Fri, Oct 17, 2025
[Archive]
Volume 7, Issue 2 (Spring 2021)
JCCNC 2021, 7(2): 87-96 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rafii F, Javaheri Tehrani F, Nikbakht Nasrabadi A, Shariatpanahi S. How Do Nurses Apply Personal Knowing to Patient Care? A Grounded Theory Study. JCCNC 2021; 7 (2) :87-96
URL: http://jccnc.iums.ac.ir/article-1-306-en.html
URL: http://jccnc.iums.ac.ir/article-1-306-en.html
Forough Rafii1 

 , Fereshteh Javaheri Tehrani *2
, Fereshteh Javaheri Tehrani *2 

 , Alireza Nikbakht Nasrabadi3
, Alireza Nikbakht Nasrabadi3 
 , Shabnam Shariatpanahi4
, Shabnam Shariatpanahi4 



 , Fereshteh Javaheri Tehrani *2
, Fereshteh Javaheri Tehrani *2 

 , Alireza Nikbakht Nasrabadi3
, Alireza Nikbakht Nasrabadi3 
 , Shabnam Shariatpanahi4
, Shabnam Shariatpanahi4 

1- Nursing Care Research Center, Faculty of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Nursing Care Research Center, Faculty of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,fereshte.javaheri@yahoo.com
3- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Community Health Nursing, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Nursing Care Research Center, Faculty of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Community Health Nursing, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Keywords: Nurse-patient relations, Nurse practice patterns, Knowledge, Nursing care, Grounded theory
Full-Text [PDF 610 kb]
(3195 Downloads)
| Abstract (HTML) (9818 Views)
• Nurses use the pattern of personal knowing in three ways; the therapeutic use of self, self-centering, and eliminating therapeutic communication.
• The therapeutic use of self is characterized as effective care and nurse-patient interaction.
• The nurse’s insistence on biases and prejudices is associated with self-centering in patient care.
• The nurse’s discriminatory beliefs are manifested by eliminating therapeutic communications as well as reluctant and mechanical care
Plain Language Summary
Personal knowing refers to the awareness and knowledge of the nurse about the personal characteristics of herself/himself and the patient; it required putting aside biases and prejudices about the patient and using this knowledge for better and higher quality care. If nurses apply personal knowing properly, they will provide interactive and effective care. However, if they have prejudices and biases towards the patient, their care will be focused on themselves rather than the patient. The findings showed that the nurses have used the pattern of personal knowing in 3 ways, including the therapeutic use of self, self-centering, and eliminating therapeutic communication.
• The therapeutic use of self is characterized as effective care and nurse-patient interaction.
• The nurse’s insistence on biases and prejudices is associated with self-centering in patient care.
• The nurse’s discriminatory beliefs are manifested by eliminating therapeutic communications as well as reluctant and mechanical care
Plain Language Summary
Personal knowing refers to the awareness and knowledge of the nurse about the personal characteristics of herself/himself and the patient; it required putting aside biases and prejudices about the patient and using this knowledge for better and higher quality care. If nurses apply personal knowing properly, they will provide interactive and effective care. However, if they have prejudices and biases towards the patient, their care will be focused on themselves rather than the patient. The findings showed that the nurses have used the pattern of personal knowing in 3 ways, including the therapeutic use of self, self-centering, and eliminating therapeutic communication.
Full-Text: (2445 Views)
1. Introduction
Nursing, as a growing knowledge foundation, has authority in education, altruistic social services, ethical codes, workforce employment, and independence. Besides, it is undoubtedly a thriving, motivated, and evolving profession (McEwen & Wills 2018). Nursing requires a strong knowledge foundation to be a profession and the relevant staff has worked hard to achieve this goal. Nursing practice has been based on formal knowledge since Florence Nightingale founded the first formal training for nurses (Cook 2018).
The nature of nursing knowledge has changed over time; however, the fundamental values of nursing practice have been maintained to a considerable extent. Examining the initial nursing texts led to the classification of 4 basic patterns of knowledge. Carper (Carper 1999) referred to the most familiar and noteworthy patterns of knowing as the empirics; ethical knowledge as the moral pattern; self and others’ knowledge in communication as the personal pattern, and the art of nursing, as the aesthetic pattern. These patterns were perfected by Chinn and Kramer (Chinn & Kramer 2013) with the fifth pattern, emancipatory knowledge.
Personal Knowing (PK) as a fundamental pattern of knowing in nursing is the most challenging pattern for learning and teaching. Furthermore, the PK pattern is perhaps the most essential model for understanding the meaning of health concerning individuals’ wellbeing. Nursing as an interpersonal process involves interactions, communication, and exchanges between the nurse and the patient or client. Moreover, growing evidence indicates the quality of interpersonal communication, its potential impact on clients’ getting ill or getting better, and adaptation to illness for clients. Certainly, the therapeutic use of self, i.e., recently received special attention in the literature, refers to an approach in which the nurse considers herself/himself and the client itself; this is the major issue in any therapeutic communication (Carper 1999) . In other words, PK is an expression of self-knowledge concerning others. Moreover, it is also characterized as the most difficult pattern but the most critical one. Nurses must recognize themselves as individuals. They are expected to be able to establish therapeutic and reliable communication between themselves and patients; such measures are a necessity for the nursing profession assisting individuals with their relief process (Escobar-Castellanos & Sanhueza-Alvarado 2018). This pattern refers to the quality and validity of the interpersonal process between nurse and patient. Besides, PK focuses on the importance of recognizing nurses’ genuine selves and their role in respecting patients, as well as how to express their concern and caring for others (Fawcett et al. 2001). The genuine or authentic self is crucial in providing proper nursing care. Authenticity requires the questioning, identifying, and understanding of these factors as personal biases, personality strengths and weaknesses, feelings, values, and attitudes. After identifying and understanding these characteristics, nurses can resolve internal conflicts; therefore, they can provide the best nursing care (Chinn & Kramer 2013).
Caring is the heart of nursing and the communication between individuals, i.e., accompanied by love, compassion, and forgiveness (Watson 2008). Good therapeutic communication is a necessity for authentic care. Furthermore, it requires attention to the environment and context of care, as well as attention to the needs, expectations, values, awareness, and abilities of the patient. Consequently, such measures create effective therapeutic communication, indicating trust between patients and nurses (Wiechula et al. 2016). A desirable therapeutic communication, i.e., continuous, compassionate, associated with trust, respect, and intimacy, facilitates the nurse to understand the viewpoints of patients, makes them aware of patients’ needs and views as an individual, and motivates the patient to intervene in health-related matters. It also causes the nurse to identify patient’s different requirements to provide comprehensive and continuous care and improves the quality of care and achieving wellbeing (Strandås & Bondas 2018). Conversely, without achieving authentic self, personal conflicts and biases interfere with caring for individuals. For example, an unresolved negative bias toward the elderly in an individual will be reflected in their performance (Chinn & Kramer 2013).
Watson’s theory emphasizes caring as a therapeutic communication. Watson believes that nursing is a human-to-human communication in which the nurse influences and is influenced by another individual (Grant & Goodman 2018). Nurses’ proper communication with patients helps them understand patients ‘conditions, improve the quality of care, and patient’s quality of life (Adib-Hajbaghery & Tahmouresi 2018). Nurses’ communication with patients plays a key role in strengthening patients’ health; helps nurses empathy with patients, makes them understand the patients’ views and needs as an individual, and makes it possible for patients to be aware of their treatment process. Nurses’ communication with patients also makes patients active and motivates them. Accordingly, it results in comprehensive care along with the identification of needs and changes, continuous care, trust and intimacy, mutual therapeutic communication, experiencing recovery and wellbeing during illness, and improving patient’s quality of life (Strandås & Bondas 2018). However, according to a study (Agha Mohammad Hasani et al. 2018), >85% of nurses fail to establish proper interpersonal communication, and their ability to communicate, listen and express is moderate. A study on the quality of care in hospitalized patients indicated that most of the patients’ dissatisfaction concerns nurse-patient communication and providing an insufficient and unclear explanation about the tests and treatment process (Karaca & Durna 2018).
Therefore, considering the importance of therapeutic communication in nursing care and contradictory findings of the quality of nurses’ communication with patients, the present study aimed to explore how nurses apply PK to patient care.
The nature of nursing knowledge has changed over time; however, the fundamental values of nursing practice have been maintained to a considerable extent. Examining the initial nursing texts led to the classification of 4 basic patterns of knowledge. Carper (Carper 1999) referred to the most familiar and noteworthy patterns of knowing as the empirics; ethical knowledge as the moral pattern; self and others’ knowledge in communication as the personal pattern, and the art of nursing, as the aesthetic pattern. These patterns were perfected by Chinn and Kramer (Chinn & Kramer 2013) with the fifth pattern, emancipatory knowledge.
Personal Knowing (PK) as a fundamental pattern of knowing in nursing is the most challenging pattern for learning and teaching. Furthermore, the PK pattern is perhaps the most essential model for understanding the meaning of health concerning individuals’ wellbeing. Nursing as an interpersonal process involves interactions, communication, and exchanges between the nurse and the patient or client. Moreover, growing evidence indicates the quality of interpersonal communication, its potential impact on clients’ getting ill or getting better, and adaptation to illness for clients. Certainly, the therapeutic use of self, i.e., recently received special attention in the literature, refers to an approach in which the nurse considers herself/himself and the client itself; this is the major issue in any therapeutic communication (Carper 1999) . In other words, PK is an expression of self-knowledge concerning others. Moreover, it is also characterized as the most difficult pattern but the most critical one. Nurses must recognize themselves as individuals. They are expected to be able to establish therapeutic and reliable communication between themselves and patients; such measures are a necessity for the nursing profession assisting individuals with their relief process (Escobar-Castellanos & Sanhueza-Alvarado 2018). This pattern refers to the quality and validity of the interpersonal process between nurse and patient. Besides, PK focuses on the importance of recognizing nurses’ genuine selves and their role in respecting patients, as well as how to express their concern and caring for others (Fawcett et al. 2001). The genuine or authentic self is crucial in providing proper nursing care. Authenticity requires the questioning, identifying, and understanding of these factors as personal biases, personality strengths and weaknesses, feelings, values, and attitudes. After identifying and understanding these characteristics, nurses can resolve internal conflicts; therefore, they can provide the best nursing care (Chinn & Kramer 2013).
Caring is the heart of nursing and the communication between individuals, i.e., accompanied by love, compassion, and forgiveness (Watson 2008). Good therapeutic communication is a necessity for authentic care. Furthermore, it requires attention to the environment and context of care, as well as attention to the needs, expectations, values, awareness, and abilities of the patient. Consequently, such measures create effective therapeutic communication, indicating trust between patients and nurses (Wiechula et al. 2016). A desirable therapeutic communication, i.e., continuous, compassionate, associated with trust, respect, and intimacy, facilitates the nurse to understand the viewpoints of patients, makes them aware of patients’ needs and views as an individual, and motivates the patient to intervene in health-related matters. It also causes the nurse to identify patient’s different requirements to provide comprehensive and continuous care and improves the quality of care and achieving wellbeing (Strandås & Bondas 2018). Conversely, without achieving authentic self, personal conflicts and biases interfere with caring for individuals. For example, an unresolved negative bias toward the elderly in an individual will be reflected in their performance (Chinn & Kramer 2013).
Watson’s theory emphasizes caring as a therapeutic communication. Watson believes that nursing is a human-to-human communication in which the nurse influences and is influenced by another individual (Grant & Goodman 2018). Nurses’ proper communication with patients helps them understand patients ‘conditions, improve the quality of care, and patient’s quality of life (Adib-Hajbaghery & Tahmouresi 2018). Nurses’ communication with patients plays a key role in strengthening patients’ health; helps nurses empathy with patients, makes them understand the patients’ views and needs as an individual, and makes it possible for patients to be aware of their treatment process. Nurses’ communication with patients also makes patients active and motivates them. Accordingly, it results in comprehensive care along with the identification of needs and changes, continuous care, trust and intimacy, mutual therapeutic communication, experiencing recovery and wellbeing during illness, and improving patient’s quality of life (Strandås & Bondas 2018). However, according to a study (Agha Mohammad Hasani et al. 2018), >85% of nurses fail to establish proper interpersonal communication, and their ability to communicate, listen and express is moderate. A study on the quality of care in hospitalized patients indicated that most of the patients’ dissatisfaction concerns nurse-patient communication and providing an insufficient and unclear explanation about the tests and treatment process (Karaca & Durna 2018).
Therefore, considering the importance of therapeutic communication in nursing care and contradictory findings of the quality of nurses’ communication with patients, the present study aimed to explore how nurses apply PK to patient care.
2. Materials and Methods
Due to the research question and given that PK is rooted in nurse-patient interactions, grounded theory was used in this research. This method is an interactive, constant comparison method for social processes that uses inductive data to develop theory (Charmaz & Henwood 2017). The data collection was initiated in parallel with their analysis. Thus, data analysis began with the first observation and interview and the findings led to the next other interviews or observations (Corbin & Strauss 2008). According to the specific characteristics of grounded theory, the steps of data collection, and data coding and analysis were simultaneous, systematic, and fluid from the beginning of the study. Additionally, the constant comparison method was used for each part of the coding.
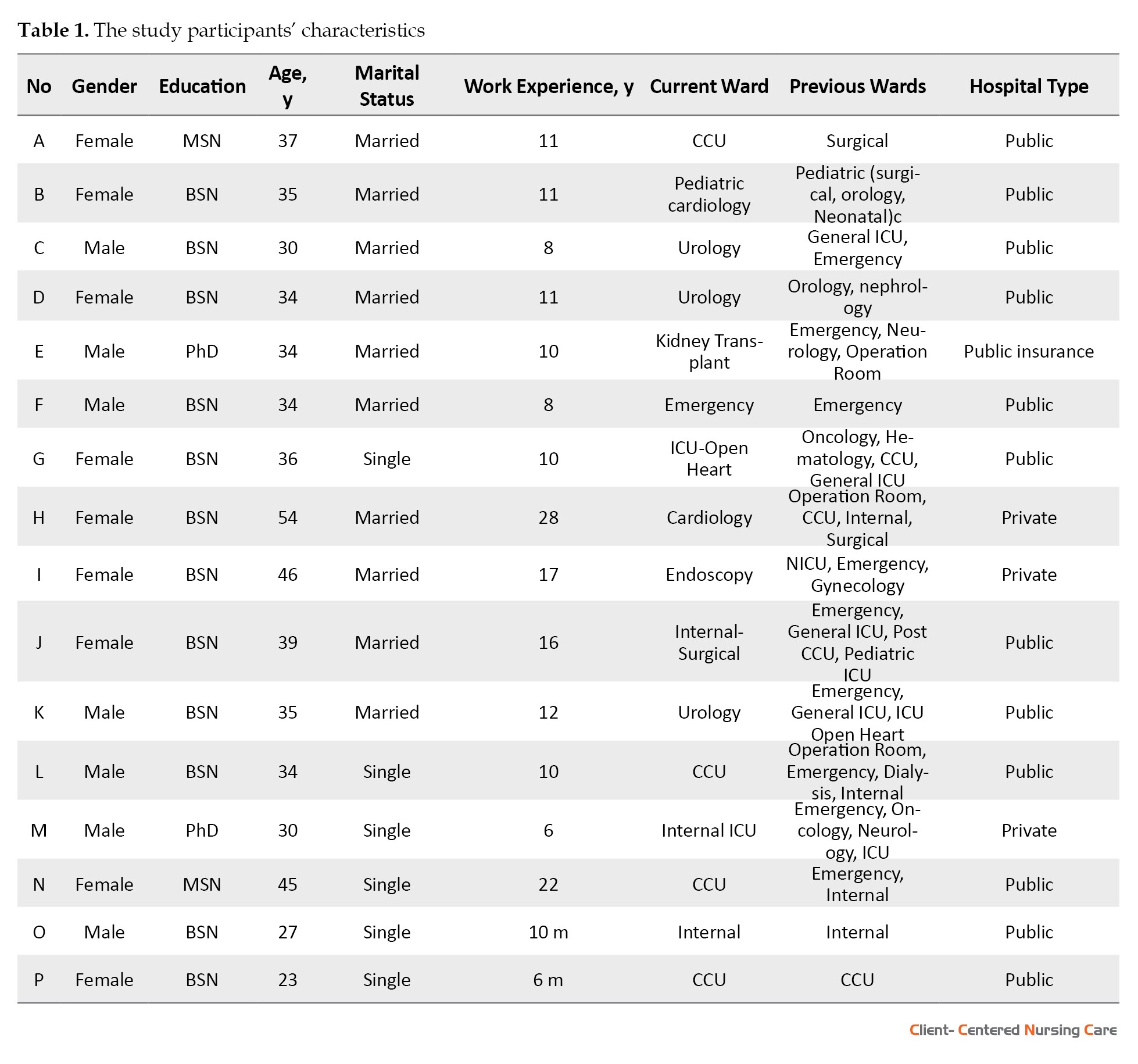
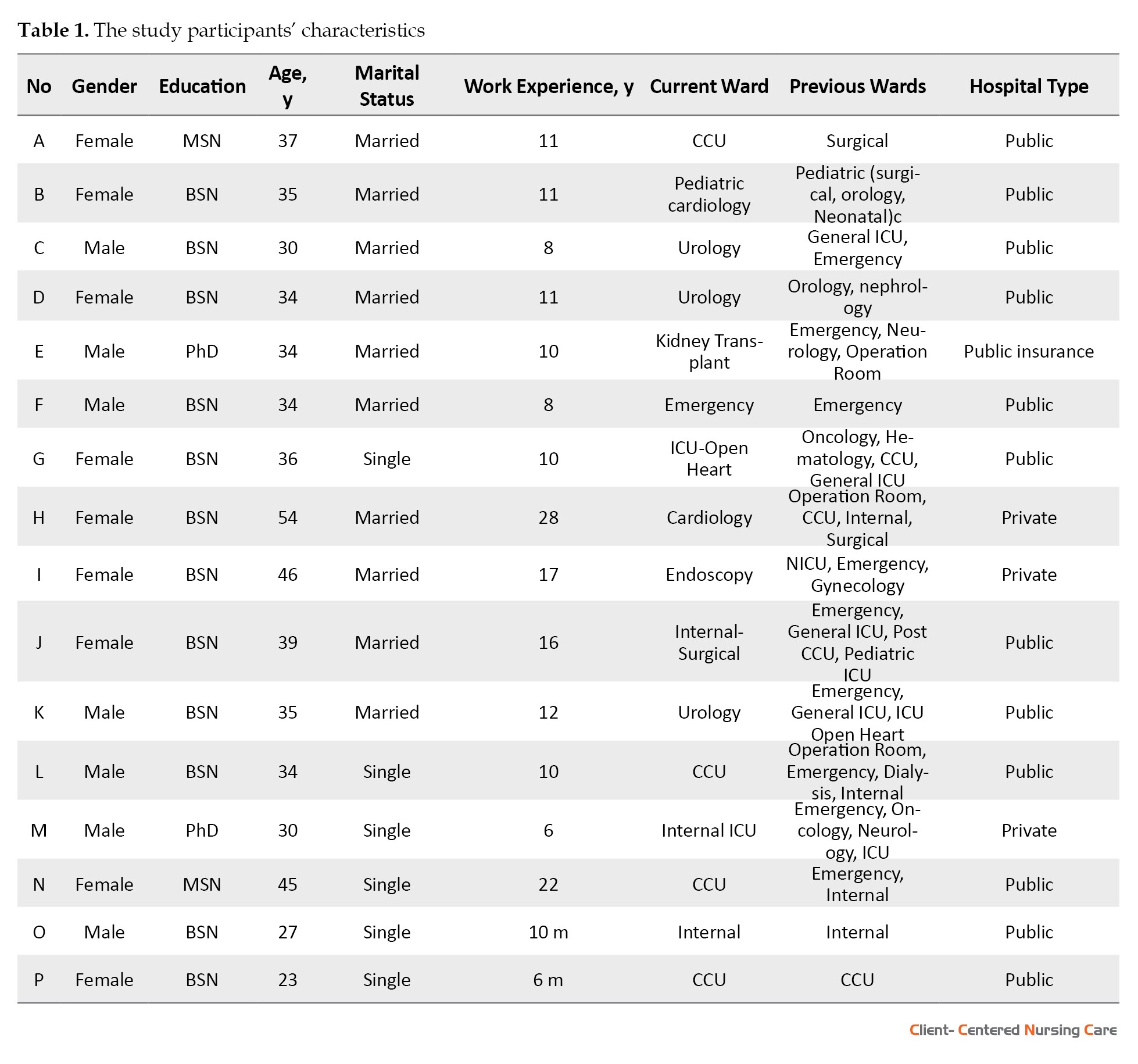
The hospital environment was a natural, common, and uncontrolled environment for observing the interaction between the nurse and the patient and the researcher did not manipulate it (Grove, Burns & Gray 2012); thus, it was selected to obtain the data on how nurses apply PK to patient care. The researchers obtained appropriate information about the contextual application of this pattern and nurses’ experiences (Polit & Beck 2018). The research environment in the present study was different wards of the hospitals in Tehran City, Iran (governed by universities, private sector, & public insurance). Observations were made in the wards of accidents and burns, male urological surgery, emergency, internal medicine, internal Intensive Care Unit (ICU), and post-Coronary Care Unit (CCU). Individual, face-to-face, in-depth, and semi-structured interviews were conducted with the study participant. The study subjects voluntarily answered the research questions (Grove et al. 2012). Furthermore, clinical observations were conducted (Polit & Beck 2018). All study participants held a BA degree or higher in nursing, and all were clinical nurses directly in charge of patient care. Maximum variation sampling was met by selecting male and female nurses with BA, MA, and PhD degrees, different age groups, single and married participants, those employed in private or public insurance-covered hospitals, also different inpatient wards. Finally, 15 interviews were included in the analysis. Eight observation sessions were also held in different wards. The characteristics of the study participants are presented in Table 1.
The collected data were analyzed according to Strauss and Corbin’s grounded theory method (Corbin & Strauss 2008) in 4 consecutive steps, i.e., analyzing for concepts; analyzing for context; bringing the process into the analysis, and integrating categories. Each step of data collection was accompanied by constant analysis and comparison. Moreover, at each step, the paradigm respecting the underlying concepts and the diagram concerning the drawing of categories were compared with the previous diagrams. Finally, after completing the categories and constantly comparing the diagrams, the main process and the core variable were obtained; accordingly, the theoretical model was presented.
The hospital environment was a natural, common, and uncontrolled environment for observing the interaction between the nurse and the patient and the researcher did not manipulate it (Grove, Burns & Gray 2012); thus, it was selected to obtain the data on how nurses apply PK to patient care. The researchers obtained appropriate information about the contextual application of this pattern and nurses’ experiences (Polit & Beck 2018). The research environment in the present study was different wards of the hospitals in Tehran City, Iran (governed by universities, private sector, & public insurance). Observations were made in the wards of accidents and burns, male urological surgery, emergency, internal medicine, internal Intensive Care Unit (ICU), and post-Coronary Care Unit (CCU). Individual, face-to-face, in-depth, and semi-structured interviews were conducted with the study participant. The study subjects voluntarily answered the research questions (Grove et al. 2012). Furthermore, clinical observations were conducted (Polit & Beck 2018). All study participants held a BA degree or higher in nursing, and all were clinical nurses directly in charge of patient care. Maximum variation sampling was met by selecting male and female nurses with BA, MA, and PhD degrees, different age groups, single and married participants, those employed in private or public insurance-covered hospitals, also different inpatient wards. Finally, 15 interviews were included in the analysis. Eight observation sessions were also held in different wards. The characteristics of the study participants are presented in Table 1.
The collected data were analyzed according to Strauss and Corbin’s grounded theory method (Corbin & Strauss 2008) in 4 consecutive steps, i.e., analyzing for concepts; analyzing for context; bringing the process into the analysis, and integrating categories. Each step of data collection was accompanied by constant analysis and comparison. Moreover, at each step, the paradigm respecting the underlying concepts and the diagram concerning the drawing of categories were compared with the previous diagrams. Finally, after completing the categories and constantly comparing the diagrams, the main process and the core variable were obtained; accordingly, the theoretical model was presented.
3. Results
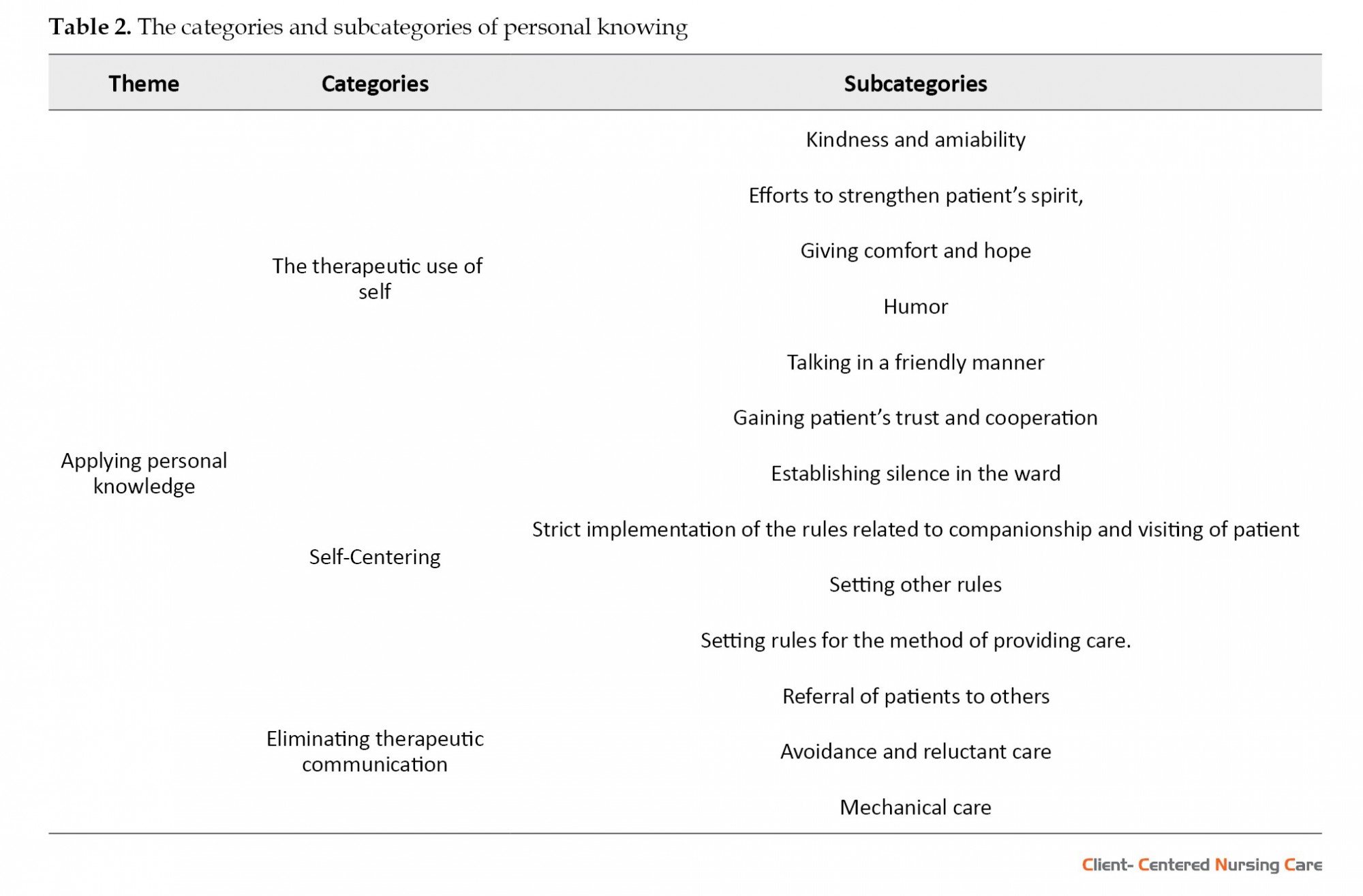
The present study findings revealed that nurses apply the pattern of PK to patient care in 3 general ways; the therapeutic use of self, self-centering, and the elimination of therapeutic communication (Table 2).
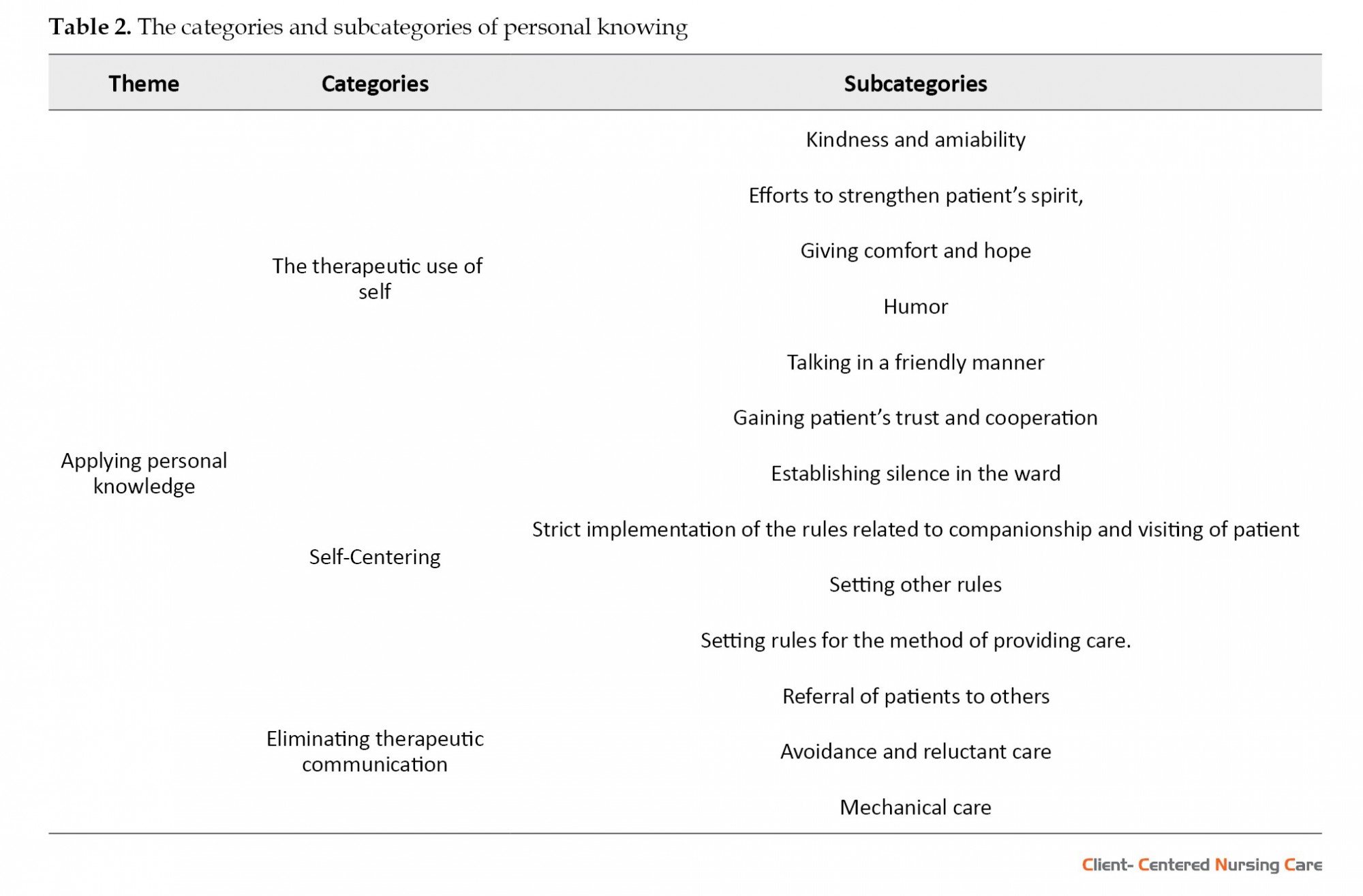
The subcategories of these themes are described as follows:
Therapeutic use of self
The collected findings suggested that nurses, who used therapeutic communication for their patients, presented the following characteristics: kindness and amiability; efforts to strengthen patient’s spirit; providing comfort and hope; humor; talking in a friendly manner, as well as gaining patient’s trust and cooperation. These communications led to positive patient feedback. For example, the following observation in the post-CCU ward demonstrated warm and friendly behavior of the nurse and their answering of the questions of patients and companions:
“While she was writing her nursing reports, she responded to the patients’ visitors. She answered all the questions, even some questions about the location information of other wards. She had good public relations and spoke in a friendly manner with everyone. ...... In each room, she first checked the patient’s medication with a cardex, then took it to the patient. “She greeted all the patients and almost all of the patients gave her positive feedback and treated her warmly and intimately.” Sometimes, nurses used a sense of humor to satisfy patients and achieve a positive outcome of care. For example, Nurse C described the use of humor to cheer up elderly patients, as follows:
“If the patient is old ..... I’d go to him and call him a young man. He says: young?! (surprisingly). I say: Yes, you are young. The patient says: I am 70 years old. I say: Okay, when you are walking, it means you are young.Well, it helps to have better communication. It may not have been written anywhere, but it helps a lot. This gets our job done, and their job done, too.”
The achieved results indicated that using strategies, like holding a birthday party for the patient cheers the patient up. For example, Nurse G mentioned having a birthday party for a patient at the end of her life:
“I was in the CCU, there was a patient with congenital heart disease, she was 21 years old, she was in the end stage of life and there was no hope for her. Her consciousness was at a very low level at that time. A tracheostomy tube had also been performed for her before. Since it was close to her birthday, we got up very early in the morning, went to her bed, inflated balloons, bought cakes and so on, when she woke up, she became very happy at that time, we clapped for her, we invited other nurses and physicians. The patient died later on, but at that moment, the patient and her mother were very happy.”
Self-centering
We observed that sometimes nurses’ biases and prejudices caused them to become self-centered in caring for patients. Biases made nurses prioritize their ability and comfort. The current study findings identified various cases of self-centering, such as establishing silence in the ward, a strict implementation of the rules related to companionship and visiting patients, setting other rules, and developing rules for the method of care provision. An essential case of self-centering was the attempt to create absolute silence in the ward. In such cases, nurses using bullying, coercion, medication, setting sleep rules, or any other possible means, tried to stay away from patients’ noise and questions. For example, in the following observation in the urology surgery ward, one of the cases, i.e., evidently trying to avoid the patient and their companions’ questions.
“A young lady who was the companion of one of the patients came to the nursing station and said to the nurse who had 3 years of experience: “Can I stay until 7 o’clock?
Nurse: Do you promise not to come here and ask any questions?
The young woman while laughing: I promise!
Nurse: Okay, you can stay.”
Sometimes, the nurses, in line with enforcing the ward and hospital regulations, neglected the patient’s condition and have even set various rules. For example, nurse A stated the following reason for not allowing the companions to enter the ward at night:
“I made this rule myself and that refers to the nights and after 9 PM, the companion or the visitor should not be allowed to enter the ward ... this is because patients usually take oxazepam or alprazolam. In this time, if somebody comes in, they will make them and the other patients sleepless... For this reason, I made a rule that I will not let anyone enter the ward after 9 PM. Most of my colleagues follow such a rule, of course, “we made this rule, not the hospital.”
The collected findings indicated that nurse’s bias can lead to self-centering in the method of care provision and nurses prioritizes their comfort, not the patient’s comfort in providing care. For example, nurse A discussed prioritizing care and medication according to her schedule:
“We give patients’ medicine one hour earlier than the prescribed time This is because we should have time to perform other tasks. At the beginning of each work shift, we usually do the routines regarding caring prioritization. In other words, only emergency cases are the priority and based on the patients’ needs, other tasks are performed according to the routine schedules of the wards.”
Eliminating therapeutic relationships
The present study results demonstrated that sometimes the biases and prejudices of nurses lead to discriminatory beliefs; therefore, they provide care without therapeutic communication, resulting in poor care without achieving a positive therapeutic outcome. We identified different cases of the referral of patients to others, avoidance, as well as reluctant and mechanical care. Sometimes nurses referred patients to others. For example, nurse K explained how responding to a patient who frequently calls the nurse has led to referring them to an assistant nurse. “When a patient calls me, I go to him/her once; I know what his problem is; I know he is raising the same issue again and he is in a hurry. Therefore, the second time he/she calls, I think she is dishonest, and I will not go immediately, I will go later or I will send them an assistant nurse.”
Sometimes, discriminatory beliefs caused nurses to attempt to avoid the patient, or if they were forced to provide care, their care was reluctant. This happened in various cases, such as caring for a patient with Acquired Immunodeficiency Syndrome (AIDS), hepatitis, tuberculosis, and substance/alcohol dependence. For example, nurse O addressed her stress concerning a patient with AIDS and hepatitis:
“I’m afraid of patients with AIDS and hepatitis because maybe we become infected with a needle stick, we often put patients like this on a CV-LINE, as we are stressed. The first time when I came here, a patient was HIV-positive; my colleagues mentioned: “why don’t you go to find his vein?” “I said I know if I go to find his vein, I’ll be infected with the needle stick.”
The current research findings indicated that discriminatory biases and beliefs may lead to providing mechanical and heartless care for patients. In other words, the patient was considered as a machine, not a human being; therefore, nurses failed to use emotions to provide care. The relevant findings include numerous cases, such as the following: responding casually without eye contact, not greeting patients, not welcoming newly admitted patients, failure to explain before conducting a procedure, performing a procedure without verbal communication, and not accompanying the newly admitted patient to their bed. The following observation in the urology ward reflects the training during discharge, i.e., performed entirely mechanically.
“The nurse is talking to the companion of a patient who is being discharged: “give her medication according to the instructions, dialysis should be performed according to the routine, clinic time is the month of …. There is nothing else to be mentioned...”
Field note: “Fully mechanical and casual. “She did not even get up from her chair. She also looked at the training sheet of the patient’s record and mentioned a few sentences.”
The following observation that occurs during the transfer of a patient from the emergency room to the ward reflects another instance of mechanical care, as follows:
“When we got to the ward, there was no one at the station to welcome the patient. After about two minutes, a nurse came and took the patient’s record from another nurse. The nurse began to explain: She is 82 years old, diagnosed with hyponatremia, and uses no medication. The nephrology nurse took the record and put it on the station counter, without even glancing at the patient; she went past the stretcher and us and to another room, no greetings, no welcoming, and even no clinical examinations... . ”
The subcategories of these themes are described as follows:
Therapeutic use of self
The collected findings suggested that nurses, who used therapeutic communication for their patients, presented the following characteristics: kindness and amiability; efforts to strengthen patient’s spirit; providing comfort and hope; humor; talking in a friendly manner, as well as gaining patient’s trust and cooperation. These communications led to positive patient feedback. For example, the following observation in the post-CCU ward demonstrated warm and friendly behavior of the nurse and their answering of the questions of patients and companions:
“While she was writing her nursing reports, she responded to the patients’ visitors. She answered all the questions, even some questions about the location information of other wards. She had good public relations and spoke in a friendly manner with everyone. ...... In each room, she first checked the patient’s medication with a cardex, then took it to the patient. “She greeted all the patients and almost all of the patients gave her positive feedback and treated her warmly and intimately.” Sometimes, nurses used a sense of humor to satisfy patients and achieve a positive outcome of care. For example, Nurse C described the use of humor to cheer up elderly patients, as follows:
“If the patient is old ..... I’d go to him and call him a young man. He says: young?! (surprisingly). I say: Yes, you are young. The patient says: I am 70 years old. I say: Okay, when you are walking, it means you are young.Well, it helps to have better communication. It may not have been written anywhere, but it helps a lot. This gets our job done, and their job done, too.”
The achieved results indicated that using strategies, like holding a birthday party for the patient cheers the patient up. For example, Nurse G mentioned having a birthday party for a patient at the end of her life:
“I was in the CCU, there was a patient with congenital heart disease, she was 21 years old, she was in the end stage of life and there was no hope for her. Her consciousness was at a very low level at that time. A tracheostomy tube had also been performed for her before. Since it was close to her birthday, we got up very early in the morning, went to her bed, inflated balloons, bought cakes and so on, when she woke up, she became very happy at that time, we clapped for her, we invited other nurses and physicians. The patient died later on, but at that moment, the patient and her mother were very happy.”
Self-centering
We observed that sometimes nurses’ biases and prejudices caused them to become self-centered in caring for patients. Biases made nurses prioritize their ability and comfort. The current study findings identified various cases of self-centering, such as establishing silence in the ward, a strict implementation of the rules related to companionship and visiting patients, setting other rules, and developing rules for the method of care provision. An essential case of self-centering was the attempt to create absolute silence in the ward. In such cases, nurses using bullying, coercion, medication, setting sleep rules, or any other possible means, tried to stay away from patients’ noise and questions. For example, in the following observation in the urology surgery ward, one of the cases, i.e., evidently trying to avoid the patient and their companions’ questions.
“A young lady who was the companion of one of the patients came to the nursing station and said to the nurse who had 3 years of experience: “Can I stay until 7 o’clock?
Nurse: Do you promise not to come here and ask any questions?
The young woman while laughing: I promise!
Nurse: Okay, you can stay.”
Sometimes, the nurses, in line with enforcing the ward and hospital regulations, neglected the patient’s condition and have even set various rules. For example, nurse A stated the following reason for not allowing the companions to enter the ward at night:
“I made this rule myself and that refers to the nights and after 9 PM, the companion or the visitor should not be allowed to enter the ward ... this is because patients usually take oxazepam or alprazolam. In this time, if somebody comes in, they will make them and the other patients sleepless... For this reason, I made a rule that I will not let anyone enter the ward after 9 PM. Most of my colleagues follow such a rule, of course, “we made this rule, not the hospital.”
The collected findings indicated that nurse’s bias can lead to self-centering in the method of care provision and nurses prioritizes their comfort, not the patient’s comfort in providing care. For example, nurse A discussed prioritizing care and medication according to her schedule:
“We give patients’ medicine one hour earlier than the prescribed time This is because we should have time to perform other tasks. At the beginning of each work shift, we usually do the routines regarding caring prioritization. In other words, only emergency cases are the priority and based on the patients’ needs, other tasks are performed according to the routine schedules of the wards.”
Eliminating therapeutic relationships
The present study results demonstrated that sometimes the biases and prejudices of nurses lead to discriminatory beliefs; therefore, they provide care without therapeutic communication, resulting in poor care without achieving a positive therapeutic outcome. We identified different cases of the referral of patients to others, avoidance, as well as reluctant and mechanical care. Sometimes nurses referred patients to others. For example, nurse K explained how responding to a patient who frequently calls the nurse has led to referring them to an assistant nurse. “When a patient calls me, I go to him/her once; I know what his problem is; I know he is raising the same issue again and he is in a hurry. Therefore, the second time he/she calls, I think she is dishonest, and I will not go immediately, I will go later or I will send them an assistant nurse.”
Sometimes, discriminatory beliefs caused nurses to attempt to avoid the patient, or if they were forced to provide care, their care was reluctant. This happened in various cases, such as caring for a patient with Acquired Immunodeficiency Syndrome (AIDS), hepatitis, tuberculosis, and substance/alcohol dependence. For example, nurse O addressed her stress concerning a patient with AIDS and hepatitis:
“I’m afraid of patients with AIDS and hepatitis because maybe we become infected with a needle stick, we often put patients like this on a CV-LINE, as we are stressed. The first time when I came here, a patient was HIV-positive; my colleagues mentioned: “why don’t you go to find his vein?” “I said I know if I go to find his vein, I’ll be infected with the needle stick.”
The current research findings indicated that discriminatory biases and beliefs may lead to providing mechanical and heartless care for patients. In other words, the patient was considered as a machine, not a human being; therefore, nurses failed to use emotions to provide care. The relevant findings include numerous cases, such as the following: responding casually without eye contact, not greeting patients, not welcoming newly admitted patients, failure to explain before conducting a procedure, performing a procedure without verbal communication, and not accompanying the newly admitted patient to their bed. The following observation in the urology ward reflects the training during discharge, i.e., performed entirely mechanically.
“The nurse is talking to the companion of a patient who is being discharged: “give her medication according to the instructions, dialysis should be performed according to the routine, clinic time is the month of …. There is nothing else to be mentioned...”
Field note: “Fully mechanical and casual. “She did not even get up from her chair. She also looked at the training sheet of the patient’s record and mentioned a few sentences.”
The following observation that occurs during the transfer of a patient from the emergency room to the ward reflects another instance of mechanical care, as follows:
“When we got to the ward, there was no one at the station to welcome the patient. After about two minutes, a nurse came and took the patient’s record from another nurse. The nurse began to explain: She is 82 years old, diagnosed with hyponatremia, and uses no medication. The nephrology nurse took the record and put it on the station counter, without even glancing at the patient; she went past the stretcher and us and to another room, no greetings, no welcoming, and even no clinical examinations... . ”
4. Discussion
The current research findings indicated that some nurses present therapeutic relationships that reflect mutual trust, along with intimacy and kindness, intending to improve patient’s spirit and comfort them, providing hope, as well as gaining patient’s trust and cooperation. They use humor and talking in a friendly manner with their patients. The nurse gave the patient the right to listen to an apology and comforted them in the event of a mistake. Some study participants described situations in which the patient was reluctant to communicate, and the nurse, through her communicative methods, could communicate with them and gain their trust. The therapeutic use of self, which according to Rolfe (Rolfe 2006) roots in psychotherapy. Besides, it was later introduced in the health and nursing sciences, including a set of conscious or thoughtful individual or human competencies, i.e., used in a therapeutic interaction with individuals, mostly in the form of a caring and supportive counseling relationship. Freshwater was quoted as saying by Travelbee, the therapeutic use of self occurs when the nurse uses himself/herself, his/her personality, and knowledge to make changes in the patient. This change is treatment because it relieves the patient’s stress (Freshwater 2002). The therapeutic use of self, as defined by Peloquin, refers to the planned use of personality, insights, perception, and judgment as part of the therapeutic process (Solman & Clouston 2016). Chinn and Kramer considered the therapeutic use of self as a coherent expression of the pattern of knowing in practice, i.e., central to a nurse’s healing art. This is because the authentic self becomes more apparent than ever and allows real interaction with others to facilitate patient health and remedy. To achieve this ability, a nurse needs to recognize and acknowledge her/his nature and overcome biases and attitudes which disturb understanding and caring for others (Chinn & Kramer 2013). The authentic self in this regard requires the unconditional acceptance of others and their identification as a constantly evolving being, not a fixed and unchanging being (Carper 1999). Individuals around each person recognize them by a certain appearance and name; however, this identification is not limited to appearances. Besides, individuals are known by the characteristics of self. For example, a subject may be known with a sense of humor, or another for liking legumes and not carrots or being afraid of height. These characteristics distinguish “you” from “others”. Your recognition of self is, to some extent, consistent with what others have perceived. For example, you may not consider yourself humorous unless others provide you with such feedback; or you may not be aware of your interest in or hatred of certain foods per what has been revealed to others. After gaining this awareness, you reflect on it and gradually choose how to be and how to be known in the world. Accordingly, this is the process of PK. Furthermore, PK continues until one reaches change and growth towards wholeness, authenticity, validity, as well as the harmony of mind-body and spirit. With sufficient self-knowledge, the nurse gaining sufficient knowledge of self has achieved authentic self, i.e., a tool for thoughtful action and interaction (Chinn & Kramer 2013).
We observed that nurses, sometimes under the influence of their preconceptions and mindsets, might provide self-centered care. In these situations, the nurse adopts a method, i.e., more appropriate for their mindsets, beliefs, abilities, and values. It may be possible to make a semantic connection between the concept of self-centering and arrogance. Arrogance reflects selfishness, in which a subject considers their values to be more valuable than those of others and considers self, needless of others’ respect, advice, and feedback (Hareli & Weiner 2000). In a literature review, hospital routines were introduced as an obstacle to patient-centered care; it is explained that some nurses consider the routines and traditions of hospital and ward necessary. They believe that without their implementation, the discipline of the ward will be disrupted. These routines, like equipment testing, seem so necessary, i.e., preferred over the patient-nurse relationship. Excessively controlled and disciplined work environments have less safety and less creativity for developing nurse-patient relationships. The nurse’s high desire for professionalism and personal development was another barrier to patient-centered care in this study. From this perspective, nurses further focus on acquiring their knowledge and skills than on their patients. Professional competition between nurses is an obstacle to their compassion in patient care; care without compassion cannot be patient-centered (Kelly 2007).
Sometimes, nurses’ discriminatory beliefs and biases may lead to eliminating therapeutic relationships with the patient; therefore, nurses may offer mechanical, avoidance-based care, along with a sense of reluctance and coercion. Regarding the cause of discrimination between patients, some occupational discrimination, such as the division of duties, organizational structure, and workforce turnover, the limitation of resources, and work environment are the source of organizational differences. Such conditions pressurize healthcare providers in a complex clinical environment with a large volume of patient care (Kim et al. 2017). Resource allocation, professional communication between health personnel, increased workload, the job satisfaction of nurses, and their decision to continue their profession are associated with a lack of nursing care. In other words, it results in a reduction in the quality of care (Blackman et al. 2015). Besides, interpersonal and inter-colleague conflicts were also significantly related to the omission of care; subsequently, they present long-term effects on care provision, especially in the geriatric care unit (Hogh, Baernholdt & Clausen 2018).
We observed that nurses, sometimes under the influence of their preconceptions and mindsets, might provide self-centered care. In these situations, the nurse adopts a method, i.e., more appropriate for their mindsets, beliefs, abilities, and values. It may be possible to make a semantic connection between the concept of self-centering and arrogance. Arrogance reflects selfishness, in which a subject considers their values to be more valuable than those of others and considers self, needless of others’ respect, advice, and feedback (Hareli & Weiner 2000). In a literature review, hospital routines were introduced as an obstacle to patient-centered care; it is explained that some nurses consider the routines and traditions of hospital and ward necessary. They believe that without their implementation, the discipline of the ward will be disrupted. These routines, like equipment testing, seem so necessary, i.e., preferred over the patient-nurse relationship. Excessively controlled and disciplined work environments have less safety and less creativity for developing nurse-patient relationships. The nurse’s high desire for professionalism and personal development was another barrier to patient-centered care in this study. From this perspective, nurses further focus on acquiring their knowledge and skills than on their patients. Professional competition between nurses is an obstacle to their compassion in patient care; care without compassion cannot be patient-centered (Kelly 2007).
Sometimes, nurses’ discriminatory beliefs and biases may lead to eliminating therapeutic relationships with the patient; therefore, nurses may offer mechanical, avoidance-based care, along with a sense of reluctance and coercion. Regarding the cause of discrimination between patients, some occupational discrimination, such as the division of duties, organizational structure, and workforce turnover, the limitation of resources, and work environment are the source of organizational differences. Such conditions pressurize healthcare providers in a complex clinical environment with a large volume of patient care (Kim et al. 2017). Resource allocation, professional communication between health personnel, increased workload, the job satisfaction of nurses, and their decision to continue their profession are associated with a lack of nursing care. In other words, it results in a reduction in the quality of care (Blackman et al. 2015). Besides, interpersonal and inter-colleague conflicts were also significantly related to the omission of care; subsequently, they present long-term effects on care provision, especially in the geriatric care unit (Hogh, Baernholdt & Clausen 2018).
5. Conclusion
The present study findings indicated that nurses use the pattern of PK in 3 forms, as follows: the therapeutic use of self, self-centering, and eliminating therapeutic communication. The therapeutic use of self leads to providing care with effective interaction between nurse and patient; accordingly, a positive outcome of care and satisfaction of nurse and patient is achieved. However, in the case of self-centering in providing care, this relationship will fade; consequently, care will be without an effective relationship and the insistence will be on biases and prejudices. If prejudices and biases lead to discriminatory beliefs, therapeutic relationships in care will be eliminated and the nurse provides reluctant and mechanical care; thus, it results in poor care and failure to achieve a positive care outcome. The obtained data added to the knowledge of patterns of knowing. Accordingly, these data can be implemented in nursing that can be used in planning nursing education concerning care associated with therapeutic communication. Researchers can also use the collected findings to perform research on other patterns of knowing, like ethical or aesthetic patterns. Despite the innovation in the topic discussed in the present study, it was associated with limitations; one of its limitations has been the abstractness of the topic and the difficulty of understanding the concept by the research participants.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Iran University of Medical Sciences (Code: IR.IUMS.FMD.REC).All ethical principles are considered in this article. The participants were informed about the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This study was financially supported by the Iran University of Medical Sciences.
Authors' contributions
Conceptualization and methodology: Forough Rafii and Fereshteh Javaheri Tehrani; Supervision: Forough Rafii and Alireza Nikbakht Nasrabadi; Investigation, writing – original draft: Fereshteh Javaheri Tehrani, Shabnam Shariat Panahi; Review & editing: All authors; Data analysis: Fereshteh Javaheri Tehrani and Forough Rafii; Funding acquisition; Forough Rafii.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgments
We would like to thank the Research Committee of Iran University of Medical Sciences for its financial support.
References:
Adib-Hajbaghery, M. & Tahmouresi, M., 2018. Nurse-patient relationship based on the imogene king’s theory of goal attainment. Nursing and Midwifery Studies, 7(3), pp. 141-4. [DOI:10.4103/2322-1488.235636]
Agha Mohammad Hasani, P., et al. 2018. Interpersonal communication skills and its association with personality dimensions of nurses in Rafsanjan University of Medical Sciences, Iran, in 2015. Journal of Occupational Health and Epidemiology, 7(2), pp. 112-8. [DOI:10.29252/johe.7.2.112]
Blackman, I., et al. 2015. Factors influencing why nursing care is missed. Journal of Clinical Nursing, 24(1-2), pp. 47-56. [DOI:10.1111/jocn.12688] [PMID]
Carper, B. A., 1999. Fundamental patterns of knowing in nursing. In: E. C. Polifroni. & M. Welch (eds), Perspectives on philosophy of science in nursing: An historical and contemporary anthology. Philadelphia: Lippincott. https://books.google.com/books?id=PorUZQ0m2YgC&dq
Charmaz, K. & Henwood, K., 2017. Grounded theory methods for qualitative psychology. In: C. Willing. & W. S. Rogers (eds), The SAGE handbook of qualitative research in psychology. Thousand Oaks: SAGE [DOI:10.4135/9781526405555.n14]
Chinn, P. L. & Kramer, M. K., 2013. Integrated theory & knowledge development in nursing- E-Book. Riverport Lane: Elsevier Health Sciences. https://books.google.com/books?id=kdPsAwAAQBAJ&dq
Cook, E. T., 2018. The life of Florence Nightingale. Vol 1. Norderstedt: BoD-Books on Demand. https://books.google.com/books?id=8ylwDwAAQBAJ&dq
Corbin, J. & Strauss, A., 2008. Basic of qualitative research techniques and procedures for developing grounded theory. Thousand Oaks: SAGE. https://books.google.com/books?id=Lp9UzAEACAAJ&dq
Escobar-Castellanos, B. & Sanhueza-Alvarado, O., 2018. Carper knowledge patterns and expression in nursing care: Review study. Enfermería: Cuidados Humanizados, 7(1), pp. 73-87. [DOI:10.22235/ech.v7i1.1540]
Fawcett, J., et al. 2001. On nursing theories and evidence. Journal of Nursing Scholarship, 33, pp. 115-9. [DOI:10.1111/j.1547-5069.2001.00115.x] [PMID]
Freshwater, D., 2002. Therapeutic nursing: Improving patient care through self-awareness and reflection. London: SAGE. https://books.google.com/books?id=ZXut4lprSTAC&dq
Grant, A. & Goodman, B., 2018. Communication and interpersonal skills in nursing. London: Learning Matters. https://books.google.com/books?id=6uN3DwAAQBAJ&dq
Grove, S. K., Burns, N. & Gray, J., 2012. The practice of nursing research: Appraisal, synthesis, and generation of evidence. Riverport Lane: Elsevier Health Sciences. https://books.google.com/books?id=r32jPNVYIacC&dq
Hareli, S. & Weiner, B., 2000. Accounts for success as determinants of perceived arrogance and modesty. Motivation and Emotion, 24(3), pp. 215-36. [DOI:10.1023/A:1005666212320]
Hogh, A., Baernholdt, M. & Clausen, T., 2018. Impact of workplace bullying on missed nursing care and quality of care in the eldercare sector. International Archives of Occupational and Environmental Health, 91(8), pp. 963-70. [DOI:10.1007/s00420-018-1337-0] [PMID]
Karaca, A. & Durna, Z., 2018. [Psychosocial support in epilepsy patient (Turkish)]. Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi, 7(1), pp. 218-25. https://atif.sobiad.com/index.jsp?modul=makale-detay&Alan=tip&Id=AWQ3Jh42HDbCZb_mQbJ6
Kelly, J., 2007. Barriers to achieving patient-centered care in Ireland. Dimensions of Critical Care Nursing, 26(1), pp. 29-34. [DOI:10.1097/00003465-200701000-00008] [PMID]
Kim, S., et al. 2017. Individual, interpersonal, and organisational factors of healthcare conflict: A scoping review. Journal of Interprofessional Care, 31(3), pp. 282-90. [DOI:10.1080/13561820.2016.1272558] [PMID]
McEwen, M. & Wills, E. M., 2018. Theoretical basis for nursing.Philadelphia PA: Wolters Kluwer. https://books.google.com/books?id=IfKQswEACAAJ&dq
Polit, D. F. & Beck, C. T., 2018. Essentials of nursing research: Appraising evidence for nursing practice. Philadelphia PA: Wolters Kluwer. https://books.google.com/books?id=Z6DwjwEACAAJ&dq
Rolfe, G., 2006. Nursing praxis and the science of the unique. Nursing Science Quarterly, 19(1), pp. 39-43. [DOI:10.1177/0894318405284128] [PMID]
Solman, B. & Clouston, T., 2016. Occupational therapy and the therapeutic use of self. British Journal of Occupational Therapy, 79(8), pp. 514-6. [DOI:10.1177/0308022616638675]
Strandås, M. & Bondas, T., 2018. The nurse-patient relationship as a story of health enhancement in community care: A meta‐ethnography. Journal of Advanced Nursing, 74(1), pp. 11-22. [DOI:10.1111/jan.13389] [PMID]
Watson, J., 2008. Assessing and measuring caring in nursing and health science. New York: Springer Publishing Company. https://books.google.com/books?id=7eAKbr-TqgEC&dq
Wiechula, R., et al. 2016. Umbrella review of the evidence: what factors influence the caring relationship between a nurse and patient? Journal of Advanced Nursing, 72(4), pp. 723-34. [DOI:10.1111/jan.12862] [PMID]
Agha Mohammad Hasani, P., et al. 2018. Interpersonal communication skills and its association with personality dimensions of nurses in Rafsanjan University of Medical Sciences, Iran, in 2015. Journal of Occupational Health and Epidemiology, 7(2), pp. 112-8. [DOI:10.29252/johe.7.2.112]
Blackman, I., et al. 2015. Factors influencing why nursing care is missed. Journal of Clinical Nursing, 24(1-2), pp. 47-56. [DOI:10.1111/jocn.12688] [PMID]
Carper, B. A., 1999. Fundamental patterns of knowing in nursing. In: E. C. Polifroni. & M. Welch (eds), Perspectives on philosophy of science in nursing: An historical and contemporary anthology. Philadelphia: Lippincott. https://books.google.com/books?id=PorUZQ0m2YgC&dq
Charmaz, K. & Henwood, K., 2017. Grounded theory methods for qualitative psychology. In: C. Willing. & W. S. Rogers (eds), The SAGE handbook of qualitative research in psychology. Thousand Oaks: SAGE [DOI:10.4135/9781526405555.n14]
Chinn, P. L. & Kramer, M. K., 2013. Integrated theory & knowledge development in nursing- E-Book. Riverport Lane: Elsevier Health Sciences. https://books.google.com/books?id=kdPsAwAAQBAJ&dq
Cook, E. T., 2018. The life of Florence Nightingale. Vol 1. Norderstedt: BoD-Books on Demand. https://books.google.com/books?id=8ylwDwAAQBAJ&dq
Corbin, J. & Strauss, A., 2008. Basic of qualitative research techniques and procedures for developing grounded theory. Thousand Oaks: SAGE. https://books.google.com/books?id=Lp9UzAEACAAJ&dq
Escobar-Castellanos, B. & Sanhueza-Alvarado, O., 2018. Carper knowledge patterns and expression in nursing care: Review study. Enfermería: Cuidados Humanizados, 7(1), pp. 73-87. [DOI:10.22235/ech.v7i1.1540]
Fawcett, J., et al. 2001. On nursing theories and evidence. Journal of Nursing Scholarship, 33, pp. 115-9. [DOI:10.1111/j.1547-5069.2001.00115.x] [PMID]
Freshwater, D., 2002. Therapeutic nursing: Improving patient care through self-awareness and reflection. London: SAGE. https://books.google.com/books?id=ZXut4lprSTAC&dq
Grant, A. & Goodman, B., 2018. Communication and interpersonal skills in nursing. London: Learning Matters. https://books.google.com/books?id=6uN3DwAAQBAJ&dq
Grove, S. K., Burns, N. & Gray, J., 2012. The practice of nursing research: Appraisal, synthesis, and generation of evidence. Riverport Lane: Elsevier Health Sciences. https://books.google.com/books?id=r32jPNVYIacC&dq
Hareli, S. & Weiner, B., 2000. Accounts for success as determinants of perceived arrogance and modesty. Motivation and Emotion, 24(3), pp. 215-36. [DOI:10.1023/A:1005666212320]
Hogh, A., Baernholdt, M. & Clausen, T., 2018. Impact of workplace bullying on missed nursing care and quality of care in the eldercare sector. International Archives of Occupational and Environmental Health, 91(8), pp. 963-70. [DOI:10.1007/s00420-018-1337-0] [PMID]
Karaca, A. & Durna, Z., 2018. [Psychosocial support in epilepsy patient (Turkish)]. Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi, 7(1), pp. 218-25. https://atif.sobiad.com/index.jsp?modul=makale-detay&Alan=tip&Id=AWQ3Jh42HDbCZb_mQbJ6
Kelly, J., 2007. Barriers to achieving patient-centered care in Ireland. Dimensions of Critical Care Nursing, 26(1), pp. 29-34. [DOI:10.1097/00003465-200701000-00008] [PMID]
Kim, S., et al. 2017. Individual, interpersonal, and organisational factors of healthcare conflict: A scoping review. Journal of Interprofessional Care, 31(3), pp. 282-90. [DOI:10.1080/13561820.2016.1272558] [PMID]
McEwen, M. & Wills, E. M., 2018. Theoretical basis for nursing.Philadelphia PA: Wolters Kluwer. https://books.google.com/books?id=IfKQswEACAAJ&dq
Polit, D. F. & Beck, C. T., 2018. Essentials of nursing research: Appraising evidence for nursing practice. Philadelphia PA: Wolters Kluwer. https://books.google.com/books?id=Z6DwjwEACAAJ&dq
Rolfe, G., 2006. Nursing praxis and the science of the unique. Nursing Science Quarterly, 19(1), pp. 39-43. [DOI:10.1177/0894318405284128] [PMID]
Solman, B. & Clouston, T., 2016. Occupational therapy and the therapeutic use of self. British Journal of Occupational Therapy, 79(8), pp. 514-6. [DOI:10.1177/0308022616638675]
Strandås, M. & Bondas, T., 2018. The nurse-patient relationship as a story of health enhancement in community care: A meta‐ethnography. Journal of Advanced Nursing, 74(1), pp. 11-22. [DOI:10.1111/jan.13389] [PMID]
Watson, J., 2008. Assessing and measuring caring in nursing and health science. New York: Springer Publishing Company. https://books.google.com/books?id=7eAKbr-TqgEC&dq
Wiechula, R., et al. 2016. Umbrella review of the evidence: what factors influence the caring relationship between a nurse and patient? Journal of Advanced Nursing, 72(4), pp. 723-34. [DOI:10.1111/jan.12862] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2021/01/29 | Accepted: 2021/04/7 | Published: 2021/05/1
Received: 2021/01/29 | Accepted: 2021/04/7 | Published: 2021/05/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |