk factors, scoring system, and nursing consideration of UGIB.
Validity and reliability
To assess the content validity index, criteria to evaluate the instruments were given to seven experts from the field of medical-surgical nursing and hepatologists to check the instruments and confirm these items for relevance, representativeness, comprehensiveness, clarity, ambiguity, and simplicity. Comments and suggestions were incorporated, and suggested modifications for the items were made to prepare the final draft of the tools and the teaching program. The content validity index of the tools ranged between 0.82 and 0.87. Experts from nursing and medical faculty, as well as hepatology and gastroenterologist teams, approved the content of the teaching program.
The Cronbach α of the structured knowledge questionnaire was calculated as 0.86. Inter-rater reliability was calculated to determine the reliability of the observation checklist. For this purpose, the performance of the nursing team in the management of three chronic liver patients with UGIB referring to the Emergency Room of the Pushpawati Singhania Hospital and Research Institute (PSRI) was simultaneously observed and recorded by the researcher and the Emergency Room sister in-charge. The Kappa coefficient was calculated as 0.87.
Study procedure
First, a pilot study was applied to three nurses of the study sample to examine the tool’s applicability and arrangement of items, estimate the time needed to complete each tool, and test the feasibility of the research process.
To perform the pre-test, the nurses’ knowledge regarding UGIB management was first assessed using the structured knowledge questionnaire. From day 2 to day 15, nurses’ practice and response time related to UGIB management were evaluated utilizing the observation checklist. To avoid any effect of the teaching program on nurses’ practice, the intervention was administered after practice, and the response time of all the nurses was pre-tested.
The educational program was implemented by the investigator through face-to-face lecture-cum and small group discussions with the aid of powerpoint presentation (PPT) and auto-visual materials in six 30-minute sessions and in groups of 3 to 4 nurses over three days from day 16 to day 18. A copy of the handout was given to each nurse to facilitate their retention of the knowledge and to help with reviewing at any time. After the administration of the teaching program, nurses’ knowledge, practice, and response time were assessed using the same structured knowledge questionnaire and observation checklist from day 19 to day 35. In the pre-test and post-test stages, the performance and response time of the nursing team concerning the management of 35 events were observed and recorded. A comparison between the pre-test and post-test findings was made to evaluate the effect of the teaching program on the nurses’ knowledge and practice toward managing patients with UGIB.
Data analysis
All collected data were organized, categorized, tabulated, and analyzed using SPSS software, version 20. The variables’ frequency distribution, Mean±SD, were calculated. Then, the paired t-test, Wilcoxon signed ranks test (Z), Kruskal-Wallis H test (for three or more groups), and Mann-Whitney U test (for two groups) were used to detect the relationships between the variables. The significance level was set at P≤0.05.
Results
Distribution of the studied nurses according to their sociodemographic characteristics (n=20) is shown in Figure 1, which portrays that about 50% of the studied nurses were in the age group of 31–40 years, 75% of them worked as an executive nurse, and 95% of the studied nurses had more than one year of experience. None of the studied nurses had previous teaching programs regarding UGIB management.

According to Table 1, the Mean±SD score of nurses’ total knowledge was 18.75±2.36 in the pre-test, which improved to 29.75±0.55 in the post-test stage. The non-parametric Wilcoxon signed rank test result was 3.94 (P<0.001), indicating a significant difference. The nurses’ total practice Mean±SD score was 25.94±1.55 in the pre-test, which promoted to 33.74±0.66 in the post-test with t=27.24 (P<0.001), indicating a significant difference. The Mean±SD score of nurses’ total response time was 48.20±12.46 min in the pre-test, which improved to 34.14±4.53 min in the post-test stage with t=6.05 (P<0.001), indicating a significant difference.

Figure 2 reveals that the mean response time of the nurses in the management of UGIB in the pre-test and post-test stages was 48.20 minutes and 34.14 minutes, respectively.
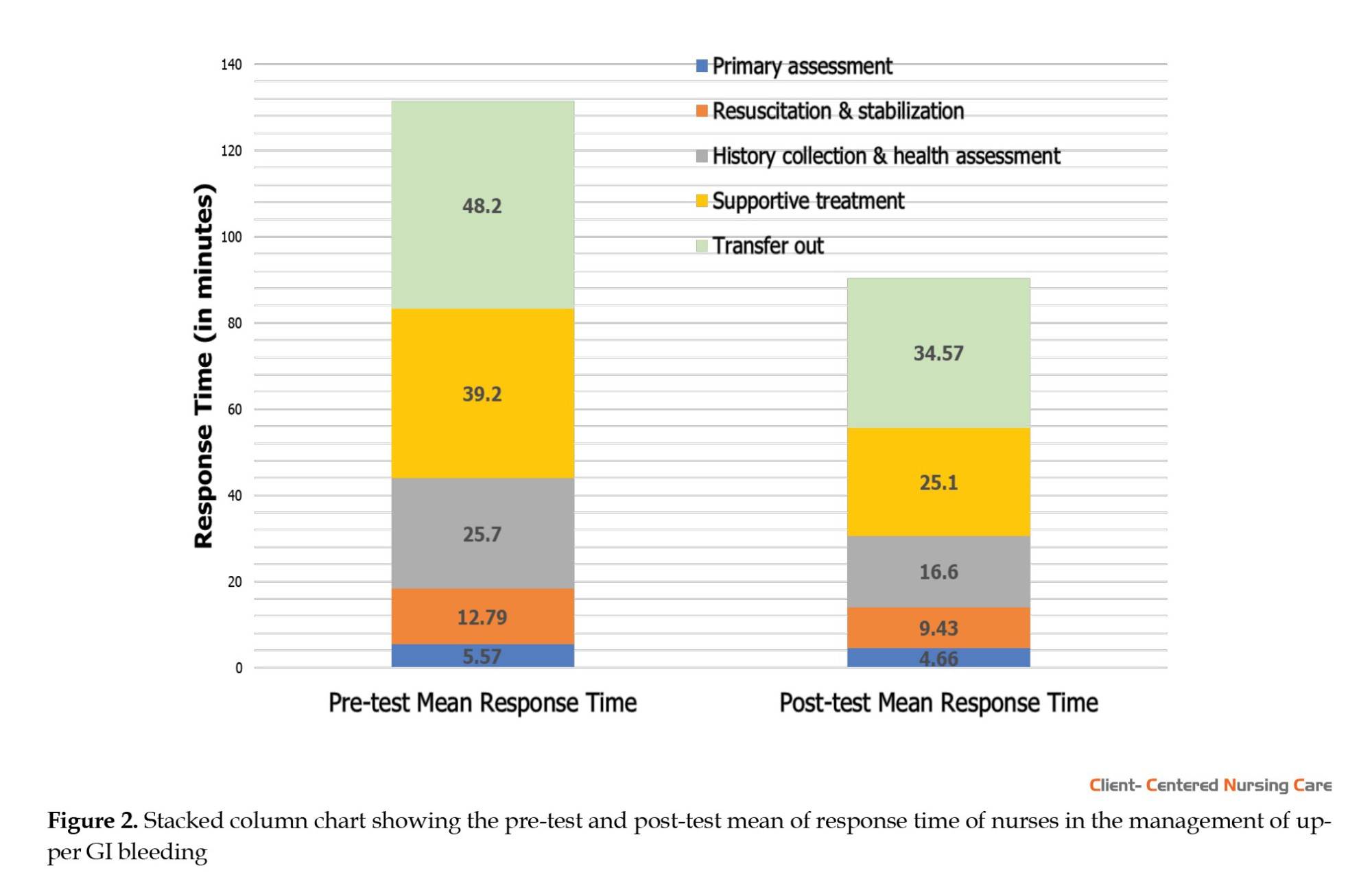
The standard deviation of nurses’ response time in the pre-test stage was 12.46 minutes, whereas their response time in the post-test stage was 4.53 minutes. The narrowing of the standard deviation of nurses’ response time in the post-test stage shows that the group is more homogenous after the teaching program. The nurses’ response time in the pre-test ranged from 25 to 78 minutes, and their response time in the post-test ranged from 28 to 46 minutes.
Table 2 indicates a significant association between the work experience of the nurses in the emergency room and their post-test knowledge score (P=0.018). The nurses with more than one year of experience had better knowledge than those with less than one year of experience.

Discussion
Acute UGIB is a common, costly, and potentially life-threatening medical emergency that requires prompt assessment and aggressive medical management. Elderly patients and those with chronic medical diseases such as hepatic failure, chronic renal failure, and ischemic heart disease are more vulnerable to acute UGIB than younger, fitter patients and have a higher risk of death (Reda et al., 2015).
The results reveal that about three-quarters of the studied nurses had an average level of knowledge and practice about the care of patients with UGIB before the teaching program implementation. In contrast, most nurses had very good knowledge and practice after the teaching program, with significant differences at all phases of implementing the program.
Consistent with our finding, another study reported that less than half of nurses had average knowledge before the implementation of a nursing protocol, while most nurses working with patients undergoing upper endoscopy had a very good level of expertise with a high significance level in the post-test stage (Mohamad et al., 2014). Also, our findings agree with another study, which revealed that most participating nurses handling acute UGIB in Ibn Sina Hospital had acceptable knowledge regarding the preliminary care of patients with UGIB (Suleiman, 2018). In addition, the present study supports another study that showed that most nurses who dealt with hematemesis patients had a moderate level of knowledge about infection control and nursing care of these patients before the protocol training. However, all nurses acquired good knowledge after the training protocol (Mohammed, 2011; Sayed, 2018).
Unfortunately, no study was found regarding the impact of training on nurses’ performance and response time in managing patients with UGIB. However, a review study showed that the level of knowledge and performance of nurses about cardiopulmonary resuscitation (CPR) improved considerably after training protocol compared with before training. Researchers in this study believe that most nurses perform CPR based on old protocols because they do not have the necessary knowledge and skills, so repeating these courses at regular intervals seems mandatory (Kuchaki et al., 2022).
A systematic review on the impact of education on the clinical alarm response and management of nurses indicated that response accurateness, response time, and time perception were consistent in different interventions. Simulation interventions had a positive effect, but the impact of training provided in the care unit was more significant. Educational activities improved clinical alarm responsiveness (Yue et al., 2017).
According to the present study findings, a statistically significant association existed between nurses’ work experience in the emergency room and their post-test knowledge score (P=0.018).
A study conducted in northeast Ethiopia regarding the knowledge of nurses about caring for older people and its predictors showed that the knowledge of nurses who had 1-5 years of work experience compared to the group with more than ten years of experience was 2.7 times lower (Amsalu et al., 2021).
Conclusion
According to the study’s findings, the training program significantly improved the knowledge and performance of nurses and reduced the response time in managing patients with UGIB. Keeping educational booklets, pamphlets, and posters in the emergency department containing all instructions and information related to UGIB and continuous in-service training on UGIB is recommended. Further studies with larger sample sizes, control groups, and random recruitment are suggested.
Among the limitations of this study, we can point to the lack of standardized tools; hence, we had to develop tools for the study. Also, no evidence was found regarding the title of this research. This shortcoming can affect the discussion and comparison of findings.
Ethical Considerations
Compliance with ethical guidelines
Before the study, official permission was granted by the Institutional Ethics Committee, ILBS. The protocol, NCT05207410, was registered with ClinicalTrials.gov and received ethical approval from the Institutional Review Board Services (IRB) as F15(2/2.25)/2017/HO(M)/ILBS, College of Nursing Ethics Committee, ILBS, New Delhi. Written consent was obtained from the nurses, and they were assured of the confidentiality of their information.
Funding
The present article was extracted from the master's thesis of Prakash Shashi, approved by Department of Gastroenterology Nursing, College of Nursing, ILBS.
Authors' contributions
Data collection: Shashi Prakash; Writing the original draft, review, and editing: Shashi Prakash; Conceptualization, study design, data analysis, data interpretation and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their earnest gratefulness to my family, friends, batchmates and ILBS team for their co-operation.
References
South East Sydney Local Health District., 2021. Adult Emergency Nurse Protocol - Gastrointestinal bleed. Sydney: South East Sydney Local Health District.
Amer, W. M., Taha, N. M. & Zaton, H. K., 2015. Nurses knowledge and practice regarding gastrointestinal endoscopy and suggested nursing guidelines. Afro-Egyptian Journal of Infectious and Endemic Diseases, 5(2), pp. 115–30. [DOI:10.21608/AEJI.2015.17820]
Amsalu, E. T., Messele, T. A. & Adane, M., 2021. Exploring the effect of professional experience on knowledge towards geriatric care among nurses working in adult care units. BMC Geriatrics, 21(1), pp. 227. [DOI:10.1186/s12877-021-02156-3] [PMID]
Antunes, C. & Copelin II, E. L., 2023. Upper gastrointestinal bleeding. In StatPearls. StatPearls Publishing. [PMID]
Bayumi, H., 2016. Clinical outcomes and patient satisfaction assessment among upper gastrointestinal bleeding at qena university hospital at upper Egypt. Journal of Nursing and Health Science, 5 (6), pp. 130-9. [Link]
Dewit, S. C. & Kumagai, C. K., 2013. Medical-surgical nursing: Concept and practice. Amsterdam: Elsevier. [Link]
Khalifa, Z. I., et al., 2015. Effect of designed implemented nurses’ educational program on minimizing incidence of complications for patients with upper gastrointestinal bleeding. Egyptian Journal of Health Care, 6(1), pp. 41-65. [Link]
Kuchaki, Z., et al., 2022. The effect of CPR educational package on knowledge and performance of nurses working in intensive care units: A review study. Journal of Family Medicine and Primary Care, 11(5), pp. 1677–82. [DOI:10.4103/jfmpc.jfmpc_1938_21] [PMID]
Laine, L., et al., 2021. ACG clinical guideline: Upper gastrointestinal and ulcer bleeding. The American Journal of Gastroenterology, 116(5), pp. 899–917. [DOI:10.14309/ajg.0000000000001245] [PMID]
Mohamad, A., Mohamad, Z. & Sayed, Z., 2014.“Esophagogastroduodenoscopy”: Impact of a designed nursing teaching protocol on nurse’s performance and patient’s outcome. Journal of American Science, 10(10), pp. 56-65. [Link]
Mohammed, G., 2011. Infection control: Effect of a designed teaching protocol on nurses’ knowledge and practice regarding to hematemesis patients [MA thesis]. Assiut: Assiut University. [Link]
National Institute for Health and Care Excellence., 2012. Acute upper gastrointestinal bleeding in over 16s: Management. London: National Institute for Health and Care Excellence. [Link]
Othman, S., 2018. Nursing guidelines for hematemesis patients undergoing upper gastrointestinal endoscopy [MA. thesis]. Mansoura: Mansoura University.
Reda, M., et al., 2015. Prospective assessment of the rockall risk scoring system in Egyptian patients with upper gastrointestinal Bleeding. Open Journal of Gastroenterology, 5(6), pp. 66-76. [DOI:10.4236/ojgas.2015.56012]
Sayed, S., 2018. Infection control: Effect of a structured nursing protocol on practice scores of nurses working with hematemsis patients. Journal of Nursing and Health Science, 7(4), pp. 38-45. [Link]
Siau, K., et al., 2017. Management of acute upper gastrointestinal bleeding: An update for the general physician. The Journal of the Royal College of Physicians of Edinburgh, 47(3), pp. 218–230.[DOI:10.4997/jrcpe.2017.303] [PMID]
Smith, G. D., 2004. The management of upper gastrointestinal bleeding. Nursing Times, 100 (26), pp. 40-3. [PMID]
Suleiman, A., 2018. Nurses’ performance regarding emergency management of patient with acute upper gastrointestinal bleeding in Ibinsinaa Hospital 2017. [PhD dissertation]. Khartoum: Neelain University. [Link]
Tielleman, T., Bujanda, D. & Cryer, B., 2015. Epidemiology and risk factors for upper gastrointestinal bleeding. Gastrointestinal Endoscopy Clinics of North America, 25 (3), pp. 415-28. [DOI:10.1016/j.giec.2015.02.010] [PMID]
Urden, L., Stacy, K. & Lough, M., 2015. Priorities in critical care nursing. Gastrointestinal disorder and therapeutic management. Missouri: Mosby. [Link]
Yue, L., Plummer, V. & Cross, W., 2017. The effectiveness of nurse education and training for clinical alarm response and management: A systematic review. Journal of Clinical Nursing, 26(17-18), pp. 2511–26. [DOI:10.1111/jocn.13605] [PMID]


Upper gastrointestinal bleeding (UGIB) is a potentially life-threatening abdominal emergency that remains a common cause of hospitalization. It is a hemorrhage involving the mouth to the duodenum proximal to the ligament of Treitz (Tielleman et al., 2015).
Although significant advances have been made in diagnosing, preventing, and treating nonvariceal bleeding in the upper gastrointestinal tract, it is still a serious problem in clinical practice (Siau et al., 2017). UGIB accounts for 75% of all acute gastrointestinal (GI) bleeding cases. It is a common condition with an annual incidence of approximately 80 to 150 per 100000 people, with estimated mortality rates between 2% and 15%. UGIB can manifest as hematemesis (bright red or coffee-ground emesis), hematochezia, or melena. Patients can also present with symptoms secondary to blood loss, such as syncopal episodes, fatigue, and weakness. UGIB can be acute, occult, or faint (Antunes & Copelin, 2023).
Nurses play an essential part in managing patients with UGIB. In the first instance, they assist a patient in hypovolemic shock; patient comfort can be maintained by assessing the need for analgesia. The nurse should also be an expert in ABC (airway, breathing, chest compressions) resuscitation and assess the patient’s fluid and electrolyte status (Bayumi, 2016; Smith, 2012).
Patients with UGIB need special nursing care. To ensure the quality of this care, it is important to use a special nursing training program that includes the knowledge and skills nurses require to effectively perform care, increase cost-effectiveness, reduce patient problems and complications, and improve patient clinical outcomes (Bayumi, 2016).
With their knowledge and expertise, professional nurses have a significant role in diagnosing, managing, and improving the condition of patients with UGIB. The nurse’s role ranges from assessing the patient’s condition, helping to perform diagnostic and therapeutic procedures, prescribing fluids and other treatments, evaluating implemented interventions, and conservative management (Khalifa, 2011).
Based on what was said, the current study was conducted to assess the effect of a teaching program on the knowledge, practice, and reduction of nurses’ response time regarding the management of UGIB.
Materials and Methods
Study design, setting, and sample
It was a quasi-experimental study with a pre-test and post-test design. The study setting was the Emergency Room of the Institute of Liver and Biliary Sciences (ILBS), New Delhi, India. All available nurses (20 nurses) providing care for patients with UGIB at the above-mentioned setting were recruited through a total enumeration sampling. Also, 70 events (35 events before and 35 after the intervention) were observed during the data collection period.
Nurses with at least three months of experience in the Emergency Room of ILBS and consent to participate in the study were included. There was no sample attrition until the end of the study.
Operational definitions
In this study, “practice” refers to the performance of requisite interventions by the nursing team to manage UGIB in patients with chronic liver disease visiting the Emergency Room. The nursing practice is assessed per the interventional activities performed by the nursing team and measured as practice scores using an observation checklist.
In this study, “response time” refers to the time spent by the nursing team implementing appropriate nursing intervention for managing a chronic liver disease patient with UGIB, from the patient’s entry to the emergency room to the patient’s transfer to the outside. An observational checklist evaluates the response time.
In this study, the “event” refers to the referral of a chronic liver disease patient with UGIB to the Emergency Room of ILBS during the data collection period. It includes the patient’s management from the time of entrance to the emergency room until the time of his/her transfer to the endoscopy room, intensive care unit (ICU), upper GI bleeding ward, and so on.
Instruments
The data were collected using a demographic questionnaire, a nurses’ knowledge assessment questionnaire, and an observation checklist.
Demographic characteristics of the nurses were collected using closed-ended questions about their age, gender, and marital status. Nurses’ knowledge assessment self-administrated questionnaire includes 30 true-false questions that were developed by the researcher based on reviewing relevant literature (Lewis et al., 2016; Urden et al., 2015; Dewit & Kumagai, 2013) to collect data related to two main aspects of UGIB. The first was nurses’ knowledge associated with UGIB, and the second was nurses’ knowledge about caring for patients with UGIB. Based upon the literature review and expert guidance, the items were constructed under five domains: General assessment, primary assessment, resuscitation and stabilization, history taking and health assessment, and supportive treatment. Each correct answer in this questionnaire was scored 1, and a wrong answer or “didn’t know” was scored 0. The total score of the questionnaire ranged from 0 to 30 (100%). The total knowledge score was classified as the following: Very good, 27-30 (>90%); good, 24-26 (80%-89%); average, 21-23 (70%-79%); and poor, 0-20 (<70%).
Observation checklist
The researchers developed an observation checklist based on available assets in the Emergency Room, the UGI bleed-nursing checklist of the institution, reviewing relevant literature, i.e. the National Institute for Health and Care Excellence (NICE) pathway of acute upper gastrointestinal bleeding guidelines (2016), American Journal of Gastroenterology (ACG), clinical guidelines of upper gastrointestinal and ulcer bleeding (Laine et al., 2021), the South East Sydney Local Health District (SESLHD), adult emergency nurse protocol of gastrointestinal bleeding.
The researchers also sought guidance from the experts, gastroenterologists, and hepatology team of ILBS to assess the practice score and response time of nurses in managing UGIB. This checklist consisted of 34 items, including primary assessment, resuscitation and stabilization, history collection and health assessment, supportive treatment, and transfer out (to GI bleed ward/endoscopy room/ICU). The researchers observed the nurses’ practice in each event. The performance of the nursing team was marked by the researcher in the ‘Done’ column if it had been performed. If the nursing team had not performed the activity or did it incorrectly, the observer recorded it in the ‘not done’ or ‘done incorrect/incomplete’ column. The performance of an activity was given a score of 1, and its non-implementation was given a score of 0. The maximum possible score was 34, and the minimum was 0. The level of practice was categorized as follows: Very good, 30-34 (>90%); good, 27-29 (80%-89%); average, 23-26 (70%-79%); and poor, 0-22 (<70%). The checklist also had two columns for the activity’s time and the response time. The researcher measured the response time in minutes using the same watch (Appendix 1).
Development of teaching program
A teaching program on UGIB was prepared based on the current and past, local and international recent related literature and different studies related to theoretical knowledge of the research and various aspects of this issue using books, articles, journals, and official databases as PubMed, eMedicineHealth, Medscape, Medline Plus and National Health Library of India. Some related documents were the NICE AUGIB guidelines (2016), ACG clinical guidelines of UGIB (2021), and the SESLHD adult emergency nurse protocol of UGIB.
The content of the teaching program was organized under some subheadings, including definition, classification, causes, initial evaluation, general management, risk factors, scoring system, and nursing consideration of UGIB.
Validity and reliability
To assess the content validity index, criteria to evaluate the instruments were given to seven experts from the field of medical-surgical nursing and hepatologists to check the instruments and confirm these items for relevance, representativeness, comprehensiveness, clarity, ambiguity, and simplicity. Comments and suggestions were incorporated, and suggested modifications for the items were made to prepare the final draft of the tools and the teaching program. The content validity index of the tools ranged between 0.82 and 0.87. Experts from nursing and medical faculty, as well as hepatology and gastroenterologist teams, approved the content of the teaching program.
The Cronbach α of the structured knowledge questionnaire was calculated as 0.86. Inter-rater reliability was calculated to determine the reliability of the observation checklist. For this purpose, the performance of the nursing team in the management of three chronic liver patients with UGIB referring to the Emergency Room of the Pushpawati Singhania Hospital and Research Institute (PSRI) was simultaneously observed and recorded by the researcher and the Emergency Room sister in-charge. The Kappa coefficient was calculated as 0.87.
Study procedure
First, a pilot study was applied to three nurses of the study sample to examine the tool’s applicability and arrangement of items, estimate the time needed to complete each tool, and test the feasibility of the research process.
To perform the pre-test, the nurses’ knowledge regarding UGIB management was first assessed using the structured knowledge questionnaire. From day 2 to day 15, nurses’ practice and response time related to UGIB management were evaluated utilizing the observation checklist. To avoid any effect of the teaching program on nurses’ practice, the intervention was administered after practice, and the response time of all the nurses was pre-tested.
The educational program was implemented by the investigator through face-to-face lecture-cum and small group discussions with the aid of powerpoint presentation (PPT) and auto-visual materials in six 30-minute sessions and in groups of 3 to 4 nurses over three days from day 16 to day 18. A copy of the handout was given to each nurse to facilitate their retention of the knowledge and to help with reviewing at any time. After the administration of the teaching program, nurses’ knowledge, practice, and response time were assessed using the same structured knowledge questionnaire and observation checklist from day 19 to day 35. In the pre-test and post-test stages, the performance and response time of the nursing team concerning the management of 35 events were observed and recorded. A comparison between the pre-test and post-test findings was made to evaluate the effect of the teaching program on the nurses’ knowledge and practice toward managing patients with UGIB.
Data analysis
All collected data were organized, categorized, tabulated, and analyzed using SPSS software, version 20. The variables’ frequency distribution, Mean±SD, were calculated. Then, the paired t-test, Wilcoxon signed ranks test (Z), Kruskal-Wallis H test (for three or more groups), and Mann-Whitney U test (for two groups) were used to detect the relationships between the variables. The significance level was set at P≤0.05.
Results
Distribution of the studied nurses according to their sociodemographic characteristics (n=20) is shown in Figure 1, which portrays that about 50% of the studied nurses were in the age group of 31–40 years, 75% of them worked as an executive nurse, and 95% of the studied nurses had more than one year of experience. None of the studied nurses had previous teaching programs regarding UGIB management.

According to Table 1, the Mean±SD score of nurses’ total knowledge was 18.75±2.36 in the pre-test, which improved to 29.75±0.55 in the post-test stage. The non-parametric Wilcoxon signed rank test result was 3.94 (P<0.001), indicating a significant difference. The nurses’ total practice Mean±SD score was 25.94±1.55 in the pre-test, which promoted to 33.74±0.66 in the post-test with t=27.24 (P<0.001), indicating a significant difference. The Mean±SD score of nurses’ total response time was 48.20±12.46 min in the pre-test, which improved to 34.14±4.53 min in the post-test stage with t=6.05 (P<0.001), indicating a significant difference.

Figure 2 reveals that the mean response time of the nurses in the management of UGIB in the pre-test and post-test stages was 48.20 minutes and 34.14 minutes, respectively.
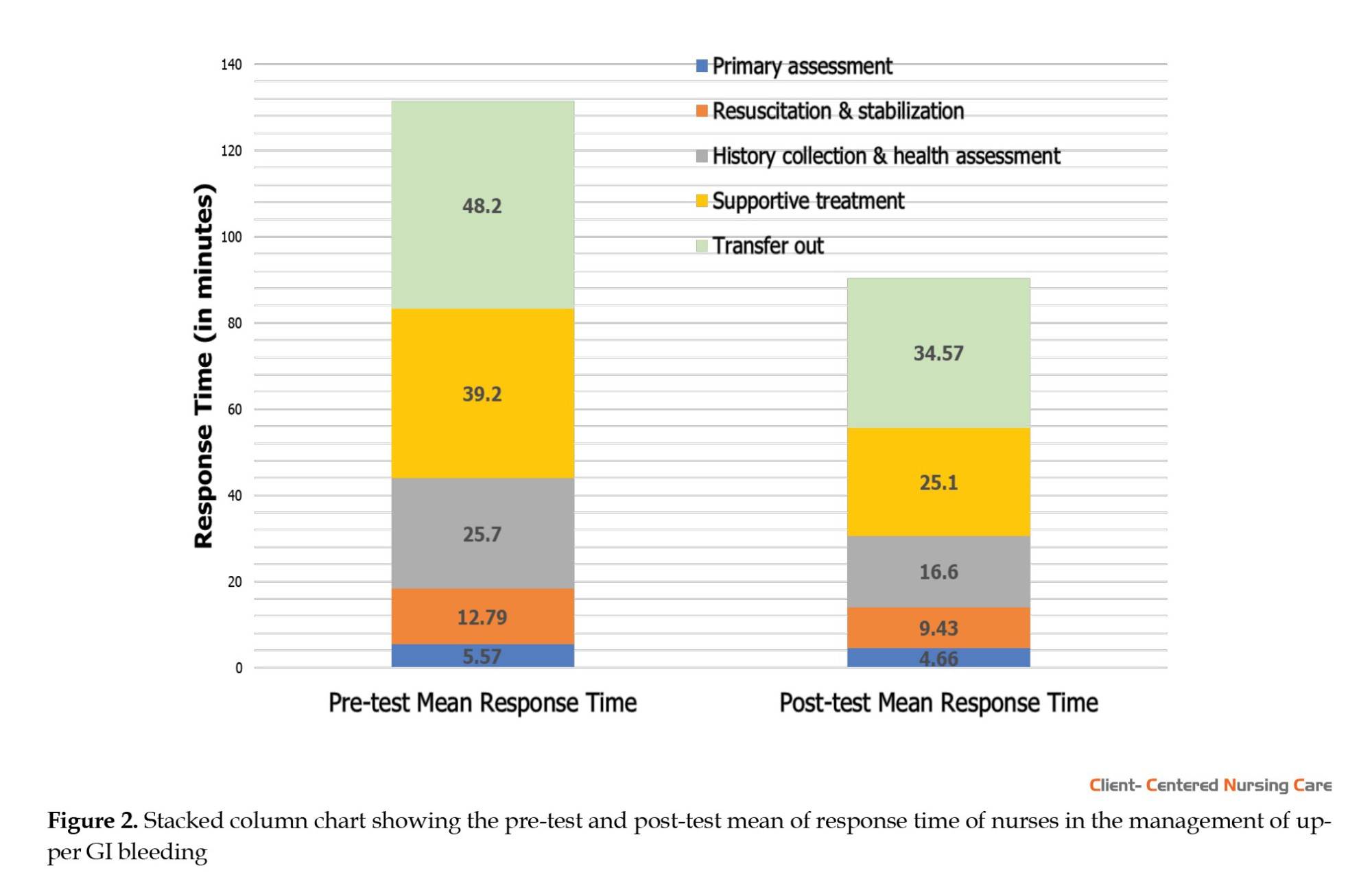
The standard deviation of nurses’ response time in the pre-test stage was 12.46 minutes, whereas their response time in the post-test stage was 4.53 minutes. The narrowing of the standard deviation of nurses’ response time in the post-test stage shows that the group is more homogenous after the teaching program. The nurses’ response time in the pre-test ranged from 25 to 78 minutes, and their response time in the post-test ranged from 28 to 46 minutes.
Table 2 indicates a significant association between the work experience of the nurses in the emergency room and their post-test knowledge score (P=0.018). The nurses with more than one year of experience had better knowledge than those with less than one year of experience.

Discussion
Acute UGIB is a common, costly, and potentially life-threatening medical emergency that requires prompt assessment and aggressive medical management. Elderly patients and those with chronic medical diseases such as hepatic failure, chronic renal failure, and ischemic heart disease are more vulnerable to acute UGIB than younger, fitter patients and have a higher risk of death (Reda et al., 2015).
The results reveal that about three-quarters of the studied nurses had an average level of knowledge and practice about the care of patients with UGIB before the teaching program implementation. In contrast, most nurses had very good knowledge and practice after the teaching program, with significant differences at all phases of implementing the program.
Consistent with our finding, another study reported that less than half of nurses had average knowledge before the implementation of a nursing protocol, while most nurses working with patients undergoing upper endoscopy had a very good level of expertise with a high significance level in the post-test stage (Mohamad et al., 2014). Also, our findings agree with another study, which revealed that most participating nurses handling acute UGIB in Ibn Sina Hospital had acceptable knowledge regarding the preliminary care of patients with UGIB (Suleiman, 2018). In addition, the present study supports another study that showed that most nurses who dealt with hematemesis patients had a moderate level of knowledge about infection control and nursing care of these patients before the protocol training. However, all nurses acquired good knowledge after the training protocol (Mohammed, 2011; Sayed, 2018).
Unfortunately, no study was found regarding the impact of training on nurses’ performance and response time in managing patients with UGIB. However, a review study showed that the level of knowledge and performance of nurses about cardiopulmonary resuscitation (CPR) improved considerably after training protocol compared with before training. Researchers in this study believe that most nurses perform CPR based on old protocols because they do not have the necessary knowledge and skills, so repeating these courses at regular intervals seems mandatory (Kuchaki et al., 2022).
A systematic review on the impact of education on the clinical alarm response and management of nurses indicated that response accurateness, response time, and time perception were consistent in different interventions. Simulation interventions had a positive effect, but the impact of training provided in the care unit was more significant. Educational activities improved clinical alarm responsiveness (Yue et al., 2017).
According to the present study findings, a statistically significant association existed between nurses’ work experience in the emergency room and their post-test knowledge score (P=0.018).
A study conducted in northeast Ethiopia regarding the knowledge of nurses about caring for older people and its predictors showed that the knowledge of nurses who had 1-5 years of work experience compared to the group with more than ten years of experience was 2.7 times lower (Amsalu et al., 2021).
Conclusion
According to the study’s findings, the training program significantly improved the knowledge and performance of nurses and reduced the response time in managing patients with UGIB. Keeping educational booklets, pamphlets, and posters in the emergency department containing all instructions and information related to UGIB and continuous in-service training on UGIB is recommended. Further studies with larger sample sizes, control groups, and random recruitment are suggested.
Among the limitations of this study, we can point to the lack of standardized tools; hence, we had to develop tools for the study. Also, no evidence was found regarding the title of this research. This shortcoming can affect the discussion and comparison of findings.
Ethical Considerations
Compliance with ethical guidelines
Before the study, official permission was granted by the Institutional Ethics Committee, ILBS. The protocol, NCT05207410, was registered with ClinicalTrials.gov and received ethical approval from the Institutional Review Board Services (IRB) as F15(2/2.25)/2017/HO(M)/ILBS, College of Nursing Ethics Committee, ILBS, New Delhi. Written consent was obtained from the nurses, and they were assured of the confidentiality of their information.
Funding
The present article was extracted from the master's thesis of Prakash Shashi, approved by Department of Gastroenterology Nursing, College of Nursing, ILBS.
Authors' contributions
Data collection: Shashi Prakash; Writing the original draft, review, and editing: Shashi Prakash; Conceptualization, study design, data analysis, data interpretation and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their earnest gratefulness to my family, friends, batchmates and ILBS team for their co-operation.
References
South East Sydney Local Health District., 2021. Adult Emergency Nurse Protocol - Gastrointestinal bleed. Sydney: South East Sydney Local Health District.
Amer, W. M., Taha, N. M. & Zaton, H. K., 2015. Nurses knowledge and practice regarding gastrointestinal endoscopy and suggested nursing guidelines. Afro-Egyptian Journal of Infectious and Endemic Diseases, 5(2), pp. 115–30. [DOI:10.21608/AEJI.2015.17820]
Amsalu, E. T., Messele, T. A. & Adane, M., 2021. Exploring the effect of professional experience on knowledge towards geriatric care among nurses working in adult care units. BMC Geriatrics, 21(1), pp. 227. [DOI:10.1186/s12877-021-02156-3] [PMID]
Antunes, C. & Copelin II, E. L., 2023. Upper gastrointestinal bleeding. In StatPearls. StatPearls Publishing. [PMID]
Bayumi, H., 2016. Clinical outcomes and patient satisfaction assessment among upper gastrointestinal bleeding at qena university hospital at upper Egypt. Journal of Nursing and Health Science, 5 (6), pp. 130-9. [Link]
Dewit, S. C. & Kumagai, C. K., 2013. Medical-surgical nursing: Concept and practice. Amsterdam: Elsevier. [Link]
Khalifa, Z. I., et al., 2015. Effect of designed implemented nurses’ educational program on minimizing incidence of complications for patients with upper gastrointestinal bleeding. Egyptian Journal of Health Care, 6(1), pp. 41-65. [Link]
Kuchaki, Z., et al., 2022. The effect of CPR educational package on knowledge and performance of nurses working in intensive care units: A review study. Journal of Family Medicine and Primary Care, 11(5), pp. 1677–82. [DOI:10.4103/jfmpc.jfmpc_1938_21] [PMID]
Laine, L., et al., 2021. ACG clinical guideline: Upper gastrointestinal and ulcer bleeding. The American Journal of Gastroenterology, 116(5), pp. 899–917. [DOI:10.14309/ajg.0000000000001245] [PMID]
Mohamad, A., Mohamad, Z. & Sayed, Z., 2014.“Esophagogastroduodenoscopy”: Impact of a designed nursing teaching protocol on nurse’s performance and patient’s outcome. Journal of American Science, 10(10), pp. 56-65. [Link]
Mohammed, G., 2011. Infection control: Effect of a designed teaching protocol on nurses’ knowledge and practice regarding to hematemesis patients [MA thesis]. Assiut: Assiut University. [Link]
National Institute for Health and Care Excellence., 2012. Acute upper gastrointestinal bleeding in over 16s: Management. London: National Institute for Health and Care Excellence. [Link]
Othman, S., 2018. Nursing guidelines for hematemesis patients undergoing upper gastrointestinal endoscopy [MA. thesis]. Mansoura: Mansoura University.
Reda, M., et al., 2015. Prospective assessment of the rockall risk scoring system in Egyptian patients with upper gastrointestinal Bleeding. Open Journal of Gastroenterology, 5(6), pp. 66-76. [DOI:10.4236/ojgas.2015.56012]
Sayed, S., 2018. Infection control: Effect of a structured nursing protocol on practice scores of nurses working with hematemsis patients. Journal of Nursing and Health Science, 7(4), pp. 38-45. [Link]
Siau, K., et al., 2017. Management of acute upper gastrointestinal bleeding: An update for the general physician. The Journal of the Royal College of Physicians of Edinburgh, 47(3), pp. 218–230.[DOI:10.4997/jrcpe.2017.303] [PMID]
Smith, G. D., 2004. The management of upper gastrointestinal bleeding. Nursing Times, 100 (26), pp. 40-3. [PMID]
Suleiman, A., 2018. Nurses’ performance regarding emergency management of patient with acute upper gastrointestinal bleeding in Ibinsinaa Hospital 2017. [PhD dissertation]. Khartoum: Neelain University. [Link]
Tielleman, T., Bujanda, D. & Cryer, B., 2015. Epidemiology and risk factors for upper gastrointestinal bleeding. Gastrointestinal Endoscopy Clinics of North America, 25 (3), pp. 415-28. [DOI:10.1016/j.giec.2015.02.010] [PMID]
Urden, L., Stacy, K. & Lough, M., 2015. Priorities in critical care nursing. Gastrointestinal disorder and therapeutic management. Missouri: Mosby. [Link]
Yue, L., Plummer, V. & Cross, W., 2017. The effectiveness of nurse education and training for clinical alarm response and management: A systematic review. Journal of Clinical Nursing, 26(17-18), pp. 2511–26. [DOI:10.1111/jocn.13605] [PMID]


Type of Study: Research |
Subject:
Special
Received: 2023/07/23 | Accepted: 2023/09/9 | Published: 2024/01/10
Received: 2023/07/23 | Accepted: 2023/09/9 | Published: 2024/01/10
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






