Sat, Jul 12, 2025
[Archive]
Volume 10, Issue 3 (Summer 2024)
JCCNC 2024, 10(3): 199-210 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Herrera C N, Brito Guirardello E D. Patient Safety Climate in the Hospital Setting: Perception of Nursing Professionals. JCCNC 2024; 10 (3) :199-210
URL: http://jccnc.iums.ac.ir/article-1-550-en.html
URL: http://jccnc.iums.ac.ir/article-1-550-en.html
1- Department of General and Specialized Nursing, College of Nursing, University of São Paulo, Ribeirão Preto, Brazil. , claire.nierher@usp.br
2- School of Nursing, University of Campinas, São Paulo, Brazil.
2- School of Nursing, University of Campinas, São Paulo, Brazil.
Full-Text [PDF 601 kb]
(388 Downloads)
| Abstract (HTML) (1832 Views)
Full-Text: (255 Views)
Introduction
Unsafe healthcare practices represent a significant global public health challenge and are among the leading causes of disability and mortality on a worldwide scale. Within this context, it is estimated that approximately 2.6 million deaths occur annually due to adverse events resulting from unsafe care in healthcare organizations in the low- and middle-income countries (WHO, 2021).
The COVID-19 pandemic has led to the collapse of healthcare services, which in turn has the potential to worsen patient safety (Taylor et al., 2020; González-Gil et al., 2021; Brborović et al., 2022). One of the first studies in the United States that examined event notifications during the pandemic found that the primary contributing factors were related to laboratory tests, protocols, and safe isolation. These events’ frequency varied across different healthcare areas (Taylor et al., 2020). During the pandemic, there was a decrease in event reporting (Taylor et al., 2020; Denning et al., 2020; Brborović et al., 2022), along with a diminished perception of specific safety climate dimensions (Denning et al., 2020; González-Gil et al., 2021; Brborović et al., 2022).
The global patient safety action plan outlines objectives, including developing protocols to eliminate avoidable harm, building high-reliability healthcare systems, ensuring safety in all clinical processes, and empowering healthcare professionals to enhance care quality and patient safety (WHO, 2021). Evaluating the safety climate is crucial in reducing harm from healthcare delivery, as a positive organizational culture supports a safe environment (Karaca et al., 2022). However, sustaining such a culture requires a strong commitment to patient safety (Karaca et al., 2022). The safety climate is a measurable component of the safety culture within the organization. It is related to the attitudes and perceptions of individuals within the organization at a given moment, encompassing an even broader spectrum of organizational characteristics (Halligan & Zecevic, 2011).
Researchers have emphasized that professionals hold diverse perceptions of the safety climate (Castilho et al., 2020; Dorigan et al., 2020; Kolankiewicz et al., 2020), which can be influenced by cultural factors (Castilho et al., 2020) and demographic characteristics like gender, age, education, and year of experience (Jiang et al., 2019; Denning et al., 2020; Karaca et al., 2022). Significant differences exist between these characteristics and the dimensions of patient safety climate, as professionals may have contrasting experiences and perspectives on this subject (Jiang et al., 2019; Karaca et al., 2022).
The patient safety climate in healthcare organizations (PSCHO) is one of the measures used to evaluate the safety climate and identify issues in interpersonal, organizational, and work unit contexts (Singer et al., 2009a). It is a valuable tool for managers to oversee vital safety processes, facilitating early detection and prevention (Singer et al., 2009a). It is grounded in the theory of high-reliability organizations (HROs), which excel in managing safety in hazardous conditions and preventing accidents in high-risk environments (Singer et al., 2009a; Hartmann, 2009; Benzer et al., 2017). HROs attain safety, quality, and efficiency by implementing five core principles: Attentiveness to operations, continuous concern for potential failures, reluctance to simplify, resilience, and deference to expertise (Veazie et al., 2019). Thus, this study aimed to evaluate the percentage of problematic responses (PPR) for patient safety climate dimensions and verify whether they differ among personal, professional, and work unit variables.
Materials and Methods
Design, setting and sample
A cross-sectional study was conducted in a Tertiary Teaching Hospital in São Paulo, Brazil. The research population involved 982 nursing professionals, comprising 242 registered nurses and 740 nurse technicians (NT), working across various units, including adult inpatient unit (AIU), adult intensive care unit (AICU), emergency unit (EU) and pediatrics unit (PED).
The sample size was determined by considering the calculation methodology used to estimate the population proportion (Medronho et al., 2008). A significance level and sampling error of 5% were considered, with a proportion of P=0.05 to represent the maximum variability of the binomial distribution. The calculation resulted in a minimum sample requirement of 69 registered nurses (RN) and 208 NT.Top of Form The study included nursing professionals in direct patient care or managerial roles but excluded those on leave of absence during the data collection period.
Data gathering occurred from July to October 2021, using an online format due to COVID-19 precautions. The nursing professionals were invited to participate through posters with QR codes, which were placed in different units and led to the Google Forms questionnaire.
Study measures
Personal and professional variables: A data form was employed to gather personal and professional information, which included sex, age, nursing professional category, job type, work unit, years of experience in the profession and the institution, work shift and other employment. Nursing professionals were also asked about the number of patients they cared for during their last shift and three questions related to the COVID-19 pandemic: “Have you worked or are you currently working in places/units providing care to COVID-19 patients?” “Have you been diagnosed with COVID-19?” and “During the pandemic, have you had any periods of absence?” The first and second questions were answered with either yes or no, while the third question was answered with either yes, due to a diagnosis of COVID-19, yes, for other health reasons, or no.
PSCHO
PSCHO is used to assess the safety climate in healthcare organizations and identify the PPR (Singer et al., 2009a; Benzer et al., 2017). It consists of 38 items with 12 dimensions, divided into three categories: Organizational aspects (senior managers’ engagement, overall emphasis on patient safety, and organizational resources for safety), work unit (unit recognition and support for safety efforts, unit managers’ support, unit safety norms, collective learning, psychological safety and problem responsiveness), and interpersonal aspects (fear of shame, fear of blame and punishment). Additionally, the dimension known as “provision of safe care,” while not explicitly falling under any of these categories, is considered part of the PSCHO dimension due to its significance (Cunha, 2018; Benzer et al., 2017).
It is scored on a 5-point Likert scale ranging from strongly disagree (1 point) to strongly agree (5 points). For the calculation of the PPR, the options strongly disagree (1 point) and disagree (2 points) should be considered. Percentage levels above 10% suggest a negative perception of the safety climate (Singer et al., 2009a; Hartmann et al., 2009). The reliability of the PSCHO dimensions, assessed by the Cronbach α, ranged from 0.61 to 0.89 for the original version (Hartmann et al., 2008), 0.52 to 0.77 for the Brazilian version (Cunha, 2018) and 0.50 to 0.80 in the context of this study.
Statistical analysis
The data were analyzed using SAS software, version 9.4. Descriptive statistics included frequency (n), Mean±SD, interquartile range (IQR), median (MED), and percentage (%). For comparing variables and dimensions of PSCHO, tests such as the Mann-Whitney, analysis of variance, or the Kruskal-Wallis were utilized, followed by the Dunn or Tukey post hoc test. The data distribution was assessed using the Shapiro-Wilk test, and a significance level of 0.05 was applied to all analyses.
Results
There were 325 nursing professionals, including 100 RNs and 225 NTs, with a mean age of 41.66± 9.11 years. Their mean years of experience in the profession was 16.36±8.24 years and 10.24±8.20 years in the institution. Table 1 presents other characteristics of the participants. Most subjects, 260(80%), worked or had worked in units caring for COVID-19 patients.

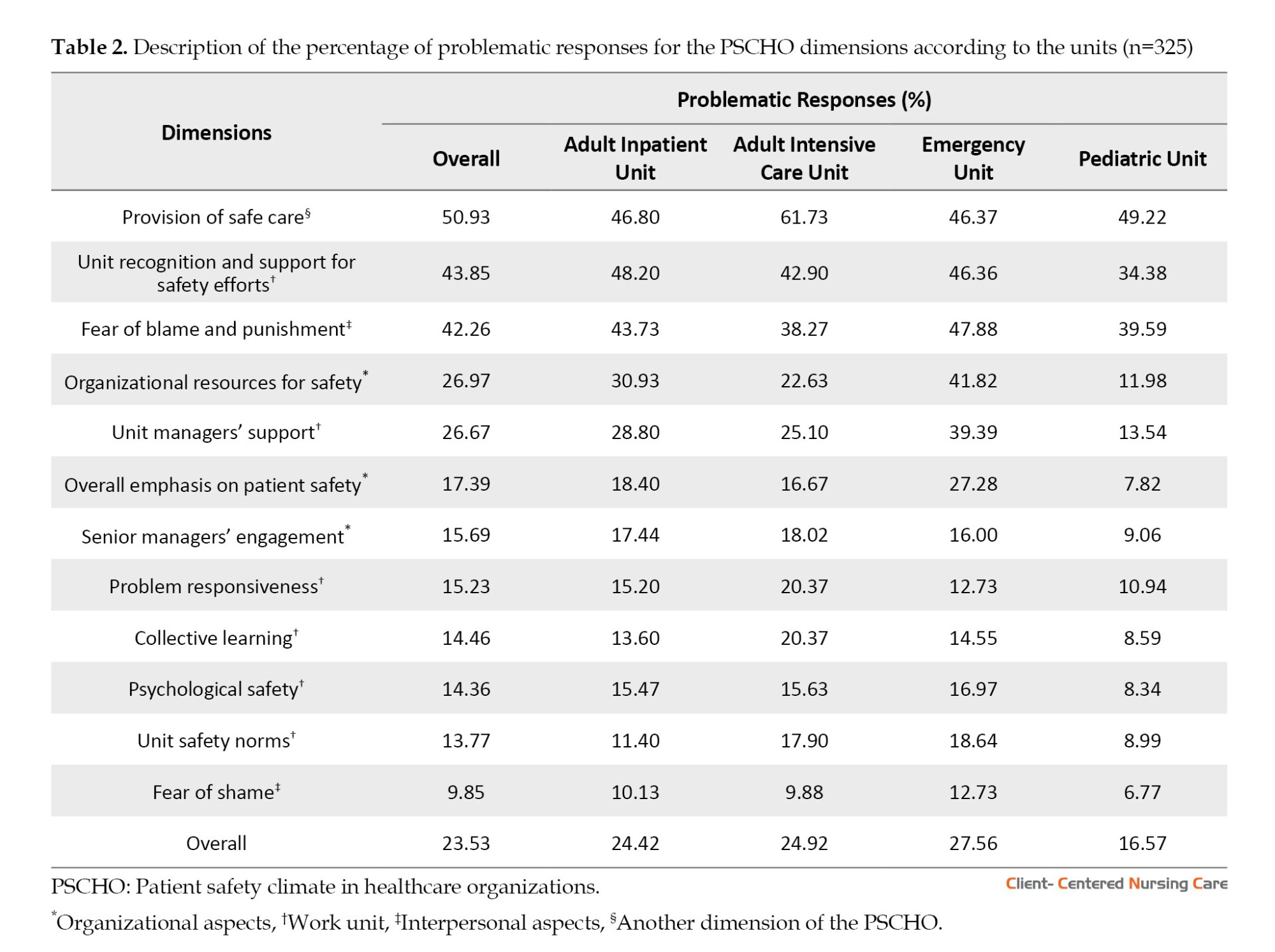
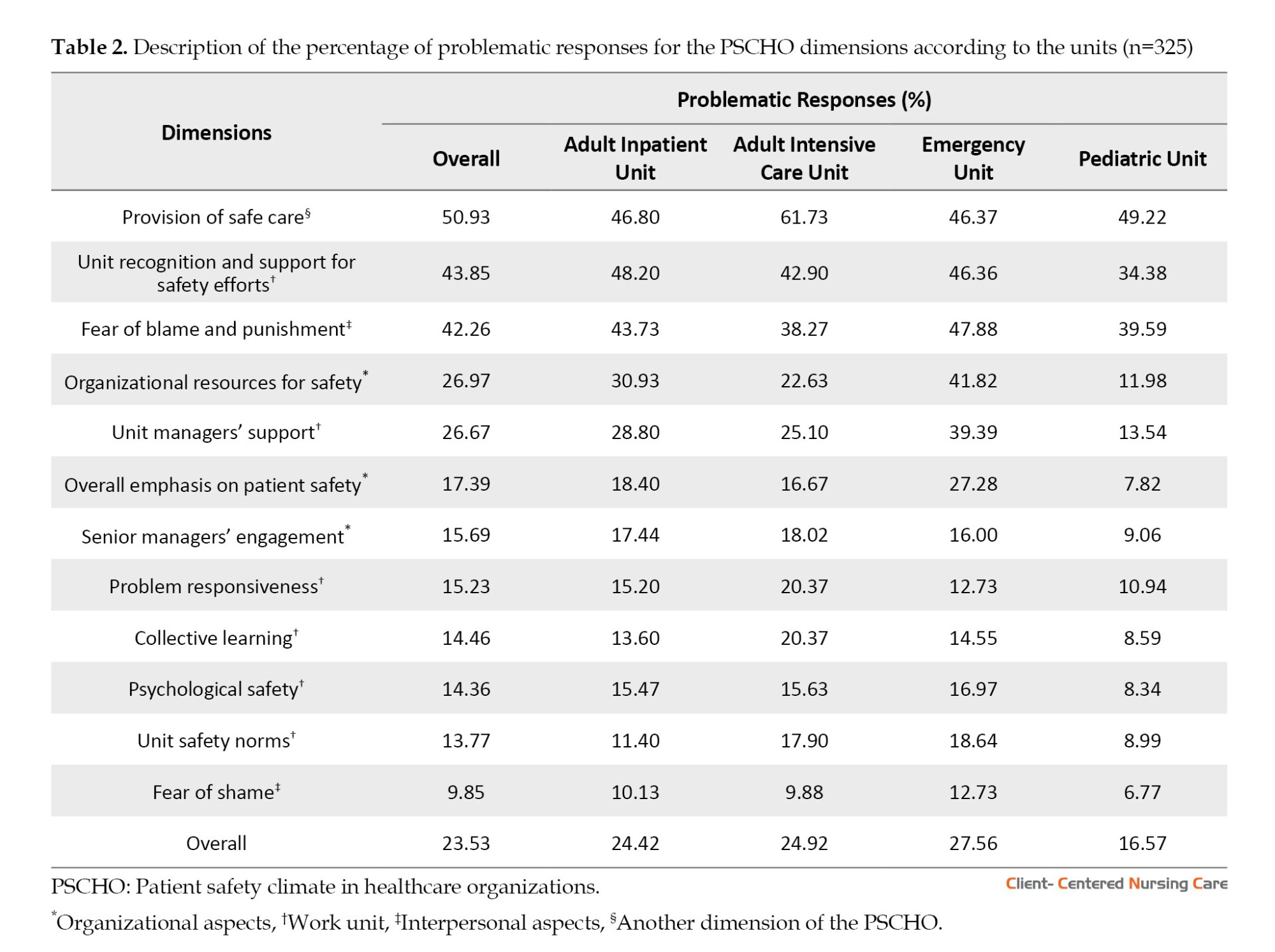
Among them, 164(50.46%) had been diagnosed with COVID-19. Regarding health-related absences, 145(44.62%) reported being absent due to COVID-19, while 65(20%) reported being absent for other health reasons. There were no significant differences regarding the participants who worked or are currently working in places/units providing care to COVID-19 patients and who have been diagnosed with COVID-19. Table 2 presents the PPR considering the overall sample and work unit, wherein a PPR lower than 10% may suggest or indicate a more positive perception of the safety climate.
The comparison of the study variables with the PSCHO dimensions showed statistically significant differences regarding sex, nursing professional category, work shift, other employment, and absence due to health reasons (Table 3). According to Table 3, female participants reported higher scores for fear of shame (P<0.02) and fear of blame and punishment (P<0.006) but lower scores in the provision of safe care compared to males (P<0.0007). RNs reported higher scores in fear of blame and punishment (P<0.0001) and lower in the provision of safe care (P<0.0001) compared to NTs.
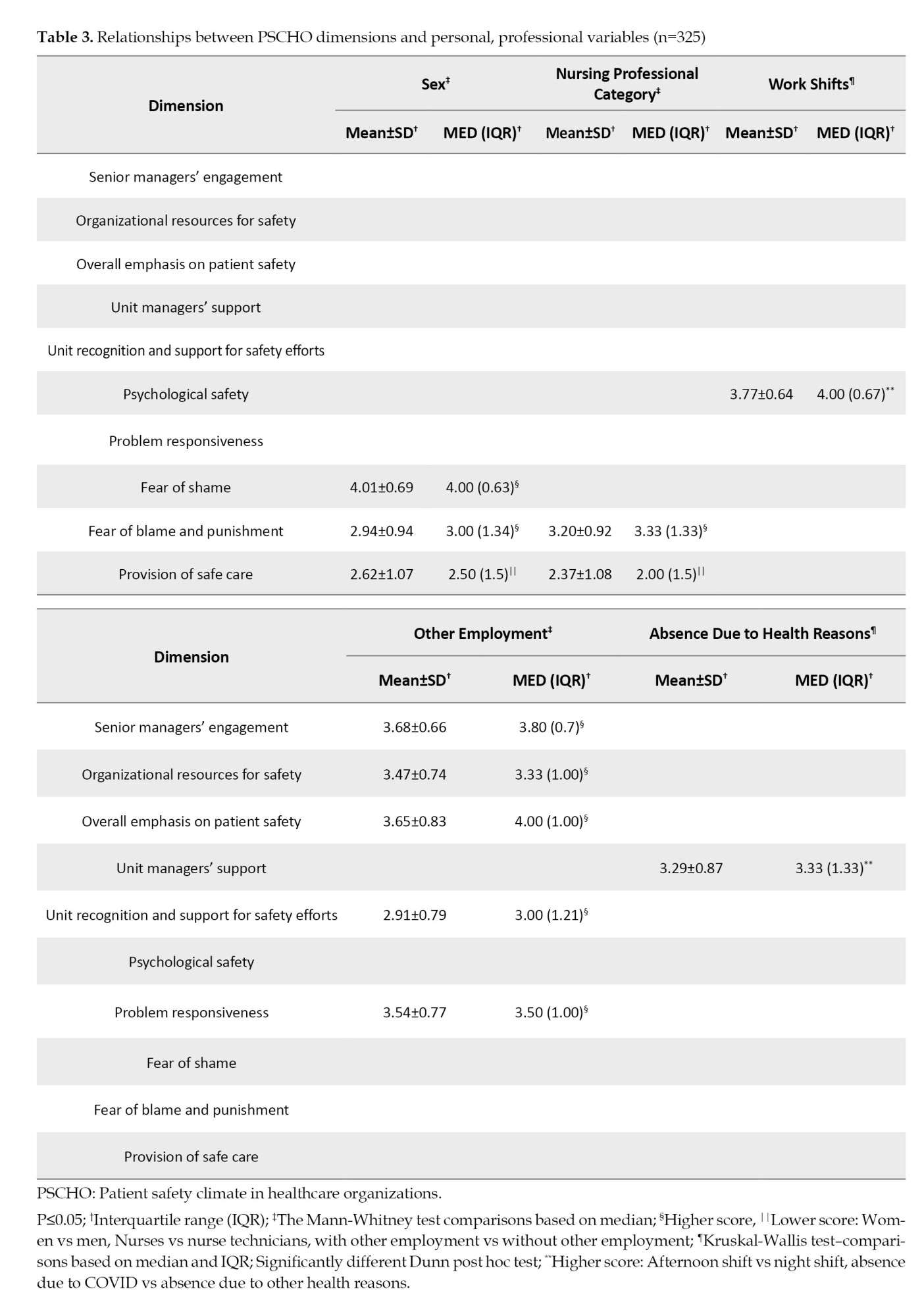
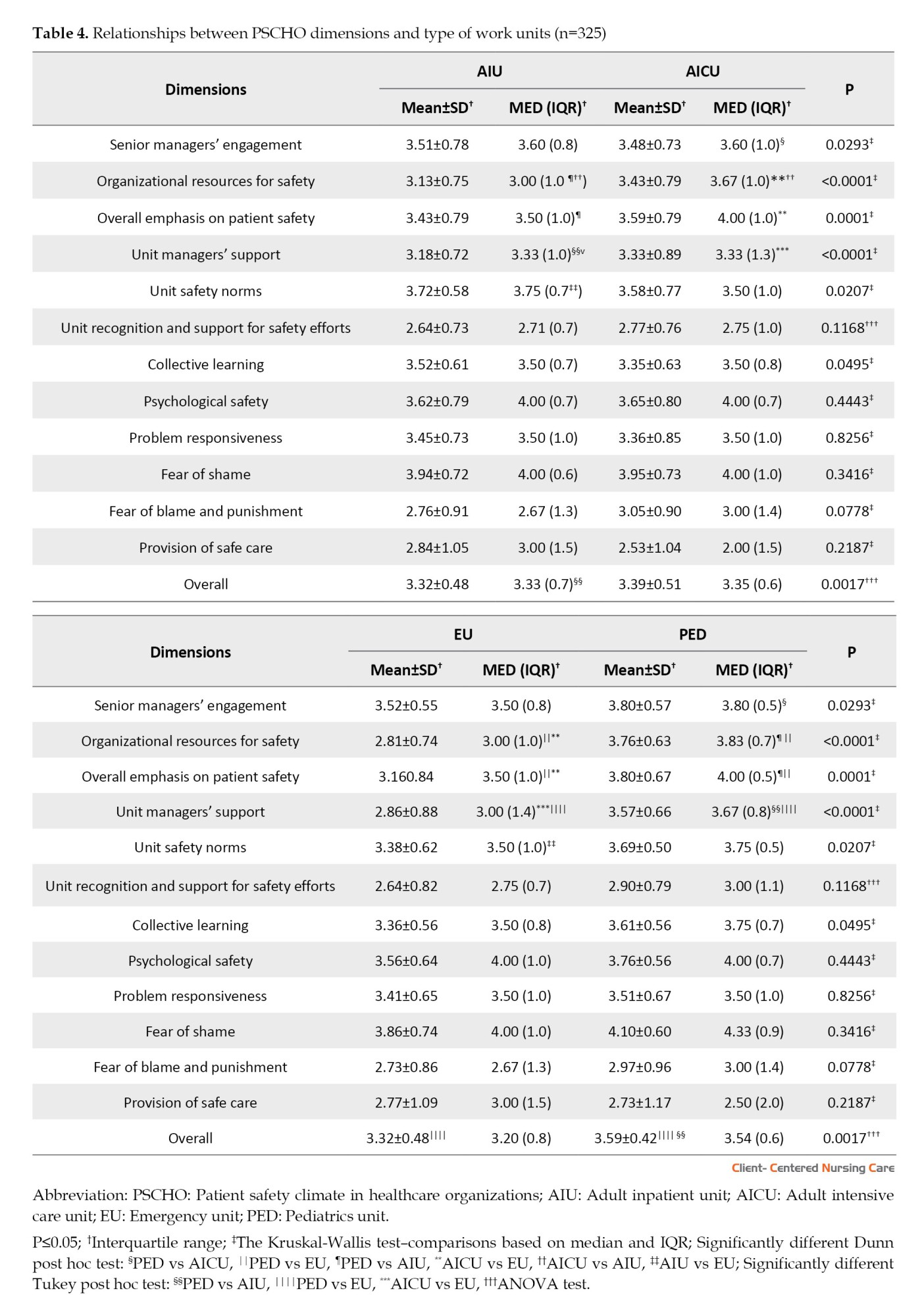
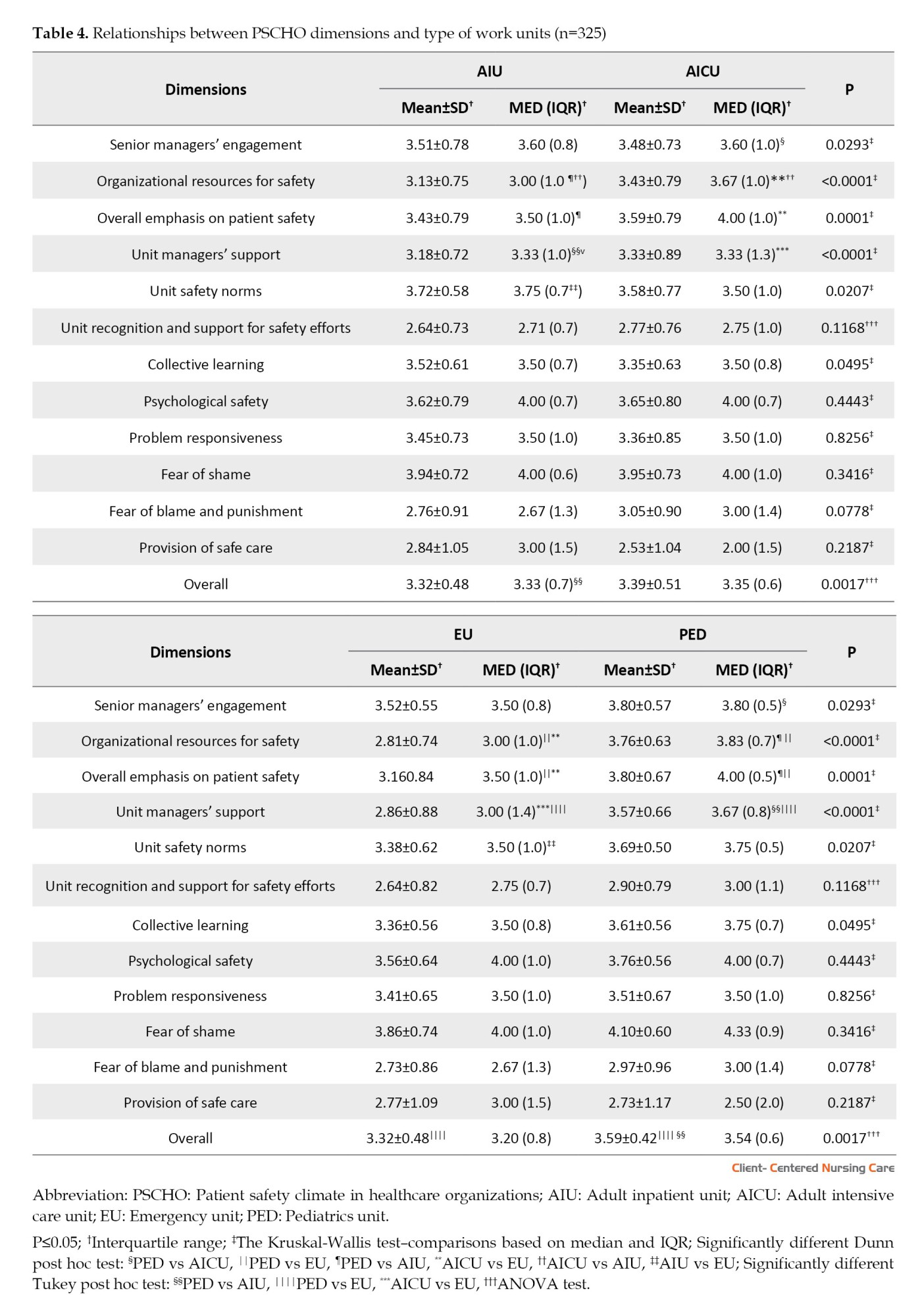
Nursing professionals with other employments reported higher scores on five dimensions than participants with only one job. These dimensions were senior managers’ engagement (P=0.048), organizational resources for safety (P=0.005), overall emphasis on patient safety (P=0.012), unit recognition and support for safety efforts (P=0.006) and problem responsiveness (P=0.044). They differed among work shifts regarding their perception of psychological safety (P=0.041), with participants working the afternoon shift (P=0.039) scoring higher in this dimension compared to those working the night shift (P=0.039). Regarding absences due to health reasons (P=0.039), those who had absences due to COVID-19 (P=0.039) reported higher scores in unit manager’s support compared with absences due to other health reasons (P=0.049) (Table 3). Table 4 presents the relationship between PSCHO dimensions and work units.
Discussion
The high PPR for most dimensions indicates the need for improvement in the patient safety culture within the institution. Among the dimensions with higher rates of PPR, the provision of safe care stands out, followed by unit recognition and support for safety efforts and fear of blame and punishment. The dimensions with higher PPR can be compared to another study that used the hospital survey on patient safety culture (HSOPSC) (Melo et al., 2020). In that study, it was observed that the dimensions of non-punitive response to errors and supervisor/manager expectations and actions promoting safety received lower positive responses.
These findings can be related to the dimensions of unit recognition, support for safety efforts, and fear of blame and punishment in PSCHO. The negative perception of safety climate, considering the theory of HROs (Hartmann et al., 2008; Hartmann, 2009), which prioritizes safety and emphasizes key components like strong institutional commitment, robust organizational support, and comprehensive professional training, structural aspects of hospitals, including size, type, location, nursing staff ratios and financial resources, can significantly influence patient safety (Singer et al., 2009a; Singer et al., 2009b).
Regarding work units, professionals from the AICU reported the highest PPR compared to other units. Nurses in this unit not only care for critically ill patients but also work during chaotic scenarios, potentially leading to issues like dynamic changes in directives and guidelines, the increased need for personal protective equipment, isolation protocols, and preparedness for handling COVID-19 patients. However, nursing professionals in the AICU showed low PPR for the dimension of fear of shame, indicating a positive perception of a safe climate only for this dimension. The low PPR on fear of shame in the AICU was different from other studies in which professionals that make mistakes not only embarrass themselves but also the team (Zhou et al., 2015). In other studies, communication openness showed a weaker positive response (Melo et al., 2020). Consequently, communication with immediate managers was not perceived as effective (González-Gil et al., 2021) and these nurses may be considered a vulnerable population because they are often exposed to COVID-19 at work, making them susceptible to developing psycho-emotional problems in the short and medium term (González-Gil et al., 2021).
Among the units, PED stood out for having six dimensions with lower PPR, including fear of shame, overall emphasis on patient safety, psychological safety, collective learning, unit safety norms, and senior managers’ engagement. This finding highlights the importance of good working conditions in shaping a safety culture within the institution, establishing a high-quality hospital service system (Denning et al., 2020) and the role played by nurses and the necessity for adequate support and resources to enhance their effectiveness in managing critical care situations (González-Gil et al., 2021). It may indicate that, in terms of organizational aspects, the unit managers support a climate that promotes patient safety. Overall, it also suggests that the institution invests in improvements for patient safety (Singer et al., 2009b).
Behaviors, whether positive or negative, towards patient safety culture significantly impact the formation and strength of patient safety cultures within institutions (Karaca et al., 2022). A high PPR may suggest significant concerns regarding patient safety and the working conditions of nursing professionals. It is crucial for all healthcare personnel, including nurses, to be actively encouraged to foster a harmonious work environment and maintain open and constant communication (Karaca et al., 2022).
Perceptions of safety climate differed among participants concerning sex, professional category, shift, and employment status, as observed in previous studies (Jiang et al., 2019; Castilho et al., 2020; Kolankiewicz et al., 2020). The present study showed statistically significant differences between women and men; in contrast, another study found no statistically significant differences between nurses’ scores in terms of sex (Karaca et al., 2022). Women tend to view the interpersonal aspect more positively than men, while men have a more positive perception of providing safe care than women. Gender differences in the perception of these dimensions may be influenced by various factors, including societal norms, gender roles, and individual experiences (Karaca et al., 2022).
Nursing professionals in this study differed in their perception of the patient safety climate for providing safe care and fear of blame and punishment. The fear of punishment can make healthcare professionals reluctant to report errors. When leaders view errors as valuable learning opportunities rather than punishable offenses, they can foster a culture where employees feel secure in reporting errors and seeking assistance (Karaca et al., 2022). Such a positive approach to handling mistakes encourages transparency and promotes a supportive and learning-oriented environment within the organization (Karaca et al., 2022).
In this study, work shifts also influenced participants’ perceptions of the safety climate. The findings revealed that the participants on the afternoon shift exhibited a more positive perception of psychological safety than those on the night shift. Other national studies have also found significant differences in these variables among work shifts, with some dimensions (Castilho et al., 2020; Melo et al., 2020).
Having multiple employment also influenced a better perception of issues related to organizational aspects and work units, such as unit recognition and support for safety efforts and problem responsiveness. This result may also indicate the institution’s support for the well-being of nursing professionals and the quality of care provided to patients. The positive perception of these dimensions may be due to the comparison with their other job since many have been exposed to different practice settings during the pandemic. However, there are no studies that allow for direct comparisons. On the other hand, a study conducted in Brazil before the pandemic found no difference among professionals regarding having multiple employment (Kolankiewicz et al., 2020).
Regarding absences due to health reasons, the findings indicated that individuals who were absent due to a diagnosis of COVID-19 reported a positive perception of unit manager support compared to those absent for other health reasons. This finding aligns with findings from other studies (Denning et al., 2020), where institutional managers demonstrated sensitivity to the needs of participants who contracted COVID-19. These findings also demonstrate that by coordinating within working units and prioritizing patient safety over adherence to work schedules or emphasizing productivity, institutional managers play a crucial role in assigning high importance to patient safety (Singer et al., 2009a; Singer et al., 2009b).
Significant differences were observed in perceptions among work units for six out of twelve dimensions. However, after the post hoc test, the collective learning dimension presented no statistically significant differences among the units. Nursing professionals in the PED reported more positive perceptions than those in the AICU regarding senior managers’ engagement. Additionally, participants in the PED also reported more positive perceptions of organizational resources for safety, overall emphasis on patient safety, unit managers’ support, and the overall score compared to participants in the AIU and EU. These results can be explained by the characteristics of the patients, who are children and infants. These groups are considered highly vulnerable, requiring a greater complexity of care compared to adult patients. During the data collection period, a significantly higher demand for care was observed in adult patients compared to children and infants.
Nursing professionals in the AICU better perceived organizational resources for safety compared to those in the AIU and EU. AICU participants also reported positive perceptions regarding the dimensions of unit managers’ support and overall emphasis on patient safety compared to participants in the EU. The AICU stood out compared to the AIU and EU because it depends on a structure with human and material resources to meet the complexity of care required by patients 24 hours a day and these resources were intensified during the pandemic period. These findings also reflect the PPR among the units. Although participants in the AICU reported the highest PPR for providing safe care in the unit, the comparison still implies that the unit manager in the AICU coordinated and placed high importance on patient safety.
Nursing professionals in AIU had a higher perception of unit safety norms than those in the EU. This finding suggests that nursing professionals in the EU are exposed to the unknown compared to AIU, and maintaining stability and control regarding patient and professional safety climate is unlikely. This finding also reflects the PPR results among the units regarding the dimensions of safety norms.
The COVID-19 pandemic had a profound effect on logistics in the workplace, potentially influencing perceptions and introducing additional stressors related to patient safety. The dynamic changes in directives and guidelines during the pandemic and the increased need for personal protective equipment and isolation protocols present challenges in patient care within an uncertain environment. Consequently, the study results should be cautiously approached, considering the pervasive impact of the COVID-19 crisis during the research period. Finally, this also reflects the findings that participants in the EU had lower averages for all PSCHO dimensions. This unit is known for its high patient turnover, which may lead to experiencing symptoms of stress, fatigue, distress, mental exhaustion, and workload burden among professionals (Castilho et al., 2020).
Nurses’ sociodemographic and occupational characteristics significantly shape the patient safety culture and the effectiveness of quality nursing care delivery. The quality of care and patient safety are deeply influenced by individual factors, including perception, attitudes, beliefs, culture, values and personality traits among nursing professionals (Karaca et al., 2022). In addition to individual attributes, factors such as the work environment, working conditions, team cohesion, organizational behavior, and corporate policies can also influence the quality of care and the prevailing patient safety culture within healthcare institutions (Castilho et al., 2020).
Nursing professionals’ perspectives were shaped by personal experiences, work environments, and organizational culture. These insights can help senior nurse managers prioritize factors in organizational, work unit, and interpersonal contexts. However, this study has limitations, including using self-report online questionnaires due to pandemic restrictions and the inability to generalize findings to healthcare settings beyond a single tertiary teaching hospital in Brazil. Lastly, the study’s cross-sectional design does not allow for causal relationships.
Conclusion
The perception of patient safety climate differed among work units, nursing professional category, sex, work shift, absence due to health reasons, and other employments. The nursing professionals reported a high PPR for most dimensions, except for fear of shame. When comparing the work units, the AICU had the highest PPR for providing safe care compared to the other work units. On the other hand, the PED had the highest dimensions with lower PPR. Standardized policies and protocols vary among units, and it is crucial to analyze findings considering personal and professional factors like work shifts and health-related absences. This condition can enhance nursing satisfaction and the quality of care in each unit.
The hospital’s patient safety nucleus should actively share results with all healthcare professionals and users to promote awareness and emphasize their roles in improving the hospital. Future research should involve a larger, multidisciplinary sample, including doctors, to investigate how various professional variables influence patient safety climate.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Tertiary Teaching Hospital where the study took place (Code: 4.452.598). Participants were provided with an informed consent form that they could access electronically before starting the survey. Participation in the study was voluntary and they were assured complete anonymity.
Funding
This work was supported by the Coordination for the Improvement of Higher Education Personnel-Brazil (CAPES) (Grant No.: 001).
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the nursing professionals who participated in this study and research group that helped disseminate this study. Additionally, we extend our gratitude to our university statistician for assisting us with our analysis methods.
References
Unsafe healthcare practices represent a significant global public health challenge and are among the leading causes of disability and mortality on a worldwide scale. Within this context, it is estimated that approximately 2.6 million deaths occur annually due to adverse events resulting from unsafe care in healthcare organizations in the low- and middle-income countries (WHO, 2021).
The COVID-19 pandemic has led to the collapse of healthcare services, which in turn has the potential to worsen patient safety (Taylor et al., 2020; González-Gil et al., 2021; Brborović et al., 2022). One of the first studies in the United States that examined event notifications during the pandemic found that the primary contributing factors were related to laboratory tests, protocols, and safe isolation. These events’ frequency varied across different healthcare areas (Taylor et al., 2020). During the pandemic, there was a decrease in event reporting (Taylor et al., 2020; Denning et al., 2020; Brborović et al., 2022), along with a diminished perception of specific safety climate dimensions (Denning et al., 2020; González-Gil et al., 2021; Brborović et al., 2022).
The global patient safety action plan outlines objectives, including developing protocols to eliminate avoidable harm, building high-reliability healthcare systems, ensuring safety in all clinical processes, and empowering healthcare professionals to enhance care quality and patient safety (WHO, 2021). Evaluating the safety climate is crucial in reducing harm from healthcare delivery, as a positive organizational culture supports a safe environment (Karaca et al., 2022). However, sustaining such a culture requires a strong commitment to patient safety (Karaca et al., 2022). The safety climate is a measurable component of the safety culture within the organization. It is related to the attitudes and perceptions of individuals within the organization at a given moment, encompassing an even broader spectrum of organizational characteristics (Halligan & Zecevic, 2011).
Researchers have emphasized that professionals hold diverse perceptions of the safety climate (Castilho et al., 2020; Dorigan et al., 2020; Kolankiewicz et al., 2020), which can be influenced by cultural factors (Castilho et al., 2020) and demographic characteristics like gender, age, education, and year of experience (Jiang et al., 2019; Denning et al., 2020; Karaca et al., 2022). Significant differences exist between these characteristics and the dimensions of patient safety climate, as professionals may have contrasting experiences and perspectives on this subject (Jiang et al., 2019; Karaca et al., 2022).
The patient safety climate in healthcare organizations (PSCHO) is one of the measures used to evaluate the safety climate and identify issues in interpersonal, organizational, and work unit contexts (Singer et al., 2009a). It is a valuable tool for managers to oversee vital safety processes, facilitating early detection and prevention (Singer et al., 2009a). It is grounded in the theory of high-reliability organizations (HROs), which excel in managing safety in hazardous conditions and preventing accidents in high-risk environments (Singer et al., 2009a; Hartmann, 2009; Benzer et al., 2017). HROs attain safety, quality, and efficiency by implementing five core principles: Attentiveness to operations, continuous concern for potential failures, reluctance to simplify, resilience, and deference to expertise (Veazie et al., 2019). Thus, this study aimed to evaluate the percentage of problematic responses (PPR) for patient safety climate dimensions and verify whether they differ among personal, professional, and work unit variables.
Materials and Methods
Design, setting and sample
A cross-sectional study was conducted in a Tertiary Teaching Hospital in São Paulo, Brazil. The research population involved 982 nursing professionals, comprising 242 registered nurses and 740 nurse technicians (NT), working across various units, including adult inpatient unit (AIU), adult intensive care unit (AICU), emergency unit (EU) and pediatrics unit (PED).
The sample size was determined by considering the calculation methodology used to estimate the population proportion (Medronho et al., 2008). A significance level and sampling error of 5% were considered, with a proportion of P=0.05 to represent the maximum variability of the binomial distribution. The calculation resulted in a minimum sample requirement of 69 registered nurses (RN) and 208 NT.Top of Form The study included nursing professionals in direct patient care or managerial roles but excluded those on leave of absence during the data collection period.
Data gathering occurred from July to October 2021, using an online format due to COVID-19 precautions. The nursing professionals were invited to participate through posters with QR codes, which were placed in different units and led to the Google Forms questionnaire.
Study measures
Personal and professional variables: A data form was employed to gather personal and professional information, which included sex, age, nursing professional category, job type, work unit, years of experience in the profession and the institution, work shift and other employment. Nursing professionals were also asked about the number of patients they cared for during their last shift and three questions related to the COVID-19 pandemic: “Have you worked or are you currently working in places/units providing care to COVID-19 patients?” “Have you been diagnosed with COVID-19?” and “During the pandemic, have you had any periods of absence?” The first and second questions were answered with either yes or no, while the third question was answered with either yes, due to a diagnosis of COVID-19, yes, for other health reasons, or no.
PSCHO
PSCHO is used to assess the safety climate in healthcare organizations and identify the PPR (Singer et al., 2009a; Benzer et al., 2017). It consists of 38 items with 12 dimensions, divided into three categories: Organizational aspects (senior managers’ engagement, overall emphasis on patient safety, and organizational resources for safety), work unit (unit recognition and support for safety efforts, unit managers’ support, unit safety norms, collective learning, psychological safety and problem responsiveness), and interpersonal aspects (fear of shame, fear of blame and punishment). Additionally, the dimension known as “provision of safe care,” while not explicitly falling under any of these categories, is considered part of the PSCHO dimension due to its significance (Cunha, 2018; Benzer et al., 2017).
It is scored on a 5-point Likert scale ranging from strongly disagree (1 point) to strongly agree (5 points). For the calculation of the PPR, the options strongly disagree (1 point) and disagree (2 points) should be considered. Percentage levels above 10% suggest a negative perception of the safety climate (Singer et al., 2009a; Hartmann et al., 2009). The reliability of the PSCHO dimensions, assessed by the Cronbach α, ranged from 0.61 to 0.89 for the original version (Hartmann et al., 2008), 0.52 to 0.77 for the Brazilian version (Cunha, 2018) and 0.50 to 0.80 in the context of this study.
Statistical analysis
The data were analyzed using SAS software, version 9.4. Descriptive statistics included frequency (n), Mean±SD, interquartile range (IQR), median (MED), and percentage (%). For comparing variables and dimensions of PSCHO, tests such as the Mann-Whitney, analysis of variance, or the Kruskal-Wallis were utilized, followed by the Dunn or Tukey post hoc test. The data distribution was assessed using the Shapiro-Wilk test, and a significance level of 0.05 was applied to all analyses.
Results
There were 325 nursing professionals, including 100 RNs and 225 NTs, with a mean age of 41.66± 9.11 years. Their mean years of experience in the profession was 16.36±8.24 years and 10.24±8.20 years in the institution. Table 1 presents other characteristics of the participants. Most subjects, 260(80%), worked or had worked in units caring for COVID-19 patients.

Among them, 164(50.46%) had been diagnosed with COVID-19. Regarding health-related absences, 145(44.62%) reported being absent due to COVID-19, while 65(20%) reported being absent for other health reasons. There were no significant differences regarding the participants who worked or are currently working in places/units providing care to COVID-19 patients and who have been diagnosed with COVID-19. Table 2 presents the PPR considering the overall sample and work unit, wherein a PPR lower than 10% may suggest or indicate a more positive perception of the safety climate.
The comparison of the study variables with the PSCHO dimensions showed statistically significant differences regarding sex, nursing professional category, work shift, other employment, and absence due to health reasons (Table 3). According to Table 3, female participants reported higher scores for fear of shame (P<0.02) and fear of blame and punishment (P<0.006) but lower scores in the provision of safe care compared to males (P<0.0007). RNs reported higher scores in fear of blame and punishment (P<0.0001) and lower in the provision of safe care (P<0.0001) compared to NTs.
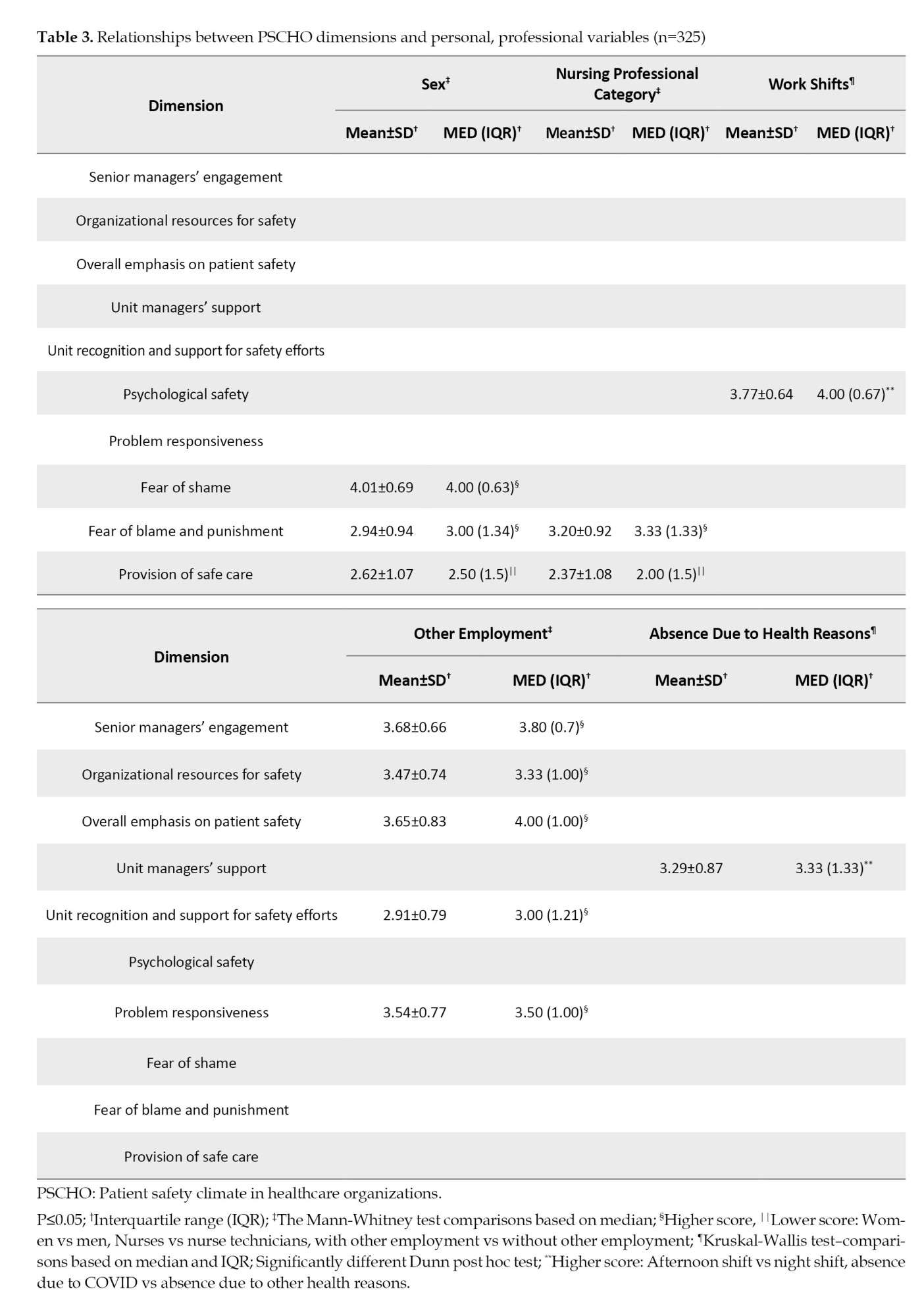
Nursing professionals with other employments reported higher scores on five dimensions than participants with only one job. These dimensions were senior managers’ engagement (P=0.048), organizational resources for safety (P=0.005), overall emphasis on patient safety (P=0.012), unit recognition and support for safety efforts (P=0.006) and problem responsiveness (P=0.044). They differed among work shifts regarding their perception of psychological safety (P=0.041), with participants working the afternoon shift (P=0.039) scoring higher in this dimension compared to those working the night shift (P=0.039). Regarding absences due to health reasons (P=0.039), those who had absences due to COVID-19 (P=0.039) reported higher scores in unit manager’s support compared with absences due to other health reasons (P=0.049) (Table 3). Table 4 presents the relationship between PSCHO dimensions and work units.
Discussion
The high PPR for most dimensions indicates the need for improvement in the patient safety culture within the institution. Among the dimensions with higher rates of PPR, the provision of safe care stands out, followed by unit recognition and support for safety efforts and fear of blame and punishment. The dimensions with higher PPR can be compared to another study that used the hospital survey on patient safety culture (HSOPSC) (Melo et al., 2020). In that study, it was observed that the dimensions of non-punitive response to errors and supervisor/manager expectations and actions promoting safety received lower positive responses.
These findings can be related to the dimensions of unit recognition, support for safety efforts, and fear of blame and punishment in PSCHO. The negative perception of safety climate, considering the theory of HROs (Hartmann et al., 2008; Hartmann, 2009), which prioritizes safety and emphasizes key components like strong institutional commitment, robust organizational support, and comprehensive professional training, structural aspects of hospitals, including size, type, location, nursing staff ratios and financial resources, can significantly influence patient safety (Singer et al., 2009a; Singer et al., 2009b).
Regarding work units, professionals from the AICU reported the highest PPR compared to other units. Nurses in this unit not only care for critically ill patients but also work during chaotic scenarios, potentially leading to issues like dynamic changes in directives and guidelines, the increased need for personal protective equipment, isolation protocols, and preparedness for handling COVID-19 patients. However, nursing professionals in the AICU showed low PPR for the dimension of fear of shame, indicating a positive perception of a safe climate only for this dimension. The low PPR on fear of shame in the AICU was different from other studies in which professionals that make mistakes not only embarrass themselves but also the team (Zhou et al., 2015). In other studies, communication openness showed a weaker positive response (Melo et al., 2020). Consequently, communication with immediate managers was not perceived as effective (González-Gil et al., 2021) and these nurses may be considered a vulnerable population because they are often exposed to COVID-19 at work, making them susceptible to developing psycho-emotional problems in the short and medium term (González-Gil et al., 2021).
Among the units, PED stood out for having six dimensions with lower PPR, including fear of shame, overall emphasis on patient safety, psychological safety, collective learning, unit safety norms, and senior managers’ engagement. This finding highlights the importance of good working conditions in shaping a safety culture within the institution, establishing a high-quality hospital service system (Denning et al., 2020) and the role played by nurses and the necessity for adequate support and resources to enhance their effectiveness in managing critical care situations (González-Gil et al., 2021). It may indicate that, in terms of organizational aspects, the unit managers support a climate that promotes patient safety. Overall, it also suggests that the institution invests in improvements for patient safety (Singer et al., 2009b).
Behaviors, whether positive or negative, towards patient safety culture significantly impact the formation and strength of patient safety cultures within institutions (Karaca et al., 2022). A high PPR may suggest significant concerns regarding patient safety and the working conditions of nursing professionals. It is crucial for all healthcare personnel, including nurses, to be actively encouraged to foster a harmonious work environment and maintain open and constant communication (Karaca et al., 2022).
Perceptions of safety climate differed among participants concerning sex, professional category, shift, and employment status, as observed in previous studies (Jiang et al., 2019; Castilho et al., 2020; Kolankiewicz et al., 2020). The present study showed statistically significant differences between women and men; in contrast, another study found no statistically significant differences between nurses’ scores in terms of sex (Karaca et al., 2022). Women tend to view the interpersonal aspect more positively than men, while men have a more positive perception of providing safe care than women. Gender differences in the perception of these dimensions may be influenced by various factors, including societal norms, gender roles, and individual experiences (Karaca et al., 2022).
Nursing professionals in this study differed in their perception of the patient safety climate for providing safe care and fear of blame and punishment. The fear of punishment can make healthcare professionals reluctant to report errors. When leaders view errors as valuable learning opportunities rather than punishable offenses, they can foster a culture where employees feel secure in reporting errors and seeking assistance (Karaca et al., 2022). Such a positive approach to handling mistakes encourages transparency and promotes a supportive and learning-oriented environment within the organization (Karaca et al., 2022).
In this study, work shifts also influenced participants’ perceptions of the safety climate. The findings revealed that the participants on the afternoon shift exhibited a more positive perception of psychological safety than those on the night shift. Other national studies have also found significant differences in these variables among work shifts, with some dimensions (Castilho et al., 2020; Melo et al., 2020).
Having multiple employment also influenced a better perception of issues related to organizational aspects and work units, such as unit recognition and support for safety efforts and problem responsiveness. This result may also indicate the institution’s support for the well-being of nursing professionals and the quality of care provided to patients. The positive perception of these dimensions may be due to the comparison with their other job since many have been exposed to different practice settings during the pandemic. However, there are no studies that allow for direct comparisons. On the other hand, a study conducted in Brazil before the pandemic found no difference among professionals regarding having multiple employment (Kolankiewicz et al., 2020).
Regarding absences due to health reasons, the findings indicated that individuals who were absent due to a diagnosis of COVID-19 reported a positive perception of unit manager support compared to those absent for other health reasons. This finding aligns with findings from other studies (Denning et al., 2020), where institutional managers demonstrated sensitivity to the needs of participants who contracted COVID-19. These findings also demonstrate that by coordinating within working units and prioritizing patient safety over adherence to work schedules or emphasizing productivity, institutional managers play a crucial role in assigning high importance to patient safety (Singer et al., 2009a; Singer et al., 2009b).
Significant differences were observed in perceptions among work units for six out of twelve dimensions. However, after the post hoc test, the collective learning dimension presented no statistically significant differences among the units. Nursing professionals in the PED reported more positive perceptions than those in the AICU regarding senior managers’ engagement. Additionally, participants in the PED also reported more positive perceptions of organizational resources for safety, overall emphasis on patient safety, unit managers’ support, and the overall score compared to participants in the AIU and EU. These results can be explained by the characteristics of the patients, who are children and infants. These groups are considered highly vulnerable, requiring a greater complexity of care compared to adult patients. During the data collection period, a significantly higher demand for care was observed in adult patients compared to children and infants.
Nursing professionals in the AICU better perceived organizational resources for safety compared to those in the AIU and EU. AICU participants also reported positive perceptions regarding the dimensions of unit managers’ support and overall emphasis on patient safety compared to participants in the EU. The AICU stood out compared to the AIU and EU because it depends on a structure with human and material resources to meet the complexity of care required by patients 24 hours a day and these resources were intensified during the pandemic period. These findings also reflect the PPR among the units. Although participants in the AICU reported the highest PPR for providing safe care in the unit, the comparison still implies that the unit manager in the AICU coordinated and placed high importance on patient safety.
Nursing professionals in AIU had a higher perception of unit safety norms than those in the EU. This finding suggests that nursing professionals in the EU are exposed to the unknown compared to AIU, and maintaining stability and control regarding patient and professional safety climate is unlikely. This finding also reflects the PPR results among the units regarding the dimensions of safety norms.
The COVID-19 pandemic had a profound effect on logistics in the workplace, potentially influencing perceptions and introducing additional stressors related to patient safety. The dynamic changes in directives and guidelines during the pandemic and the increased need for personal protective equipment and isolation protocols present challenges in patient care within an uncertain environment. Consequently, the study results should be cautiously approached, considering the pervasive impact of the COVID-19 crisis during the research period. Finally, this also reflects the findings that participants in the EU had lower averages for all PSCHO dimensions. This unit is known for its high patient turnover, which may lead to experiencing symptoms of stress, fatigue, distress, mental exhaustion, and workload burden among professionals (Castilho et al., 2020).
Nurses’ sociodemographic and occupational characteristics significantly shape the patient safety culture and the effectiveness of quality nursing care delivery. The quality of care and patient safety are deeply influenced by individual factors, including perception, attitudes, beliefs, culture, values and personality traits among nursing professionals (Karaca et al., 2022). In addition to individual attributes, factors such as the work environment, working conditions, team cohesion, organizational behavior, and corporate policies can also influence the quality of care and the prevailing patient safety culture within healthcare institutions (Castilho et al., 2020).
Nursing professionals’ perspectives were shaped by personal experiences, work environments, and organizational culture. These insights can help senior nurse managers prioritize factors in organizational, work unit, and interpersonal contexts. However, this study has limitations, including using self-report online questionnaires due to pandemic restrictions and the inability to generalize findings to healthcare settings beyond a single tertiary teaching hospital in Brazil. Lastly, the study’s cross-sectional design does not allow for causal relationships.
Conclusion
The perception of patient safety climate differed among work units, nursing professional category, sex, work shift, absence due to health reasons, and other employments. The nursing professionals reported a high PPR for most dimensions, except for fear of shame. When comparing the work units, the AICU had the highest PPR for providing safe care compared to the other work units. On the other hand, the PED had the highest dimensions with lower PPR. Standardized policies and protocols vary among units, and it is crucial to analyze findings considering personal and professional factors like work shifts and health-related absences. This condition can enhance nursing satisfaction and the quality of care in each unit.
The hospital’s patient safety nucleus should actively share results with all healthcare professionals and users to promote awareness and emphasize their roles in improving the hospital. Future research should involve a larger, multidisciplinary sample, including doctors, to investigate how various professional variables influence patient safety climate.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Tertiary Teaching Hospital where the study took place (Code: 4.452.598). Participants were provided with an informed consent form that they could access electronically before starting the survey. Participation in the study was voluntary and they were assured complete anonymity.
Funding
This work was supported by the Coordination for the Improvement of Higher Education Personnel-Brazil (CAPES) (Grant No.: 001).
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the nursing professionals who participated in this study and research group that helped disseminate this study. Additionally, we extend our gratitude to our university statistician for assisting us with our analysis methods.
References
Benzer, J. K., Meterko, M. & Singer S. J., 2017. The patient safety climate in healthcare organizations (PSCHO) survey: Short-form development. Journal of Evaluation in Clinical Practice, 23(4), PP. 853-9. [DOI:10.1111/jep.12731] [PMID]
Brborović, O., Brborović, H. & Hrain L., 2022. The COVID-19 pandemic crisis and Patient Safety Culture: A mixed-method study. International Journal of Environmental Research and Public Health, 19(4), pp. 2237. [DOI:10.3390/ijerph19042237] [PMID] [PMCID]
Castilho, D. E. C., et al., 2020. Factors related to the patient safety climate in an emergency hospital. Revista Latino-Americana de Enfermagem, 28, pp. e3273. [DOI:10.1590/1518-8345.3353.3273] [PMID] [PMCID]
Cunha, M. R. P. D., 2018. Cross-cultural adaptation and measurement properties evaluatio of the instrument Patient Safety in Healthcare Organizations (Original Work Published in University of Campinas [Portuguese]) [PhD dissertation]. São Paulo: UNICAMP Universidade Estadual de Campinas.
Denning M., et al., 2020. What has been the impact of Covid-19 on safety culture? A case study from a large metropolitan healthcare trust. International Journal of Environmental Research and Public Health, 17(19), pp. 7034. [DOI:10.3390/ijerph17197034] [PMID] [PMCID]
Dorigan, G. H., Mingato, D. F. P. & de Brito Guirardello, E., 2020. Nursing safety attitudes: Relationship with time of experience and intention to leave the job. Revista Gaucha de Enfermagem, 41, pp. e20190274. [DOI:10.1590/1983-1447.2020.20190274] [PMID]
González-Gil M.T., et al. 2021. Nurses’ perceptions and demands regarding COVID-19 care delivery in critical care units and hospital emergency services. Intensive & Critical Care Nursing: The Official Journal of the British Association of Critical Care Nurses, 62, pp. 102966. [DOI:10.1016/j.iccn.2020.102966] [PMID] [PMCID]
Halligan, M. & Zecevic, A., 2011. Safety culture in healthcare: A review of concepts, dimensions, measures and progress. BMJ Quality & Safety, 20(4), pp. 338-43. [DOI:10.1136/bmjqs.2010.040964] [PMID]
Hartmann C. W., et al., 2008. An overview of patient safety climate in the VA. Health Services Research, 43(4), pp. 1263–84. [DOI:10.1111/j.1475-6773.2008.00839.x] [PMID] [PMCID]
Hartmann C. W., et al., 2009. Relationship of hospital organizational culture to patient safety climate in the Veterans Health Administration. Medical Care Research and Review, 66(3), pp. 320-38. [DOI:10.1177/1077558709331812] [PMID]
Jiang K., et al., 2019. A cross-sectional survey on patient safety culture in secondary hospitals of Northeast China. Plos One, 14(3), pp. e0213055. [DOI:10.1371/journal.pone.0213055] [PMID] [PMCID]
Karaca A., et al., 2022. The relationship between perceived quality of care and the patient safety culture of Turkish nurses. Journal of Nursing Research, 30(4), pp. e223, [DOI:10.1097/jnr.0000000000000505] [PMID]
Kolankiewicz, A. C. B., et al. 2020. Patient safety culture from the perspective of all the workers of a general hospital. Revista Gaucha de Enfermagem, 41, pp. e20190177. [DOI:10.1590/1983-1447.2020.20190177] [PMID]
Melo, E., et al. 2020. Patient safety culture according to nursing professionals of an accredited hospital. Revista Gaucha de Enfermagem, 41, pp. e20190288. [DOI:10.1590/1983-1447.2020.20190288] [PMID]
Singer, S. J., et al. 2009a. Comparing safety climate between two populations of hospitals in the United States. Health Services Research, 44(5 Pt 1), pp. 1563–84. [DOI:10.1111/j.1475-6773.2009.00994.x] [PMID] [PMCID]
Singer, S. J., et al. 2009b. Identifying organizational cultures that promote patient safety. Health Care Management Review, 34, pp. 300-11. [DOI:10.1097/HMR.0b013e3181afc10c] [PMID]
Taylor M., et al., 2020. Patient safety concerns in COVID 19-related events: A study of 343 event reports from 71 hospitals in Pennsylvania. Patient Safety, 2, pp. 16-27. [DOI:10.33940/data/2020.6.3]
Veazie, S, Peterson, K. & Bourne, D., 2019. Evidence brief: Implementation of high reliability organization principles. Washington (DC): Department of Veterans Affairs. [Link]
Type of Study: Research |
Subject:
Special
Received: 2023/11/6 | Accepted: 2024/01/6 | Published: 2024/08/1
Received: 2023/11/6 | Accepted: 2024/01/6 | Published: 2024/08/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






