Sat, Jul 12, 2025
[Archive]
Volume 10, Issue 2 (Spring 2024)
JCCNC 2024, 10(2): 91-100 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hafedh Ahmed S, Salman Khudhair A K, Haghani S, Najafi Ghezeljeh T. Knowledge, Attitude, and Practice of Iraqi Intensive Care Nursing Staff Regarding Pressure Ulcer Prevention. JCCNC 2024; 10 (2) :91-100
URL: http://jccnc.iums.ac.ir/article-1-463-en.html
URL: http://jccnc.iums.ac.ir/article-1-463-en.html
Sukaina Hafedh Ahmed1 

 , Abdul Kareem Salman Khudhair2
, Abdul Kareem Salman Khudhair2 

 , Shima Haghani3
, Shima Haghani3 

 , Tahereh Najafi Ghezeljeh *4
, Tahereh Najafi Ghezeljeh *4 




 , Abdul Kareem Salman Khudhair2
, Abdul Kareem Salman Khudhair2 

 , Shima Haghani3
, Shima Haghani3 

 , Tahereh Najafi Ghezeljeh *4
, Tahereh Najafi Ghezeljeh *4 


1- Department of Nursing, Nursing and Midwifery School, Iran University of Medical Sciences, Tehran, Iran.
2- College of Nursing, University of Basra, Basra, Iraq.
3- Nursing Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- Cardiovascular Nursing Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran. ,najafi.t@iums.ac.ir
2- College of Nursing, University of Basra, Basra, Iraq.
3- Nursing Care Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- Cardiovascular Nursing Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 593 kb]
(573 Downloads)
| Abstract (HTML) (1948 Views)
● Pressure ulcer (PU) is one of the most serious and prevalent concerns in healthcare, and its incidence is commonly considered a marker for measuring the quality of care.
● Regarding PU prevention, in this study, the Iraqi nurses’ knowledge was low, and their attitudes and practices were unfavorable.
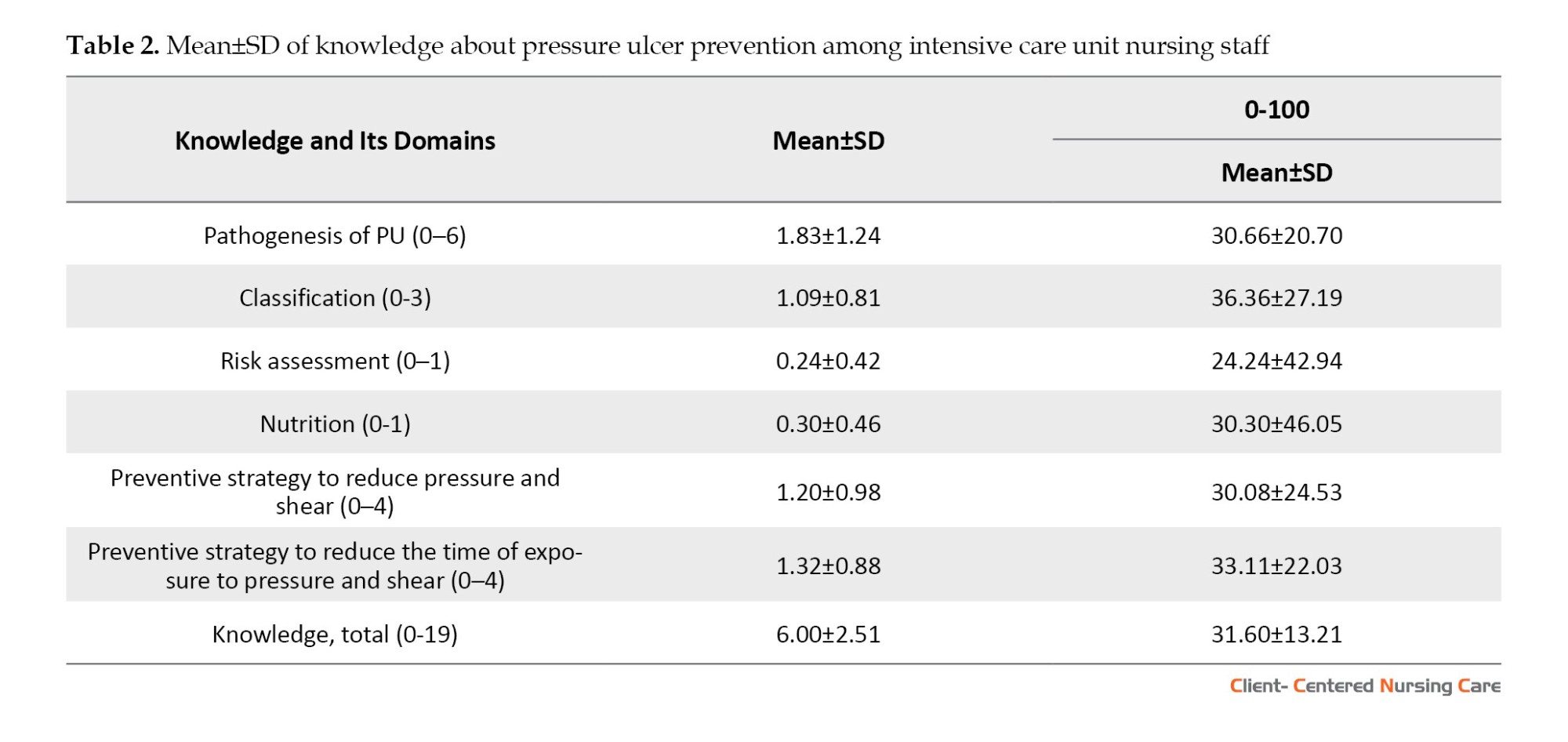
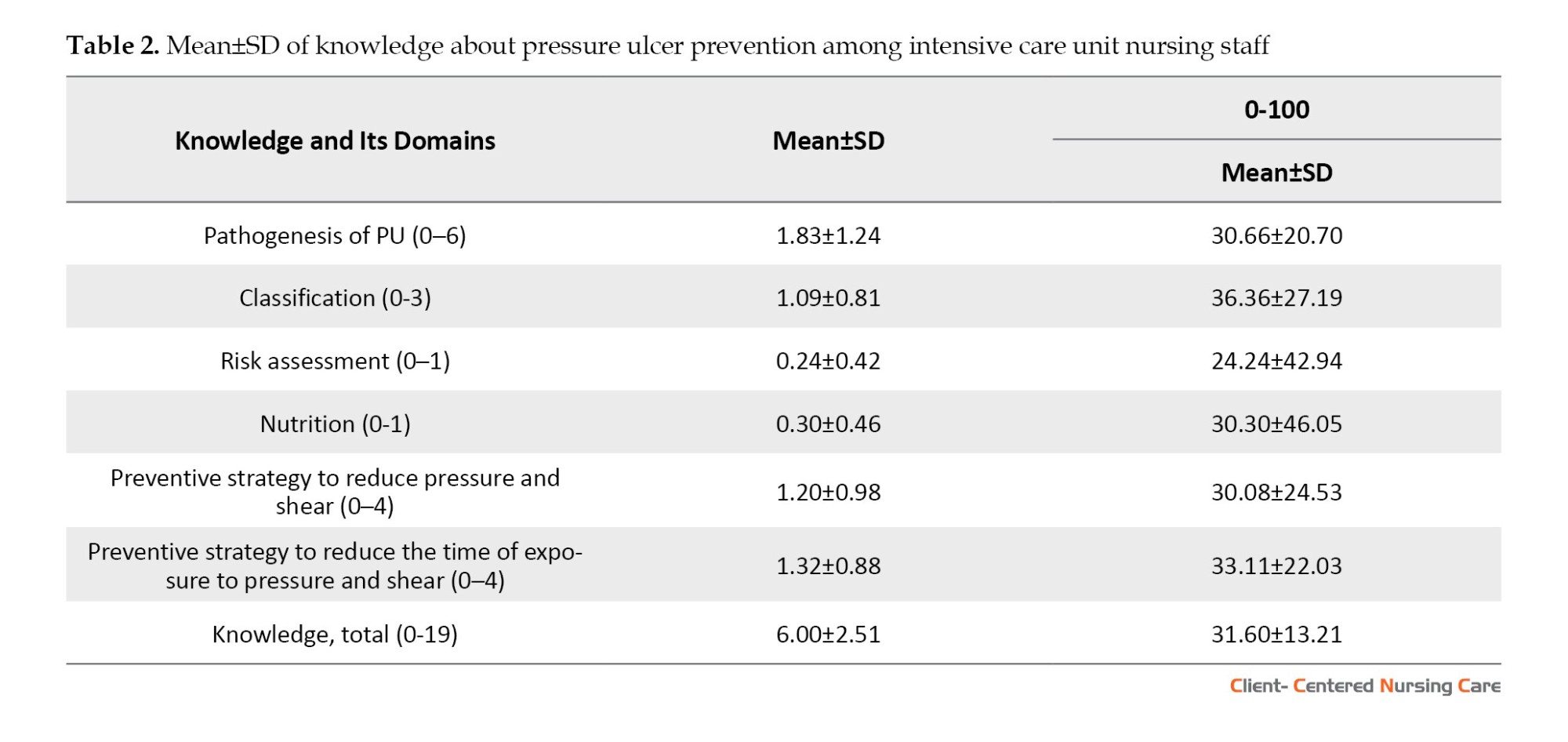
• The knowledge about risk assessment of PU had the lowest mean score, while the knowledge about classification and observation of PU obtained the highest score.
● Nurses’ attitudes toward the “impact of pressure ulcers” had the lowest mean score.
● Nurses considered it important to have “confidence in the effectiveness of prevention” and “prioritize pressure ulcer prevention”.
● There was a significant relationship between knowledge about PU and participation in an in-service training program on PU.
● There was also a significant relationship between the practice of PU and years of experience in the intensive care unit.
● Regarding PU prevention, in this study, the Iraqi nurses’ knowledge was low, and their attitudes and practices were unfavorable.
• The knowledge about risk assessment of PU had the lowest mean score, while the knowledge about classification and observation of PU obtained the highest score.
● Nurses’ attitudes toward the “impact of pressure ulcers” had the lowest mean score.
● Nurses considered it important to have “confidence in the effectiveness of prevention” and “prioritize pressure ulcer prevention”.
● There was a significant relationship between knowledge about PU and participation in an in-service training program on PU.
● There was also a significant relationship between the practice of PU and years of experience in the intensive care unit.
Plain Language Summary
Pressure ulcer (PU) incidence is an essential indicator of care quality. These ulcers could cause serious complications for patients, including increased morbidity and mortality rates. PU occurrence is even more prevalent among intensive care unit (ICU) patients. Given nurses’ critical role in PU prevention, evaluating their knowledge, attitude, and practice in this area is essential. This study evaluated the knowledge, attitude, and practice of ICU nurses working in Al-Basra and Dhi Qar cities, Iraq, regarding preventing PU. The findings revealed a lack of knowledge, an unfavorable attitude, and a lack of practice among nurses, emphasizing the need for targeted interventions and education to enhance PU prevention and patient care.
Full-Text: (414 Views)
Introduction
Pressure ulcers (PUs) are localized injuries to the skin, underlying tissues, or both, usually over a bony prominence. It is caused by pressure alone or combined with shear and friction (Kim & Lee, 2019). The incidence of PU among intensive care unit (ICU) patients is even higher, ranging from 6.60% to 36.80% globally (Chaboyer et al., 2018). Patients in the ICU have a 4-time higher chance of developing PU, longer stays, and poor tissue perfusion (Yilmazer et al., 2019). According to the international PU prevalence survey, the medical ICU had the greatest prevalence (12.1%) of facility-acquired PU (Zuo & Meng, 2015).
Basically, PU is a severe burden for patients and clients of all ages, resulting in difficulties and issues such as discomfort, pain, and decreased quality of life (Grešš Halász et al., 2021). Developing PU can cause prolonged hospital stays and more significant costs for the healthcare system (Olsho et al., 2014). U causes complications for patients and increases their morbidity and mortality rates (Hu et al., 2021). Other serious consequences include delayed rehabilitation, prolonged illness, increased healthcare costs, disability, and death. These complications impose extensive supplies, nursing hours, and long-term physiotherapies (Ingwu et al., 2019). In addition, PU can increase the risk of infection (Grešš Halász et al., 2021). It is reported that up to 53% of PUs have become clinically infected, which can result in cellulitis, abscess, osteomyelitis, and bacteremia—all of which can lead to significant mortality (Hu et al., 2021). The incidence and prevention of PU represent a marker of quality of care and safety for healthcare organizations and facilities (Sham et al., 2020; Dlungwane, 2020).
Hence, increased attention to PU prevention is anticipated to improve patient care while also lowering the expenses associated with ICU treatment (Dilie & Mengistu, 2015). anagement and prevention of PU include regulations and auditing, the implementation of appropriate procedures, and the cooperation of healthcare providers (Dlungwane, 2020). The National Pressure Injury Advisory Panel (NPIAP) and European Pressure Ulcer Advisory Panel (EPUAP) developed guidelines for PU prevention (Dlungwane, 2020). Prevention and treatment of PUs require multidisciplinary collaboration (Ingwu et al., 2019). However, nurses’ roles are more significant as they are the frontline in providing patient care (Finkelman & Kenner, 2016).
The nurse’s primary role is to assess the individuals at risk, take measures to eliminate causative factors, and ensure a PU healing process (Nuru et al., 2015). PUs are a primary nurse-sensitive outcome, and nursing care significantly affects PU development and prevention (Sham et al., 2020). As nurses play a critical role in PU prevention and management, evaluating their knowledge, attitude, and practice in this area is paramount. Notably, nurses’ lack of knowledge, skills, and negative attitudes contribute significantly to the occurrence or worsening of PUs (Moore & Patton, 2019).
Previous studies in different countries that have focused on nurses’ knowledge, attitude, and practice regarding PU, yielded dissimilar results (Khojastehfar et al., 2020; Dlungwane, 2020; Ingwu et al., 2019; Awoke et al., 2022; Kim & Lee, 2019; Yilmazer et al., 2019; Hu et al., 2021). However, these findings cannot be generalized to the specific context of Iraq, where there is a lack of information in this field and only one related study has been found in Iraq. In that study, 100 nurses in an acute care setting reported a positive attitude toward PU prevention (Hussein et al., 2006). The researcher developed the instrument used in the study, but its validity and reliability have not been reported.
Given that evaluating ICU nurses’ current knowledge, attitude, and practice is critical for planning appropriate interventions and revising nursing education programs, this study was designed to investigate knowledge, attitude, and practice regarding PU prevention among ICU nursing staff in governmental (teaching and non-teaching) hospitals in Al-Basra and Dhi-Qar cities, Iraq.
Materials and Methods
In this cross-sectional study with a descriptive design, 231 ICU nursing staff in 8 governmental hospitals (6 hospitals in Al-Basra and 2 hospitals in Dhi-Qar), Iraq, were recruited through the census method. The study data were collected from August to September 2022 using electronic versions of a demographic form and questionnaires to assess pressure ulcer prevention knowledge, attitude, and practice. The questionnaires were designed using Google Forms and distributed through a WhatsApp group. Nurses’ cell phone numbers were obtained to form the WhatsApp group, and the questionnaires were shared via this platform. To encourage timely completion, reminder messages were sent to the nurses daily for a week.
Study instruments
Demographic questionnaire
This questionnaire was prepared by reviewing related texts, and its content validity was checked and confirmed by a group of experts, which consisted of three members of the Faculty of Nursing and Midwifery of Basra University. The demographic form included the variables of age, gender, marital status, education level, nursing work experience, ICU work experience, working hours per week, and the experience of participating in an in-service training program related to PU prevention within the last year.
Pressure ulcer prevention knowledge questionnaire
This questionnaire was developed by Beeckman et al. (2010) and modified by Lee et al. (2014). It includes 19 multiple-choice questions with three answer options. It reflects six domains expressing the most relevant aspects of PU prevention: Pathogenesis of PU (6 items), classification (3 items), risk assessment (1 item), nutrition (1 item), preventive strategy to reduce pressure and shear (4 items), and preventive strategy to reduce the time of exposure to pressure and shear (4 items). The total score ranges from 0 to 19, which means a higher knowledge of PU prevention (Beeckman et al., 2010). To determine the adequacy of nurses’ knowledge, a threshold of correctly answering 90% or more of the questions on the questionnaire was considered The original instrument demonstrated a Cronbach α 0.77 (Beeckman et al., 2010). Another study reported its Cronbach α as 0.73 (Kim & Lee, 2019).
In this study, the questionnaire underwent a translation and back translation method for cross-cultural adaptation. A translator familiar with medical concepts translated the original text into Arabic to achieve this. Subsequently, the translated Arabic version was independently translated back into English by a bilingual specialist who had no prior knowledge of the original questionnaire. Following this, the researchers compared the translated and original versions to ensure accuracy and finalized the questionnaire for psychometric evaluation. To assess the content validity of the Arabic version of the questionnaire, a panel of experts consisting of three faculty members from the School of Nursing and Midwifery at Basra University reviewed it. Their input and feedback were taken into consideration during the adaptation process. In the studied population, the internal consistency of the questionnaire was measured using the Kuder-Richardson 20 coefficient, resulting in a value of 0.67. This value indicates that the questionnaire demonstrated an appropriate level of internal consistency.
Attitude towards pressure ulcers prevention questionnaire
This questionnaire, developed by Beeckman et al. (2010), has 13 questions. Nurses indicated their attitude using a 4-point Likert scale (1=strongly disagree, 2=disagree, 3=agree, 4=strongly agree). It is important to note that the scoring is inverse for some items (3, 5, 7, 10, and 13) in the questionnaire. The total score ranged from 13 to 52. Higher scores indicate a more favorable attitude. In particular, the attitude was considered favorable if its mean score was more than or equal to 75% of the maximum score, which was 39 (Beeckman et al., 2010). The questionnaire has 5 subscales: Personal competence to prevent PU, priority of PU prevention, impact of PU, responsibility in PU prevention, and confidence in the effectiveness of prevention. A study confirmed its content validity, and its Cronbach α coefficient was also reported to be 0.88 (Simonetti et al., 2015). In this study, the translation was done in the same way as the knowledge questionnaire. In the studied population, the internal consistency of the questionnaire was measured using the Cronbach α coefficient, resulting in a value of 0.71.
The practice of pressure ulcerprevention questionnaire
This self-report questionnaire, which was developed by Nasreen et al. (2017), has 20 items and scores on a 3-point Likert scale from “always”=2 to “never”=0 to measure people’s practice concerning PU prevention. The total score ranges from 0 to 40, and a higher score indicates better practice of nurses in preventing PU. The practice was considered favorable if its mean score was more than or equal to 90% of the maximum score, which was 36 (Nasreen et al., 2017). In a study on nurses, the Cronbach α coefficient was reported to be 0.95 (Nuru et al., 2015). The translation and back translation of this tool was similar to the knowledge questionnaire. In the studied population, the internal consistency of the questionnaire was measured using the Cronbach α coefficient, resulting in a value of 0.78.
Data analysis
The Excel output of the Google Form was taken and transferred to SPSS software, version 22, for analysis. The data was analyzed by descriptive and inferential statistical tests in SPSS software, version 22. The scores of the main variables were rescaled to a range of 0 to 100. Descriptive (absolute and relative frequency, Mean±SD) and inferential statistics (the independent t-test, chi-square test, and Fisher exact test) were used to analyze the data per the research objectives. The Kolmogorov-Smirnov test was used to evaluate the normal distribution of the variables. The significance level was considered <0.05. The tables related to the frequency distribution of the knowledge, attitude, and practice questionnaire items were attached in a supplementary file.
Results
According to Table 1, the majority of the subjects (66.2%) were <30 years old; more than half of them (53.7%) were female and married (52.4%). Most samples (61.0%) had a BSc, 51.9% of the subjects had less than 5 years of practical experience in nursing, and more than half of the samples (73.2%) had less than 5 years of practical experience in ICU. The results revealed that 88.3% of the subjects worked 50 hours or less weekly. Finally, Table 1 shows that 56.7% of the samples have participated in an in-service training program.

Table 2 presents the mean scores of different domains of knowledge. The lowest mean score (24.24±42.94) was related to “risk assessment”, whereas the highest mean score (36.36±27.19) was obtained for “knowledge about PU classification”. The vast majority of the nurses (93.5%) responded incorrectly to the item “repositioning is an accurate preventive method because the duration of pressure and shear will be reduced” in the knowledge questionnaire. The lowest percentage of incorrect answers (38.5%) was related to the item “Fewer patients will have PU if patients are mobilized”. The knowledge of all nurses was insufficient and weak because they had answered less than 90% of the questions correctly.
Based on Table 3, the staff attitude towards the impact of PU received the lowest mean score (45.79±13.71), while the highest mean score was recorded for confidence in the effectiveness of prevention (72.00±19.42). The total mean attitude score was found to be 35.52±3.97. Additionally, the attitude of most nurses (79.7%) was unfavorable. The nurses’ attitudes related to the item “The impact of pressure ulcers on a patient should not be exaggerated” had the lowest mean score (1.79±0.75). In contrast, the highest mean score (3.50±0.73) was related to the item “pressure ulcers are never preventable”.

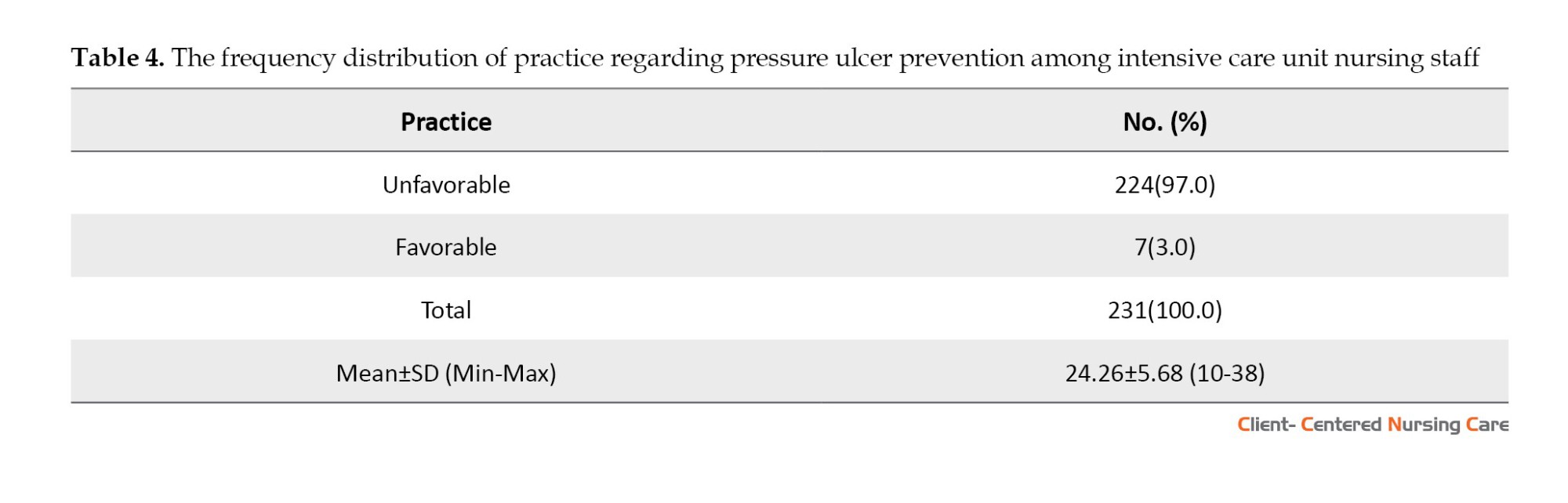
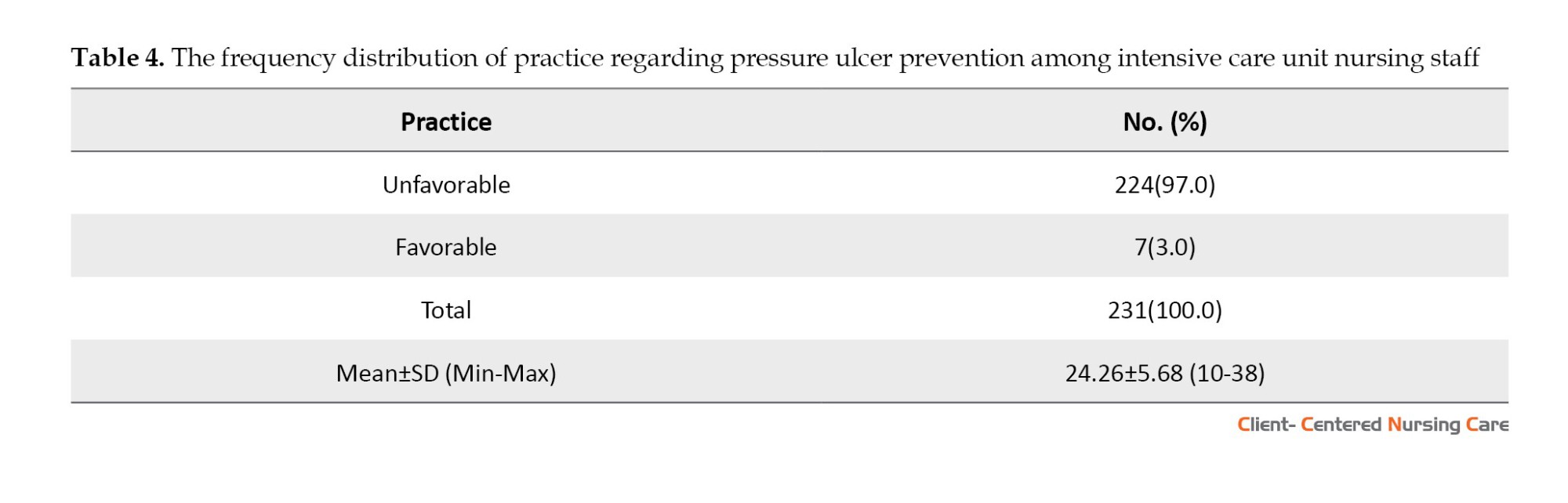
According to Table 4, most nurses in the study (97%) demonstrated unfavorable levels of practice in PU prevention (24.26±5.68). In the practice questionnaire, the item “I perform lab test for assessing nutritional status followed by physician’s instruction” had the lowest mean score (0.73±0.74). In contrast, the highest mean score (1.57±0.62) was related to the item “I use special mattress to prevent pressure loadings, such as foam, air”.
The results of the independent t-test (Table 1) revealed a significant relationship between the nurses’ knowledge about PU and participation in an in-service training program (P=0.021). Nurses who underwent PU training exhibited higher knowledge levels compared to their counterparts who did not participate in such training. Furthermore, the findings in Table 1 indicated a significant relationship between the mean score of practice and years of practical experience in the ICU (P=0.017). A Tukey test further disclosed that nurses with 5 to 10 years of ICU experience were more likely to practice PU optimally than those with more than 10 years of ICU experience (P=0.013).
Discussion
According to the results, the nursing staff in this study lacked proper knowledge and had unfavorable attitudes and practices regarding PU.
In this study, nurses’ knowledge was low in total and all dimensions. The low level of knowledge among ICU nurses regarding PU can be attributed to the lack of attention to PU in nursing education and in-service training programs. This study revealed that more than half of the nurses had not participated in any training program. Nurses’ busy schedules might also be an issue, preventing them from engaging in training programs. Given the importance of prevention in caring for patients at risk of developing PU, nurses’ proper knowledge plays a crucial role. Therefore, healthcare facility managers should take necessary measures to empower the healthcare team, especially nurses, as PU poses a significant risk to patient safety. By providing adequate training and educational opportunities, healthcare facilities can enhance the knowledge and expertise of their nursing staff in PU prevention and management.
The findings revealed a significant relationship between knowledge about PU and participation in an in-service training program on PU. Nurses who underwent PU training exhibited higher knowledge levels compared to those who did not receive such training. This finding emphasizes the importance of education and its effectiveness in enhancing nurses’ understanding of PU. To make these educational programs successful, careful planning is essential to address the specific educational needs of nurses.
The present study findings are in line with previous studies. A cross-sectional survey by Jiang et al. (2020) in China showed that 41.7% of nurses had insufficient knowledge regarding PU prevention. Similarly, a cross-sectional descriptive study in China by Li et al. (2023) revealed that critical care nurses’ knowledge about PU was assessed as insufficient. Another study reported that Belgian nurses in nursing homes had low levels of knowledge about PU (Demarré et al., 2012). Another study indicated that the knowledge of Iranian ICU nurses was insufficient (Khojastehfar et al., 2020), though nurses had more knowledge than the present study. Contrary to the present study’s findings, a descriptive cross-sectional survey by Köse & Öztunc (2016) showed that most participants had good knowledge about PU preventative strategies. This difference in findings may be attributed to variations in the scales used to assess knowledge levels and the threshold score set to define sufficient knowledge.
The present study revealed that the attitudes of most nurses, both total and across all dimensions, were unfavorable. This unfavorable attitude among ICU nurses can be attributed to their lack of knowledge about the effects of PU. Nurses must recognize PU as a significant patient safety indicator and be aware of its potential harm and detrimental impact on patients. By understanding the seriousness of PU, nurses can take proactive measures to prevent its development and effectively manage at-risk patients. Addressing these unfavorable attitudes is essential for promoting evidence-based practice among healthcare professionals (Simonetti et al., 2015). Proper interventions are needed to change nurses’ attitudes; education can influence these changes. Nursing administrators should develop programs to increase ICU nurses’ confidence in PU prevention (Hu et al., 2021).
In line with the current research, a cross-sectional survey by Jiang et al. (2020) revealed that nurses’ attitudes were unfavorable. Similarly, the present study aligns with research indicating that most Iranian nurses are unfavorable toward PU prevention (Khojastehfar et al., 2020). However, it is noteworthy that in that study, the mean score of attitude was higher than the current research. Another study, inconsistent with our findings, indicated moderate nurses’ attitudes toward PU prevention (Tirgari et al., 2018). This difference can be attributed to the differences in instruments used to assess attitudes and the fact that the current research explicitly focused on ICU nurses.
The results showed that ICU nurses’ practice regarding PU was unfavorable. This finding could be attributed to the fact that the ICU nurses in this study had insufficient knowledge about PU and unfavorable attitudes regarding its prevention. Consequently, their practice in preventing PU may have been adversely affected. Enhancing nurses’ knowledge and attitudes through targeted education and interventions could improve their practice and ultimately improve PU prevention outcomes.
In line with the study, the results of two studies revealed that more than 82% of nurses’ practices were unfavorable in terms of preventing PU (Nasreen et al., 2017; Berihu et al., 2020). Contrary to the findings of this study, a descriptive cross-sectional study showed that most nurses have favorable practices for preventing PU (Sham et al., 2020). Another study (Khojastehfar et al., 2020) revealed that Iranian ICU nurses’ practices in terms of PU prevention were favorable. The differences in findings among these studies could be attributed to variations in the availability of protocols and facilities in different healthcare settings.
The current study revealed a relationship between the practice of PU and years of working in the ICU. The results revealed that nurses with 5 to 10 years of ICU experience were more likely to practice appropriate PU than those with more than 10 years of ICU experience. This experience-based difference in PU prevention practice among Iraqi ICU nurses calls for further investigation to identify its possible underlying causes.
Conclusion
This study highlights insufficient knowledge, unfavorable attitudes, and suboptimal practice in PU prevention among ICU nurses in Al-Basrah and Dhi-Qar cities, Iraq. Proactive planning and targeted training initiatives are necessary to improve healthcare quality. Efficient in-service nursing programs should be developed to provide comprehensive information to enhance nurses’ knowledge about PU prevention. Also, cultivating a favorable attitude towards PU prevention through training will encourage nurses to prioritize this aspect of patient care, benefiting patients’ safety. Moreover, hands-on practice sessions should be incorporated to boost nurses’ confidence and competence in implementing PU prevention strategies. Considering the demanding nature of ICU work, these training programs should be designed to be efficient and practical.
This study was conducted in two cities in Iraq, which may limit the generalizability of the findings to other regions. Additionally, using a self-report questionnaire to measure nurses’ practice and the study’s cross-sectional nature are considered among the limitations. To overcome these limitations, we recommended that future studies consider measuring nurses’ practice through direct observation, which can provide more objective data.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Iran University of Medical Sciences (IUMS) (Code: IR.IUMS.REC.1401.648). Necessary permissions were obtained from the Faculty of Nursing and IUMS and the Al-Basra and Dhi-Qar Health Directorates. Written informed consent was obtained from all study participants after thoroughly explaining the study objectives and process. It was emphasized that participation was entirely voluntary for all participants.
Funding
This article is a part of the research project approved by the Research Department of the International Campus at Iran University of Medical Sciences, Tehran, Iran, in 2022 (Code: 2022/1380; 2022-05-28).
Authors' contributions
Study design and data analysis: Tahereh Najafi Ghezeljeh, Sukaina Hafedh Ahmed, and Shima Haghani; Initial draft preparation: Tahereh Najafi Ghezeljeh, Sukaina Hafedh Ahmed, and Abdul Kareem Salman Khudhair; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers would like to express their gratitude to the officials and nursing staff of the following hospitals: Al-Basra Teaching Hospital, Al-Sadr Teaching Hospital, Al-Mawani Teaching Hospital, Al-Fayha Teaching Hospital, Al-Qurna General Hospital, Al-Mudaina General Hospital, Nasiriyah Teaching Hospital, and Nasiriyah Heart Center. Their cooperation and support were invaluable for the successful completion of this study.
References
Awoke, N., et al., 2022. Pressure injury prevention practice and associated factors among nurses at Wolaita Sodo University Teaching and Referral Hospital, South Ethiopia: A cross-sectional study. BMJ Open, 12(3), pp. e047687. [DOI:10.1136/bmjopen-2020-047687] [PMID]
Beeckman, D., et al., 2010. Pressure ulcers: Development and psychometric evaluation of the attitude towards pressure ulcer prevention instrument (APuP). International Journal of Nursing Studies, 47(11), pp. 1432–41. [DOI:10.1016/j.ijnurstu.2010.04.004] [PMID]
Beeckman, D., et al., 2010. Pressure ulcer prevention: Development and psychometric validation of a knowledge assessment instrument. International Journal of Nursing Studies, 47(4), pp. 399–410. [DOI:10.1016/j.ijnurstu.2009.08.010] [PMID]
Berihu, H., et al., 2020. Practice on pressure ulcer prevention among nurses in selected public hospitals, Tigray, Ethiopia. BMC Research Notes, 13(1), pp. 207. [DOI:10.1186/s13104-020-05049-7] [PMID]
Chaboyer, W. P., et al., 2018. Incidence and prevalence of pressure injuries in adult intensive care patients: A systematic review and meta-analysis. Critical Care Medicine, 46(11), pp. e1074–81. [DOI:10.1097/CCM.0000000000003366] [PMID]
Demarré, L., et al., 2012. Pressure ulcers: Knowledge and attitude of nurses and nursing assistants in Belgian nursing homes. Journal of Clinical Nursing, 21(9-10), pp. 1425–34.[DOI:10.1111/j.1365-2702.2011.03878.x] [PMID]
Dilie, A. & Mengistu, D., 2015. Assessment of nurses’ knowledge, attitude, and perceived barriers to expressed pressure ulcer prevention practice in Addis Ababa government hospitals, Addis Ababa, Ethiopia, 2015. Advances in Nursing, 2015. [DOI:10.1155/2015/796927]
Malinga, S. & Dlungwane, T., 2020. Nurses’ knowledge, attitudes and practices regarding pressure ulcer prevention in the Umgungundlovu District, South Africa. Africa Journal of Nursing And Midwifery, 22(2), pp. 17. [DOI:10.25159/2520-5293/7691]
Finkelman, A. & Kenner, C. 2014. Professional nursing concepts: competencies for quality leadership, Burlington, Jones & Bartlett. [Link]
Grešš Halász, B., et al., 2021. Nurses’ knowledge and attitudes towards prevention of pressure Ulcers. International Journal of Environmental Research and Public Health, 18(4), pp. 1705.[DOI:10.3390/ijerph18041705] [PMID]
Hu, L., Sae-Sia, W. & Kitrungrote, L., 2021. Intensive care nurses’ knowledge, attitude, and practice of pressure injury prevention in China: A cross-sectional study. Risk Management and Healthcare Policy, 14, pp. 4257–4267. [DOI:10.2147/RMHP.S323839] [PMID]
Hussein, R., Hazim Al Mukhtar, S. & Jabar Mahmmod, H., 2006. Nurses’ attitudes, towards bed sores prevention. College of Basic Education Researchers Journal, 4(2), pp. 203-15. [Link]
Ingwu, J., et al., 2019. Caregivers’ knowledge and practice toward pressure ulcer prevention in national orthopedic hospital, Enugu, Nigeria. Nigerian Journal of Clinical Practice, 22(7), pp. 1014–21. [DOI:10.4103/njcp.njcp_413_17] [PMID]
Khojastehfar, S., Najafi Ghezeljeh, T. & Haghani, S., 2020. Factors related to knowledge, attitude, and practice of nurses in intensive care unit in the area of pressure ulcer prevention: A multicenter study. Journal of Tissue Viability, 29(2), pp. 76–81.[DOI:10.1016/j.jtv.2020.02.002] [PMID]
Kim, J. Y. & LEE, Y. J., 2019. A study on the nursing knowledge, Attitude, and Performance towards pressure ulcer prevention among nurses in Korea long-term care facilities. International Wound Journal, 16 Suppl 1(Suppl 1), pp. 29–35. [DOI:10.1111/iwj.13021] [PMID]
Köse, I., et al., 2016. Knowledge of nurses working in intensive care units in relation to preventive interventions for pressure ulcer. International Journal of Caring Sciences, 9(2), pp. 677-86. [Link]
Jiang, L., Li, L. & Lommel, L., 2020. Nurses’ knowledge, attitudes, and behaviours related to pressure injury prevention: A large-scale cross-sectional survey in mainland China. Journal of Clinical Nursing, 29(17-18), pp. 3311-24. [DOI:10.1111/jocn.15358] [PMID]
Lee YJ. 2014. The Development and effectiveness of blended-learning program of pressure ulcer management [PhD Dissertation]. Seoul, South Korea: Yonsei University.
Li, J., et al., 2023. Critical care nurses’ knowledge, attitudes, and practices of pressure injury prevention in China: A multicentric cross-sectional survey. International Wound Journal, 20(2), pp. 381–90. [DOI:10.1111/iwj.13886] [PMID]
Moore, Z. E. & Patton, D., 2019. Risk assessment tools for the prevention of pressure ulcers. The Cochrane Database of Systematic Reviews, 1(1), pp. CD006471. [DOI:10.1002/14651858.CD006471.pub4] [PMID]
Nasreen, S., et al., 2017. Nurses knowledge and practices toward pressure ulcer prevention in general hospital Lahore. Saudi Journal of Medical and Pharmaceutical Sciences, 3(6), pp. 520-7. [Link]
Nuru, N., et al., 2015. Knowledge and practice of nurses towards prevention of pressure ulcer and associated factors in Gondar University Hospital, Northwest Ethiopia. BMC Nursing, 14, pp. 34. [DOI:10.1186/s12912-015-0076-8] [PMID]
Olsho, L. E., et al., 2014. Evaluation of AHRQ’s on-time pressure ulcer prevention program: A facilitator-assisted clinical decision support intervention for nursing homes. Medical Care, 52(3), pp. 258–66. [DOI:10.1097/MLR.0000000000000080] [PMID]
Sham, F., et al., 2020. Knowledge, practice and perceived barrier of pressure ulcer prevention among nurses in a public hospital in Selangor. Malaysian Journal of Public Health Medicine, 20(Special1), pp. 325-35. [DOI:10.37268/mjphm/vol.20/no.Special1/art.738]
Simonetti, V., et al., 2015. Nursing students’ knowledge and Attitude on pressure ulcer prevention evidence-based guidelines: A multicenter cross-sectional study. Nurse Education Today, 35(4), pp. 573–9. [DOI:10.1016/j.nedt.2014.12.020] [PMID]
Tirgari, B., Mirshekari, L. & Forouzi, M. A., 2018. Pressure injury prevention: Knowledge and attitudes of Iranian intensive care nurses. Advances in Skin & Wound Care, 31(4), pp. 1–8.[DOI:10.1097/01.ASW.0000530848.50085.ef] [PMID]
Yilmazer, T., Tüzer, H. & Erciyas, A., 2019. Knowledge and attitudes towards prevention of pressure ulcer: Intensive care units sample in Turkey. Turkiye Klinikleri Journal of Nursing Sciences, 11(2), pp. 140-7 [DOI:10.5336/nurses.2018-63157]
Zuo, X. L. & Meng, F. J., 2015. A care bundle for pressure ulcer treatment in intensive care units. International Journal of Nursing Sciences, 2(4), pp. 340-7. [DOI:10.1016/j.ijnss.2015.10.008]
Pressure ulcers (PUs) are localized injuries to the skin, underlying tissues, or both, usually over a bony prominence. It is caused by pressure alone or combined with shear and friction (Kim & Lee, 2019). The incidence of PU among intensive care unit (ICU) patients is even higher, ranging from 6.60% to 36.80% globally (Chaboyer et al., 2018). Patients in the ICU have a 4-time higher chance of developing PU, longer stays, and poor tissue perfusion (Yilmazer et al., 2019). According to the international PU prevalence survey, the medical ICU had the greatest prevalence (12.1%) of facility-acquired PU (Zuo & Meng, 2015).
Basically, PU is a severe burden for patients and clients of all ages, resulting in difficulties and issues such as discomfort, pain, and decreased quality of life (Grešš Halász et al., 2021). Developing PU can cause prolonged hospital stays and more significant costs for the healthcare system (Olsho et al., 2014). U causes complications for patients and increases their morbidity and mortality rates (Hu et al., 2021). Other serious consequences include delayed rehabilitation, prolonged illness, increased healthcare costs, disability, and death. These complications impose extensive supplies, nursing hours, and long-term physiotherapies (Ingwu et al., 2019). In addition, PU can increase the risk of infection (Grešš Halász et al., 2021). It is reported that up to 53% of PUs have become clinically infected, which can result in cellulitis, abscess, osteomyelitis, and bacteremia—all of which can lead to significant mortality (Hu et al., 2021). The incidence and prevention of PU represent a marker of quality of care and safety for healthcare organizations and facilities (Sham et al., 2020; Dlungwane, 2020).
Hence, increased attention to PU prevention is anticipated to improve patient care while also lowering the expenses associated with ICU treatment (Dilie & Mengistu, 2015). anagement and prevention of PU include regulations and auditing, the implementation of appropriate procedures, and the cooperation of healthcare providers (Dlungwane, 2020). The National Pressure Injury Advisory Panel (NPIAP) and European Pressure Ulcer Advisory Panel (EPUAP) developed guidelines for PU prevention (Dlungwane, 2020). Prevention and treatment of PUs require multidisciplinary collaboration (Ingwu et al., 2019). However, nurses’ roles are more significant as they are the frontline in providing patient care (Finkelman & Kenner, 2016).
The nurse’s primary role is to assess the individuals at risk, take measures to eliminate causative factors, and ensure a PU healing process (Nuru et al., 2015). PUs are a primary nurse-sensitive outcome, and nursing care significantly affects PU development and prevention (Sham et al., 2020). As nurses play a critical role in PU prevention and management, evaluating their knowledge, attitude, and practice in this area is paramount. Notably, nurses’ lack of knowledge, skills, and negative attitudes contribute significantly to the occurrence or worsening of PUs (Moore & Patton, 2019).
Previous studies in different countries that have focused on nurses’ knowledge, attitude, and practice regarding PU, yielded dissimilar results (Khojastehfar et al., 2020; Dlungwane, 2020; Ingwu et al., 2019; Awoke et al., 2022; Kim & Lee, 2019; Yilmazer et al., 2019; Hu et al., 2021). However, these findings cannot be generalized to the specific context of Iraq, where there is a lack of information in this field and only one related study has been found in Iraq. In that study, 100 nurses in an acute care setting reported a positive attitude toward PU prevention (Hussein et al., 2006). The researcher developed the instrument used in the study, but its validity and reliability have not been reported.
Given that evaluating ICU nurses’ current knowledge, attitude, and practice is critical for planning appropriate interventions and revising nursing education programs, this study was designed to investigate knowledge, attitude, and practice regarding PU prevention among ICU nursing staff in governmental (teaching and non-teaching) hospitals in Al-Basra and Dhi-Qar cities, Iraq.
Materials and Methods
In this cross-sectional study with a descriptive design, 231 ICU nursing staff in 8 governmental hospitals (6 hospitals in Al-Basra and 2 hospitals in Dhi-Qar), Iraq, were recruited through the census method. The study data were collected from August to September 2022 using electronic versions of a demographic form and questionnaires to assess pressure ulcer prevention knowledge, attitude, and practice. The questionnaires were designed using Google Forms and distributed through a WhatsApp group. Nurses’ cell phone numbers were obtained to form the WhatsApp group, and the questionnaires were shared via this platform. To encourage timely completion, reminder messages were sent to the nurses daily for a week.
Study instruments
Demographic questionnaire
This questionnaire was prepared by reviewing related texts, and its content validity was checked and confirmed by a group of experts, which consisted of three members of the Faculty of Nursing and Midwifery of Basra University. The demographic form included the variables of age, gender, marital status, education level, nursing work experience, ICU work experience, working hours per week, and the experience of participating in an in-service training program related to PU prevention within the last year.
Pressure ulcer prevention knowledge questionnaire
This questionnaire was developed by Beeckman et al. (2010) and modified by Lee et al. (2014). It includes 19 multiple-choice questions with three answer options. It reflects six domains expressing the most relevant aspects of PU prevention: Pathogenesis of PU (6 items), classification (3 items), risk assessment (1 item), nutrition (1 item), preventive strategy to reduce pressure and shear (4 items), and preventive strategy to reduce the time of exposure to pressure and shear (4 items). The total score ranges from 0 to 19, which means a higher knowledge of PU prevention (Beeckman et al., 2010). To determine the adequacy of nurses’ knowledge, a threshold of correctly answering 90% or more of the questions on the questionnaire was considered The original instrument demonstrated a Cronbach α 0.77 (Beeckman et al., 2010). Another study reported its Cronbach α as 0.73 (Kim & Lee, 2019).
In this study, the questionnaire underwent a translation and back translation method for cross-cultural adaptation. A translator familiar with medical concepts translated the original text into Arabic to achieve this. Subsequently, the translated Arabic version was independently translated back into English by a bilingual specialist who had no prior knowledge of the original questionnaire. Following this, the researchers compared the translated and original versions to ensure accuracy and finalized the questionnaire for psychometric evaluation. To assess the content validity of the Arabic version of the questionnaire, a panel of experts consisting of three faculty members from the School of Nursing and Midwifery at Basra University reviewed it. Their input and feedback were taken into consideration during the adaptation process. In the studied population, the internal consistency of the questionnaire was measured using the Kuder-Richardson 20 coefficient, resulting in a value of 0.67. This value indicates that the questionnaire demonstrated an appropriate level of internal consistency.
Attitude towards pressure ulcers prevention questionnaire
This questionnaire, developed by Beeckman et al. (2010), has 13 questions. Nurses indicated their attitude using a 4-point Likert scale (1=strongly disagree, 2=disagree, 3=agree, 4=strongly agree). It is important to note that the scoring is inverse for some items (3, 5, 7, 10, and 13) in the questionnaire. The total score ranged from 13 to 52. Higher scores indicate a more favorable attitude. In particular, the attitude was considered favorable if its mean score was more than or equal to 75% of the maximum score, which was 39 (Beeckman et al., 2010). The questionnaire has 5 subscales: Personal competence to prevent PU, priority of PU prevention, impact of PU, responsibility in PU prevention, and confidence in the effectiveness of prevention. A study confirmed its content validity, and its Cronbach α coefficient was also reported to be 0.88 (Simonetti et al., 2015). In this study, the translation was done in the same way as the knowledge questionnaire. In the studied population, the internal consistency of the questionnaire was measured using the Cronbach α coefficient, resulting in a value of 0.71.
The practice of pressure ulcerprevention questionnaire
This self-report questionnaire, which was developed by Nasreen et al. (2017), has 20 items and scores on a 3-point Likert scale from “always”=2 to “never”=0 to measure people’s practice concerning PU prevention. The total score ranges from 0 to 40, and a higher score indicates better practice of nurses in preventing PU. The practice was considered favorable if its mean score was more than or equal to 90% of the maximum score, which was 36 (Nasreen et al., 2017). In a study on nurses, the Cronbach α coefficient was reported to be 0.95 (Nuru et al., 2015). The translation and back translation of this tool was similar to the knowledge questionnaire. In the studied population, the internal consistency of the questionnaire was measured using the Cronbach α coefficient, resulting in a value of 0.78.
Data analysis
The Excel output of the Google Form was taken and transferred to SPSS software, version 22, for analysis. The data was analyzed by descriptive and inferential statistical tests in SPSS software, version 22. The scores of the main variables were rescaled to a range of 0 to 100. Descriptive (absolute and relative frequency, Mean±SD) and inferential statistics (the independent t-test, chi-square test, and Fisher exact test) were used to analyze the data per the research objectives. The Kolmogorov-Smirnov test was used to evaluate the normal distribution of the variables. The significance level was considered <0.05. The tables related to the frequency distribution of the knowledge, attitude, and practice questionnaire items were attached in a supplementary file.
Results
According to Table 1, the majority of the subjects (66.2%) were <30 years old; more than half of them (53.7%) were female and married (52.4%). Most samples (61.0%) had a BSc, 51.9% of the subjects had less than 5 years of practical experience in nursing, and more than half of the samples (73.2%) had less than 5 years of practical experience in ICU. The results revealed that 88.3% of the subjects worked 50 hours or less weekly. Finally, Table 1 shows that 56.7% of the samples have participated in an in-service training program.

Table 2 presents the mean scores of different domains of knowledge. The lowest mean score (24.24±42.94) was related to “risk assessment”, whereas the highest mean score (36.36±27.19) was obtained for “knowledge about PU classification”. The vast majority of the nurses (93.5%) responded incorrectly to the item “repositioning is an accurate preventive method because the duration of pressure and shear will be reduced” in the knowledge questionnaire. The lowest percentage of incorrect answers (38.5%) was related to the item “Fewer patients will have PU if patients are mobilized”. The knowledge of all nurses was insufficient and weak because they had answered less than 90% of the questions correctly.
Based on Table 3, the staff attitude towards the impact of PU received the lowest mean score (45.79±13.71), while the highest mean score was recorded for confidence in the effectiveness of prevention (72.00±19.42). The total mean attitude score was found to be 35.52±3.97. Additionally, the attitude of most nurses (79.7%) was unfavorable. The nurses’ attitudes related to the item “The impact of pressure ulcers on a patient should not be exaggerated” had the lowest mean score (1.79±0.75). In contrast, the highest mean score (3.50±0.73) was related to the item “pressure ulcers are never preventable”.

According to Table 4, most nurses in the study (97%) demonstrated unfavorable levels of practice in PU prevention (24.26±5.68). In the practice questionnaire, the item “I perform lab test for assessing nutritional status followed by physician’s instruction” had the lowest mean score (0.73±0.74). In contrast, the highest mean score (1.57±0.62) was related to the item “I use special mattress to prevent pressure loadings, such as foam, air”.
The results of the independent t-test (Table 1) revealed a significant relationship between the nurses’ knowledge about PU and participation in an in-service training program (P=0.021). Nurses who underwent PU training exhibited higher knowledge levels compared to their counterparts who did not participate in such training. Furthermore, the findings in Table 1 indicated a significant relationship between the mean score of practice and years of practical experience in the ICU (P=0.017). A Tukey test further disclosed that nurses with 5 to 10 years of ICU experience were more likely to practice PU optimally than those with more than 10 years of ICU experience (P=0.013).
Discussion
According to the results, the nursing staff in this study lacked proper knowledge and had unfavorable attitudes and practices regarding PU.
In this study, nurses’ knowledge was low in total and all dimensions. The low level of knowledge among ICU nurses regarding PU can be attributed to the lack of attention to PU in nursing education and in-service training programs. This study revealed that more than half of the nurses had not participated in any training program. Nurses’ busy schedules might also be an issue, preventing them from engaging in training programs. Given the importance of prevention in caring for patients at risk of developing PU, nurses’ proper knowledge plays a crucial role. Therefore, healthcare facility managers should take necessary measures to empower the healthcare team, especially nurses, as PU poses a significant risk to patient safety. By providing adequate training and educational opportunities, healthcare facilities can enhance the knowledge and expertise of their nursing staff in PU prevention and management.
The findings revealed a significant relationship between knowledge about PU and participation in an in-service training program on PU. Nurses who underwent PU training exhibited higher knowledge levels compared to those who did not receive such training. This finding emphasizes the importance of education and its effectiveness in enhancing nurses’ understanding of PU. To make these educational programs successful, careful planning is essential to address the specific educational needs of nurses.
The present study findings are in line with previous studies. A cross-sectional survey by Jiang et al. (2020) in China showed that 41.7% of nurses had insufficient knowledge regarding PU prevention. Similarly, a cross-sectional descriptive study in China by Li et al. (2023) revealed that critical care nurses’ knowledge about PU was assessed as insufficient. Another study reported that Belgian nurses in nursing homes had low levels of knowledge about PU (Demarré et al., 2012). Another study indicated that the knowledge of Iranian ICU nurses was insufficient (Khojastehfar et al., 2020), though nurses had more knowledge than the present study. Contrary to the present study’s findings, a descriptive cross-sectional survey by Köse & Öztunc (2016) showed that most participants had good knowledge about PU preventative strategies. This difference in findings may be attributed to variations in the scales used to assess knowledge levels and the threshold score set to define sufficient knowledge.
The present study revealed that the attitudes of most nurses, both total and across all dimensions, were unfavorable. This unfavorable attitude among ICU nurses can be attributed to their lack of knowledge about the effects of PU. Nurses must recognize PU as a significant patient safety indicator and be aware of its potential harm and detrimental impact on patients. By understanding the seriousness of PU, nurses can take proactive measures to prevent its development and effectively manage at-risk patients. Addressing these unfavorable attitudes is essential for promoting evidence-based practice among healthcare professionals (Simonetti et al., 2015). Proper interventions are needed to change nurses’ attitudes; education can influence these changes. Nursing administrators should develop programs to increase ICU nurses’ confidence in PU prevention (Hu et al., 2021).
In line with the current research, a cross-sectional survey by Jiang et al. (2020) revealed that nurses’ attitudes were unfavorable. Similarly, the present study aligns with research indicating that most Iranian nurses are unfavorable toward PU prevention (Khojastehfar et al., 2020). However, it is noteworthy that in that study, the mean score of attitude was higher than the current research. Another study, inconsistent with our findings, indicated moderate nurses’ attitudes toward PU prevention (Tirgari et al., 2018). This difference can be attributed to the differences in instruments used to assess attitudes and the fact that the current research explicitly focused on ICU nurses.
The results showed that ICU nurses’ practice regarding PU was unfavorable. This finding could be attributed to the fact that the ICU nurses in this study had insufficient knowledge about PU and unfavorable attitudes regarding its prevention. Consequently, their practice in preventing PU may have been adversely affected. Enhancing nurses’ knowledge and attitudes through targeted education and interventions could improve their practice and ultimately improve PU prevention outcomes.
In line with the study, the results of two studies revealed that more than 82% of nurses’ practices were unfavorable in terms of preventing PU (Nasreen et al., 2017; Berihu et al., 2020). Contrary to the findings of this study, a descriptive cross-sectional study showed that most nurses have favorable practices for preventing PU (Sham et al., 2020). Another study (Khojastehfar et al., 2020) revealed that Iranian ICU nurses’ practices in terms of PU prevention were favorable. The differences in findings among these studies could be attributed to variations in the availability of protocols and facilities in different healthcare settings.
The current study revealed a relationship between the practice of PU and years of working in the ICU. The results revealed that nurses with 5 to 10 years of ICU experience were more likely to practice appropriate PU than those with more than 10 years of ICU experience. This experience-based difference in PU prevention practice among Iraqi ICU nurses calls for further investigation to identify its possible underlying causes.
Conclusion
This study highlights insufficient knowledge, unfavorable attitudes, and suboptimal practice in PU prevention among ICU nurses in Al-Basrah and Dhi-Qar cities, Iraq. Proactive planning and targeted training initiatives are necessary to improve healthcare quality. Efficient in-service nursing programs should be developed to provide comprehensive information to enhance nurses’ knowledge about PU prevention. Also, cultivating a favorable attitude towards PU prevention through training will encourage nurses to prioritize this aspect of patient care, benefiting patients’ safety. Moreover, hands-on practice sessions should be incorporated to boost nurses’ confidence and competence in implementing PU prevention strategies. Considering the demanding nature of ICU work, these training programs should be designed to be efficient and practical.
This study was conducted in two cities in Iraq, which may limit the generalizability of the findings to other regions. Additionally, using a self-report questionnaire to measure nurses’ practice and the study’s cross-sectional nature are considered among the limitations. To overcome these limitations, we recommended that future studies consider measuring nurses’ practice through direct observation, which can provide more objective data.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Iran University of Medical Sciences (IUMS) (Code: IR.IUMS.REC.1401.648). Necessary permissions were obtained from the Faculty of Nursing and IUMS and the Al-Basra and Dhi-Qar Health Directorates. Written informed consent was obtained from all study participants after thoroughly explaining the study objectives and process. It was emphasized that participation was entirely voluntary for all participants.
Funding
This article is a part of the research project approved by the Research Department of the International Campus at Iran University of Medical Sciences, Tehran, Iran, in 2022 (Code: 2022/1380; 2022-05-28).
Authors' contributions
Study design and data analysis: Tahereh Najafi Ghezeljeh, Sukaina Hafedh Ahmed, and Shima Haghani; Initial draft preparation: Tahereh Najafi Ghezeljeh, Sukaina Hafedh Ahmed, and Abdul Kareem Salman Khudhair; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers would like to express their gratitude to the officials and nursing staff of the following hospitals: Al-Basra Teaching Hospital, Al-Sadr Teaching Hospital, Al-Mawani Teaching Hospital, Al-Fayha Teaching Hospital, Al-Qurna General Hospital, Al-Mudaina General Hospital, Nasiriyah Teaching Hospital, and Nasiriyah Heart Center. Their cooperation and support were invaluable for the successful completion of this study.
References
Awoke, N., et al., 2022. Pressure injury prevention practice and associated factors among nurses at Wolaita Sodo University Teaching and Referral Hospital, South Ethiopia: A cross-sectional study. BMJ Open, 12(3), pp. e047687. [DOI:10.1136/bmjopen-2020-047687] [PMID]
Beeckman, D., et al., 2010. Pressure ulcers: Development and psychometric evaluation of the attitude towards pressure ulcer prevention instrument (APuP). International Journal of Nursing Studies, 47(11), pp. 1432–41. [DOI:10.1016/j.ijnurstu.2010.04.004] [PMID]
Beeckman, D., et al., 2010. Pressure ulcer prevention: Development and psychometric validation of a knowledge assessment instrument. International Journal of Nursing Studies, 47(4), pp. 399–410. [DOI:10.1016/j.ijnurstu.2009.08.010] [PMID]
Berihu, H., et al., 2020. Practice on pressure ulcer prevention among nurses in selected public hospitals, Tigray, Ethiopia. BMC Research Notes, 13(1), pp. 207. [DOI:10.1186/s13104-020-05049-7] [PMID]
Chaboyer, W. P., et al., 2018. Incidence and prevalence of pressure injuries in adult intensive care patients: A systematic review and meta-analysis. Critical Care Medicine, 46(11), pp. e1074–81. [DOI:10.1097/CCM.0000000000003366] [PMID]
Demarré, L., et al., 2012. Pressure ulcers: Knowledge and attitude of nurses and nursing assistants in Belgian nursing homes. Journal of Clinical Nursing, 21(9-10), pp. 1425–34.[DOI:10.1111/j.1365-2702.2011.03878.x] [PMID]
Dilie, A. & Mengistu, D., 2015. Assessment of nurses’ knowledge, attitude, and perceived barriers to expressed pressure ulcer prevention practice in Addis Ababa government hospitals, Addis Ababa, Ethiopia, 2015. Advances in Nursing, 2015. [DOI:10.1155/2015/796927]
Malinga, S. & Dlungwane, T., 2020. Nurses’ knowledge, attitudes and practices regarding pressure ulcer prevention in the Umgungundlovu District, South Africa. Africa Journal of Nursing And Midwifery, 22(2), pp. 17. [DOI:10.25159/2520-5293/7691]
Finkelman, A. & Kenner, C. 2014. Professional nursing concepts: competencies for quality leadership, Burlington, Jones & Bartlett. [Link]
Grešš Halász, B., et al., 2021. Nurses’ knowledge and attitudes towards prevention of pressure Ulcers. International Journal of Environmental Research and Public Health, 18(4), pp. 1705.[DOI:10.3390/ijerph18041705] [PMID]
Hu, L., Sae-Sia, W. & Kitrungrote, L., 2021. Intensive care nurses’ knowledge, attitude, and practice of pressure injury prevention in China: A cross-sectional study. Risk Management and Healthcare Policy, 14, pp. 4257–4267. [DOI:10.2147/RMHP.S323839] [PMID]
Hussein, R., Hazim Al Mukhtar, S. & Jabar Mahmmod, H., 2006. Nurses’ attitudes, towards bed sores prevention. College of Basic Education Researchers Journal, 4(2), pp. 203-15. [Link]
Ingwu, J., et al., 2019. Caregivers’ knowledge and practice toward pressure ulcer prevention in national orthopedic hospital, Enugu, Nigeria. Nigerian Journal of Clinical Practice, 22(7), pp. 1014–21. [DOI:10.4103/njcp.njcp_413_17] [PMID]
Khojastehfar, S., Najafi Ghezeljeh, T. & Haghani, S., 2020. Factors related to knowledge, attitude, and practice of nurses in intensive care unit in the area of pressure ulcer prevention: A multicenter study. Journal of Tissue Viability, 29(2), pp. 76–81.[DOI:10.1016/j.jtv.2020.02.002] [PMID]
Kim, J. Y. & LEE, Y. J., 2019. A study on the nursing knowledge, Attitude, and Performance towards pressure ulcer prevention among nurses in Korea long-term care facilities. International Wound Journal, 16 Suppl 1(Suppl 1), pp. 29–35. [DOI:10.1111/iwj.13021] [PMID]
Köse, I., et al., 2016. Knowledge of nurses working in intensive care units in relation to preventive interventions for pressure ulcer. International Journal of Caring Sciences, 9(2), pp. 677-86. [Link]
Jiang, L., Li, L. & Lommel, L., 2020. Nurses’ knowledge, attitudes, and behaviours related to pressure injury prevention: A large-scale cross-sectional survey in mainland China. Journal of Clinical Nursing, 29(17-18), pp. 3311-24. [DOI:10.1111/jocn.15358] [PMID]
Lee YJ. 2014. The Development and effectiveness of blended-learning program of pressure ulcer management [PhD Dissertation]. Seoul, South Korea: Yonsei University.
Li, J., et al., 2023. Critical care nurses’ knowledge, attitudes, and practices of pressure injury prevention in China: A multicentric cross-sectional survey. International Wound Journal, 20(2), pp. 381–90. [DOI:10.1111/iwj.13886] [PMID]
Moore, Z. E. & Patton, D., 2019. Risk assessment tools for the prevention of pressure ulcers. The Cochrane Database of Systematic Reviews, 1(1), pp. CD006471. [DOI:10.1002/14651858.CD006471.pub4] [PMID]
Nasreen, S., et al., 2017. Nurses knowledge and practices toward pressure ulcer prevention in general hospital Lahore. Saudi Journal of Medical and Pharmaceutical Sciences, 3(6), pp. 520-7. [Link]
Nuru, N., et al., 2015. Knowledge and practice of nurses towards prevention of pressure ulcer and associated factors in Gondar University Hospital, Northwest Ethiopia. BMC Nursing, 14, pp. 34. [DOI:10.1186/s12912-015-0076-8] [PMID]
Olsho, L. E., et al., 2014. Evaluation of AHRQ’s on-time pressure ulcer prevention program: A facilitator-assisted clinical decision support intervention for nursing homes. Medical Care, 52(3), pp. 258–66. [DOI:10.1097/MLR.0000000000000080] [PMID]
Sham, F., et al., 2020. Knowledge, practice and perceived barrier of pressure ulcer prevention among nurses in a public hospital in Selangor. Malaysian Journal of Public Health Medicine, 20(Special1), pp. 325-35. [DOI:10.37268/mjphm/vol.20/no.Special1/art.738]
Simonetti, V., et al., 2015. Nursing students’ knowledge and Attitude on pressure ulcer prevention evidence-based guidelines: A multicenter cross-sectional study. Nurse Education Today, 35(4), pp. 573–9. [DOI:10.1016/j.nedt.2014.12.020] [PMID]
Tirgari, B., Mirshekari, L. & Forouzi, M. A., 2018. Pressure injury prevention: Knowledge and attitudes of Iranian intensive care nurses. Advances in Skin & Wound Care, 31(4), pp. 1–8.[DOI:10.1097/01.ASW.0000530848.50085.ef] [PMID]
Yilmazer, T., Tüzer, H. & Erciyas, A., 2019. Knowledge and attitudes towards prevention of pressure ulcer: Intensive care units sample in Turkey. Turkiye Klinikleri Journal of Nursing Sciences, 11(2), pp. 140-7 [DOI:10.5336/nurses.2018-63157]
Zuo, X. L. & Meng, F. J., 2015. A care bundle for pressure ulcer treatment in intensive care units. International Journal of Nursing Sciences, 2(4), pp. 340-7. [DOI:10.1016/j.ijnss.2015.10.008]
Type of Study: Research |
Subject:
Special
Received: 2023/02/9 | Accepted: 2023/10/25 | Published: 2024/05/1
Received: 2023/02/9 | Accepted: 2023/10/25 | Published: 2024/05/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |