Mon, Feb 2, 2026
[Archive]
Volume 5, Issue 1 (Winter 2019)
JCCNC 2019, 5(1): 53-62 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezaei M, Vatankhah M, Mirbagher Ajorpaz N, Gholami M, Zamani B. The Effect of Osteoporosis Prevention Empowerment Program on the Self-Efficacy of Iranian Older Adults. JCCNC 2019; 5 (1) :53-62
URL: http://jccnc.iums.ac.ir/article-1-213-en.html
URL: http://jccnc.iums.ac.ir/article-1-213-en.html
1- Autoimmune Diseases Research Center, School of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran.
2- Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran.
3- Autoimmune Diseases Research Center, School of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran. ,salam_20012003@yahoo.co.uk
4- Autoimmune Diseases Research Center, Department of Internal Medicine, Kashan University of Medical Sciences, Kashan, Iran.
2- Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran.
3- Autoimmune Diseases Research Center, School of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran. ,
4- Autoimmune Diseases Research Center, Department of Internal Medicine, Kashan University of Medical Sciences, Kashan, Iran.
Full-Text [PDF 648 kb]
(1350 Downloads)
| Abstract (HTML) (3878 Views)
● Patients with osteoporosis have multiple physical problems related to their disease and the adverse effects of traditional treatments.
● Self-efficacy education can encourage osteoporosis preventing behaviors.
● Empowerment based on health model is effective in promoting self-efficacy and osteoporosis preventing behaviors.
Plain Language Summary
Osteoporosis is a disease in which bone weakness increases the risk of a broken bone. It is the most common reason for a broken bone among the elderly. In recent years, the focus is on using empowerment interventions combined with self-efficacy technique for its treatment. This clinical trial study investigated the effect of “osteoporosis prevention empowerment program” based on the Health Belief Model (HBM) on the self-efficacy of Iranian older adults. The study results showed that education based on HBM is effective in promoting self-efficacy and osteoporosis preventing behaviors.
4. Discussion
The objective of this randomized controlled clinical trial was to determine whether osteoporosis self-efficacy would improve after an empowerment program based on the health belief model.
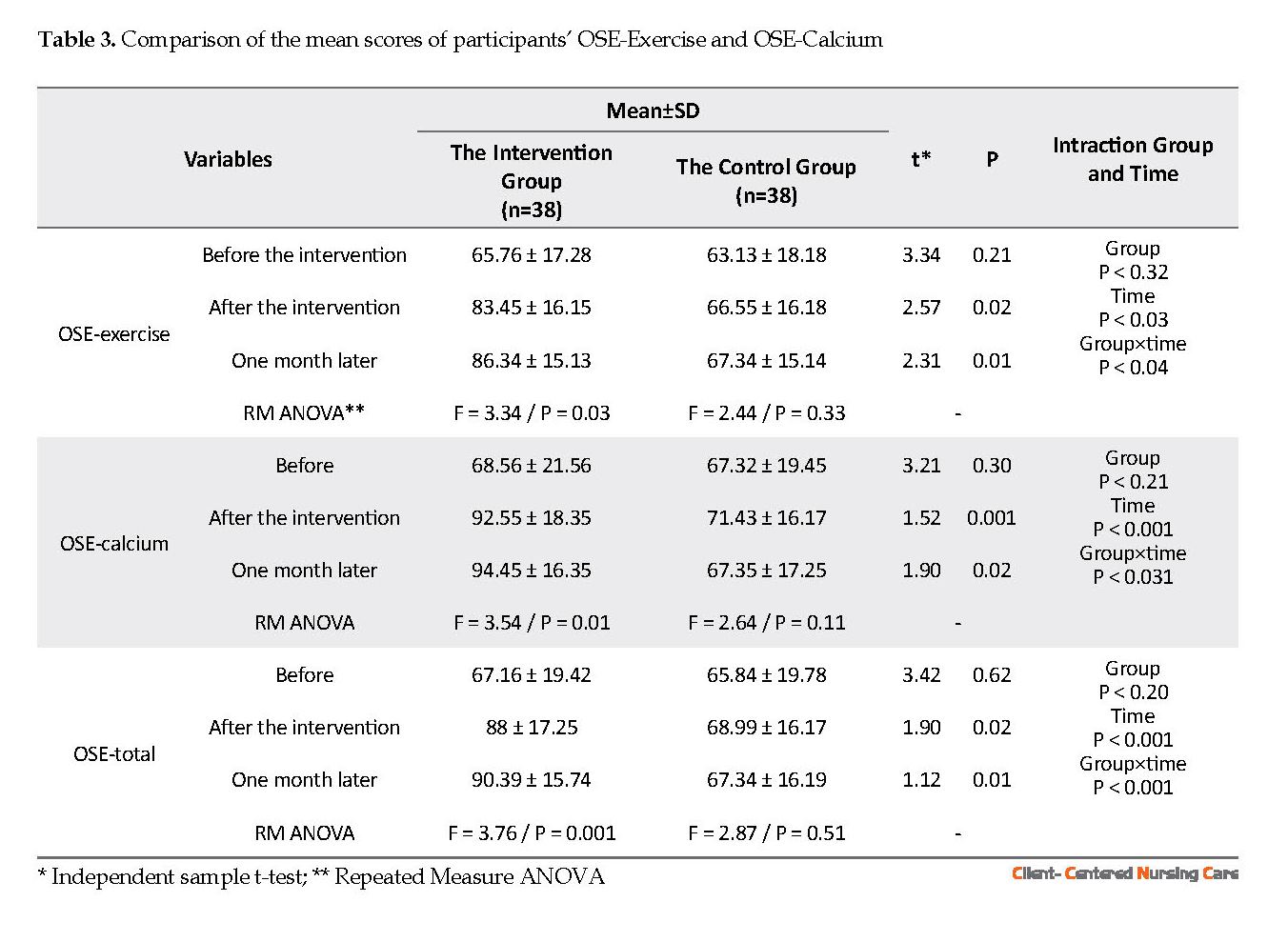
The findings showed that empowerment program based on HBM could be an effective strategy for increasing osteoporosis self-efficacy among older adults. After the empowerment program, the mean score of self-efficacy, both in the subscales of exercise and calcium intake, was significantly higher in the intervention group compared to the control group.
Follow-up assessment also revealed that this increase had been maintained one month later. Improvement was observed over time in the level of osteoporosis self-efficacy among the participants in the intervention group compared to the control group. Other researchers have found that educational programs can improve osteoporosis self-efficacy in elderly populations (Baheiraei et al. 2005; Park et al., 2017). It has been found that osteoporosis prevention education can increase self-efficacy related to calcium intake (Tussing & Chapman-Novakofski, 2005).
However, Sedlak et al. (Sedlak et al. 2005) reported that interventions to enhance osteoporosis prevention did not have any effect on calcium intake in post-menopausal women. They also found that these interventions led to a decrease in weight-bearing exercises in these women. It has been shown that osteoporosis preventive interventions have no effect on calcium intake and physical activity subscales of self-efficacy in older women (Jessup et al. 2003).
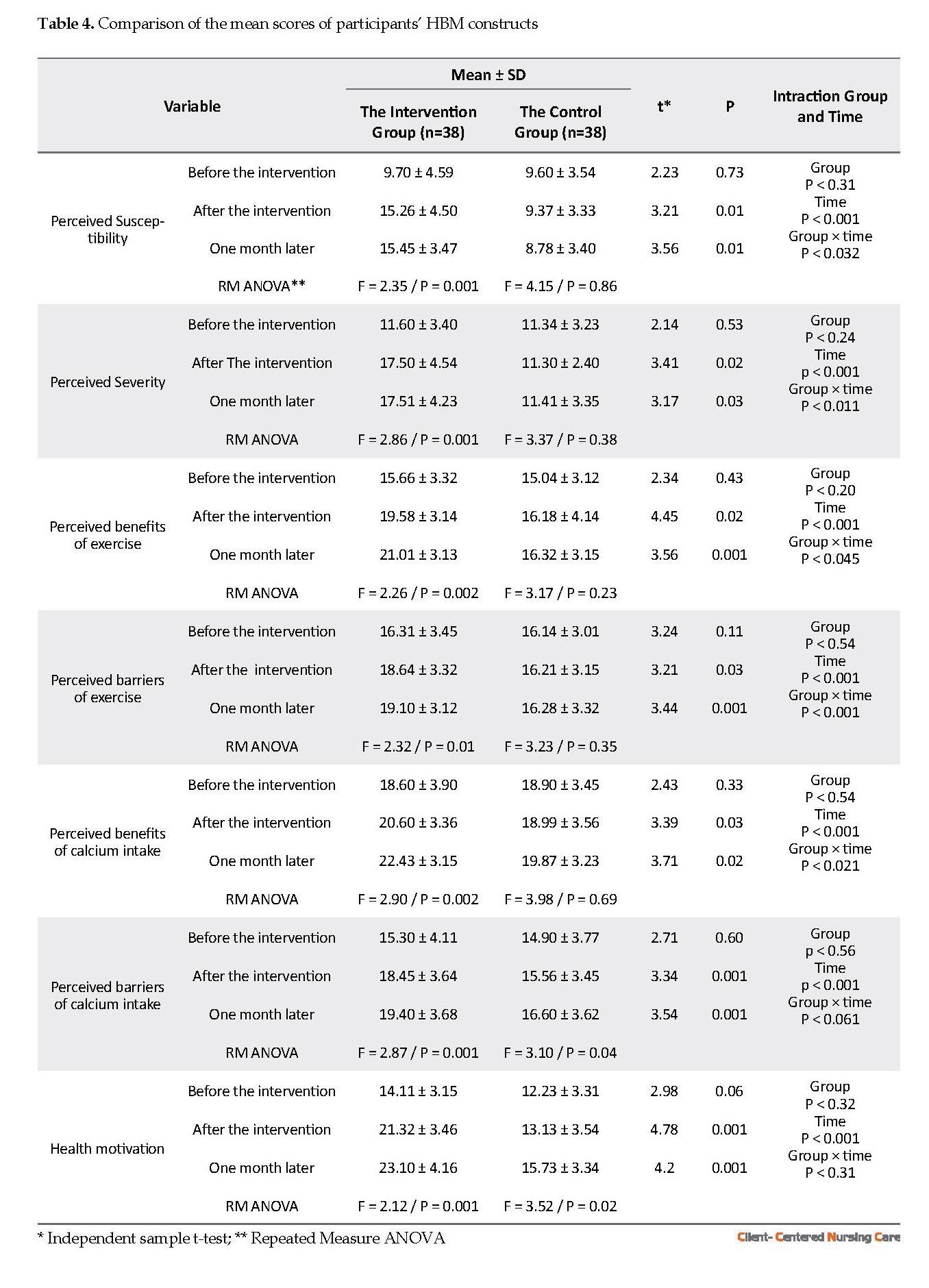
In this study, all HBM constructs (perceived susceptibility, perceived severity, perceived benefits, barriers of exercise, perceived benefits, barriers to calcium intake, and health motivation) were influenced by the empowerment program. Improvement was observed over time in all these constructs among participants in the intervention group compared to the control group. These significant findings of the study can be attributed to the richness of the education program that was presented in multiple sessions with different educational approaches, using assignments related to osteoporosis prevention behaviors, inviting an old volunteer with a history of osteoporosis, and engagement of the family members in the management of the disease.
Sharing and providing information on osteoporosis in the HBM-based education program and discussion about related cases could be useful in raising sensitivity perception, promoting the perceptions of benefits (Hsieh et al. 2014; Kalkim & Dağhan 2017) and barriers (Hsieh et al. 2014; Khani Jeihooni et al., 2017) and health motivation (Kalkim & Dağhan 2017)that result in osteoporosis preventive behaviors (Kalkim & Dağhan, 2017). In this area, different results have been reported in previous studies, and the osteoporosis prevention program had different effects on the various constructs of HBM. For example, it has been found that osteoporosis preventive interventions could increase perceived susceptibility to osteoporosis and perceived benefits related to increased calcium intake (Tussing & Chapman-Novakofski 2005).
A significant improvement was reported in osteoporosis perceived susceptibility, perceived benefits of exercise, perceived barriers to calcium, and perceived barriers to exercise in older adults (Aree-Ue et al. 2006). It has also been revealed that tailored interventions to enhance osteoporosis prevention can improve perceived barriers to calcium intake and perceived barriers to exercise in postmenopausal women (Sedlak et al. 2005). In another study, however, the osteoporosis education program was only associated with improvement in calcium intake and did not affect other health belief subscales (Babatunde 2011).
The findings of the current study suggest the value of empowerment programs with a theoretical underpinning to improve osteoporosis self-efficacy and health beliefs in older adults. It can increase the ability to control hardships and side-effects of the disease in this population.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in this study were in accordance with the ethical standards of the Institutional and or National Research Committee and with the 1964 Helsinki Declaration and its amendments or comparable ethical standards. This trial was registered to the Iranian Randomized Controlled Trial with the registry number: IRCT201707248348N36. The Ethics Committee of Vice Chancellor for Research, KUMS approved the study (Ethics code: IR.KAUMS.NUHEPM.REC.1396.14). All participants were informed on the study procedure and its objectives and signed informed consent. They were fully aware of their voluntary participation and the right to withdraw at any time. Also, they were assured that their anonymity would be protected and their personal information would be kept confidential.
Funding
This research was financially supported by the Kashan University of Medical Science (Grant No.: 9697).
Authors' contributions
Conceptualization, Investigation, Writing-Original Draft, Supervision: Neda Mirbagher Ajorpaz; Collecting data: MehdiVtankhah and Mostafa Gholami; Writing review and Editing: Mahboubeh Rezaei, Batool Zamani; and Funding Acquisition: All authors.
Conflict of interest
All authors of this article declare no conflicts of interest.
Acknowledgments
The authors acknowledge Kashan University of Medical Sciences for its financial support.
References
Anderson, E. S., et al., 2010. Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: Social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. Journal of Health Psychology, 15(1), pp. 21-32. [DOI:10.1177/1359105309342297] [PMID]
Aree-Ue, S., et al., 2006. Osteoporosis preventive behavior in Thai older adults: Feasibility and acceptability. Journal of Gerontological Nursing, 32(7), pp. 23-30. [PMID]
Babatunde, O. T., et al., 2011. Theory-driven intervention improves calcium intake, osteoporosis knowledge, and self-efficacy in community-dwelling older black adults. Journal of Nutrition Education and Behavior, 43(6), pp. 434-40. [DOI:10.1016/j.jneb.2010.07.004] [PMID]
Baheiraei, A., et al., 2005. Psychometric properties of the Persian version of the osteoporosis knowledge and health belief questionnaires. Maturitas, 50(2), pp. 134-9. [DOI:10.1016/j.maturitas.2004.05.001] [PMID]
Bastani, F., et al., 2016. Factors associated with fear of falling and functional independence in older adults in Iranian Nursing Homes. Journal of Client-Centered Nursing Care, 2(3), pp. 135-44. [DOI:10.32598/jccnc.2.3.135]
Dan, X., et al., 2018. Relationships among structural empowerment, innovative behaviour, self‐efficacy, and career success in nursing field in mainland China. International Journal of Nursing Practice, 24(5), p. e12674. [DOI:10.1111/ijn.12674] [PMID]
Doba, N., et al., 2016. Assessment of self-efficacy and its relationship with frailty in the elderly. Internal Medicine, 55(19), pp. 2785-92. [DOI:10.2169/internalmedicine.55.6924] [PMID] [PMCID]
Doosti-Irani, A., Ghafari, M. & Cheraghi, Z., 2018. The high prevalence of osteoporosis as a preventable disease: The need for greater attention to prevention programs in Iran. Iranian Journal of Public Health, 47(8), pp. 1220-1. [PMID] [PMCID]
Ebrahimi, H., et al., 2016. Evaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial study. Primary Care Diabetes, 10(2), pp. 129-35. [DOI:10.1016/j.pcd.2015.09.003] [PMID]
French, D. P., et al., 2014. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Annals of Behavioral Medicine, 48(2), pp. 225-34. [DOI:10.1007/s12160-014-9593-z] [PMID]
Gallaghe, N. A., et al., 2015. Self-efficacy, neighborhood walking, and fall history in older adults. Journal of Aging and Physical Activity, 23(1), pp. 64-71. [DOI:10.1123/JAPA.2012-0287] [PMID]
Heidari, S., et al., 2017. Religious practices and self-care in Iranian patients with type 2 diabetes. Journal of Religion and Health, 56(2), pp. 683-96. [DOI:10.1007/s10943-016-0320-x] [PMID]
Horan, M. L., et al., 1998. Development and evaluation of the osteoporosis self‐efficacy scale. Research in Nursing & Health, 21(5), pp. 395-403. [DOI:10.1002/(SICI)1098-240X(199810)21:53.0.CO;2-I]
Hosseinian, M., Ajorpaz, N. M. & Manesh, S. E., 2015. Mothers’ satisfaction with two systems of providing care to their hospitalized children. Iranian Red Crescent Medical Journal, 17(2), p. e23333. [DOI:10.5812/ircmj.23333] [PMID] [PMCID]
Hsieh, E., et al., 2014. Osteoporosis knowledge, self-efficacy, and health beliefs among Chinese individuals with HIV. Archives of Osteoporosis, 9(1), p. 201. [DOI:10.1007/s11657-014-0201-4] [PMID] [PMCID]
Janiszewska, M., et al., 2017. General self-efficacy level and health behaviours in women over the age of 45 years who have undergone osteoporosis treatment. Menopause Review, 16(3), p. 86. [DOI:10.5114/pm.2017.70584] [PMID] [PMCID]
Jessup, J. V., et al., 2003. Effects of exercise on bone density, balance, and self-efficacy in older women. Biological Research for Nursing, 4(3), pp. 171-80. [DOI:10.1177/1099800402239628] [PMID]
Kalkım, A. & Dağhan, Ş., 2017. Theory-based osteoporosis prevention education and counseling program for women: a randomized controlled trial. Asian Nursing Research, 11(2), pp. 119-27. [DOI:10.1016/j.anr.2017.05.010] [PMID]
Kanis, J. A., et al., 2013. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporosis International, 24(1), pp. 23-57. [DOI:10.1007/s00198-012-2074-y] [PMID] [PMCID]
Keshtkar, A., et al., 2015. Clinical performance of seven prescreening tools for osteoporosis in Iranian postmenopausal women. Rheumatology International, 35(12), pp.1995-2004. [DOI:10.1007/s00296-015-3286-1] [PMID]
Khani Jeihooni, A., et al., 2017. RETRACTED: The effect of an educational program based on health belief model and social cognitive theory in prevention of osteoporosis in women. Journal of Health Psychology, 22(5), pp. NP1-11. [DOI:10.1177/1359105315603696] [PMID]
Kim, K. K., et al., 1991. Development and evaluation of the osteoporosis health belief scale. Research in Nursing & Health, 14(2), pp. 155-63. [DOI:10.1002/nur.4770140210]
Lindberg, M. & Fernandes, M. A. M., 2010. Self‐efficacy in relation to limited fluid intake amongst Portuguese haemodialysis patients. Journal of Renal Care, 36(3), pp.133-8. [DOI:10.1111/j.1755-6686.2010.00182.x] [PMID]
Moein, M., et al., 2017. Effect of an empowerment program on self-efficacy of patients with type 2 diabetes. Iranian Red Crescent Medical Journal, 19(1), p. 29252. [DOI:10.5812/ircmj.29252]
Omidvar, S., Jafari Jozani, M. & Nematollahi, N., 2018. Judgment post‐stratification in finite mixture modeling: An example in estimating the prevalence of osteoporosis. Statistics in medicine, 37(30), pp. 4823-36. [DOI:10.1002/sim.7984] [PMID]
Park, K. S., et al., 2017. Education and exercise program improves osteoporosis knowledge and changes calcium and vitamin D dietary intake in community dwelling elderly. BMC Public Health, 17(1), p. 966. [DOI:10.1186/s12889-017-4966-4] [PMID] [PMCID]
Rodrigues, A. M., et al., 2018. Portuguese recommendations for the prevention, diagnosis and management of primary osteoporosis-2018 update. Acta Reumatologica Portuguesa, 43(1), pp. 123-44.
Royani, Z., et al., 2013. The effect of empowerment program on empowerment level and self-care self-efficacy of patients on hemodialysis treatment. Iranian Journal of Nursing and Midwifery Research, 18(1), pp. 84-7. [PMID] [PMCID]
Sedlak, C. A., et al., 2005. Tailored interventions to enhance osteoporosis prevention in women. Orthopaedic Nursing, 24(4), pp. 270-6. [DOI:10.1097/00006416-200507000-00007]
Shin, D. S., Kim, C. J. & Choi, Y. J., 2016. Effects of an empowerment program for self‐management among rural older adults with hypertension in S outh K orea. Australian Journal of Rural Health, 24(3), pp. 213-9. [DOI:10.1111/ajr.12253] [PMID]
Tussing, L. & Chapman-Novakofski, K., 2005. Osteoporosis prevention education: Behavior theories and calcium intake. Journal of the American Dietetic Association, 105(1), pp. 92-7. [DOI:10.1016/j.jada.2004.10.025] [PMID]
Zhang, M., 2017. Effect of HBM rehabilitation exercises on depression, anxiety and health belief in elderly patients with osteoporotic fracture. Psychiatria Danubina, 29(4), pp. 466-72. [DOI:10.24869/psyd.2017.466] [PMID]
● Patients with osteoporosis have multiple physical problems related to their disease and the adverse effects of traditional treatments.
● Self-efficacy education can encourage osteoporosis preventing behaviors.
● Empowerment based on health model is effective in promoting self-efficacy and osteoporosis preventing behaviors.
Plain Language Summary
Osteoporosis is a disease in which bone weakness increases the risk of a broken bone. It is the most common reason for a broken bone among the elderly. In recent years, the focus is on using empowerment interventions combined with self-efficacy technique for its treatment. This clinical trial study investigated the effect of “osteoporosis prevention empowerment program” based on the Health Belief Model (HBM) on the self-efficacy of Iranian older adults. The study results showed that education based on HBM is effective in promoting self-efficacy and osteoporosis preventing behaviors.
Full-Text: (1551 Views)
1. Background
Osteoporosis is a serious health problem and is called the silent disease of the century (Janiszewska et al., 2017). It is the fourth basic enemy of humans after heart failure, stroke, and cancer (Khani Jeihooni et al. 2017) and the most prevalent cause of fractures in the world (Keshtkar et al. 2015). Low bone mass and loss of bone microarchitecture quality are characteristics of osteoporosis, which leads to higher bone fracture risk. Many people above 65 years are at risk of falling and this rate increases with age (Bastani et al. 2016).
Bone density reduces very slowly and majority of the symptoms do not appear until the first fracture occurs. This disease is one of the basic causes of disability and mortality in older adults (Rodrigues et al. 2018). Like many other developing countries, life expectancy has been increased in Iran. Since the chance of osteoporosis increases with age, the disease should be considered as a health-related priority (Doosti-Irani et al., 2018). In Iran, the national program for prevention, diagnosis, and treatment of osteoporosis reported that 70% of women and 50% of men over 50 years suffer from osteoporosis and osteopenia (Omidvar, Jafari Jozani & Nematollahi, 2018).
Health promotion of older adults depends on their contribution to the care process and their self-efficacy to acquire a favorite life (Khani Jeihooni et al. 2017). Self-efficacy is an individual’s trust in being able to do self-care activities to achieve desirable results (Royani et al. 2013). It is an essential prerequisite for behavior which can affect the life and health behaviors (Anderson et al. 2010; Heidari et al. 2017; Moein et al. 2017; Omidvar et al. 2018). Improved self-efficacy in aging populations has been associated with increased energy, better sleep, decreased pain and discomfort, increased satisfaction with life and better overall health (Gallaghe et al. 2015; Hosseinian, Ajorpaz & Manesh, 2015). However, the level of self-efficacy in this population is undesirable (French et al. 2014).
An essential aspect of osteoporosis prevention is lifestyle modification and daily habits (Lindberg & Fernandes 2010). Teaching preventive behaviors such as physical activity and a healthy diet can help disease prevention, health promotion, and preservation (Lindberg & Fernandes 2010). Empowerment is a process which facilitates behavioral changes and improves independence in adopting behavioral changes (Dan et al. 2018). There is a significant relationship between empowerment and self-efficacy in older adults (Doba et al. 2016).
Implementation of empowerment programs increases confidence in self-care activities (Ebrahimi et al. 2016; Shin, Kim & Choi 2016), improves health care management and self-efficacy, and promotes the general health of older adults (Anderson et al. 2010). However, some studies have argued that empowerment programs are ineffective and inefficient. For instance, Zhang (2017) reported that despite the effect of empowerment program on the knowledge of older adults, it did not have a permanent effect on health belief scores in this population (Zhang, 2017).
Researchers have used some models to change the participants’ behavior. One of the effective models in health education and promotion is the Health Belief Model (HBM). The constructs of the HBM include perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and health motivation. Unhealthy behaviors may not turn into healthy behaviors unless, based on HBM, people understand that their disease is serious (Khani Jeihooni et al. 2017). Perceived susceptibility was used to evaluate older adult’s perception about the extent to which they are at risk of osteoporosis. Also, their perceived severity of osteoporosis complications was assessed.
Other constructs were the perceived benefits and barriers of calcium intake and physical activity. It was included in the individual’s analysis about the benefits of following osteoporosis preventive behaviors such as diet and walking and potential barriers to preventive practices in osteoporosis. The present study aimed to evaluate the effect of an empowerment program based on HBM on self-efficacy in the prevention of osteoporosis among Iranian older adults. The authors hypothesized that positive changes would take place in self-efficacy and health beliefs in the intervention group as compared to the control group.
2. Materials and Methods
Study design
This research was a randomized controlled clinical trial. Older adults referred to health centers affiliated to Kashan University of Medical Sciences (KUMS) between April and June 2018 were invited to participate in this study.
Study sample
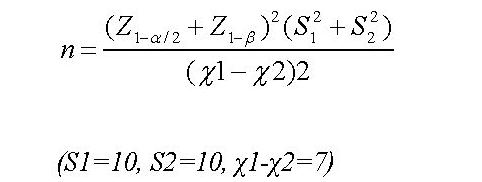
To estimate the sample size, the standard formula suggested for parallel clinical trials was used. According to a similar study (Khani Jeihooni, Hidarnia et al., 2017), considering the type 1 error (α) of 0.05, type 2 error (β) of 0.20 (statistical power = 80%), and a possible attrition rate of 10%, the required sample size was calculated as 40 participants in each group.
Osteoporosis is a serious health problem and is called the silent disease of the century (Janiszewska et al., 2017). It is the fourth basic enemy of humans after heart failure, stroke, and cancer (Khani Jeihooni et al. 2017) and the most prevalent cause of fractures in the world (Keshtkar et al. 2015). Low bone mass and loss of bone microarchitecture quality are characteristics of osteoporosis, which leads to higher bone fracture risk. Many people above 65 years are at risk of falling and this rate increases with age (Bastani et al. 2016).
Bone density reduces very slowly and majority of the symptoms do not appear until the first fracture occurs. This disease is one of the basic causes of disability and mortality in older adults (Rodrigues et al. 2018). Like many other developing countries, life expectancy has been increased in Iran. Since the chance of osteoporosis increases with age, the disease should be considered as a health-related priority (Doosti-Irani et al., 2018). In Iran, the national program for prevention, diagnosis, and treatment of osteoporosis reported that 70% of women and 50% of men over 50 years suffer from osteoporosis and osteopenia (Omidvar, Jafari Jozani & Nematollahi, 2018).
Health promotion of older adults depends on their contribution to the care process and their self-efficacy to acquire a favorite life (Khani Jeihooni et al. 2017). Self-efficacy is an individual’s trust in being able to do self-care activities to achieve desirable results (Royani et al. 2013). It is an essential prerequisite for behavior which can affect the life and health behaviors (Anderson et al. 2010; Heidari et al. 2017; Moein et al. 2017; Omidvar et al. 2018). Improved self-efficacy in aging populations has been associated with increased energy, better sleep, decreased pain and discomfort, increased satisfaction with life and better overall health (Gallaghe et al. 2015; Hosseinian, Ajorpaz & Manesh, 2015). However, the level of self-efficacy in this population is undesirable (French et al. 2014).
An essential aspect of osteoporosis prevention is lifestyle modification and daily habits (Lindberg & Fernandes 2010). Teaching preventive behaviors such as physical activity and a healthy diet can help disease prevention, health promotion, and preservation (Lindberg & Fernandes 2010). Empowerment is a process which facilitates behavioral changes and improves independence in adopting behavioral changes (Dan et al. 2018). There is a significant relationship between empowerment and self-efficacy in older adults (Doba et al. 2016).
Implementation of empowerment programs increases confidence in self-care activities (Ebrahimi et al. 2016; Shin, Kim & Choi 2016), improves health care management and self-efficacy, and promotes the general health of older adults (Anderson et al. 2010). However, some studies have argued that empowerment programs are ineffective and inefficient. For instance, Zhang (2017) reported that despite the effect of empowerment program on the knowledge of older adults, it did not have a permanent effect on health belief scores in this population (Zhang, 2017).
Researchers have used some models to change the participants’ behavior. One of the effective models in health education and promotion is the Health Belief Model (HBM). The constructs of the HBM include perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and health motivation. Unhealthy behaviors may not turn into healthy behaviors unless, based on HBM, people understand that their disease is serious (Khani Jeihooni et al. 2017). Perceived susceptibility was used to evaluate older adult’s perception about the extent to which they are at risk of osteoporosis. Also, their perceived severity of osteoporosis complications was assessed.
Other constructs were the perceived benefits and barriers of calcium intake and physical activity. It was included in the individual’s analysis about the benefits of following osteoporosis preventive behaviors such as diet and walking and potential barriers to preventive practices in osteoporosis. The present study aimed to evaluate the effect of an empowerment program based on HBM on self-efficacy in the prevention of osteoporosis among Iranian older adults. The authors hypothesized that positive changes would take place in self-efficacy and health beliefs in the intervention group as compared to the control group.
2. Materials and Methods
Study design
This research was a randomized controlled clinical trial. Older adults referred to health centers affiliated to Kashan University of Medical Sciences (KUMS) between April and June 2018 were invited to participate in this study.
Study sample
To estimate the sample size, the standard formula suggested for parallel clinical trials was used. According to a similar study (Khani Jeihooni, Hidarnia et al., 2017), considering the type 1 error (α) of 0.05, type 2 error (β) of 0.20 (statistical power = 80%), and a possible attrition rate of 10%, the required sample size was calculated as 40 participants in each group.
Older adults who met the inclusion criteria and were willing to participate in the study were recruited. The inclusion criteria were aged over 60 years; abled to answer the questions and attend meetings; had no restriction on calcium and vitamin D consumption, dairy products, and daily physical activity. The participants who were absent in more than two training sessions; had been admitted to a hospital; or suffered from disabilities, disease, or any other problems that prevented their participation in the study were excluded.
Study randomization
The participants were selected by convenience sampling method and were assessed for their eligibility (n=150). Then they were randomly assigned to either control (n=40) or intervention (n=40) groups using computer-generated random numbers.
Before the random allocation of the participants into study groups, 70 participants were excluded because 51 participants didn’t meet the inclusion criteria, and 19 participants declined to participate in the study. Two participants in the intervention group participated irregularly in the sessions. Also, two participants in the control group filled out the questionnaires incompletely and were excluded from the study. Finally, the data from 38 participants in each group were analyzed.
Study intervention
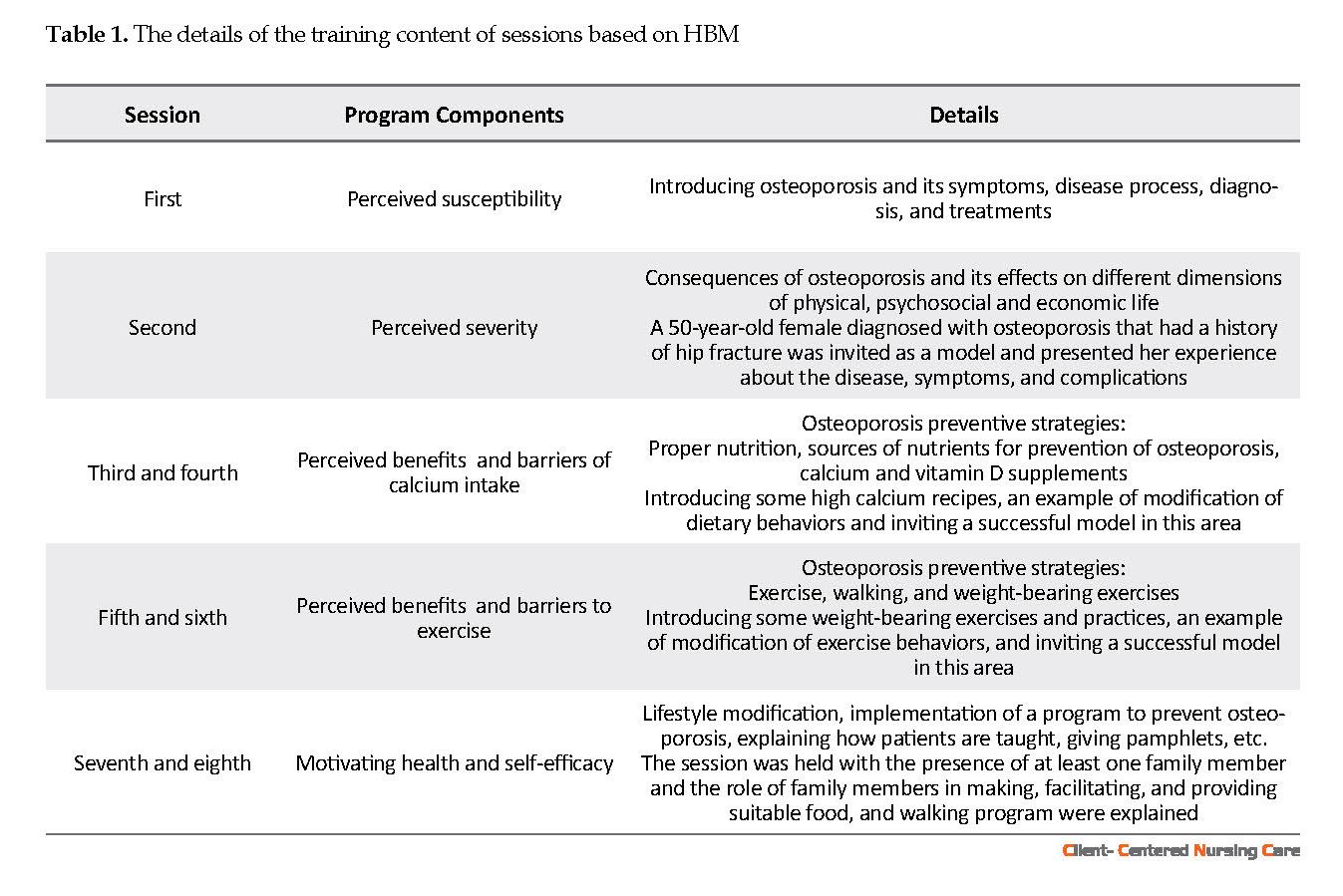
The empowerment program was prepared based on the HBM and followed the intervention protocol introduced in previous studies (Tussing & Chapman-Novakofski, 2005; Babatunde et al., 2011; Park et al. 2017). The program consisted of an 8-session empowerment course and was according to the International Osteoporosis Foundation (IOF) recommendations for protection against osteoporosis (Kanis et al. 2013).
Study randomization
The participants were selected by convenience sampling method and were assessed for their eligibility (n=150). Then they were randomly assigned to either control (n=40) or intervention (n=40) groups using computer-generated random numbers.
Before the random allocation of the participants into study groups, 70 participants were excluded because 51 participants didn’t meet the inclusion criteria, and 19 participants declined to participate in the study. Two participants in the intervention group participated irregularly in the sessions. Also, two participants in the control group filled out the questionnaires incompletely and were excluded from the study. Finally, the data from 38 participants in each group were analyzed.
Study intervention
The empowerment program was prepared based on the HBM and followed the intervention protocol introduced in previous studies (Tussing & Chapman-Novakofski, 2005; Babatunde et al., 2011; Park et al. 2017). The program consisted of an 8-session empowerment course and was according to the International Osteoporosis Foundation (IOF) recommendations for protection against osteoporosis (Kanis et al. 2013).
The program was conducted over a 4-week group education, and a 4-week individual follow up. The content of sessions is presented in Table 1. The participants attended each session for 50-60 minutes twice a week and received phone calls from the researchers once a week for 4 consecutive weeks. The phone calls were made to encourage the participants to initiate and continue their new behaviors, ensure proper implementation of the empowerment program, and answer any questions. The researchers held all the sessions.
To training better, a combination of different educational approaches such as lectures, group discussions, question and answer, as well as educational poster and pamphlet, and PowerPoint presentation was used. Each session was started by checking the assignments related to osteoporosis prevention behaviors and receiving feedbacks.
To increase the elderly’s attention and their perceived severity, an older volunteer with osteoporosis who had experienced a fracture was invited to participate in one group discussion. To sensitize the families of the subjects, a booklet on the disease was also provided. The subjects in the control group received routine care and education. In addition, at the end of the study, the control group received an educational booklet designed according to the IOF recommendations.
Study instruments
In this study, three questionnaires were used: sociodemographic and clinical data questionnaire, Osteoporosis Health Belief Scale (OHBS), and Osteoporosis Self-Efficacy Scale (OSES).
Sociodemographic and clinical data questionnaire
This questionnaire included questions about age, gender, education level, marital status, tobacco use, body mass index (BMI), height, and weight.
Osteoporosis Health Belief Scale (OHBS)
This questionnaire includes 42 items according to the constructs of HBM and has been specially developed to measure health beliefs related to osteoporosis in older adults (Kim et al. 1991).
The OHBS is divided into seven subscales: perceived susceptibility of osteoporosis (6 items), perceived severity of osteoporosis (6 items), perceived benefits of exercise and calcium taking (12 items), perceived barriers to exercise and calcium taking (12 items), and motivation to perform preventive behaviors (6 items). The OHBS has 5-point Likert-type scale ranging from 1 to 5, where 1 is “strongly disagree”, and 5 is “strongly agree”. The potential range for each subscale is 6 to 30, and the total score range is 42 to 210.
In the original study by Kim et al. (1991), the internal consistency coefficients ranged from 0.61 to 0.80. The psychometric properties of the Iranian version of the OHBS have been confirmed, and the Cronbach α values for the OHBS subscales ranged between 0.70 (barriers to calcium intake) and 0.87 (benefit of exercise) (Baheiraei et al. 2005). In the present study, the content validity of the OHBS was confirmed by 10 Nursing Faculty members. Reliability of the OHBS was demonstrated by the Cronbach α value of 0.81 for the total scale and 0.77 to 0.91 for the subscales.
To training better, a combination of different educational approaches such as lectures, group discussions, question and answer, as well as educational poster and pamphlet, and PowerPoint presentation was used. Each session was started by checking the assignments related to osteoporosis prevention behaviors and receiving feedbacks.
To increase the elderly’s attention and their perceived severity, an older volunteer with osteoporosis who had experienced a fracture was invited to participate in one group discussion. To sensitize the families of the subjects, a booklet on the disease was also provided. The subjects in the control group received routine care and education. In addition, at the end of the study, the control group received an educational booklet designed according to the IOF recommendations.
Study instruments
In this study, three questionnaires were used: sociodemographic and clinical data questionnaire, Osteoporosis Health Belief Scale (OHBS), and Osteoporosis Self-Efficacy Scale (OSES).
Sociodemographic and clinical data questionnaire
This questionnaire included questions about age, gender, education level, marital status, tobacco use, body mass index (BMI), height, and weight.
Osteoporosis Health Belief Scale (OHBS)
This questionnaire includes 42 items according to the constructs of HBM and has been specially developed to measure health beliefs related to osteoporosis in older adults (Kim et al. 1991).
The OHBS is divided into seven subscales: perceived susceptibility of osteoporosis (6 items), perceived severity of osteoporosis (6 items), perceived benefits of exercise and calcium taking (12 items), perceived barriers to exercise and calcium taking (12 items), and motivation to perform preventive behaviors (6 items). The OHBS has 5-point Likert-type scale ranging from 1 to 5, where 1 is “strongly disagree”, and 5 is “strongly agree”. The potential range for each subscale is 6 to 30, and the total score range is 42 to 210.
In the original study by Kim et al. (1991), the internal consistency coefficients ranged from 0.61 to 0.80. The psychometric properties of the Iranian version of the OHBS have been confirmed, and the Cronbach α values for the OHBS subscales ranged between 0.70 (barriers to calcium intake) and 0.87 (benefit of exercise) (Baheiraei et al. 2005). In the present study, the content validity of the OHBS was confirmed by 10 Nursing Faculty members. Reliability of the OHBS was demonstrated by the Cronbach α value of 0.81 for the total scale and 0.77 to 0.91 for the subscales.
Osteoporosis Self-Efficacy Scale (OSES)
It is a 21-item rating scale and reflects self-efficacy perception about calcium intake and weight-bearing exercise in osteoporosis prevention. The OSES has two subscales: the OSE-Exercise scale and OSE-Calcium scale. The items are rated by the study subjects based on their confidence in practicing healthy behaviors to prevent osteoporosis. They respond on a 100-point Likert-type scale from 0 to 100 (0=not confident at all, 100=very confident). The highest possible score would be100. A high score on the scale shows that the self- efficacy perception is at a high level. The internal consistency values of OSE-Exercise and OSE-Calcium have been estimated as 0.94 and 0.93, respectively (Horan et al. 1998). In this study, the content validity of the Persian version of OSES was confirmed by 10 Nursing Faculty members. Reliability of the OSES was demonstrated by the Cronbach α value of 0.79.
Data collection
The study data were collected before the empowerment program as the pre-test, immediately after the intervention as the post-test, and one month after the end of the study as follow up test in the intervention and control groups. Follow-up test was done one month after the end of the intervention to be ensured of the impact of the provided training in the long run. The instruments were self-administered, and the illiterate and disabled subjects were being interviewed.
Data analysis
Statistical analyses were done in SPSS (version 13) (SPSS Inc., Chicago, IL, USA). Kolmogorov-Smirnov test (K-S test) was performed to evaluate the normal distribution of the variables. The data analysis was done by descriptive statistics like mean and standard deviation for quantitative variables and frequencies and percentages for categorical variables. The Independent samples t-test, Chi-square or Fisher’s exact-tests were utilized to assess statistically significant differences between the intervention and control groups. The Independent samples t-test was also applied to compare the mean scores of the self-efficacy and constructs of HBM between the two groups at the beginning, immediately after the intervention and one month after the end of the study. Repeated Measures Analysis of Variance (RM ANOVA) was performed to compare the mean scores of self-efficacy and constructs of HBM within two groups before, immediately after the intervention, and one month after the end of the study. The significance level of less than 0.05 was considered in all tests.
3. Results
Study participants
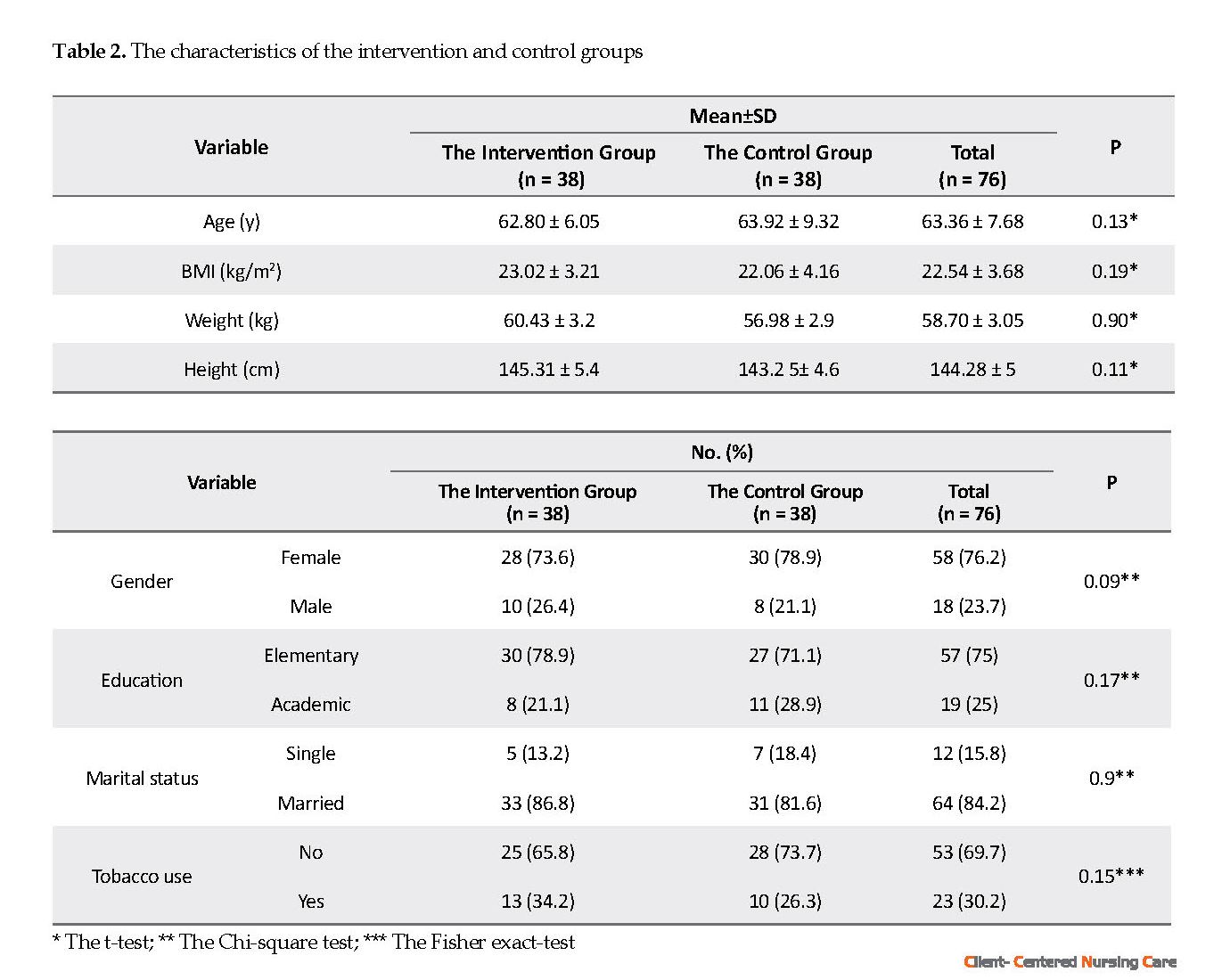
Seventy-six subjects (38 participants in each group) participated in all 8 sessions of empowerment course and completed baseline and follow-up assessments. Significant differences were not found between the intervention and control groups in terms of sociodemographic and clinical characteristics at baseline (P>0.05). The range of the samples’ age was between 60 to 68 years. The majority (76.2%) of the subjects were female, 84.2% were married, and 75% had elementary school education. The Mean±SD BMI of the participants were 22.54±3.68 kg/m2. More than half of the participants (69.7%) did not use tobacco (Table 2).
It is a 21-item rating scale and reflects self-efficacy perception about calcium intake and weight-bearing exercise in osteoporosis prevention. The OSES has two subscales: the OSE-Exercise scale and OSE-Calcium scale. The items are rated by the study subjects based on their confidence in practicing healthy behaviors to prevent osteoporosis. They respond on a 100-point Likert-type scale from 0 to 100 (0=not confident at all, 100=very confident). The highest possible score would be100. A high score on the scale shows that the self- efficacy perception is at a high level. The internal consistency values of OSE-Exercise and OSE-Calcium have been estimated as 0.94 and 0.93, respectively (Horan et al. 1998). In this study, the content validity of the Persian version of OSES was confirmed by 10 Nursing Faculty members. Reliability of the OSES was demonstrated by the Cronbach α value of 0.79.
Data collection
The study data were collected before the empowerment program as the pre-test, immediately after the intervention as the post-test, and one month after the end of the study as follow up test in the intervention and control groups. Follow-up test was done one month after the end of the intervention to be ensured of the impact of the provided training in the long run. The instruments were self-administered, and the illiterate and disabled subjects were being interviewed.
Data analysis
Statistical analyses were done in SPSS (version 13) (SPSS Inc., Chicago, IL, USA). Kolmogorov-Smirnov test (K-S test) was performed to evaluate the normal distribution of the variables. The data analysis was done by descriptive statistics like mean and standard deviation for quantitative variables and frequencies and percentages for categorical variables. The Independent samples t-test, Chi-square or Fisher’s exact-tests were utilized to assess statistically significant differences between the intervention and control groups. The Independent samples t-test was also applied to compare the mean scores of the self-efficacy and constructs of HBM between the two groups at the beginning, immediately after the intervention and one month after the end of the study. Repeated Measures Analysis of Variance (RM ANOVA) was performed to compare the mean scores of self-efficacy and constructs of HBM within two groups before, immediately after the intervention, and one month after the end of the study. The significance level of less than 0.05 was considered in all tests.
3. Results
Study participants
Seventy-six subjects (38 participants in each group) participated in all 8 sessions of empowerment course and completed baseline and follow-up assessments. Significant differences were not found between the intervention and control groups in terms of sociodemographic and clinical characteristics at baseline (P>0.05). The range of the samples’ age was between 60 to 68 years. The majority (76.2%) of the subjects were female, 84.2% were married, and 75% had elementary school education. The Mean±SD BMI of the participants were 22.54±3.68 kg/m2. More than half of the participants (69.7%) did not use tobacco (Table 2).
Effectiveness of the empowerment program on osteoporosis self-efficacy
There were no significant differences between the intervention and control groups in OSES and its two subscales scores (OSE-Exercise and OSE-Calcium) at baseline (P≥0.05). However, the mean scores of OSES and its subscales were significantly different between the groups immediately after the end of the sessions and one month later (P<0.05).
The repeated measures ANOVA test showed a significant difference between the mean scores of OSES and its two subscales before, immediately after the last session, and one month after the intervention in the intervention group (P<0.05). There was no significant difference between the mean scores of OSES and its subscales in the control group before, immediately after the last session, and one month later (P≥0.05) (Table 3).
There were no significant differences between the intervention and control groups in OSES and its two subscales scores (OSE-Exercise and OSE-Calcium) at baseline (P≥0.05). However, the mean scores of OSES and its subscales were significantly different between the groups immediately after the end of the sessions and one month later (P<0.05).
The repeated measures ANOVA test showed a significant difference between the mean scores of OSES and its two subscales before, immediately after the last session, and one month after the intervention in the intervention group (P<0.05). There was no significant difference between the mean scores of OSES and its subscales in the control group before, immediately after the last session, and one month later (P≥0.05) (Table 3).
Effectiveness of the empowerment program on HBM constructs
Before the intervention, there were no significant differences between the two groups in terms of HBM constructs scores (P≥0.05). However, the mean scores of the HBM constructs were significantly different between the two groups immediately after the end of the sessions and one month later (P<0.05). The repeated measures ANOVA test showed a significant difference between the mean scores of HBM constructs before, immediately after the last session, and one month later in the intervention group (P<0.05).
There was no significant difference between the mean scores of HBM constructs in the control group before, immediately after the last session, and one month after the intervention (P≥0.05) except for the perceived barriers to calcium intake (P=0.04) and health motivation (P=0.02) (Table 4).
Before the intervention, there were no significant differences between the two groups in terms of HBM constructs scores (P≥0.05). However, the mean scores of the HBM constructs were significantly different between the two groups immediately after the end of the sessions and one month later (P<0.05). The repeated measures ANOVA test showed a significant difference between the mean scores of HBM constructs before, immediately after the last session, and one month later in the intervention group (P<0.05).
There was no significant difference between the mean scores of HBM constructs in the control group before, immediately after the last session, and one month after the intervention (P≥0.05) except for the perceived barriers to calcium intake (P=0.04) and health motivation (P=0.02) (Table 4).
4. Discussion
The objective of this randomized controlled clinical trial was to determine whether osteoporosis self-efficacy would improve after an empowerment program based on the health belief model.
The findings showed that empowerment program based on HBM could be an effective strategy for increasing osteoporosis self-efficacy among older adults. After the empowerment program, the mean score of self-efficacy, both in the subscales of exercise and calcium intake, was significantly higher in the intervention group compared to the control group.
Follow-up assessment also revealed that this increase had been maintained one month later. Improvement was observed over time in the level of osteoporosis self-efficacy among the participants in the intervention group compared to the control group. Other researchers have found that educational programs can improve osteoporosis self-efficacy in elderly populations (Baheiraei et al. 2005; Park et al., 2017). It has been found that osteoporosis prevention education can increase self-efficacy related to calcium intake (Tussing & Chapman-Novakofski, 2005).
However, Sedlak et al. (Sedlak et al. 2005) reported that interventions to enhance osteoporosis prevention did not have any effect on calcium intake in post-menopausal women. They also found that these interventions led to a decrease in weight-bearing exercises in these women. It has been shown that osteoporosis preventive interventions have no effect on calcium intake and physical activity subscales of self-efficacy in older women (Jessup et al. 2003).
In this study, all HBM constructs (perceived susceptibility, perceived severity, perceived benefits, barriers of exercise, perceived benefits, barriers to calcium intake, and health motivation) were influenced by the empowerment program. Improvement was observed over time in all these constructs among participants in the intervention group compared to the control group. These significant findings of the study can be attributed to the richness of the education program that was presented in multiple sessions with different educational approaches, using assignments related to osteoporosis prevention behaviors, inviting an old volunteer with a history of osteoporosis, and engagement of the family members in the management of the disease.
Sharing and providing information on osteoporosis in the HBM-based education program and discussion about related cases could be useful in raising sensitivity perception, promoting the perceptions of benefits (Hsieh et al. 2014; Kalkim & Dağhan 2017) and barriers (Hsieh et al. 2014; Khani Jeihooni et al., 2017) and health motivation (Kalkim & Dağhan 2017)that result in osteoporosis preventive behaviors (Kalkim & Dağhan, 2017). In this area, different results have been reported in previous studies, and the osteoporosis prevention program had different effects on the various constructs of HBM. For example, it has been found that osteoporosis preventive interventions could increase perceived susceptibility to osteoporosis and perceived benefits related to increased calcium intake (Tussing & Chapman-Novakofski 2005).
A significant improvement was reported in osteoporosis perceived susceptibility, perceived benefits of exercise, perceived barriers to calcium, and perceived barriers to exercise in older adults (Aree-Ue et al. 2006). It has also been revealed that tailored interventions to enhance osteoporosis prevention can improve perceived barriers to calcium intake and perceived barriers to exercise in postmenopausal women (Sedlak et al. 2005). In another study, however, the osteoporosis education program was only associated with improvement in calcium intake and did not affect other health belief subscales (Babatunde 2011).
The findings of the current study suggest the value of empowerment programs with a theoretical underpinning to improve osteoporosis self-efficacy and health beliefs in older adults. It can increase the ability to control hardships and side-effects of the disease in this population.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in this study were in accordance with the ethical standards of the Institutional and or National Research Committee and with the 1964 Helsinki Declaration and its amendments or comparable ethical standards. This trial was registered to the Iranian Randomized Controlled Trial with the registry number: IRCT201707248348N36. The Ethics Committee of Vice Chancellor for Research, KUMS approved the study (Ethics code: IR.KAUMS.NUHEPM.REC.1396.14). All participants were informed on the study procedure and its objectives and signed informed consent. They were fully aware of their voluntary participation and the right to withdraw at any time. Also, they were assured that their anonymity would be protected and their personal information would be kept confidential.
Funding
This research was financially supported by the Kashan University of Medical Science (Grant No.: 9697).
Authors' contributions
Conceptualization, Investigation, Writing-Original Draft, Supervision: Neda Mirbagher Ajorpaz; Collecting data: MehdiVtankhah and Mostafa Gholami; Writing review and Editing: Mahboubeh Rezaei, Batool Zamani; and Funding Acquisition: All authors.
Conflict of interest
All authors of this article declare no conflicts of interest.
Acknowledgments
The authors acknowledge Kashan University of Medical Sciences for its financial support.
References
Anderson, E. S., et al., 2010. Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: Social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. Journal of Health Psychology, 15(1), pp. 21-32. [DOI:10.1177/1359105309342297] [PMID]
Aree-Ue, S., et al., 2006. Osteoporosis preventive behavior in Thai older adults: Feasibility and acceptability. Journal of Gerontological Nursing, 32(7), pp. 23-30. [PMID]
Babatunde, O. T., et al., 2011. Theory-driven intervention improves calcium intake, osteoporosis knowledge, and self-efficacy in community-dwelling older black adults. Journal of Nutrition Education and Behavior, 43(6), pp. 434-40. [DOI:10.1016/j.jneb.2010.07.004] [PMID]
Baheiraei, A., et al., 2005. Psychometric properties of the Persian version of the osteoporosis knowledge and health belief questionnaires. Maturitas, 50(2), pp. 134-9. [DOI:10.1016/j.maturitas.2004.05.001] [PMID]
Bastani, F., et al., 2016. Factors associated with fear of falling and functional independence in older adults in Iranian Nursing Homes. Journal of Client-Centered Nursing Care, 2(3), pp. 135-44. [DOI:10.32598/jccnc.2.3.135]
Dan, X., et al., 2018. Relationships among structural empowerment, innovative behaviour, self‐efficacy, and career success in nursing field in mainland China. International Journal of Nursing Practice, 24(5), p. e12674. [DOI:10.1111/ijn.12674] [PMID]
Doba, N., et al., 2016. Assessment of self-efficacy and its relationship with frailty in the elderly. Internal Medicine, 55(19), pp. 2785-92. [DOI:10.2169/internalmedicine.55.6924] [PMID] [PMCID]
Doosti-Irani, A., Ghafari, M. & Cheraghi, Z., 2018. The high prevalence of osteoporosis as a preventable disease: The need for greater attention to prevention programs in Iran. Iranian Journal of Public Health, 47(8), pp. 1220-1. [PMID] [PMCID]
Ebrahimi, H., et al., 2016. Evaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial study. Primary Care Diabetes, 10(2), pp. 129-35. [DOI:10.1016/j.pcd.2015.09.003] [PMID]
French, D. P., et al., 2014. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Annals of Behavioral Medicine, 48(2), pp. 225-34. [DOI:10.1007/s12160-014-9593-z] [PMID]
Gallaghe, N. A., et al., 2015. Self-efficacy, neighborhood walking, and fall history in older adults. Journal of Aging and Physical Activity, 23(1), pp. 64-71. [DOI:10.1123/JAPA.2012-0287] [PMID]
Heidari, S., et al., 2017. Religious practices and self-care in Iranian patients with type 2 diabetes. Journal of Religion and Health, 56(2), pp. 683-96. [DOI:10.1007/s10943-016-0320-x] [PMID]
Horan, M. L., et al., 1998. Development and evaluation of the osteoporosis self‐efficacy scale. Research in Nursing & Health, 21(5), pp. 395-403. [DOI:10.1002/(SICI)1098-240X(199810)21:53.0.CO;2-I]
Hosseinian, M., Ajorpaz, N. M. & Manesh, S. E., 2015. Mothers’ satisfaction with two systems of providing care to their hospitalized children. Iranian Red Crescent Medical Journal, 17(2), p. e23333. [DOI:10.5812/ircmj.23333] [PMID] [PMCID]
Hsieh, E., et al., 2014. Osteoporosis knowledge, self-efficacy, and health beliefs among Chinese individuals with HIV. Archives of Osteoporosis, 9(1), p. 201. [DOI:10.1007/s11657-014-0201-4] [PMID] [PMCID]
Janiszewska, M., et al., 2017. General self-efficacy level and health behaviours in women over the age of 45 years who have undergone osteoporosis treatment. Menopause Review, 16(3), p. 86. [DOI:10.5114/pm.2017.70584] [PMID] [PMCID]
Jessup, J. V., et al., 2003. Effects of exercise on bone density, balance, and self-efficacy in older women. Biological Research for Nursing, 4(3), pp. 171-80. [DOI:10.1177/1099800402239628] [PMID]
Kalkım, A. & Dağhan, Ş., 2017. Theory-based osteoporosis prevention education and counseling program for women: a randomized controlled trial. Asian Nursing Research, 11(2), pp. 119-27. [DOI:10.1016/j.anr.2017.05.010] [PMID]
Kanis, J. A., et al., 2013. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporosis International, 24(1), pp. 23-57. [DOI:10.1007/s00198-012-2074-y] [PMID] [PMCID]
Keshtkar, A., et al., 2015. Clinical performance of seven prescreening tools for osteoporosis in Iranian postmenopausal women. Rheumatology International, 35(12), pp.1995-2004. [DOI:10.1007/s00296-015-3286-1] [PMID]
Khani Jeihooni, A., et al., 2017. RETRACTED: The effect of an educational program based on health belief model and social cognitive theory in prevention of osteoporosis in women. Journal of Health Psychology, 22(5), pp. NP1-11. [DOI:10.1177/1359105315603696] [PMID]
Kim, K. K., et al., 1991. Development and evaluation of the osteoporosis health belief scale. Research in Nursing & Health, 14(2), pp. 155-63. [DOI:10.1002/nur.4770140210]
Lindberg, M. & Fernandes, M. A. M., 2010. Self‐efficacy in relation to limited fluid intake amongst Portuguese haemodialysis patients. Journal of Renal Care, 36(3), pp.133-8. [DOI:10.1111/j.1755-6686.2010.00182.x] [PMID]
Moein, M., et al., 2017. Effect of an empowerment program on self-efficacy of patients with type 2 diabetes. Iranian Red Crescent Medical Journal, 19(1), p. 29252. [DOI:10.5812/ircmj.29252]
Omidvar, S., Jafari Jozani, M. & Nematollahi, N., 2018. Judgment post‐stratification in finite mixture modeling: An example in estimating the prevalence of osteoporosis. Statistics in medicine, 37(30), pp. 4823-36. [DOI:10.1002/sim.7984] [PMID]
Park, K. S., et al., 2017. Education and exercise program improves osteoporosis knowledge and changes calcium and vitamin D dietary intake in community dwelling elderly. BMC Public Health, 17(1), p. 966. [DOI:10.1186/s12889-017-4966-4] [PMID] [PMCID]
Rodrigues, A. M., et al., 2018. Portuguese recommendations for the prevention, diagnosis and management of primary osteoporosis-2018 update. Acta Reumatologica Portuguesa, 43(1), pp. 123-44.
Royani, Z., et al., 2013. The effect of empowerment program on empowerment level and self-care self-efficacy of patients on hemodialysis treatment. Iranian Journal of Nursing and Midwifery Research, 18(1), pp. 84-7. [PMID] [PMCID]
Sedlak, C. A., et al., 2005. Tailored interventions to enhance osteoporosis prevention in women. Orthopaedic Nursing, 24(4), pp. 270-6. [DOI:10.1097/00006416-200507000-00007]
Shin, D. S., Kim, C. J. & Choi, Y. J., 2016. Effects of an empowerment program for self‐management among rural older adults with hypertension in S outh K orea. Australian Journal of Rural Health, 24(3), pp. 213-9. [DOI:10.1111/ajr.12253] [PMID]
Tussing, L. & Chapman-Novakofski, K., 2005. Osteoporosis prevention education: Behavior theories and calcium intake. Journal of the American Dietetic Association, 105(1), pp. 92-7. [DOI:10.1016/j.jada.2004.10.025] [PMID]
Zhang, M., 2017. Effect of HBM rehabilitation exercises on depression, anxiety and health belief in elderly patients with osteoporotic fracture. Psychiatria Danubina, 29(4), pp. 466-72. [DOI:10.24869/psyd.2017.466] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2018/07/17 | Accepted: 2018/12/12 | Published: 2019/02/1
Received: 2018/07/17 | Accepted: 2018/12/12 | Published: 2019/02/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |