Tue, Sep 2, 2025
[Archive]
Volume 11, Issue 2 (Spring 2025)
JCCNC 2025, 11(2): 137-148 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Taleb F, Altahari A, Mohammed M, Alemrany E, AL-a'ameri E, kareem Al Qaidy A, et al . Phantom Pain, Mental Health Problems, and Depression Among Yemenis With Amputated Limbs: Victims of the Recent Conflict. JCCNC 2025; 11 (2) :137-148
URL: http://jccnc.iums.ac.ir/article-1-659-en.html
URL: http://jccnc.iums.ac.ir/article-1-659-en.html
Fuad Taleb *1 

 , Asmaa Altahari2
, Asmaa Altahari2 

 , Morad Mohammed2
, Morad Mohammed2 
 , Eman Alemrany2
, Eman Alemrany2 
 , Enas AL-a'ameri2
, Enas AL-a'ameri2 
 , Abdul Kareem Al Qaidy2
, Abdul Kareem Al Qaidy2 
 , Hassam Alwageeh2
, Hassam Alwageeh2 
 , Samah Alhijri2
, Samah Alhijri2 
 , Ayat AlHamdany2
, Ayat AlHamdany2 
 , Khadija Ahmed2
, Khadija Ahmed2 
 , Aziza Alazazi2
, Aziza Alazazi2 



 , Asmaa Altahari2
, Asmaa Altahari2 

 , Morad Mohammed2
, Morad Mohammed2 
 , Eman Alemrany2
, Eman Alemrany2 
 , Enas AL-a'ameri2
, Enas AL-a'ameri2 
 , Abdul Kareem Al Qaidy2
, Abdul Kareem Al Qaidy2 
 , Hassam Alwageeh2
, Hassam Alwageeh2 
 , Samah Alhijri2
, Samah Alhijri2 
 , Ayat AlHamdany2
, Ayat AlHamdany2 
 , Khadija Ahmed2
, Khadija Ahmed2 
 , Aziza Alazazi2
, Aziza Alazazi2 

1- Vision Colleges, Riyadh, Saudi Arabia. , fuadtal6@gmail.com
2- Department of Nursing, Faculty of Medicine and Health Sciences, Taiz University, Taiz, Yemen.
2- Department of Nursing, Faculty of Medicine and Health Sciences, Taiz University, Taiz, Yemen.
Full-Text [PDF 628 kb]
(265 Downloads)
| Abstract (HTML) (1230 Views)
Full-Text: (221 Views)
Introduction
With increasing global unrest and conflicts worldwide, the cases of amputation are rising, resulting in broken health systems and a fragmented continuum of care (Barth et al., 2021). Amputation disrupts an individual’s social values, impacting their sense of vitality, body image, and fitness, and can often be perceived as a sign of personal loss or failure (Stancu et al., 2016).
The data on war-related amputations and injuries among Yemeni civilians is based on findings from a study of 254 patients treated at the Omani National Trauma Center. This retrospective cohort study documented injuries from 2015 to 2017, showing that blast (63%) and gunshot wounds (29%) were the primary causes, leading to traumatic amputations in 5% of cases and permanent disabilities in 50% (Ramaraj et al., 2023).
Amputation is a significant concern around the world. In 2017, it was estimated that 57.7 million people were living with an amputated limb due to trauma (McDonald et al., 2021). Unfortunately, these injuries are becoming increasingly common in wartime; for example, as of January 2023, over 40000 Ukrainians have been injured in the recent war, and it is estimated that up to 33% of injuries result in amputations (Tomilenko, 2023).
Yemen had the highest disability burden, measured by years lived with disability, among 195 countries (Vos et al., 2017). Thousands of people have lost limbs in Yemen since the conflict started in 2015. The United Nations (UN) estimates that about 2.2% of people in Yemen have at least one disability (Ngo & Bjork, 2018). The health care system in Yemen collapsed due to war. According to the UN, only 50% of health care facilities are fully functional, and more than 80% of the Yemeni population faces significant challenges in reaching health care services (OCHA, 2021). Explosive weapons cause more severe and complex disabilities, such as amputations and spinal cord injuries (Humanity & Inclusion, 2017). Millions of landmines and remnants of war remain in Ukraine, Yemen, Syria, Afghanistan, and other contaminated areas, putting people’s lives and work at risk (Loddo, 2022).
Amputation negatively impacts function, sensation, and body image, leading to financial difficulties, isolation, and low self-esteem. Post-amputation pain and suffering can also disrupt personal relationships, including marriage (Gilg, 2016). While mental health comorbidity is prevalent in amputees (Muzaffar et al., 2012), the majority of them have not received comprehensive care that includes psychological management (Barth et al., 2021).
A narrative review study that included research from the United States, France, Canada, Italy, Germany, Denmark, Japan, and the United Kingdom, among others, shows that phantom limb pain (PLP) is experienced by up to 87% of amputees. It is a complex phenomenon characterized by pain sensations such as stabbing, throbbing, burning, or cramping in a limb or organ that has been removed, commonly following amputation. As a result of unknown causes involving both central and peripheral nervous system changes—such as cortical reorganization and neuroma formation—a personalized approach is required due to the lack of a single gold-standard treatment. This approach may combine various therapies, including pharmacologic treatments like opioids, n-methyl-D-aspartate receptor antagonists like ketamine, antidepressants, and other treatments such as mirror therapy, motor imagery, and targeted muscle reinnervation (Culp & Abdi, 2022).
It has been shown that PLP could be triggered and exacerbated by psychological factors such as stress (Fuchs et al., 2018). However, Katz (1993) suggested that while amputees suffering from PLP exhibited higher than normal levels of psychological and emotional distress, including depression, it did not imply a causal relationship. The consensus is that there is no difference in the prevalence of pain of psychological origin among amputees and the general population. Therefore, phantom pain and depression may co-occur, but one is not necessarily the cause of the other.
Recovery from traumatic amputation needs to be comprehensive and coordinated and requires addressing the personal’s physical, psychological, and socioeconomic needs within the context of family, community, and the sociocultural environment in which they live (Ferguson et al., 2004). Furthermore, awareness of the co-morbid psychiatric disorders in amputated patients can be invaluable in proper management and preventing further chronic debilitating disorders associated with amputation (Muzaffar et al., 2012).
To the best of our knowledge, no prior study has examined the prevalence of phantom pain and the effect of amputation on the mental health and mood state of Yemenis with amputated limbs due to the recent conflict. Therefore, our study aimed to assess phantom pain, mental health problems, and depression among amputee victims of the recent Yemeni conflict.
Materials and Methods
Design, setting, and sample
A descriptive cross-sectional research design was utilized to fulfill the research aim. This study was conducted in Taiz, where King Salman Humanitarian Aid & Relief Center (KSrelief) established and operated the Artificial Limbs Center over three phases: Producing a wide range of prosthetic devices, providing physical and psychological rehabilitation for patients, and meeting patients’ medical and non-medical needs. To date, 8530 patients have received services at the Taiz Center through the support of KSrelief (Qahtani, 2021).
A convenience sample of 60 adult patients with amputated limbs admitted to the above-mentioned setting were recruited to participate in this study. There are no official statistics on the number of amputees due to the recent conflict; however, according to media sources, the number of amputees between December 2014 and December 2016 (the period of intensified conflict in Taiz) reached 274 cases (Sky News Arabia, 2018). The sample of 60 cases was chosen due to practical constraints and the limited time available. Patients who met the following criteria were eligible for the study: Consent to participate, age 18 years and older, ability to communicate, amputation due to recent war, and no cognitive impairment.
Instruments
The data were collected using a sociodemographic and clinical data sheet, general health questionnaire (GHQ-28 items), and Beck depression inventory-II (BDI-II).
Sociodemographic and clinical data sheet
The researchers developed this sheet after reviewing the relevant literature (Ali & Haider, 2017; Ngo & Bjork, 2018; Nizamli, 2020). For pain level determination, we reviewed and relied on the studies by Roullet et al. (2009) and Graziottin et al. (2022). This sheet was attached to the tools used in the study and consisted of two parts:
Part 1 covers sociodemographic data, including the respondent’s age, gender, marital status, level of education, residence (classified as urban or rural), and occupation.
Part 2 covers clinical data, which includes the type and date of amputation, presence of phantom pain, description and level of phantom pain (assessed using a visual and verbal pain scale: 1-3 for mild pain with minimal impact on activities of daily living [ADLs], 4-6 for moderate pain with moderate impact on ADLs, and 7-10 for severe pain with significant implications on ADLs). It also collects information on permanent medications, the probability of mental disorders, and depression status.
GHQ-28
This tool, which was developed by Goldberg & Hillier (1979), has 28 items in four subscales: Somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression. Each subscale has 7 items, rated on a 4-point Likert scale (0: Never; 1: Almost never; 2: sometimes; 3: Often), and the maximum possible score on the questionnaire is 84. To differentiate the studied subjects with mental health problems from those without problems, a score of 23 and above indicates a mental health problem, and a score below 23 indicates no mental health problem. The Arabic version of GHQ-28 was used in Saudi Arabia and Lebanon and was valid and reliable, with a Cronbach α reliability estimate of 0.89 (Alhamad & Al-Faris, 1998).
BDI-II
This tool is a 1996 revision of BDI. It is widely used to assess the severity of depression (Beck et al., 1996). BDI-II contains 21 questions, each with four answers scored on a scale of 0 to 3, resulting in a total score range of 0 to 63. Lower total scores indicate more severe depressive symptoms during the past two weeks. The Arabic version of BDI-II was used in Qatar, Egypt, and most Arabic countries and was valid and reliable, with Cronbach α values ranging between 0.82-0.93 (Alansari, 2006; Naja et al., 2019). The scores of a depression state on the BDI were categorized as follows: 0-5 indicating “non-depressed,” 6-11 “marginal depression,” 12-22 “simple depression,” 23- 30 “moderate depression,” 31-40 “severe depression,” and 41-60 indicating “more severe depression.”
Results
Table 1 shows the sociodemographic characteristics of the studied subjects. It appears from this Table that the majority of adults with amputated limbs due to the recent conflict in Yemen are less than 30 years old (63.3%). The highest percentage are males, 88.3%, and married, 68.3%. Regarding educational level, more than a third of the study population (36.7%) have a secondary education. Moreover, more than two-thirds of the studied subjects (70.0%) live in urban areas. Concerning subjects’ occupations, 60% are military, and 40% are civilian.
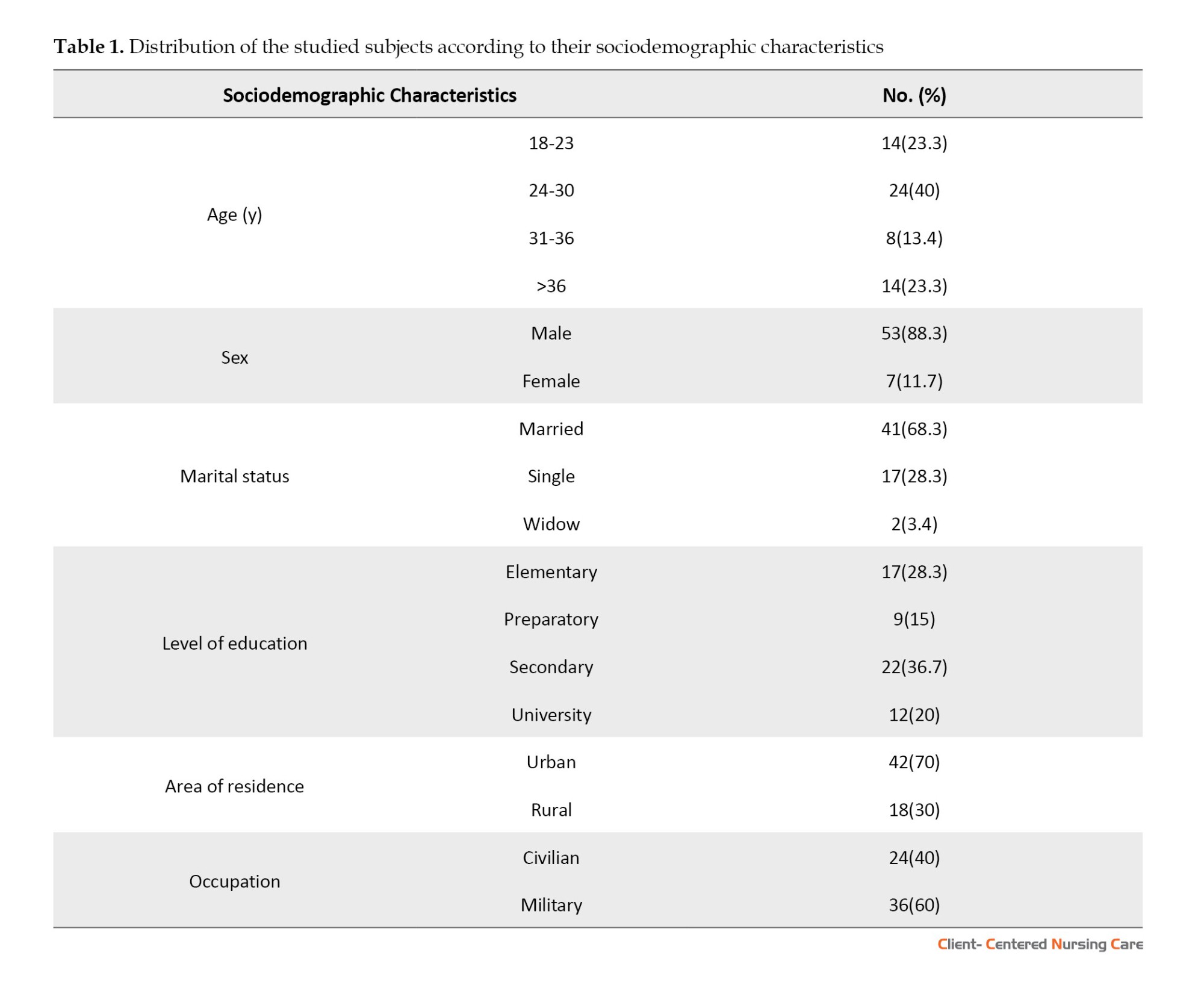
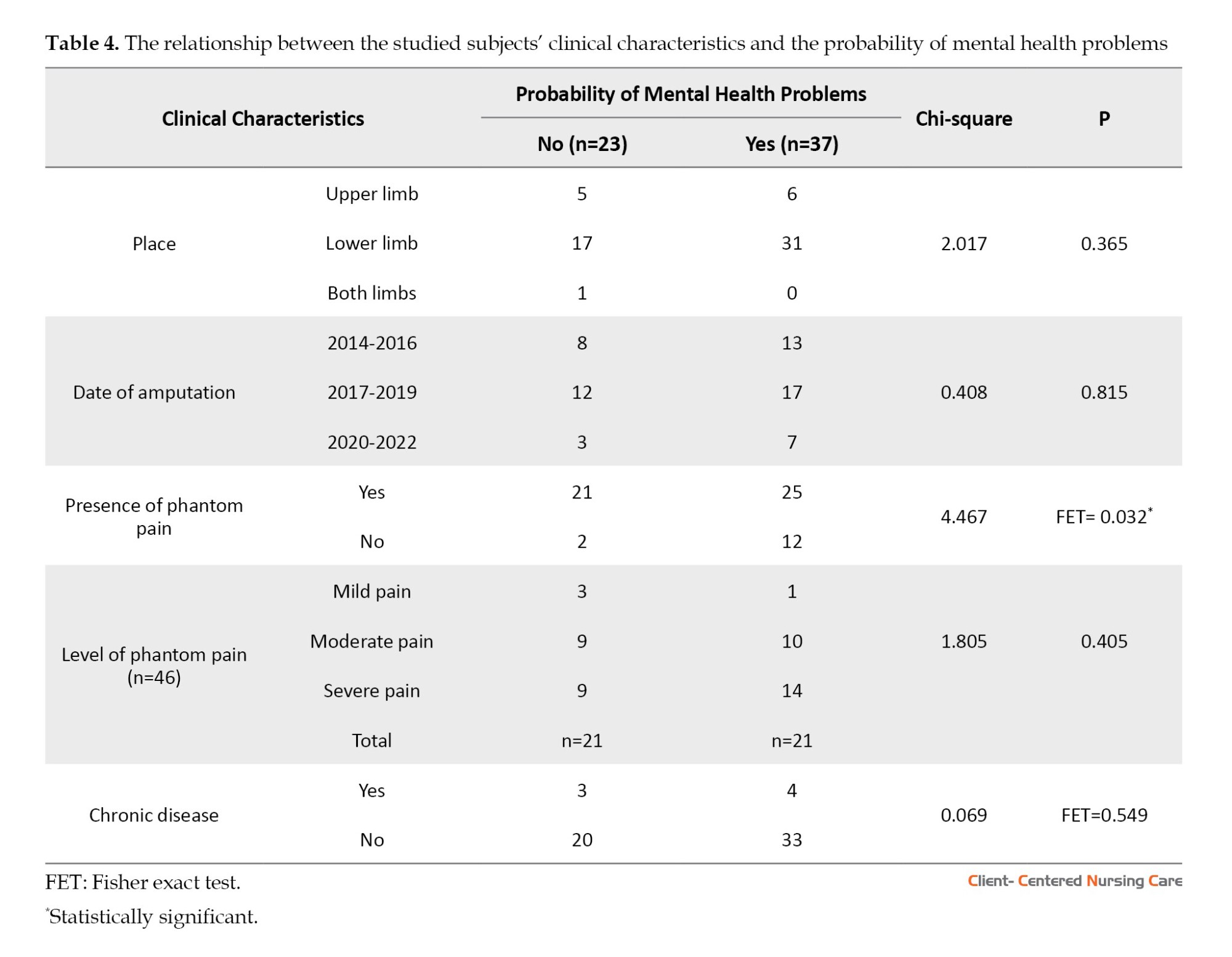
Table 2 displays the clinical characteristics of the studied subjects. Concerning the type of amputation, about 80% of the patients have lower limb amputation, and more than three-quarters of them (83.3%) lost their limbs before 2019. About the presence of phantom pain, 80% of the participants suffer from it, and one-half of them have severe pain. Considering physical health, most studied subjects (88.3%) are free from chronic diseases. Regarding the mental health of the studied subjects, this table indicates that 61.7% might have mental health problems, and almost all the studied subjects (93.4%) have some degree of depression; 75.0% of them have marginal or simple depression.
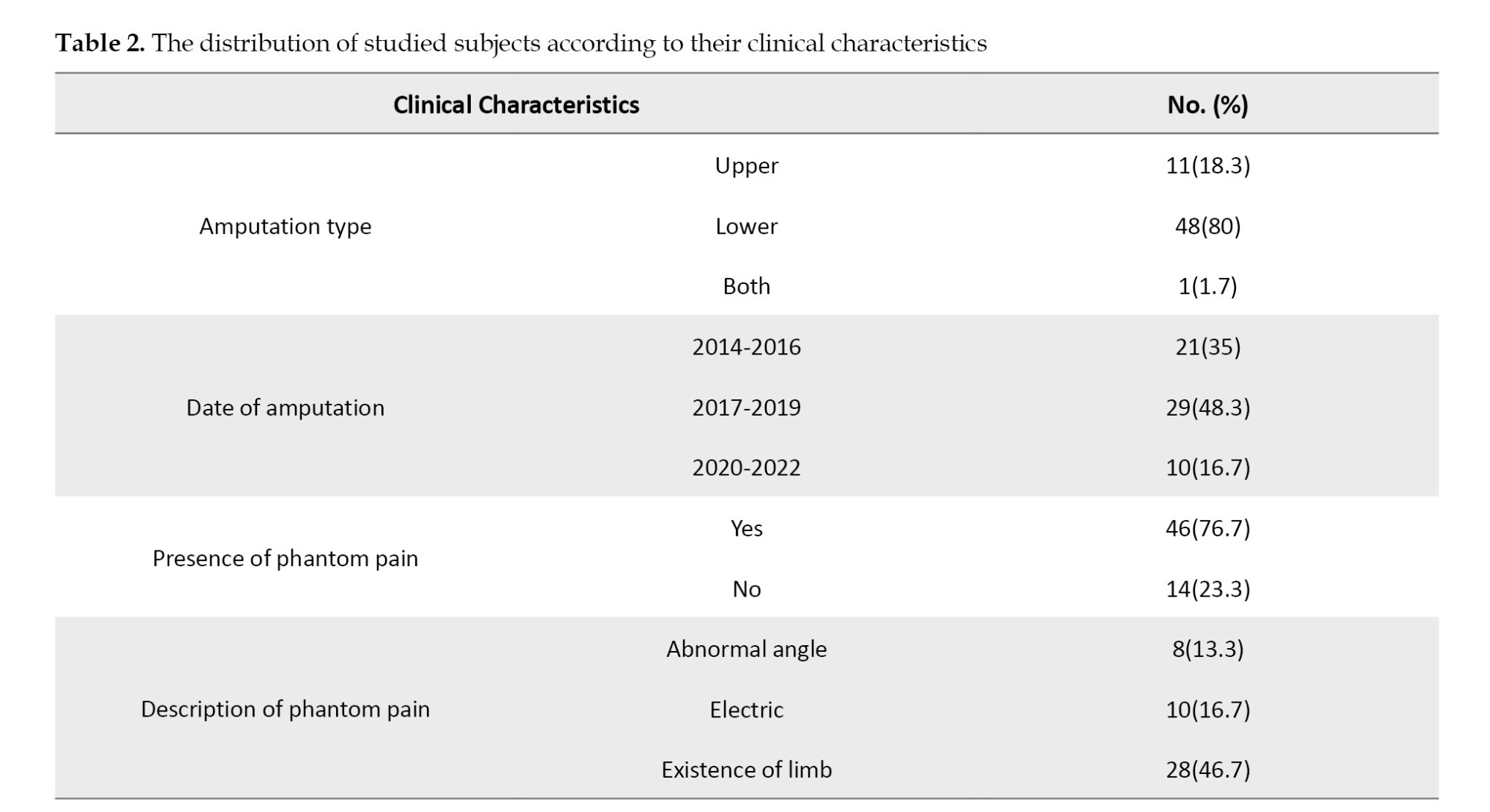
Table 3 reveals the relationship between the studied subject’s mental health problems and their sociodemographic characteristics. The table shows no statistically significant relationships between age, gender, education level, and residence of the studied subjects and the probability of mental health problems (P>0.05). On the other hand, it shows a statistically significant association between the likelihood of mental health problems and the presence of a partner and having military occupation, with P of 0.045 and 0.021, respectively.
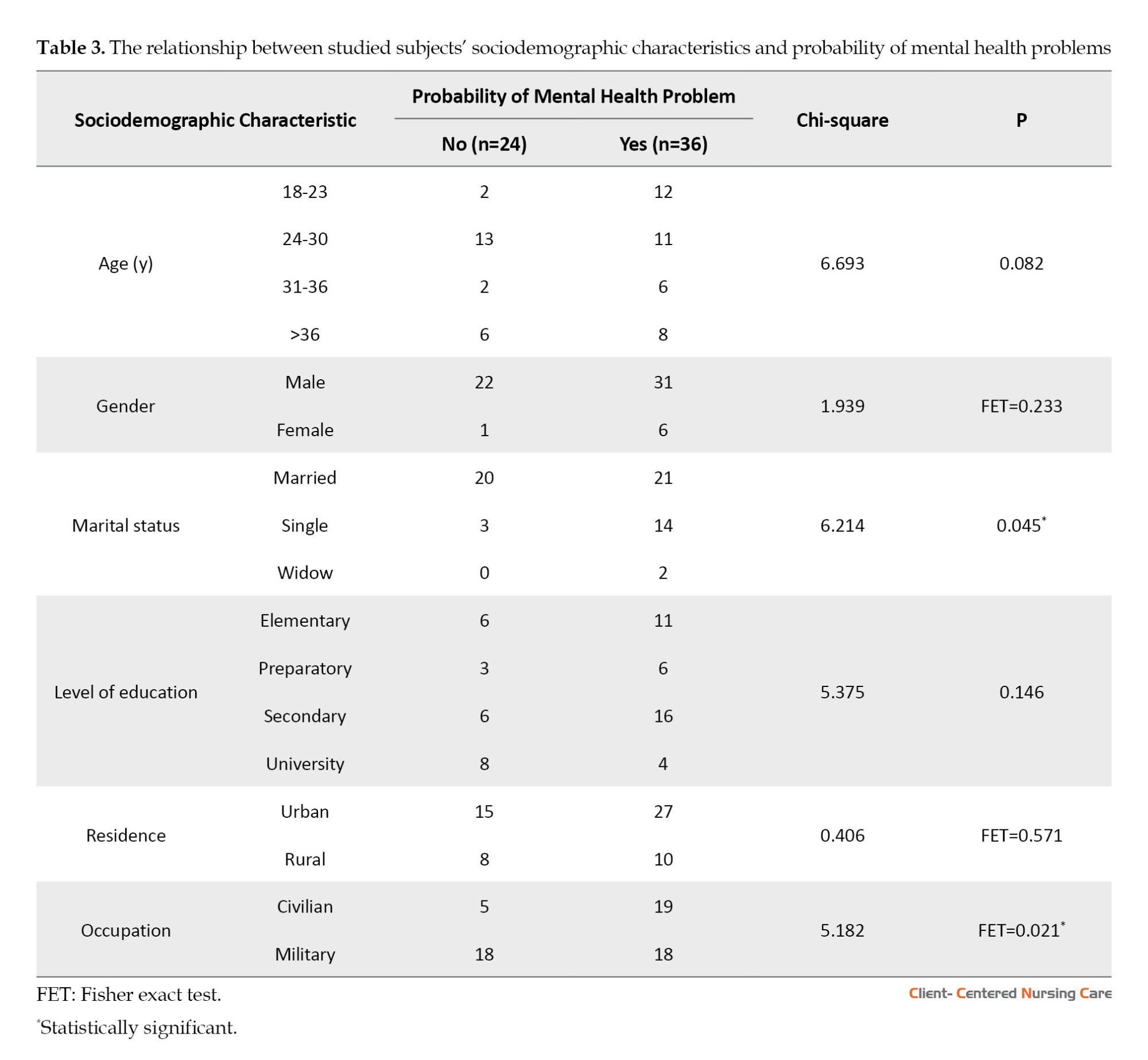
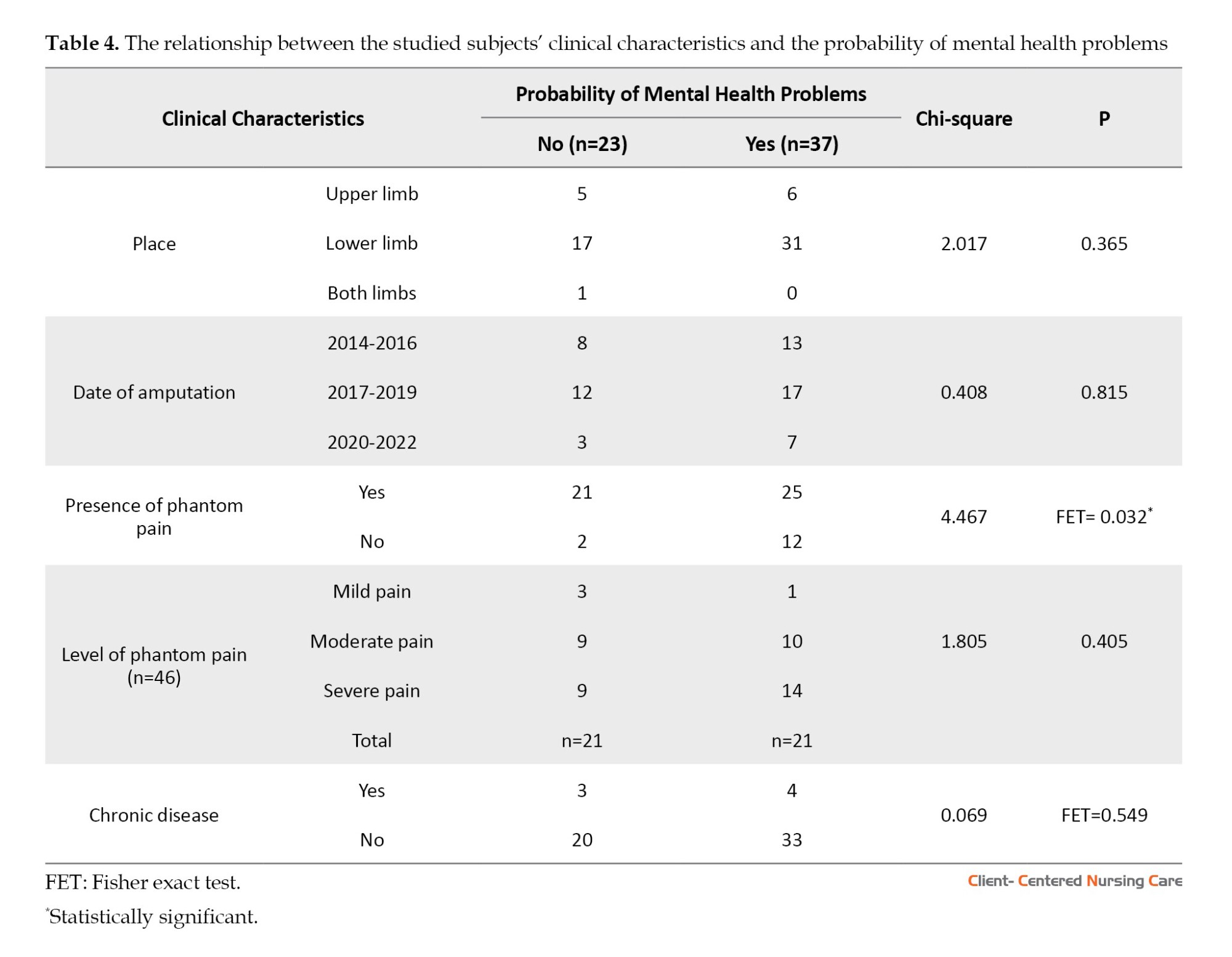
Table 4 presents the relationship between the studied subjects’ clinical characteristics and the probability of mental health problems. Among individuals with the likelihood of mental health problems, 25(67.6%) reported phantom pain, while 12(32.4%) did not. This finding suggests that individuals with phantom pain are more likely to experience mental health problems. However, there is no association between the place of amputation, date of amputation, level of pain and chronic diseases, and the probability of psychiatric disorders (P>0.05).
There were no statistically significant relationships between almost all subjects’ sociodemographic characteristics and depression state. The only significant association was found in connection with gender and depression state (P=0.036), with the females having more severe depression than males. It is worth mentioning that there was no significant relationship between the clinical characteristics of the subjects and their depression state (P>0.05).
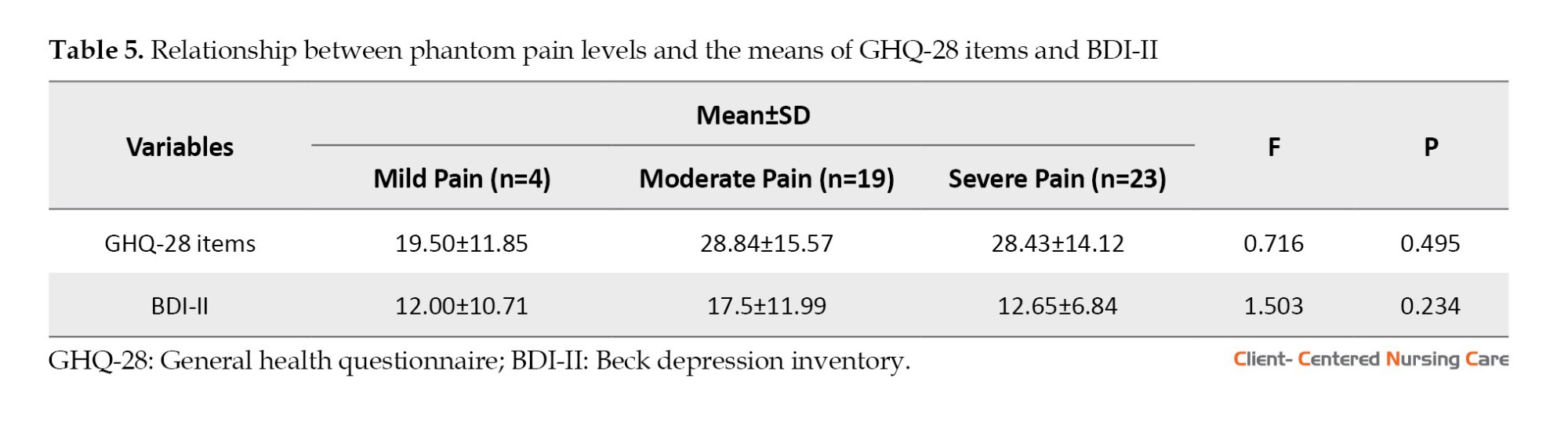
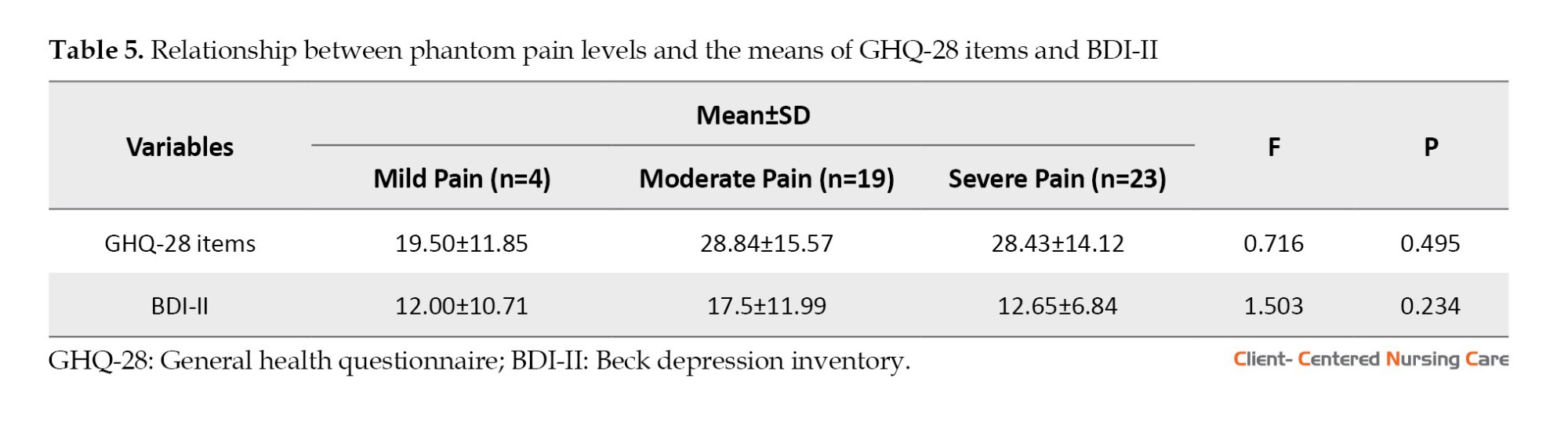
Table 5 shows no association between the levels of phantom pain and the probability of the presence of mental health problems and depression, with P of 0.495 and 0.234, respectively.
Discussion
Limb loss as a devastating injury creates a significant health burden, affecting the physical and emotional well-being of victims, as well as impacting their families, society, and health care services (Sahu et al., 2016). In Yemen, amputation results mainly from a blast, a mine, or sustaining a gunshot. According to the American Center for Law and Justice (ACLJ), 75% of those affected by landmines will suffer permanent disabilities and lifelong psychological distress (Dashela, 2022). In this regard, this study was conducted to evaluate depression, phantom pain, and the probability of psychiatric disorders among Yemenis with amputated limbs as a result of the recent conflict.
Concerning the sociodemographic characteristics of the sample, most study victims were male and under 30 years old. This finding is congruent with studies conducted in countries facing civil conflicts. Previous studies in Syria and Pakistan concluded that most amputees are young and male (Ikram et al., 2014; Nizamli, 2020).
However, this finding is contrary to the finding in countries not suffering from civil conflicts, where the leading cause of amputations is physical diseases, such as diabetes mellitus and infection. For example, the average age of American amputees is 53.5±11 years (Petersen et al., 2023).
Unfortunately, young victims will live most of their lives with pain, disability, and psychological problems that undermine their quality of life. Accordingly, they require great attention to provide the best possible health care to reduce this suffering and enhance their quality of life. Younger participants in previous studies have shown limited acceptance of their new identity as amputees, and this has negatively impacted their self-esteem among family and loved ones (Akarsu et al., 2013; Weiss, 2013).
Regarding the clinical characteristics of the study subjects, the majority of war-related amputations involved the lower limb, and most patients had undergone amputation of one limb. This finding is congruent with an analysis of amputations that was conducted in 2016 in south Ukraine on the victims of actual combat conflict (Ie & Bespalenko, 2016).
However, almost all of the studied subjects were free from chronic diseases, which is related to the fact that most conflict victims were young and physically fit. Rehabilitative therapists should consider these advantages during the rehabilitation process. It has been shown that young amputees undergoing active physical therapy have better improvement in using prostheses and gait skills. Moreover, their musculo-articular and functional status will be enhanced, improving their psychoemotional state (Herasymenko et al., 2018).
Psychologically, the present study found that the likelihood of mental health problems, depression, and phantom pain was high among amputees. This finding is consistent with recent research on conflict victims in Uganda (Okello et al., 2022). Furthermore, this finding is consistent with another study that reported a prevalence of psychiatric disorders among amputees ranging from 32% to 84%, depression rates from 10.4% to 63%, and post-traumatic stress disorder (3.3% to 56.3%) (Sahu et al., 2016). Furthermore, the current study shows that the possibility of mental health problems and depression is common among amputees, even after years of amputation.
In the same context, previous studies (Ali & Haider, 2017; Khan et al., 2018) have concluded the same result. Ali & Haider (2017) examined psychological adjustment among 100 adult amputees in Peshawar, Pakistan, and found that factors like gender, age, and cause of amputation influenced adjustment levels. Nearly all participants experienced psychological maladjustment, with males and younger adults showing greater distress, while planned medical amputations led to fewer adjustment issues compared to unplanned accidental amputations. Similarly, Khan et al. (2018), in a systematic review of anxiety and depression following traumatic amputation, highlighted the high prevalence of mental health challenges among amputees and stressed the need for comprehensive rehabilitation to address these physical, psychological, and socioeconomic impacts. Moreover, according to another study, depression and anxiety are moderately high up to two years after amputation (Waqar et al., 2015).
As for depression, psychiatric disorders were still present after a considerable period of limb loss. This finding is supported by another study, which represented that more than half of the traumatic amputees in Gaza have reported psychological distress, with symptoms persisting for several years following amputation (Heszlein-Lossius et al., 2019). In the same context, lower limb injury is associated with significant psychological distress even years after amputation (McCarthy et al., 2003).
Most of the subjects in our study suffered from the presence of phantom pain, which is also shown in other related studies (Abdi, 2022; Sahu et al., 2016). In the same context, a longitudinal study reported these false sensations in 50%–85% of amputees, with varying intensity and duration (Margalit et al., 2013). Phantom pain is associated with feelings of depression (Murray & Forshaw, 2013) and mood dysregulation (Trevelyan et al., 2016) and predisposes the person to accidents (Senra et al., 2012). This aspect of amputation generates frustration and stress, and it can become a threat to the rehabilitation process and the psychological and physical well-being of the person (Roșca et al., 2021)
Our findings indicate a positive and direct relationship between the presence of phantom pain and mental health problems. This outcome suggests that individuals with phantom pain are at increased risk of experiencing mental health issues. This finding is consistent with the study by Hogan et al. (2022), which examined over 44000 patients with below-knee amputations and found that those with phantom limb syndrome had significantly higher rates of psychiatric comorbidities compared to individuals without documented phantom pain. However, in contrast to our study, there is another study that did not report any association between the presence or intensity of phantom pain and psychological problems (Gunterstockman et al., 2023). It has also been shown in a study that depression in younger amputees is not related to the presence of phantom pain (Padovani et al., 2015). Along the same line, another study indicated that depression and mental health may be associated with the disability itself rather than the presence of phantom pain (Whyte & Niven, 2001). The difference in the results could be due to the type of amputation, as in our study, most of the samples had lower limb amputations. Also, the impact of horrific war memories and other personal and social characteristics could play a role in the difference in results. The present study shows that the probability of the presence of mental health problems among amputees is higher in civilians than in veterans. This result might be attributed to receiving veterans’ financial support. Many of them consider it as a sacrifice for their country, while civilians usually do not receive support, and their loss of a limb is accidental under being at the wrong place at the wrong time. This explanation is supported by previous studies that argue that amputees’ spiritual beliefs play a crucial role in stabilizing their lives, providing meaning for the experience of disability, and assisting them in coping with the situations (Gündüz et al., 2024). Additionally, veterans receive financial support, contributing to their lower distress levels. This view is supported by another study showing that psychological distress is associated with reduced financial income after amputation and that the frequency of pain is higher among the poorest patients and increases with decreasing family income (Geiling et al., 2012).
Similarly, single patients in this study were at greater risk of developing psychiatric disorders than married patients. This finding explains the importance of family support. Previous studies have concluded that family support is the primary source of psychological strength among amputees (Abouammoh et al., 2021; Valizadeh et al., 2014). Therefore, rehabilitation centers should involve the patient’s family members in educational programs to enable them to understand the psychological distress that disrupts the lives of amputees and to be able to help the patient overcome it or at least reduce it to improve the effectiveness of the rehabilitation process.
Limitations of this study include its cross-sectional design, which does not allow for causal relationships; self-report questionnaires may also have introduced bias, as some subjects may have under- or over-reported their phantom pain, depressive status, and mental health status. Potential issues related to sample size and generalizability, limited demographic diversity, and focus on specific populations may also impact the applicability of the findings to a broader group of amputees.
Conclusion
Victims of conflict-related amputation face serious mental health problems associated with complex trauma and disability. Therefore, rehabilitation professionals need to pay attention to psychiatric disorders and phantom pain experiences among patients with war-related amputation. However, being married and having a military job appeared to be protective against psychiatric disorders among amputees in the Yemeni war. Educating the family, caregivers, and peers about the physical and psychological needs of patients with amputated limbs is crucial for holistic care and improving the quality of their lives. To increase generalizability, the researchers suggest collecting data from a larger sample size and more diverse geographical locations in Yemen.
Ethical Considerations
Compliance with ethical guidelines
Official approval was obtained from the Dean of the Faculty of Medicine and Health Sciences and the directors of the KS Relief Center (Code: 2022-11-362). Consent was obtained from each subject after the study’s purpose was explained. The anonymity, privacy, and confidentiality of the subjects were assured. Participation was entirely voluntary, and withdrawal from the study did not affect the care provided.
Funding
This research received no specific grant from public, commercial, or not-for-profit funding agencies.
Authors' contributions
Conceptualization, supervision, analysis, and writing the initial draft: Fuad Taleb, and Asmaa Altahari; Data collection: Morad Mohammed, Eman Alemrany, Enas AL-a'ameri, Hassam Alwageeh, Samah Alhijri, Ayat AlHamdany, Khadija Ahmed, and Aziza Alazazi Data entry, and writing: Morad Mohammed, Eman Alemrany, and Enas AL-a'ameri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors especially thank Fathi Alqadasi, Director of the King Salman Humanitarian Aid and Relief Center, for his cooperation and also thank the nursing and rehabilitation staff.
References
Abouammoh, N., Aldebeya, W. & Abuzaid, R., 2021. Experiences and needs of patients with lower limb amputation in Saudi Arabia: A qualitative study. Eastern Mediterranean Health Journal, 27(4), pp. 407-13. [DOI:10.26719/emhj.20.124] [PMID]
Akarsu, S., et al., 2013. Quality of life and functionality after lower limb amputations: comparison between uni-vs. bilateral amputee patients. Prosthetics and Orthotics International, 37(1), pp. 9-13. [DOI:10.1177/0309364612438795] [PMID]
Alansari, B. M., 2006. Internal consistency of an Arabic adaptation of the Beck Depression Inventory-II with college students in eighteen Arab countries. Social Behavior and Personality: An International Journal, 34(4), pp. 425-30. [Link]
Alhamad, A. & Al-Faris, E. A., 1998. The validation of the general health questionnaire (GHQ-28) in a primary care setting in Saudi Arabia. Journal of Family & Community Medicine, 5(1), pp. 13-19. [PMID]
Ali, S. & Haider, S. K., 2017. Psychological adjustment to amputation: variations on the bases of sex, age and cause of limb loss. Journal of Ayub Medical College Abbottabad, 29(2), pp. 303-7. [PMID]
Barth, C. A., et al., 2021. Retrospective observational study of characteristics of persons with amputations accessing International Committee of the Red Cross (ICRC) rehabilitation centres in five conflict and postconflict countries. BMJ Open, 11(12), pp. e049533. [DOI:10.1136/bmjopen-2021-049533] [PMID]
Beck, A. T., Steer, R. A. & Brown, G. K., 1996. Beck Depression Inventory Manual (2nd ed.). San Antonio, TX: Psychological Corporation. [DOI:10.1037/t00742-000]
Culp, C. & Abdi, S., 2022. Current understanding of phantom pain and its treatment. Pain Physician, 25(7), PP. E941–57. [PMID]
Culp, C. J. & Abdi, S., 2022. Current understanding of phantom pain and its treatment. Pain Physician, 25(7), pp. E941-57. [PMID]
Dashela, A., 2022. The Calamity of Landmines in Yemen. Washington: Sada. [Link]
Ferguson, A. D., Sperber Richie, B. & Gomez, M. J., 2004. Psychological factors after traumatic amputation in landmine survivors: the bridge between physical healing and full recovery. Disability and Rehabilitation, 26(14-15), pp. 931-8. [DOI:10.1080/09638280410001708968] [PMID]
Fuchs, X., Flor, H. & Bekrater-Bodmann, R., 2018. Psychological factors associated with phantom limb pain: A review of recent findings. Pain Research and Management, 2018(1), pp. 5080123. [DOI:10.1155/2018/5080123] [PMID]
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators., 2017. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England), 390(10100), pp. 1211–59. [PMID]
Geiling, J., Rosen, J. M. & Edwards, R. D., 2012. Medical costs of war in 2035: Long-term care challenges for veterans of Iraq and Afghanistan. Military Medicine, 177(11), pp. 1235-44. [DOI:10.7205/MILMED-D-12-00031] [PMID]
Gilg, A., 2016. The impact of amputation on Body Image [Honors Theses]. Mississippi: The University of Southern Mississippi. [Link]
Goldberg, D. P. & Hillier, V. F., 1979. A scaled version of the General Health Questionnaire. Psychological Medicine, 9(1), pp. 139-45. [DOI:10.1017/S0033291700021644] [PMID]
Graziottin, A., Cuccarollo, A. & Donini, M., 2022. Diagnosi e cura del dolore sessuale dopo il parto. pp. 100-9. [Link]
Gündüz, E. S., Durmaz, M. & Aydın, B. K., 2024. “ Both My Body and My Spirit are Incomplete”: Care needs and difficulties experienced by patients with amputation. Turkish Journal of Diabetes and Obesity, 8(2), pp. 191-201. [DOI:10.25048/tudod.1469602]
Gunterstockman, B. M., et al., 2023. Relationship between phantom limb pain, function, and psychosocial health in individuals with lower-limb loss. Prosthetics and Orthotics International, 47(2), pp. 181-8. [DOI:10.1097/PXR.0000000000000191] [PMID]
Herasymenko, O., et al., 2018. Effectiveness of physical therapy interventions for young adults after lower limb transtibial amputation. Journal of Physical Education and Sport, 18(2), pp. 1084-91. [Link]
Heszlein-Lossius, H. E., et al., 2019. Does pain, psychological distress and deteriorated family economy follow traumatic amputation among war casualties? A retrospective, cross-sectional study from Gaza. BMJ Open, 9(6), pp. e029892.[DOI:10.1136/bmjopen-2019-029892] [PMID]
Hogan, W. B., et al., 2022. Phantom limb syndrome: Assessment of psychiatric and medical comorbidities associated with Phantom pain in 44,028 below knee amputees. Injury, 53(11), pp. 3697-701. [DOI:10.1016/j.injury.2022.09.018] [PMID]
Humanity. & Inclusion., 2017. Urgent need for rehabilitation services in Yemen. Georgia: Humanity & Inclusion. [Link]
Ie, T. & Bespalenko, A., 2016. Analysis of limb amputations during armed conflict at the East of Ukraine. Norwegian Journal of development of the International Science, (1), pp. 79-80. [Link]
Ikram, M., et al., 2014. Frequency and sociodemographic predictors of clinical depression in combat amputees at a military rehabilitation setup. Rawal Medical Journal, 39(2), pp. 167-70. [Link]
Katz, J., 1993. Phantom limb experience in children and adults: Cognitive and affective contributions. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 25(3), pp. 335-54. [Link]
Khan, M. J., Dogar, S. F. & Masroor, U., 2018. Family relations, quality of life and post-traumatic stress among amputees and prosthetics. Pakistan Armed Forces Medical Journal, 68(1), pp. 125-30. [Link]
Margalit, D., et al., 2013. Phantom fighters: Coping mechanisms of amputee patients with phantom limb pain: A longitudinal study. Open Journal of Orthopedics, 3(07), pp. 300-5. [DOI:10.4236/ojo.2013.37055]
McCarthy, M. L., et al., 2003. Psychological distress associated with severe lower-limb injury. The Journal of Bone and Joint Surgery. American volume, 85(9), pp. 1689–97.[DOI:10.2106/00004623-200309000-00006] [PMID]
McDonald, C. L., et al., 2021. Global prevalence of traumatic non-fatal limb amputation. Prosthetics and Orthotics International, 45(2), pp. 105–14. [DOI:10.1177/0309364620972258] [PMID]
Monitoring and Research Committee., et al., 2022. Landmine Monitor. Geneva: International Campaign to Ban Landmines. [Link]
Murray, C. D. & Forshaw, M. J., 2013. The experience of amputation and prosthesis use for adults: A metasynthesis. Disability and Rehabilitation, 35(14), pp. 1133-42. [DOI:10.3109/09638288.2012.723790] [PMID]
Muzaffar, N., et al., 2012. Psychiatric comorbidity in amputees with average sociodemographic status and the role of theologic and family support in a conflict zone. Australasian Journal of Disaster and Trauma Studies, 2012(1), pp. 31-8. [Link]
Naja, S., et al., 2019. Psychometric properties of the Arabic version of EPDS and BDI-II as a screening tool for antenatal depression: Evidence from Qatar. BMJ Open, 9(9), pp. e030365.[DOI:10.1136/bmjopen-2019-030365] [PMID]
Ngo, L. & Bjork, A., 2018. Disability in the Arab Region. New York: United Nations. [Link]
Nizamli, F. M., 2020. Quality of life among Syrian patients with war-related lower limb amputation at the Military Hospital in Lattakia. International Journal of Nursing Sciences, 7(3), pp. 297-302. [DOI:10.1016/j.ijnss.2020.05.001] [PMID]
Okello, T. R., et al., 2022. Major Limb Loss and Prosthesis Use in the Post Conflict era in Acholi Sub-Region, Northern Uganda International Journal of Science Academic Research, 3(6), pp. 3998-4004. [Link]
Padovani, M. T., et al., 2015. Anxiety, depression and quality of life in individuals with phantom limb pain. Acta Ortopedica Brasileira, 23(2), pp. 107–10. [DOI:10.1590/1413-78522015230200990] [PMID]
Petersen, B., Sparto, P. & Fisher, L., 2023. Clinical measures of balance and gait cannot differentiate somatosensory impairments in people with lower-limb amputation. Gait & Posture, 99, pp. 104-10. [DOI:10.1016/j.gaitpost.2022.10.018] [PMID]
Qahtani, B. A., 2021. KSrelief-supported Artificial Limbs Centers in Yemen Have Provided Services for 25,000+ Patients. Riyadh: King Salman Humanitarian Aid and Relief Center. [Link]
Ramaraj, P., et al., 2023. Epidemiology of traumatically injured Yemeni civilians treated at the Omani National Trauma Centre over a 2-year period: A retrospective cohort study. BMJ Military Health, 171(1), pp. 19–25. [DOI:10.1136/military-2023-002509] [PMID]
Roșca, A. C., et al., 2021. Psychological consequences in patients with amputation of a limb. An interpretative-phenomenological analysis. Frontiers in Psychology, 12, pp. 537493. [DOI:10.3389/fpsyg.2021.537493] [PMID]
Roullet, S., et al., 2009. [Phantom limb pain: from physiopathology to prevention (French)]. Annales Francaises D'anesthesie et de Reanimation, 28(5), pp. 460–72. [DOI:10.1016/j.annfar.2009.03.012] [PMID]
Sahu, A., et al., 2016. Psychological effects of amputation: A review of studies from India. Industrial Psychiatry Journal, 25(1), pp. 4-10. [DOI:10.4103/0972-6748.196041] [PMID]
Senra, H., et al., 2012. Beyond the body image: A qualitative study on how adults experience lower limb amputation. Clinical Rehabilitation, 26(2), pp. 180–91. [DOI:10.1177/0269215511410731] [PMID]
Sky News Arabia., 2018. Saudi Arabia launches “Masam” project to clear landmines in Yemen. Viewe 25 June 2018.
Stancu, B., et al., 2016. Medical, social and christian aspects in patients with major lower limb amputations. Journal for the Study of Religions and Ideologies, 15(43), pp. 82-101. [Link]
Tomilenko, M., 2023. Bridging Additive Manufacturing and Assistive Technology Networks in Ukraine Through Systems Mapping and Education [MA thesis]. New York: New York University Tandon School of Engineering. [Link]
Trevelyan, E. G., Turner, W. A. & Robinson, N., 2016. Perceptions of phantom limb pain in lower limb amputees and its effect on quality of life: A qualitative study. British Journal of Pain, 10(2), pp. 70-7. [DOI:10.1177/2049463715590884] [PMID]
United Nations Office for the Coordination of Humanitarian Affairs (OCHA)., 2021. Yemen humanitarian needs overview. New York: United Nations Office for the Coordination of Humanitarian Affairs. [Link]
Valizadeh, S., et al., 2014. The perception of trauma patients from social support in adjustment to lower-limb amputation: A qualitative study. Indian Journal of Palliative Care, 20(3), pp. 229-38. [DOI:10.4103/0973-1075.138401] [PMID]
Waqar, S., Noor, R. & Khan, M. M. H.,2015. Depression, anxiety & psychological adjustment among amputees. International Journal of Rehabilitation Research, 4(2), pp. 14-18. [Link]
Weiss, G., 2013. Body images: Embodiment as intercorporeality. New York: Routledge. [DOI:10.4324/9780203699003]
Whyte, A. S. & Niven, C. A., 2001. Psychological distress in amputees with phantom limb pain. Journal of Pain and Symptom Management, 22(5), pp. 938–46. [DOI:10.1016/S0885-3924(01)00352-9] [PMID]
With increasing global unrest and conflicts worldwide, the cases of amputation are rising, resulting in broken health systems and a fragmented continuum of care (Barth et al., 2021). Amputation disrupts an individual’s social values, impacting their sense of vitality, body image, and fitness, and can often be perceived as a sign of personal loss or failure (Stancu et al., 2016).
The data on war-related amputations and injuries among Yemeni civilians is based on findings from a study of 254 patients treated at the Omani National Trauma Center. This retrospective cohort study documented injuries from 2015 to 2017, showing that blast (63%) and gunshot wounds (29%) were the primary causes, leading to traumatic amputations in 5% of cases and permanent disabilities in 50% (Ramaraj et al., 2023).
Amputation is a significant concern around the world. In 2017, it was estimated that 57.7 million people were living with an amputated limb due to trauma (McDonald et al., 2021). Unfortunately, these injuries are becoming increasingly common in wartime; for example, as of January 2023, over 40000 Ukrainians have been injured in the recent war, and it is estimated that up to 33% of injuries result in amputations (Tomilenko, 2023).
Yemen had the highest disability burden, measured by years lived with disability, among 195 countries (Vos et al., 2017). Thousands of people have lost limbs in Yemen since the conflict started in 2015. The United Nations (UN) estimates that about 2.2% of people in Yemen have at least one disability (Ngo & Bjork, 2018). The health care system in Yemen collapsed due to war. According to the UN, only 50% of health care facilities are fully functional, and more than 80% of the Yemeni population faces significant challenges in reaching health care services (OCHA, 2021). Explosive weapons cause more severe and complex disabilities, such as amputations and spinal cord injuries (Humanity & Inclusion, 2017). Millions of landmines and remnants of war remain in Ukraine, Yemen, Syria, Afghanistan, and other contaminated areas, putting people’s lives and work at risk (Loddo, 2022).
Amputation negatively impacts function, sensation, and body image, leading to financial difficulties, isolation, and low self-esteem. Post-amputation pain and suffering can also disrupt personal relationships, including marriage (Gilg, 2016). While mental health comorbidity is prevalent in amputees (Muzaffar et al., 2012), the majority of them have not received comprehensive care that includes psychological management (Barth et al., 2021).
A narrative review study that included research from the United States, France, Canada, Italy, Germany, Denmark, Japan, and the United Kingdom, among others, shows that phantom limb pain (PLP) is experienced by up to 87% of amputees. It is a complex phenomenon characterized by pain sensations such as stabbing, throbbing, burning, or cramping in a limb or organ that has been removed, commonly following amputation. As a result of unknown causes involving both central and peripheral nervous system changes—such as cortical reorganization and neuroma formation—a personalized approach is required due to the lack of a single gold-standard treatment. This approach may combine various therapies, including pharmacologic treatments like opioids, n-methyl-D-aspartate receptor antagonists like ketamine, antidepressants, and other treatments such as mirror therapy, motor imagery, and targeted muscle reinnervation (Culp & Abdi, 2022).
It has been shown that PLP could be triggered and exacerbated by psychological factors such as stress (Fuchs et al., 2018). However, Katz (1993) suggested that while amputees suffering from PLP exhibited higher than normal levels of psychological and emotional distress, including depression, it did not imply a causal relationship. The consensus is that there is no difference in the prevalence of pain of psychological origin among amputees and the general population. Therefore, phantom pain and depression may co-occur, but one is not necessarily the cause of the other.
Recovery from traumatic amputation needs to be comprehensive and coordinated and requires addressing the personal’s physical, psychological, and socioeconomic needs within the context of family, community, and the sociocultural environment in which they live (Ferguson et al., 2004). Furthermore, awareness of the co-morbid psychiatric disorders in amputated patients can be invaluable in proper management and preventing further chronic debilitating disorders associated with amputation (Muzaffar et al., 2012).
To the best of our knowledge, no prior study has examined the prevalence of phantom pain and the effect of amputation on the mental health and mood state of Yemenis with amputated limbs due to the recent conflict. Therefore, our study aimed to assess phantom pain, mental health problems, and depression among amputee victims of the recent Yemeni conflict.
Materials and Methods
Design, setting, and sample
A descriptive cross-sectional research design was utilized to fulfill the research aim. This study was conducted in Taiz, where King Salman Humanitarian Aid & Relief Center (KSrelief) established and operated the Artificial Limbs Center over three phases: Producing a wide range of prosthetic devices, providing physical and psychological rehabilitation for patients, and meeting patients’ medical and non-medical needs. To date, 8530 patients have received services at the Taiz Center through the support of KSrelief (Qahtani, 2021).
A convenience sample of 60 adult patients with amputated limbs admitted to the above-mentioned setting were recruited to participate in this study. There are no official statistics on the number of amputees due to the recent conflict; however, according to media sources, the number of amputees between December 2014 and December 2016 (the period of intensified conflict in Taiz) reached 274 cases (Sky News Arabia, 2018). The sample of 60 cases was chosen due to practical constraints and the limited time available. Patients who met the following criteria were eligible for the study: Consent to participate, age 18 years and older, ability to communicate, amputation due to recent war, and no cognitive impairment.
Instruments
The data were collected using a sociodemographic and clinical data sheet, general health questionnaire (GHQ-28 items), and Beck depression inventory-II (BDI-II).
Sociodemographic and clinical data sheet
The researchers developed this sheet after reviewing the relevant literature (Ali & Haider, 2017; Ngo & Bjork, 2018; Nizamli, 2020). For pain level determination, we reviewed and relied on the studies by Roullet et al. (2009) and Graziottin et al. (2022). This sheet was attached to the tools used in the study and consisted of two parts:
Part 1 covers sociodemographic data, including the respondent’s age, gender, marital status, level of education, residence (classified as urban or rural), and occupation.
Part 2 covers clinical data, which includes the type and date of amputation, presence of phantom pain, description and level of phantom pain (assessed using a visual and verbal pain scale: 1-3 for mild pain with minimal impact on activities of daily living [ADLs], 4-6 for moderate pain with moderate impact on ADLs, and 7-10 for severe pain with significant implications on ADLs). It also collects information on permanent medications, the probability of mental disorders, and depression status.
GHQ-28
This tool, which was developed by Goldberg & Hillier (1979), has 28 items in four subscales: Somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression. Each subscale has 7 items, rated on a 4-point Likert scale (0: Never; 1: Almost never; 2: sometimes; 3: Often), and the maximum possible score on the questionnaire is 84. To differentiate the studied subjects with mental health problems from those without problems, a score of 23 and above indicates a mental health problem, and a score below 23 indicates no mental health problem. The Arabic version of GHQ-28 was used in Saudi Arabia and Lebanon and was valid and reliable, with a Cronbach α reliability estimate of 0.89 (Alhamad & Al-Faris, 1998).
BDI-II
This tool is a 1996 revision of BDI. It is widely used to assess the severity of depression (Beck et al., 1996). BDI-II contains 21 questions, each with four answers scored on a scale of 0 to 3, resulting in a total score range of 0 to 63. Lower total scores indicate more severe depressive symptoms during the past two weeks. The Arabic version of BDI-II was used in Qatar, Egypt, and most Arabic countries and was valid and reliable, with Cronbach α values ranging between 0.82-0.93 (Alansari, 2006; Naja et al., 2019). The scores of a depression state on the BDI were categorized as follows: 0-5 indicating “non-depressed,” 6-11 “marginal depression,” 12-22 “simple depression,” 23- 30 “moderate depression,” 31-40 “severe depression,” and 41-60 indicating “more severe depression.”
Results
Table 1 shows the sociodemographic characteristics of the studied subjects. It appears from this Table that the majority of adults with amputated limbs due to the recent conflict in Yemen are less than 30 years old (63.3%). The highest percentage are males, 88.3%, and married, 68.3%. Regarding educational level, more than a third of the study population (36.7%) have a secondary education. Moreover, more than two-thirds of the studied subjects (70.0%) live in urban areas. Concerning subjects’ occupations, 60% are military, and 40% are civilian.
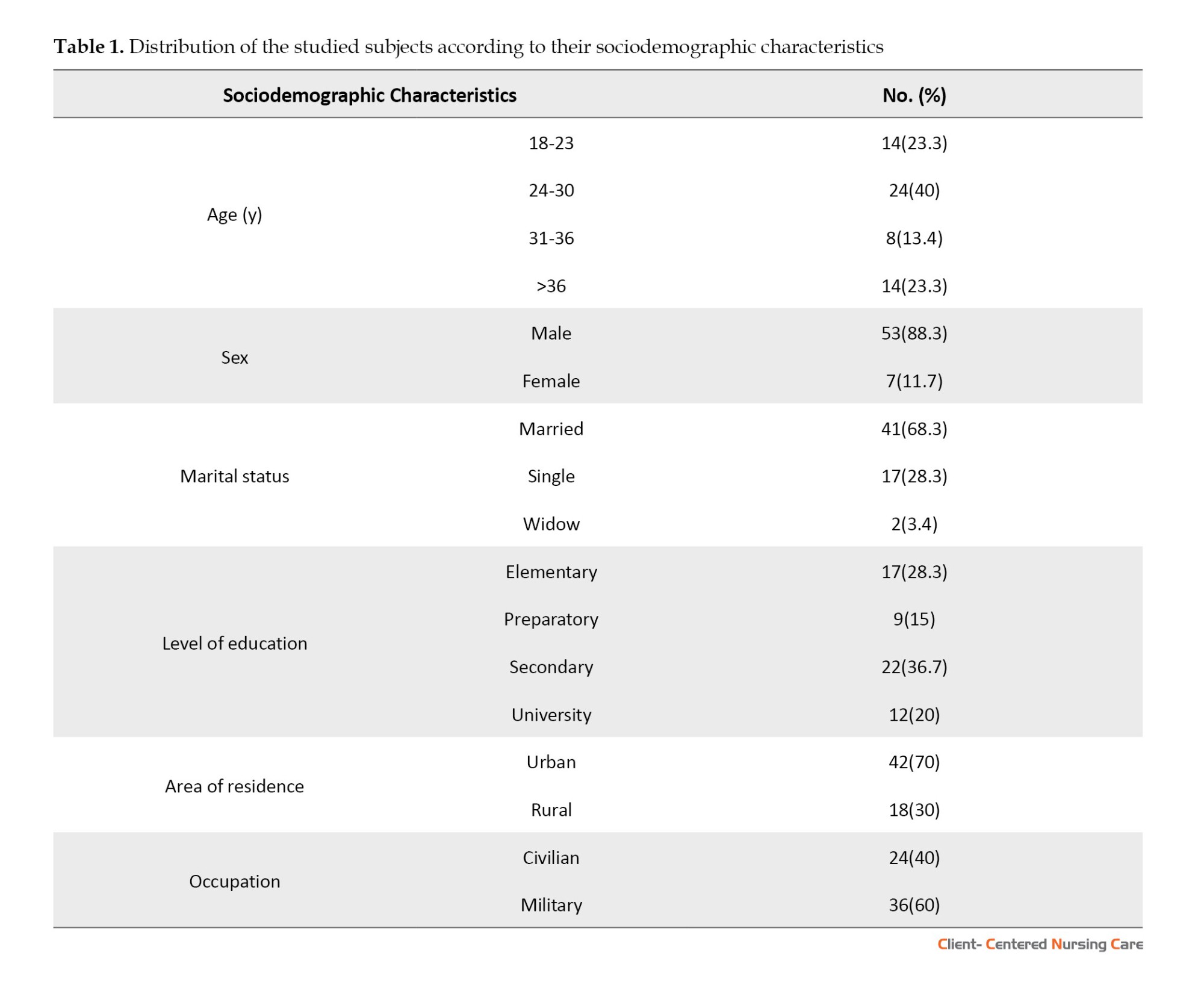
Table 2 displays the clinical characteristics of the studied subjects. Concerning the type of amputation, about 80% of the patients have lower limb amputation, and more than three-quarters of them (83.3%) lost their limbs before 2019. About the presence of phantom pain, 80% of the participants suffer from it, and one-half of them have severe pain. Considering physical health, most studied subjects (88.3%) are free from chronic diseases. Regarding the mental health of the studied subjects, this table indicates that 61.7% might have mental health problems, and almost all the studied subjects (93.4%) have some degree of depression; 75.0% of them have marginal or simple depression.
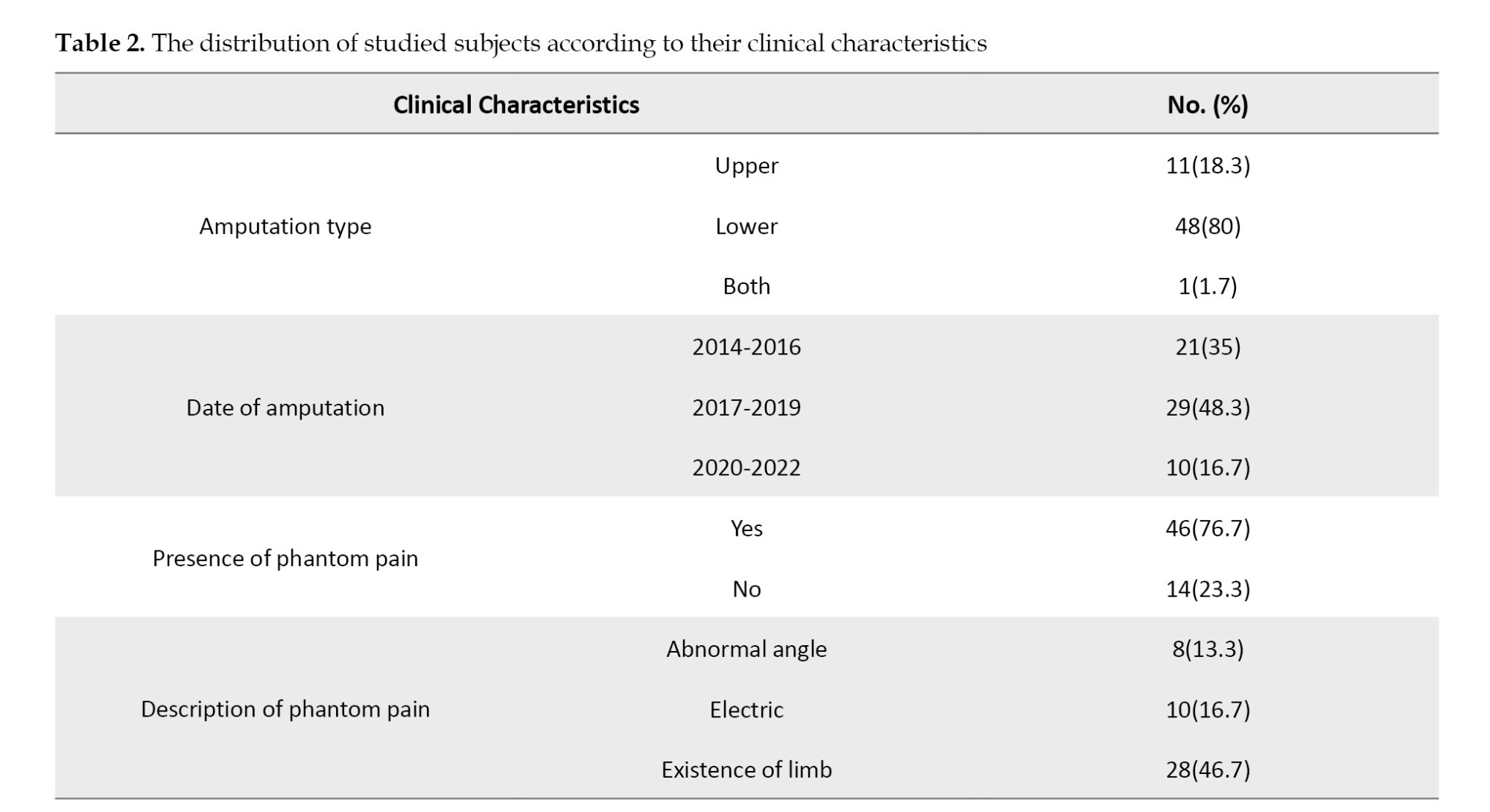
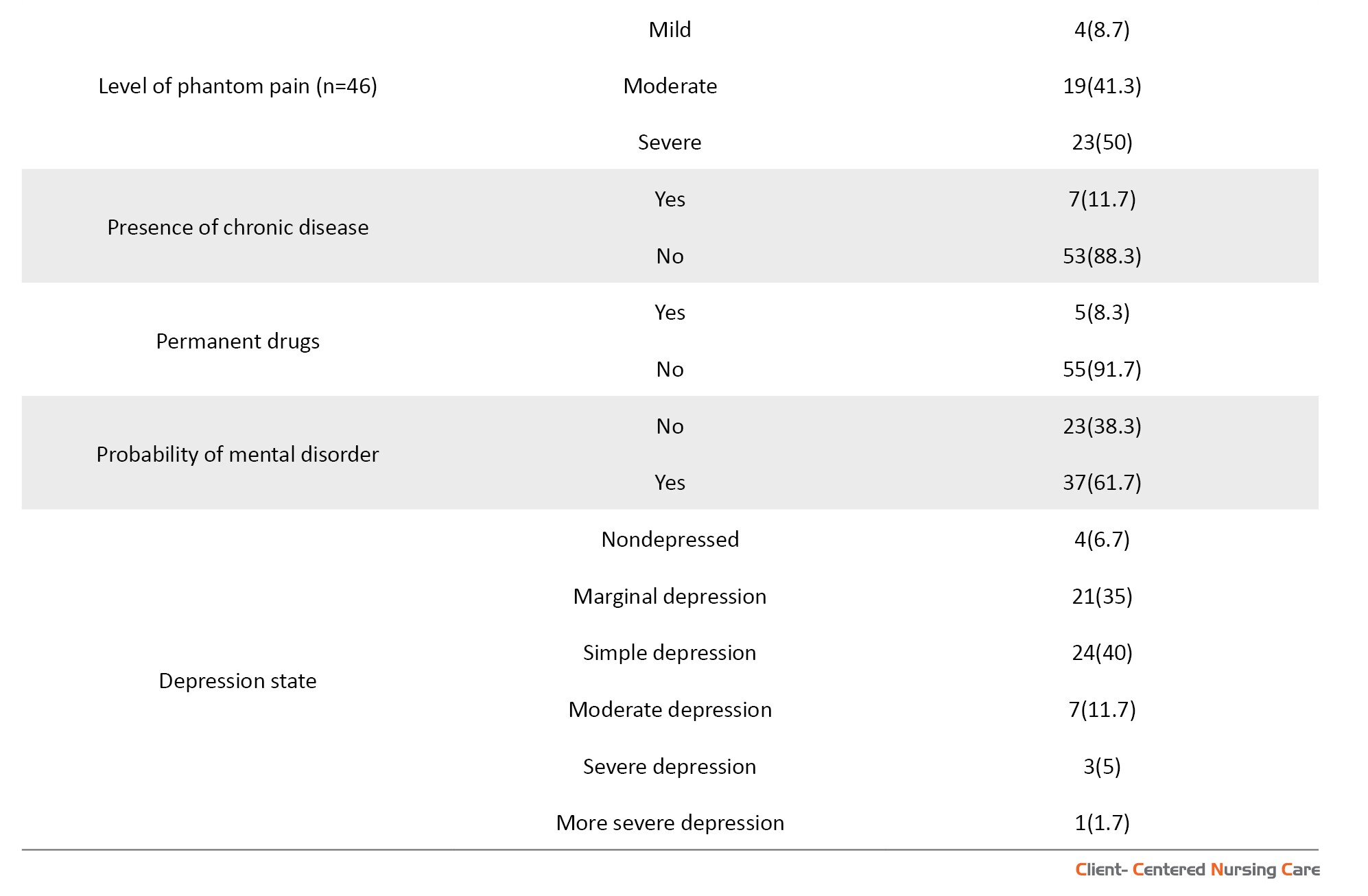
Table 3 reveals the relationship between the studied subject’s mental health problems and their sociodemographic characteristics. The table shows no statistically significant relationships between age, gender, education level, and residence of the studied subjects and the probability of mental health problems (P>0.05). On the other hand, it shows a statistically significant association between the likelihood of mental health problems and the presence of a partner and having military occupation, with P of 0.045 and 0.021, respectively.
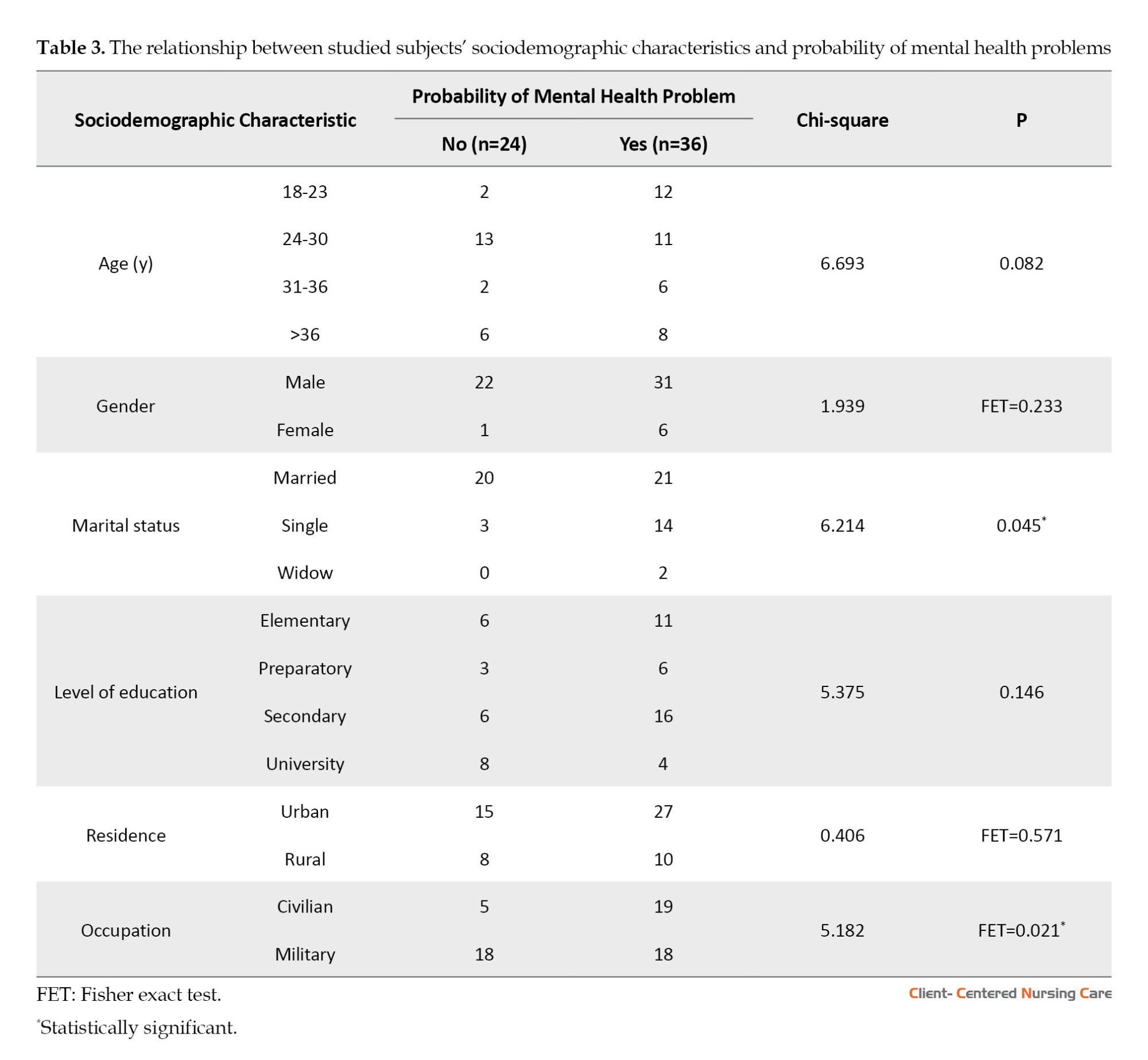
Table 4 presents the relationship between the studied subjects’ clinical characteristics and the probability of mental health problems. Among individuals with the likelihood of mental health problems, 25(67.6%) reported phantom pain, while 12(32.4%) did not. This finding suggests that individuals with phantom pain are more likely to experience mental health problems. However, there is no association between the place of amputation, date of amputation, level of pain and chronic diseases, and the probability of psychiatric disorders (P>0.05).
There were no statistically significant relationships between almost all subjects’ sociodemographic characteristics and depression state. The only significant association was found in connection with gender and depression state (P=0.036), with the females having more severe depression than males. It is worth mentioning that there was no significant relationship between the clinical characteristics of the subjects and their depression state (P>0.05).
Table 5 shows no association between the levels of phantom pain and the probability of the presence of mental health problems and depression, with P of 0.495 and 0.234, respectively.
Discussion
Limb loss as a devastating injury creates a significant health burden, affecting the physical and emotional well-being of victims, as well as impacting their families, society, and health care services (Sahu et al., 2016). In Yemen, amputation results mainly from a blast, a mine, or sustaining a gunshot. According to the American Center for Law and Justice (ACLJ), 75% of those affected by landmines will suffer permanent disabilities and lifelong psychological distress (Dashela, 2022). In this regard, this study was conducted to evaluate depression, phantom pain, and the probability of psychiatric disorders among Yemenis with amputated limbs as a result of the recent conflict.
Concerning the sociodemographic characteristics of the sample, most study victims were male and under 30 years old. This finding is congruent with studies conducted in countries facing civil conflicts. Previous studies in Syria and Pakistan concluded that most amputees are young and male (Ikram et al., 2014; Nizamli, 2020).
However, this finding is contrary to the finding in countries not suffering from civil conflicts, where the leading cause of amputations is physical diseases, such as diabetes mellitus and infection. For example, the average age of American amputees is 53.5±11 years (Petersen et al., 2023).
Unfortunately, young victims will live most of their lives with pain, disability, and psychological problems that undermine their quality of life. Accordingly, they require great attention to provide the best possible health care to reduce this suffering and enhance their quality of life. Younger participants in previous studies have shown limited acceptance of their new identity as amputees, and this has negatively impacted their self-esteem among family and loved ones (Akarsu et al., 2013; Weiss, 2013).
Regarding the clinical characteristics of the study subjects, the majority of war-related amputations involved the lower limb, and most patients had undergone amputation of one limb. This finding is congruent with an analysis of amputations that was conducted in 2016 in south Ukraine on the victims of actual combat conflict (Ie & Bespalenko, 2016).
However, almost all of the studied subjects were free from chronic diseases, which is related to the fact that most conflict victims were young and physically fit. Rehabilitative therapists should consider these advantages during the rehabilitation process. It has been shown that young amputees undergoing active physical therapy have better improvement in using prostheses and gait skills. Moreover, their musculo-articular and functional status will be enhanced, improving their psychoemotional state (Herasymenko et al., 2018).
Psychologically, the present study found that the likelihood of mental health problems, depression, and phantom pain was high among amputees. This finding is consistent with recent research on conflict victims in Uganda (Okello et al., 2022). Furthermore, this finding is consistent with another study that reported a prevalence of psychiatric disorders among amputees ranging from 32% to 84%, depression rates from 10.4% to 63%, and post-traumatic stress disorder (3.3% to 56.3%) (Sahu et al., 2016). Furthermore, the current study shows that the possibility of mental health problems and depression is common among amputees, even after years of amputation.
In the same context, previous studies (Ali & Haider, 2017; Khan et al., 2018) have concluded the same result. Ali & Haider (2017) examined psychological adjustment among 100 adult amputees in Peshawar, Pakistan, and found that factors like gender, age, and cause of amputation influenced adjustment levels. Nearly all participants experienced psychological maladjustment, with males and younger adults showing greater distress, while planned medical amputations led to fewer adjustment issues compared to unplanned accidental amputations. Similarly, Khan et al. (2018), in a systematic review of anxiety and depression following traumatic amputation, highlighted the high prevalence of mental health challenges among amputees and stressed the need for comprehensive rehabilitation to address these physical, psychological, and socioeconomic impacts. Moreover, according to another study, depression and anxiety are moderately high up to two years after amputation (Waqar et al., 2015).
As for depression, psychiatric disorders were still present after a considerable period of limb loss. This finding is supported by another study, which represented that more than half of the traumatic amputees in Gaza have reported psychological distress, with symptoms persisting for several years following amputation (Heszlein-Lossius et al., 2019). In the same context, lower limb injury is associated with significant psychological distress even years after amputation (McCarthy et al., 2003).
Most of the subjects in our study suffered from the presence of phantom pain, which is also shown in other related studies (Abdi, 2022; Sahu et al., 2016). In the same context, a longitudinal study reported these false sensations in 50%–85% of amputees, with varying intensity and duration (Margalit et al., 2013). Phantom pain is associated with feelings of depression (Murray & Forshaw, 2013) and mood dysregulation (Trevelyan et al., 2016) and predisposes the person to accidents (Senra et al., 2012). This aspect of amputation generates frustration and stress, and it can become a threat to the rehabilitation process and the psychological and physical well-being of the person (Roșca et al., 2021)
Our findings indicate a positive and direct relationship between the presence of phantom pain and mental health problems. This outcome suggests that individuals with phantom pain are at increased risk of experiencing mental health issues. This finding is consistent with the study by Hogan et al. (2022), which examined over 44000 patients with below-knee amputations and found that those with phantom limb syndrome had significantly higher rates of psychiatric comorbidities compared to individuals without documented phantom pain. However, in contrast to our study, there is another study that did not report any association between the presence or intensity of phantom pain and psychological problems (Gunterstockman et al., 2023). It has also been shown in a study that depression in younger amputees is not related to the presence of phantom pain (Padovani et al., 2015). Along the same line, another study indicated that depression and mental health may be associated with the disability itself rather than the presence of phantom pain (Whyte & Niven, 2001). The difference in the results could be due to the type of amputation, as in our study, most of the samples had lower limb amputations. Also, the impact of horrific war memories and other personal and social characteristics could play a role in the difference in results. The present study shows that the probability of the presence of mental health problems among amputees is higher in civilians than in veterans. This result might be attributed to receiving veterans’ financial support. Many of them consider it as a sacrifice for their country, while civilians usually do not receive support, and their loss of a limb is accidental under being at the wrong place at the wrong time. This explanation is supported by previous studies that argue that amputees’ spiritual beliefs play a crucial role in stabilizing their lives, providing meaning for the experience of disability, and assisting them in coping with the situations (Gündüz et al., 2024). Additionally, veterans receive financial support, contributing to their lower distress levels. This view is supported by another study showing that psychological distress is associated with reduced financial income after amputation and that the frequency of pain is higher among the poorest patients and increases with decreasing family income (Geiling et al., 2012).
Similarly, single patients in this study were at greater risk of developing psychiatric disorders than married patients. This finding explains the importance of family support. Previous studies have concluded that family support is the primary source of psychological strength among amputees (Abouammoh et al., 2021; Valizadeh et al., 2014). Therefore, rehabilitation centers should involve the patient’s family members in educational programs to enable them to understand the psychological distress that disrupts the lives of amputees and to be able to help the patient overcome it or at least reduce it to improve the effectiveness of the rehabilitation process.
Limitations of this study include its cross-sectional design, which does not allow for causal relationships; self-report questionnaires may also have introduced bias, as some subjects may have under- or over-reported their phantom pain, depressive status, and mental health status. Potential issues related to sample size and generalizability, limited demographic diversity, and focus on specific populations may also impact the applicability of the findings to a broader group of amputees.
Conclusion
Victims of conflict-related amputation face serious mental health problems associated with complex trauma and disability. Therefore, rehabilitation professionals need to pay attention to psychiatric disorders and phantom pain experiences among patients with war-related amputation. However, being married and having a military job appeared to be protective against psychiatric disorders among amputees in the Yemeni war. Educating the family, caregivers, and peers about the physical and psychological needs of patients with amputated limbs is crucial for holistic care and improving the quality of their lives. To increase generalizability, the researchers suggest collecting data from a larger sample size and more diverse geographical locations in Yemen.
Ethical Considerations
Compliance with ethical guidelines
Official approval was obtained from the Dean of the Faculty of Medicine and Health Sciences and the directors of the KS Relief Center (Code: 2022-11-362). Consent was obtained from each subject after the study’s purpose was explained. The anonymity, privacy, and confidentiality of the subjects were assured. Participation was entirely voluntary, and withdrawal from the study did not affect the care provided.
Funding
This research received no specific grant from public, commercial, or not-for-profit funding agencies.
Authors' contributions
Conceptualization, supervision, analysis, and writing the initial draft: Fuad Taleb, and Asmaa Altahari; Data collection: Morad Mohammed, Eman Alemrany, Enas AL-a'ameri, Hassam Alwageeh, Samah Alhijri, Ayat AlHamdany, Khadija Ahmed, and Aziza Alazazi Data entry, and writing: Morad Mohammed, Eman Alemrany, and Enas AL-a'ameri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors especially thank Fathi Alqadasi, Director of the King Salman Humanitarian Aid and Relief Center, for his cooperation and also thank the nursing and rehabilitation staff.
References
Abouammoh, N., Aldebeya, W. & Abuzaid, R., 2021. Experiences and needs of patients with lower limb amputation in Saudi Arabia: A qualitative study. Eastern Mediterranean Health Journal, 27(4), pp. 407-13. [DOI:10.26719/emhj.20.124] [PMID]
Akarsu, S., et al., 2013. Quality of life and functionality after lower limb amputations: comparison between uni-vs. bilateral amputee patients. Prosthetics and Orthotics International, 37(1), pp. 9-13. [DOI:10.1177/0309364612438795] [PMID]
Alansari, B. M., 2006. Internal consistency of an Arabic adaptation of the Beck Depression Inventory-II with college students in eighteen Arab countries. Social Behavior and Personality: An International Journal, 34(4), pp. 425-30. [Link]
Alhamad, A. & Al-Faris, E. A., 1998. The validation of the general health questionnaire (GHQ-28) in a primary care setting in Saudi Arabia. Journal of Family & Community Medicine, 5(1), pp. 13-19. [PMID]
Ali, S. & Haider, S. K., 2017. Psychological adjustment to amputation: variations on the bases of sex, age and cause of limb loss. Journal of Ayub Medical College Abbottabad, 29(2), pp. 303-7. [PMID]
Barth, C. A., et al., 2021. Retrospective observational study of characteristics of persons with amputations accessing International Committee of the Red Cross (ICRC) rehabilitation centres in five conflict and postconflict countries. BMJ Open, 11(12), pp. e049533. [DOI:10.1136/bmjopen-2021-049533] [PMID]
Beck, A. T., Steer, R. A. & Brown, G. K., 1996. Beck Depression Inventory Manual (2nd ed.). San Antonio, TX: Psychological Corporation. [DOI:10.1037/t00742-000]
Culp, C. & Abdi, S., 2022. Current understanding of phantom pain and its treatment. Pain Physician, 25(7), PP. E941–57. [PMID]
Culp, C. J. & Abdi, S., 2022. Current understanding of phantom pain and its treatment. Pain Physician, 25(7), pp. E941-57. [PMID]
Dashela, A., 2022. The Calamity of Landmines in Yemen. Washington: Sada. [Link]
Ferguson, A. D., Sperber Richie, B. & Gomez, M. J., 2004. Psychological factors after traumatic amputation in landmine survivors: the bridge between physical healing and full recovery. Disability and Rehabilitation, 26(14-15), pp. 931-8. [DOI:10.1080/09638280410001708968] [PMID]
Fuchs, X., Flor, H. & Bekrater-Bodmann, R., 2018. Psychological factors associated with phantom limb pain: A review of recent findings. Pain Research and Management, 2018(1), pp. 5080123. [DOI:10.1155/2018/5080123] [PMID]
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators., 2017. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England), 390(10100), pp. 1211–59. [PMID]
Geiling, J., Rosen, J. M. & Edwards, R. D., 2012. Medical costs of war in 2035: Long-term care challenges for veterans of Iraq and Afghanistan. Military Medicine, 177(11), pp. 1235-44. [DOI:10.7205/MILMED-D-12-00031] [PMID]
Gilg, A., 2016. The impact of amputation on Body Image [Honors Theses]. Mississippi: The University of Southern Mississippi. [Link]
Goldberg, D. P. & Hillier, V. F., 1979. A scaled version of the General Health Questionnaire. Psychological Medicine, 9(1), pp. 139-45. [DOI:10.1017/S0033291700021644] [PMID]
Graziottin, A., Cuccarollo, A. & Donini, M., 2022. Diagnosi e cura del dolore sessuale dopo il parto. pp. 100-9. [Link]
Gündüz, E. S., Durmaz, M. & Aydın, B. K., 2024. “ Both My Body and My Spirit are Incomplete”: Care needs and difficulties experienced by patients with amputation. Turkish Journal of Diabetes and Obesity, 8(2), pp. 191-201. [DOI:10.25048/tudod.1469602]
Gunterstockman, B. M., et al., 2023. Relationship between phantom limb pain, function, and psychosocial health in individuals with lower-limb loss. Prosthetics and Orthotics International, 47(2), pp. 181-8. [DOI:10.1097/PXR.0000000000000191] [PMID]
Herasymenko, O., et al., 2018. Effectiveness of physical therapy interventions for young adults after lower limb transtibial amputation. Journal of Physical Education and Sport, 18(2), pp. 1084-91. [Link]
Heszlein-Lossius, H. E., et al., 2019. Does pain, psychological distress and deteriorated family economy follow traumatic amputation among war casualties? A retrospective, cross-sectional study from Gaza. BMJ Open, 9(6), pp. e029892.[DOI:10.1136/bmjopen-2019-029892] [PMID]
Hogan, W. B., et al., 2022. Phantom limb syndrome: Assessment of psychiatric and medical comorbidities associated with Phantom pain in 44,028 below knee amputees. Injury, 53(11), pp. 3697-701. [DOI:10.1016/j.injury.2022.09.018] [PMID]
Humanity. & Inclusion., 2017. Urgent need for rehabilitation services in Yemen. Georgia: Humanity & Inclusion. [Link]
Ie, T. & Bespalenko, A., 2016. Analysis of limb amputations during armed conflict at the East of Ukraine. Norwegian Journal of development of the International Science, (1), pp. 79-80. [Link]
Ikram, M., et al., 2014. Frequency and sociodemographic predictors of clinical depression in combat amputees at a military rehabilitation setup. Rawal Medical Journal, 39(2), pp. 167-70. [Link]
Katz, J., 1993. Phantom limb experience in children and adults: Cognitive and affective contributions. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 25(3), pp. 335-54. [Link]
Khan, M. J., Dogar, S. F. & Masroor, U., 2018. Family relations, quality of life and post-traumatic stress among amputees and prosthetics. Pakistan Armed Forces Medical Journal, 68(1), pp. 125-30. [Link]
Margalit, D., et al., 2013. Phantom fighters: Coping mechanisms of amputee patients with phantom limb pain: A longitudinal study. Open Journal of Orthopedics, 3(07), pp. 300-5. [DOI:10.4236/ojo.2013.37055]
McCarthy, M. L., et al., 2003. Psychological distress associated with severe lower-limb injury. The Journal of Bone and Joint Surgery. American volume, 85(9), pp. 1689–97.[DOI:10.2106/00004623-200309000-00006] [PMID]
McDonald, C. L., et al., 2021. Global prevalence of traumatic non-fatal limb amputation. Prosthetics and Orthotics International, 45(2), pp. 105–14. [DOI:10.1177/0309364620972258] [PMID]
Monitoring and Research Committee., et al., 2022. Landmine Monitor. Geneva: International Campaign to Ban Landmines. [Link]
Murray, C. D. & Forshaw, M. J., 2013. The experience of amputation and prosthesis use for adults: A metasynthesis. Disability and Rehabilitation, 35(14), pp. 1133-42. [DOI:10.3109/09638288.2012.723790] [PMID]
Muzaffar, N., et al., 2012. Psychiatric comorbidity in amputees with average sociodemographic status and the role of theologic and family support in a conflict zone. Australasian Journal of Disaster and Trauma Studies, 2012(1), pp. 31-8. [Link]
Naja, S., et al., 2019. Psychometric properties of the Arabic version of EPDS and BDI-II as a screening tool for antenatal depression: Evidence from Qatar. BMJ Open, 9(9), pp. e030365.[DOI:10.1136/bmjopen-2019-030365] [PMID]
Ngo, L. & Bjork, A., 2018. Disability in the Arab Region. New York: United Nations. [Link]
Nizamli, F. M., 2020. Quality of life among Syrian patients with war-related lower limb amputation at the Military Hospital in Lattakia. International Journal of Nursing Sciences, 7(3), pp. 297-302. [DOI:10.1016/j.ijnss.2020.05.001] [PMID]
Okello, T. R., et al., 2022. Major Limb Loss and Prosthesis Use in the Post Conflict era in Acholi Sub-Region, Northern Uganda International Journal of Science Academic Research, 3(6), pp. 3998-4004. [Link]
Padovani, M. T., et al., 2015. Anxiety, depression and quality of life in individuals with phantom limb pain. Acta Ortopedica Brasileira, 23(2), pp. 107–10. [DOI:10.1590/1413-78522015230200990] [PMID]
Petersen, B., Sparto, P. & Fisher, L., 2023. Clinical measures of balance and gait cannot differentiate somatosensory impairments in people with lower-limb amputation. Gait & Posture, 99, pp. 104-10. [DOI:10.1016/j.gaitpost.2022.10.018] [PMID]
Qahtani, B. A., 2021. KSrelief-supported Artificial Limbs Centers in Yemen Have Provided Services for 25,000+ Patients. Riyadh: King Salman Humanitarian Aid and Relief Center. [Link]
Ramaraj, P., et al., 2023. Epidemiology of traumatically injured Yemeni civilians treated at the Omani National Trauma Centre over a 2-year period: A retrospective cohort study. BMJ Military Health, 171(1), pp. 19–25. [DOI:10.1136/military-2023-002509] [PMID]
Roșca, A. C., et al., 2021. Psychological consequences in patients with amputation of a limb. An interpretative-phenomenological analysis. Frontiers in Psychology, 12, pp. 537493. [DOI:10.3389/fpsyg.2021.537493] [PMID]
Roullet, S., et al., 2009. [Phantom limb pain: from physiopathology to prevention (French)]. Annales Francaises D'anesthesie et de Reanimation, 28(5), pp. 460–72. [DOI:10.1016/j.annfar.2009.03.012] [PMID]
Sahu, A., et al., 2016. Psychological effects of amputation: A review of studies from India. Industrial Psychiatry Journal, 25(1), pp. 4-10. [DOI:10.4103/0972-6748.196041] [PMID]
Senra, H., et al., 2012. Beyond the body image: A qualitative study on how adults experience lower limb amputation. Clinical Rehabilitation, 26(2), pp. 180–91. [DOI:10.1177/0269215511410731] [PMID]
Sky News Arabia., 2018. Saudi Arabia launches “Masam” project to clear landmines in Yemen. Viewe 25 June 2018.
Stancu, B., et al., 2016. Medical, social and christian aspects in patients with major lower limb amputations. Journal for the Study of Religions and Ideologies, 15(43), pp. 82-101. [Link]
Tomilenko, M., 2023. Bridging Additive Manufacturing and Assistive Technology Networks in Ukraine Through Systems Mapping and Education [MA thesis]. New York: New York University Tandon School of Engineering. [Link]
Trevelyan, E. G., Turner, W. A. & Robinson, N., 2016. Perceptions of phantom limb pain in lower limb amputees and its effect on quality of life: A qualitative study. British Journal of Pain, 10(2), pp. 70-7. [DOI:10.1177/2049463715590884] [PMID]
United Nations Office for the Coordination of Humanitarian Affairs (OCHA)., 2021. Yemen humanitarian needs overview. New York: United Nations Office for the Coordination of Humanitarian Affairs. [Link]
Valizadeh, S., et al., 2014. The perception of trauma patients from social support in adjustment to lower-limb amputation: A qualitative study. Indian Journal of Palliative Care, 20(3), pp. 229-38. [DOI:10.4103/0973-1075.138401] [PMID]
Waqar, S., Noor, R. & Khan, M. M. H.,2015. Depression, anxiety & psychological adjustment among amputees. International Journal of Rehabilitation Research, 4(2), pp. 14-18. [Link]
Weiss, G., 2013. Body images: Embodiment as intercorporeality. New York: Routledge. [DOI:10.4324/9780203699003]
Whyte, A. S. & Niven, C. A., 2001. Psychological distress in amputees with phantom limb pain. Journal of Pain and Symptom Management, 22(5), pp. 938–46. [DOI:10.1016/S0885-3924(01)00352-9] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2024/08/25 | Accepted: 2024/12/25 | Published: 2025/05/1
Received: 2024/08/25 | Accepted: 2024/12/25 | Published: 2025/05/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |