Sun, Nov 23, 2025
[Archive]
Volume 10, Issue 4 (Autumn 2024)
JCCNC 2024, 10(4): 269-276 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dabis H A M, Sachit A, Talib Hameed A. Barriers to Sexual Counseling for Patients With Myocardial Infarction: A Nursing Point of View. JCCNC 2024; 10 (4) :269-276
URL: http://jccnc.iums.ac.ir/article-1-593-en.html
URL: http://jccnc.iums.ac.ir/article-1-593-en.html
1- Department of Adult Nursing, College of Nursing, University of Thi-Qar, Thi-Qar, Iraq. , hussein-ab@utq.edu.iq
2- Department of Pediatric Nursing, College of Nursing, University of Thi-Qar, Thi-Qar, Iraq.
3- Department of Nursing, Technical Institute-Nasiriya/Southern Technical University, Thi-Qar, Iraq.
2- Department of Pediatric Nursing, College of Nursing, University of Thi-Qar, Thi-Qar, Iraq.
3- Department of Nursing, Technical Institute-Nasiriya/Southern Technical University, Thi-Qar, Iraq.
Full-Text [PDF 568 kb]
(602 Downloads)
| Abstract (HTML) (1589 Views)
Full-Text: (424 Views)
Introduction
Myocardial infarction (MI), also known as a heart attack, poses a potentially fatal threat and exerts a significant negative impact on the physical and mental health of an individual (Jacquet‐Smailovic et al., 2021). MI substantially impacts intimacy and sexual function; however, post-MI care frequently overlooks the crucial aspect of sexual health (Smith, 2020). Cardiac rehabilitation heavily relies on sexual counseling to aid MI patients in addressing their intimate issues; this call not only nurtures healthy sexual activity but also enhances the overall quality of life (QoL) for these individuals (Park et al., 2023).
A heart attack may cause a variety of concerns, such as fear, worry, depression, and resentment in a person. Meanwhile, the potential of sexual activity to intensify these emotional responses is significant (Karki & Mahara, 2022). Physical restrictions, the threat of another heart attack, or strain on their cardiovascular system could be among the concerns that individuals harbor. Emotional variables potentially induce a reluctance towards sexual activity, strain relationships, and diminish overall QoL (Rashed et al., 2020). Consequently, it becomes crucial to comprehend the psychological impacts of MI and proactively address them through supportive sexual counseling (Karani & McLuskey, 2020).
Sexual counseling provides individuals and couples who have experienced an MI with the necessary direction, information, and encouragement to overcome both mental and physical hurdles, thus playing an integral role in their recovery (Mangolian Shahrbabaki et al., 2021). Professionals endowed with specific training, such as sex therapists or counselors, can then step forward to address particular issues, respond effectively to inquiries, and provide a secure environment for candid discussions about personal problems. The overarching objectives of this form of therapy involve empowering people, reducing anxiety levels, enhancing communication not only within relationships but also internally, and, most importantly, aiding in the creation of coping mechanisms that facilitate adjustment post-heart attack (Özlem & Hatice, 2022).
Despite its value, sexual counseling is still underutilized for MI patients due to a multitude of organizational, patient, and healthcare provider-related barriers (Bachmann et al., 2022). Comprehending these challenges becomes crucial to enhancing procedures in sexual counseling and optimizing the results of MI patients’ sexual health (Fennell & Grant, 2019).
In the realm of literature, a myriad of obstacles often stands as potential challenges for organizations. These challenges may include the absence of standardized protocols and guidelines, insufficient resources and support, or even issues within healthcare providers themselves, such as inadequate training in sexual counseling coupled with intense clinical practice. However, there is another factor, the patients themselves, whose concerns can range from fear of physical activity to cultural conventions that affect their readiness to discuss sexual issues due to religious beliefs (Gazestani et al., 2019; Mangolian Shahrbabaki et al., 2021; Karani & McLuskey, 2020; Simeone et al., 2020; Sadatinejad et al., 2021).
Islamic teachings pose a challenge for clients seeking sexual counseling due to the prohibition of discussing sex with non-marital partners; however, this ban may be allowed in therapeutic contexts (Akhu-Zaheya & Masadeh, 2015). Islam not only encourages the enjoyment of sex and emphasizes meeting one’s partner’s needs in monogamous marriages but also strictly prohibits any extramarital sexual activity. However, Islamic regulations’ limited stance on sexual matters can potentially give rise to contextual sexual difficulties. Also, diverse Muslim communities and various other variables hold contrasting personal interpretations of Islamic teachings: These interpretations subsequently guide their daily activities (Sungur & Bez, 2016). To the researcher’s knowledge, no previous studies have discussed this subject among cardiac patients in Iraq. So, this study aims to investigate barriers to sexual counseling for patients with MI from the nurses’ viewpoints.
Materials and Methods
Design, setting, and sample
A cross-sectional study was conducted from March 2 to November 29, 2023. As sample size estimation is usually irrelevant when using non-probability sampling (Althubaiti, 2022), 126 nurses were recruited through convenient sampling; the response rate was about 89%. The subjects were recruited from different departments of Al-Nasiriyah Heart Center, the only specialized center for treating and caring for individuals with cardiovascular problems in Dhi-Qar Governorate.
Data collection
The questionnaire was adapted from (Mangolian Shahrbabaki et al., 2021) with permission. It consists of two parts. Part one includes 7 items related to demographic and background information (age, sex, marital status, educational level, department, job experience, and taking courses involving sexual counseling).
Part two includes 30 items that have been organized down into three categories: Barriers related to patients (13 items), barriers related to nurses (12 items), and barriers related to organizations (5 items). A 3-point rating scale (agree=3, no idea=2, and disagree=1) was utilized to score the items. The researcher used the mean score, where “one” represented the lowest possible score and “three” the maximum; higher scores indicate a higher perception level of the barriers. In this study, the original English questionnaire was used, and it was not translated into Arabic because all nurses from all educational levels have completed their nursing studies in English. The content validity index of the main questionnaire was 0.80, and its content validity ratio was 0.79. The Cronbach α coefficient was 0.78 for the total scale, 0.79 for the patient-related barriers, 0.83 for nurse-related barriers, and 0.79 for the organizational barriers (Mangolian Shahrbabaki et al., 2021). In this study, the questionnaire was reviewed by a panel of 7 experts (1 psychologist, 1 cardiologist, 1 from the Human Resources Department at Dhi-Qar Health Directorate, and 3 cardiovascular nurses) with more than 10 years of experience in their respective fields. The item level content validity index was 0.83, and the scale level content validity index was 0.80, while the coefficient of variation ratio was equal to 0.79. The Cronbach α was used to examine the questionnaire’s reliability, and the results showed a correlation coefficient of 0.83 for the entire scale, 0.82 for the barriers related to patient, 0.76 for barriers related to nurse, and 0.79 for the barriers related to organization.
Statistical analyses
The data collected during this study were analyzed using SPSS software, version 27. Descriptive statistics included frequency, percentage, mean, and standard deviation. ANOVA and independent t test were used to assess the mean score of the barriers in terms of demographic variables. P≤0.05 were determined as significant.
Results
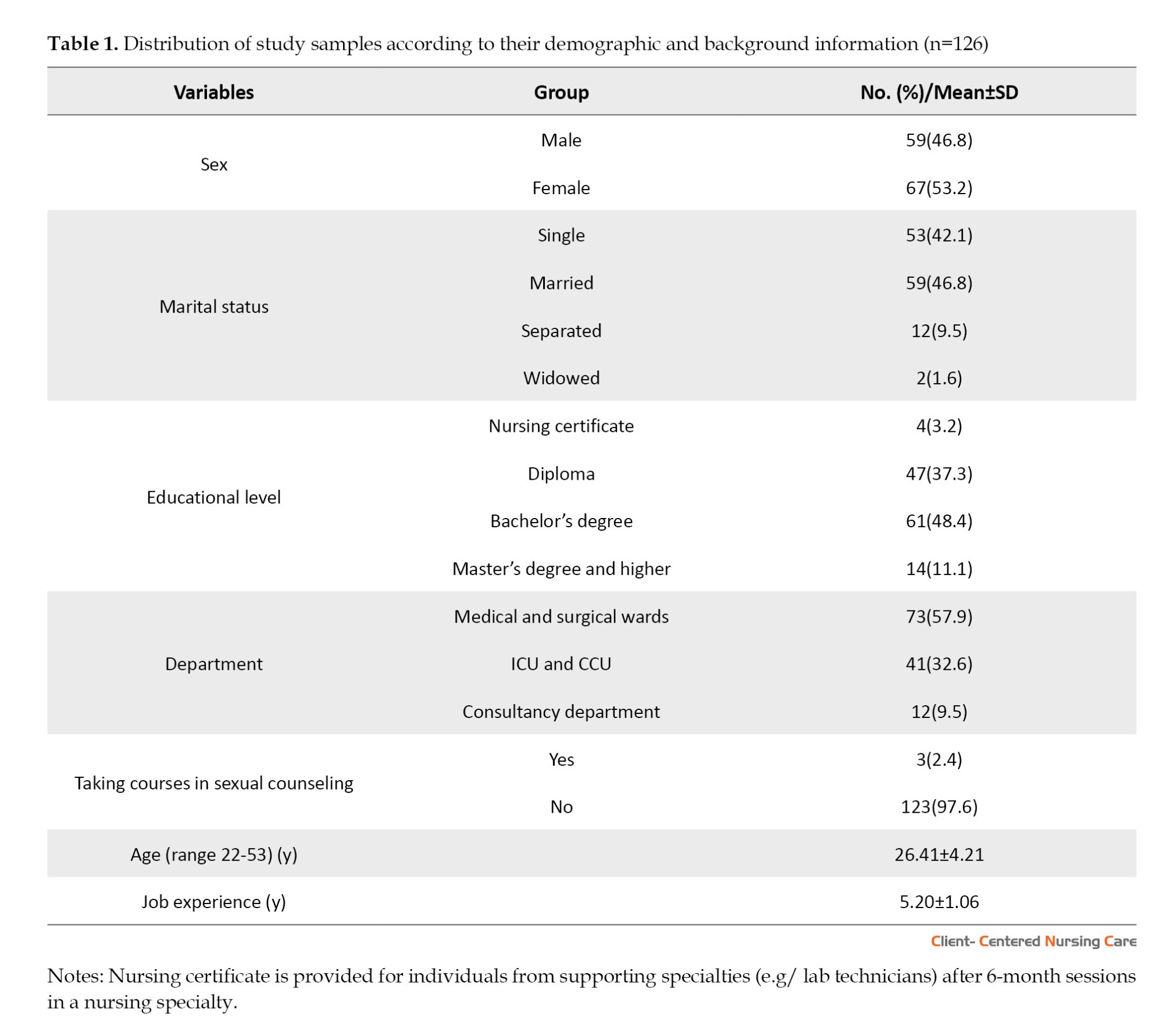
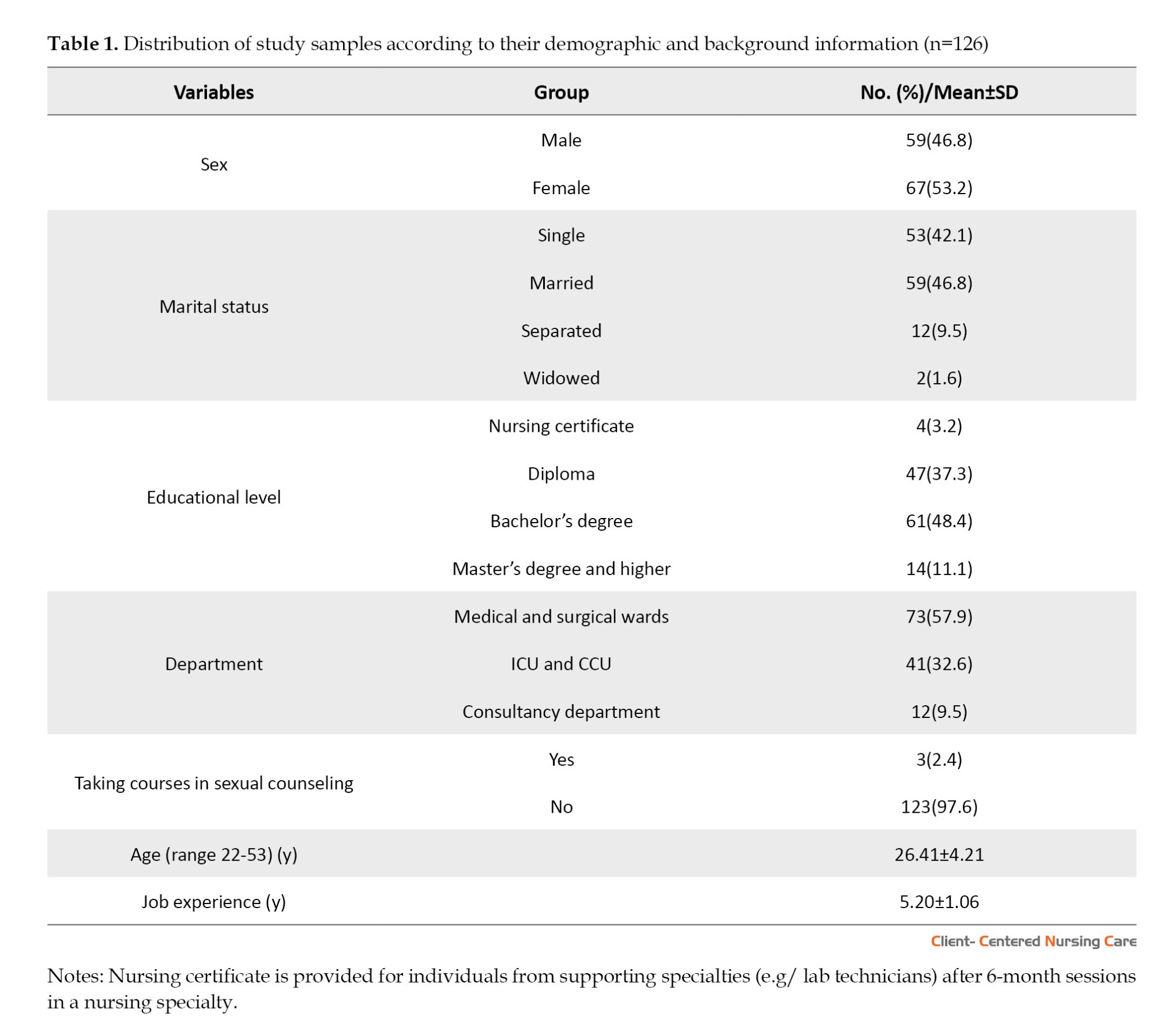
Table 1 shows that the majority of nurses were females (53.2%), married (46.8%), had BS in nursing (48.4%), working in medical and surgical wards (57.9%), and did not take any courses in sexual counseling (97.6%). The Mean±SD age of nurses was 26.41±4.21 years, with a Mean±SD experience of 5.20±1.06 years.
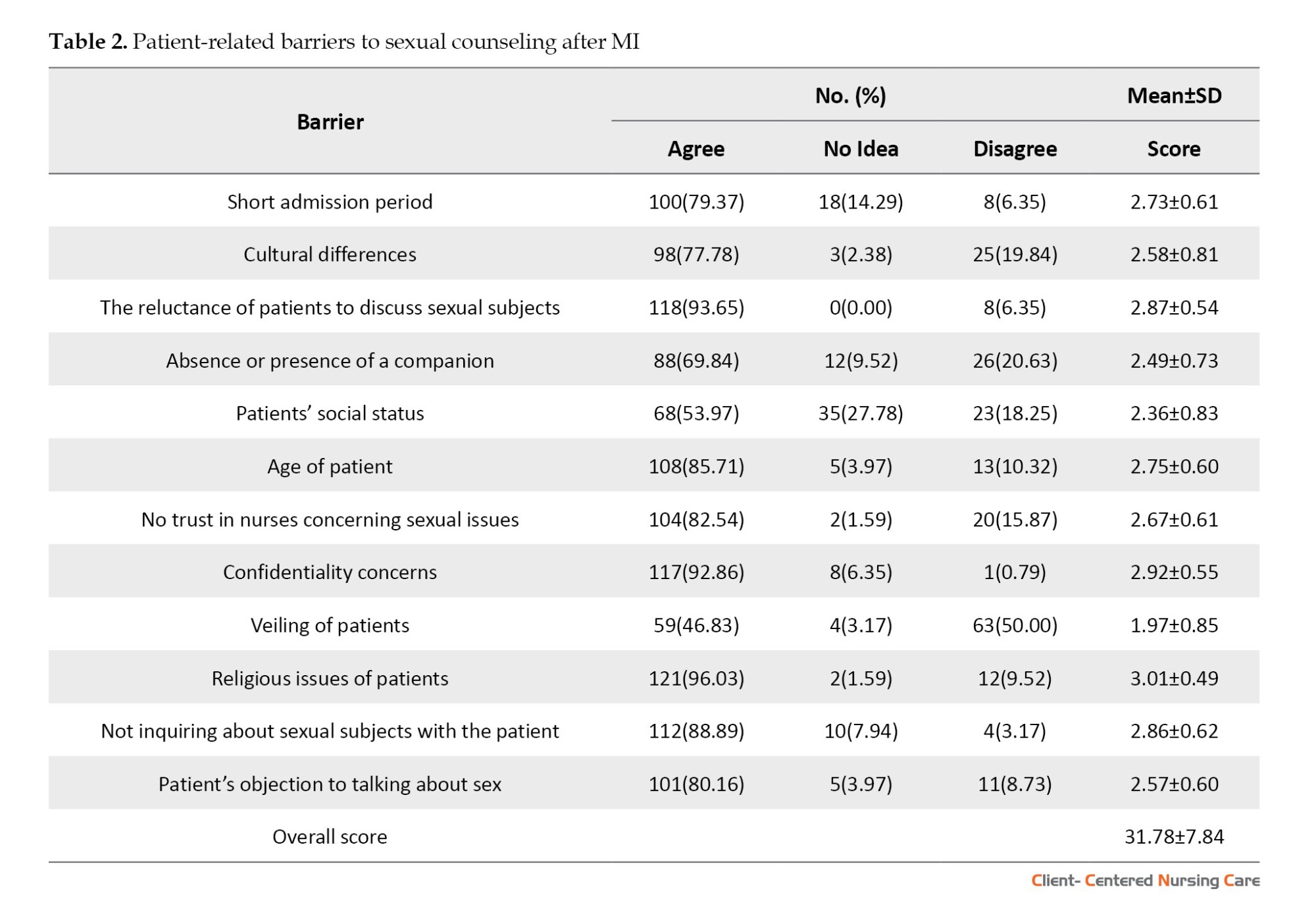
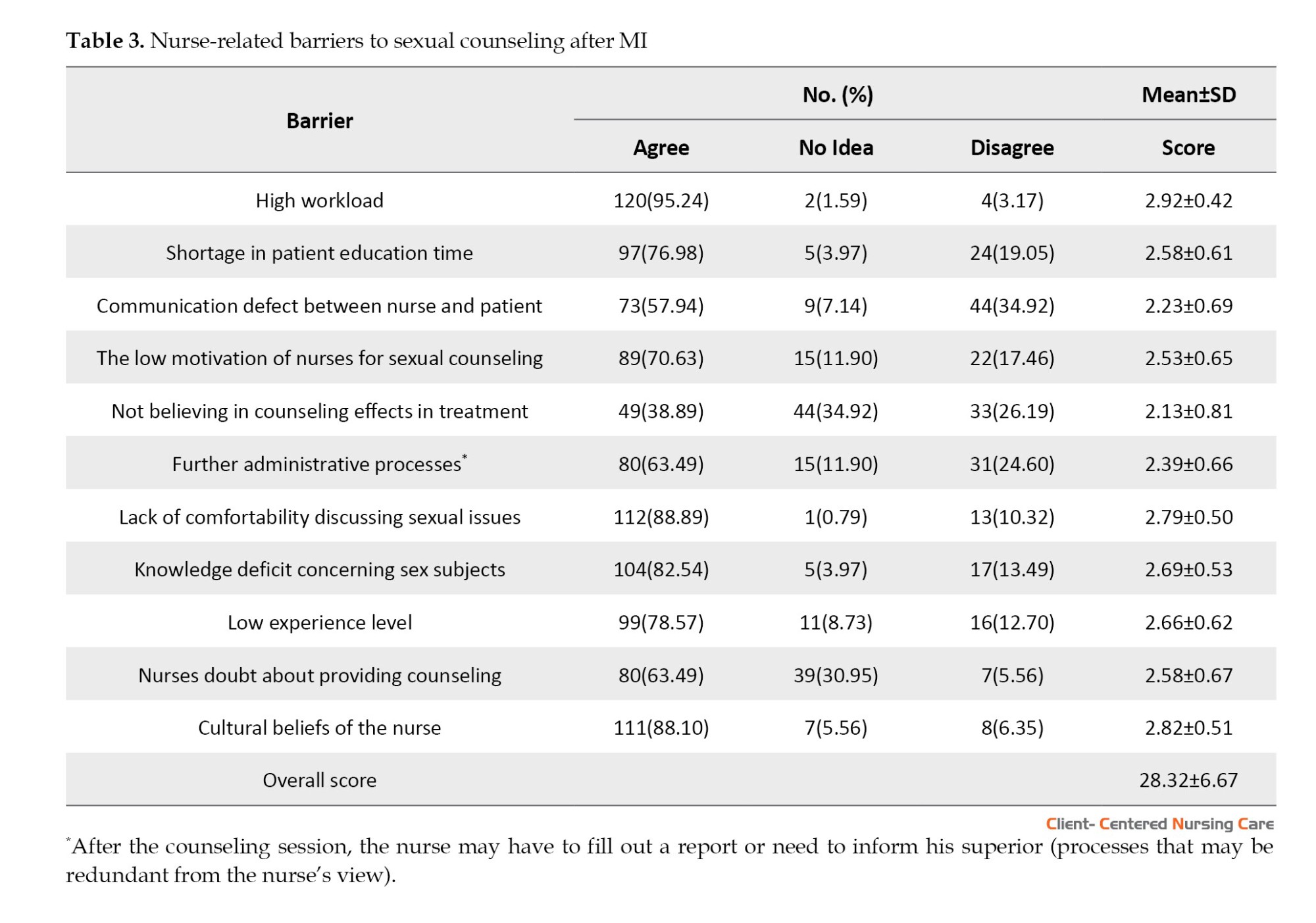
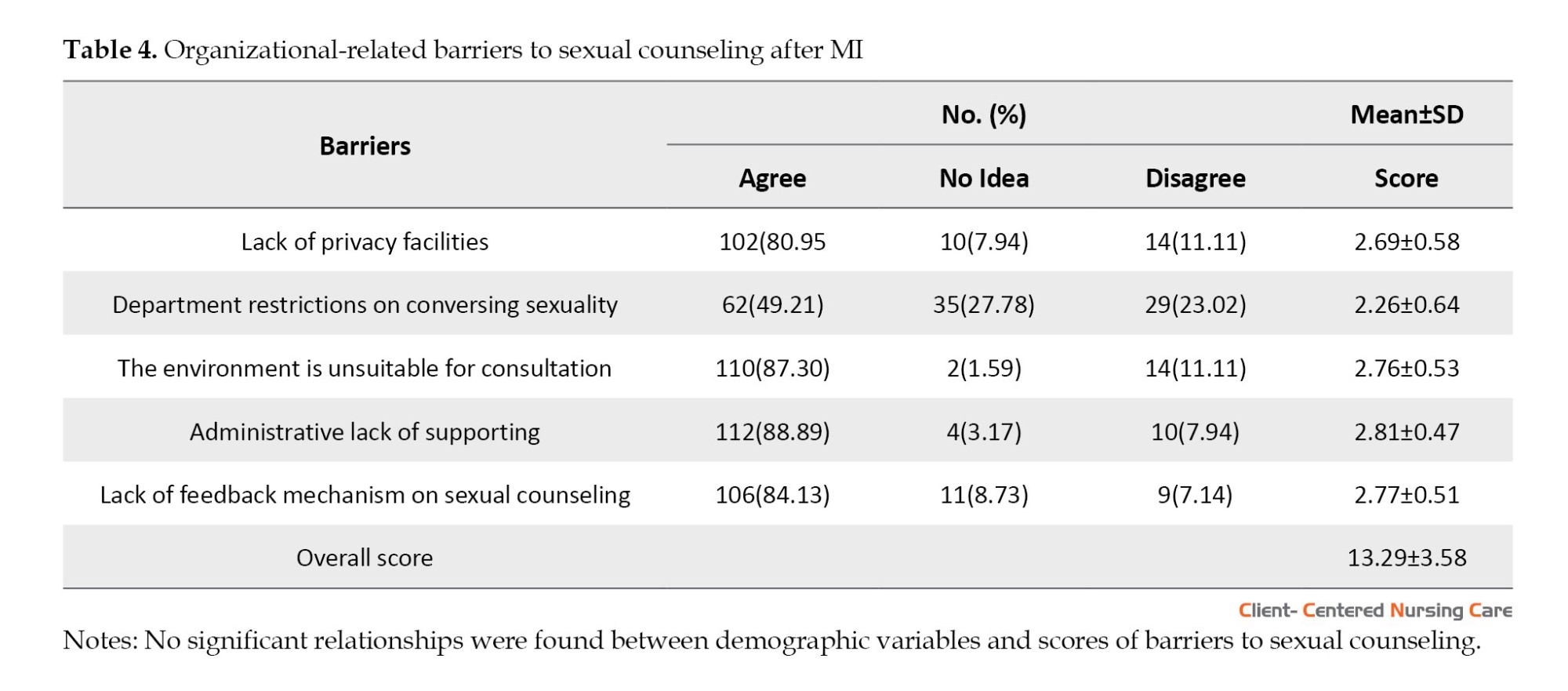
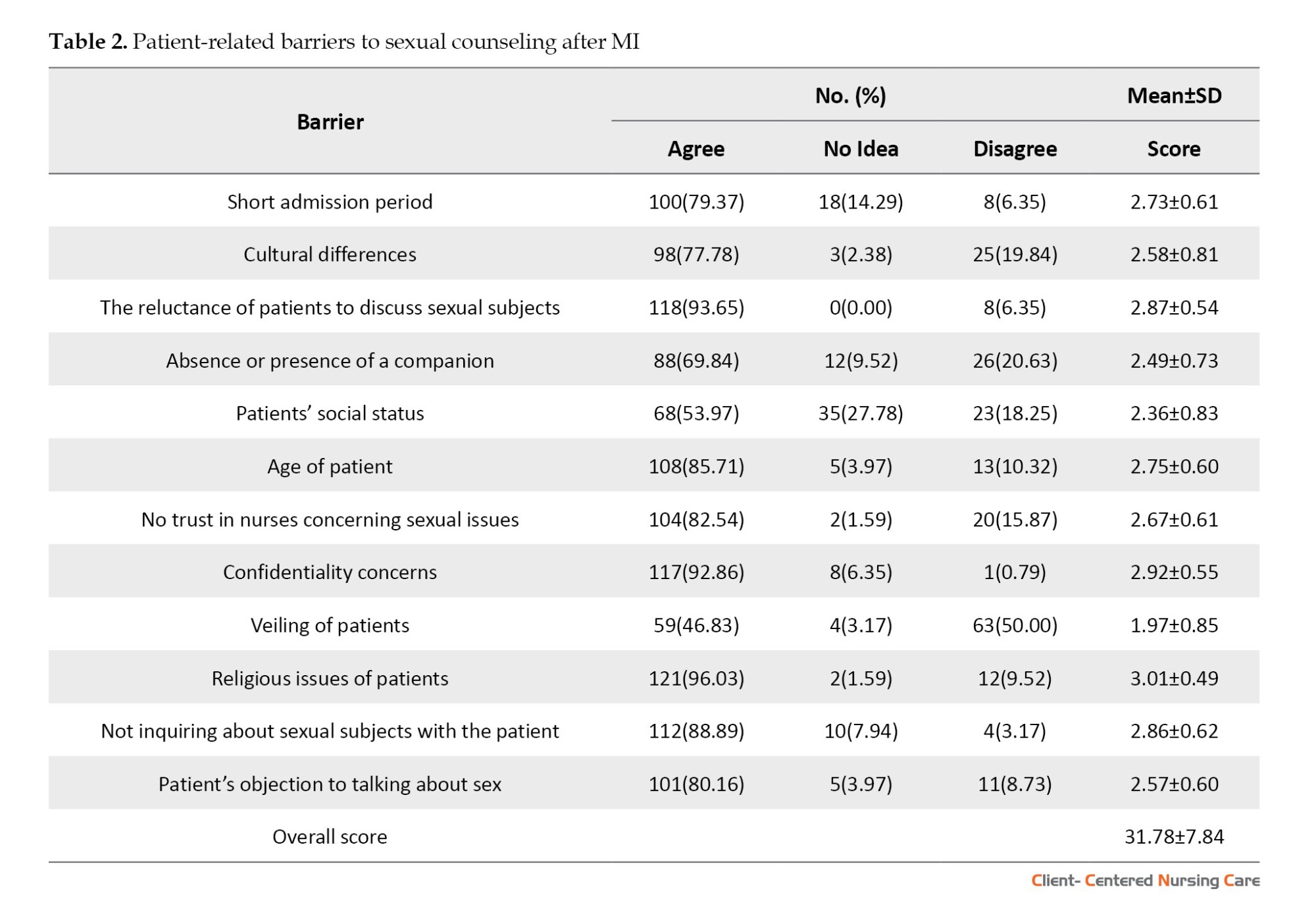
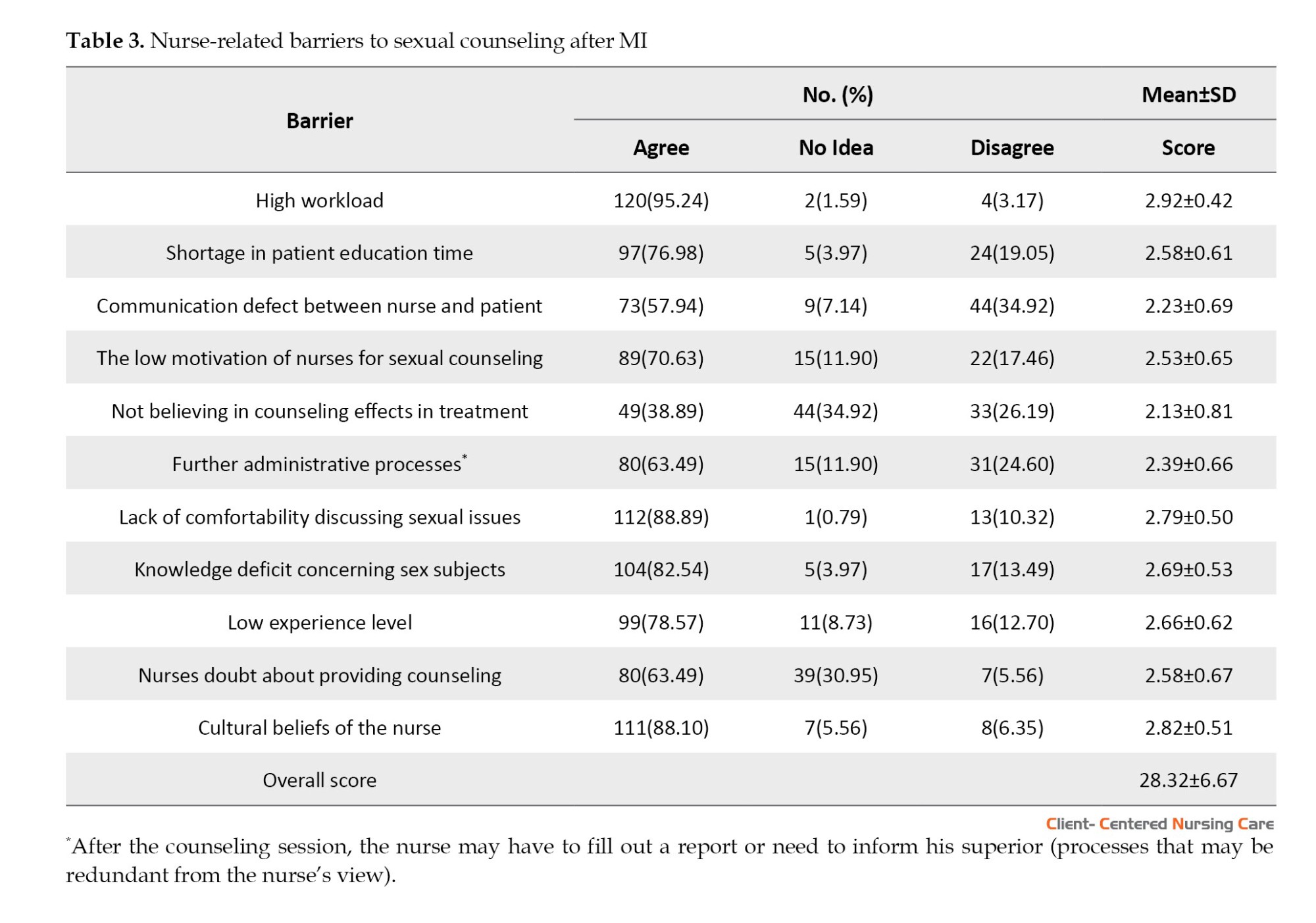
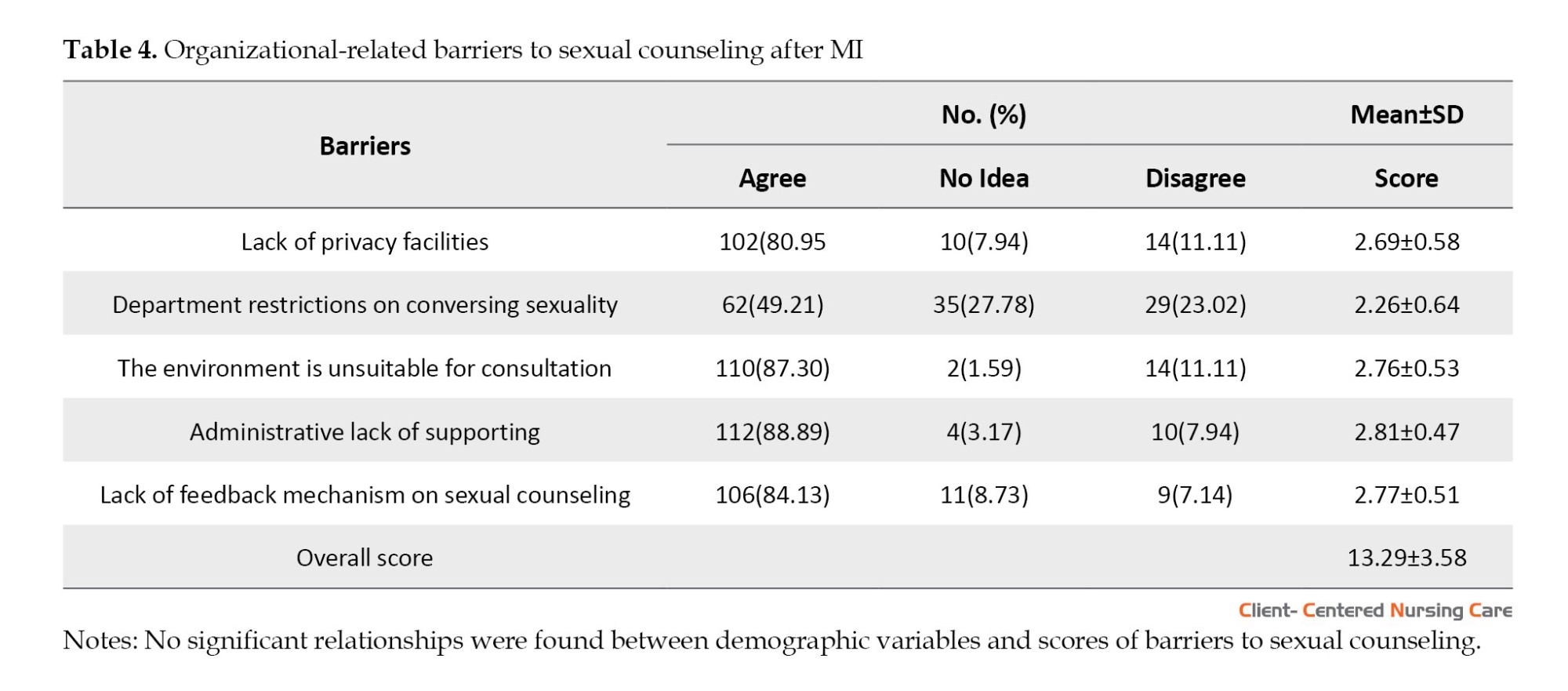
The highest mean scores concerning barriers to sexual counseling in patients with MI were related to patient (31.78±7.84), nurse (28.32±6.67), and organization (13.29±3.58) as shown in Tables 2, 3, and 4, respectively.
Among patient-related obstacles, the highest three barriers were religious issues of patients (3.01±0.49), confidentiality concerns (2.92±0.55), and the reluctance of patients to discuss sexual subjects (2.87±0.54) (Table 2).
Among nurse-related obstacles, the three barriers with the highest mean were high workload (2.92±0.42), cultural beliefs of the nurse (2.82±0.51), and lack of comfortability discussing sexual issues (2.79±0.50) (Table 3).
Also, the three barriers with the highest mean among organization-related variables were administrative lack of support (2.81±0.47), lack of feedback mechanism on sexual counseling (2.77±0.51), and environment is unsuitable for consultation (2.76±0.53) (Table 4).
Discussion
The nurse’s active participation in post-MI sexual counseling forms a crucial part of comprehensive patient care because heart attacks can yield both physical and psychological effects. Engaging in sexual activity after a heart attack may pose significant dangers; thus, the guidance provided by nurses is essential for patients. This guidance equips them to make informed decisions about their sexual health with their partners after such an event (Hyde et al., 2020).
The findings of this study show that the religious issues of patients, confidentiality concerns, and the reluctance of patients to discuss sexual subjects are the three with the highest mean score among patient-related barriers. Among the nurse-related barriers, high workload, cultural beliefs of the nurse, and lack of comfortability discussing sexual issues have the highest mean score. Also, the three barriers with the highest mean score among organization-related barriers were administrative lack of support, lack of feedback mechanism on sexual counseling, and unsuitable environment for consultation.
Our findings showed that patient-related barriers had the highest impact. Individuals’ views on sexuality are influenced by their religious beliefs and values, which in turn affect their openness towards such consultations, particularly concerning premarital sex or marital roles. Studies by Rahnavardi et al. (2022) and Mangolian Shahrbabaki et al., (2021) highlight how certain religious convictions can create significant barriers post-MI when it comes to seeking or initiating conversations about sexual health. Further complicating matters is the potential conflict between advice from medical professionals and directives issued by influential figures within various faith communities, a situation where patients may find themselves torn between divergent (Alomair et al., 2020).
Numerous challenges confront the revelation of sexual health information in Islamic countries, including stigmas linked to discussions about sexuality, premarital relationships, and reproductive health, forming a culture of silence. Fear, notably fear of judgment, social ostracization, and perceived moral transgressions, frequently dissuade individuals from seeking or providing crucial information regarding their sexual wellbeing (Rassool et al., 2020). A burgeoning acknowledgment of the imperative to confront sexual health issues in Islamic nations persists. Emerging initiatives and blending modern healthcare practices with Islamic values strive to align cultural sensitivity and the critical need for sexual education (Cense et al., 2018).
Patients frequently hold anxieties and concerns about their sexual health, especially after experiencing an MI. The fear of judgment, embarrassment, and potential privacy breaches often effectively inhibit them from seeking assistance or starting discussions with healthcare professionals. Studies by Coffelt et al. (2021) and Pampati et al. (2019) underscore the significant role confidentiality concerns play as a substantial obstacle to revealing sexual health issues; this condition results in postponed diagnosis, insufficient treatment, and ultimately compromising wellbeing.
Sexual health concerns after MI necessitate essential communication between patients and their healthcare providers. Nonetheless, nurses might face obstacles in instigating discussions about sexual health, including personal discomfort, inadequate training, or apprehension regarding patient reactions (Steinke et al., 2013). The quality and depth of patient-nurse interactions can suffer under work overload. Nurses, constrained by limited time for each patient, may prioritize essential clinical information; however, discussions about more sensitive topics such as sexual health might be relegated. This prioritization could impede comprehensive post-MI care provision (Halter et al., 2017).
The provision of sexual counseling after MI can significantly be impacted by the intersection of cultural beliefs and nurses’ comfortability with discussing sexual issues. This condition may result in patients not receiving the necessary guidance, causing unmet needs, compromising their overall recovery and QoL (Abosetugn & Yehualashet, 2021; Arredondo, 2020).
Conversely, many healthcare organizations grapple with the integration of sexual counseling into their post-MI care protocols. The lack of standardized guidelines or specific protocols addressing sexual health often results in inconsistent provision of information and support (O’Connor et al., 2019). A study by Hoekstra et al. (2012) reveals that organizational barriers pose the most significant challenge for implementing effective sexual counseling. Many healthcare organizations may not integrate sexual counseling into the standard post-MI care protocol (Steinke et al., 2013). Administratively, they prioritize immediate medical interventions over recovery’s long-term psychological and emotional aspects. A lack of dedicated resources, trained personnel, and institutional policies for sexual counseling can impede effective addressment by healthcare providers of their patients’ intimate concerns (Hyde et al., 2020; Zwack et al., 2023).
It is imperative to create an encouraging environment for discussing sensitive topics, such as sexual health. Inadequate privacy, insufficient time during medical appointments, and an overall discomfort in addressing intimate concerns are among the factors that might contribute towards an unsuitable consultation environment, thus impeding effective sexual counseling (Tremayne & Norton, 2017).
Conclusion
This study highlights several critical barriers to sexual counseling for patients with MI. Addressing these barriers is crucial to ensure that patients receive the sexual healthcare they need. Interventions to address patient-related barriers could include educational programs to address religious beliefs and concerns about confidentiality, as well as creating a more open and supportive environment for discussing sexual issues. For nurses, training programs could be developed to help them overcome cultural barriers and feel more comfortable discussing sexual health. Finally, organizations could provide more administrative support, implement feedback mechanisms to monitor the quality of sexual counseling services, and create more suitable consultation environments. Future research should look into understanding patient perspectives, developing and evaluating interventions, measuring and improving counseling service quality, and focusing on specific subgroups (i.e. differences between genders). Qualitative research can also clarify the different dimensions and factors of sexual counseling in these patients.
This study has some limitations. First, it is based on self-reported data, which may be subject to bias. Second, the study design does not explore the underlying reasons, and an interventional study would have a greater effect in eliminating the barriers. Third, the results of this study may be generalized with caution due to the limited sample size. Finally, the barriers are only from nurses’ views, not those of patients themselves.
Ethical Considerations
Compliance with ethical guidelines
Each participant was provided with informed consent, indicating whether they would like to participate in the current study. Also, formal ethical approval was received from the Dhi-Qar Health Directorate/Council of Ethics (Code: 1372) on 13/2/2023. Anonymity was strictly assured during the researcher’s data handling due to the study subject’s sensitivity.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All of the authors have contributed to different aspects of the study (such as conception and design, data collection and analysis, drafting the manuscript, etc.). The final version of the manuscript was approved by all the authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors especially thank Mansooreh Azzizadeh Forouzi for her tremendous help. The authors also sincerely thank the nurses for their efforts and valuable time.
References
Myocardial infarction (MI), also known as a heart attack, poses a potentially fatal threat and exerts a significant negative impact on the physical and mental health of an individual (Jacquet‐Smailovic et al., 2021). MI substantially impacts intimacy and sexual function; however, post-MI care frequently overlooks the crucial aspect of sexual health (Smith, 2020). Cardiac rehabilitation heavily relies on sexual counseling to aid MI patients in addressing their intimate issues; this call not only nurtures healthy sexual activity but also enhances the overall quality of life (QoL) for these individuals (Park et al., 2023).
A heart attack may cause a variety of concerns, such as fear, worry, depression, and resentment in a person. Meanwhile, the potential of sexual activity to intensify these emotional responses is significant (Karki & Mahara, 2022). Physical restrictions, the threat of another heart attack, or strain on their cardiovascular system could be among the concerns that individuals harbor. Emotional variables potentially induce a reluctance towards sexual activity, strain relationships, and diminish overall QoL (Rashed et al., 2020). Consequently, it becomes crucial to comprehend the psychological impacts of MI and proactively address them through supportive sexual counseling (Karani & McLuskey, 2020).
Sexual counseling provides individuals and couples who have experienced an MI with the necessary direction, information, and encouragement to overcome both mental and physical hurdles, thus playing an integral role in their recovery (Mangolian Shahrbabaki et al., 2021). Professionals endowed with specific training, such as sex therapists or counselors, can then step forward to address particular issues, respond effectively to inquiries, and provide a secure environment for candid discussions about personal problems. The overarching objectives of this form of therapy involve empowering people, reducing anxiety levels, enhancing communication not only within relationships but also internally, and, most importantly, aiding in the creation of coping mechanisms that facilitate adjustment post-heart attack (Özlem & Hatice, 2022).
Despite its value, sexual counseling is still underutilized for MI patients due to a multitude of organizational, patient, and healthcare provider-related barriers (Bachmann et al., 2022). Comprehending these challenges becomes crucial to enhancing procedures in sexual counseling and optimizing the results of MI patients’ sexual health (Fennell & Grant, 2019).
In the realm of literature, a myriad of obstacles often stands as potential challenges for organizations. These challenges may include the absence of standardized protocols and guidelines, insufficient resources and support, or even issues within healthcare providers themselves, such as inadequate training in sexual counseling coupled with intense clinical practice. However, there is another factor, the patients themselves, whose concerns can range from fear of physical activity to cultural conventions that affect their readiness to discuss sexual issues due to religious beliefs (Gazestani et al., 2019; Mangolian Shahrbabaki et al., 2021; Karani & McLuskey, 2020; Simeone et al., 2020; Sadatinejad et al., 2021).
Islamic teachings pose a challenge for clients seeking sexual counseling due to the prohibition of discussing sex with non-marital partners; however, this ban may be allowed in therapeutic contexts (Akhu-Zaheya & Masadeh, 2015). Islam not only encourages the enjoyment of sex and emphasizes meeting one’s partner’s needs in monogamous marriages but also strictly prohibits any extramarital sexual activity. However, Islamic regulations’ limited stance on sexual matters can potentially give rise to contextual sexual difficulties. Also, diverse Muslim communities and various other variables hold contrasting personal interpretations of Islamic teachings: These interpretations subsequently guide their daily activities (Sungur & Bez, 2016). To the researcher’s knowledge, no previous studies have discussed this subject among cardiac patients in Iraq. So, this study aims to investigate barriers to sexual counseling for patients with MI from the nurses’ viewpoints.
Materials and Methods
Design, setting, and sample
A cross-sectional study was conducted from March 2 to November 29, 2023. As sample size estimation is usually irrelevant when using non-probability sampling (Althubaiti, 2022), 126 nurses were recruited through convenient sampling; the response rate was about 89%. The subjects were recruited from different departments of Al-Nasiriyah Heart Center, the only specialized center for treating and caring for individuals with cardiovascular problems in Dhi-Qar Governorate.
Data collection
The questionnaire was adapted from (Mangolian Shahrbabaki et al., 2021) with permission. It consists of two parts. Part one includes 7 items related to demographic and background information (age, sex, marital status, educational level, department, job experience, and taking courses involving sexual counseling).
Part two includes 30 items that have been organized down into three categories: Barriers related to patients (13 items), barriers related to nurses (12 items), and barriers related to organizations (5 items). A 3-point rating scale (agree=3, no idea=2, and disagree=1) was utilized to score the items. The researcher used the mean score, where “one” represented the lowest possible score and “three” the maximum; higher scores indicate a higher perception level of the barriers. In this study, the original English questionnaire was used, and it was not translated into Arabic because all nurses from all educational levels have completed their nursing studies in English. The content validity index of the main questionnaire was 0.80, and its content validity ratio was 0.79. The Cronbach α coefficient was 0.78 for the total scale, 0.79 for the patient-related barriers, 0.83 for nurse-related barriers, and 0.79 for the organizational barriers (Mangolian Shahrbabaki et al., 2021). In this study, the questionnaire was reviewed by a panel of 7 experts (1 psychologist, 1 cardiologist, 1 from the Human Resources Department at Dhi-Qar Health Directorate, and 3 cardiovascular nurses) with more than 10 years of experience in their respective fields. The item level content validity index was 0.83, and the scale level content validity index was 0.80, while the coefficient of variation ratio was equal to 0.79. The Cronbach α was used to examine the questionnaire’s reliability, and the results showed a correlation coefficient of 0.83 for the entire scale, 0.82 for the barriers related to patient, 0.76 for barriers related to nurse, and 0.79 for the barriers related to organization.
Statistical analyses
The data collected during this study were analyzed using SPSS software, version 27. Descriptive statistics included frequency, percentage, mean, and standard deviation. ANOVA and independent t test were used to assess the mean score of the barriers in terms of demographic variables. P≤0.05 were determined as significant.
Results
Table 1 shows that the majority of nurses were females (53.2%), married (46.8%), had BS in nursing (48.4%), working in medical and surgical wards (57.9%), and did not take any courses in sexual counseling (97.6%). The Mean±SD age of nurses was 26.41±4.21 years, with a Mean±SD experience of 5.20±1.06 years.
The highest mean scores concerning barriers to sexual counseling in patients with MI were related to patient (31.78±7.84), nurse (28.32±6.67), and organization (13.29±3.58) as shown in Tables 2, 3, and 4, respectively.
Among patient-related obstacles, the highest three barriers were religious issues of patients (3.01±0.49), confidentiality concerns (2.92±0.55), and the reluctance of patients to discuss sexual subjects (2.87±0.54) (Table 2).
Among nurse-related obstacles, the three barriers with the highest mean were high workload (2.92±0.42), cultural beliefs of the nurse (2.82±0.51), and lack of comfortability discussing sexual issues (2.79±0.50) (Table 3).
Also, the three barriers with the highest mean among organization-related variables were administrative lack of support (2.81±0.47), lack of feedback mechanism on sexual counseling (2.77±0.51), and environment is unsuitable for consultation (2.76±0.53) (Table 4).
Discussion
The nurse’s active participation in post-MI sexual counseling forms a crucial part of comprehensive patient care because heart attacks can yield both physical and psychological effects. Engaging in sexual activity after a heart attack may pose significant dangers; thus, the guidance provided by nurses is essential for patients. This guidance equips them to make informed decisions about their sexual health with their partners after such an event (Hyde et al., 2020).
The findings of this study show that the religious issues of patients, confidentiality concerns, and the reluctance of patients to discuss sexual subjects are the three with the highest mean score among patient-related barriers. Among the nurse-related barriers, high workload, cultural beliefs of the nurse, and lack of comfortability discussing sexual issues have the highest mean score. Also, the three barriers with the highest mean score among organization-related barriers were administrative lack of support, lack of feedback mechanism on sexual counseling, and unsuitable environment for consultation.
Our findings showed that patient-related barriers had the highest impact. Individuals’ views on sexuality are influenced by their religious beliefs and values, which in turn affect their openness towards such consultations, particularly concerning premarital sex or marital roles. Studies by Rahnavardi et al. (2022) and Mangolian Shahrbabaki et al., (2021) highlight how certain religious convictions can create significant barriers post-MI when it comes to seeking or initiating conversations about sexual health. Further complicating matters is the potential conflict between advice from medical professionals and directives issued by influential figures within various faith communities, a situation where patients may find themselves torn between divergent (Alomair et al., 2020).
Numerous challenges confront the revelation of sexual health information in Islamic countries, including stigmas linked to discussions about sexuality, premarital relationships, and reproductive health, forming a culture of silence. Fear, notably fear of judgment, social ostracization, and perceived moral transgressions, frequently dissuade individuals from seeking or providing crucial information regarding their sexual wellbeing (Rassool et al., 2020). A burgeoning acknowledgment of the imperative to confront sexual health issues in Islamic nations persists. Emerging initiatives and blending modern healthcare practices with Islamic values strive to align cultural sensitivity and the critical need for sexual education (Cense et al., 2018).
Patients frequently hold anxieties and concerns about their sexual health, especially after experiencing an MI. The fear of judgment, embarrassment, and potential privacy breaches often effectively inhibit them from seeking assistance or starting discussions with healthcare professionals. Studies by Coffelt et al. (2021) and Pampati et al. (2019) underscore the significant role confidentiality concerns play as a substantial obstacle to revealing sexual health issues; this condition results in postponed diagnosis, insufficient treatment, and ultimately compromising wellbeing.
Sexual health concerns after MI necessitate essential communication between patients and their healthcare providers. Nonetheless, nurses might face obstacles in instigating discussions about sexual health, including personal discomfort, inadequate training, or apprehension regarding patient reactions (Steinke et al., 2013). The quality and depth of patient-nurse interactions can suffer under work overload. Nurses, constrained by limited time for each patient, may prioritize essential clinical information; however, discussions about more sensitive topics such as sexual health might be relegated. This prioritization could impede comprehensive post-MI care provision (Halter et al., 2017).
The provision of sexual counseling after MI can significantly be impacted by the intersection of cultural beliefs and nurses’ comfortability with discussing sexual issues. This condition may result in patients not receiving the necessary guidance, causing unmet needs, compromising their overall recovery and QoL (Abosetugn & Yehualashet, 2021; Arredondo, 2020).
Conversely, many healthcare organizations grapple with the integration of sexual counseling into their post-MI care protocols. The lack of standardized guidelines or specific protocols addressing sexual health often results in inconsistent provision of information and support (O’Connor et al., 2019). A study by Hoekstra et al. (2012) reveals that organizational barriers pose the most significant challenge for implementing effective sexual counseling. Many healthcare organizations may not integrate sexual counseling into the standard post-MI care protocol (Steinke et al., 2013). Administratively, they prioritize immediate medical interventions over recovery’s long-term psychological and emotional aspects. A lack of dedicated resources, trained personnel, and institutional policies for sexual counseling can impede effective addressment by healthcare providers of their patients’ intimate concerns (Hyde et al., 2020; Zwack et al., 2023).
It is imperative to create an encouraging environment for discussing sensitive topics, such as sexual health. Inadequate privacy, insufficient time during medical appointments, and an overall discomfort in addressing intimate concerns are among the factors that might contribute towards an unsuitable consultation environment, thus impeding effective sexual counseling (Tremayne & Norton, 2017).
Conclusion
This study highlights several critical barriers to sexual counseling for patients with MI. Addressing these barriers is crucial to ensure that patients receive the sexual healthcare they need. Interventions to address patient-related barriers could include educational programs to address religious beliefs and concerns about confidentiality, as well as creating a more open and supportive environment for discussing sexual issues. For nurses, training programs could be developed to help them overcome cultural barriers and feel more comfortable discussing sexual health. Finally, organizations could provide more administrative support, implement feedback mechanisms to monitor the quality of sexual counseling services, and create more suitable consultation environments. Future research should look into understanding patient perspectives, developing and evaluating interventions, measuring and improving counseling service quality, and focusing on specific subgroups (i.e. differences between genders). Qualitative research can also clarify the different dimensions and factors of sexual counseling in these patients.
This study has some limitations. First, it is based on self-reported data, which may be subject to bias. Second, the study design does not explore the underlying reasons, and an interventional study would have a greater effect in eliminating the barriers. Third, the results of this study may be generalized with caution due to the limited sample size. Finally, the barriers are only from nurses’ views, not those of patients themselves.
Ethical Considerations
Compliance with ethical guidelines
Each participant was provided with informed consent, indicating whether they would like to participate in the current study. Also, formal ethical approval was received from the Dhi-Qar Health Directorate/Council of Ethics (Code: 1372) on 13/2/2023. Anonymity was strictly assured during the researcher’s data handling due to the study subject’s sensitivity.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All of the authors have contributed to different aspects of the study (such as conception and design, data collection and analysis, drafting the manuscript, etc.). The final version of the manuscript was approved by all the authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors especially thank Mansooreh Azzizadeh Forouzi for her tremendous help. The authors also sincerely thank the nurses for their efforts and valuable time.
References
Abosetugn, A. E. & Yehualashet, S. S., 2021. Estimate the burden of sexual dysfunction due to non-communicable diseases in Ethiopia: Systematic review and meta-analysis. Plos One, 16(10), pp. e0258938. [DOI:10.1371/journal.pone.0258938] [PMID]
Akhu-Zaheya, L. M. & Masadeh, A. B., 2015. Sexual information needs of Arab-Muslim patients with cardiac problems. European Journal of Cardiovascular Nursing, 14(6), pp. 478–85.[DOI:10.1177/1474515115597353] [PMID]
Alomair, N., et al., 2020. Factors influencing sexual and reproductive health of Muslim women: A systematic review. Reproductive Health, 17(1), pp. 33. [DOI:10.1186/s12978-020-0888-1] [PMID]
Althubaiti A., 2022. Sample size determination: A practical guide for health researchers. Journal of General and Family Medicine, 24(2), pp. 72-8. [DOI:10.1002/jgf2.600] [PMID]
Arredondo, E., 2020. Cultural competence. In: M. D. Gellman, (Ed), Encyclopedia of behavioral medicine (pp. 582-584). Cham: Springer. [DOI:10.1007/978-3-030-39903-0_172]
Bachmann, G., et al., 2022. Myocardial infarction: Need for sexual counseling for both partners. The Journal of Sexual Medicine, 19(Issue Supplement_3), pp. S38-9. [DOI:10.1016/j.jsxm.2022.05.129]
Cense, M., de Neef, M. & Visscher, W., 2018. Culture, religion and sexual and reproductive health & rights. New Jersey: Rutgers. [Link]
Coffelt, T. A., Ritland, R. & LeFebvre, L., 2021. Revealing and receiving sexual health information. Health Communication, 36(2), pp. 136-45. [DOI:10.1080/10410236.2019.1669128]
Fennell, R. & Grant, B., 2019. Discussing sexuality in health care: A systematic review. Journal of Clinical Nursing, 28, pp. 3065-76. [DOI:10.1111/jocn.14900]
Gazestani, T., et al., 2019. Sexual counseling to patients with myocardial infarction: Nurses’ performance, responsibility and confidence. Nursing Practice Today. [DOI:10.18502/npt.v6i4.1943]
Halter, M., et al., 2017. The determinants and consequences of adult nursing staff turnover: A systematic review of systematic reviews. BMC Health Services Research, 17(1), pp. 824.[DOI:10.1186/s12913-017-2707-0] [PMID]
Hoekstra, T., et al., 2012. What keeps nurses from the sexual counseling of patients with heart failure? Heart & Lung, 41(5), pp. 492–9. [DOI:10.1016/j.hrtlng.2012.04.009] [PMID]
Hyde, E. K., Martin, D. E. & Rieger, K. L., 2020. Factors shaping the provision of sexual health education for adults with acute coronary syndrome: A scoping review. Patient Education and Counseling, 103(5), pp. 877–87. [DOI:10.1016/j.pec.2019.11.017] [PMID]
Jacquet-Smailovic, M., et al., 2021. Posttraumatic stress disorder following myocardial infarction: A systematic review. Journal of Traumatic Stress, 34(1), pp. 190–9. [DOI:10.1002/jts.22591] [PMID]
Karani, S. & McLuskey, J., 2020. Facilitators and barriers for nurses in providing sexual education to myocardial-infarction patients: A qualitative systematic review. Intensive and Critical Care Nursing, 58, pp. 102802. [DOI:10.1016/j.iccn.2020.102802] [PMID]
Karki, M., & Mahara, G., 2022. Heart diseases, anxiety disorders, and negative thoughts. Heart and Mind, 6(1), pp. 22-5. [DOI:10.4103/hm.hm_45_21]
Mangolian Shahrbabaki, P., et al., 2021. Iranian nurses’ perspective of barriers to sexual counseling for patients with myocardial infarction. BMC Nursing, 20(196), pp. 1-8. [DOI:10.1186/s12912-021-00697-x]
O’'Connor, S. R., et al., 2019. Healthcare professional perceived barriers and facilitators to discussing sexual wellbeing with patients after diagnosis of chronic illness: A mixed-methods evidence synthesis. Patient Education and Counseling, 102(5), pp. 850–63. [DOI:10.1016/j.pec.2018.12.015] [PMID]
Özlem, D. & Hatice, K., 2022. Sexual activity after myocardial infarction: Systematic review. Güncel Hemşirelik Araştırmaları Dergisi, 2, pp. 70-83. [Link]
Pampati, S., et al., 2019. Confidentiality matters but how do we improve implementation in adolescent sexual and reproductive health care? The Journal of Adolescent Health, 65(3), pp. 315–22. [DOI:10.1016/j.jadohealth.2019.03.021] [PMID]
Park, J. J., et al., 2023. Effects of sexual rehabilitation on sexual dysfunction in patients with cardiovascular disease: A systematic review and meta-analysis. The World Journal of Men’s Health, 41(2), pp. 330–41. [DOI:10.5534/wjmh.220124] [PMID]
Rahnavardi, M., Bostani Khalesi, Z. & Rezaie-Chamani, S., 2022. Parents’ and experts’ views on the sexual health education of adolescent girls: A qualitative study. Sexual and Relationship Therapy, pp. 1-13. [DOI:10.1080/14681994.2022.2087870]
Rashed, M., et al., 2020. Cardiac rehabilitation: Future of heart health in Saudi Arabia, a perceptual view. World Journal of Cardiovascular Diseases, 10(9), pp. 666-77. [DOI:10.4236/wjcd.2020.109064]
Rassool, G. H., et al., 2020. Sexuality education from an Islamic perspective. Newcastle: Cambridge Scholars Publishing. [Link]
Mohsen Sadatinejad, S., et al., 2021. The effect of sexual counseling on depression, anxiety, stress, sexual knowledge and sexual quality of life in men who have undergone invasive coronary interventions: An RCT. International Journal of Reproductive Biomedicine, 19(11), pp. 969–78. [PMID]
Simeone, S., et al., 2020. Sexual health after acute myocardial infarction: The lived experience of women during the first-year post discharge. Sexuality and Disability, 38, pp. 547-60. [DOI:10.1007/s11195-020-09627-2]
SMITH, A., 2020. Exploratory description and longitudinal modeling of predictors of sexual function and satisfaction post-myocardial infarction. [PhD dissertation]. Michigan: University of Michigan. [Link]
Steinke, E. E., et al., 2013. Sexual counselling for individuals with cardiovascular disease and their partners: A consensus document from the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP). European Heart Journal, 34(41), pp. 3217–35.[DOI:10.1093/eurheartj/eht270] [PMID]
Sungur, M. Z. & Bez, Y., 2016. Cultural factors in the treatment of sexual dysfunction in Muslim clients. Current Sexual Health Reports, 8, pp. 57-63. [DOI:10.1007/s11930-016-0068-z]
Type of Study: Research |
Subject:
General
Received: 2024/03/5 | Accepted: 2024/06/1 | Published: 2024/11/1
Received: 2024/03/5 | Accepted: 2024/06/1 | Published: 2024/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






