Sat, Feb 21, 2026
[Archive]
Volume 10, Issue 4 (Autumn 2024)
JCCNC 2024, 10(4): 249-262 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Temple T A, Uthman T J, Idehen E E, Ahmed Karatu B. Examining the Moderating Role of Self-Compassion in the Relationship Between Psychache, Compassion Fatigue, and General Well-Being among Nurses in the Aftermath of COVID-19. JCCNC 2024; 10 (4) :249-262
URL: http://jccnc.iums.ac.ir/article-1-555-en.html
URL: http://jccnc.iums.ac.ir/article-1-555-en.html
Tamuno-Opubo Addah Temple *1 

 , Tinuoye Jamiu Uthman2
, Tinuoye Jamiu Uthman2 

 , Egbewuare Emmanuel Idehen2
, Egbewuare Emmanuel Idehen2 

 , Baba Ahmed Karatu3
, Baba Ahmed Karatu3 




 , Tinuoye Jamiu Uthman2
, Tinuoye Jamiu Uthman2 

 , Egbewuare Emmanuel Idehen2
, Egbewuare Emmanuel Idehen2 

 , Baba Ahmed Karatu3
, Baba Ahmed Karatu3 


1- Department of Psychology, Olabisi Onabanjo University, Ago-Iwoye, Nigeria. , addahson5@gmail.com
2- Department of Psychology, Obafemi Awolowo University, Ile-Ife, Nigeria.
3- Department of Psychology, Federal University of Gashua, Gashua, Nigeria.
2- Department of Psychology, Obafemi Awolowo University, Ile-Ife, Nigeria.
3- Department of Psychology, Federal University of Gashua, Gashua, Nigeria.
Full-Text [PDF 758 kb]
(1081 Downloads)
| Abstract (HTML) (2347 Views)
Full-Text: (481 Views)
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) pandemic, the most significant health disaster of the 21st century, has brought about numerous challenges, affecting all aspects of society. Healthcare personnel, especially nurses, who have been in charge of fighting this pandemic, are among those most severely impacted. Their already tricky work has been made more challenging by the unrelenting increase in COVID-19 cases, frequently pushing their emotional and physical limits. The effects of the pandemic on nurses’ psychological wellbeing are examined in this study. We focused on the concepts of “psychache,” which denotes extreme emotional suffering, and “compassion fatigue,” which describes the gradual loss of compassion over time, often as a result of prolonged exposure to traumatic events. These two concepts not only substantially affect people’s overall wellbeing but may also have a detrimental effect on nurses’ capacity to serve patients with the utmost care and their mental health. However, despite many challenges, some innate characteristics may offer resilience to these harmful psychological impacts. One such element is “self-compassion,” which may lessen the detrimental impacts of psychache and compassion fatigue on the overall wellbeing of nurses.
Psychological or general wellbeing combines positive affective states and effective functioning. Accordingly, this state includes some resources like physical (good work environment, job satisfaction, and positive affectivity), social (workplace-family conflict, social support), and psychological (sadness, depression, anxiety, mood disorders, or symptoms of post-traumatic stress) resources (Dodge et al., 2012; Rezai et al., 2020). Nurses, constituting the backbone of patient care, have faced intense physical and psychological challenges during and after COVID-19. The general wellbeing of nurses is not only crucial for optimal patient care but also for their personal and professional sustenance. Prior research has consistently shown that nurses’ wellbeing is closely related to the quality of care they deliver and their intention to remain in the profession (Aiken et al., 2002). Studies during (Cordova et al., 2020; Hurley et al., 2020) and after (Ericsson et al., 2022; Kohnen et al., 2023) the pandemic hold similar intense notions, hence necessitating the study on the nursing profession.
Nurses frequently experience the intense physical and emotional distress of their patients due to their exposure to suffering, trauma, and human issues. Before COVID-19, some studies (Wicks, 2005; Nolte et al., 2017) indicated that the nursing profession, known for its inherent demands, requires clinical and technical skills and deep wells of compassion and emotional resilience. However, the ravaging COVID-19 exposed nurses to psychological conditions that may threaten their general wellbeing. Si et al. (2020) assessed the psychological conditions of frontline nurses during the COVID-19 pandemic in China. They reported that 13.6% of those surveyed had depression, 13.9% had anxiety, 8.6% had stress, and 40.2% had post-traumatic stress disorder. Nevertheless, another way to think about general or mental wellbeing in nurses is as an internal and external component influenced by several psychological elements such as psychache, compassion fatigue, and self-compassion.
A critical yet understudied facet in the context of healthcare is “psychache”—the profound emotional pain stemming from perceived thwarted psychological needs (Shneidman, 1993). Psychache was Shneidman’s concept to explain suicide and its underlying cause. The original meaning of the word psyche is soul, so psychache means aching soul or soul in pain. According to Micheal (2011), psychache stems from thwarted or distorted psychological needs. Research has indicated a noteworthy inverse correlation between psychache and an individual’s general wellbeing (Mills et al., 2005; Troister & Holden, 2012; Tanrıverdi et al., 2024). Although healthcare professionals across all specialties perceive the healthcare sector as particularly taxing and stressful, notwithstanding, in the course of an epidemic, nurses make up the majority of the medical staff and carry out the majority of the tasks related to controlling infectious diseases. Carleton et al. (2018) acknowledged that nurses frequently deal with a heavy workload, workplace violence, burnout/compassion fatigue, and exposure to potentially psychologically traumatic events. These factors have all been scientifically linked to an increase in the symptoms of mental illnesses, such as psychache (Sun et al., 2020). For nurses, given their close encounters with suffering, death, and the fragility of life, understanding the effects of psychache becomes imperative.
Nurses frequently experience compassion fatigue, characterized by physical and emotional exhaustion after prolonged exposure to patients’ suffering or tragic events. This condition is especially true during emergencies such as the COVID-19 epidemic. Compassion fatigue was first described by Joinson (1992) and refers to a weakened state of compassion brought on by the weariness of persistently interacting with the suffering of others. According to the Royal College of Nursing (2019), this syndrome affects healthcare workers in various fields and is marked by diminished interpersonal interactions, emotional exhaustion, impaired psychological functions, and physiological disturbances. In addition to their direct involvement in patient care, nurses are especially vulnerable to compassion fatigue in their caregiving roles. This condition can result in feelings of helplessness, guilt, or distress when they are unable to prevent patients’ health conditions from worsening or dying (Yoder, 2010). Empirical research, including that conducted by Kolthoff and Hickman (2017) among geriatric unit nurses and Patel (2018) among mental health professionals, highlights the widespread occurrence of compassion fatigue and its correlation with unfavorable health consequences such as obesity, sleep disorders, decreased physical activity, and symptoms of stress such as anxiety, insomnia, and avoidance behaviors. These results underline the importance of treating compassion fatigue to protect nurses’ general health and ability to deliver high-quality care.
Self-compassion could be a protective factor against challenges like psychache and compassion fatigue. Self-compassion is feeling and being open to one’s sorrow, not running away from it or distancing oneself from it, and feeling the need to heal and lessen one’s suffering lovingly. According to Neff (2003), it promotes resilience by providing a calm, non-judgmental acceptance of one’s suffering as a natural part of life. The significance of being aware of and empathetic towards one’s pain is emphasized by this idea, which has been associated with numerous positive psychological effects, such as decreased psychological symptoms, improved psychological wellbeing, emotional intelligence, wisdom, contentment with life, and social connectedness (Rowe et al., 2013; Raab, 2014; Beasley, 2021; Alabi et al., 2023). Practicing self-compassion might lessen the adverse effects of compassion fatigue and improve interpersonal functioning and mental health by reducing rumination (Chinweuba et al., 2023), avoidance (Alquwez et al., 2021), and suppression of unwanted thoughts and feelings (Aliado, 2022) and emotional validating abilities (Oginyi et al., 2022). Further empirical data supports the idea that practicing self-compassion enhances psychological health, reduces psychological distress, and fortifies empathy, perspective-taking, and forgiveness (Neff & Pommier, 2013; Stapleton et al., 2018; du Plessis et al., 2023; Obi et al., 2023). Research conducted in nursing settings, including studies by Durkin et al. (2016), Dev et al. (2020), and Akanni et al. (2023), highlights the connection between self-compassion and higher levels of compassion satisfaction, enhanced quality of life, and reduced burnout for healthcare workers. These findings emphasize self-compassion’s critical role in protecting against work-related stress and promoting general wellbeing in demanding care environments.
Traditionally, nursing has been a female-dominated profession (Wynn et al., 2023). While this has begun to shift, arguably, gender norms and stereotypes still play a significant role in how nurses experience their work. According to Andina-Diaz et al. (2023), women are traditionally expected to be caregivers, and this societal norm might make them more vulnerable to compassion fatigue. Additionally, women are often socialized to prioritize others’ needs over their own, possibly leading to reduced self-compassion (Jessome, 2023). Male nurses, on the other hand, might face societal stigma for choosing a female-dominated profession (Yokoya et al., 2023). This condition could result in increased psychache due to the tension of breaking traditional gender roles. They might also be less encouraged to express vulnerability, making it more challenging to seek support; hence, the rationale for this study is also to examine gender differences in general wellbeing among nurses.
Examining the complex relationship between psychache, compassion fatigue, and self-compassion among nurses at the Obafemi Awolowo University Teaching Hospital Complex (OAUTHC) in the stressful environment following COVID-19 is crucial when considering the self-compassion theory. This theoretical perspective suggests that self-compassion, which includes self-kindness, common humanity, and mindfulness, may protect nurses from the negative impacts of psychache and compassion fatigue, thereby preserving their wellbeing. The research aims to provide practical insights that might guide the creation of specific treatments and support systems for frontline healthcare personnel by clarifying these dynamics. Comprehending the significance of self-compassion improves our understanding of the elements affecting nurses’ health. It boosts the resilience of the healthcare system, assuring the wellbeing of carers and the quality of patient care.
The study’s general objective was to examine the moderating role of self-compassion in the relationship between psychache, compassionate fatigue, and the general wellbeing of nurses during COVID-19.
In this regard, the following hypotheses would be examined:
Self-compassion will significantly moderate the relationship between psychache and the general wellbeing of nurses in the aftermath of COVID-19.
Self-compassion will significantly moderate the relationship between compassion fatigue and the general wellbeing of nurses in the aftermath of COVID-19.
There will be gender differences in general wellbeing among nurses.
Materials and Methods
A cross-sectional correlational design was used for this investigation. The study population comprised nurses at OAUTHC across various departments. Based on preliminary inquiry, the total number of nurses at OAUTHC was 1438 during COVID-19. Considering the pandemic, Yamane’s (1967) formula was used to decide the sample frame, including 20% attrition. All nurses who had at least one year of nursing experience and had been working during the pandemic and agreed to participate in the study were eligible. The sample size was estimated at three hundred and sixty (376). Using convenience sampling, the questionnaires were distributed among eligible nurses. As a result, 554 nurses from different departments (Emergency, Clinical Services, Community Health, Dental, Dietetics, Dermatology, Environmental Health, Mental Health, Anesthesia, Pediatrics, Surgery, Outpatient, Inpatient, Medical, And Radiology) completed them, which was more than we expected. This adjustment ensured that the sample size remained robust despite unforeseen circumstances affecting participation. Additionally, the response rate exceeded the expected sample frame, indicating higher interest and engagement among the nurses surveyed. This higher response rate suggests that the study findings are more likely to accurately reflect the psychache, compassion fatigue, and general wellbeing of nurses within the hospital setting.
Study instruments
General wellbeing was assessed using the scales of psychological wellbeing (SPWB), developed by Ryff (1995). The SPWB is a well-structured self-report instrument based on the six psychological wellbeing dimensions. The scale includes three items for each of the six aspects of wellbeing: Self-acceptance, autonomy, environmental mastery, purpose in life, positive relations with others, and personal growth. Some items on the scale are: “I tend to be influenced by people with strong opinions” and “I am quite good at managing the many responsibilities of my daily life.” Each item is responded to on a 7-point Likert-type scale: 1=strongly agree; 2=somewhat agree; 3=a little agree; 4=neither agree nor disagree; 5=a little disagree; 6=somewhat disagree; 7=strongly disagree. Items 1, 5, 9, 10,12, 13, 15, 18 are reversely scored.
The total score is obtained by summarising the item ratings across all 18 items. The study used this scoring scheme: The higher the respondent’s overall scores, the better their psychological wellbeing. According to Ryff (1989), the internal consistency reliability coefficients of six subscales range from 0.86 to 0.93. Mefoh et al. (2016) employed 71 inmates from the Nigerian prison Nsukka to revalidate this scale. The pilot study’s reliability analysis yielded Cronbach α values of 0.72 for self-acceptance, 0.50 for positive relations, 0.46 for autonomy, 0.60 for environmental mastery, 0.62 for purpose in life, and 0.57 for personal growth. The reliability coefficient of the composite variables was calculated as 0.87. In Nigeria, the reliability coefficient for the whole scale was calculated as 0.63 among undergraduate students (Onyedibe et al., 2015). The current study found a reliability coefficient of 0.68 among nurses.
Psychache was assessed using the psychache scale (PAS) developed by Holden et al. (2001). Based on Shneidman’s (1993) definition of psychache, it is a persistent, free-floating, non-situation-specific psychological pain brought on by the unfulfilled requirements of one’s essential organs. The 13-item PAS is a self-report tool and evaluates psychological pain at the moment. Every response is scored using a 5-point Likert scale, with ‘1’ denoting strongly disagree and ‘5’ denoting strongly agree. Respondents are asked to rate how frequently they experience each of the first nine elements on the scale. In contrast, the final four items request confirmation of the degree to which each responder agrees or disagrees with the experience being recounted.
In this instance, the total score is obtained by summarising the item ratings across all 13 items, and the scoring scheme was used for this study. A score below the norm denotes the absence of psychache, whereas a score equal to or over the standard implies the presence of psychache. Previous studies have established the psychometric features of the psychache scale, indicating good validity and great scale reliability (Holden et al., 2001; Mills et al., 2005). The Cronbach α reliability among widows in Imo state, Nigeria, was found to be 0.88, with a norm of 36.87 (n=71) (Sydney-Agbor, 2021). The reliability coefficient was calculated as 0.78 among nurses in our study.
Compassion fatigue was assessed using the compassion fatigue scale (CFS). Several earlier research studies have employed variants of the scale that Figley (1995) created based on clinical experience. Russ et al. (2009) ultimately changed and shortened the scale. The 13-item CFS is divided into two domains: A secondary trauma subscale with five items and an 8-item burnout subscale. Respondents are asked to rate how often each item pertains to them on a 10-point Likert scale ranging from 1 (rarely/never) to 10 (very often). Adams et al. (2006) stated that the Cronbach α coefficients of sub-dimensions vary from 0.80 to 0.90 and show acceptable internal reliability. The scale’s possible scores fall between 13 and 130, and as a score rises, so does the degree of compassion fatigue. This study found a 0.77 reliability coefficient among nurses using the same scoring scheme.
Self-compassion was assessed using the self-compassion scale-short form (SCS-SF) developed by Raes et al. (2011). The SCS-SF is a 12-item self-report measure designed to determine self-compassion and is composed of 6 subscales: Self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification. The responses to each item are rated on a 5-point Likert scale (0=almost never to 5=Almost always) to record how often individuals behave kindly and caringly towards themselves in difficult life situations.
No clinical standards or ratings categorize people according to their level of self-compassion. Nevertheless, ratings are primarily utilized compared to the results for those with higher or lower self-compassion ratings. However, using ad hoc criteria, scores between 1.0 and 2.49 are classified as low, 2.5 and 3.5 as moderate, and 3.51 and 5.0 as high. This scoring scheme was used in this investigation. According to Garcia-Campayo et al. (2014), the SCS-SF showed good internal consistency (Cronbach α≥0.86 in all samples) and an almost perfect correlation with the long-form SCS (r≥0.97 in all samples). When examining overall self-compassion scores, the SCS-SF is a valid substitute for the long-form SCS (Babenko & Guo, 2019). Ogueji (2021) found a reliability coefficient of 0.75 among pregnant HIV-positive women in Nigeria. The current study found a reliability coefficient of 0.85 among the nurses.
Study procedure
A computer-assisted personal interview (CAPI) facilitated the participants’ answers. The rationale was to ensure mobile responsiveness and that nurses could easily access it with their mobile devices. SurveyCTO and Kobo toolbox were used to achieve this. The link to the survey was distributed to nurses, their WhatsApp platforms, and emails. The link contained assurances of the data’s confidentiality and clear instructions for completing the survey. Nurses used CAPI to respond to questions on the scales, and their answers were immediately recorded and kept on secure servers. Additionally, it enabled the nurses to pause the survey and pick up where they left off later. A helpline or support email was set up in case of any technical problems, and frequent reminders were sent to individuals who had not yet completed the survey to encourage maximum participation. The process took about 5 months, from November 2022 to March 2023.
Data analysis
Data collected in the study were analyzed using both descriptive and inferential statistics. Descriptive statistics was used to determine the frequency of psychache, compassion fatigue, self-compassion, and general wellbeing. On the other hand, inferential statistics such as Hayes PROCESS macro model 1, zero-order correlation, and t-test were used to examine the hypotheses. The analyses were carried out with sub-programs (Thomas Haye plugin) of the IBM/SPSS software, version 230.
Results
Of 544 respondents, 410(75.4%) were women, and 144(26.5%) were men, reflecting a higher proportion of female nurses in the cohort. The Mean±SD age of nurses was 35±7.12 years, indicating a middle-aged workforce with a moderate age spread. The majority of nurses followed Christianity (313, 57.5%), then Islam (203, 37.2%), with a smaller number adhering to traditional beliefs (27, 5.0%) or uncertain beliefs (11, 0.2%). Nurses worked across various departments, with the highest numbers in surgery with 61(11.2%), outpatient with 46(8.5%), and medical with 41(7.5%) units. The remaining 72.8% were distributed across other specialized units. This distribution shows diverse specialties and service areas within the nursing cohort. Many nurses, 231(42.5%), had 1-3 years of service, suggesting a considerable influx of newer professionals into the nursing field. Those with 4-6 years (146, 26.8%) and 7-9 years (113, 20.8%) of service represent mid-career nurses, while 64 nurses (9.9%) had a decade or more of experience, indicating a seasoned group of practitioners.
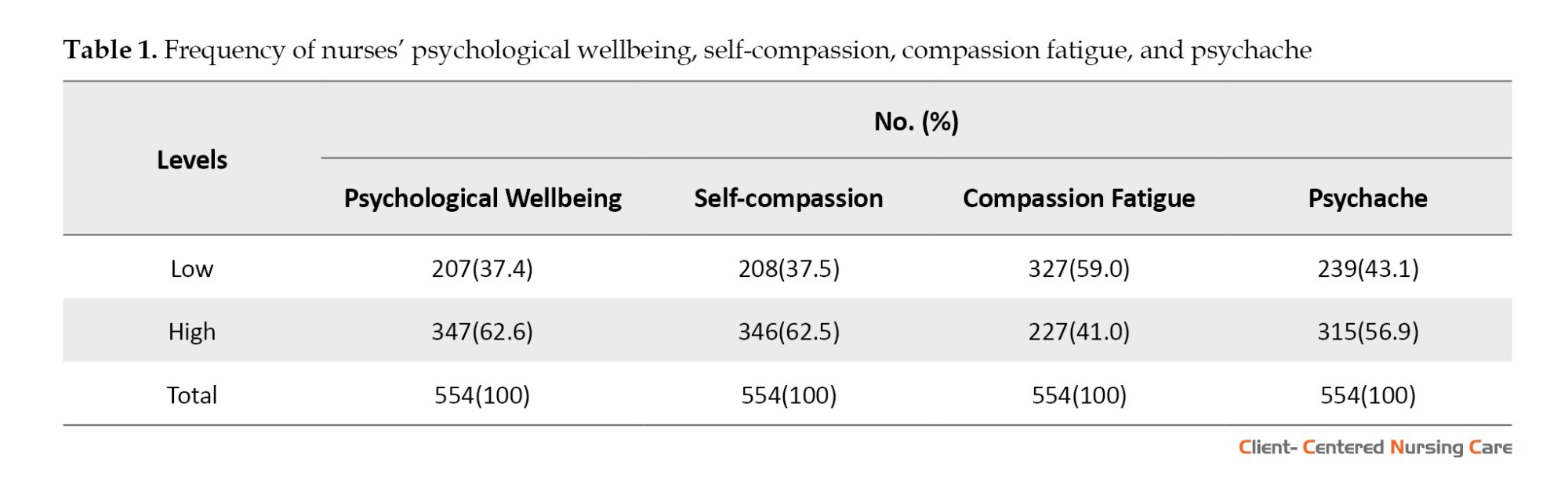
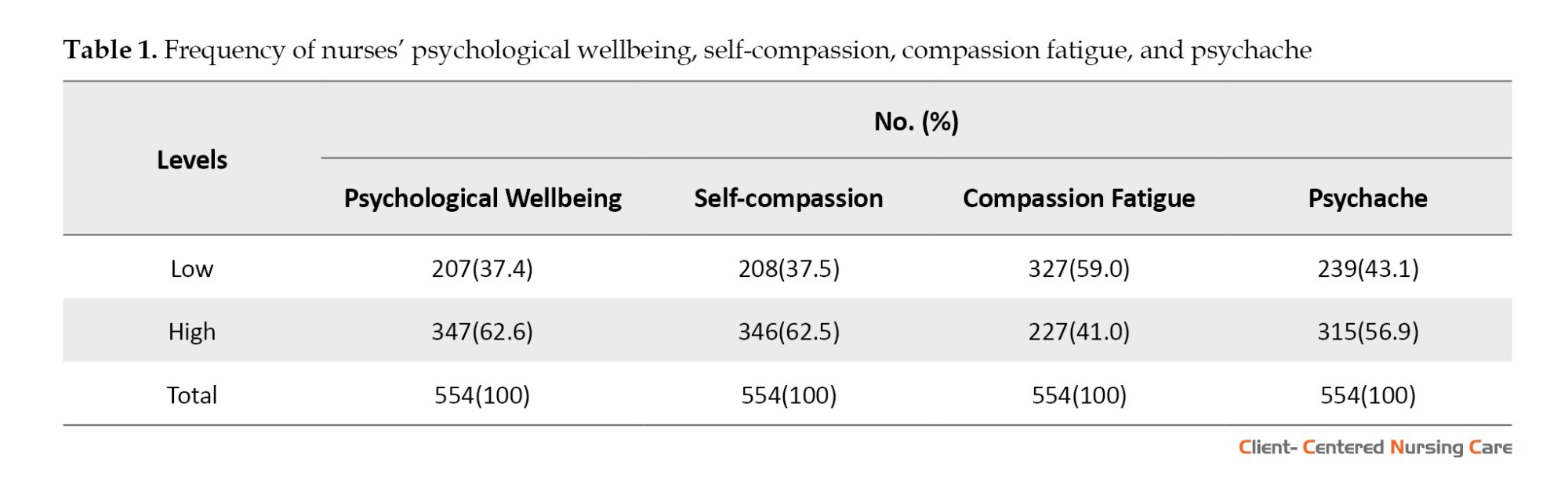
Frequency of the study variables
This aspect of the study provides the frequency of self-compassion, psychache, compassion fatigue, and psychological wellbeing of nurses in the study setting. The mean values (39.1, 43.01, 19.17, and 48.65, respectively) were used to categorize the low and high categories. Scores below the mean were classified as low, while scores above the mean were labeled as high. Table 1 presents the outcome of the analysis.
Relationships among the study variables
The correlation coefficients between the studied variables are presented in Table 2.
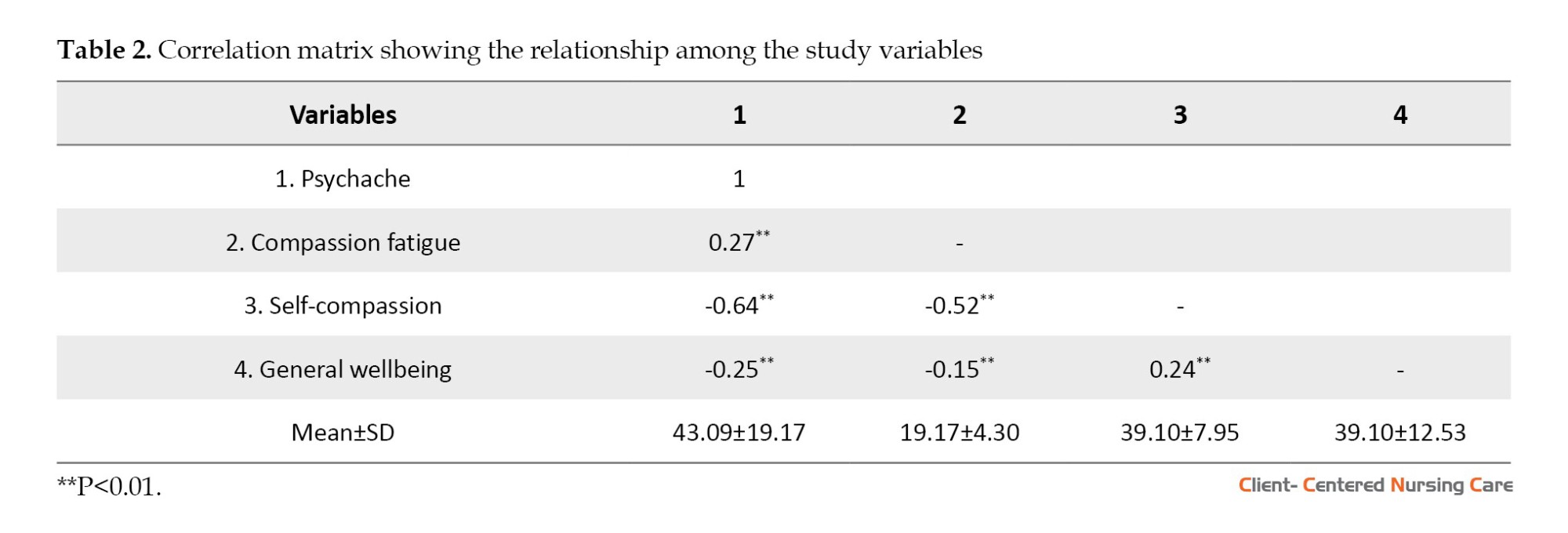
The result is a significant negative relationship between psychache and general wellbeing (r552=-0.25, P<0.01). This finding implies that nurses who reported high psychache tend to have increased negative or lower general wellbeing. Compassion fatigue and general wellbeing also had a significant negative relationship (r552=-0.15, P<0.01). This finding also implies that nurses who experience a high level of compassion fatigue tend to have low general wellbeing. Finally, a significant positive relationship was also between self-compassion and general wellbeing (r552=0.24, P<0.05). This finding means that nurses who reported high self-compassion tend to have high general wellbeing.
Hypothesis one
Self-compassion will significantly moderate the relationship between psychache and the general wellbeing of the nurses in the aftermath of the pandemic.
According to Table 3, a statistically significant direct effect of psychache (β=2.467, SE=0.115, P<0.001) and self-compassion (β=2.945, SE=0.143, P<0.001) on general wellbeing. Both psychache and self-compassion jointly explained a 30% variance in the general wellbeing of the nurses.
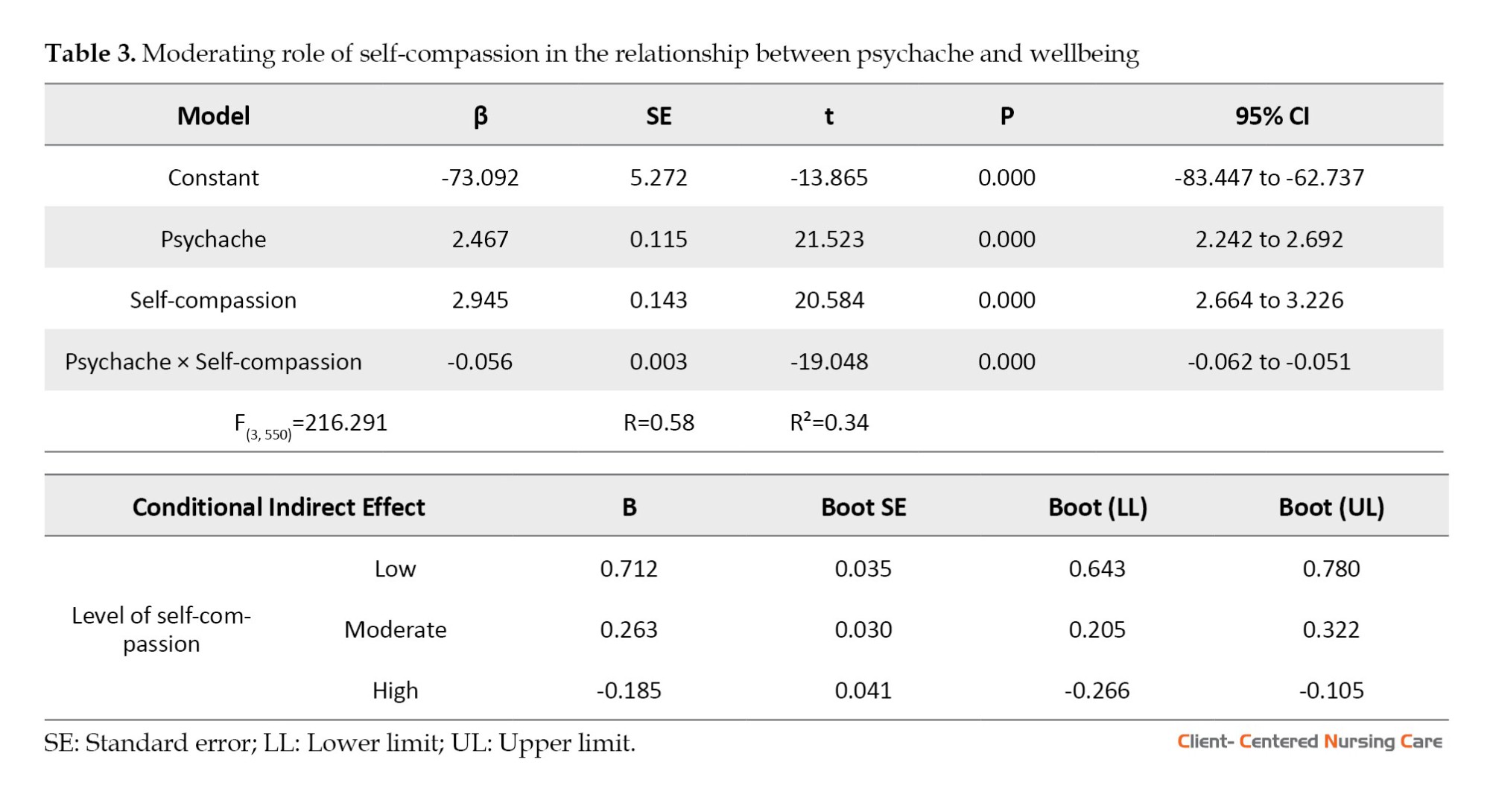
Self-compassion significantly moderated the relationship between psychache and general wellbeing (β=0.03; SE=0.01; 95% CI, -0.07%, -0.00%), where higher self-compassion levels weakened the negative impact of psychache on wellbeing. The direction of the moderating effect is also graphically presented in Figure 1.
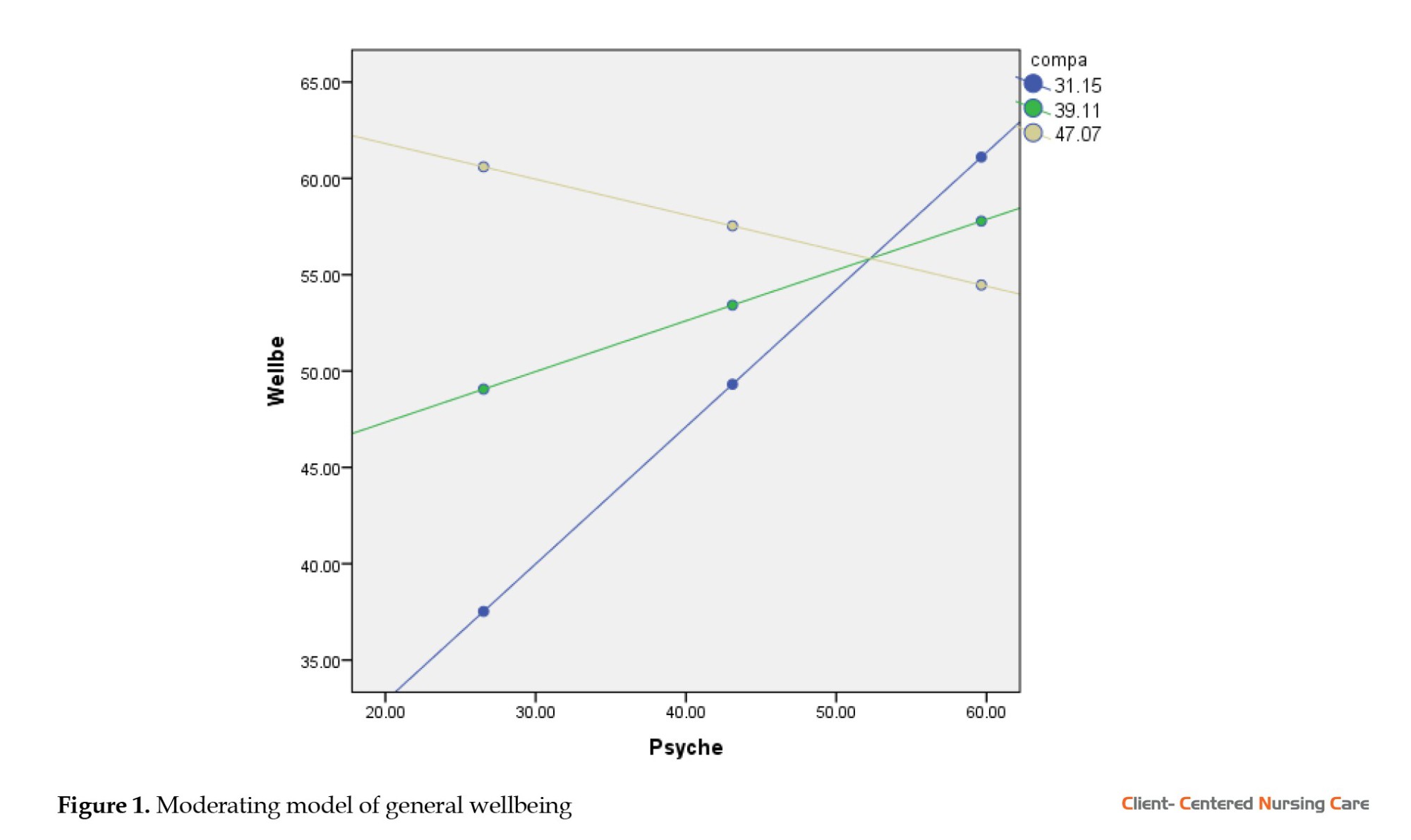
The blue line on the graph implies low self-compassion, the green line means moderate self-compassion, and the light yellow line means high self-compassion. It, therefore, implies that self-compassion strengthens the negative relationship between psychache and general wellbeing, with this relationship much stronger among nurses with lower levels of self-compassion than those with moderate and high self-compassion levels. Further observation suggests that the conditional indirect effect of psychache on general wellbeing through self-compassion is significantly much stronger among nurses with a lower level of self-compassion (B=0.712; 95% CI, 0.643%, 0.780%) than those with moderate (B=0.263; 95% CI, 0.205%, 0.322%) and high self-compassion (B=-0.185; 95% CI, -0.266%, -0.105%).
Hypothesis two
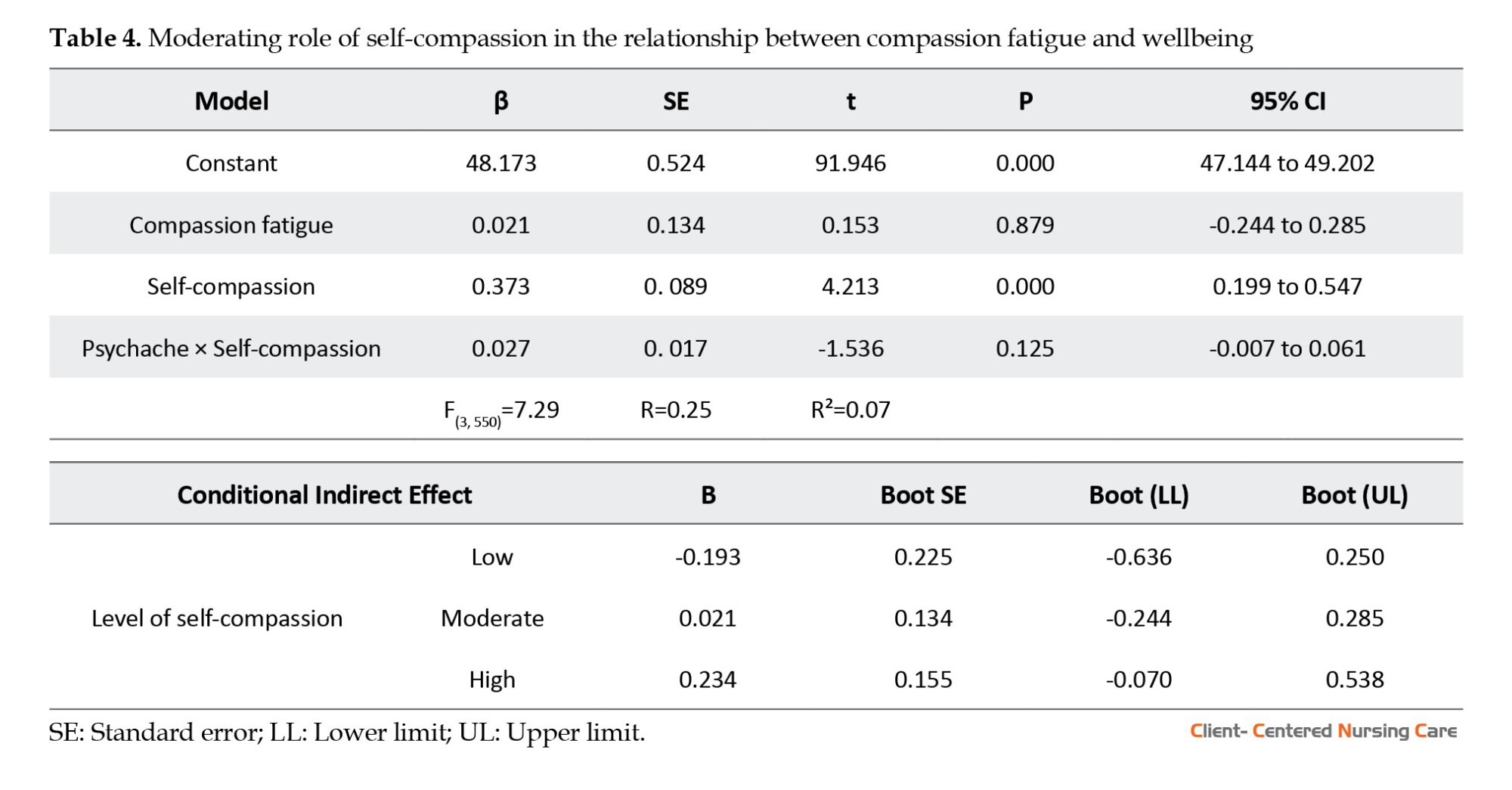
Self-compassion will significantly moderate the relationship between compassion fatigue and the general wellbeing of the nurses in the aftermath of the pandemic.
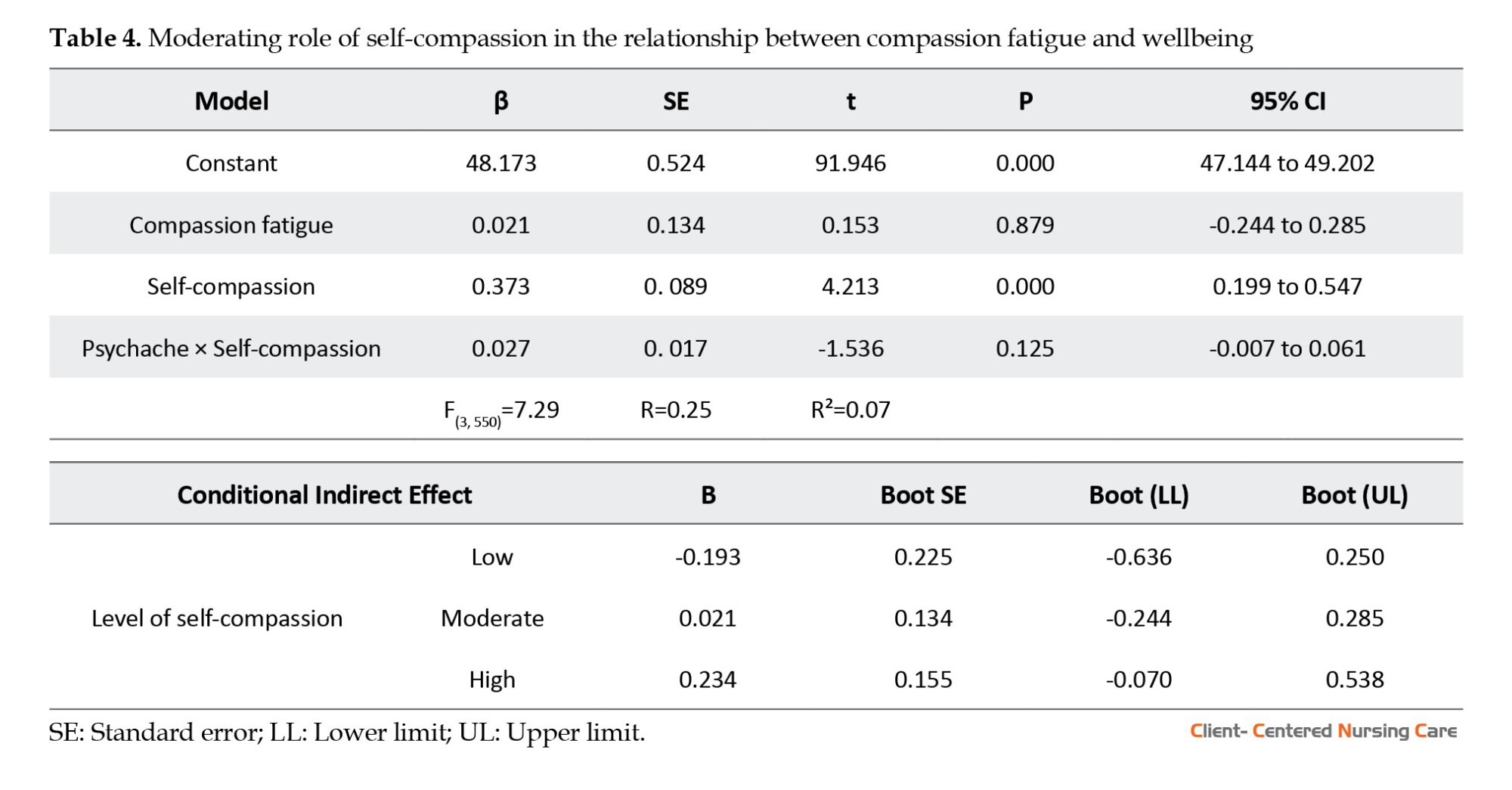
Table 4 reveals that compassion fatigue (β=0.021; SE=0.134; P=0.879) did not predict general wellbeing among nurses. There was a statistically significant direct effect of self-compassion on general wellbeing (β=0.373; SE=0.089; P<0.001), which suggests the independent predicting role of self-compassion on general wellbeing. Compassion fatigue and self-compassion jointly explained a 7% variation in the general wellbeing of the nurses. The result also found that self-compassion did not significantly moderate the impact of compassion fatigue on wellbeing (β=0.027; SE=0.017; 95% CI, -0.007%, 0.061%), suggesting that self-compassion might be less effective in contexts of chronic emotional exhaustion compared to acute psychological distress.
Hypothesis three
There will be gender differences in general wellbeing among the nurses.
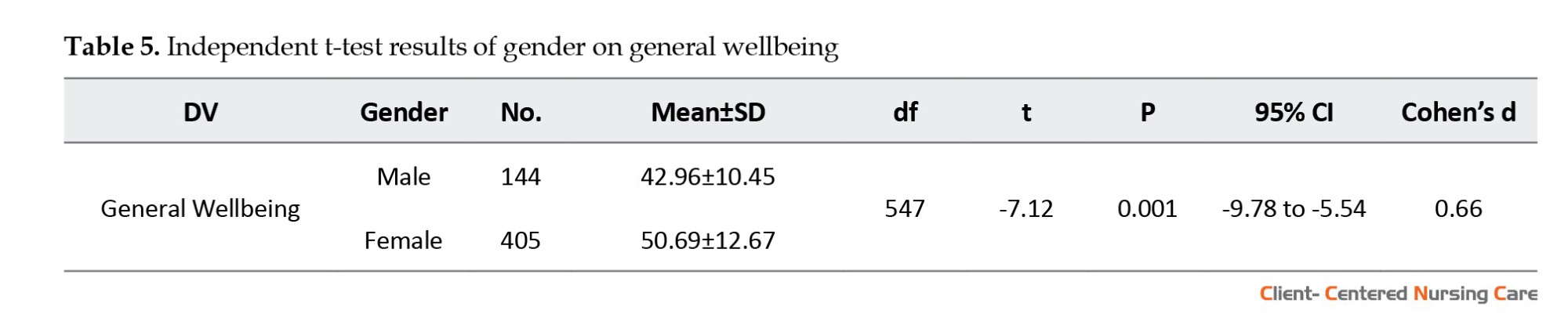
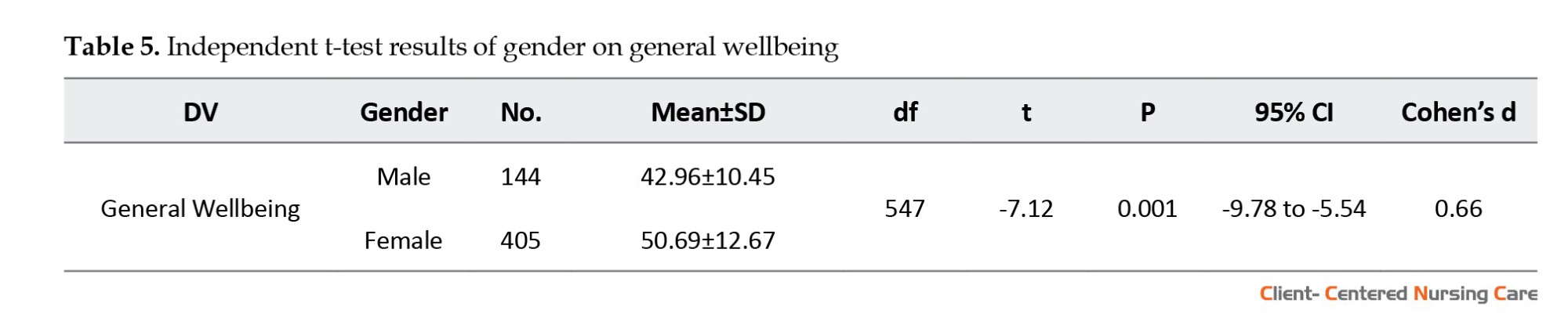
According to Table 5, there is a significant difference in the scores of general wellbeing between male (Mean±SD 42.96±10.45) and female nurses (Mean±SD 50.69±12.67), with female nurses reporting higher wellbeing (t547=-7.12; P<0.001; 95% CI, -9.78%, -5.54%). This means that females significantly scored higher on general wellbeing than their male counterparts with a medium effect size, as shown by Cohen’s d value of 0.66.
Discussion
This research aimed to determine the prevalence of psychache, compassion fatigue, self-compassion, and general wellbeing of nurses at Obafemi Awolowo University Teaching Hospital Complex (OAUTHC) in the aftermath of the pandemic. Moreover, the study further intended to evaluate the moderating role of self-compassion in the relationship between psychache and compassion fatigue on the general wellbeing of the nurses. The findings of the study imply that a notable portion of the nurses have low psychological wellbeing, suggesting that many may be grappling with mental or emotional challenges in the aftermath of the pandemic. In contrast, a majority reported adequate psychological wellbeing above the average. This status is encouraging, but it also emphasizes the contrast and disparity among the nurses. The research also highlights the critical role of self-compassion, with many nurses manifesting high self-compassion, indicating potential disparity struggles in treating themselves with kindness and understanding during challenging times. Furthermore, compassion fatigue, a phenomenon common among healthcare professionals due to the emotional strain of caring for patients, is evident in this study. Many nurses faced high levels of compassion fatigue, pointing to the need for interventions that address this specific form of burnout. Lastly, the concept of psychache, which pertains to profound emotional pain and distress, was also examined. Many nurses reported experiencing high levels of psychache, underlining the depth of emotional distress they might be undergoing. These findings underscore the complexity of nurses’ challenges, especially during a global crisis. Healthcare institutions must recognize these issues and implement strategies to support and bolster the wellbeing of their frontline workers.
The results of this study show a statistically significant inverse association between the nurses’ overall wellbeing and psychache. This result suggests that psychological wellbeing decreases with increasing psychache. This result supports Michael’s (2011) claim that psychological wellbeing is skewed by pain owing to unmet needs. However, the positive relationships that self-compassion has with life satisfaction and psychological wellbeing are consistent with research by Neff et al. (2007, 2007b), Neely et al. (2009), Raes (2010), Johnson and O’Brien (2013), and Odou and Brinker (2014). The study’s findings also show that self-compassion moderates the association between psychological wellbeing and psychache, which may explain why it has a positive relationship with psychological wellbeing. The descriptive analysis clearly shows that most nurses have high levels of self-compassion, indicating the role of self-compassion in the connection between psychological wellbeing and psychache. This finding implies that elevated levels of self-compassion could function as a safeguard or buffer, potentially mitigating the deleterious impacts of psychache on general wellbeing. Dev et al. (2020) also put forth the idea, highlighting the correlation between strong self-compassion, improved quality of life, and decreased burnout.
Interestingly, there is no moderating effect between general wellbeing and compassion fatigue when self-compassion is present. This distinction highlights the complex function of self-compassion and its fluctuating impacts on various psychological stressors. In addition, the study findings indicate a negative relationship between compassion fatigue and psychological wellbeing, which is commensurate with existing studies like Yoder, (2010), Kolthoff and Hickman (2017), and Ricciardelli et al. (2018), which suggests that compassion fatigue exposes nurses to trauma which is detrimental to their psychological wellbeing.
This study found a gender gap in general wellbeing scores. Overall, women scored higher on general wellbeing than men. With a medium effect size, this statistically significant difference suggests gender-related differences in coping mechanisms, resilience, nursing experiences, and expectancies. Nurses’ gender differences in general wellbeing are significant. Female nurses have higher general wellbeing scores than male nurses, suggesting they use better or more diverse coping mechanisms in stressful situations. Social conditioning encourages women to express emotions and seek support, which may improve emotional processing.
Another possibility is that female nurses are more resilient to adversity. According to Canal-Rivero et al. (2023), personal experiences, professional training, and social support systems that are more accessible to female nurses may contribute to their resilience. Male and female nurses may have different job experiences. These differences could involve patient contacts, peer relationships, or administrative dynamics. Such differences may affect their health differently. The nursing profession, traditionally female (Adekoya, 2023), may have gender-based expectations and standards. Male nurses may encounter specific problems or pressures that affect their wellbeing scores due to their minority status. Given this gender gap, healthcare organizations should consider gender-sensitive support. Recognizing that male and female nurses may have different needs or obstacles can improve solutions. This research emphasizes the necessity for a diversified approach to nursing wellbeing that considers gender disparities.
The findings from this study accentuate the profound psychological challenges nurses face in OAUTHC after the COVID-19 pandemic. Health institutions must recognize and address these issues, considering the critical role of nurses in healthcare delivery. Interventions focusing on enhancing self-compassion could be instrumental, given its protective role. Moreover, understanding gender-specific needs and challenges can lead to more tailored and effective wellness programs.
When planning measures to ensure the health of nurses working at OAUTHC following COVID-19, it is essential to take gender inequalities into account. More effective wellness programs for nurses can be achieved by considering gender-specific requirements and using treatments that promote self-compassion.
Conclusion
The research delved into the psychological wellbeing of nurses at OAUTHC, revealing complex dynamics around psychache, compassion fatigue, self-compassion, and general mental health. While some nurses reported low wellbeing, the majority showed satisfactory mental health levels, highlighting the diversity of experiences within the nursing community during the crisis. Self-compassion emerged as a crucial factor, potentially buffering against mental distress, although its effects vary between psychache and compassion fatigue. Additionally, a gender-based disparity in wellbeing was observed, suggesting the need for tailored support mechanisms. Overall, the study underscores the importance of comprehensive interventions to support nurses’ mental wellbeing, including counseling, self-compassion workshops, gender-sensitive support groups, and strategies to address compassion fatigue.
The study, though insightful, has limitations: Its quantitative focus may overlook nuanced narratives, its localized scope raises concerns about generalisability, and its cross-sectional design may not capture evolving dynamics. Additionally, the limited sample size may not fully represent diverse backgrounds, warranting cautious interpretation of findings.
Future research can address limitations by combining quantitative and qualitative methods, expanding beyond OAUTHC to capture regional differences, adopting a longitudinal design to track wellbeing dynamics, and diversifying data collection techniques. Observational methods and diverse participant pools can offer multifaceted insights while exploring additional variables like workload intensity and gender-specific experiences can enrich understanding. These efforts aim to comprehensively address nurses’ experiences and challenges, ensuring more effective support strategies.
Ethical Considerations
Compliance with ethical guidelines
This study followed ethical requirements to protect and care for participants. All participants were told of the study’s goal and its ramifications before it began. Each participant gave informed consent, knowing their rights, including the ability to leave the study without penalty. Confidentiality and anonymity were strictly preserved to protect participant data and responses. The ethical approval under protocol number FSS/OAU/RREC/0299 shows that the research team upheld the highest ethical standards, ensuring that the study was conducted with integrity, respect for human dignity, and by international ethical guidelines for human subject research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Tamuno-opubo Addah Temple; Data collection and analysis: Uthman Jamiu Tinuoye; Writing: Idehen Egbewuare Emmanuel and Baba Ahmed Karatu; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are indeed grateful to these persons and groups, in no particular order: The Nursing Department of the OAUTHC, students of the School of Health Information Management, Obafemi Awolowo University Teaching Hospital Complex (OAUTHC), the Mental Health Support Initiative (MHSI-OAU) and the Psychcare Humaniterex Foundation, Aladanla, Ile-Ife, Osun State.
References
The severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) pandemic, the most significant health disaster of the 21st century, has brought about numerous challenges, affecting all aspects of society. Healthcare personnel, especially nurses, who have been in charge of fighting this pandemic, are among those most severely impacted. Their already tricky work has been made more challenging by the unrelenting increase in COVID-19 cases, frequently pushing their emotional and physical limits. The effects of the pandemic on nurses’ psychological wellbeing are examined in this study. We focused on the concepts of “psychache,” which denotes extreme emotional suffering, and “compassion fatigue,” which describes the gradual loss of compassion over time, often as a result of prolonged exposure to traumatic events. These two concepts not only substantially affect people’s overall wellbeing but may also have a detrimental effect on nurses’ capacity to serve patients with the utmost care and their mental health. However, despite many challenges, some innate characteristics may offer resilience to these harmful psychological impacts. One such element is “self-compassion,” which may lessen the detrimental impacts of psychache and compassion fatigue on the overall wellbeing of nurses.
Psychological or general wellbeing combines positive affective states and effective functioning. Accordingly, this state includes some resources like physical (good work environment, job satisfaction, and positive affectivity), social (workplace-family conflict, social support), and psychological (sadness, depression, anxiety, mood disorders, or symptoms of post-traumatic stress) resources (Dodge et al., 2012; Rezai et al., 2020). Nurses, constituting the backbone of patient care, have faced intense physical and psychological challenges during and after COVID-19. The general wellbeing of nurses is not only crucial for optimal patient care but also for their personal and professional sustenance. Prior research has consistently shown that nurses’ wellbeing is closely related to the quality of care they deliver and their intention to remain in the profession (Aiken et al., 2002). Studies during (Cordova et al., 2020; Hurley et al., 2020) and after (Ericsson et al., 2022; Kohnen et al., 2023) the pandemic hold similar intense notions, hence necessitating the study on the nursing profession.
Nurses frequently experience the intense physical and emotional distress of their patients due to their exposure to suffering, trauma, and human issues. Before COVID-19, some studies (Wicks, 2005; Nolte et al., 2017) indicated that the nursing profession, known for its inherent demands, requires clinical and technical skills and deep wells of compassion and emotional resilience. However, the ravaging COVID-19 exposed nurses to psychological conditions that may threaten their general wellbeing. Si et al. (2020) assessed the psychological conditions of frontline nurses during the COVID-19 pandemic in China. They reported that 13.6% of those surveyed had depression, 13.9% had anxiety, 8.6% had stress, and 40.2% had post-traumatic stress disorder. Nevertheless, another way to think about general or mental wellbeing in nurses is as an internal and external component influenced by several psychological elements such as psychache, compassion fatigue, and self-compassion.
A critical yet understudied facet in the context of healthcare is “psychache”—the profound emotional pain stemming from perceived thwarted psychological needs (Shneidman, 1993). Psychache was Shneidman’s concept to explain suicide and its underlying cause. The original meaning of the word psyche is soul, so psychache means aching soul or soul in pain. According to Micheal (2011), psychache stems from thwarted or distorted psychological needs. Research has indicated a noteworthy inverse correlation between psychache and an individual’s general wellbeing (Mills et al., 2005; Troister & Holden, 2012; Tanrıverdi et al., 2024). Although healthcare professionals across all specialties perceive the healthcare sector as particularly taxing and stressful, notwithstanding, in the course of an epidemic, nurses make up the majority of the medical staff and carry out the majority of the tasks related to controlling infectious diseases. Carleton et al. (2018) acknowledged that nurses frequently deal with a heavy workload, workplace violence, burnout/compassion fatigue, and exposure to potentially psychologically traumatic events. These factors have all been scientifically linked to an increase in the symptoms of mental illnesses, such as psychache (Sun et al., 2020). For nurses, given their close encounters with suffering, death, and the fragility of life, understanding the effects of psychache becomes imperative.
Nurses frequently experience compassion fatigue, characterized by physical and emotional exhaustion after prolonged exposure to patients’ suffering or tragic events. This condition is especially true during emergencies such as the COVID-19 epidemic. Compassion fatigue was first described by Joinson (1992) and refers to a weakened state of compassion brought on by the weariness of persistently interacting with the suffering of others. According to the Royal College of Nursing (2019), this syndrome affects healthcare workers in various fields and is marked by diminished interpersonal interactions, emotional exhaustion, impaired psychological functions, and physiological disturbances. In addition to their direct involvement in patient care, nurses are especially vulnerable to compassion fatigue in their caregiving roles. This condition can result in feelings of helplessness, guilt, or distress when they are unable to prevent patients’ health conditions from worsening or dying (Yoder, 2010). Empirical research, including that conducted by Kolthoff and Hickman (2017) among geriatric unit nurses and Patel (2018) among mental health professionals, highlights the widespread occurrence of compassion fatigue and its correlation with unfavorable health consequences such as obesity, sleep disorders, decreased physical activity, and symptoms of stress such as anxiety, insomnia, and avoidance behaviors. These results underline the importance of treating compassion fatigue to protect nurses’ general health and ability to deliver high-quality care.
Self-compassion could be a protective factor against challenges like psychache and compassion fatigue. Self-compassion is feeling and being open to one’s sorrow, not running away from it or distancing oneself from it, and feeling the need to heal and lessen one’s suffering lovingly. According to Neff (2003), it promotes resilience by providing a calm, non-judgmental acceptance of one’s suffering as a natural part of life. The significance of being aware of and empathetic towards one’s pain is emphasized by this idea, which has been associated with numerous positive psychological effects, such as decreased psychological symptoms, improved psychological wellbeing, emotional intelligence, wisdom, contentment with life, and social connectedness (Rowe et al., 2013; Raab, 2014; Beasley, 2021; Alabi et al., 2023). Practicing self-compassion might lessen the adverse effects of compassion fatigue and improve interpersonal functioning and mental health by reducing rumination (Chinweuba et al., 2023), avoidance (Alquwez et al., 2021), and suppression of unwanted thoughts and feelings (Aliado, 2022) and emotional validating abilities (Oginyi et al., 2022). Further empirical data supports the idea that practicing self-compassion enhances psychological health, reduces psychological distress, and fortifies empathy, perspective-taking, and forgiveness (Neff & Pommier, 2013; Stapleton et al., 2018; du Plessis et al., 2023; Obi et al., 2023). Research conducted in nursing settings, including studies by Durkin et al. (2016), Dev et al. (2020), and Akanni et al. (2023), highlights the connection between self-compassion and higher levels of compassion satisfaction, enhanced quality of life, and reduced burnout for healthcare workers. These findings emphasize self-compassion’s critical role in protecting against work-related stress and promoting general wellbeing in demanding care environments.
Traditionally, nursing has been a female-dominated profession (Wynn et al., 2023). While this has begun to shift, arguably, gender norms and stereotypes still play a significant role in how nurses experience their work. According to Andina-Diaz et al. (2023), women are traditionally expected to be caregivers, and this societal norm might make them more vulnerable to compassion fatigue. Additionally, women are often socialized to prioritize others’ needs over their own, possibly leading to reduced self-compassion (Jessome, 2023). Male nurses, on the other hand, might face societal stigma for choosing a female-dominated profession (Yokoya et al., 2023). This condition could result in increased psychache due to the tension of breaking traditional gender roles. They might also be less encouraged to express vulnerability, making it more challenging to seek support; hence, the rationale for this study is also to examine gender differences in general wellbeing among nurses.
Examining the complex relationship between psychache, compassion fatigue, and self-compassion among nurses at the Obafemi Awolowo University Teaching Hospital Complex (OAUTHC) in the stressful environment following COVID-19 is crucial when considering the self-compassion theory. This theoretical perspective suggests that self-compassion, which includes self-kindness, common humanity, and mindfulness, may protect nurses from the negative impacts of psychache and compassion fatigue, thereby preserving their wellbeing. The research aims to provide practical insights that might guide the creation of specific treatments and support systems for frontline healthcare personnel by clarifying these dynamics. Comprehending the significance of self-compassion improves our understanding of the elements affecting nurses’ health. It boosts the resilience of the healthcare system, assuring the wellbeing of carers and the quality of patient care.
The study’s general objective was to examine the moderating role of self-compassion in the relationship between psychache, compassionate fatigue, and the general wellbeing of nurses during COVID-19.
In this regard, the following hypotheses would be examined:
Self-compassion will significantly moderate the relationship between psychache and the general wellbeing of nurses in the aftermath of COVID-19.
Self-compassion will significantly moderate the relationship between compassion fatigue and the general wellbeing of nurses in the aftermath of COVID-19.
There will be gender differences in general wellbeing among nurses.
Materials and Methods
A cross-sectional correlational design was used for this investigation. The study population comprised nurses at OAUTHC across various departments. Based on preliminary inquiry, the total number of nurses at OAUTHC was 1438 during COVID-19. Considering the pandemic, Yamane’s (1967) formula was used to decide the sample frame, including 20% attrition. All nurses who had at least one year of nursing experience and had been working during the pandemic and agreed to participate in the study were eligible. The sample size was estimated at three hundred and sixty (376). Using convenience sampling, the questionnaires were distributed among eligible nurses. As a result, 554 nurses from different departments (Emergency, Clinical Services, Community Health, Dental, Dietetics, Dermatology, Environmental Health, Mental Health, Anesthesia, Pediatrics, Surgery, Outpatient, Inpatient, Medical, And Radiology) completed them, which was more than we expected. This adjustment ensured that the sample size remained robust despite unforeseen circumstances affecting participation. Additionally, the response rate exceeded the expected sample frame, indicating higher interest and engagement among the nurses surveyed. This higher response rate suggests that the study findings are more likely to accurately reflect the psychache, compassion fatigue, and general wellbeing of nurses within the hospital setting.
Study instruments
General wellbeing was assessed using the scales of psychological wellbeing (SPWB), developed by Ryff (1995). The SPWB is a well-structured self-report instrument based on the six psychological wellbeing dimensions. The scale includes three items for each of the six aspects of wellbeing: Self-acceptance, autonomy, environmental mastery, purpose in life, positive relations with others, and personal growth. Some items on the scale are: “I tend to be influenced by people with strong opinions” and “I am quite good at managing the many responsibilities of my daily life.” Each item is responded to on a 7-point Likert-type scale: 1=strongly agree; 2=somewhat agree; 3=a little agree; 4=neither agree nor disagree; 5=a little disagree; 6=somewhat disagree; 7=strongly disagree. Items 1, 5, 9, 10,12, 13, 15, 18 are reversely scored.
The total score is obtained by summarising the item ratings across all 18 items. The study used this scoring scheme: The higher the respondent’s overall scores, the better their psychological wellbeing. According to Ryff (1989), the internal consistency reliability coefficients of six subscales range from 0.86 to 0.93. Mefoh et al. (2016) employed 71 inmates from the Nigerian prison Nsukka to revalidate this scale. The pilot study’s reliability analysis yielded Cronbach α values of 0.72 for self-acceptance, 0.50 for positive relations, 0.46 for autonomy, 0.60 for environmental mastery, 0.62 for purpose in life, and 0.57 for personal growth. The reliability coefficient of the composite variables was calculated as 0.87. In Nigeria, the reliability coefficient for the whole scale was calculated as 0.63 among undergraduate students (Onyedibe et al., 2015). The current study found a reliability coefficient of 0.68 among nurses.
Psychache was assessed using the psychache scale (PAS) developed by Holden et al. (2001). Based on Shneidman’s (1993) definition of psychache, it is a persistent, free-floating, non-situation-specific psychological pain brought on by the unfulfilled requirements of one’s essential organs. The 13-item PAS is a self-report tool and evaluates psychological pain at the moment. Every response is scored using a 5-point Likert scale, with ‘1’ denoting strongly disagree and ‘5’ denoting strongly agree. Respondents are asked to rate how frequently they experience each of the first nine elements on the scale. In contrast, the final four items request confirmation of the degree to which each responder agrees or disagrees with the experience being recounted.
In this instance, the total score is obtained by summarising the item ratings across all 13 items, and the scoring scheme was used for this study. A score below the norm denotes the absence of psychache, whereas a score equal to or over the standard implies the presence of psychache. Previous studies have established the psychometric features of the psychache scale, indicating good validity and great scale reliability (Holden et al., 2001; Mills et al., 2005). The Cronbach α reliability among widows in Imo state, Nigeria, was found to be 0.88, with a norm of 36.87 (n=71) (Sydney-Agbor, 2021). The reliability coefficient was calculated as 0.78 among nurses in our study.
Compassion fatigue was assessed using the compassion fatigue scale (CFS). Several earlier research studies have employed variants of the scale that Figley (1995) created based on clinical experience. Russ et al. (2009) ultimately changed and shortened the scale. The 13-item CFS is divided into two domains: A secondary trauma subscale with five items and an 8-item burnout subscale. Respondents are asked to rate how often each item pertains to them on a 10-point Likert scale ranging from 1 (rarely/never) to 10 (very often). Adams et al. (2006) stated that the Cronbach α coefficients of sub-dimensions vary from 0.80 to 0.90 and show acceptable internal reliability. The scale’s possible scores fall between 13 and 130, and as a score rises, so does the degree of compassion fatigue. This study found a 0.77 reliability coefficient among nurses using the same scoring scheme.
Self-compassion was assessed using the self-compassion scale-short form (SCS-SF) developed by Raes et al. (2011). The SCS-SF is a 12-item self-report measure designed to determine self-compassion and is composed of 6 subscales: Self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification. The responses to each item are rated on a 5-point Likert scale (0=almost never to 5=Almost always) to record how often individuals behave kindly and caringly towards themselves in difficult life situations.
No clinical standards or ratings categorize people according to their level of self-compassion. Nevertheless, ratings are primarily utilized compared to the results for those with higher or lower self-compassion ratings. However, using ad hoc criteria, scores between 1.0 and 2.49 are classified as low, 2.5 and 3.5 as moderate, and 3.51 and 5.0 as high. This scoring scheme was used in this investigation. According to Garcia-Campayo et al. (2014), the SCS-SF showed good internal consistency (Cronbach α≥0.86 in all samples) and an almost perfect correlation with the long-form SCS (r≥0.97 in all samples). When examining overall self-compassion scores, the SCS-SF is a valid substitute for the long-form SCS (Babenko & Guo, 2019). Ogueji (2021) found a reliability coefficient of 0.75 among pregnant HIV-positive women in Nigeria. The current study found a reliability coefficient of 0.85 among the nurses.
Study procedure
A computer-assisted personal interview (CAPI) facilitated the participants’ answers. The rationale was to ensure mobile responsiveness and that nurses could easily access it with their mobile devices. SurveyCTO and Kobo toolbox were used to achieve this. The link to the survey was distributed to nurses, their WhatsApp platforms, and emails. The link contained assurances of the data’s confidentiality and clear instructions for completing the survey. Nurses used CAPI to respond to questions on the scales, and their answers were immediately recorded and kept on secure servers. Additionally, it enabled the nurses to pause the survey and pick up where they left off later. A helpline or support email was set up in case of any technical problems, and frequent reminders were sent to individuals who had not yet completed the survey to encourage maximum participation. The process took about 5 months, from November 2022 to March 2023.
Data analysis
Data collected in the study were analyzed using both descriptive and inferential statistics. Descriptive statistics was used to determine the frequency of psychache, compassion fatigue, self-compassion, and general wellbeing. On the other hand, inferential statistics such as Hayes PROCESS macro model 1, zero-order correlation, and t-test were used to examine the hypotheses. The analyses were carried out with sub-programs (Thomas Haye plugin) of the IBM/SPSS software, version 230.
Results
Of 544 respondents, 410(75.4%) were women, and 144(26.5%) were men, reflecting a higher proportion of female nurses in the cohort. The Mean±SD age of nurses was 35±7.12 years, indicating a middle-aged workforce with a moderate age spread. The majority of nurses followed Christianity (313, 57.5%), then Islam (203, 37.2%), with a smaller number adhering to traditional beliefs (27, 5.0%) or uncertain beliefs (11, 0.2%). Nurses worked across various departments, with the highest numbers in surgery with 61(11.2%), outpatient with 46(8.5%), and medical with 41(7.5%) units. The remaining 72.8% were distributed across other specialized units. This distribution shows diverse specialties and service areas within the nursing cohort. Many nurses, 231(42.5%), had 1-3 years of service, suggesting a considerable influx of newer professionals into the nursing field. Those with 4-6 years (146, 26.8%) and 7-9 years (113, 20.8%) of service represent mid-career nurses, while 64 nurses (9.9%) had a decade or more of experience, indicating a seasoned group of practitioners.
Frequency of the study variables
This aspect of the study provides the frequency of self-compassion, psychache, compassion fatigue, and psychological wellbeing of nurses in the study setting. The mean values (39.1, 43.01, 19.17, and 48.65, respectively) were used to categorize the low and high categories. Scores below the mean were classified as low, while scores above the mean were labeled as high. Table 1 presents the outcome of the analysis.
Relationships among the study variables
The correlation coefficients between the studied variables are presented in Table 2.
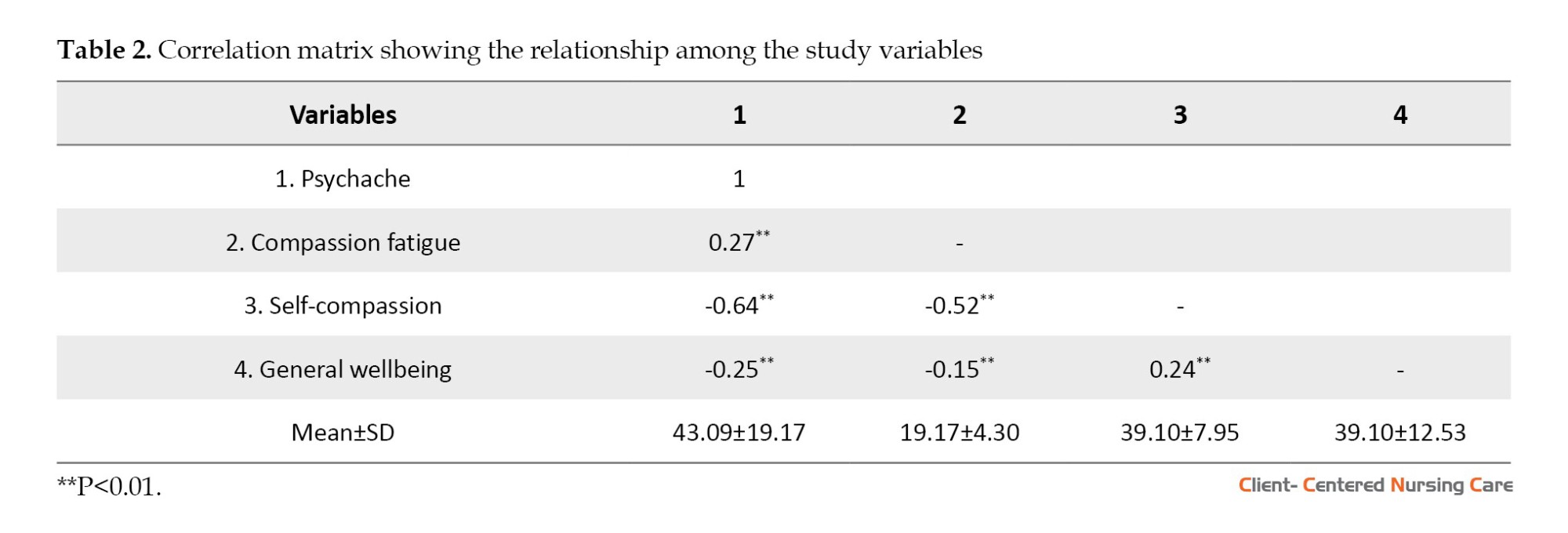
The result is a significant negative relationship between psychache and general wellbeing (r552=-0.25, P<0.01). This finding implies that nurses who reported high psychache tend to have increased negative or lower general wellbeing. Compassion fatigue and general wellbeing also had a significant negative relationship (r552=-0.15, P<0.01). This finding also implies that nurses who experience a high level of compassion fatigue tend to have low general wellbeing. Finally, a significant positive relationship was also between self-compassion and general wellbeing (r552=0.24, P<0.05). This finding means that nurses who reported high self-compassion tend to have high general wellbeing.
Hypothesis one
Self-compassion will significantly moderate the relationship between psychache and the general wellbeing of the nurses in the aftermath of the pandemic.
According to Table 3, a statistically significant direct effect of psychache (β=2.467, SE=0.115, P<0.001) and self-compassion (β=2.945, SE=0.143, P<0.001) on general wellbeing. Both psychache and self-compassion jointly explained a 30% variance in the general wellbeing of the nurses.
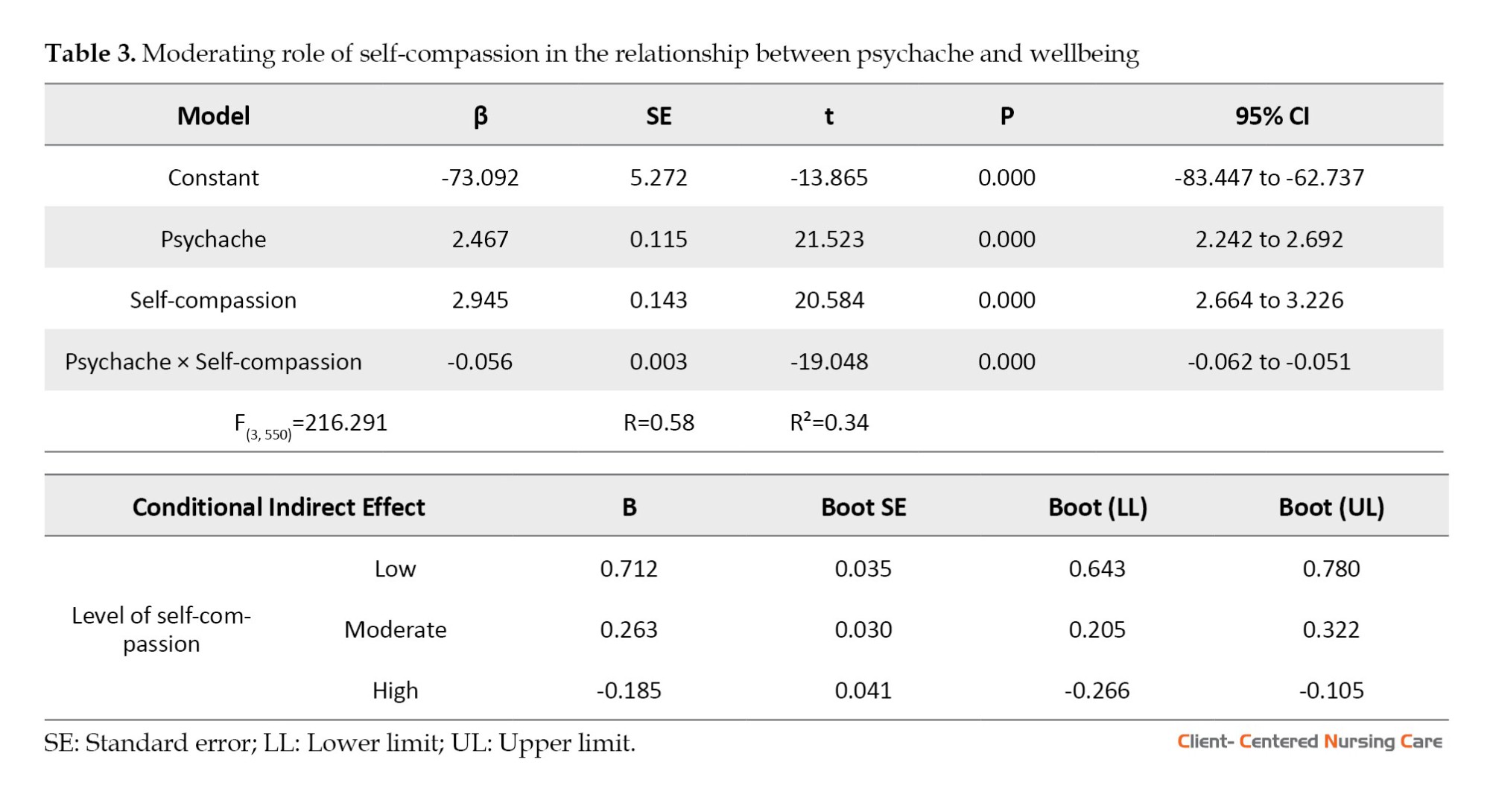
Self-compassion significantly moderated the relationship between psychache and general wellbeing (β=0.03; SE=0.01; 95% CI, -0.07%, -0.00%), where higher self-compassion levels weakened the negative impact of psychache on wellbeing. The direction of the moderating effect is also graphically presented in Figure 1.
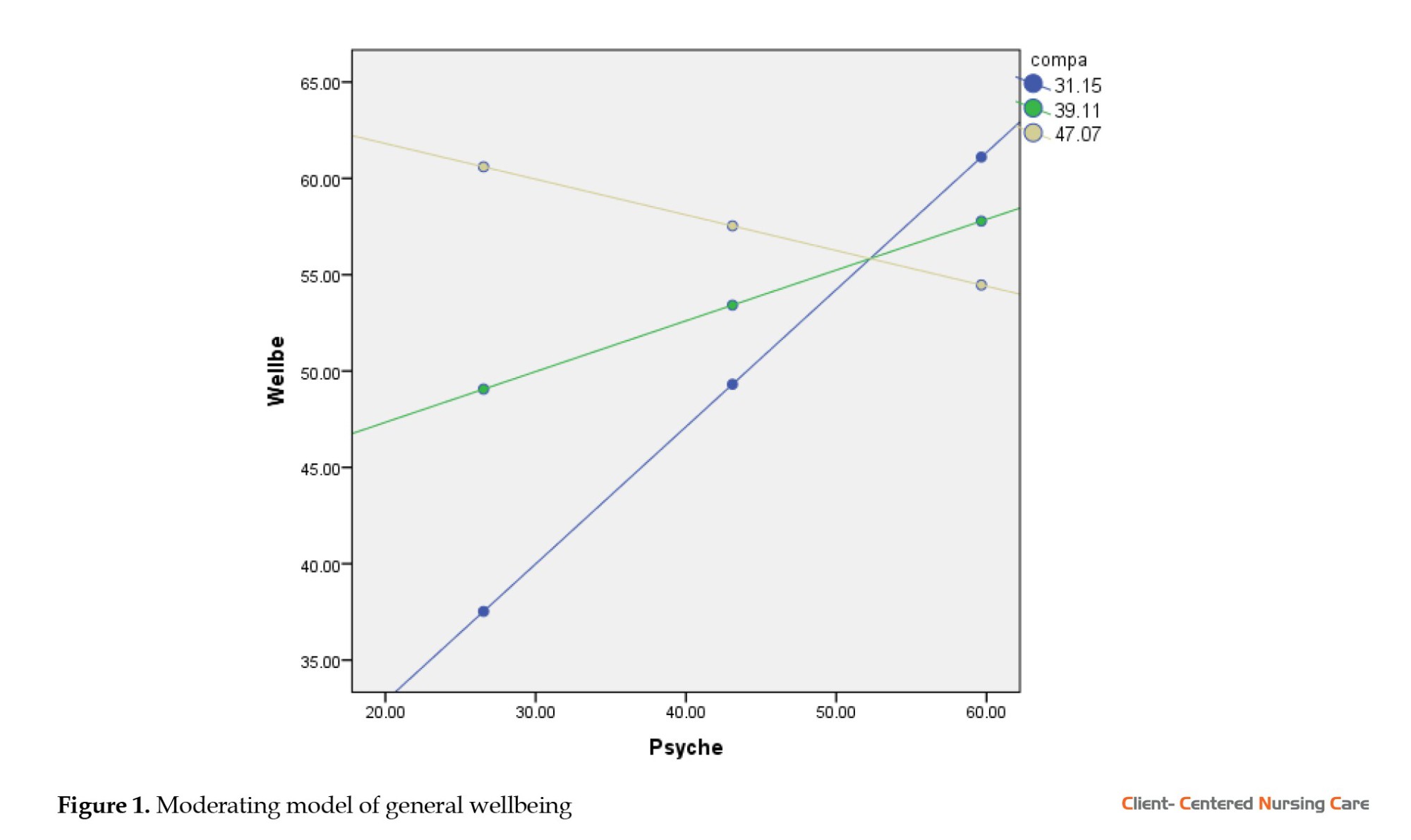
The blue line on the graph implies low self-compassion, the green line means moderate self-compassion, and the light yellow line means high self-compassion. It, therefore, implies that self-compassion strengthens the negative relationship between psychache and general wellbeing, with this relationship much stronger among nurses with lower levels of self-compassion than those with moderate and high self-compassion levels. Further observation suggests that the conditional indirect effect of psychache on general wellbeing through self-compassion is significantly much stronger among nurses with a lower level of self-compassion (B=0.712; 95% CI, 0.643%, 0.780%) than those with moderate (B=0.263; 95% CI, 0.205%, 0.322%) and high self-compassion (B=-0.185; 95% CI, -0.266%, -0.105%).
Hypothesis two
Self-compassion will significantly moderate the relationship between compassion fatigue and the general wellbeing of the nurses in the aftermath of the pandemic.
Table 4 reveals that compassion fatigue (β=0.021; SE=0.134; P=0.879) did not predict general wellbeing among nurses. There was a statistically significant direct effect of self-compassion on general wellbeing (β=0.373; SE=0.089; P<0.001), which suggests the independent predicting role of self-compassion on general wellbeing. Compassion fatigue and self-compassion jointly explained a 7% variation in the general wellbeing of the nurses. The result also found that self-compassion did not significantly moderate the impact of compassion fatigue on wellbeing (β=0.027; SE=0.017; 95% CI, -0.007%, 0.061%), suggesting that self-compassion might be less effective in contexts of chronic emotional exhaustion compared to acute psychological distress.
Hypothesis three
There will be gender differences in general wellbeing among the nurses.
According to Table 5, there is a significant difference in the scores of general wellbeing between male (Mean±SD 42.96±10.45) and female nurses (Mean±SD 50.69±12.67), with female nurses reporting higher wellbeing (t547=-7.12; P<0.001; 95% CI, -9.78%, -5.54%). This means that females significantly scored higher on general wellbeing than their male counterparts with a medium effect size, as shown by Cohen’s d value of 0.66.
Discussion
This research aimed to determine the prevalence of psychache, compassion fatigue, self-compassion, and general wellbeing of nurses at Obafemi Awolowo University Teaching Hospital Complex (OAUTHC) in the aftermath of the pandemic. Moreover, the study further intended to evaluate the moderating role of self-compassion in the relationship between psychache and compassion fatigue on the general wellbeing of the nurses. The findings of the study imply that a notable portion of the nurses have low psychological wellbeing, suggesting that many may be grappling with mental or emotional challenges in the aftermath of the pandemic. In contrast, a majority reported adequate psychological wellbeing above the average. This status is encouraging, but it also emphasizes the contrast and disparity among the nurses. The research also highlights the critical role of self-compassion, with many nurses manifesting high self-compassion, indicating potential disparity struggles in treating themselves with kindness and understanding during challenging times. Furthermore, compassion fatigue, a phenomenon common among healthcare professionals due to the emotional strain of caring for patients, is evident in this study. Many nurses faced high levels of compassion fatigue, pointing to the need for interventions that address this specific form of burnout. Lastly, the concept of psychache, which pertains to profound emotional pain and distress, was also examined. Many nurses reported experiencing high levels of psychache, underlining the depth of emotional distress they might be undergoing. These findings underscore the complexity of nurses’ challenges, especially during a global crisis. Healthcare institutions must recognize these issues and implement strategies to support and bolster the wellbeing of their frontline workers.
The results of this study show a statistically significant inverse association between the nurses’ overall wellbeing and psychache. This result suggests that psychological wellbeing decreases with increasing psychache. This result supports Michael’s (2011) claim that psychological wellbeing is skewed by pain owing to unmet needs. However, the positive relationships that self-compassion has with life satisfaction and psychological wellbeing are consistent with research by Neff et al. (2007, 2007b), Neely et al. (2009), Raes (2010), Johnson and O’Brien (2013), and Odou and Brinker (2014). The study’s findings also show that self-compassion moderates the association between psychological wellbeing and psychache, which may explain why it has a positive relationship with psychological wellbeing. The descriptive analysis clearly shows that most nurses have high levels of self-compassion, indicating the role of self-compassion in the connection between psychological wellbeing and psychache. This finding implies that elevated levels of self-compassion could function as a safeguard or buffer, potentially mitigating the deleterious impacts of psychache on general wellbeing. Dev et al. (2020) also put forth the idea, highlighting the correlation between strong self-compassion, improved quality of life, and decreased burnout.
Interestingly, there is no moderating effect between general wellbeing and compassion fatigue when self-compassion is present. This distinction highlights the complex function of self-compassion and its fluctuating impacts on various psychological stressors. In addition, the study findings indicate a negative relationship between compassion fatigue and psychological wellbeing, which is commensurate with existing studies like Yoder, (2010), Kolthoff and Hickman (2017), and Ricciardelli et al. (2018), which suggests that compassion fatigue exposes nurses to trauma which is detrimental to their psychological wellbeing.
This study found a gender gap in general wellbeing scores. Overall, women scored higher on general wellbeing than men. With a medium effect size, this statistically significant difference suggests gender-related differences in coping mechanisms, resilience, nursing experiences, and expectancies. Nurses’ gender differences in general wellbeing are significant. Female nurses have higher general wellbeing scores than male nurses, suggesting they use better or more diverse coping mechanisms in stressful situations. Social conditioning encourages women to express emotions and seek support, which may improve emotional processing.
Another possibility is that female nurses are more resilient to adversity. According to Canal-Rivero et al. (2023), personal experiences, professional training, and social support systems that are more accessible to female nurses may contribute to their resilience. Male and female nurses may have different job experiences. These differences could involve patient contacts, peer relationships, or administrative dynamics. Such differences may affect their health differently. The nursing profession, traditionally female (Adekoya, 2023), may have gender-based expectations and standards. Male nurses may encounter specific problems or pressures that affect their wellbeing scores due to their minority status. Given this gender gap, healthcare organizations should consider gender-sensitive support. Recognizing that male and female nurses may have different needs or obstacles can improve solutions. This research emphasizes the necessity for a diversified approach to nursing wellbeing that considers gender disparities.
The findings from this study accentuate the profound psychological challenges nurses face in OAUTHC after the COVID-19 pandemic. Health institutions must recognize and address these issues, considering the critical role of nurses in healthcare delivery. Interventions focusing on enhancing self-compassion could be instrumental, given its protective role. Moreover, understanding gender-specific needs and challenges can lead to more tailored and effective wellness programs.
When planning measures to ensure the health of nurses working at OAUTHC following COVID-19, it is essential to take gender inequalities into account. More effective wellness programs for nurses can be achieved by considering gender-specific requirements and using treatments that promote self-compassion.
Conclusion
The research delved into the psychological wellbeing of nurses at OAUTHC, revealing complex dynamics around psychache, compassion fatigue, self-compassion, and general mental health. While some nurses reported low wellbeing, the majority showed satisfactory mental health levels, highlighting the diversity of experiences within the nursing community during the crisis. Self-compassion emerged as a crucial factor, potentially buffering against mental distress, although its effects vary between psychache and compassion fatigue. Additionally, a gender-based disparity in wellbeing was observed, suggesting the need for tailored support mechanisms. Overall, the study underscores the importance of comprehensive interventions to support nurses’ mental wellbeing, including counseling, self-compassion workshops, gender-sensitive support groups, and strategies to address compassion fatigue.
The study, though insightful, has limitations: Its quantitative focus may overlook nuanced narratives, its localized scope raises concerns about generalisability, and its cross-sectional design may not capture evolving dynamics. Additionally, the limited sample size may not fully represent diverse backgrounds, warranting cautious interpretation of findings.
Future research can address limitations by combining quantitative and qualitative methods, expanding beyond OAUTHC to capture regional differences, adopting a longitudinal design to track wellbeing dynamics, and diversifying data collection techniques. Observational methods and diverse participant pools can offer multifaceted insights while exploring additional variables like workload intensity and gender-specific experiences can enrich understanding. These efforts aim to comprehensively address nurses’ experiences and challenges, ensuring more effective support strategies.
Ethical Considerations
Compliance with ethical guidelines
This study followed ethical requirements to protect and care for participants. All participants were told of the study’s goal and its ramifications before it began. Each participant gave informed consent, knowing their rights, including the ability to leave the study without penalty. Confidentiality and anonymity were strictly preserved to protect participant data and responses. The ethical approval under protocol number FSS/OAU/RREC/0299 shows that the research team upheld the highest ethical standards, ensuring that the study was conducted with integrity, respect for human dignity, and by international ethical guidelines for human subject research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Tamuno-opubo Addah Temple; Data collection and analysis: Uthman Jamiu Tinuoye; Writing: Idehen Egbewuare Emmanuel and Baba Ahmed Karatu; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are indeed grateful to these persons and groups, in no particular order: The Nursing Department of the OAUTHC, students of the School of Health Information Management, Obafemi Awolowo University Teaching Hospital Complex (OAUTHC), the Mental Health Support Initiative (MHSI-OAU) and the Psychcare Humaniterex Foundation, Aladanla, Ile-Ife, Osun State.
References
Adams, R. E., Boscarino, J. A. & Figley, C. R., 2006. Compassion fatigue and psychological distress among social workers: A validation study. The American Journal of Orthopsychiatry, 76(1), pp. 103–8. [DOI:10.1037/0002-9432.76.1.103] [PMID]
Adekoya, C., 2023. Feminization and image of librarianship in academic environment: The Nigerian perspective. International Journal of Library and Information Science Studies, 9(1), pp. 47-66. [Link]
Aiken, L. H., et al., 2002. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA, 288(16), pp. 1987-93. [DOI:10.1001/jama.288.16.1987] [PMID]
Akanni, A. A., Ajele, K. W. & Oduaran, C. A., 2023. Moderating effect of resilience in the relationship between compassion fatigue and mental wellbeing among frontline health workers exposed to COVID-19 Patients. Romanian Journal of Applied Psychology, 25(1-2), pp. 9-13. [Link]
Alabi, O. T., et al., 2023. Relationship between psychological distress and perceived stigma on mental wellbeing in people with epilepsy: Self-compassion as a moderator. Arab Journal of Psychiatry, 34(1), pp. 56. [Link]
Aliado, B., 2022. The relationship between self-compassion and relational assertiveness for women in psychotherapy [PhD dissertation]. California: Alliant International University. [Link]
Alquwez, N., et al., 2021. Self‐compassion influences the caring behaviour and compassion competence among saudi nursing students: A multi‐university study. Nursing Open, 8(5), pp. 2732-42. [DOI:10.1002/nop2.848] [PMID]
Andina-Díaz, E., et al., 2023. Nursing students’ perception about gender inequalities presented on social networks: A qualitative study. International Journal of Environmental Research and Public Health, 20(3), pp. 1962. [DOI:10.3390/ijerph20031962] [PMID]
Babenko, O. & Guo, Q., 2019. Measuring self-compassion in medical students: Factorial validation of the Self-Compassion Scale-Short Form (SCS-SF). Academic Psychiatry, 43(6), pp. 590-4. [DOI:10.1007/s40596-019-01095-x] [PMID]
Beasley, B. E., 2021. Suicide prevention through self-compassion in a virtual world: A proposed treatment intervention for suicidality in young men [PhD dissertation]. California: Antioch University. [Link]
Canal-Rivero, M., et al., 2023. The impact of COVID-19 pandemic on the psychological wellbeing among health care workers: A 6-month cohort longitudinal survey study. Revista de Psiquiatria y Salud Mental, 16, pp. 25–37. [DOI:10.1016/j.rpsm.2022.08.001] [PMID]
Carleton, R. N., et al., 2018. Mental disorder symptoms among public safety personnel in Canada. The Canadian Journal of Psychiatry, 63(1), pp. 54-64. [PMID]
Chinweuba, D. C., et al., 2023. Does self-concealment and self-compassion differentially influence substance use for male versus female adolescents? Journal of Substance Use, 28(1), pp. 117-22. [DOI:10.1080/14659891.2021.2018726]
Cordova, M. J., et al., 2020. Foster wellbeing throughout the career trajectory: A developmental model of physician resilience training. Mayo Clinic Proceedings, 95(12), pp. 2719–33. [DOI:10.1016/j.mayocp.2020.05.002] [PMID]
Dev, V., Fernando, A. T., 3rd. & Consedine, N. S., 2020. Self-compassion as a Stress Moderator: A cross-sectional study of 1700 doctors, nurses, and medical students. Mindfulness, 11(5), pp. 1170–81. [DOI:10.1007/s12671-020-01325-6] [PMID]
Dodge, B., et al., 2012. The significance of privacy and trust in providing health-related services to behaviorally bisexual men in the United States. AIDS Education and Prevention : Official Publication of the International Society for AIDS Education, 24(3), pp. 242–56. [DOI:10.1521/aeap.2012.24.3.242] [PMID]
du Plessis, M., 2023. Trait emotional intelligence and flourishing: The mediating role of positive coping behaviour. SA Journal of Industrial Psychology, 49(1), pp. 1-14. [DOI:10.4102/sajip.v49i0.2063]
Durkin, M., et al., 2016. A pilot study exploring the relationship between self-compassion, self-judgement, self-kindness, compassion, professional quality of life and wellbeing among UK community nurses. Nurse Education Today, 46, pp. 109-14 [DOI:10.1016/j.nedt.2016.08.030] [PMID]
Ericsson, C. R., et al., 2022. Paramedics’ perceptions of job demands and resources in Finnish emergency medical services: A qualitative study. BMC Health Services Research, 22(1), pp. 1469. [DOI:10.1186/s12913-022-08856-9] [PMID]
Figley, C. R., 1995. Compassion fatigue as secondary traumatic stress disorder: An overview. In C. R. Figley (Ed.), Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized (pp. 1–20). Brunner/Mazel. [Link]
Garcia-Campayo, J., et al., 2014. Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self-Compassion Scale (SCS). Health and Quality of life Outcomes, 12, pp. 4. [DOI:10.1186/1477-7525-12-4] [PMID]
Holden, R. R., et al., 2001. Development and preliminary validation of a scale of psychache. Canadian Journal of Behavioural Science/Revue canadienne des Sciences du Comportement, 33(4), pp. 224–32. [DOI:10.1037/h0087144]
Hurley, J., et al., 2020. Emotional intelligence as a mechanism to build resilience and non‐technical skills in undergraduate nurses undertaking clinical placement. International Journal of Mental Health Nursing, 29(1), pp. 47-55. [DOI:10.1111/inm.12607] [PMID]
Jessome, M. G., 2024. Gendered meanings and mechanisms of intimacy for people living with chronic pain. Culture, Health & Sexuality, 26(3), pp. 391–404. [DOI:10.1080/13691058.2023.2212294] [PMID]
Johnson, E. A. & O’Brien, K. A., 2013. Self-compassion soothes the savage ego-threat system: Effects on negative affect, shame, rumination, and depressive symptoms. Journal of social and Clinical Psychology, 32(9), pp. 939-63. [DOI:10.1521/jscp.2013.32.9.939]
Joinson, C., 1992. Coping with compassion fatigue. Nursing, 22(4), pp. 116–20. [DOI:10.1097/00152193-199204000-00035] [PMID]
Kohnen, D., et al., 2023. What makes nurses flourish at work? How the perceived clinical work environment relates to nurse motivation and wellbeing: A cross-sectional study. International Journal of Nursing Studies, 148, pp. 104567. [DOI:10.1016/j.ijnurstu.2023.104567] [PMID]
Kolthoff, K. L. & Hickman, S. E., 2017. Compassion fatigue among nurses working with older adults. Geriatric Nursing, 38(2), pp. 106-9. [DOI:10.1016/j.gerinurse.2016.08.003] [PMID]
Mefoh P. C., et al., 2016. Psychological wellbeing in awaiting-trial inmates: The roles of loneliness and social support. Social Sciences, 5(5), pp. 64-9. [DOI:10.11648/j.ss.20160505.11]
Mills, J. F., Green, K. & Reddon, J. R., 2005. An evaluation of the Psychache Scale on an offender population. Suicide & Life-Threatening Behavior, 35(5), pp. 570–80. [DOI:10.1521/suli.2005.35.5.570] [PMID]
Neely, M. E., et al., 2009. Self-kindness when facing stress: The role of self-compassion, goal regulation, and support in college students’ wellbeing. Motivation and Emotion, 33, pp. 88-97. [DOI:10.1007/s11031-008-9119-8]
Neff, K. D., 2003. The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), pp. 223-50. [DOI:10.1080/15298860309027]
Neff, K. D. & Pommier, E., 2013. The relationship between self-compassion and other-focused concern among college undergraduates, community adults, and practicing meditators. Self and Identity, 12(2), pp. 160-76. [DOI:10.1080/15298868.2011.649546]
Neff, K. D., Kirkpatrick, K. L. & Rude, S. S., 2007. Self-compassion and adaptive psychological functioning. Journal of Research in Personality, 41(1), pp. 139-54. [DOI:10.1016/j.jrp.2006.03.004]
Neff, K. D., Rude, S. S. & Kirkpatrick, K. L., 2007. An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of Research in Personality, 41(4), pp. 908-16. [DOI:10.1016/j.jrp.2006.08.002]
Nolte, A. G., et al., 2017. Compassion fatigue in nurses: A metasynthesis. Journal of Clinical Nursing, 26(23-24), pp. 4364-78. [DOI:10.1111/jocn.13766] [PMID]
Obi, C. U., et al., 2023. Self-compassion and Empathic Concerns as Correlates of Prosocial Behaviour Among Youths in Awka Metropolis. Practicum Psychologia, 13(1), pp. 45-60. [Link]
Odou, N. & Brinker, J., 2014. Exploring the relationship between rumination, self-compassion, and mood. Self and Identity, 13(4), pp. 449-59. [DOI:10.1080/15298868.2013.840332]
Oginyi, C., et al., 2023. Roles of self-compassion and coping strategies in burnout among catholic clergy and religious in Benue State, Nigeria. Nigerian Journal of Social Psychology, 5(2), pp. 175-93. [Link]
Ogueji, I. A., 2021. Experiences and predictors of psychological distress in pregnant women living with HIV. British Journal of Health Psychology, 26(3), pp. 882-901. [DOI:10.1111/bjhp.12510] [PMID]
Onyedibe, M. C. C., Onyekwelu, C. A. & Ugwu, L. I., 2015. An evaluation of the relationship between coping, emotional intelligence and psychological wellbeing among Nigerian undergraduates. International Journal of English Language, Literature and Humanities, 2(10), pp. 1-18. [Link]
Patel, R., 2018. “Compassion fatigue among mental healthcare providers and the impact on overall wellbein. [PhD dissertations]. San Francisco: University of San Francisco. [Link]
Raab, K., 2014. Mindfulness, self-compassion, and empathy among health care professionals: A review of the literature. Journal of Health Care Chaplaincy, 20(3), pp. 95-108. [DOI:10.1080/08854726.2014.913876]
Raes, F., 2010. Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and Individual Differences, 48(6), pp. 757-761. [DOI:10.1016/j.paid.2010.01.023]
Raes, F., et al., 2011. Construction and factorial validation of a short form of the self‐compassion scale. Clinical Psychology & Psychotherapy, 18(3), pp. 250-5. [DOI:10.1002/cpp.702] [PMID]
Rezai, M., et al., 2020. Measures of workplace inclusion: A systematic review using the COSMIN methodology. Journal of Occupational Rehabilitation, 30(3), pp. 420–54. [DOI:10.1007/s10926-020-09872-4] [PMID]
Ricciardelli, R., et al., 2018. Qualitatively unpacking Canadian public safety personnel experiences of trauma and their wellbeing. Canadian Journal of Criminology and Criminal Justice, 60(4), pp. 566-77. [DOI:10.3138/cjccj.2017-0053.r2]
Rowe, C. A., et al., 2013. The relationship between negative life events and suicidal behavior. Crisis, 34(4). [DOI:10.1027/0227-5910/a000173]
Royal College of Nursing., 2019. RCN International Nursing Research Conference and Exhibition 2019. 3-5 September 2019, Sheffield, England, UK.
Russ, E., Lonne, B. & Darlington, Y., 2009. Using resilience to reconceptualise child protection workforce capacity. Australian Social Work, 62(3), pp. 324-38. [DOI:10.1080/03124070903060042]
Ryff, C. D., 1989. Happiness is everything, or is it? Explorations on the meaning of psychological wellbeing. Journal of Personality and Social Psychology, 57(6), pp. 1069-81. [DOI:10.1037/0022-3514.57.6.1069]
Ryff, C. D. & Keyes, C. L. M., 1995. The structure of psychological wellbeing revisited. Journal of Personality and Social Psychology, 69(4), pp. 719-27. [DOI:10.1037/0022-3514.69.4.719]
Shneidman, E. S., 1993. Suicide as psychache. The Journal of Nervous and Mental Disease, 181(3), pp. 145–7. [DOI:10.1097/00005053-199303000-00001] [PMID]
Si, M. Y., et al., 2020. Psychological impact of COVID-19 on medical care workers in China. Infectious Diseases of Poverty, 9(1), pp. 113. [DOI:10.1186/s40249-020-00724-0]
Stapleton, P. B., Richardsom, K. & Kalla, M., 2018. How aspects of self-compassion contribute to wellbeing and the effect of age. International Journal of Healing and Caring, 18(3), pp. 1-12. [Link]
Sun, N., et al., 2020. A qualitative study on the psychological experience of caregivers of COVID-19 patients. American Journal of Infection Control, 48(6), pp. 592-8. [DOI:10.1016/j.ajic.2020.03.018] [PMID]
Sydney-Agbor, N. N., 2021. Prevalence and predictors of psychache among widows in Imo State, Nigeria. Nigerian Journal of Social Psychology, 4(1), pp. 27-39. [Link]
Tanrıverdi, D., Bekircan, E. & Koç, Z., 2024. The relationship between psychache and suicide risk with spiritual wellbeing levels of patients diagnosed with depression. Journal of the American Psychiatric Nurses Association, 30(1), pp. 132-40. [DOI:10.1177/10783903221079796]
Troister, T. & Holden, R. R., 2012. Comparing psychache, depression, and hopelessness in their associations with suicidality: A test of Shneidman’s theory of suicide. Personality and Individual Differences, 49(7), pp. 689-93. [DOI:10.1016/j.paid.2010.06.006]
Wicks, R. J., 2005. Overcoming secondary stress in medical and nursing practice: A guide to professional resilience and personal wellbeing. Oxford: Oxford University Press. [DOI:10.1093/oso/9780195172232.001.0001]
Wynn, M., et al., 2023. Digitizing nursing: A theoretical and holistic exploration to understand the adoption and use of digital technologies by nurses. Journal of Advanced Nursing, 79(10), pp.3737-47. [DOI:10.1111/jan.15810]
Type of Study: Research |
Subject:
Special
Received: 2023/11/20 | Accepted: 2024/05/11 | Published: 2024/11/1
Received: 2023/11/20 | Accepted: 2024/05/11 | Published: 2024/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |