Wed, Oct 15, 2025
[Archive]
Volume 11, Issue 1 (Winter 2025)
JCCNC 2025, 11(1): 67-74 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Okgün Alcan A, Yavuz van Giersbergen M, Doğan O. Perceived Social Support and Social Appearance Anxiety After Bariatric Surgery. JCCNC 2025; 11 (1) :67-74
URL: http://jccnc.iums.ac.ir/article-1-636-en.html
URL: http://jccnc.iums.ac.ir/article-1-636-en.html
1- Department of Nursing, Faculty of Health Sciences, Izmir Bakircay University, Izmir, Turkey. , aliyeokgun@gmail.com
2- Department of Surgical Nursing, Faculty of Nursing, Ege University, Izmir, Turkey.
3- Department of General Surgery, Firat University Hospital, Elazig, Turkey.
2- Department of Surgical Nursing, Faculty of Nursing, Ege University, Izmir, Turkey.
3- Department of General Surgery, Firat University Hospital, Elazig, Turkey.
Full-Text [PDF 663 kb]
(691 Downloads)
| Abstract (HTML) (1268 Views)
Full-Text: (337 Views)
Introduction
Obesity is a disease that needs to be treated for reasons, such as psychosocial problems, additional diseases, and high mortality rates. Although weight loss could be achieved by non-surgical methods, it is known that 66% of patients regain weight in 24 months. Therefore, bariatric surgery is generally considered an everlasting treatment for the complications of obesity (Hilgendorf et al., 2021).
A total of 507298 bariatric or metabolic surgery procedures are performed annually; Italy, the United Kingdom, and Sweden are the three countries with the most reported bariatric or metabolic surgery procedures, respectively. Meanwhile, 1878 bariatric or metabolic surgery procedures have been performed in Turkey in 2021 (Brown et al., 2021). It is estimated that a total of 198651 bariatric surgery procedures were carried out in 2020 in the United States (American Society for Metabolic and Bariatric Surgery, 2024).
One of the most important reasons why patients prefer bariatric surgery is to eliminate dissatisfaction with body image and improve self-esteem (Hart et al., 2008; Hilgendorf et al., 2021). Having body dissatisfaction is associated with experiencing social appearance anxiety (SAA) (Ayhan et al., 2022). SAA is the anxiety about the physical visual aspect and concerns about others’ evaluation (Hart et al., 2008). People suffering from SAA have concerns about being negatively judged regarding their body’s visual aspect (Doori et al., 2022).
Studies have reported that patients feel reborn, and increase self-confidence and self-esteem in parallel with weight loss in the postoperative period. In a way, this situation reflects the effect of changes in body image. People with improved body image feel more positive. But this process takes a long time. In addition, the occurrence of sagging skin in various parts of the patient’s body due to weight loss may cause patients to choose to be obese again by experiencing psychosocial problems (Hart et al., 2008; Hilgendorf et al., 2021). Therefore, bariatric surgery patients tend to experience more SAA levels than patients undergoing other types of surgeries (İnanır & Akkuş, 2022).
Bariatric surgery is a highly prevalent surgical procedure with a high incidence of complications. Patients must be subjected to rigorous monitoring throughout the postoperative period. This is necessary to guarantee that they lose weight in a safe and controlled manner and to forestall the occurrence of complications. Changes in eating patterns, self-esteem, body image, and interpersonal relationships that occur after bariatric surgery and experiencing SAA can negatively affect the individual’s quality of life in the long run (Hart et al., 2008; Atik et al., 2015; Hilgendorf et al., 2021).
Since social support is an effective coping strategy, these effects can be aggravated without it (Atik et al., 2015; Ozkaraman et al., 2015; Ayhan et al., 2022). Social support is a psychological and social network that provides individuals with psychological and tangible resources to confront and cope with the problems that they may encounter in their lives (Doori et al., 2022). It refers to the amount of affection, attention, and support received from family members, friends, and others (Hassani et al., 2021). In accordance with the tenets of social support theory, the quality and quantity of social connections and relationships are of paramount importance for the well-being of individuals (Leahy-Warren, 2014). Social support provides the individual with healthy coping, reduces the sense of hopelessness and depression, increases personal efficacy in times of stress, and also provides emotional balance, life satisfaction, and psychological well-being (Atik et al., 2015). Individuals may enhance their overall health outcomes and augment their capacity to cope with stress by cultivating robust social connections and relationships. The theory emphasizes that social support can come from a variety of sources. The sources can be classified into four principal categories: Informational, emotional, instrumental, and appraisal support. It is important to note that the effectiveness of social support can vary depending on the individual’s personality, cultural background, and social environment (Leahy-Warren, 2014).
Perceived social support (PSS) can be defined as a cognitive appraisal of the reliability of social support from others (Leahy-Warren, 2014). Accordingly, PSS plays a more significant role in predicting health and well-being outcomes than the actual receipt of support (Leahy-Warren, 2014; Cobo-Rendón et al., 2020), because it has been demonstrated to influence the manner in which individuals perceive themselves and their surrounding environment (Cobo-Rendón et al., 2020).
Patients undergoing bariatric surgery need much more psychological and social support from their formal and informal caregivers to maintain weight loss, recovery, and cope with SAA (Atik et al., 2015). Data from several sources have identified that increased social support is associated with lower SAA (Ozkaraman et al., 2015; Niroomand et al., 2016; Spatuzzi et al., 2016). Although there are studies on the anxiety level, self-esteem, and social support resources of bariatric surgery patients, studies reporting the relationship between the social support perceived by the patients and their SAA are lacking (Conceição et al., 2020; Hilgendorf et al., 2021; İnanır & Akkuş, 2022) but limited tools exist for brief and effective assessment preoperatively. The aims of the study were to determine the extent to which two ratings of social support can predict bariatric surgery outcomes, and to examine any associations between these two methods. In this retrospective study, patients were included for whom the Cleveland clinic behavioral rating system (CCBRS). Hence, this study determines the relationship between PSS and SAA of patients after bariatric surgery in Turkey.
Material and Methods
This descriptive and correlational study was conducted from October to December 2022 at an obesity and metabolic surgery unit of a university hospital in Turkey. The study population consisted of 600 patients who underwent bariatric surgery in that hospital. Inclusion criteria were patients who underwent obesity and metabolic surgery, were older than 18 years, and consented to participate. The exclusion criterion was undergoing surgery less than six months before the study. The sample of the study consisted of 121 patients. The sample size was determined by the result of a priori power analysis using the G*Power statistical software, version 3.1. In the power analysis based on the data in the research conducted by Hilgendorf et al., the type 1 error was 0.05, the power of the test was 0.9, while the required minimum sample was determined as 98 (with a 5% margin of error) (Hilgendorf et al., 2021). Considering the potential of missing data, the minimum sample size was estimated at 108.
In this study, data were collected using the data collection form, the multidimensional scale of PSS (MSPSS), and the SAAS. The data collection form consisted of questions to determine the socio-demographic characteristics of the patients (i.e. gender, marital, educational, and employment status), their chronic diseases, and the time elapsed after bariatric surgery.
Meanwhile, MSPSS is a self-reported scale. It is composed of 12 items grouped into 3 sub-dimensions of family, friends, and significant others (Zimet et al., 1990; Eker et al., 2001). Each sub-dimension consists of 4 items and the items are scored based on a 7-point Likert scale ranging from 1 (very strongly disagree) to 7 (very strongly agree). The scores of sub-dimensions and total scale are evaluated by summing up the responses to all the items. The range of total scores varies from 12 to 84. Higher scores denote high perceived support. The Cronbach α value of the original scale is 0.88 (Zimet et al., 1990). The Cronbach α value of the Turkish version of MSPSS is 0.89 (Eker et al., 2001). In this study, the Cronbach α coefficient of the MSPSS was 0.92.
In addition, SAAS consists of 16 items. The items are scored based on a 5-point Likert scale ranging from 1 (not suitable at all) to 5 (completely suitable). The total score ranges from 16 to 80 with higher scores indicating higher appearance anxiety. The validity and reliability studies of the scale were conducted on three different samples of university students and the internal consistency coefficients of the scale were obtained as 0.94, 0.95, and 0.94 for the three samples (Hart et al., 2008). The Cronbach α for the Turkish version of SAAS was 0.93 (Doğan, 2010). In this study, the Cronbach α of the SAAS was 0.95.
After obtaining the necessary permissions to carry out the study, the data collection tools were published through a web-based survey. The subjects were contacted using the phone number information recorded in their files when bariatric surgery was performed. In this regard, a nurse in the research team called the eligible patients one by one and invited them to participate in the study. Phone calls were made between 09:00 and 17:00 on working days. Patients who could not be reached in the first call were called again on another day. An invitation letter containing the link to the study was sent to the patients who agreed to participate in the study.
The study data were analyzed using the SPSS (statistical package for the social sciences for Windows) software, version 21 (IBM SPSS Inc, Armonk, NY). Descriptive data on patients were expressed as frequency, percentages, and mean values. For numerical variables, the fit to the normal distribution of the data was assessed using the Shapiro-Wilk test. The Mann-Whitney U and Kruskal-Wallis tests were performed to analyze nonparametric data. Also, the Spearman rho correlation coefficient (ρ) was used to examine the associations between variables. For these results, a P<0.05 was considered statistically significant.
Results
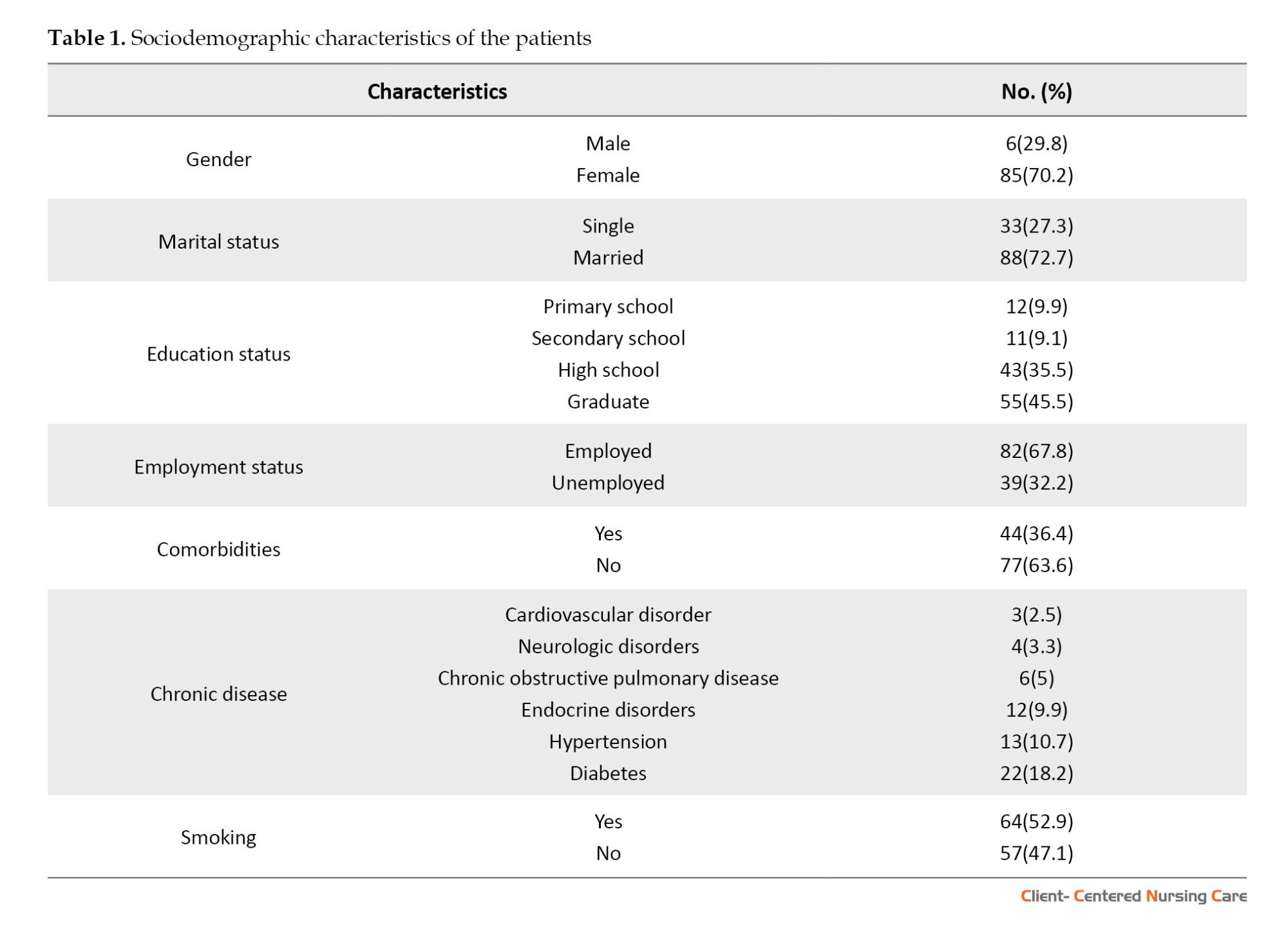
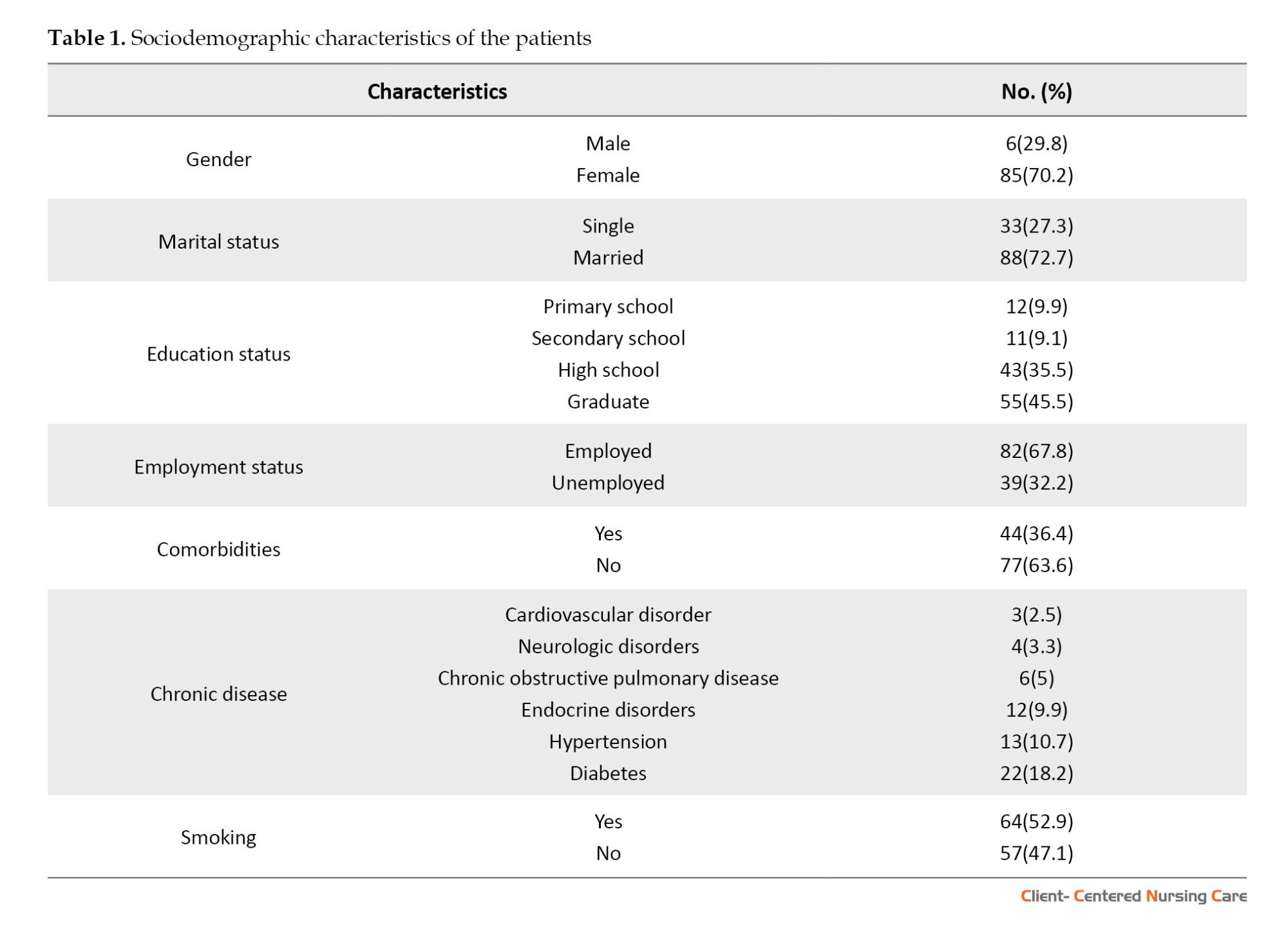
In this study, the mean age of the patients was determined as 39.07±9.02 years (minimum=22 years and maximum=67 years). The mean body mass index (BMI) of the patients was 44.61±6.60 kg/m2 (minimum=26.3 kg/m2 and maximum=74.23 kg/m2) in the preoperative period and 27.76±4.58 kg/m2 (minimum=20.28 kg/m2 and maximum=42.97 kg/m2) in the postoperative phase. The patients had undergone bariatric surgery a median of 36 (interquartile range=157) months ago. The distribution of patients according to their sociodemographic characteristics is reported in Table 1.
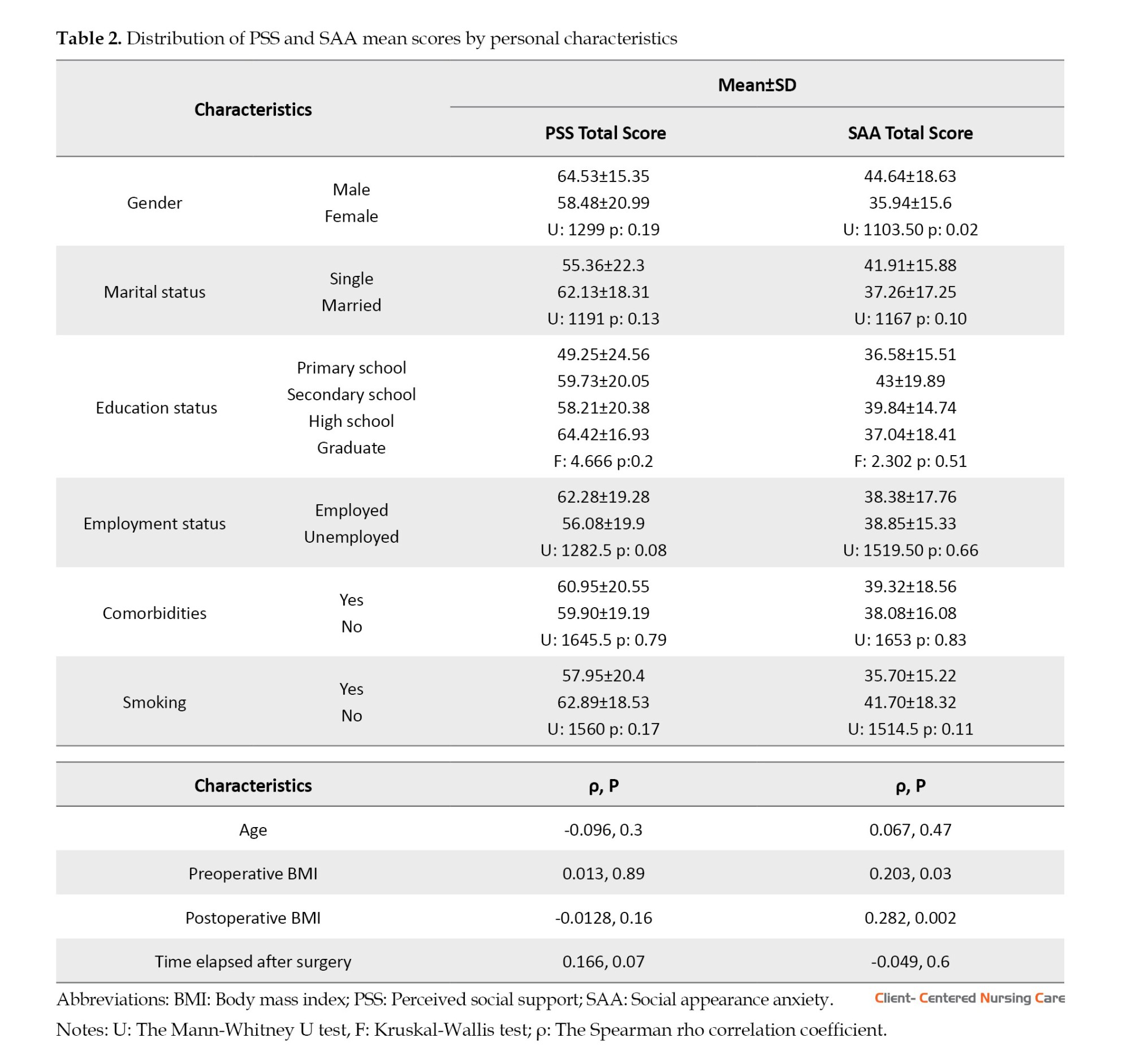
The mean MSPSS score of the patients was 60.28±19.62 (minimum=12 and maximum=84). The mean score of family, friends, and significant others regarding the source of the support was 24.88±7.19, 19.7±7.06, and 18.69±8.69, respectively. The mean SAAS score was 38.53±16.95 (minimum=16 and maximum=76). The distribution of MSPSS and SAAS mean scores by personal characteristics is given in Table 2. The SAAS total score of male patients was significantly higher than that of females (P<0.05). There was a significantly positive relationship between preoperative BMI, postoperative BMI, and SAAS total score (P<0.05; Table 2).
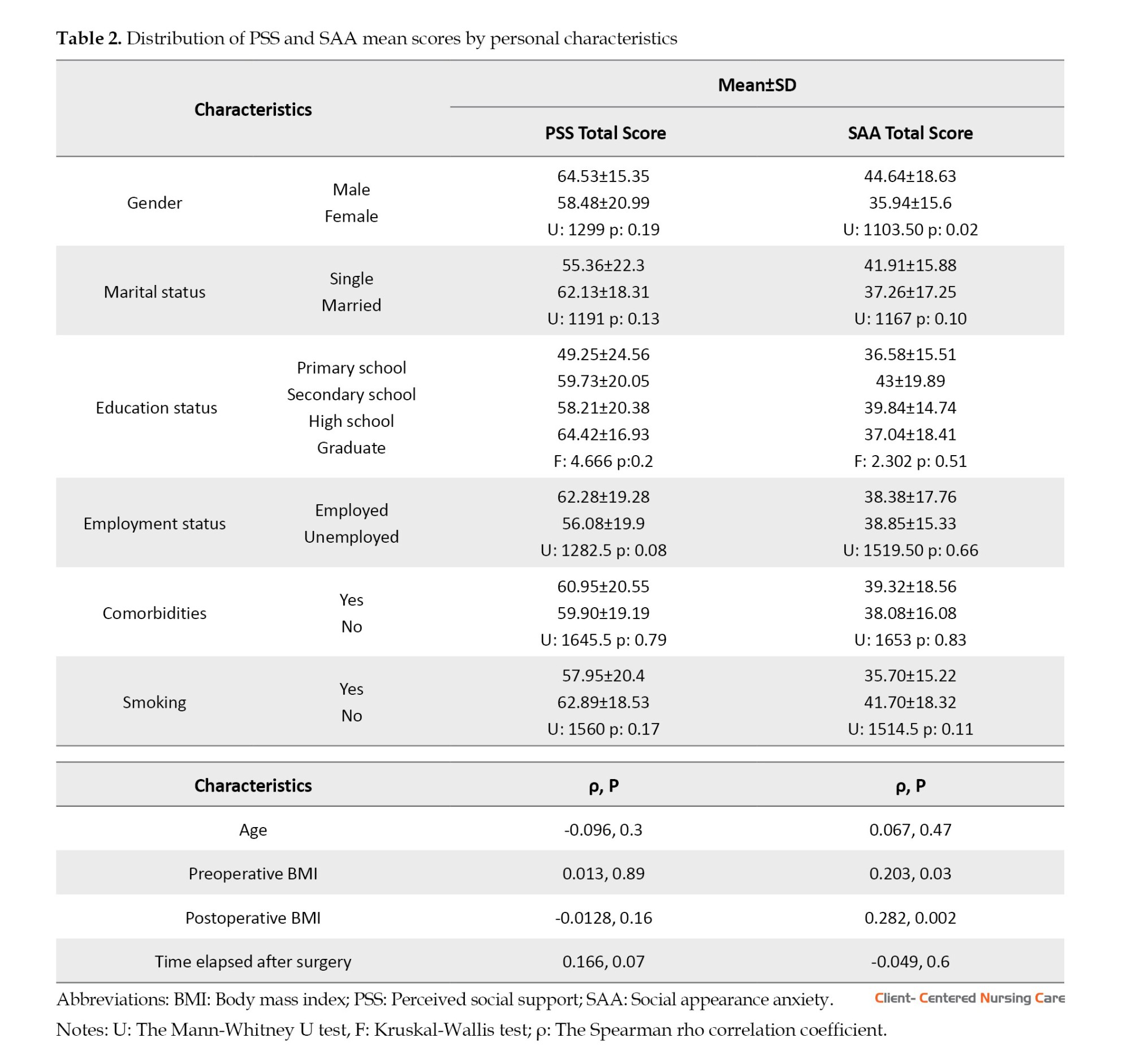
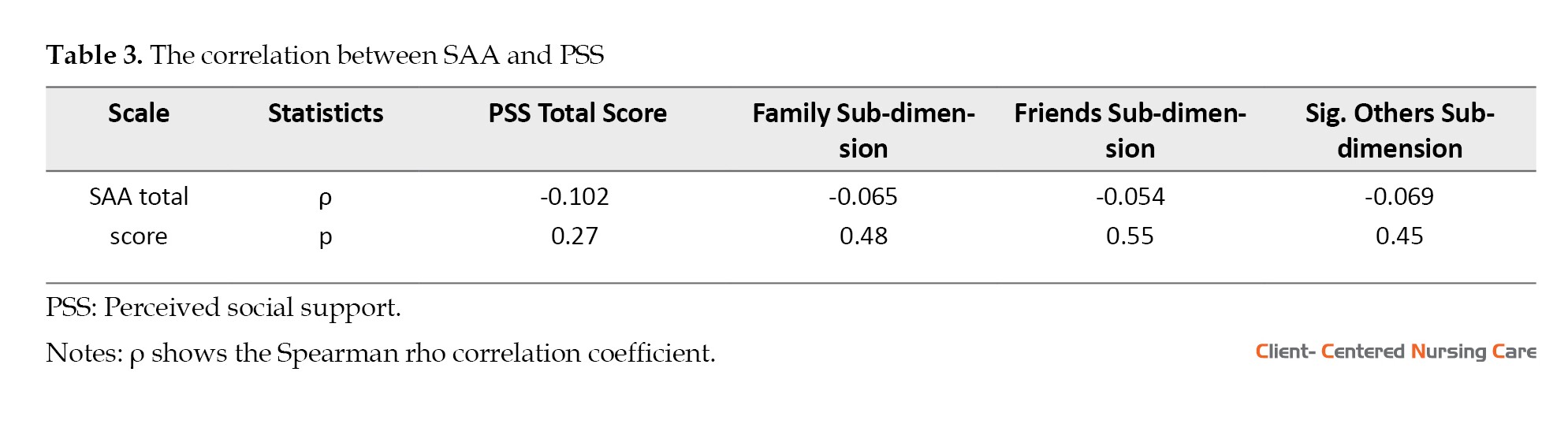
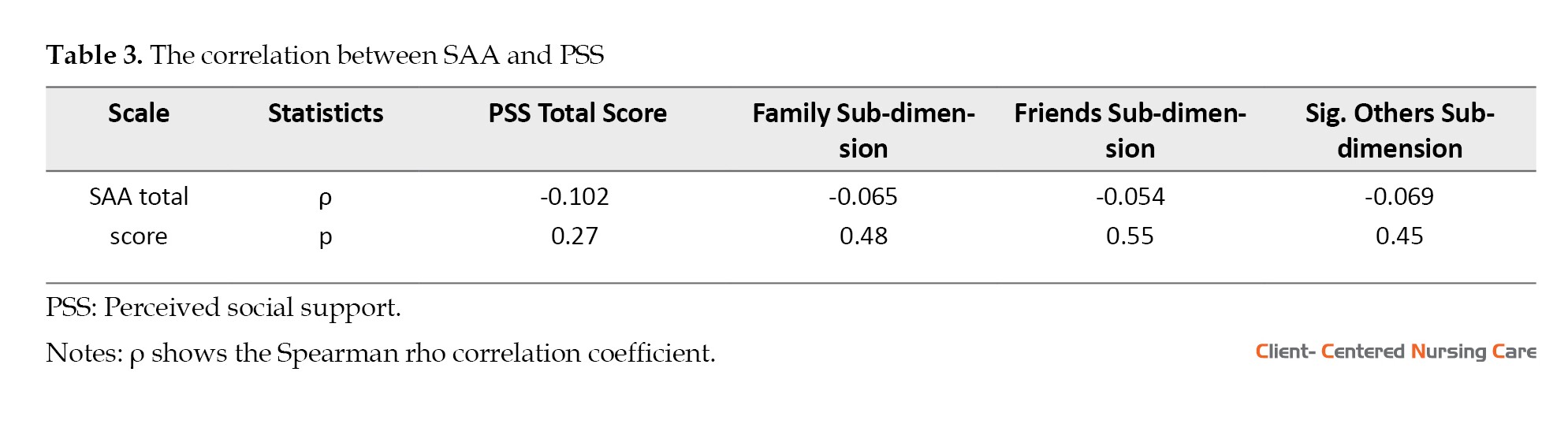
There was a negative relationship between the social support perceived by the patients after bariatric surgery and their SAA, but this relationship was not statistically significant (ρ=-0.102, P=0.27; Table 3).
Discussion
Social support is an important component for patients to be successful in lifestyle changes, especially in eating habits which they need to make in order to achieve weight management after bariatric surgery (Geraci et al., 2014; Hilgendorf et al., 2021) but limited tools exist for brief and effective assessment preoperatively. The aims of the study were to determine the extent to which two ratings of social support can predict bariatric surgery outcomes, and to examine any associations between these two methods. In this retrospective study, patients were included for whom the CCBRS. Also, it is associated with improved post-surgery results and decreased levels of stress (Geraci et al., 2014; Hilgendorf et al., 2021) but limited tools exist for brief and effective assessment preoperatively. The aims of the study were to determine the extent to which two ratings of social support can predict bariatric surgery outcomes, and to examine any associations between these two methods. In this retrospective study, patients were included for whom the CCBRS. In this study, the mean PSS score of the patients was 60.28±19.62. This result is similar to the results of Conceição and colleagues’ study. They noted that the PSS total score was 59.14 after bariatric surgery (Conceição et al., 2020). A current study reported a similar PSS level (68.7±18.18) six months after bariatric surgery (Yildiz & Karagözoǧlu, 2021). Similar levels of PSS have been reported among cancer patients (58.48±17.84) (Erdoğan & Cömert, 2015), oral cancer patients (60.17±11.34) (Gao et al., 2019), patients undergoing hemodialysis treatment (60.36±7.32) (Atik et al., 2015) and patients suffering from burn (68.34±18.08) (Ayhan et al., 2022).
The mean SAA score of the patients was 38.53±16.95. Accordingly, the SAA of the patients in our study group is below the moderate level. In Inanir and Akkuş study, the mean SAA score after bariatric surgery was 37.62±16.48 among women and 33.8±15.87 among men (İnanır & Akkuş, 2022). In line with our findings, similar levels of SAA scores have also been reported among women with breast cancer (34.30±9.35) (Ozkaraman et al., 2015), people with facial palsy (36.2±16.3) (Siemann et al., 2023), patients suffering from burns (39.38±17.71) (Ayhan et al., 2022), overweight young girls (43.36±17.07) (Unver et al., 2022) the Oxford happiness questionnaire-short form (OHQ-SF), and patients undergoing hemodialysis treatment (45.9±10.96) (Atik et al., 2015).
In this study, the total SAA score of men was higher than those of women (P<0.05). This result is contrary to previous studies which have suggested that male sex is associated with lower SAA scores (Atik et al., 2015; Siemann et al., 2023). However, Ayhan et al., (2022) demonstrated no significant differences between SAA scores and gender. The difference observed in the present study may be due to the composition of the sample which included bariatric surgery patients. The results of this study demonstrated that preoperative and postoperative BMI were positively correlated with the total score of SAA (P<0.05). İnanır & Akkuş, (2022) also reported a significant weak positive correlation between the preoperative and postoperative BMI of bariatric surgery patients and their SAA score. In the present study, the PSS and SAA scores of the patients were inversely correlated. In other words, the SAA scores were found to increase with a decrease in PSS scores; however, this correlation was not statistically significant (ρ=-0.102, P=0.27). Ozkaraman et al., (2015) reported a negative association between PSS and SAA among women with breast cancer; however, this correlation was not statistically significant which is consistent with the present study results. According to the results of another study, the relationship between PSS and the evaluation of physical appearance was not significant (Gila et al., 2005) a self-report questionnaire designed specifically to evaluate these variables. The SEED was used to compare social and body self-esteem in 170 eating disorder adolescent patients, 115 with anorexia nervosa (mean age 15.6. Similarly, previous research indicates that social support does not affect the SAA of patients suffering from burns (Ayhan et al., 2022). These results pointed out that PSS is not effective in helping patients having severe appearance changes to cope with SAA.
Some diseases or treatment modalities lead to the transformation of patients’ perception of their own body and negatively affect body image which in turn results in psychological issues including depression, SAA, and low self-esteem (İnanır & Akkuş, 2022). Prostate cancer patients with good body image tend to maintain lower social support than their counterparts (Scandurra et al., 2022). Meanwhile, there is a direct relationship between PSS and body image in women with breast cancer (Yilmazer et al., 1994; Spatuzzi et al., 2016; Wu et al., 2021; Doori et al., 2022). Similarly, burn patients who received more social support were reported to focus less on their appearance and were more satisfied with their body image (Hodder et al., 2014; Niroomand et al., 2016). A significant relationship was also reported between body satisfaction and PSS among patients suffering from multiple sclerosis (Ghodusi et al., 2013).
Conclusion
The findings of this study revealed no statistically significant relationship between PSS and SAA after bariatric surgery. Considering the limitations of the study which could have affected the results, multicenter studies with more homogeneous samples in terms of time elapsed after bariatric surgery are recommended.
Study limitations
There are some limitations to be noted in this study. This is a single-center study, consequently, the results cannot be generalized to all patients undergoing bariatric surgery. Also, the study was conducted in a bariatric surgery center in the eastern region of Turkey, so the results may have been influenced by the culture of the area. Also, the time elapsed after surgery (6 to 157 months) was heterogeneous, which could have affected the results.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Non-interventional Clinical Ethics Committee of Izmir Bakircay University (No.: 700, date: 14.09.2022). Detailed information was provided in the introduction part of the data collection form. In accordance with the design of the study, online consent was obtained from the patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Aliye Okgün Alcan, and Meryem Yavuz van Giersbergen, and Oğuz Doğan; Data collection: Oğuz Doğan; Review and editing: Aliye Okgün Alcan, and Meryem Yavuz van Giersbergen; Writing the original draft and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to appreciate the patients who participated in this research.
References
Obesity is a disease that needs to be treated for reasons, such as psychosocial problems, additional diseases, and high mortality rates. Although weight loss could be achieved by non-surgical methods, it is known that 66% of patients regain weight in 24 months. Therefore, bariatric surgery is generally considered an everlasting treatment for the complications of obesity (Hilgendorf et al., 2021).
A total of 507298 bariatric or metabolic surgery procedures are performed annually; Italy, the United Kingdom, and Sweden are the three countries with the most reported bariatric or metabolic surgery procedures, respectively. Meanwhile, 1878 bariatric or metabolic surgery procedures have been performed in Turkey in 2021 (Brown et al., 2021). It is estimated that a total of 198651 bariatric surgery procedures were carried out in 2020 in the United States (American Society for Metabolic and Bariatric Surgery, 2024).
One of the most important reasons why patients prefer bariatric surgery is to eliminate dissatisfaction with body image and improve self-esteem (Hart et al., 2008; Hilgendorf et al., 2021). Having body dissatisfaction is associated with experiencing social appearance anxiety (SAA) (Ayhan et al., 2022). SAA is the anxiety about the physical visual aspect and concerns about others’ evaluation (Hart et al., 2008). People suffering from SAA have concerns about being negatively judged regarding their body’s visual aspect (Doori et al., 2022).
Studies have reported that patients feel reborn, and increase self-confidence and self-esteem in parallel with weight loss in the postoperative period. In a way, this situation reflects the effect of changes in body image. People with improved body image feel more positive. But this process takes a long time. In addition, the occurrence of sagging skin in various parts of the patient’s body due to weight loss may cause patients to choose to be obese again by experiencing psychosocial problems (Hart et al., 2008; Hilgendorf et al., 2021). Therefore, bariatric surgery patients tend to experience more SAA levels than patients undergoing other types of surgeries (İnanır & Akkuş, 2022).
Bariatric surgery is a highly prevalent surgical procedure with a high incidence of complications. Patients must be subjected to rigorous monitoring throughout the postoperative period. This is necessary to guarantee that they lose weight in a safe and controlled manner and to forestall the occurrence of complications. Changes in eating patterns, self-esteem, body image, and interpersonal relationships that occur after bariatric surgery and experiencing SAA can negatively affect the individual’s quality of life in the long run (Hart et al., 2008; Atik et al., 2015; Hilgendorf et al., 2021).
Since social support is an effective coping strategy, these effects can be aggravated without it (Atik et al., 2015; Ozkaraman et al., 2015; Ayhan et al., 2022). Social support is a psychological and social network that provides individuals with psychological and tangible resources to confront and cope with the problems that they may encounter in their lives (Doori et al., 2022). It refers to the amount of affection, attention, and support received from family members, friends, and others (Hassani et al., 2021). In accordance with the tenets of social support theory, the quality and quantity of social connections and relationships are of paramount importance for the well-being of individuals (Leahy-Warren, 2014). Social support provides the individual with healthy coping, reduces the sense of hopelessness and depression, increases personal efficacy in times of stress, and also provides emotional balance, life satisfaction, and psychological well-being (Atik et al., 2015). Individuals may enhance their overall health outcomes and augment their capacity to cope with stress by cultivating robust social connections and relationships. The theory emphasizes that social support can come from a variety of sources. The sources can be classified into four principal categories: Informational, emotional, instrumental, and appraisal support. It is important to note that the effectiveness of social support can vary depending on the individual’s personality, cultural background, and social environment (Leahy-Warren, 2014).
Perceived social support (PSS) can be defined as a cognitive appraisal of the reliability of social support from others (Leahy-Warren, 2014). Accordingly, PSS plays a more significant role in predicting health and well-being outcomes than the actual receipt of support (Leahy-Warren, 2014; Cobo-Rendón et al., 2020), because it has been demonstrated to influence the manner in which individuals perceive themselves and their surrounding environment (Cobo-Rendón et al., 2020).
Patients undergoing bariatric surgery need much more psychological and social support from their formal and informal caregivers to maintain weight loss, recovery, and cope with SAA (Atik et al., 2015). Data from several sources have identified that increased social support is associated with lower SAA (Ozkaraman et al., 2015; Niroomand et al., 2016; Spatuzzi et al., 2016). Although there are studies on the anxiety level, self-esteem, and social support resources of bariatric surgery patients, studies reporting the relationship between the social support perceived by the patients and their SAA are lacking (Conceição et al., 2020; Hilgendorf et al., 2021; İnanır & Akkuş, 2022) but limited tools exist for brief and effective assessment preoperatively. The aims of the study were to determine the extent to which two ratings of social support can predict bariatric surgery outcomes, and to examine any associations between these two methods. In this retrospective study, patients were included for whom the Cleveland clinic behavioral rating system (CCBRS). Hence, this study determines the relationship between PSS and SAA of patients after bariatric surgery in Turkey.
Material and Methods
This descriptive and correlational study was conducted from October to December 2022 at an obesity and metabolic surgery unit of a university hospital in Turkey. The study population consisted of 600 patients who underwent bariatric surgery in that hospital. Inclusion criteria were patients who underwent obesity and metabolic surgery, were older than 18 years, and consented to participate. The exclusion criterion was undergoing surgery less than six months before the study. The sample of the study consisted of 121 patients. The sample size was determined by the result of a priori power analysis using the G*Power statistical software, version 3.1. In the power analysis based on the data in the research conducted by Hilgendorf et al., the type 1 error was 0.05, the power of the test was 0.9, while the required minimum sample was determined as 98 (with a 5% margin of error) (Hilgendorf et al., 2021). Considering the potential of missing data, the minimum sample size was estimated at 108.
In this study, data were collected using the data collection form, the multidimensional scale of PSS (MSPSS), and the SAAS. The data collection form consisted of questions to determine the socio-demographic characteristics of the patients (i.e. gender, marital, educational, and employment status), their chronic diseases, and the time elapsed after bariatric surgery.
Meanwhile, MSPSS is a self-reported scale. It is composed of 12 items grouped into 3 sub-dimensions of family, friends, and significant others (Zimet et al., 1990; Eker et al., 2001). Each sub-dimension consists of 4 items and the items are scored based on a 7-point Likert scale ranging from 1 (very strongly disagree) to 7 (very strongly agree). The scores of sub-dimensions and total scale are evaluated by summing up the responses to all the items. The range of total scores varies from 12 to 84. Higher scores denote high perceived support. The Cronbach α value of the original scale is 0.88 (Zimet et al., 1990). The Cronbach α value of the Turkish version of MSPSS is 0.89 (Eker et al., 2001). In this study, the Cronbach α coefficient of the MSPSS was 0.92.
In addition, SAAS consists of 16 items. The items are scored based on a 5-point Likert scale ranging from 1 (not suitable at all) to 5 (completely suitable). The total score ranges from 16 to 80 with higher scores indicating higher appearance anxiety. The validity and reliability studies of the scale were conducted on three different samples of university students and the internal consistency coefficients of the scale were obtained as 0.94, 0.95, and 0.94 for the three samples (Hart et al., 2008). The Cronbach α for the Turkish version of SAAS was 0.93 (Doğan, 2010). In this study, the Cronbach α of the SAAS was 0.95.
After obtaining the necessary permissions to carry out the study, the data collection tools were published through a web-based survey. The subjects were contacted using the phone number information recorded in their files when bariatric surgery was performed. In this regard, a nurse in the research team called the eligible patients one by one and invited them to participate in the study. Phone calls were made between 09:00 and 17:00 on working days. Patients who could not be reached in the first call were called again on another day. An invitation letter containing the link to the study was sent to the patients who agreed to participate in the study.
The study data were analyzed using the SPSS (statistical package for the social sciences for Windows) software, version 21 (IBM SPSS Inc, Armonk, NY). Descriptive data on patients were expressed as frequency, percentages, and mean values. For numerical variables, the fit to the normal distribution of the data was assessed using the Shapiro-Wilk test. The Mann-Whitney U and Kruskal-Wallis tests were performed to analyze nonparametric data. Also, the Spearman rho correlation coefficient (ρ) was used to examine the associations between variables. For these results, a P<0.05 was considered statistically significant.
Results
In this study, the mean age of the patients was determined as 39.07±9.02 years (minimum=22 years and maximum=67 years). The mean body mass index (BMI) of the patients was 44.61±6.60 kg/m2 (minimum=26.3 kg/m2 and maximum=74.23 kg/m2) in the preoperative period and 27.76±4.58 kg/m2 (minimum=20.28 kg/m2 and maximum=42.97 kg/m2) in the postoperative phase. The patients had undergone bariatric surgery a median of 36 (interquartile range=157) months ago. The distribution of patients according to their sociodemographic characteristics is reported in Table 1.
The mean MSPSS score of the patients was 60.28±19.62 (minimum=12 and maximum=84). The mean score of family, friends, and significant others regarding the source of the support was 24.88±7.19, 19.7±7.06, and 18.69±8.69, respectively. The mean SAAS score was 38.53±16.95 (minimum=16 and maximum=76). The distribution of MSPSS and SAAS mean scores by personal characteristics is given in Table 2. The SAAS total score of male patients was significantly higher than that of females (P<0.05). There was a significantly positive relationship between preoperative BMI, postoperative BMI, and SAAS total score (P<0.05; Table 2).
There was a negative relationship between the social support perceived by the patients after bariatric surgery and their SAA, but this relationship was not statistically significant (ρ=-0.102, P=0.27; Table 3).
Discussion
Social support is an important component for patients to be successful in lifestyle changes, especially in eating habits which they need to make in order to achieve weight management after bariatric surgery (Geraci et al., 2014; Hilgendorf et al., 2021) but limited tools exist for brief and effective assessment preoperatively. The aims of the study were to determine the extent to which two ratings of social support can predict bariatric surgery outcomes, and to examine any associations between these two methods. In this retrospective study, patients were included for whom the CCBRS. Also, it is associated with improved post-surgery results and decreased levels of stress (Geraci et al., 2014; Hilgendorf et al., 2021) but limited tools exist for brief and effective assessment preoperatively. The aims of the study were to determine the extent to which two ratings of social support can predict bariatric surgery outcomes, and to examine any associations between these two methods. In this retrospective study, patients were included for whom the CCBRS. In this study, the mean PSS score of the patients was 60.28±19.62. This result is similar to the results of Conceição and colleagues’ study. They noted that the PSS total score was 59.14 after bariatric surgery (Conceição et al., 2020). A current study reported a similar PSS level (68.7±18.18) six months after bariatric surgery (Yildiz & Karagözoǧlu, 2021). Similar levels of PSS have been reported among cancer patients (58.48±17.84) (Erdoğan & Cömert, 2015), oral cancer patients (60.17±11.34) (Gao et al., 2019), patients undergoing hemodialysis treatment (60.36±7.32) (Atik et al., 2015) and patients suffering from burn (68.34±18.08) (Ayhan et al., 2022).
The mean SAA score of the patients was 38.53±16.95. Accordingly, the SAA of the patients in our study group is below the moderate level. In Inanir and Akkuş study, the mean SAA score after bariatric surgery was 37.62±16.48 among women and 33.8±15.87 among men (İnanır & Akkuş, 2022). In line with our findings, similar levels of SAA scores have also been reported among women with breast cancer (34.30±9.35) (Ozkaraman et al., 2015), people with facial palsy (36.2±16.3) (Siemann et al., 2023), patients suffering from burns (39.38±17.71) (Ayhan et al., 2022), overweight young girls (43.36±17.07) (Unver et al., 2022) the Oxford happiness questionnaire-short form (OHQ-SF), and patients undergoing hemodialysis treatment (45.9±10.96) (Atik et al., 2015).
In this study, the total SAA score of men was higher than those of women (P<0.05). This result is contrary to previous studies which have suggested that male sex is associated with lower SAA scores (Atik et al., 2015; Siemann et al., 2023). However, Ayhan et al., (2022) demonstrated no significant differences between SAA scores and gender. The difference observed in the present study may be due to the composition of the sample which included bariatric surgery patients. The results of this study demonstrated that preoperative and postoperative BMI were positively correlated with the total score of SAA (P<0.05). İnanır & Akkuş, (2022) also reported a significant weak positive correlation between the preoperative and postoperative BMI of bariatric surgery patients and their SAA score. In the present study, the PSS and SAA scores of the patients were inversely correlated. In other words, the SAA scores were found to increase with a decrease in PSS scores; however, this correlation was not statistically significant (ρ=-0.102, P=0.27). Ozkaraman et al., (2015) reported a negative association between PSS and SAA among women with breast cancer; however, this correlation was not statistically significant which is consistent with the present study results. According to the results of another study, the relationship between PSS and the evaluation of physical appearance was not significant (Gila et al., 2005) a self-report questionnaire designed specifically to evaluate these variables. The SEED was used to compare social and body self-esteem in 170 eating disorder adolescent patients, 115 with anorexia nervosa (mean age 15.6. Similarly, previous research indicates that social support does not affect the SAA of patients suffering from burns (Ayhan et al., 2022). These results pointed out that PSS is not effective in helping patients having severe appearance changes to cope with SAA.
Some diseases or treatment modalities lead to the transformation of patients’ perception of their own body and negatively affect body image which in turn results in psychological issues including depression, SAA, and low self-esteem (İnanır & Akkuş, 2022). Prostate cancer patients with good body image tend to maintain lower social support than their counterparts (Scandurra et al., 2022). Meanwhile, there is a direct relationship between PSS and body image in women with breast cancer (Yilmazer et al., 1994; Spatuzzi et al., 2016; Wu et al., 2021; Doori et al., 2022). Similarly, burn patients who received more social support were reported to focus less on their appearance and were more satisfied with their body image (Hodder et al., 2014; Niroomand et al., 2016). A significant relationship was also reported between body satisfaction and PSS among patients suffering from multiple sclerosis (Ghodusi et al., 2013).
Conclusion
The findings of this study revealed no statistically significant relationship between PSS and SAA after bariatric surgery. Considering the limitations of the study which could have affected the results, multicenter studies with more homogeneous samples in terms of time elapsed after bariatric surgery are recommended.
Study limitations
There are some limitations to be noted in this study. This is a single-center study, consequently, the results cannot be generalized to all patients undergoing bariatric surgery. Also, the study was conducted in a bariatric surgery center in the eastern region of Turkey, so the results may have been influenced by the culture of the area. Also, the time elapsed after surgery (6 to 157 months) was heterogeneous, which could have affected the results.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Non-interventional Clinical Ethics Committee of Izmir Bakircay University (No.: 700, date: 14.09.2022). Detailed information was provided in the introduction part of the data collection form. In accordance with the design of the study, online consent was obtained from the patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Aliye Okgün Alcan, and Meryem Yavuz van Giersbergen, and Oğuz Doğan; Data collection: Oğuz Doğan; Review and editing: Aliye Okgün Alcan, and Meryem Yavuz van Giersbergen; Writing the original draft and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to appreciate the patients who participated in this research.
References
American Society for Metabolic and Bariatric Surgery., 2024. Estimate of bariatric surgery numbers, 2011-2022. Retrieved from: [Link]
Atik, D., et al., 2015. [The effect of perceived social support by hemodialysis patients on their social appearance anxiety (Turkish)]. Medicine Science, 4(2), pp. 2210-23. [Link]
Ayhan, H. et al., 2022. ‘Investigation of the relationship between social appearance anxiety and perceived social support in patients with burns’, Burns. Burns: Journal of the International Society for Burn Injuries, 48(4), pp. 816–23. [DOI:10.1016/j.burns.2021.08.020] [PMID]
Brown, W. A., et al., 2021. The IFSO Global Registry IFSO Global Registry Report, 6th IFSO Global Registry Report. United Kingdom: Dendrite Clinical Systems Ltd Fifth. [Link]
Cobo-Rendón, R., et al., 2020. ‘Perceived social support and its effects on changes in the affective and eudaimonic well-being of Chilean University Students’. Frontiers in Psychology, 11, pp. 590513. [DOI:10.3389/fpsyg.2020.590513] [PMID]
Conceição, E. M., et al., 2020. ‘Perceived social support before and after bariatric surgery: Association with depression, problematic eating behaviors, and weight outcomes. Eating and Weight Disorders : EWD, 25(3), pp. 679–92. [DOI:10.1007/s40519-019-00671-2] [PMID]
Doğan, T., 2010. Adaptation of the social appearance anxiety scale (SAAS) to Turkish: A validity and reliability study. Journal of Education, 39, pp. 151-9. [Link]
Doori, Z., et al., 2022. Investigation of the relationship between perceived social support and body image in women with breast cancer. Middle East Current Psychiatry, 29(49).[DOI:10.1186/s43045-021-00165-x]
Eker, D. & Arkar, H., 2001. Factorial structure, validity, and reliability of revised form of the multidimensional scale of perceived social support. Turkish Journal of Psychiatry, 12(1), pp. 17-25. [Link]
Erdoğan, H., 2015. [Evaluation of the association between perceived social support and post traumatic stress disorder, depression, anxiety and stress with cancer patients. Hasan Kalyoncu (Turkish)] [MA thesis]. Gaziantep: Hasan Kalyoncu Üniversitesi. [Link]
Gao, Y., et al., 2019. Resilience and associated factors among Chinese patients diagnosed with oral cancer. BMC Cancer, 19(1), pp. 447. [DOI:10.1186/s12885-019-5679-0] [PMID]
Geraci, A. A., Brunt, A. R. & Marihart, C. L., 2014. Social support systems: A qualitative analysis of female bariatric patients after the first two years postoperative. Bariatric Surgical Practice and Patient Care, 9(2), pp. 66-71. [DOI:10.1089/bari.2014.0004]
Ghodusi, M., Heidari, M. & Hoseini, E., 2013. [Correlation between body esteem and perceived social support in patients with multiple sclerosis (MS) referred to the MS Society in Tehran (Persian)]. Journal of Ilam University of Medical Sciences, 21(6), pp. 215-23. [Link]
Trallero, J. T., et al., 2005. Social and body self-esteem in adolescents with eating disorders. International Journal of Psychology and Psychological Therapy, 5(1), pp. 63-71. [Link]
Hart, T. A., et al., 2008. Development and examination of the social appearance anxiety scale. Assessment, 15(1), pp. 48-59. [DOI:10.1177/1073191107306673] [PMID]
Hassani, S. F., Tizdast, T. & Zarbakhsh, M. R., 2021. The role of self-compassion and hope in the relationship between psychological wellbeing, maladaptive schemas, resilience, and social support in women with multiple sclerosis. Journal of Client-Centered Nursing Care, 7(3), pp. 195-204. [DOI:10.32598/JCCNC.7.3.372.1]
Hilgendorf, W., et al., 2021. Can a brief assessment of social support predict outcomes after bariatric surgery?’ Clinical Obesity, 11(1), pp. e12419. [DOI:10.1111/cob.12419] [PMID]
Hodder, K., Chur-Hansen, A. & Parker, A., 2014. A thematic study of the role of social support in the body image of burn survivors. Health Psychology Research, 2(1), pp. 1196. [DOI:10.4081/hpr.2014.1196] [PMID]
İnanır, T. & Akkuş, Y., 2022. The relationship between social appearance anxiety and sexuality in individuals undergoing bariatric surgery. Kafkas University.
Leahy-Warren, P., 2014. Social support theory. In J. Fitzpatrick & G. McCarthy (Eds), Theories guiding nursing research and practice: Making nursing knowledge development explicit (pp. 85-101). New York: Springer Publishing Company. [DOI:10.1891/9780826164056.0006]
Niroumand-Zandi, K., et al., 2016. [Relationship between socio familial support with satisfaction of body image in patients with burn (Persian)]. Iranian Journal of Psychiatric Nursing, 3(4), pp. 1-9. [Link]
Ozkaraman, A., et al., 2015. Relationships between social support and social image concerns in Turkish women with breast cancer. Asian Pacific Journal of Cancer Prevention : APJCP, 16(5), pp. 1795–802. [DOI:10.7314/APJCP.2015.16.5.1795] [PMID]
Scandurra, C., et al., 2022. ‘Social support mediates the relationship between body image distress and depressive symptoms in prostate cancer patients. International Journal of Environmental Research and Public Health, 19(8), pp. 4825. [DOI:10.3390/ijerph19084825] [PMID]
Siemann, I., et al., 2023. Everybody is watching me: A closer look at anxiety in people with facial palsy. Journal of Plastic, Reconstructive & Aesthetic Surgery : JPRAS, 77, pp. 408–15. [DOI:10.1016/j.bjps.2022.11.019] [PMID]
Spatuzzi, R., et al., 2016. Evaluation of social support, quality of life, and body image in women with breast cancer. Breast Care (Basel, Switzerland), 11(1), pp. 28–32. [DOI:10.1159/000443493] [PMID]
Unver, H., Kurt, N. & Bicer Sahin, F., 2022. Happiness and social appearance anxiety in overweight young girls. European Review for Medical and Pharmacological Sciences, 26(18), pp. 6821-6. [PMID]
Wu, Q., et al., 2021. Body image and hopelessness among early-stage breast cancer survivors after surgery in China: A crosssectional study. Nursing Open, 8(6), pp. 3384–93. [DOI:10.1002/nop2.884] [PMID]
Yildiz, E. & Karagözoǧlu, S., 2021. The effects of nursing education constructed according to roy adaptation model on adaptation process of patients undergoing bariatric surgery. Bariatric Surgical Practice and Patient Care, 16(2), pp. 98-108. [DOI:10.1089/bari.2020.0030]
Yilmazer, N., et al., 1994. A comparison of body image, self-esteem and social support in total mastectomy and breast-conserving therapy in Turkish women. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 2(4), pp. 238–41. [DOI:10.1007/BF00365728] [PMID]
Type of Study: Research |
Subject:
General
Received: 2024/07/17 | Accepted: 2024/11/5 | Published: 2025/02/1
Received: 2024/07/17 | Accepted: 2024/11/5 | Published: 2025/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






