Wed, Jul 16, 2025
[Archive]
Volume 9, Issue 4 (Autumn 2023)
JCCNC 2023, 9(4): 255-266 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gheysari A, Farahaninia M, Hasanpoor-Azghady S B. Religious Coping and Health-promoting Lifestyle Among Iranian Infertile Women. JCCNC 2023; 9 (4) :255-266
URL: http://jccnc.iums.ac.ir/article-1-442-en.html
URL: http://jccnc.iums.ac.ir/article-1-442-en.html
1- Department of Community Health Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Midwifery and Reproductive Health, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,hasanpoorbatool@yahoo.com
2- Department of Midwifery and Reproductive Health, Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 690 kb]
(499 Downloads)
| Abstract (HTML) (1766 Views)
Health promotion is a process that improves people’s health and increases their control over it.
• In infertile women, the mean score of HPL was lower than the median score of the scale.
• Among the 5 dimensions of religious coping mechanisms, the highest mean score pertained to active religious coping, while the lowest means belonged to passive religious coping, followed by negative feelings towards God.
• A weak but significant inverse relationship was observed between negative feelings towards God and health-promoting lifestyle.
• A weak yet significant inverse relationship was observed between passive religious coping and interpersonal relations.
Plain Language Summary
Religion plays a crucial role in various aspects of some people’s lives. Religious coping, as well as religious beliefs and customs, can affect human well-being. Due to the physical, psychological, and financial consequences of infertility and its treatment process, infertile women may lack the motivation to enjoy a healthy lifestyle. However, religious coping can provide a new perspective by re-evaluating problems and giving these women hope. This study was conducted to determine the relationship between religious coping and health-promoting lifestyle. The results show that the health-promoting lifestyle in infertile women is lower than average. With the increase in negative feelings towards God, the health-promoting lifestyle and some of its dimensions, including physical activity, nutrition, and interpersonal relationships, decline. Also, with increased passive religious coping, interpersonal relationships decrease slightly.
• In infertile women, the mean score of HPL was lower than the median score of the scale.
• Among the 5 dimensions of religious coping mechanisms, the highest mean score pertained to active religious coping, while the lowest means belonged to passive religious coping, followed by negative feelings towards God.
• A weak but significant inverse relationship was observed between negative feelings towards God and health-promoting lifestyle.
• A weak yet significant inverse relationship was observed between passive religious coping and interpersonal relations.
Plain Language Summary
Religion plays a crucial role in various aspects of some people’s lives. Religious coping, as well as religious beliefs and customs, can affect human well-being. Due to the physical, psychological, and financial consequences of infertility and its treatment process, infertile women may lack the motivation to enjoy a healthy lifestyle. However, religious coping can provide a new perspective by re-evaluating problems and giving these women hope. This study was conducted to determine the relationship between religious coping and health-promoting lifestyle. The results show that the health-promoting lifestyle in infertile women is lower than average. With the increase in negative feelings towards God, the health-promoting lifestyle and some of its dimensions, including physical activity, nutrition, and interpersonal relationships, decline. Also, with increased passive religious coping, interpersonal relationships decrease slightly.
Full-Text: (385 Views)
1. Introduction
nfertility is recognized worldwide across all cultures as a stressful, critical, and threatening experience for individual, marital, family, and social stability (Inhorn & Patrizio, 2015; Nayebi Nia et al., 2018). Long-term treatment and medication programs, diagnostic processes, and planned sexual activities are examples of imposed stresses in infertile couples, potentially leading to psychological issues (Hasanpoor-Azghdy et al., 2014; Hadizadeh-Talasaz et al., 2020; Sohbati et al., 2021).
Infertility is defined as an inability to become pregnant despite having adequate and regular sexual intercourse for at least one year without using contraceptives. It is divided into primary and secondary infertility. In primary infertility, a couple is unable to initiate a pregnancy. In contrast, secondary infertility refers to the inability to achieve a pregnancy after one or more previous successful pregnancies (Berek, 2020).
The World Health Organization (WHO) has raised infertility as an essential reproductive health problem that causes emotional, psychological, and social disorders (Ombelet, 2011).
The rate of female infertility varies in different countries. In India, 8.9% of women of reproductive age have primary infertility (Katole & Saoji, 2019). In China, 24.58% of women suffer from infertility, 6.54% from primary infertility, and 18.04% from secondary infertility (Liang et al., 2021). It is estimated that 21%-22% of Iranian women have primary infertility (Saei Ghare Naz et al., 2020).
Despite the high prevalence of infertility, most women conceal their problems from family and friends. Infertility often becomes a silent struggle that can lead to losing control over life and reducing physical and mental health (Rooney & Domar, 2018). Giving birth and raising children are traditionally among the most prominent characteristics of the female gender role in developing societies, where a woman is complete only when she becomes a mother. This attitude leads to inequality between women and men and other gender-dependent consequences such as pain and suffering (Hasanpoor-Azghdy et al., 2015; Vitale et al., 2017). This suffering and pain affect women’s physical, mental, and social health (Pour, 2014), necessitating effective coping methods to control tension.
The psychological problems caused by infertility can contribute to the aggravation of infertility. On the other hand, people with peace of mind and good mental health experience less psychological pressure, potentially enhancing their fertility prospects (Domar et al., 2000).
Coping as a dynamic process involves cognitive and behavioral responses to reduce or resolve a crisis. Religion, too, can play a significant role in helping individuals cope with stressful events. Religious coping refers to encountering stressful situations in life armed with religious beliefs and doing religious practices (Pargament et al., 2005). Religious coping can have negative and positive aspects. Negative coping includes a negative evaluation of God as a punitive force coupled with anger and uncertainty regarding God’s ability. Positive coping includes challenging natural sciences’ explanations, seeking meaning, and redefining stressful situations as an opportunity for spiritual growth (Cooper et al., 2009; Corsini, 2009).
Health-promoting lifestyle (HPL) emerges as one of the best approaches people can employ to maintain and control their health (Haica, 2013; Psaros et al., 2012). Scientific evidence indicates that HPL increases the quality of life (Tol et al., 2013; Mak et al., 2018). An unhealthy lifestyle may have adverse consequences for fertility. Health behaviors that affect fertility may be the first important step in helping infertile people and increasing their chances of fertility (Haica, 2013). Religious coping is associated with health-related behaviors (Mehrabi et al., 2016).
It has been shown that religion may affect HPL components, including spiritual growth, health responsibility, physical activity, nutrition, interpersonal relations, and stress management. A qualitative study found that religious coping, grounded in a spiritual framework, helps deal with the emotional burden of infertility (Latifnejad et al., 2014). In another qualitative study, infertile women reported using religious coping to deal with negative feelings about infertility (Taghipour et al., 2020). Religion helps people see the positive side of a stressful situation. Religious people believe that a higher power controls their lives and consider adverse life events an opportunity for spiritual growth (Aflakseir & Mahdiyar, 2016). Religion as a great source of coping can make possible the grounds for the tendency to use health-oriented behavior (Amid et al., 2016). A systematic review study that examined people’s health behaviors and their level of religiosity showed that increasing the level of religiosity and spirituality in people leads to healthier behaviors.
These healthy behaviors include reducing smoking, increasing physical activity, improving diet, and overall health responsibility (Koenig, 2015). Increasing the level of religiosity and spirituality in pregnant women may reduce smoking (Jesse & Reed, 2004). Another study on Iranian pregnant women reports that positive religious coping has an inverse relationship with pregnant women’s anxiety, and increasing negative feelings towards God are associated with increased pregnancy anxiety (Mirzaee et al., 2022). Additionally, attending religious ceremonies, following religious traditions, and reading religious texts were predictors of health-related behaviors in pregnant Pennsylvania women (Cyphers et al., 2017).
Various religions emphasize individual responsibility for body care and nutrition. Religious teachings underscore abandoning behaviors that harm the body (Koenig, 2012). Regarding sports and religion, studies have shown a significant positive relationship between religion and physical activity (Baetz & Bowen, 2008; Koenig, 2012). The findings of other studies have shown an inverse relationship between religion/spirituality and high-risk sexual activity (Cochran et al., 2004; Burdette et al., 2009). Religiosity affects health indirectly through the health-oriented lifestyle variable (Serajzadeh et al., 2013). Religion as an excellent source of coping lays the groundwork for adopting health-oriented behaviors (Amid et al., 2016).
Religion holds a unique position in Iranian society, influencing various dimensions of people’s lives, especially in crises (Saeidi Taheri et al., 2013). Considering the high prevalence of infertility in Iran and its related treatment demands and sometimes unsuccessful, as well as the psychological consequences following treatment processes, the present study was conducted to investigate the dimensions of religious coping and HPL in infertile women and determine the relationship between these two variables.
2. Materials and Methods
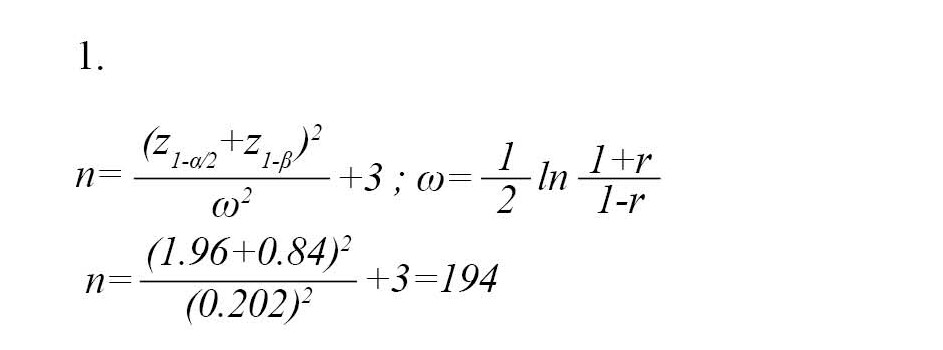
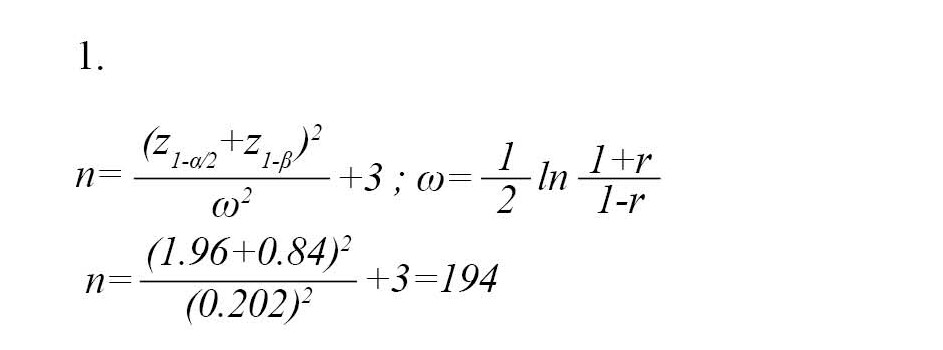
This cross-sectional correlational study was performed on 177 infertile women referring to the Sarem Sub-specialized Infertility Treatment and Research Center in Tehran City, Iran. This center is one of the most well-equipped infertility centers in Tehran. The average number of people visiting this center for the first visit is 8000 infertile couples from different parts of Iran annually. The subjects were recruited by census method from May to December 2019. The sample size was estimated through the Equation 1 to be 194 by considering the 95% CI, the test power of 80%, and the Pearson correlation coefficient of 0.2 between religious coping and HPL.
Due to the incompleteness of 17 questionnaires, 177 samples were included in the study.
The inclusion criteria were as follows: Women aged 15 to 49 (Gar-elnabi et al., 2020; Berlie & Alamerew, 2018), having reading and writing literacy, being in the first marriage, not using specific medications for mental disorders, lacking a history of mental illness based on the individual report, being a Muslim, having primary or secondary infertility approved by an obstetrician, undergoing infertility treatment for at least one year, lacking a living child in case of secondary infertility or an adopted child. The exclusion criterion was the failure to complete the questionnaire.
The study data were collected using a general information questionnaire, the Iranian religious coping scale (IRCS), and health-promoting lifestyle profile-II (HPLP-II). The available information questionnaire consisted of two parts. The first was demographic information, including age, education, occupation, and marriage duration. The second part focused on the characteristics of infertility, including infertility duration, current treatment, number of previous treatments, and the reason for requesting the treatment (personal desire, spouse insistence, family pressure).
The IRCS is a scale designed to assess Muslim religious coping. Aflakseir & Coleman (2011) developed the IRCS based on brief religious coping (brief RCOPE) (Pargament et al., 2000). The 14-item brief RCOPE measure is a widely used religious coping scale in different studies. It has positive and negative dimensions. Positive religious coping reflects a secure relationship with a transcendent power, a sense of spiritual connection with others, and a benevolent worldview. Negative religious coping reflects spiritual tensions and struggles within oneself, others, and God. Aflakseir and Coleman developed the IRCS with some items adapted from Brief RCOPE (Pargament et al., 2000) and reformulated it to apply Muslim religious beliefs. In addition, new items were added reflecting Islamic religious beliefs (e.g. “viewed my situation as a trial from God”). Since religious practices play an essential role in the Islamic faith, some Muslim practice-related items were included in this scale (e.g. “attended pilgrimage when I felt upset”). Those religious activities were selected that, based on interviews and pilot studies, Muslims often use to deal with stressful life events. In this way, after construct validity, IRCS consisted of 22 items categorized into 5 dimensions.
1. The practice of religious coping (6 items): A set of religious behaviors and actions (such as going to the mosque, reading the Quran, etc.) that a person performs when faced with stressful life events (e.g. seeking comfort and guidance by reading the Quran).
2. Benevolent reappraisal (6 items): The feelings and thoughts a person uses when faced with stressful situations to get closer to God and create peace (e.g. viewed my situation as a test from God).
3. Negative feelings toward God (4 items): Mental and spiritual tension and contradictions that a person shows about himself, others, and God (e.g. I expressed anger at God for letting this problem happen).
4. Passive religious coping (3 items): When a person does not try to solve the problem and stressful situation and considers the situation to be the result of God’s will (e.g. was destined to have this situation, so I didn’t try to change it).
5. Active religious coping (3 items): When a person puts his/her effort and energy into solving stressful situations and leaves the results of his actions in the hands of God (e.g. did what I could and turned the rest over to God).
The IRCS employs a 5-point Likert scale, ranging from 0 (not at all) to 4 (a great deal). This questionnaire does not have a total score. High scores on each dimension indicate high religious coping in that dimension. The Cronbach α of 0.89 was found acceptable for practice, 0.79 for benevolent reappraisal, 0.79 for negative feelings toward God, and 0.72 and 0.79 for passive and active religious coping, respectively (Aflakseir & Coleman, 2011).
We used IRCS in this study because the followers of monotheism, like Judaism, Christianity, and Islam, have fundamental beliefs about God and eternity. However, each religion has its own beliefs and practices to cope with particular situations. These beliefs and practices are not included in general questionnaires, the most widely used of which is the religious coping questionnaire by Pargament and colleagues. Therefore, in the present study, IRCS, which is sensitive to the beliefs and practices of Muslims, has been used.
The health-promoting lifestyle profile-II (HPLP-II) is a revised version of the HPLP developed by Walker et al. (1987). This scale consists of 52 items and 6 subscales: Spiritual growth (9 items), health responsibility (9 items), physical activity (8 items), nutrition (9 items), interpersonal relations (9 items), and stress management (8 items). The items are rated on a 4-point Likert scale ranging from 1 (never) to 4 (routinely). Walker and colleagues reported high internal consistency for the overall measure (α=0.94) and the subscales (from 0.79 to 0.87). Its 3-week test re-test stability coefficient was 0.89. A higher score indicates better health behavior Walker et al. (1987). Zeidi and colleagues confirmed the reliability and validity of the Persian version of this questionnaire. They have reported high internal consistency for the overall measure (α=0.82) and its subscales (from 0.64 to 0.91). Its 2-week test re-test stability coefficient was r=0.91 (Mohammadi Zeidi et al., 2012). The present study obtained internal consistency for the overall measure (α=0.84) and the subscales (from 0.71 to 0.89).
The data were described using frequency, Mean±SD and analyzed using the independent t-test, one-way ANOVA, and Pearson correlation coefficient in SPSS software, version 22. The significance level for all tests was set at P<0.05.
3. Results
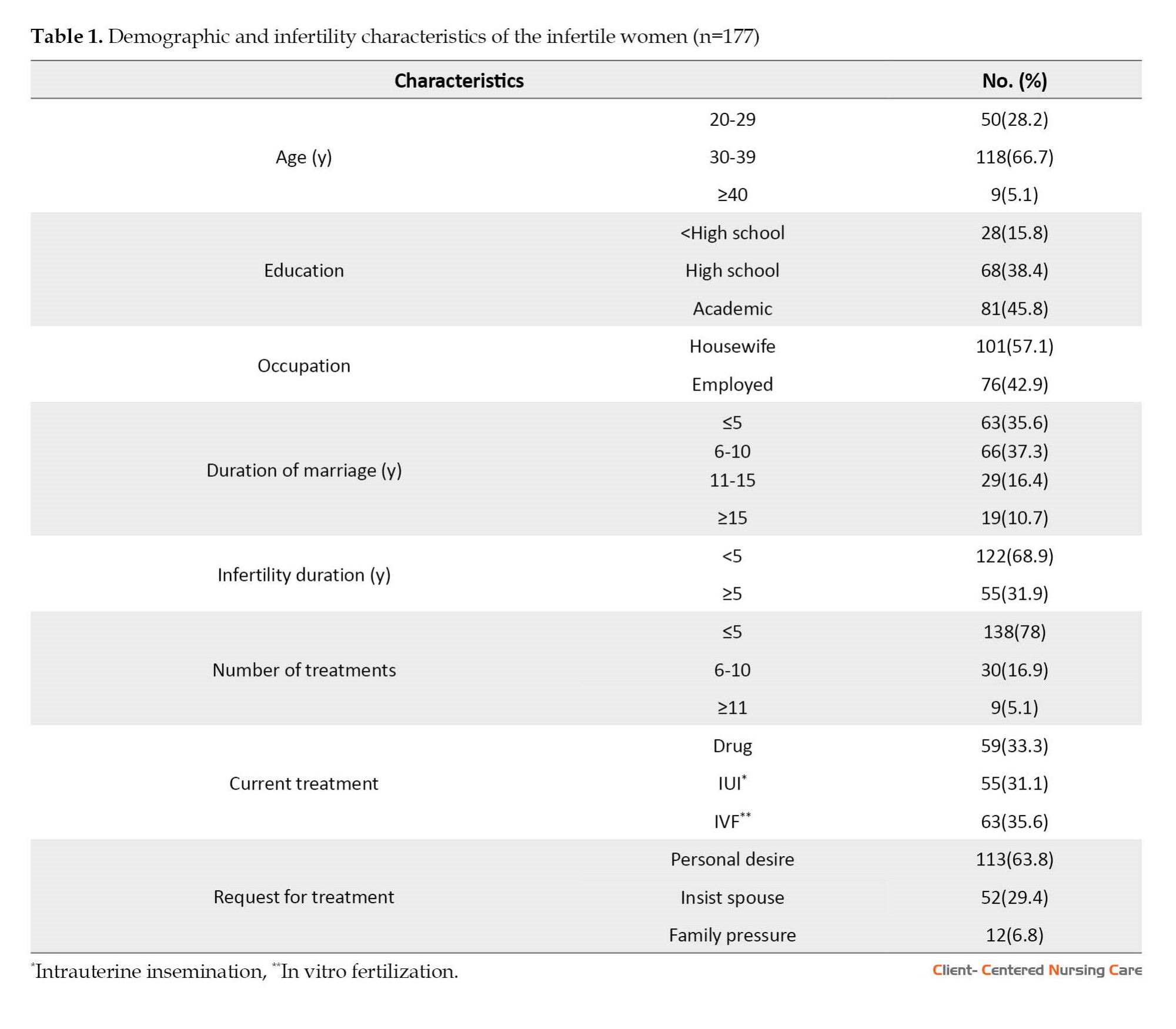
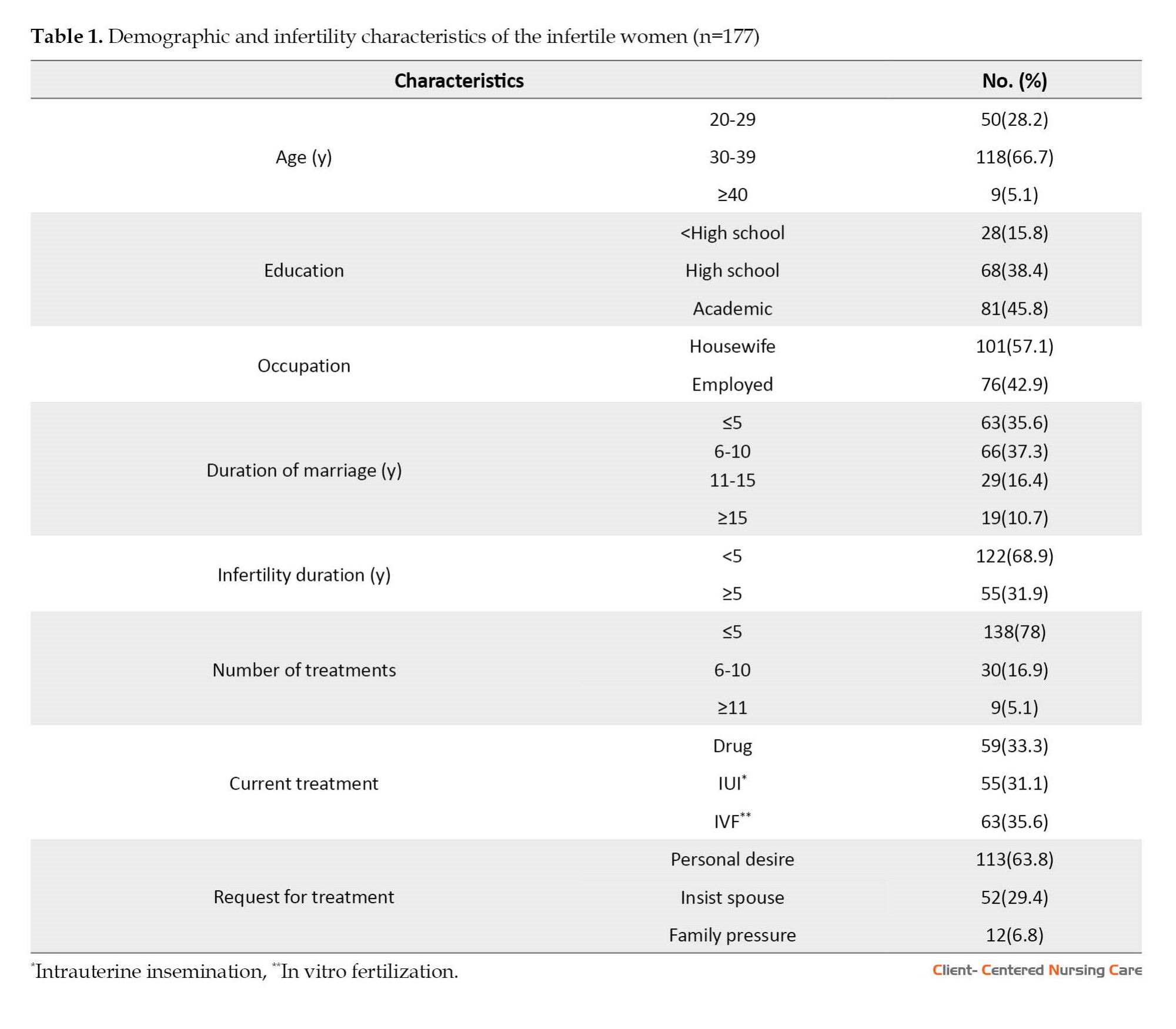
The Mean±SD age of the subjects was 34.25±5.51 years. Their Mean±SD marriage duration was 7.48±4.62 years, and the Mean±SD infertility duration was 5.27±3.68 years with a range of 1-13 years. More information about the demographic and fertility characteristics of the subjects is presented in Table 1.
To compare the mean dimensions of religious coping and HPL variables, the means were calculated based on 0 to 100 in Table 2.
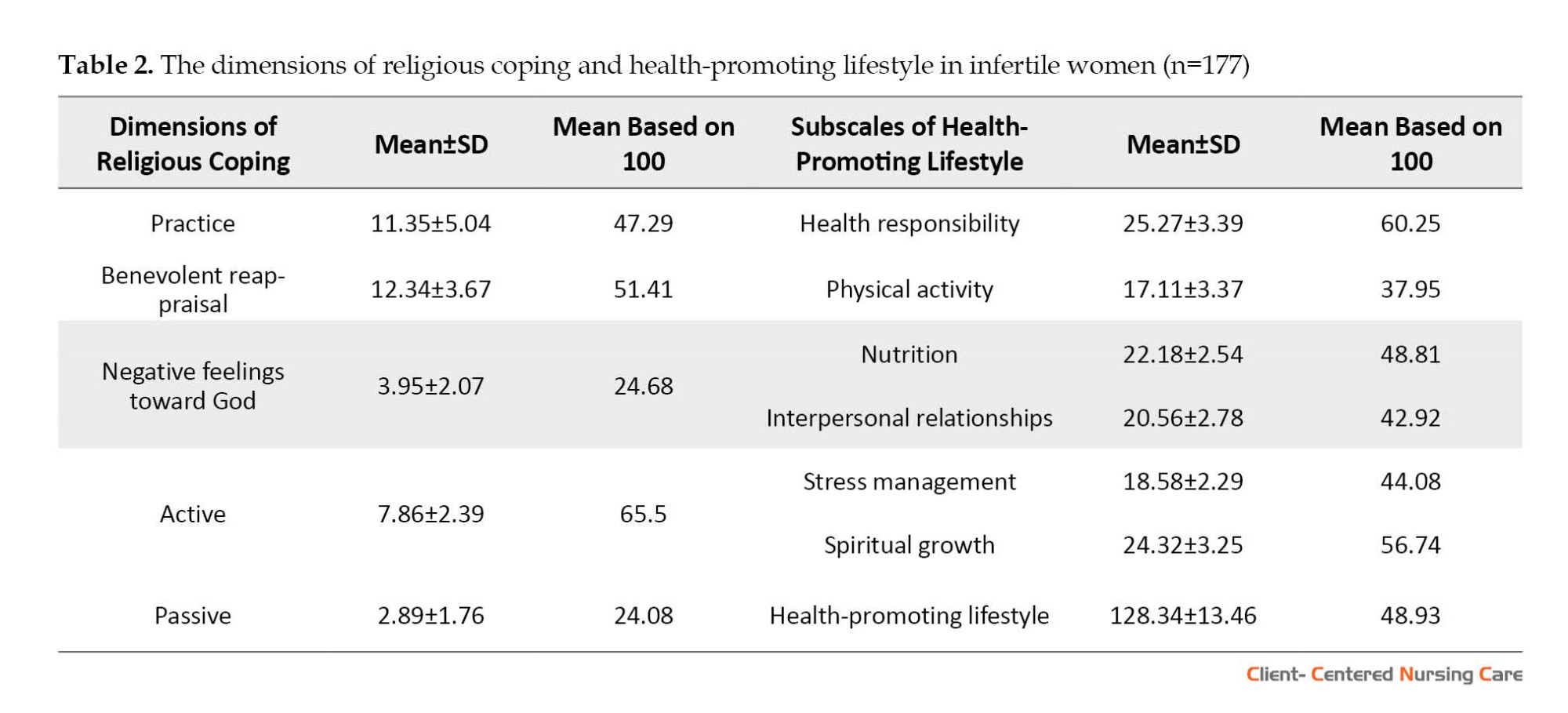
Table 3 details the relationship between religious coping with demographics and infertility characteristics of the subjects. Due to the wealth of the information, only significant items have been displayed.
Table 3 demonstrates a significant relationship between age, religious practice, and benevolent reappraisal. A two-by-two Tukey comparison showed that the mean score of religious practices of infertile women aged 30-39 years (P<0.001) and ≥40 years (P=0.016) was higher than that of women aged 20-29. Tukey’s two-by-two comparison also showed that the mean benevolent reappraisal score of infertile women aged 30-39 years (P=0.013) and ≥40 years (P=0.001) was higher than that of women aged 20-29.
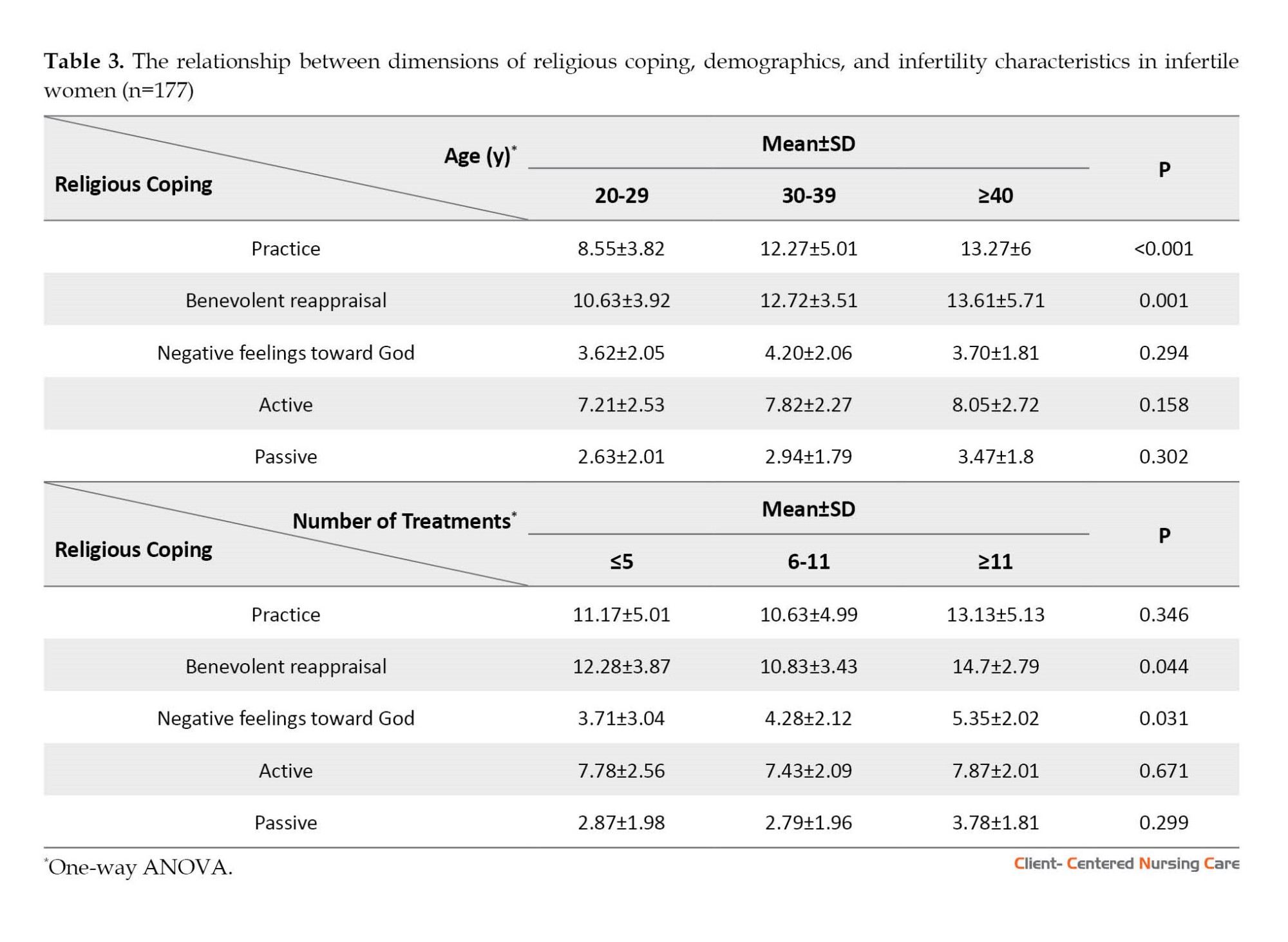
Table 3 also shows that benevolent reappraisal and negative feelings toward God significantly related to the number of infertility treatments. Tukey’s two-by-two comparison showed that the mean benevolent reappraisal score of infertile women with ≥11 times of treatment was higher than that of women with 6-11 times of treatment (P=0.046). Tukey’s two-by-two comparison also showed that the mean score of negative feelings towards God in infertile women with ≥11 treatment times was higher than that of women with ≤5 times (P=0.029). No significant relationship was found between HPL, demographics, and fertility characteristics in infertile women.
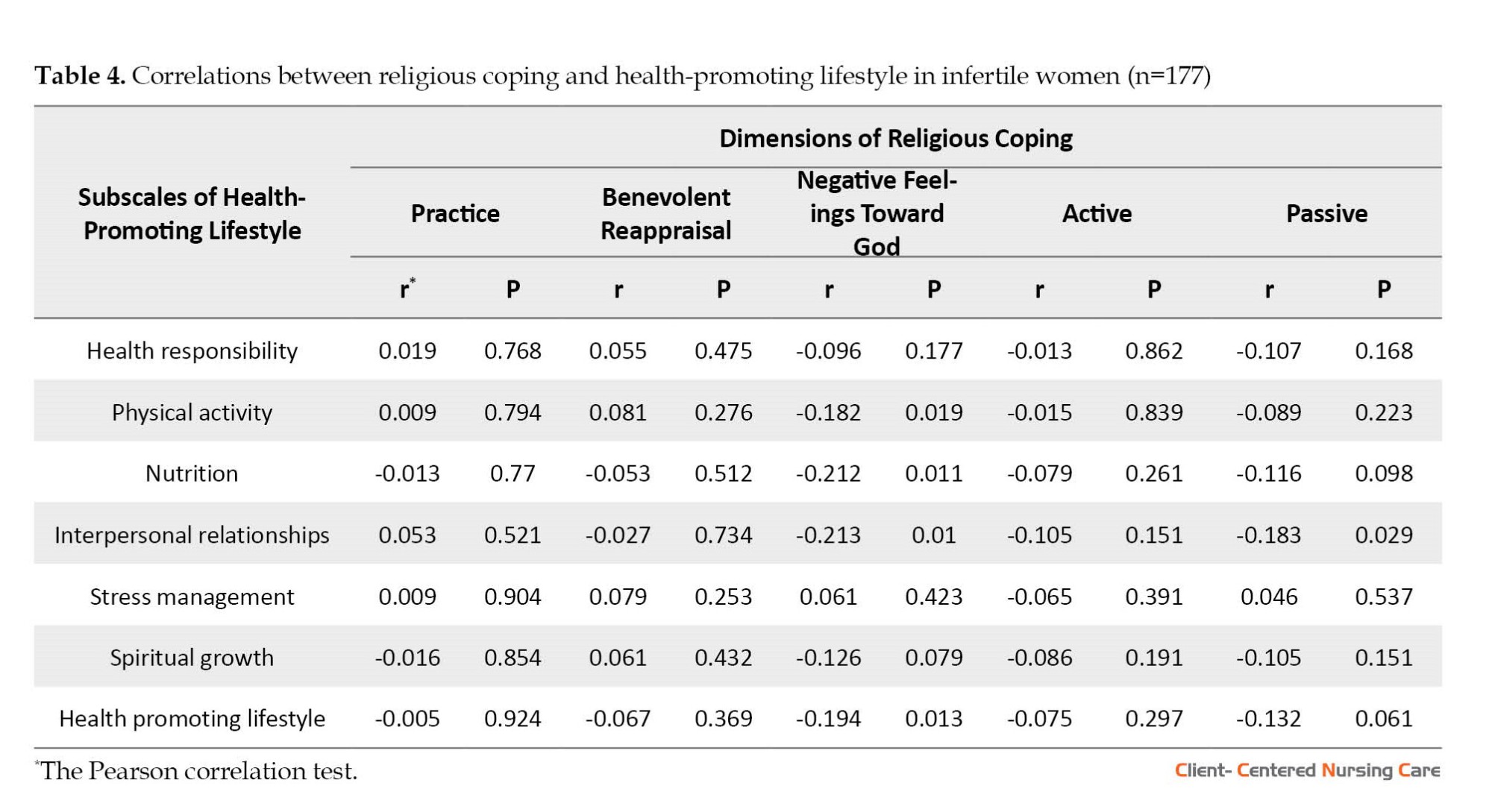
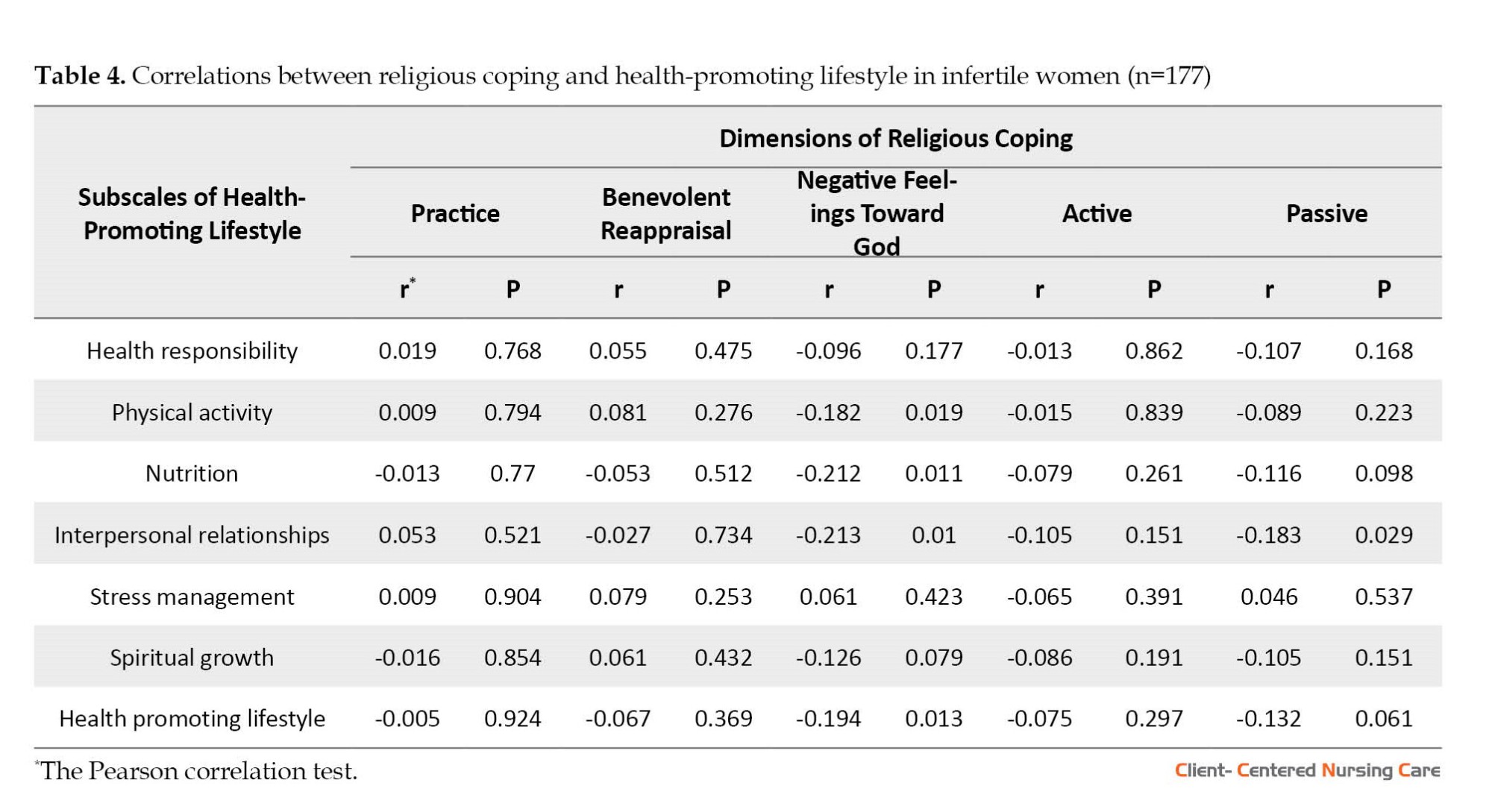
Table 4 presents the relationship between religious coping dimensions and HPL subscales.
Table 4 shows a weak yet significant inverse relationship between negative feelings toward God and health-promoting lifestyle and its 3 subscales: Physical activity, nutrition, and interpersonal relationships. Also, there is a weak but significant inverse association between passive religious coping and interpersonal relations.
4. Discussion
This study explored the relationship between religious coping and HPL in Iranian infertile women. According to the results, active religious coping had the highest mean score among various dimensions of religious coping, and negative feelings towards God and passive religious coping had the lowest mean scores. In line with our study, Aflakseir and Mahdiyar (2016) showed that the highest mean score was the practice and active religious coping in Iranian infertile women. The lowest was related to passive and negative coping. Another RCOPE scale study affirmed that the mean score of positive religious coping was higher than that of negative religious coping in infertile couples (Ghafouri et al., 2016).
In a study that measured the religious coping of infertile couples using the RCOPE scale, the mean score of positive religious coping of the women was higher than the median of the scale. The negative religious coping was lower than the scale median (Momenyan et al., 2020). In line with these results, in our study, the mean scores of benevolent reappraisal and active religious coping were higher than the scale median, and the mean score of negative feelings towards God was lower. Lopez and colleagues investigated the religious commitment of couples using the religious commitment inventory-10, whose items are similar to the items of active religious coping and benevolent evaluation of the tool used in the present study. It was found that the couples’ mean score of religious commitment was higher than the median of the tool (Lopez et al., 2011). In the present study, the mean scores obtained in the dimensions of active religious coping and the benevolent reappraisal of the infertile women were higher than the median of the related dimensions. Our study found that the mean score of infertile women’s HPL was lower than the median of the scale. Also, the health responsibility subscale had the highest mean score, and the physical activity subscale had the lowest mean score.
Mirghafourvand et al. (2017) examined the HPL of women with polycystic ovary syndrome (PCOS). More than 70% of its married subjects were infertile. They reported that the mean score of the total HPL was lower than the median value of the scale. The subscales of nutrition and then health responsibility had the highest mean scores, and stress management and physical activity had the lowest mean scores. The reason for the high average nutrition score is probably the complications of obesity (nearly 50% of the samples studied by Mirghforvand et al. had a body mass index ≥30) because women with PCOS usually try to lose weight with appropriate nutritional methods. Also, the reason for the low average score of stress management is probably due to the widespread complications of hyperandrogenism, such as hirsutism, alopecia, and acne, along with infertility and obesity, which reduce stress management in women with PCOS.
In a study to evaluate HPL and its related factors in 1200 Iranian women of reproductive age, the results showed that health responsibility had the highest, and physical activity had the lowest mean score (Abedi et al., 2017), which was similar to the results of our study. However, the mean scores of spiritual growth and health responsibility of our study subjects were lower, and the mean scores of stress management, nutrition, and physical activity of our study subjects were higher than those of the mentioned study. These differences may be due to the nature of the infertility problem and its treatment processes. Many women are challenged with infertility. Most infertile women struggle with this life event and use coping strategies, including developing flexibility and maintaining or gaining hope to deal with it and endure suffering (Romeiro et al., 2017). A qualitative study on religion and infertility reported “spiritual growth versus challenging one’s spiritual beliefs” as one of the main themes. Thus, infertility sometimes leads to spiritual growth and occasionally challenges one’s spiritual beliefs related to one’s understanding of God and sense of connection with God (Hasanpoor Azghdy et al., 2019). Regarding stress management, nutrition, and physical activity, infertile women, due to the nature of infertility, face social pressure and tension caused by the treatment process, so they may have better stress management than other women to improve their quality of life. Also, because of the treatment team’s advice to help the infertility treatment, they seek healthier nutrition and more physical activity (to lose weight) than other women. In confirmation of the findings of the present study, in most studies on HPL in Iran, where the study population was women of different ages or with conditions such as pregnancy and infertility, the lowest average has been related to physical activity (Mirghafourvand et al., 2017; Abedi et al., 2017; Rabiepoor et al., 2019). The results of a qualitative study in Iran have considered religious attitudes as one of the reasons for a decrease in the physical activity of women in Iranian society, which causes women not to be physically active in open spaces such as parks due to the presence of men (Amiri Farahani et al., 2018).
Our study found that no significant relationship was seen between practice, active religious coping, and benevolent reappraisal with HPL and its subscales among the dimensions of religious coping. However, with increasing negative religious coping in infertile women, HPL and its subscales, including physical activity, nutrition, and interpersonal relations, were decreased. Also, with increasing passive religious coping, interpersonal relationships decreased. Consistent with the present study, the findings of McKenzie et al. (2015) on black Canadians revealed a very weak relationship between religious involvement and health-related behaviors. They showed that this relationship is not an independent predictor of lifestyle practices. The results of a study on older adults also revealed no statistically significant correlation between religious orientation and HPL (Bakhtiari et al., 2019).
In the current study, a weak but significant inverse relation was observed between negative feelings towards God and the subscale of physical activity, which shows that the lower the negative feeling towards God, the higher the physical activity. The results of a study on Iranian pregnant women also show that with the increase in spiritual growth, the subjects’ physical activity increases (Rabiepoor et al., 2019). Another study on 1596 Danish men and women found that religiosity had a significant positive relationship with a healthier lifestyle, especially for those religiously educated by their parents (Herold et al., 2020). The findings of a study on 176 Malaysian Muslim men and women showed a strong relationship between religious performances and health-related behaviors (Hassan, 2015). The difference between the results of the mentioned studies and the present study’s findings may be related to the differences in the research community, the scale for measuring religious coping, the subjects’ religious beliefs, sample size, and cultural context.
In the present study, older infertile women performed more religious practices to deal with the stress caused by infertility and used benevolent reappraisal more than other age groups. Also, as the number of infertility treatments increased, benevolent reappraisal and negative feelings toward God increased. Consistent with the results of our study, a research study on religious coping of Ghanaian women with infertility showed that with increasing age, positive religious coping strategies such as benevolent reappraisal and focusing on religious practices increase. The same study also reported that as the duration of infertility and the number of treatments increased, infertile women developed negative feelings toward God, although this relationship was weak (Oti-Boadi & Oppong Asante, 2017).
A qualitative study also reported that successive treatment failures were associated with benevolent reappraisal in infertile women. However, religion has some challenges and developed negative feelings towards God (Hasanpoor Azghdy et al., 2019).
The study subjects completed the scales of the current research by the self-report method, which has specific limitations. Due to the study’s cross-sectional nature, the findings should be used cautiously. However, the results could be generalized to similar contexts.
5. Conclusion
The present study showed a weak yet significant inverse relationship between some dimensions of religious coping with HPL and some of its subscales. In other words, infertile women who had less negative feelings towards God and used less passive coping had relatively better HPL. Therefore, strengthening positive feelings towards God can be beneficial to some extent to improve the HPL of these women. However, enhancing HPL through educational interventions would be helpful. For this reason, it is suggested first to prepare the necessary coordination for designing an educational program through a mixed-method study, then evaluate the effectiveness of this educational program using interventional studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC. 1397.1006). The research aims and the confidentiality of the data were explained, and written informed consent was obtained from participants.
Funding
This study was extracted from master's thesis of Amin Gheysari, approved by the Department of Community Health Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences.
Authors' contributions
Data collection: Amin Gheysari; Writing and revising the manuscript: Amin Gheysari and Seyedeh Batool Hasanpoor-Azghady; Study design, data analysis, interpretation, and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the studied women who participated in the research and the subspecialty Center for Infertility Treatment and Research of Sarem for their cooperation in this study.
References
Abedi, P., Jorfi, M. & Afshari, P., 2017. [Evaluation of the health promotion lifestyle and its related factors in reproductive aged women in Ahvaz, Iran (Persian)]. Community Health Journal, 9(1), PP. 68-74. [Link]
Aflakseir, A. & Coleman, P .G., 2011. Initial development of the Iranian religious coping scale. Journal of Muslim Mental Health, 6(1), pp. 44-61. [DOI:10.3998/jmmh.10381607.0006.104]
Aflakseir, A. & Mahdiyar, M., 2016. The role of religious coping strategies in predicting depression among a sample of women with fertility problems in Shiraz. Journal of Reproduction & Infertility, 17(2), pp. 117–22. [PMID]
Amid, M., Shokri, O. & Zarani, F., (2016). [Casual relations model of antecedents and consequences of health behaviours in university students (Persian)]. Journal of Research in Psychological Health. 10, 70-8. [DOI:10.18869/acadpub.rph.10.3.70]
Amiri Farahani, L., Hasanpoor-Azgahdy, S. B. & Taghizadeh, Z., 2018. Iranian women’s perceptions and experiences of barriers to and facilitators of physical activity. Shiraz E-Medical Journal, 19(8), pp. e65287. [DOI:10.5812/semj.65287]
Bakhtiari, A., et al., 2019. Does religion predict health-promoting behaviors in community-dwelling elderly people? Journal of Religion and Health, 58(2), pp. 452-64. [DOI:10.1007/s10943-018-0710-3] [PMID]
Baetz, M. & Bowen, R., 2008. Chronic pain and fatigue: Associations with religion and spirituality. Pain Research and Management, 13(5), pp. 3838 [DOI:10.1155/2008/263751.] [PMID]
Berek, J.S. (2020). Berek & Novak’s gynecology essentials. Groningen :Wolters Kluwer. [Link]
Berlie, A.B. & Alamerew, Y. T., 2018. Determinants of fertility rate among reproductive age women (15-49) in Gonji-Kollela District of the Amhara National Regional State, Ethiopia. Ethiopian Journal of Health Development, 32(3), pp. 1-12. [Link]
Burdette, A. M., et al., (2009). “Hooking up” at college: Does religion make a difference? Journal for the Scientific Study of Religion, 48(3), pp. 535-51. [DOI:10.1111/j.1468-5906.2009.01464.x]
Cochran, J. K., et al., 2004. Religion, religiosity, and nonmarital sexual conduct: An application of reference group theory. Sociological Inquiry, 74(1), pp. 101-27. [Link]
Cooper, L. B., et al., 2009. Differentiated styles of attachment to God and varying religious coping efforts. Journal of Psychology and Theology, 37(2), pp. 134-41. [DOI:10.1177/009164710903700205]
Corsini, K. D., 2009. Examining the relationship between religious coping strategies, attachment beliefs and emotion regulation in a mixed sample of college students attending an evangelical university in central Virginia [PhD dissertation]. Virginia: Liberty University. [Link]
Cyphers, N. A., Clements, A. D. & Lindseth, G., 2017. The relationship between religiosity and health-promoting behaviors in pregnant women. Western Journal of Nursing Research, 39(11), pp. 1429–46. [DOI:10.1177/0193945916679623] [PMID]
Domar, A. D., et al., 2000. Impact of group psychological interventions on pregnancy rates in infertile women. Fertility and Sterility, 73(4), pp. 805-11. [PMID]
Gar-elnabi, M. E. M., et al., 2020. Assessment of infertility factors and their relative impact in pregnancy using ultrasonography & hormonal checkup. Journal of Science and Science Education, 1(1), pp. 30-4 [DOI:10.29303/jossed.v1i1.476]
Ghafouri, S. F., et al., 2016. The relation between marital adjustment and posttraumatic growth in infertile couples: The mediatory role of religious coping strategies. Journal of Reproduction & Infertility, 17(4), pp. 221-9. [PMID]
Hadizadeh-Talasaz, F., et al., 2020. Exploring infertile couples’ decisions to disclose donor conception to the future child. International Journal of Fertility & Sterility, 14(3), pp. 240-6. [DOI:10.22074/ijfs.2020.44408] [PMID]
Haica, C. C., 2013. Gender differences in quality of life, intensity of dysfunctional attitudes, unconditional self-acceptance, emotional distress and dyadic adjustment of infertile couples. Procedia-Social and Behavioral Sciences, 78, pp. 506-10. [DOI:10.1016/j.sbspro.2013.04.340]
Hasanpoor-Azghady, S. B., et al., 2019. The social construction of infertility among Iranian infertile women: A qualitative study. Journal of Reproduction & Infertility, 20(3), pp. 178-90. [PMID]
Hasanpoor-Azghdy, S. B., Simbar, M. & Vedadhir, A., 2014. The emotional-psychological consequences of infertility among infertile women seeking treatment: Results of a qualitative study. Iranian Journal of Reproductive Medicine, 12(2), pp. 131-8. [PMID]
Hasanpoor-Azghdy, S. B., Simbar, M. & Vedadhir, A., 2015. The social consequences of infertility among Iranian women: A qualitative study. International Journal of Fertility & Sterility, 8(4), pp. 409-20. [DOI:10.22074/ijfs.2015.4181] [PMID]
Hassan, S. H., 2015. Effects of religious behavior on health-related lifestyles of Muslims in Malaysia. Journal of Religion and Health, 54(4), pp. 1238–48. [DOI:10.1007/s10943-014-9861-z] [PMID]
Herold, S.C., et al., 2022. Is religiousness associated with better lifestyle and health among Danes? Findings from SHARE. Journal of Religion and Health, 61(2), pp. 1621–40. [DOI:10.1007/s10943-020-01050-3] [PMID]
Inhorn, M.C. & Patrizio, P., 2015. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Human Reproduction Update, 21(4), pp. 411–26. [DOI:10.1093/humupd/dmv016] [PMID]
Jesse, D. E. & Reed, P. G., 2004. Effects of spirituality and psychosocial well-being on health risk behaviors in Appalachian pregnant women. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 33(6), pp. 739–47. [DOI:10.1177/0884217504270669] [PMID]
Katole, A. & Saoji, A. V., 2019. Prevalence of primary infertility and its associated risk factors in urban population of central India: A community-based cross-sectional study. Indian Journal of Community Medicine, 44(4), pp. 337–41. [DOI:10.4103/ijcm.IJCM_7_19] [PMID]
Koenig, H. G., 2015. Religion, spirituality, and health: A review and update. Advances in Mind-Body Medicine, 29(3), pp. 19–26. [PMID]
Koenig, H. G., 2012. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry, 2012, pp. 278730. [DOI:10.5402/2012/278730] [PMID]
Latifnejad Roudsari, R., Allan, H. T. & Smith, P.A., 2014. Iranian and English women’s use of religion and spirituality as resources for coping with infertility. Human Fertility, 17(2), pp. 114–23. [DOI:10.3109/14647273.2014.909610] [PMID]
Liang, S., et al., 2021. Prevalence and associated factors of infertility among 20-49-year-old women in Henan Province, China. Reproductive Health, 18(1), pp. 254. [DOI:10.1186/s12978-021-01298-2] [PMID]
Lopez, J. L., et al., 2011. Religious commitment, adult attachment, and marital adjustment in newly married couples. Journal of Family Psychology, 25(2), pp. 301–9. [DOI:10.1037/a0022943] [PMID]
Mak, Y. W., et al., 2018. Health-promoting lifestyle and quality of life among Chinese nursing students. Primary Health Care Research & Development, 19(6), pp. 629-36. [DOI:10.1017/S1463423618000208] [PMID]
McKenzie, M. M., et al., 2015. Religious involvement and health-related behaviors among Black Seventh-Day Adventists in Canada. Health Promotion Practice, 16(2), pp. 264–70.[DOI:10.1177/1524839914532812] [PMID]
Mehrabi, E., et al., 2016. [Religion, spirituality and coping with breast cancer: A phenomenological study (Persian)]. Journal of Reaserch on Religion & Health, 2(2), pp. 12-23. [Link]
Mirghafourvand, M., Mohammad-Alizadeh Charandabi, S. & Aliasghari, F., 2017. [Assessment of health promoting lifestyle status and its socio-demographic predictors in women with polycystic ovarian syndrome (Persian)]. Hayat, 22(4), pp. 394-407. [Link]
Mirzaee, F., Hasanpoor-Azghady, S. B. & Amiri-Farahani, L., 2022. Correlation between religious coping, demographic and fertility factors, and pregnancy anxiety of Iranian primiparous women: A cross-sectional study. BMC Psychiatry, 22(1), pp. 298. [DOI:10.1186/s12888-022-03922-2] [PMID]
Mohammadi Zeidi, I., Pakpour Hajiagha, A. & Mohammadi Zeidi, B., 2011. [Reliability and validity of Persian version of the health-promoting lifestyle profile (Persian)]. Journal of Mazandaran University of Medical Sciences, 20(1), pp. 102-13. [Link]
Momenyan, S., et al., 2020. [The relationship between religious coping and quality of life in infertile couples (Persian)]. Iranian Journal of Nursing Research, 15(3), pp. 47-55. [Link]
Nayebi Nia, A. S., et al., 2018. [Domestic violence and its association with domains of reproductive health in women: A systematic review (Persian)]. Journal of Mazandaran University of Medical Sciences, 27(158), pp. 205-17. [Link]
Ombelet, W., 2011. Global access to infertility care in developing countries: A case of human rights, equity and social justice. Facts, Views & Vision in ObGyn, 3(4), pp. 257–66. [PMID]
Oti-Boadi, M. & Oppong Asante, K., 2017. Psychological health and religious coping of Ghanaian women with infertility. BioPsychoSocial Medicine, 11, pp. 20. [DOI:10.1186/s13030-017-0105-9] [PMID]
Pargament, K.I., Koenig, H. G. & Perez, L. M., 2000. The many methods of religious coping: Development and initial validation of the RCOPE. Journal of Clinical Psychology, 56(4), pp. 519-43. [PMID]
Pargament, K. I., Magyar-Russell, G. M. & Murray-Swank, N. A., 2005. The sacred and the search for significance: Religion as a unique process. Journal of Social Issues, 61(4), pp. 665-87. [DOI:10.1111/j.1540-4560.2005.00426.x]
Pour, T. H., 2014. The effect of cognitive behavioural therapy on anxiety in infertile women. European Journal of Experimental Biology, 4(1), pp. 415-9. [Link]
Psaros, C., et al., 2012. A brief report of depressive symptoms and health promoting behaviors among women with infertility attending a clinical mind-body program. Journal of Psychosomatic Obstetrics & Gynecology, 33(1), pp. 32–6. [DOI:10.3109/0167482X.2011.643933] [PMID]
Rabiepoor, S., Sadeghi, E. & Sayyadi, H., 2019. Spiritual health and physical activity among Iranian pregnant women. Journal of Religion and Health, 58(2), pp. 506–15. [DOI:10.1007/s10943-017-0487-9] [PMID]
Romeiro, J., et al., 2017. Spiritual aspects of living with infertility: A synthesis of qualitative studies. Journal of Clinical Nursing, 26(23-24), pp. 391735. [DOI:10.1111/jocn.13813] [PMID]
Rooney, K. L. & Domar, A. D., 2018. The relationship between stress and infertility. Dialogues in Clinical Neuroscience, 20(1), pp. 41–7. [DOI:10.31887/DCNS.2018.20.1/klrooney] [PMID]
Saeedi Taheri, Z., Asadzandi, M., & Ebadi, A. (2013). [The effect of spiritual care based on general sediment model on the spiritual experiences of patients with coronary artery disease (Persian)]. Nursing Psychology Journal, 1, pp. 45-53. [Link]
Saei Ghare Naz, M., Ozgoli, G. & Sayehmiri, K., 2020. Prevalence of infertility in Iran: A systematic review and meta-analysis. Urology Journal, 17(4), pp. 338–45. [DOI:10.22037/uj.v0i0.5610] [PMID]
Serajzadeh, S. H., Javaheri, F. & Velayati Khajeh, S., 2013. [Religion and health: An examination of the effect of religiosity on health in a sample of university students (Persian)]. Journal of Applied Sociology, 24(1), pp. 55-77. [Link]
Sohbati, F., et al., 2021. Psychological well-being of infertile women and its relationship with demographic factors and fertility history: A cross-sectional study. BMC Women’s Health, 21(1), pp. 22. [DOI:10.1186/s12905-020-01167-3] [PMID]
Taghipour, A., et al., 2020. Coping strategies of women following the diagnosis of infertility in their spouses: A qualitative study. Evidence Based Care, 10(1), pp. 15-24. [DOI:10.22038/EBCJ.2020.42136.2120]
Tol, A., et al., 2013. Health-promoting lifestyle and quality of life among undergraduate students at school of health, Isfahan university of medical sciences. Journal of Education and Health Promotion, 2, pp. 11. [DOI:10.4103/2277-9531.108006] [PMID]
Vitale, S. G., et al., 2017. Psychology of infertility and assisted reproductive treatment: The Italian situation. Journal of Psychosomatic Obstetrics & Gynecology, 38(1), pp. 1-3. [DOI:10.1080/0167482X.2016.1244184] [PMID]
Walker, S. N., Sechrist, K. R. & Pender, N. J., 1987. The health promoting lifestyle profile: Development and psychometric characteristics. Nursing Research, 36(2), pp. 76–81.[DOI:10.1097/00006199-198703000-00002] [PMID]
nfertility is recognized worldwide across all cultures as a stressful, critical, and threatening experience for individual, marital, family, and social stability (Inhorn & Patrizio, 2015; Nayebi Nia et al., 2018). Long-term treatment and medication programs, diagnostic processes, and planned sexual activities are examples of imposed stresses in infertile couples, potentially leading to psychological issues (Hasanpoor-Azghdy et al., 2014; Hadizadeh-Talasaz et al., 2020; Sohbati et al., 2021).
Infertility is defined as an inability to become pregnant despite having adequate and regular sexual intercourse for at least one year without using contraceptives. It is divided into primary and secondary infertility. In primary infertility, a couple is unable to initiate a pregnancy. In contrast, secondary infertility refers to the inability to achieve a pregnancy after one or more previous successful pregnancies (Berek, 2020).
The World Health Organization (WHO) has raised infertility as an essential reproductive health problem that causes emotional, psychological, and social disorders (Ombelet, 2011).
The rate of female infertility varies in different countries. In India, 8.9% of women of reproductive age have primary infertility (Katole & Saoji, 2019). In China, 24.58% of women suffer from infertility, 6.54% from primary infertility, and 18.04% from secondary infertility (Liang et al., 2021). It is estimated that 21%-22% of Iranian women have primary infertility (Saei Ghare Naz et al., 2020).
Despite the high prevalence of infertility, most women conceal their problems from family and friends. Infertility often becomes a silent struggle that can lead to losing control over life and reducing physical and mental health (Rooney & Domar, 2018). Giving birth and raising children are traditionally among the most prominent characteristics of the female gender role in developing societies, where a woman is complete only when she becomes a mother. This attitude leads to inequality between women and men and other gender-dependent consequences such as pain and suffering (Hasanpoor-Azghdy et al., 2015; Vitale et al., 2017). This suffering and pain affect women’s physical, mental, and social health (Pour, 2014), necessitating effective coping methods to control tension.
The psychological problems caused by infertility can contribute to the aggravation of infertility. On the other hand, people with peace of mind and good mental health experience less psychological pressure, potentially enhancing their fertility prospects (Domar et al., 2000).
Coping as a dynamic process involves cognitive and behavioral responses to reduce or resolve a crisis. Religion, too, can play a significant role in helping individuals cope with stressful events. Religious coping refers to encountering stressful situations in life armed with religious beliefs and doing religious practices (Pargament et al., 2005). Religious coping can have negative and positive aspects. Negative coping includes a negative evaluation of God as a punitive force coupled with anger and uncertainty regarding God’s ability. Positive coping includes challenging natural sciences’ explanations, seeking meaning, and redefining stressful situations as an opportunity for spiritual growth (Cooper et al., 2009; Corsini, 2009).
Health-promoting lifestyle (HPL) emerges as one of the best approaches people can employ to maintain and control their health (Haica, 2013; Psaros et al., 2012). Scientific evidence indicates that HPL increases the quality of life (Tol et al., 2013; Mak et al., 2018). An unhealthy lifestyle may have adverse consequences for fertility. Health behaviors that affect fertility may be the first important step in helping infertile people and increasing their chances of fertility (Haica, 2013). Religious coping is associated with health-related behaviors (Mehrabi et al., 2016).
It has been shown that religion may affect HPL components, including spiritual growth, health responsibility, physical activity, nutrition, interpersonal relations, and stress management. A qualitative study found that religious coping, grounded in a spiritual framework, helps deal with the emotional burden of infertility (Latifnejad et al., 2014). In another qualitative study, infertile women reported using religious coping to deal with negative feelings about infertility (Taghipour et al., 2020). Religion helps people see the positive side of a stressful situation. Religious people believe that a higher power controls their lives and consider adverse life events an opportunity for spiritual growth (Aflakseir & Mahdiyar, 2016). Religion as a great source of coping can make possible the grounds for the tendency to use health-oriented behavior (Amid et al., 2016). A systematic review study that examined people’s health behaviors and their level of religiosity showed that increasing the level of religiosity and spirituality in people leads to healthier behaviors.
These healthy behaviors include reducing smoking, increasing physical activity, improving diet, and overall health responsibility (Koenig, 2015). Increasing the level of religiosity and spirituality in pregnant women may reduce smoking (Jesse & Reed, 2004). Another study on Iranian pregnant women reports that positive religious coping has an inverse relationship with pregnant women’s anxiety, and increasing negative feelings towards God are associated with increased pregnancy anxiety (Mirzaee et al., 2022). Additionally, attending religious ceremonies, following religious traditions, and reading religious texts were predictors of health-related behaviors in pregnant Pennsylvania women (Cyphers et al., 2017).
Various religions emphasize individual responsibility for body care and nutrition. Religious teachings underscore abandoning behaviors that harm the body (Koenig, 2012). Regarding sports and religion, studies have shown a significant positive relationship between religion and physical activity (Baetz & Bowen, 2008; Koenig, 2012). The findings of other studies have shown an inverse relationship between religion/spirituality and high-risk sexual activity (Cochran et al., 2004; Burdette et al., 2009). Religiosity affects health indirectly through the health-oriented lifestyle variable (Serajzadeh et al., 2013). Religion as an excellent source of coping lays the groundwork for adopting health-oriented behaviors (Amid et al., 2016).
Religion holds a unique position in Iranian society, influencing various dimensions of people’s lives, especially in crises (Saeidi Taheri et al., 2013). Considering the high prevalence of infertility in Iran and its related treatment demands and sometimes unsuccessful, as well as the psychological consequences following treatment processes, the present study was conducted to investigate the dimensions of religious coping and HPL in infertile women and determine the relationship between these two variables.
2. Materials and Methods
This cross-sectional correlational study was performed on 177 infertile women referring to the Sarem Sub-specialized Infertility Treatment and Research Center in Tehran City, Iran. This center is one of the most well-equipped infertility centers in Tehran. The average number of people visiting this center for the first visit is 8000 infertile couples from different parts of Iran annually. The subjects were recruited by census method from May to December 2019. The sample size was estimated through the Equation 1 to be 194 by considering the 95% CI, the test power of 80%, and the Pearson correlation coefficient of 0.2 between religious coping and HPL.
Due to the incompleteness of 17 questionnaires, 177 samples were included in the study.
The inclusion criteria were as follows: Women aged 15 to 49 (Gar-elnabi et al., 2020; Berlie & Alamerew, 2018), having reading and writing literacy, being in the first marriage, not using specific medications for mental disorders, lacking a history of mental illness based on the individual report, being a Muslim, having primary or secondary infertility approved by an obstetrician, undergoing infertility treatment for at least one year, lacking a living child in case of secondary infertility or an adopted child. The exclusion criterion was the failure to complete the questionnaire.
The study data were collected using a general information questionnaire, the Iranian religious coping scale (IRCS), and health-promoting lifestyle profile-II (HPLP-II). The available information questionnaire consisted of two parts. The first was demographic information, including age, education, occupation, and marriage duration. The second part focused on the characteristics of infertility, including infertility duration, current treatment, number of previous treatments, and the reason for requesting the treatment (personal desire, spouse insistence, family pressure).
The IRCS is a scale designed to assess Muslim religious coping. Aflakseir & Coleman (2011) developed the IRCS based on brief religious coping (brief RCOPE) (Pargament et al., 2000). The 14-item brief RCOPE measure is a widely used religious coping scale in different studies. It has positive and negative dimensions. Positive religious coping reflects a secure relationship with a transcendent power, a sense of spiritual connection with others, and a benevolent worldview. Negative religious coping reflects spiritual tensions and struggles within oneself, others, and God. Aflakseir and Coleman developed the IRCS with some items adapted from Brief RCOPE (Pargament et al., 2000) and reformulated it to apply Muslim religious beliefs. In addition, new items were added reflecting Islamic religious beliefs (e.g. “viewed my situation as a trial from God”). Since religious practices play an essential role in the Islamic faith, some Muslim practice-related items were included in this scale (e.g. “attended pilgrimage when I felt upset”). Those religious activities were selected that, based on interviews and pilot studies, Muslims often use to deal with stressful life events. In this way, after construct validity, IRCS consisted of 22 items categorized into 5 dimensions.
1. The practice of religious coping (6 items): A set of religious behaviors and actions (such as going to the mosque, reading the Quran, etc.) that a person performs when faced with stressful life events (e.g. seeking comfort and guidance by reading the Quran).
2. Benevolent reappraisal (6 items): The feelings and thoughts a person uses when faced with stressful situations to get closer to God and create peace (e.g. viewed my situation as a test from God).
3. Negative feelings toward God (4 items): Mental and spiritual tension and contradictions that a person shows about himself, others, and God (e.g. I expressed anger at God for letting this problem happen).
4. Passive religious coping (3 items): When a person does not try to solve the problem and stressful situation and considers the situation to be the result of God’s will (e.g. was destined to have this situation, so I didn’t try to change it).
5. Active religious coping (3 items): When a person puts his/her effort and energy into solving stressful situations and leaves the results of his actions in the hands of God (e.g. did what I could and turned the rest over to God).
The IRCS employs a 5-point Likert scale, ranging from 0 (not at all) to 4 (a great deal). This questionnaire does not have a total score. High scores on each dimension indicate high religious coping in that dimension. The Cronbach α of 0.89 was found acceptable for practice, 0.79 for benevolent reappraisal, 0.79 for negative feelings toward God, and 0.72 and 0.79 for passive and active religious coping, respectively (Aflakseir & Coleman, 2011).
We used IRCS in this study because the followers of monotheism, like Judaism, Christianity, and Islam, have fundamental beliefs about God and eternity. However, each religion has its own beliefs and practices to cope with particular situations. These beliefs and practices are not included in general questionnaires, the most widely used of which is the religious coping questionnaire by Pargament and colleagues. Therefore, in the present study, IRCS, which is sensitive to the beliefs and practices of Muslims, has been used.
The health-promoting lifestyle profile-II (HPLP-II) is a revised version of the HPLP developed by Walker et al. (1987). This scale consists of 52 items and 6 subscales: Spiritual growth (9 items), health responsibility (9 items), physical activity (8 items), nutrition (9 items), interpersonal relations (9 items), and stress management (8 items). The items are rated on a 4-point Likert scale ranging from 1 (never) to 4 (routinely). Walker and colleagues reported high internal consistency for the overall measure (α=0.94) and the subscales (from 0.79 to 0.87). Its 3-week test re-test stability coefficient was 0.89. A higher score indicates better health behavior Walker et al. (1987). Zeidi and colleagues confirmed the reliability and validity of the Persian version of this questionnaire. They have reported high internal consistency for the overall measure (α=0.82) and its subscales (from 0.64 to 0.91). Its 2-week test re-test stability coefficient was r=0.91 (Mohammadi Zeidi et al., 2012). The present study obtained internal consistency for the overall measure (α=0.84) and the subscales (from 0.71 to 0.89).
The data were described using frequency, Mean±SD and analyzed using the independent t-test, one-way ANOVA, and Pearson correlation coefficient in SPSS software, version 22. The significance level for all tests was set at P<0.05.
3. Results
The Mean±SD age of the subjects was 34.25±5.51 years. Their Mean±SD marriage duration was 7.48±4.62 years, and the Mean±SD infertility duration was 5.27±3.68 years with a range of 1-13 years. More information about the demographic and fertility characteristics of the subjects is presented in Table 1.
To compare the mean dimensions of religious coping and HPL variables, the means were calculated based on 0 to 100 in Table 2.
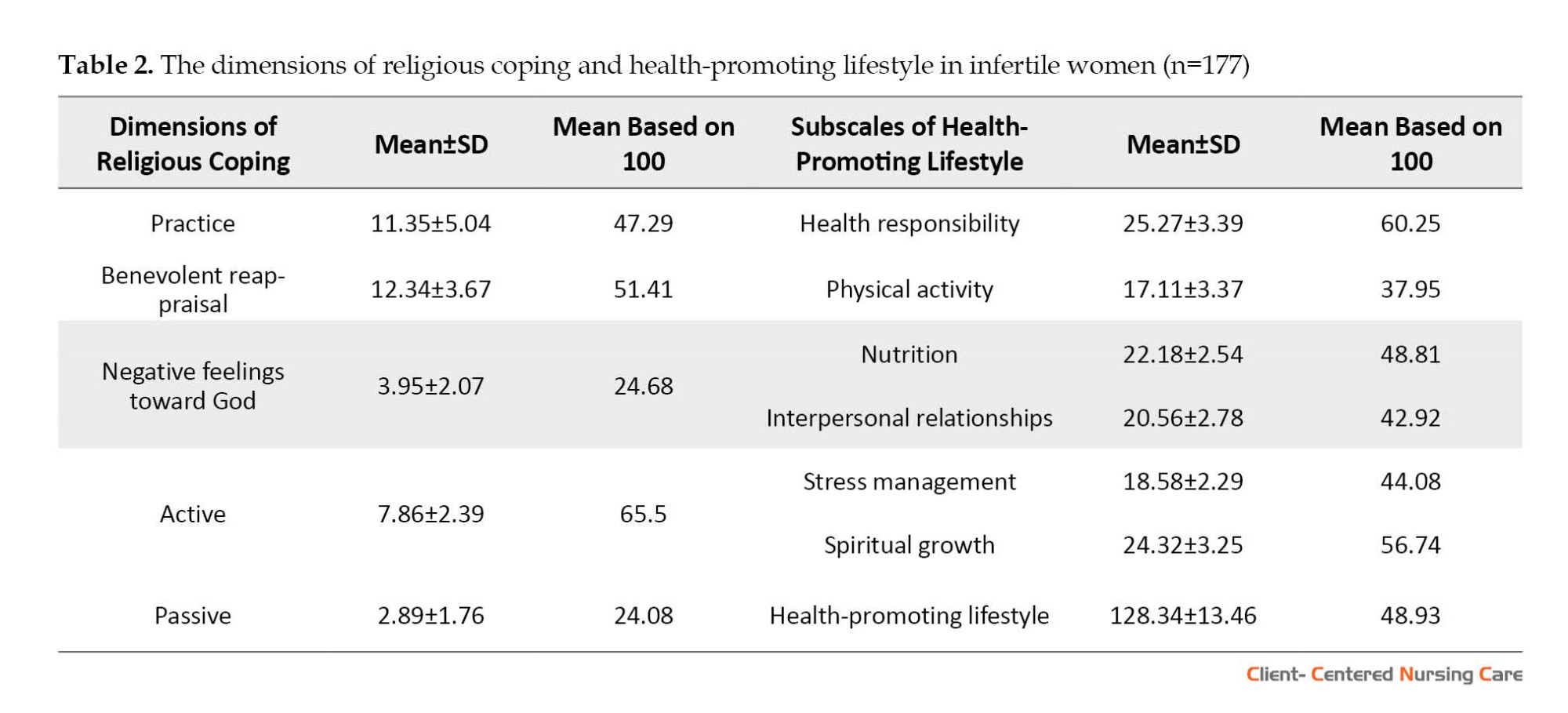
Table 3 details the relationship between religious coping with demographics and infertility characteristics of the subjects. Due to the wealth of the information, only significant items have been displayed.
Table 3 demonstrates a significant relationship between age, religious practice, and benevolent reappraisal. A two-by-two Tukey comparison showed that the mean score of religious practices of infertile women aged 30-39 years (P<0.001) and ≥40 years (P=0.016) was higher than that of women aged 20-29. Tukey’s two-by-two comparison also showed that the mean benevolent reappraisal score of infertile women aged 30-39 years (P=0.013) and ≥40 years (P=0.001) was higher than that of women aged 20-29.
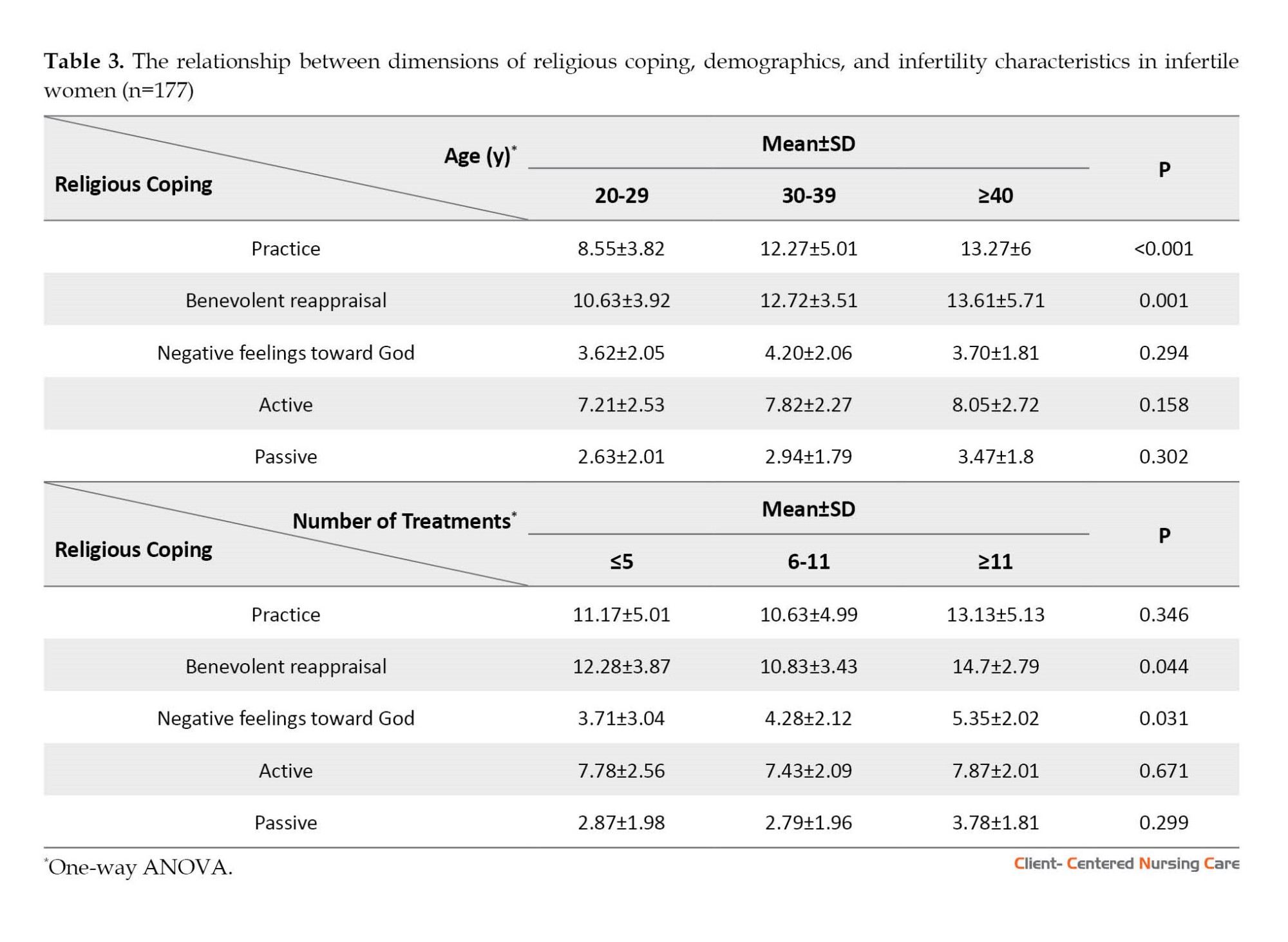
Table 3 also shows that benevolent reappraisal and negative feelings toward God significantly related to the number of infertility treatments. Tukey’s two-by-two comparison showed that the mean benevolent reappraisal score of infertile women with ≥11 times of treatment was higher than that of women with 6-11 times of treatment (P=0.046). Tukey’s two-by-two comparison also showed that the mean score of negative feelings towards God in infertile women with ≥11 treatment times was higher than that of women with ≤5 times (P=0.029). No significant relationship was found between HPL, demographics, and fertility characteristics in infertile women.
Table 4 presents the relationship between religious coping dimensions and HPL subscales.
Table 4 shows a weak yet significant inverse relationship between negative feelings toward God and health-promoting lifestyle and its 3 subscales: Physical activity, nutrition, and interpersonal relationships. Also, there is a weak but significant inverse association between passive religious coping and interpersonal relations.
4. Discussion
This study explored the relationship between religious coping and HPL in Iranian infertile women. According to the results, active religious coping had the highest mean score among various dimensions of religious coping, and negative feelings towards God and passive religious coping had the lowest mean scores. In line with our study, Aflakseir and Mahdiyar (2016) showed that the highest mean score was the practice and active religious coping in Iranian infertile women. The lowest was related to passive and negative coping. Another RCOPE scale study affirmed that the mean score of positive religious coping was higher than that of negative religious coping in infertile couples (Ghafouri et al., 2016).
In a study that measured the religious coping of infertile couples using the RCOPE scale, the mean score of positive religious coping of the women was higher than the median of the scale. The negative religious coping was lower than the scale median (Momenyan et al., 2020). In line with these results, in our study, the mean scores of benevolent reappraisal and active religious coping were higher than the scale median, and the mean score of negative feelings towards God was lower. Lopez and colleagues investigated the religious commitment of couples using the religious commitment inventory-10, whose items are similar to the items of active religious coping and benevolent evaluation of the tool used in the present study. It was found that the couples’ mean score of religious commitment was higher than the median of the tool (Lopez et al., 2011). In the present study, the mean scores obtained in the dimensions of active religious coping and the benevolent reappraisal of the infertile women were higher than the median of the related dimensions. Our study found that the mean score of infertile women’s HPL was lower than the median of the scale. Also, the health responsibility subscale had the highest mean score, and the physical activity subscale had the lowest mean score.
Mirghafourvand et al. (2017) examined the HPL of women with polycystic ovary syndrome (PCOS). More than 70% of its married subjects were infertile. They reported that the mean score of the total HPL was lower than the median value of the scale. The subscales of nutrition and then health responsibility had the highest mean scores, and stress management and physical activity had the lowest mean scores. The reason for the high average nutrition score is probably the complications of obesity (nearly 50% of the samples studied by Mirghforvand et al. had a body mass index ≥30) because women with PCOS usually try to lose weight with appropriate nutritional methods. Also, the reason for the low average score of stress management is probably due to the widespread complications of hyperandrogenism, such as hirsutism, alopecia, and acne, along with infertility and obesity, which reduce stress management in women with PCOS.
In a study to evaluate HPL and its related factors in 1200 Iranian women of reproductive age, the results showed that health responsibility had the highest, and physical activity had the lowest mean score (Abedi et al., 2017), which was similar to the results of our study. However, the mean scores of spiritual growth and health responsibility of our study subjects were lower, and the mean scores of stress management, nutrition, and physical activity of our study subjects were higher than those of the mentioned study. These differences may be due to the nature of the infertility problem and its treatment processes. Many women are challenged with infertility. Most infertile women struggle with this life event and use coping strategies, including developing flexibility and maintaining or gaining hope to deal with it and endure suffering (Romeiro et al., 2017). A qualitative study on religion and infertility reported “spiritual growth versus challenging one’s spiritual beliefs” as one of the main themes. Thus, infertility sometimes leads to spiritual growth and occasionally challenges one’s spiritual beliefs related to one’s understanding of God and sense of connection with God (Hasanpoor Azghdy et al., 2019). Regarding stress management, nutrition, and physical activity, infertile women, due to the nature of infertility, face social pressure and tension caused by the treatment process, so they may have better stress management than other women to improve their quality of life. Also, because of the treatment team’s advice to help the infertility treatment, they seek healthier nutrition and more physical activity (to lose weight) than other women. In confirmation of the findings of the present study, in most studies on HPL in Iran, where the study population was women of different ages or with conditions such as pregnancy and infertility, the lowest average has been related to physical activity (Mirghafourvand et al., 2017; Abedi et al., 2017; Rabiepoor et al., 2019). The results of a qualitative study in Iran have considered religious attitudes as one of the reasons for a decrease in the physical activity of women in Iranian society, which causes women not to be physically active in open spaces such as parks due to the presence of men (Amiri Farahani et al., 2018).
Our study found that no significant relationship was seen between practice, active religious coping, and benevolent reappraisal with HPL and its subscales among the dimensions of religious coping. However, with increasing negative religious coping in infertile women, HPL and its subscales, including physical activity, nutrition, and interpersonal relations, were decreased. Also, with increasing passive religious coping, interpersonal relationships decreased. Consistent with the present study, the findings of McKenzie et al. (2015) on black Canadians revealed a very weak relationship between religious involvement and health-related behaviors. They showed that this relationship is not an independent predictor of lifestyle practices. The results of a study on older adults also revealed no statistically significant correlation between religious orientation and HPL (Bakhtiari et al., 2019).
In the current study, a weak but significant inverse relation was observed between negative feelings towards God and the subscale of physical activity, which shows that the lower the negative feeling towards God, the higher the physical activity. The results of a study on Iranian pregnant women also show that with the increase in spiritual growth, the subjects’ physical activity increases (Rabiepoor et al., 2019). Another study on 1596 Danish men and women found that religiosity had a significant positive relationship with a healthier lifestyle, especially for those religiously educated by their parents (Herold et al., 2020). The findings of a study on 176 Malaysian Muslim men and women showed a strong relationship between religious performances and health-related behaviors (Hassan, 2015). The difference between the results of the mentioned studies and the present study’s findings may be related to the differences in the research community, the scale for measuring religious coping, the subjects’ religious beliefs, sample size, and cultural context.
In the present study, older infertile women performed more religious practices to deal with the stress caused by infertility and used benevolent reappraisal more than other age groups. Also, as the number of infertility treatments increased, benevolent reappraisal and negative feelings toward God increased. Consistent with the results of our study, a research study on religious coping of Ghanaian women with infertility showed that with increasing age, positive religious coping strategies such as benevolent reappraisal and focusing on religious practices increase. The same study also reported that as the duration of infertility and the number of treatments increased, infertile women developed negative feelings toward God, although this relationship was weak (Oti-Boadi & Oppong Asante, 2017).
A qualitative study also reported that successive treatment failures were associated with benevolent reappraisal in infertile women. However, religion has some challenges and developed negative feelings towards God (Hasanpoor Azghdy et al., 2019).
The study subjects completed the scales of the current research by the self-report method, which has specific limitations. Due to the study’s cross-sectional nature, the findings should be used cautiously. However, the results could be generalized to similar contexts.
5. Conclusion
The present study showed a weak yet significant inverse relationship between some dimensions of religious coping with HPL and some of its subscales. In other words, infertile women who had less negative feelings towards God and used less passive coping had relatively better HPL. Therefore, strengthening positive feelings towards God can be beneficial to some extent to improve the HPL of these women. However, enhancing HPL through educational interventions would be helpful. For this reason, it is suggested first to prepare the necessary coordination for designing an educational program through a mixed-method study, then evaluate the effectiveness of this educational program using interventional studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC. 1397.1006). The research aims and the confidentiality of the data were explained, and written informed consent was obtained from participants.
Funding
This study was extracted from master's thesis of Amin Gheysari, approved by the Department of Community Health Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences.
Authors' contributions
Data collection: Amin Gheysari; Writing and revising the manuscript: Amin Gheysari and Seyedeh Batool Hasanpoor-Azghady; Study design, data analysis, interpretation, and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the studied women who participated in the research and the subspecialty Center for Infertility Treatment and Research of Sarem for their cooperation in this study.
References
Abedi, P., Jorfi, M. & Afshari, P., 2017. [Evaluation of the health promotion lifestyle and its related factors in reproductive aged women in Ahvaz, Iran (Persian)]. Community Health Journal, 9(1), PP. 68-74. [Link]
Aflakseir, A. & Coleman, P .G., 2011. Initial development of the Iranian religious coping scale. Journal of Muslim Mental Health, 6(1), pp. 44-61. [DOI:10.3998/jmmh.10381607.0006.104]
Aflakseir, A. & Mahdiyar, M., 2016. The role of religious coping strategies in predicting depression among a sample of women with fertility problems in Shiraz. Journal of Reproduction & Infertility, 17(2), pp. 117–22. [PMID]
Amid, M., Shokri, O. & Zarani, F., (2016). [Casual relations model of antecedents and consequences of health behaviours in university students (Persian)]. Journal of Research in Psychological Health. 10, 70-8. [DOI:10.18869/acadpub.rph.10.3.70]
Amiri Farahani, L., Hasanpoor-Azgahdy, S. B. & Taghizadeh, Z., 2018. Iranian women’s perceptions and experiences of barriers to and facilitators of physical activity. Shiraz E-Medical Journal, 19(8), pp. e65287. [DOI:10.5812/semj.65287]
Bakhtiari, A., et al., 2019. Does religion predict health-promoting behaviors in community-dwelling elderly people? Journal of Religion and Health, 58(2), pp. 452-64. [DOI:10.1007/s10943-018-0710-3] [PMID]
Baetz, M. & Bowen, R., 2008. Chronic pain and fatigue: Associations with religion and spirituality. Pain Research and Management, 13(5), pp. 3838 [DOI:10.1155/2008/263751.] [PMID]
Berek, J.S. (2020). Berek & Novak’s gynecology essentials. Groningen :Wolters Kluwer. [Link]
Berlie, A.B. & Alamerew, Y. T., 2018. Determinants of fertility rate among reproductive age women (15-49) in Gonji-Kollela District of the Amhara National Regional State, Ethiopia. Ethiopian Journal of Health Development, 32(3), pp. 1-12. [Link]
Burdette, A. M., et al., (2009). “Hooking up” at college: Does religion make a difference? Journal for the Scientific Study of Religion, 48(3), pp. 535-51. [DOI:10.1111/j.1468-5906.2009.01464.x]
Cochran, J. K., et al., 2004. Religion, religiosity, and nonmarital sexual conduct: An application of reference group theory. Sociological Inquiry, 74(1), pp. 101-27. [Link]
Cooper, L. B., et al., 2009. Differentiated styles of attachment to God and varying religious coping efforts. Journal of Psychology and Theology, 37(2), pp. 134-41. [DOI:10.1177/009164710903700205]
Corsini, K. D., 2009. Examining the relationship between religious coping strategies, attachment beliefs and emotion regulation in a mixed sample of college students attending an evangelical university in central Virginia [PhD dissertation]. Virginia: Liberty University. [Link]
Cyphers, N. A., Clements, A. D. & Lindseth, G., 2017. The relationship between religiosity and health-promoting behaviors in pregnant women. Western Journal of Nursing Research, 39(11), pp. 1429–46. [DOI:10.1177/0193945916679623] [PMID]
Domar, A. D., et al., 2000. Impact of group psychological interventions on pregnancy rates in infertile women. Fertility and Sterility, 73(4), pp. 805-11. [PMID]
Gar-elnabi, M. E. M., et al., 2020. Assessment of infertility factors and their relative impact in pregnancy using ultrasonography & hormonal checkup. Journal of Science and Science Education, 1(1), pp. 30-4 [DOI:10.29303/jossed.v1i1.476]
Ghafouri, S. F., et al., 2016. The relation between marital adjustment and posttraumatic growth in infertile couples: The mediatory role of religious coping strategies. Journal of Reproduction & Infertility, 17(4), pp. 221-9. [PMID]
Hadizadeh-Talasaz, F., et al., 2020. Exploring infertile couples’ decisions to disclose donor conception to the future child. International Journal of Fertility & Sterility, 14(3), pp. 240-6. [DOI:10.22074/ijfs.2020.44408] [PMID]
Haica, C. C., 2013. Gender differences in quality of life, intensity of dysfunctional attitudes, unconditional self-acceptance, emotional distress and dyadic adjustment of infertile couples. Procedia-Social and Behavioral Sciences, 78, pp. 506-10. [DOI:10.1016/j.sbspro.2013.04.340]
Hasanpoor-Azghady, S. B., et al., 2019. The social construction of infertility among Iranian infertile women: A qualitative study. Journal of Reproduction & Infertility, 20(3), pp. 178-90. [PMID]
Hasanpoor-Azghdy, S. B., Simbar, M. & Vedadhir, A., 2014. The emotional-psychological consequences of infertility among infertile women seeking treatment: Results of a qualitative study. Iranian Journal of Reproductive Medicine, 12(2), pp. 131-8. [PMID]
Hasanpoor-Azghdy, S. B., Simbar, M. & Vedadhir, A., 2015. The social consequences of infertility among Iranian women: A qualitative study. International Journal of Fertility & Sterility, 8(4), pp. 409-20. [DOI:10.22074/ijfs.2015.4181] [PMID]
Hassan, S. H., 2015. Effects of religious behavior on health-related lifestyles of Muslims in Malaysia. Journal of Religion and Health, 54(4), pp. 1238–48. [DOI:10.1007/s10943-014-9861-z] [PMID]
Herold, S.C., et al., 2022. Is religiousness associated with better lifestyle and health among Danes? Findings from SHARE. Journal of Religion and Health, 61(2), pp. 1621–40. [DOI:10.1007/s10943-020-01050-3] [PMID]
Inhorn, M.C. & Patrizio, P., 2015. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Human Reproduction Update, 21(4), pp. 411–26. [DOI:10.1093/humupd/dmv016] [PMID]
Jesse, D. E. & Reed, P. G., 2004. Effects of spirituality and psychosocial well-being on health risk behaviors in Appalachian pregnant women. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 33(6), pp. 739–47. [DOI:10.1177/0884217504270669] [PMID]
Katole, A. & Saoji, A. V., 2019. Prevalence of primary infertility and its associated risk factors in urban population of central India: A community-based cross-sectional study. Indian Journal of Community Medicine, 44(4), pp. 337–41. [DOI:10.4103/ijcm.IJCM_7_19] [PMID]
Koenig, H. G., 2015. Religion, spirituality, and health: A review and update. Advances in Mind-Body Medicine, 29(3), pp. 19–26. [PMID]
Koenig, H. G., 2012. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry, 2012, pp. 278730. [DOI:10.5402/2012/278730] [PMID]
Latifnejad Roudsari, R., Allan, H. T. & Smith, P.A., 2014. Iranian and English women’s use of religion and spirituality as resources for coping with infertility. Human Fertility, 17(2), pp. 114–23. [DOI:10.3109/14647273.2014.909610] [PMID]
Liang, S., et al., 2021. Prevalence and associated factors of infertility among 20-49-year-old women in Henan Province, China. Reproductive Health, 18(1), pp. 254. [DOI:10.1186/s12978-021-01298-2] [PMID]
Lopez, J. L., et al., 2011. Religious commitment, adult attachment, and marital adjustment in newly married couples. Journal of Family Psychology, 25(2), pp. 301–9. [DOI:10.1037/a0022943] [PMID]
Mak, Y. W., et al., 2018. Health-promoting lifestyle and quality of life among Chinese nursing students. Primary Health Care Research & Development, 19(6), pp. 629-36. [DOI:10.1017/S1463423618000208] [PMID]
McKenzie, M. M., et al., 2015. Religious involvement and health-related behaviors among Black Seventh-Day Adventists in Canada. Health Promotion Practice, 16(2), pp. 264–70.[DOI:10.1177/1524839914532812] [PMID]
Mehrabi, E., et al., 2016. [Religion, spirituality and coping with breast cancer: A phenomenological study (Persian)]. Journal of Reaserch on Religion & Health, 2(2), pp. 12-23. [Link]
Mirghafourvand, M., Mohammad-Alizadeh Charandabi, S. & Aliasghari, F., 2017. [Assessment of health promoting lifestyle status and its socio-demographic predictors in women with polycystic ovarian syndrome (Persian)]. Hayat, 22(4), pp. 394-407. [Link]
Mirzaee, F., Hasanpoor-Azghady, S. B. & Amiri-Farahani, L., 2022. Correlation between religious coping, demographic and fertility factors, and pregnancy anxiety of Iranian primiparous women: A cross-sectional study. BMC Psychiatry, 22(1), pp. 298. [DOI:10.1186/s12888-022-03922-2] [PMID]
Mohammadi Zeidi, I., Pakpour Hajiagha, A. & Mohammadi Zeidi, B., 2011. [Reliability and validity of Persian version of the health-promoting lifestyle profile (Persian)]. Journal of Mazandaran University of Medical Sciences, 20(1), pp. 102-13. [Link]
Momenyan, S., et al., 2020. [The relationship between religious coping and quality of life in infertile couples (Persian)]. Iranian Journal of Nursing Research, 15(3), pp. 47-55. [Link]
Nayebi Nia, A. S., et al., 2018. [Domestic violence and its association with domains of reproductive health in women: A systematic review (Persian)]. Journal of Mazandaran University of Medical Sciences, 27(158), pp. 205-17. [Link]
Ombelet, W., 2011. Global access to infertility care in developing countries: A case of human rights, equity and social justice. Facts, Views & Vision in ObGyn, 3(4), pp. 257–66. [PMID]
Oti-Boadi, M. & Oppong Asante, K., 2017. Psychological health and religious coping of Ghanaian women with infertility. BioPsychoSocial Medicine, 11, pp. 20. [DOI:10.1186/s13030-017-0105-9] [PMID]
Pargament, K.I., Koenig, H. G. & Perez, L. M., 2000. The many methods of religious coping: Development and initial validation of the RCOPE. Journal of Clinical Psychology, 56(4), pp. 519-43. [PMID]
Pargament, K. I., Magyar-Russell, G. M. & Murray-Swank, N. A., 2005. The sacred and the search for significance: Religion as a unique process. Journal of Social Issues, 61(4), pp. 665-87. [DOI:10.1111/j.1540-4560.2005.00426.x]
Pour, T. H., 2014. The effect of cognitive behavioural therapy on anxiety in infertile women. European Journal of Experimental Biology, 4(1), pp. 415-9. [Link]
Psaros, C., et al., 2012. A brief report of depressive symptoms and health promoting behaviors among women with infertility attending a clinical mind-body program. Journal of Psychosomatic Obstetrics & Gynecology, 33(1), pp. 32–6. [DOI:10.3109/0167482X.2011.643933] [PMID]
Rabiepoor, S., Sadeghi, E. & Sayyadi, H., 2019. Spiritual health and physical activity among Iranian pregnant women. Journal of Religion and Health, 58(2), pp. 506–15. [DOI:10.1007/s10943-017-0487-9] [PMID]
Romeiro, J., et al., 2017. Spiritual aspects of living with infertility: A synthesis of qualitative studies. Journal of Clinical Nursing, 26(23-24), pp. 391735. [DOI:10.1111/jocn.13813] [PMID]
Rooney, K. L. & Domar, A. D., 2018. The relationship between stress and infertility. Dialogues in Clinical Neuroscience, 20(1), pp. 41–7. [DOI:10.31887/DCNS.2018.20.1/klrooney] [PMID]
Saeedi Taheri, Z., Asadzandi, M., & Ebadi, A. (2013). [The effect of spiritual care based on general sediment model on the spiritual experiences of patients with coronary artery disease (Persian)]. Nursing Psychology Journal, 1, pp. 45-53. [Link]
Saei Ghare Naz, M., Ozgoli, G. & Sayehmiri, K., 2020. Prevalence of infertility in Iran: A systematic review and meta-analysis. Urology Journal, 17(4), pp. 338–45. [DOI:10.22037/uj.v0i0.5610] [PMID]
Serajzadeh, S. H., Javaheri, F. & Velayati Khajeh, S., 2013. [Religion and health: An examination of the effect of religiosity on health in a sample of university students (Persian)]. Journal of Applied Sociology, 24(1), pp. 55-77. [Link]
Sohbati, F., et al., 2021. Psychological well-being of infertile women and its relationship with demographic factors and fertility history: A cross-sectional study. BMC Women’s Health, 21(1), pp. 22. [DOI:10.1186/s12905-020-01167-3] [PMID]
Taghipour, A., et al., 2020. Coping strategies of women following the diagnosis of infertility in their spouses: A qualitative study. Evidence Based Care, 10(1), pp. 15-24. [DOI:10.22038/EBCJ.2020.42136.2120]
Tol, A., et al., 2013. Health-promoting lifestyle and quality of life among undergraduate students at school of health, Isfahan university of medical sciences. Journal of Education and Health Promotion, 2, pp. 11. [DOI:10.4103/2277-9531.108006] [PMID]
Vitale, S. G., et al., 2017. Psychology of infertility and assisted reproductive treatment: The Italian situation. Journal of Psychosomatic Obstetrics & Gynecology, 38(1), pp. 1-3. [DOI:10.1080/0167482X.2016.1244184] [PMID]
Walker, S. N., Sechrist, K. R. & Pender, N. J., 1987. The health promoting lifestyle profile: Development and psychometric characteristics. Nursing Research, 36(2), pp. 76–81.[DOI:10.1097/00006199-198703000-00002] [PMID]
Type of Study: Research |
Subject:
General
Received: 2022/12/13 | Accepted: 2023/05/20 | Published: 2023/11/1
Received: 2022/12/13 | Accepted: 2023/05/20 | Published: 2023/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |