Tue, Jul 22, 2025
[Archive]
Volume 10, Issue 4 (Autumn 2024)
JCCNC 2024, 10(4): 297-306 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tavani F M, Rahmani P, Behshid M, Sheikhalipour Z, Zadi O. Professional Autonomy and Its Relationship With Patient Safety Competency Among Nurses. JCCNC 2024; 10 (4) :297-306
URL: http://jccnc.iums.ac.ir/article-1-604-en.html
URL: http://jccnc.iums.ac.ir/article-1-604-en.html
1- Department of Medical-Surgical Nursing, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran.
2- Tabriz Health Services Management Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
3- Department of Operating Room Technology, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran. ,omid.zd.axule73@gmail.com
2- Tabriz Health Services Management Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
3- Department of Operating Room Technology, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran. ,
Full-Text [PDF 973 kb]
(502 Downloads)
| Abstract (HTML) (1569 Views)
Full-Text: (426 Views)
Introduction
Service delivery systems led by nurses can play a significant role in decision-making, planning, and the process of prevention, care, and referral to a doctor in the care team. When nurses manage and plan these services on a broad scale, their professional independence is increased (Choi & De Gagne, 2016). Professional autonomy is a critical component of the nursing profession (Ko et al., 2018). In other words, professionalization in nursing is impossible without attaining professional autonomy (Pursio et al., 2021).
Professional autonomy has been defined as the level of authority that individuals possess in making decisions on a specific action (Hung et al., 2013). With the development of the nursing profession, the professional responsibilities of nurses have increased. Hence, nurses require autonomy in their activities. Professional autonomy is a vital constituent of self-motivation, enabling nurses to make timely decisions at the patient’s bedside (Mirzaei & Nasrabadi, 2021). The higher levels of autonomy in the workplace predict the retention of nurses in the profession, job satisfaction, and safety performance (Koak et al., 2023). However, decreasing autonomy levels can increase nursing attrition (Nouri et al., 2017).
A research literature review indicates contradictory findings regarding the extent to which nurses have professional autonomy. A study in Iran reported high levels of professional autonomy among nurses (Mirzaei & Nasrabadi, 2021). However, another study in Iran reported low levels of professional autonomy among nurses (Abdolmaleki et al., 2019). When nurses have high degrees of professional autonomy, their supervisors provide them with support, trust, and respect, enhancing their credibility, communication, and coordination (Labrague et al., 2019). Low levels of professional autonomy can cause negative emotions such as dissatisfaction, a lack of commitment, demotivation, burnout, and depression among nurses (Labrague et al., 2019). Nurses should comprehend their levels of professional autonomy in the workplace, as it directly impacts their competency in ensuring patient safety. This competency pertains to the knowledge, skills, and attitudes related to patient safety (Han & Roh, 2020).
As the largest professional group in the health care system, nurses are responsible for providing 24-h patient care. Hence, a nurse’s competency is essential for patient safety and high-quality care (Han et al., 2020). The term “patient safety competency” is used in the literature to refer to nursing practices that “minimize risks to patients and providers through system effectiveness and individual performance” (Rizany et al., 2018).
The safety competency of nurses working in emergency settings in Iran was found to be relatively favorable (Najafi Ghezeljeh et al., 2022). The more people’s knowledge about patient safety in the workplace, the more positive their attitude and the higher their performance regarding patient safety (Memarbashi., 2020). The skill level of nurses in safety competence is reported to be low (Cho & Choi, 2018). This condition can harm patients, decrease the quality of care, increase re-hospitalization rates and costs, decline patient satisfaction, and ultimately higher patient mortality rates (Najafi Ghezeljeh et al., 2022).
Empowering nurses by granting professional independence increases their self-confidence and improves their ability to make decisions and act based on nursing diagnoses in certain situations (Rouhi Balasi et al., 2024). Furthermore, nurses’ patient safety competency assessment is crucial for ensuring patient safety, pinpointing enhancement areas, and identifying training requirements (Najafi Ghezeljeh et al., 2022).
Recognizing the significance of nurses’ independent performance and their competence in enhancing patient safety and care quality, the studies on nurses’ competence in patient safety in Iran are limited and contradictive, and in reviewing the extensive literature, no study was found that examines the relationship between these two variables. Therefore, the present study assessed professional autonomy and its association with patient safety competency among nurses in the hospitals affiliated with Tabriz University of Medical Sciences, Tabriz City, Iran.
Materials and Methods
This research is a descriptive-correlational study on nurses employed in educational, therapeutic hospitals affiliated with Tabriz University of Medical Sciences in Iran (Imam Reza, Sina, and Madani hospitals) in 2022. The Cochran formula was utilized to calculate the sample size. Since the total number of nurses in the studied hospitals was 360, a sample size of 185 was calculated, with a confidence level of 95% and the sampling accuracy (d) of 5%. Finally, 205 subjects were selected by considering a 10% sample attrition. Five participants were excluded from the study because they answered the questionnaires incompletely; hence, the final sample included 200 nurses. The subjects were selected by stratified random sampling. Hospitals affiliated with Tabriz University of Medical Sciences formed stratification classes, and random sampling was done in each stratification class using a table of random numbers.
The data collection tool comprised three parts. First, the demographic characteristics questionnaire of nurses included age, sex, marital status, work experience, educational level, and the type of work shift. Second is the professional autonomy questionnaire. It is an 18-item questionnaire that assesses nurses’ levels of professional autonomy in three dimensions: Knowledge (items 1-6), action (items 7-12), and value (items 13-18). Responses are scored on a 6-point Likert scale ranging from “strongly disagree” (1) to “strongly agree” (6). The scores on this scale ranged from 18 to 108, signifying low autonomy for scores between 18 and 47.99, medium autonomy for scores between 48 and 77.99, and high autonomy for scores between 78 and 108 (Varjus et al., 2003). Yeganeh et al. confirmed the high reliability of the Persian version of the questionnaire in their study with a Cronbach α of 0.99 and an intraclass correlation coefficient of 0.88 in a test re-test conducted over a 2-week interval in a pilot study involving 30 subjects (Yeganeh et al., 2019).
Using the whole sample in our study, the internal consistency of the questionnaire was measured using the Cronbach α coefficient, resulting in a value of 0.90. The third part is the patient safety competency self-evaluation questionnaire. This scale was designed by Lee et al. (2014) in Korea and consists of 41 items rated on a 5-point Likert scale. This instrument assesses three dimensions of patient safety: Knowledge, attitude, and skills, with 6 items measuring knowledge (score range: 6–30), 21 items measuring skills (score range: 21–105), and 14 items measuring attitude (score range: 14–70). The item scores are added up in each dimension. A higher score in each dimension indicates a greater level of that dimension. The total score ranges from 41 to 205, with the higher scores indicating higher competency in patient safety. The Cronbach α was 0.859 for the knowledge dimension, 0.794 for the attitude dimension, 0.912 for the skills dimension, and 0.907 for overall (Lee et al., 2014).
Moreover, Najafi Ghezeljeh et al. (2022) assessed the content validity of the Persian version of the questionnaire with three members from the Faculty of Nursing and Midwifery at Iran University of Medical Sciences. The reliability coefficients for knowledge, attitude, and skills dimensions were determined using Cronbach α, yielding values of 0.908, 0.836, and 0.922, respectively. Additionally, the total questionnaire demonstrated a reliability coefficient of 0.952. In this research, the internal consistency of the questionnaire in the studied population was measured using the Cronbach α coefficient, and its value was 0.93.
The inclusion criteria were willingness to participate in the study, a bachelor’s degree or higher, and possessing at least six months of working experience as a clinical nurse. The exclusion criteria included unwillingness to cooperate, nurses performing administrative or secretarial work, incomplete questionnaires (less than 90% of questions answered), and the same response to all questions. Eligible nurses were provided with the questionnaires after being informed of the research objectives and giving consent.
The data were analyzed using descriptive statistics (frequency, percentage, and median), the Mann-Whitney U test, the Kruskal-Wallis test, and the Kendall Tau and Spearman non-parametric correlation coefficients in SPSS software, version 26. The significance level was set as P<0.05.
Results
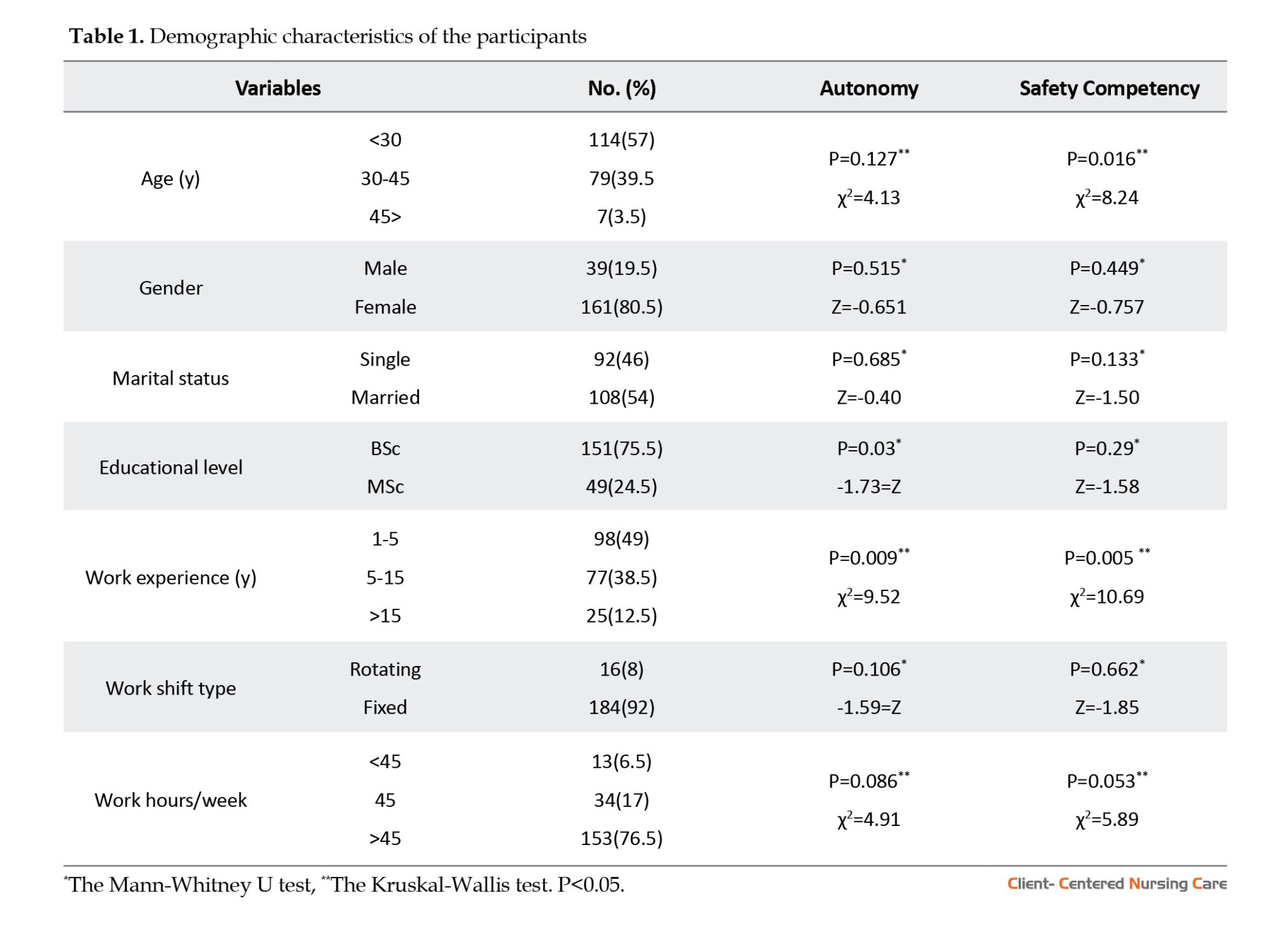
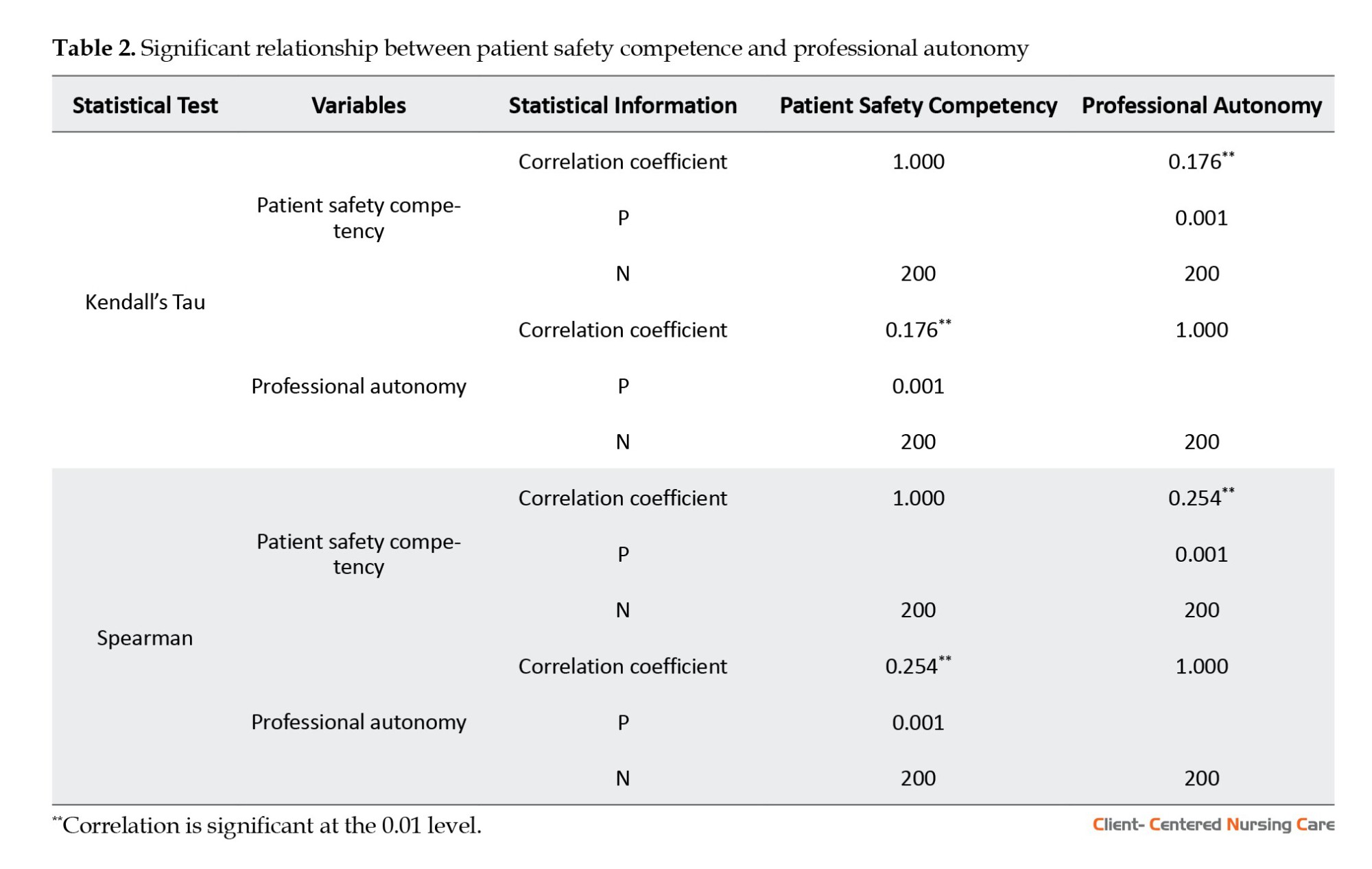
The research findings regarding demographics revealed that 161 nurses (80.5%) were females and 39(19.5%) were males. The majority of participants were married (54%) and held bachelor’s degrees (75.5%) (Table 1).
There were significant relationships between the median values of professional autonomy and work experience and also the level of nurses’ education (P<0.05) (Table 1).
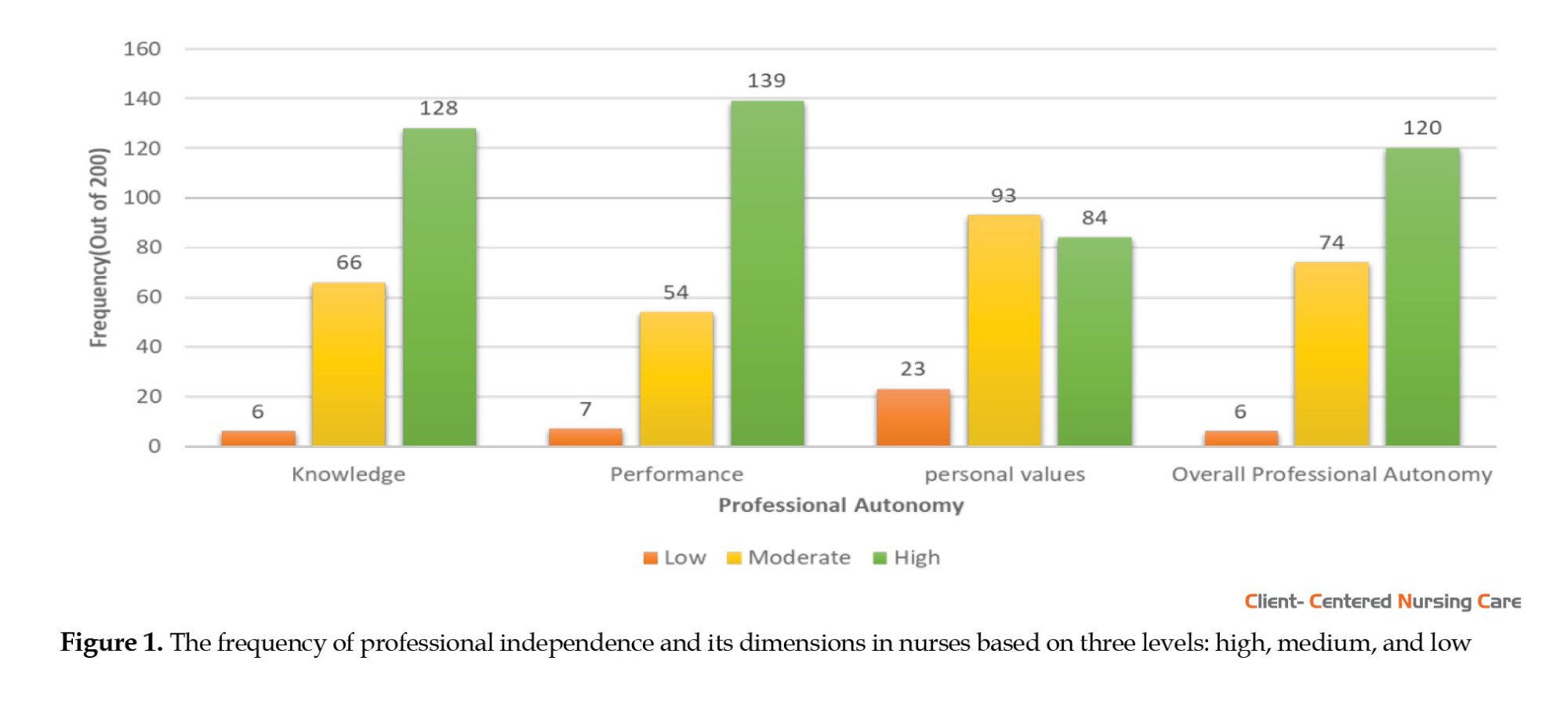
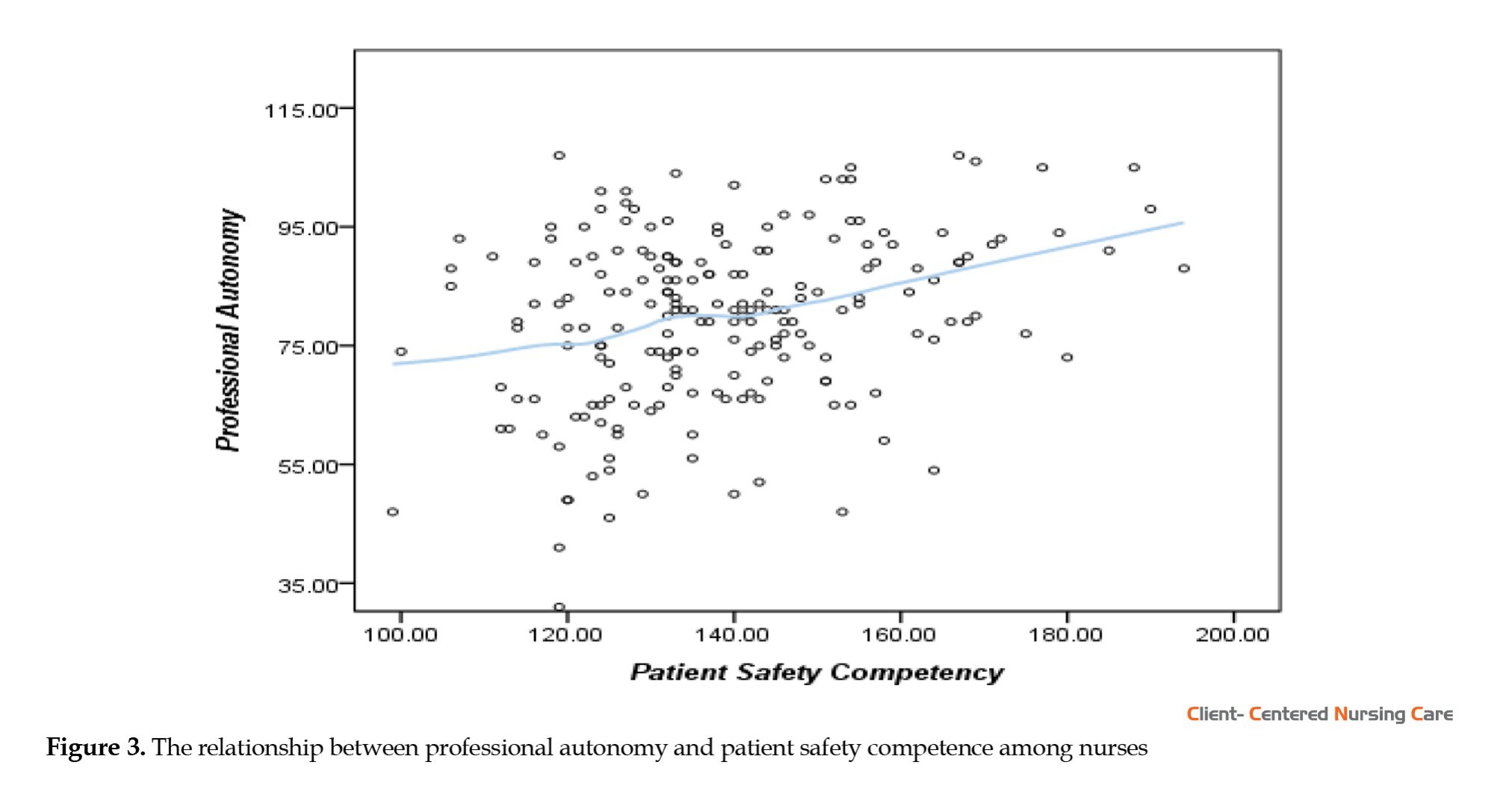
Findings concerning the nurses’ professional autonomy showed that 120(60%) experienced a high level of professional autonomy, 74(37%) had a medium level, and 6(3%) reported a low level of professional autonomy (Figure 1).
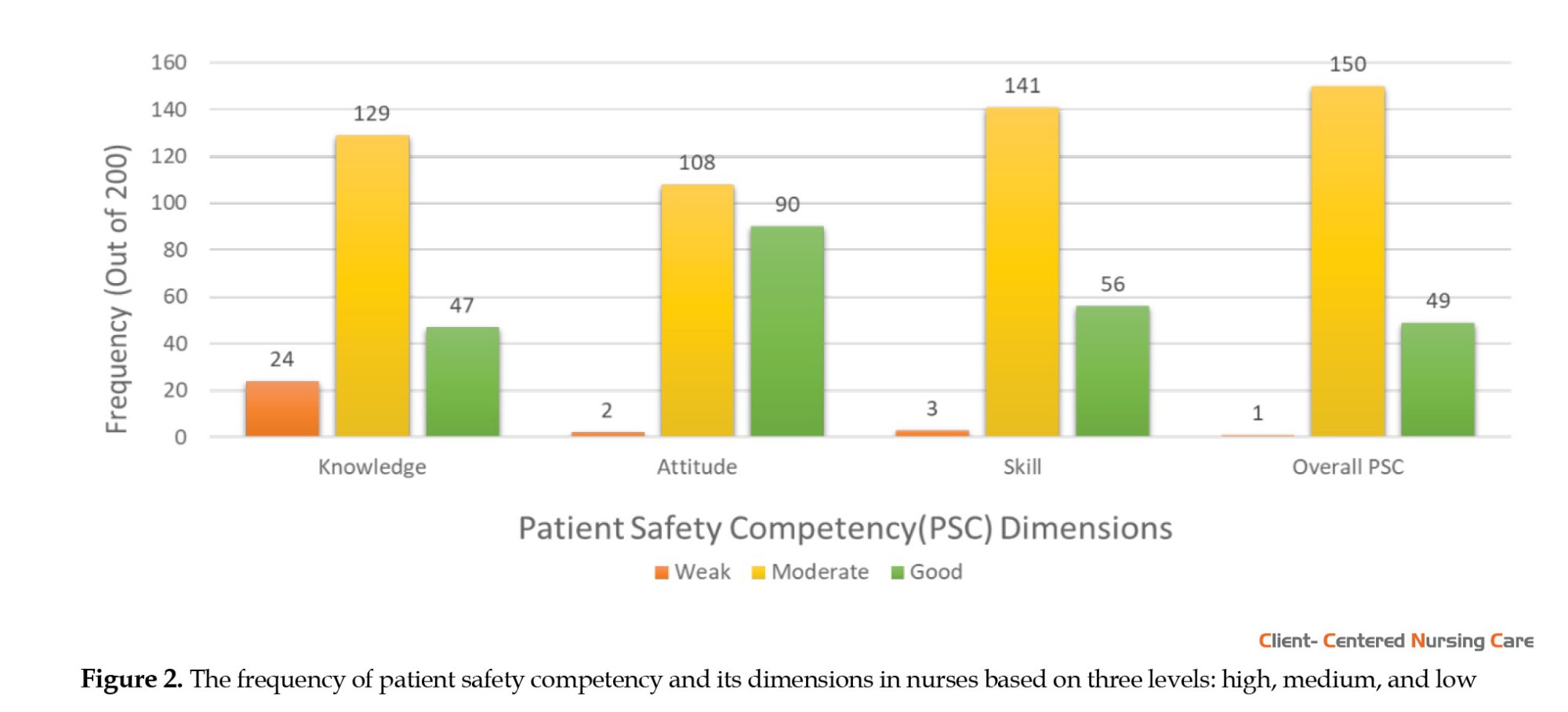
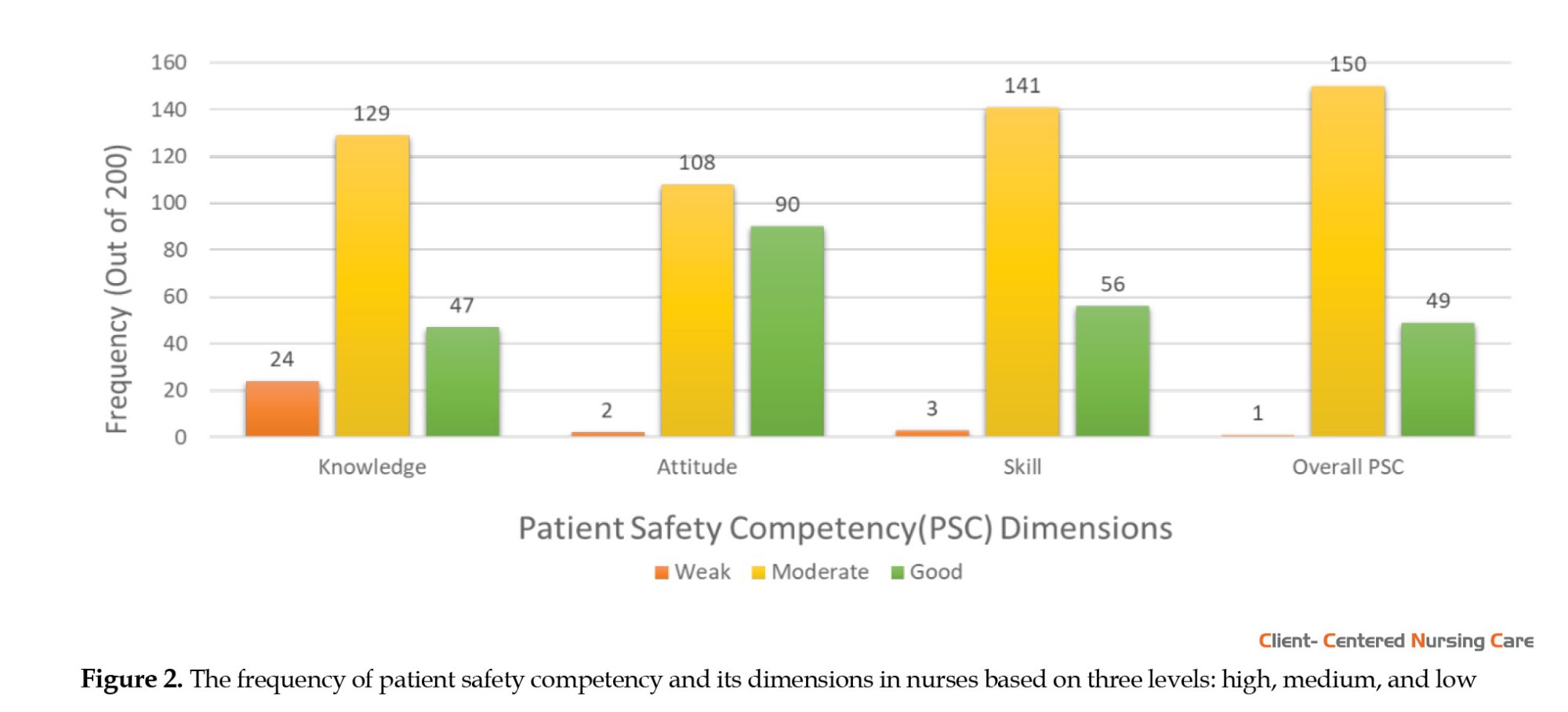
Out of 200 nurses who took part in the study, 49(24.5%) had good patient safety competency, whereas 150(75.0%) reported moderate competency, and only 1(0.5%) had a weak level of competency (Figure 2).
There were significant relationships between the median values of competency and the variables of work experience and age (P<0.05) (Table 1)
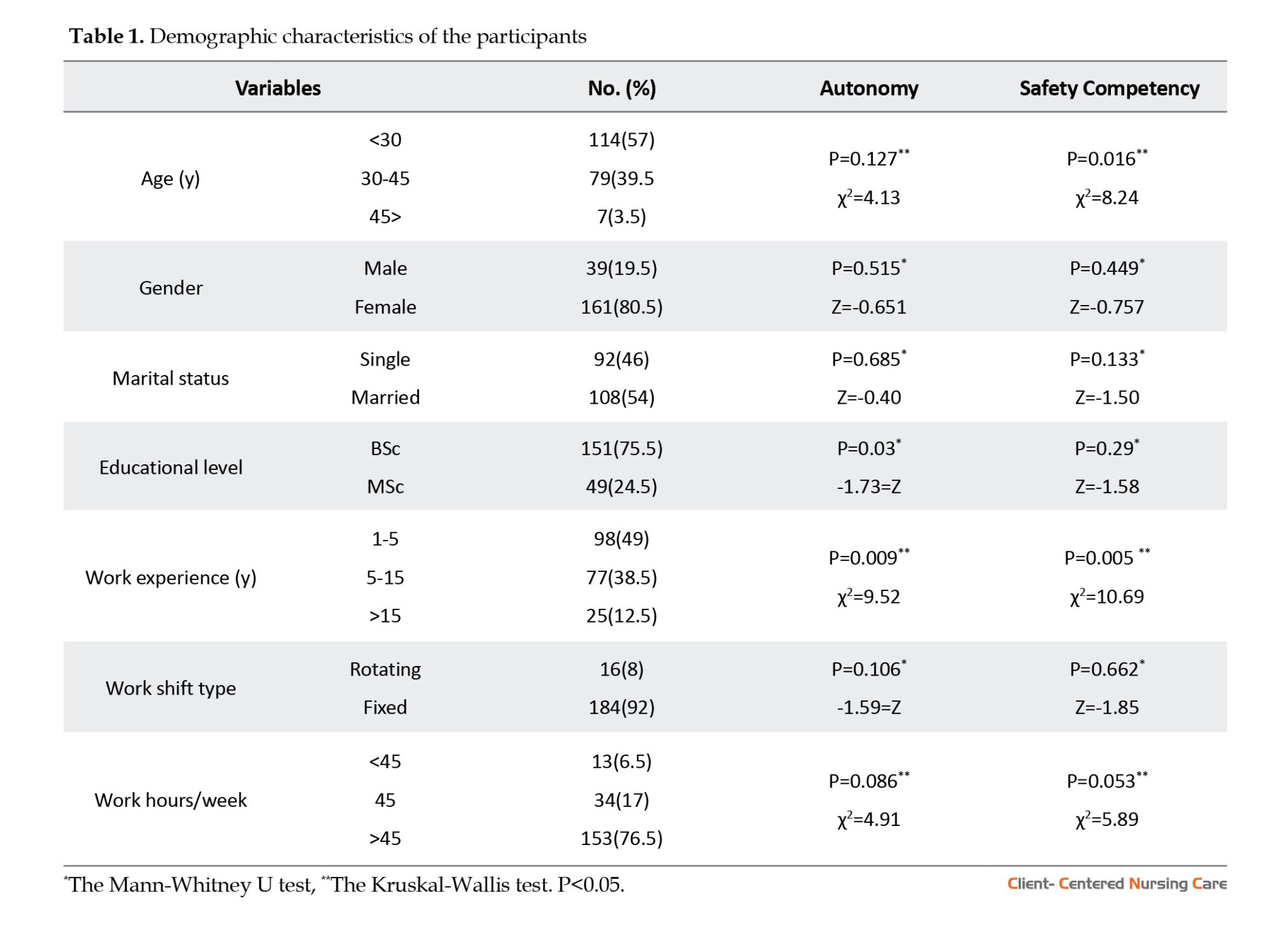
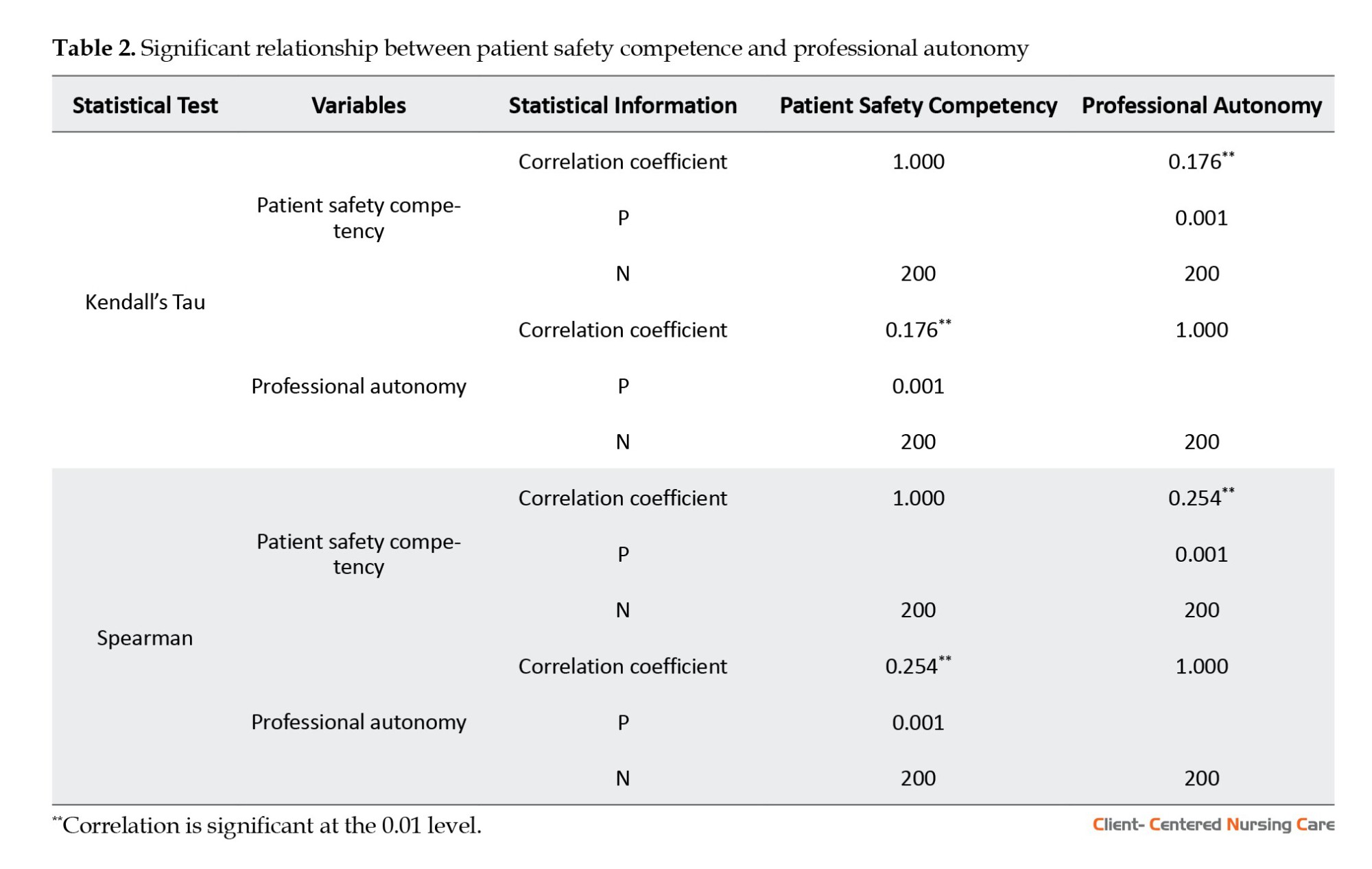
The Kolmogorov-Smirnov and Shapiro–Wilk tests indicated that neither of the variables under investigation (professional autonomy and patient safety competency) followed a normal distribution. Hence, the Kendall Tau and Spearman non-parametric correlation coefficients were employed to test the relationship between the two variables. The Kendall Tau and Spearman correlation coefficients were 0.176 and 0.254, respectively, indicating that an increase in nurses’ professional autonomy would correspond to an increase in their patient safety competency (P<0.001) (Table 2).
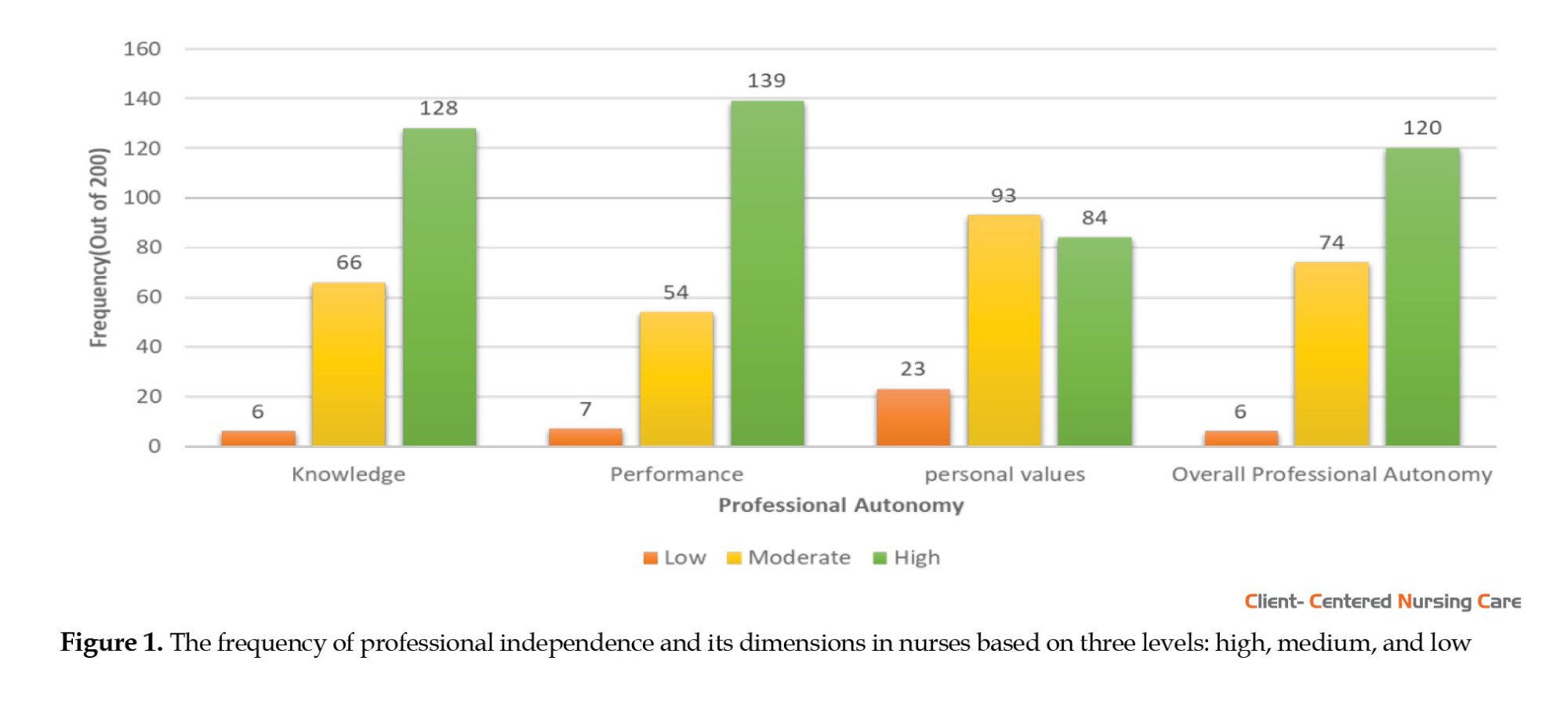
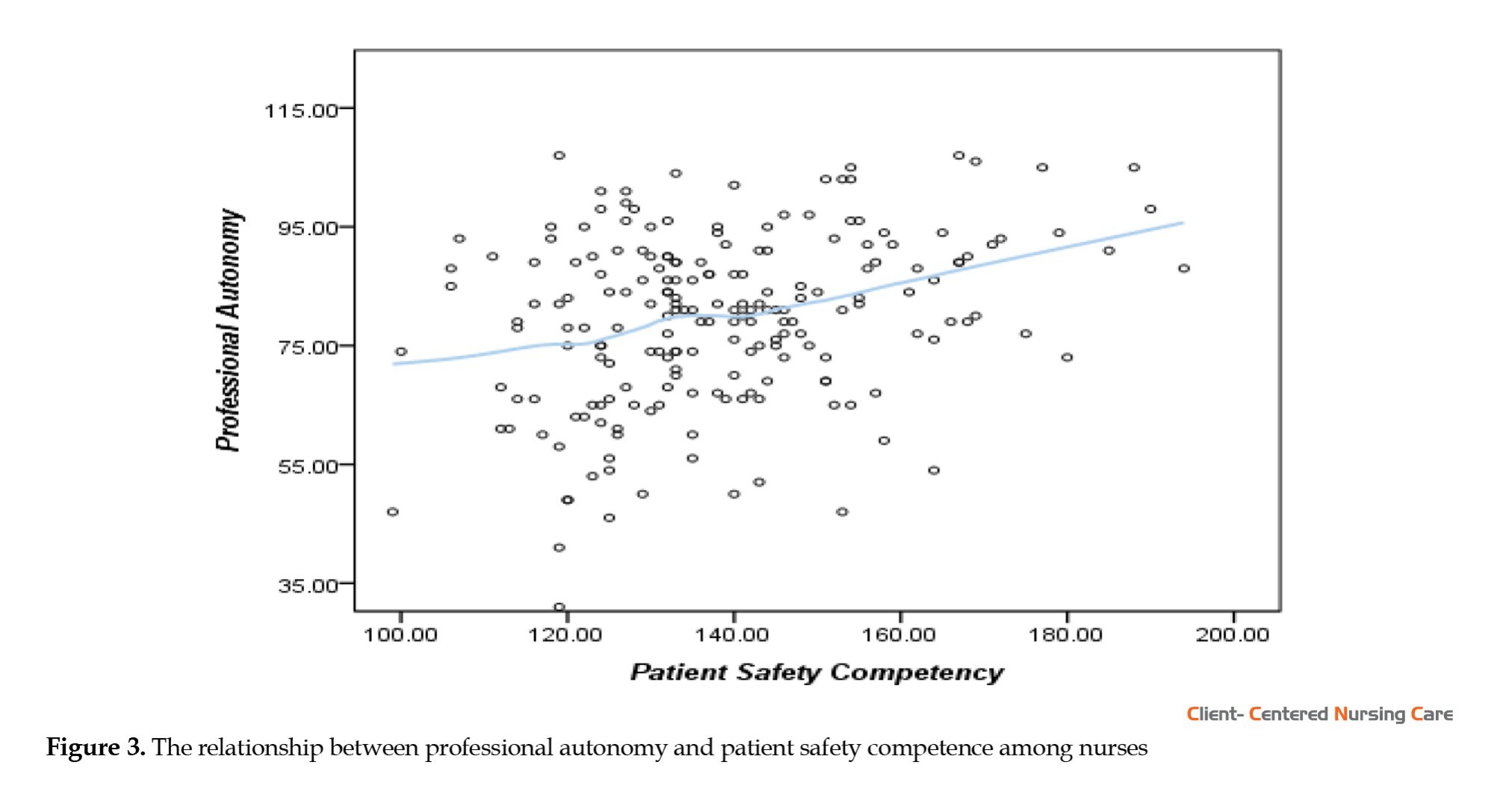
Scatter plots were drawn to examine the association between professional autonomy and patient safety competency, and a non-parametric Loess correlation curve was applied to the data. The chart illustrates that patient safety competency increased in line with professional autonomy among nurses (Figure 3).
Discussion
This study assessed the correlation between professional autonomy and patient safety competency among nurses in hospitals affiliated with Tabriz University of Medical Sciences, Iran. The findings show that most participants have experienced high professional autonomy. Professional autonomy can improve the power and ability of nurses. If nurses possess the authority to act autonomously, they can make decisions based on their judgment and select their preferred course of action (Paganini & Bousso, 2015). In line with the current research findings, nurses in Setoodegan et al. study also reported high levels of professional autonomy that allowed them to make independent decisions and make the nursing profession stronger (Setoodegan et al., 2019).
Oshodi et al. (2019) examined nurses’ views and encounters with autonomy, highlighting that clinical autonomy is a key aspect of professional autonomy in nursing and is intricately connected to decision-making in patient care. However, they acknowledged that in clinical practice, nurses also adhere to doctors’ orders and operate within the confines of established rules. Hence, absolute autonomy is impossible. Mirzaei & Nasrabadi, (2021) studied the professional autonomy among nurses working in intensive care units and other units in Iran. They observed that the level of professional autonomy was moderate in special units and low in general wards.
Contrary to the present study, another research reported low average scores for nurses’ professional autonomy (Abdolmaleki et al., 2019). Nevertheless, a study in Iran indicated that nurses’ professional autonomy was moderate (Iranmanesh et al., 2014). Filipino nurses also show moderate levels of professional autonomy (Labrague et al., 2019).
Aghamohammadi et al. (2019) assessed nurse-physician collaboration and nurses’ professional autonomy in the intensive care unit. The findings indicated that most nurses demonstrated a moderate level of professional autonomy.
Oshodi et al. (2019) highlighted that nurses’ professional autonomy is particularly evident during emergencies and when senior staff are absent. Hence, it should be noted that nurses may not always have professional autonomy in their practice, as the extent of their autonomy can vary depending on the specific circumstances. They believed nursing officials should establish and uphold conducive work environments to ensure nurses understand their expectations and responsibilities. Additionally, precise and concrete job descriptions for nurses and well-defined career plans can contribute significantly to their professional growth. In other words, if nurses’ authority is not expanded sufficiently, they cannot achieve autonomy. Organizational restrictions such as authoritarian management, ambiguous or rigid organizational rules, and lack of control over nurses’ performance prevent the realization of professional autonomy (AllahBakhshian et al., 2017).
There were notable connections between the professional autonomy of nurses and their levels of work experience and education. Consistent with the current study, Mirzaei & Nasrabadi, (2021) found that nurses’ professional autonomy had significant relationships with age, work experience, and education level. Labrague et al., (2019) observed that various individual and institutional factors, including age, education, experience, self-efficacy, professional role, empowerment, workload, type of hospital, ward, number of working nurses, and the presence of professional associations, have affected the professional autonomy of nurses.
The results of the current study show that most nurses demonstrated a moderate level of safety competency. According to Najafi Ghezeljeh et al., (2022), emergency nurses have a relatively high level of knowledge. Additionally, nurses’ skills, attitudes, and overall patient safety competency in the emergency department were reported to be relatively favorable. However, the patient safety competency of working nurses was rated as moderate in a study conducted by Hwang, (2015). Yan et al. (2021) evaluated the safety competency of nurses in China. According to their findings, nurses had a crucial role in ensuring patient safety. They also observed that the participants’ level of competency was moderate. Cho and Choi (2018) analyzed the variables related to nurses’ patient safety competency, eg, safety skills, attitude, and knowledge. They concluded that nurses were less skilled in safe practice.
The variation in results can be ascribed to the fact that most clinical nurses receive limited formal training in patient safety competency during their university education. Additionally, these findings can be elucidated by the culture of patient safety across different countries. Habibi et al. (2022) observed that emergency nurses prioritize patient-related emergency activities, whereas their understanding of patient safety is limited. Therefore, it is necessary to implement patient safety management activities, provide training, establish standardization, and address problems effectively.
There were notable correlations between the safety competency of nurses and their years of experience and age. It is believed that patient safety competency in nurses improves with age and years of experience (Najafi Ghezeljeh et al., 2022). A study found an association between patient safety knowledge and age and training experience in this field (Biresaw et al., 2020), and nurses with higher education levels demonstrated higher patient safety skills. Nurses with Master’s degrees or higher are more likely to encounter additional opportunities to learn patient safety-related subjects within their curricula. This, in turn, can enhance their confidence in implementing patient safety practices (Hwang, 2015).
The findings indicate that increased nurses’ professional autonomy improves patient safety competency. Professional autonomy refers to making independent decisions and taking responsibility for them. This authority is derived from professional knowledge and position (Hwang, 2015). An extensive literature review indicates a scarcity of studies analyzing the correlation between professional autonomy and patient safety competency. Lee et al. (2014) investigated the effect of the convergence of professional autonomy and nurses’ empathy on patient safety culture. According to their findings, professional autonomy was crucial to patient safety. Hwang, (2015) also reported a positive correlation between professional autonomy and patient safety management performance. Furthermore, Ko et al. (2018) concluded that professional autonomy was the sole structural factor affecting patient safety. Kurt and Gurdogan (2023) studied nurses’ professional autonomy and patient support levels. Their findings revealed that nurses possessed a high level of professional autonomy, and their utilization of patient support roles was above average.
Conclusion
The study results revealed that most nurses employed in educational-therapeutic hospitals of Tabriz University of Medical Sciences, Iran, had high levels of professional autonomy, whereas their patient safety competency was moderate. Nurses must understand their levels of professional autonomy in the workplace and the opportunities it provides for independent work. It also maximizes their care abilities and concern for safety performance, encouraging them to comply with patient safety standards. This directly impacts their competency in patient safety, ultimately leading to quality care provision.
The roles of nurses are evolving. This evolution will help guarantee the ongoing promotion of nurses’ autonomy and patient safety competency in ensuring patient safety. Therefore, given the significance of autonomy within the nursing community, assessing the current state of professional autonomy in nursing and its correlation with patient safety competency is essential. Findings from such studies can provide insights for hospital managers and health policymakers in identifying the strategies that will enhance the autonomy of nurses.
This study assessed nurses’ safety competence using a self-report questionnaire. Other research studies may utilize different methods, such as clinical observation and patient interactions, to evaluate nurses’ behaviors. Furthermore, this cross-sectional study does not allow for causal inferences. Thus, caution should be exercised when generalizing the results.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Ethics Committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.REC.1402.128). The participants were assured about the confidentiality of the information. Written informed consent was obtained from all the participants.
Funding
This study was funded by Tabriz Health Services Management Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Authors' contributions
Data collection: Fatemeh Molaei Tavani and Parvin Rahmani; Statistical analysis: Omid Zadi; Investigation and writing: Mozhgan Behshid and Zahra Sheikhalipour; final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers would like to thank the Faculty of Nursing and Midwifery authorities of Tabriz University of Medical Sciences and all the participating nurses.
References
Service delivery systems led by nurses can play a significant role in decision-making, planning, and the process of prevention, care, and referral to a doctor in the care team. When nurses manage and plan these services on a broad scale, their professional independence is increased (Choi & De Gagne, 2016). Professional autonomy is a critical component of the nursing profession (Ko et al., 2018). In other words, professionalization in nursing is impossible without attaining professional autonomy (Pursio et al., 2021).
Professional autonomy has been defined as the level of authority that individuals possess in making decisions on a specific action (Hung et al., 2013). With the development of the nursing profession, the professional responsibilities of nurses have increased. Hence, nurses require autonomy in their activities. Professional autonomy is a vital constituent of self-motivation, enabling nurses to make timely decisions at the patient’s bedside (Mirzaei & Nasrabadi, 2021). The higher levels of autonomy in the workplace predict the retention of nurses in the profession, job satisfaction, and safety performance (Koak et al., 2023). However, decreasing autonomy levels can increase nursing attrition (Nouri et al., 2017).
A research literature review indicates contradictory findings regarding the extent to which nurses have professional autonomy. A study in Iran reported high levels of professional autonomy among nurses (Mirzaei & Nasrabadi, 2021). However, another study in Iran reported low levels of professional autonomy among nurses (Abdolmaleki et al., 2019). When nurses have high degrees of professional autonomy, their supervisors provide them with support, trust, and respect, enhancing their credibility, communication, and coordination (Labrague et al., 2019). Low levels of professional autonomy can cause negative emotions such as dissatisfaction, a lack of commitment, demotivation, burnout, and depression among nurses (Labrague et al., 2019). Nurses should comprehend their levels of professional autonomy in the workplace, as it directly impacts their competency in ensuring patient safety. This competency pertains to the knowledge, skills, and attitudes related to patient safety (Han & Roh, 2020).
As the largest professional group in the health care system, nurses are responsible for providing 24-h patient care. Hence, a nurse’s competency is essential for patient safety and high-quality care (Han et al., 2020). The term “patient safety competency” is used in the literature to refer to nursing practices that “minimize risks to patients and providers through system effectiveness and individual performance” (Rizany et al., 2018).
The safety competency of nurses working in emergency settings in Iran was found to be relatively favorable (Najafi Ghezeljeh et al., 2022). The more people’s knowledge about patient safety in the workplace, the more positive their attitude and the higher their performance regarding patient safety (Memarbashi., 2020). The skill level of nurses in safety competence is reported to be low (Cho & Choi, 2018). This condition can harm patients, decrease the quality of care, increase re-hospitalization rates and costs, decline patient satisfaction, and ultimately higher patient mortality rates (Najafi Ghezeljeh et al., 2022).
Empowering nurses by granting professional independence increases their self-confidence and improves their ability to make decisions and act based on nursing diagnoses in certain situations (Rouhi Balasi et al., 2024). Furthermore, nurses’ patient safety competency assessment is crucial for ensuring patient safety, pinpointing enhancement areas, and identifying training requirements (Najafi Ghezeljeh et al., 2022).
Recognizing the significance of nurses’ independent performance and their competence in enhancing patient safety and care quality, the studies on nurses’ competence in patient safety in Iran are limited and contradictive, and in reviewing the extensive literature, no study was found that examines the relationship between these two variables. Therefore, the present study assessed professional autonomy and its association with patient safety competency among nurses in the hospitals affiliated with Tabriz University of Medical Sciences, Tabriz City, Iran.
Materials and Methods
This research is a descriptive-correlational study on nurses employed in educational, therapeutic hospitals affiliated with Tabriz University of Medical Sciences in Iran (Imam Reza, Sina, and Madani hospitals) in 2022. The Cochran formula was utilized to calculate the sample size. Since the total number of nurses in the studied hospitals was 360, a sample size of 185 was calculated, with a confidence level of 95% and the sampling accuracy (d) of 5%. Finally, 205 subjects were selected by considering a 10% sample attrition. Five participants were excluded from the study because they answered the questionnaires incompletely; hence, the final sample included 200 nurses. The subjects were selected by stratified random sampling. Hospitals affiliated with Tabriz University of Medical Sciences formed stratification classes, and random sampling was done in each stratification class using a table of random numbers.
The data collection tool comprised three parts. First, the demographic characteristics questionnaire of nurses included age, sex, marital status, work experience, educational level, and the type of work shift. Second is the professional autonomy questionnaire. It is an 18-item questionnaire that assesses nurses’ levels of professional autonomy in three dimensions: Knowledge (items 1-6), action (items 7-12), and value (items 13-18). Responses are scored on a 6-point Likert scale ranging from “strongly disagree” (1) to “strongly agree” (6). The scores on this scale ranged from 18 to 108, signifying low autonomy for scores between 18 and 47.99, medium autonomy for scores between 48 and 77.99, and high autonomy for scores between 78 and 108 (Varjus et al., 2003). Yeganeh et al. confirmed the high reliability of the Persian version of the questionnaire in their study with a Cronbach α of 0.99 and an intraclass correlation coefficient of 0.88 in a test re-test conducted over a 2-week interval in a pilot study involving 30 subjects (Yeganeh et al., 2019).
Using the whole sample in our study, the internal consistency of the questionnaire was measured using the Cronbach α coefficient, resulting in a value of 0.90. The third part is the patient safety competency self-evaluation questionnaire. This scale was designed by Lee et al. (2014) in Korea and consists of 41 items rated on a 5-point Likert scale. This instrument assesses three dimensions of patient safety: Knowledge, attitude, and skills, with 6 items measuring knowledge (score range: 6–30), 21 items measuring skills (score range: 21–105), and 14 items measuring attitude (score range: 14–70). The item scores are added up in each dimension. A higher score in each dimension indicates a greater level of that dimension. The total score ranges from 41 to 205, with the higher scores indicating higher competency in patient safety. The Cronbach α was 0.859 for the knowledge dimension, 0.794 for the attitude dimension, 0.912 for the skills dimension, and 0.907 for overall (Lee et al., 2014).
Moreover, Najafi Ghezeljeh et al. (2022) assessed the content validity of the Persian version of the questionnaire with three members from the Faculty of Nursing and Midwifery at Iran University of Medical Sciences. The reliability coefficients for knowledge, attitude, and skills dimensions were determined using Cronbach α, yielding values of 0.908, 0.836, and 0.922, respectively. Additionally, the total questionnaire demonstrated a reliability coefficient of 0.952. In this research, the internal consistency of the questionnaire in the studied population was measured using the Cronbach α coefficient, and its value was 0.93.
The inclusion criteria were willingness to participate in the study, a bachelor’s degree or higher, and possessing at least six months of working experience as a clinical nurse. The exclusion criteria included unwillingness to cooperate, nurses performing administrative or secretarial work, incomplete questionnaires (less than 90% of questions answered), and the same response to all questions. Eligible nurses were provided with the questionnaires after being informed of the research objectives and giving consent.
The data were analyzed using descriptive statistics (frequency, percentage, and median), the Mann-Whitney U test, the Kruskal-Wallis test, and the Kendall Tau and Spearman non-parametric correlation coefficients in SPSS software, version 26. The significance level was set as P<0.05.
Results
The research findings regarding demographics revealed that 161 nurses (80.5%) were females and 39(19.5%) were males. The majority of participants were married (54%) and held bachelor’s degrees (75.5%) (Table 1).
There were significant relationships between the median values of professional autonomy and work experience and also the level of nurses’ education (P<0.05) (Table 1).
Findings concerning the nurses’ professional autonomy showed that 120(60%) experienced a high level of professional autonomy, 74(37%) had a medium level, and 6(3%) reported a low level of professional autonomy (Figure 1).
Out of 200 nurses who took part in the study, 49(24.5%) had good patient safety competency, whereas 150(75.0%) reported moderate competency, and only 1(0.5%) had a weak level of competency (Figure 2).
There were significant relationships between the median values of competency and the variables of work experience and age (P<0.05) (Table 1)
The Kolmogorov-Smirnov and Shapiro–Wilk tests indicated that neither of the variables under investigation (professional autonomy and patient safety competency) followed a normal distribution. Hence, the Kendall Tau and Spearman non-parametric correlation coefficients were employed to test the relationship between the two variables. The Kendall Tau and Spearman correlation coefficients were 0.176 and 0.254, respectively, indicating that an increase in nurses’ professional autonomy would correspond to an increase in their patient safety competency (P<0.001) (Table 2).
Scatter plots were drawn to examine the association between professional autonomy and patient safety competency, and a non-parametric Loess correlation curve was applied to the data. The chart illustrates that patient safety competency increased in line with professional autonomy among nurses (Figure 3).
Discussion
This study assessed the correlation between professional autonomy and patient safety competency among nurses in hospitals affiliated with Tabriz University of Medical Sciences, Iran. The findings show that most participants have experienced high professional autonomy. Professional autonomy can improve the power and ability of nurses. If nurses possess the authority to act autonomously, they can make decisions based on their judgment and select their preferred course of action (Paganini & Bousso, 2015). In line with the current research findings, nurses in Setoodegan et al. study also reported high levels of professional autonomy that allowed them to make independent decisions and make the nursing profession stronger (Setoodegan et al., 2019).
Oshodi et al. (2019) examined nurses’ views and encounters with autonomy, highlighting that clinical autonomy is a key aspect of professional autonomy in nursing and is intricately connected to decision-making in patient care. However, they acknowledged that in clinical practice, nurses also adhere to doctors’ orders and operate within the confines of established rules. Hence, absolute autonomy is impossible. Mirzaei & Nasrabadi, (2021) studied the professional autonomy among nurses working in intensive care units and other units in Iran. They observed that the level of professional autonomy was moderate in special units and low in general wards.
Contrary to the present study, another research reported low average scores for nurses’ professional autonomy (Abdolmaleki et al., 2019). Nevertheless, a study in Iran indicated that nurses’ professional autonomy was moderate (Iranmanesh et al., 2014). Filipino nurses also show moderate levels of professional autonomy (Labrague et al., 2019).
Aghamohammadi et al. (2019) assessed nurse-physician collaboration and nurses’ professional autonomy in the intensive care unit. The findings indicated that most nurses demonstrated a moderate level of professional autonomy.
Oshodi et al. (2019) highlighted that nurses’ professional autonomy is particularly evident during emergencies and when senior staff are absent. Hence, it should be noted that nurses may not always have professional autonomy in their practice, as the extent of their autonomy can vary depending on the specific circumstances. They believed nursing officials should establish and uphold conducive work environments to ensure nurses understand their expectations and responsibilities. Additionally, precise and concrete job descriptions for nurses and well-defined career plans can contribute significantly to their professional growth. In other words, if nurses’ authority is not expanded sufficiently, they cannot achieve autonomy. Organizational restrictions such as authoritarian management, ambiguous or rigid organizational rules, and lack of control over nurses’ performance prevent the realization of professional autonomy (AllahBakhshian et al., 2017).
There were notable connections between the professional autonomy of nurses and their levels of work experience and education. Consistent with the current study, Mirzaei & Nasrabadi, (2021) found that nurses’ professional autonomy had significant relationships with age, work experience, and education level. Labrague et al., (2019) observed that various individual and institutional factors, including age, education, experience, self-efficacy, professional role, empowerment, workload, type of hospital, ward, number of working nurses, and the presence of professional associations, have affected the professional autonomy of nurses.
The results of the current study show that most nurses demonstrated a moderate level of safety competency. According to Najafi Ghezeljeh et al., (2022), emergency nurses have a relatively high level of knowledge. Additionally, nurses’ skills, attitudes, and overall patient safety competency in the emergency department were reported to be relatively favorable. However, the patient safety competency of working nurses was rated as moderate in a study conducted by Hwang, (2015). Yan et al. (2021) evaluated the safety competency of nurses in China. According to their findings, nurses had a crucial role in ensuring patient safety. They also observed that the participants’ level of competency was moderate. Cho and Choi (2018) analyzed the variables related to nurses’ patient safety competency, eg, safety skills, attitude, and knowledge. They concluded that nurses were less skilled in safe practice.
The variation in results can be ascribed to the fact that most clinical nurses receive limited formal training in patient safety competency during their university education. Additionally, these findings can be elucidated by the culture of patient safety across different countries. Habibi et al. (2022) observed that emergency nurses prioritize patient-related emergency activities, whereas their understanding of patient safety is limited. Therefore, it is necessary to implement patient safety management activities, provide training, establish standardization, and address problems effectively.
There were notable correlations between the safety competency of nurses and their years of experience and age. It is believed that patient safety competency in nurses improves with age and years of experience (Najafi Ghezeljeh et al., 2022). A study found an association between patient safety knowledge and age and training experience in this field (Biresaw et al., 2020), and nurses with higher education levels demonstrated higher patient safety skills. Nurses with Master’s degrees or higher are more likely to encounter additional opportunities to learn patient safety-related subjects within their curricula. This, in turn, can enhance their confidence in implementing patient safety practices (Hwang, 2015).
The findings indicate that increased nurses’ professional autonomy improves patient safety competency. Professional autonomy refers to making independent decisions and taking responsibility for them. This authority is derived from professional knowledge and position (Hwang, 2015). An extensive literature review indicates a scarcity of studies analyzing the correlation between professional autonomy and patient safety competency. Lee et al. (2014) investigated the effect of the convergence of professional autonomy and nurses’ empathy on patient safety culture. According to their findings, professional autonomy was crucial to patient safety. Hwang, (2015) also reported a positive correlation between professional autonomy and patient safety management performance. Furthermore, Ko et al. (2018) concluded that professional autonomy was the sole structural factor affecting patient safety. Kurt and Gurdogan (2023) studied nurses’ professional autonomy and patient support levels. Their findings revealed that nurses possessed a high level of professional autonomy, and their utilization of patient support roles was above average.
Conclusion
The study results revealed that most nurses employed in educational-therapeutic hospitals of Tabriz University of Medical Sciences, Iran, had high levels of professional autonomy, whereas their patient safety competency was moderate. Nurses must understand their levels of professional autonomy in the workplace and the opportunities it provides for independent work. It also maximizes their care abilities and concern for safety performance, encouraging them to comply with patient safety standards. This directly impacts their competency in patient safety, ultimately leading to quality care provision.
The roles of nurses are evolving. This evolution will help guarantee the ongoing promotion of nurses’ autonomy and patient safety competency in ensuring patient safety. Therefore, given the significance of autonomy within the nursing community, assessing the current state of professional autonomy in nursing and its correlation with patient safety competency is essential. Findings from such studies can provide insights for hospital managers and health policymakers in identifying the strategies that will enhance the autonomy of nurses.
This study assessed nurses’ safety competence using a self-report questionnaire. Other research studies may utilize different methods, such as clinical observation and patient interactions, to evaluate nurses’ behaviors. Furthermore, this cross-sectional study does not allow for causal inferences. Thus, caution should be exercised when generalizing the results.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Ethics Committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.REC.1402.128). The participants were assured about the confidentiality of the information. Written informed consent was obtained from all the participants.
Funding
This study was funded by Tabriz Health Services Management Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Authors' contributions
Data collection: Fatemeh Molaei Tavani and Parvin Rahmani; Statistical analysis: Omid Zadi; Investigation and writing: Mozhgan Behshid and Zahra Sheikhalipour; final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers would like to thank the Faculty of Nursing and Midwifery authorities of Tabriz University of Medical Sciences and all the participating nurses.
References
Abdolmaleki, M., et al., 2019. Relationship between autonomy and moral distress in emergency nurses. Indian Journal of Medical Ethics, 4(1), pp. 20–5. [DOI:10.20529/IJME.2018.076] [PMID]
Aghamohammadi, D., Dadkhah, B. & Aghamohammadi, M., 2019. Nurse-Physician collaboration and the professional autonomy of intensive care units nurses. Indian Journal of Critical Care Medicine: Peer-Reviewed, Official Publication of Indian Society of Critical Care Medicine, 23(4), pp. 178–81. [DOI:10.5005/jp-journals-10071-23149] [PMID]
Allahbakhshian, M., et al., 2017. Barriers to intensive care unit nurses’ autonomy in Iran: A qualitative study. Nursing Outlook, 65(4), pp. 392–9. [DOI:10.1016/j.outlook.2016.12.004] [PMID]
Biresaw, H., Asfaw, N. & Zewdu, F., 2020. Knowledge and attitude of nurses towards patient safety and its associated factors. International Journal of Africa Nursing Sciences, 13, pp. 100229. [DOI:10.1016/j.ijans.2020.100229]
Cho, S. M. & Choi, J., 2018. Patient safety culture associated with patient safety competencies among registered nurses. Journal of Nursing Scholarship, 50 (5), pp. 549-57. [DOI:10.1111/jnu.12413]
Choi, M. & De Gagne, J. C., 2016. Autonomy of nurse practitioners in primary care: An integrative review. Journal of The American Association of Nurse Practitioners, 28(3), pp. 170-4. [DOI:10.1002/2327-6924.12288]
Habibi Soola, A., et al., 2022. Predictors of patient safety competency among emergency nurses in Iran: A cross-sectional correlational study. BMC Health Services Research, 22( 1 ), pp. 547. [DOI:10.1186/s12913-022-07962-y]
Han, J. H. & Roh, Y. S., 2020. Teamwork, psychological safety, and patient safety competency among emergency nurses. International Emergency Nursing, 51, pp. 100892. [DOI:10.1016/j.ienj.2020.100892] [PMID]
Han, Y., Kim, J. S. & Seo, Y., 2020. Cross-sectional study on patient safety culture, patient safety competency, and adverse events. Western Journal of Nursing Research, 42(1), pp. 32–40. [DOI:10.1177/0193945919838990] [PMID]
Hung, C. C., et al., 2013. The effects of contextual and structural factors on patient safety in nursing units. The Journal of Nursing Research: JNR, 21(3), pp. 225–33. [DOI:10.1097/jnr.0b013e3182a0b004] [PMID]
Hwang, J. I., 2015. What are hospital nurses’ strengths and weaknesses in patient safety competence? Findings from three Korean hospitals. International Journal for Quality in Health Care, 27(3), pp. 232-8. [DOI:10.1093/intqhc/mzv027] [PMID]
Iranmanesh, S., et al., 2014. Nurses’ professional autonomy and attitudes toward caring for dying patients in South-East Iran. International Journal of Palliative Nursing, 20(6), pp. 294–300. [DOI:10.12968/ijpn.2014.20.6.294] [PMID]
Ko, Y. K., Jeong, S. H. & Yu, S., 2018. Job autonomy, perceptions of organizational policy, and the safety performance of nurses. International Journal of Nursing Practice, 24(6), pp. e12696. [DOI:10.1111/ijn.12696] [PMID]
Koak, B., et al., 2023. The Effects of professional autonomy, job satisfaction, and perceived patient-safety culture on nurses’ patient-safety management activities: A cross-sectional study. Korean Journal of Adult Nursing, 35(2) , pp. 117-26. [DOI:10.7475/kjan.2023.35.2.117]
Kurt, D. & Gurdogan, E. P., 2023. Professional autonomy and patient advocacy in nurses. Collegian Journal of the Royal College of Nursing, 30(2), pp. 327-34. [DOI:10.1016/j.colegn.2022.09.015]
Labrague, L. J., Mcenroe-Petitte, D. M. & Tsaras, K., 2019. Predictors and outcomes of nurse professional autonomy: A cross-sectional study. International Journal of Nursing Practice, 25(1), pp. e12711. [DOI:10.1111/ijn.12711] [PMID]
Lee, N. J., et al., 2014. Psychometric evaluation of a patient safety competency self-evaluation tool for nursing students. The Journal of Nursing Education, 53(10), pp. 550–62. [DOI:10.3928/01484834-20140922-01] [PMID]
Memarbashi, E., et al., 2020. Evaluation of the patient safety culture status and its related factors from the perspective of operating room personnel. Journal of Client-Centered Nursing Care, 6(1), pp. 23-30. [Link]
Mirzaei, M., et al., 2021. [Comparison of professional autonomy of nurses working in intensive care units and other wards in selected hospital of Iran University of Medical Sciences in 2020 (Persian)]. Quarterly Journal of Nursing Management, 10(3), pp. 97-102. [Link]
Najafi Ghezeljeh, T., et al., 2022. [Patient safety competency in emergency nurses in educational-medical centers of Iran University of Medical Sciences, 2020 (Persian)]. Iran Journal of Nursing, 34 (134), pp. 60-73. [DOI:10.32598/ijn.34.6.5]
Nouri, A., Jouybari, L. & Sanagoo, A., 2017. [Nurses’perception of factors influencing professional autonomy in nursing: A qualitative study (Persian)]. Journal of Urmia Nursing and Midwifery Faculty, 15 (6), pp. 469-77. [Link]
Oshodi, T. O., et al., 2019. Registered nurses’ perceptions and experiences of autonomy: A descriptive phenomenological study. BMC Nursing , 18, 51. [DOI:10.1186/s12912-019-0378-3]
Paganini, M. C. & Bousso, R. S., 2015. Nurses’ autonomy in end-of-life situations in intensive care units. Nursing Ethics, 22(7), pp. 803–14. [DOI:10.1177/0969733014547970] [PMID]
Pursio, K., et al., 2021. Professional autonomy in nursing: An integrative review. Journal of Nursing Management, 29(6), pp. 1565–77. [DOI:10.1111/jonm.13282] [PMID]
Rizany, I., Hariyati, R. T. S. & Handayani, H., 2018. Factors that affect the development of nurses’ competencies: A systematic review. Enfermeria Clinica, 28(Suppl 1), pp. 154-7. [DOI:10.1016/S1130-8621(18)30057-3]
Rouhi Balasi, L., et al., 2024. [Professional autonomy and safe nursing care in newly graduated nurses working in emergency departments (Persian)]. Journal of Guilan University of Medical Sciences, 33(1), pp. 32-41. [DOI:10.32598/JGUMS.33.1.541.1]
Setoodegan, E., et al., 2019. Nurses’ lived experiences of professional autonomy in Iran. International Journal of Nursing Sciences, 6(3), pp. 315-21. [DOI:10.1016/j.ijnss.2019.05.002]
Varjus, S. L., Suominen, T. & Leino-Kilpi, H., 2003. Autonomy among intensive care nurses in Finland. Intensive and Critical Care Nursing, 19(1), pp. 31-40. [DOI:10.1016/S0964-3397(03)00007-7]
Type of Study: Research |
Subject:
Special
Received: 2024/04/24 | Accepted: 2024/07/6 | Published: 2024/11/1
Received: 2024/04/24 | Accepted: 2024/07/6 | Published: 2024/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |