Tue, Jul 1, 2025
[Archive]
Volume 9, Issue 4 (Autumn 2023)
JCCNC 2023, 9(4): 297-308 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Raygan L, Jahani S, Elahi N, Maraghi E, Fakoor M, Najafi S. The Impact of Self-acupressure on the Pain, Joint Stiffness, and Physical Functioning of Patients With Knee Osteoarthritis. JCCNC 2023; 9 (4) :297-308
URL: http://jccnc.iums.ac.ir/article-1-467-en.html
URL: http://jccnc.iums.ac.ir/article-1-467-en.html
1- Student Research Committee, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
2- Nursing Care Research Center in Chronic Diseases, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,jahanisimin50@yahoo.com
3- Nursing Care Research Center in Chronic Diseases, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
4- Department of Biostatistics and Epidemiology, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
5- Department of Orthopedics, School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
6- Department of Medical and Surgical Nursing, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
2- Nursing Care Research Center in Chronic Diseases, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,
3- Nursing Care Research Center in Chronic Diseases, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
4- Department of Biostatistics and Epidemiology, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
5- Department of Orthopedics, School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
6- Department of Medical and Surgical Nursing, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
Full-Text [PDF 1508 kb]
(512 Downloads)
| Abstract (HTML) (1698 Views)
Osteoarthritis of the knee joint leads to pain and stiffness and impairs physical performance by reducing the knee’s range of motion.
• Self-acupressure reduces the intensity of pain and joint stiffness in people with knee osteoarthritis.
• Self-acupressure increases physical performance in people with knee osteoarthritis.
• Self-acupressure reduces the use of analgesics in people with knee osteoarthritis.
Plain Language Summary
Knee osteoarthritis presents as one of the common causes of pain in people over 40. However, acupressure may be beneficial for several pain conditions. Our study showed that self-acupressure reduces pain intensity and joint stiffness and improves knee movements in older adults with knee osteoarthritis. This easy and affordable method is suggested to be used by this group of people to manage the symptoms of knee osteoarthritis.
• Self-acupressure reduces the intensity of pain and joint stiffness in people with knee osteoarthritis.
• Self-acupressure increases physical performance in people with knee osteoarthritis.
• Self-acupressure reduces the use of analgesics in people with knee osteoarthritis.
Plain Language Summary
Knee osteoarthritis presents as one of the common causes of pain in people over 40. However, acupressure may be beneficial for several pain conditions. Our study showed that self-acupressure reduces pain intensity and joint stiffness and improves knee movements in older adults with knee osteoarthritis. This easy and affordable method is suggested to be used by this group of people to manage the symptoms of knee osteoarthritis.
Full-Text: (312 Views)
1. Introduction
Osteoarthritis or rheumatoid arthritis is a painful condition caused by the gradual loss of joint cartilage associated with inflammation. Osteoarthritis often affects the hands, knees, and spine. The patients experience general symptoms, such as pain, stiffness, and movement difficulties (Zeddou, 2019). Approximately 1 in 4 people in the UK complain of knee pain, most often due to osteoarthritis (Weber et al., 2019). In Iran, the incidence rates of knee arthritis in the age group of 15-85 years are 15.3% in urban population and 19.3% in rural population (Abedian et al., 2015). As the aging population increases, the prevalence of osteoarthritis increases, resulting in a growing concern regarding its indirect costs (Safiri et al., 2020; Ruiz Iban et al., 2018). Chronic knee pain adversely affects daily routine and quality of life in 25% of adults (Levinger et al., 2017). The resulting pain is one of the causes of disability among people over 50 years old (Weber et al., 2019). Needless to say that pain represents one of the priorities to be addressed (Covey & Shmerling, 2021). The patients constantly complain of pain originating from multiple regions (Weber et al., 2019). This chronic pain leads to inadequate activity, limited participation in activities of daily living (ADL), and reduced physical functioning. It also damages the quality of life, mood, and sleep, leading to fatigue. People with chronic pain have the lowest quality of life compared with other patients. This condition usually accompanies the feeling of hopelessness and doubles the risk of suicide compared to people without chronic pain. In the United States alone, approximately 15 million people complain of their poor quality of life due to pain (Safiri et al., 2020).
Acupressure is an alternative therapy usually employed in conjunction with acupuncture or reflexology. Acupressure is an ancient Chinese method based on the belief in the human body’s flow of vital energy called QI (or Chi, life energy). The energy flows in body channels, regulated by the individual’s body system. The unbalanced flow of QI results in the disease. Stimulation and pressure on specific body points open the channels, regulate energy flow, and balance the QI energy in the body, thus restoring health (Li et al., 2016).
Furthermore, applying acupressure in specific trigger points is believed to transmit pleasant beats to the brain 4 times faster than painful stimulants, blocking neural impulses’ path and preventing slower pain messages from reaching the brain. This technique helps improve or strengthen the threshold of pain perception in the body. In addition, mechanical pressure such as massaging and acupressure reduces tissue adhesion, stimulates relaxation, increases local blood circulation, increases parasympathetic nerve activity, increases muscle temperature, and reduces neuromuscular irritability (Sharif Nia et al., 2017). Acupressure can be performed by nurses, midwives, and even patients themselves if they are appropriately trained (Yu et al., 2019; Shariati et al., 2012).
Positive effects of acupressure have already been reported for various conditions, such as pain in primary dysmenorrhea (Mehta et al., 2017; Tiwari et al., 2016), severe back pain in patients with ankylosing spondylitis (Yang et al., 2017), extreme fatigue in women with multiple sclerosis (Bastani et al., 2015), the pain and fatigue in patients with chronic heart failure (Shafiee-Darabi et al., 2015), and the sleep quality of hemodialysis patients (Shariati et al., 2012). Some advantages of self-acupressure are flexibility in time and place, low intervention cost, empowering the patient, and increasing self-care. This therapy is also safe and acceptable from the patient’s perspective, as it can be implemented at home and reduces health care costs (Sharif Nia et al., 2017). Even studies that reported no positive outcome have suggested repeating the research with larger populations (Zhang et al., 2012; Li et al, 2018; Gupta et al., 2019).
Therefore, this study was performed to determine the impact of self-acupressure on pain, joint stiffness, and physical performance of patients with knee osteoarthritis.
2. Materials and Methods
Study design, setting, and sample
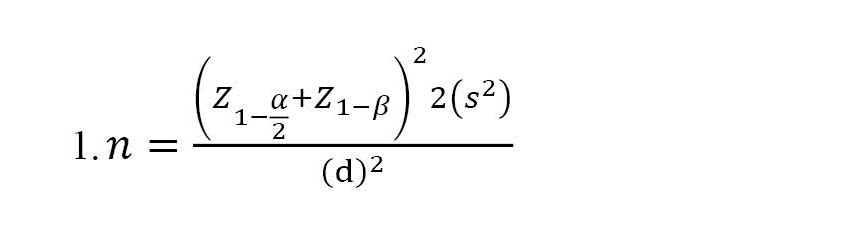
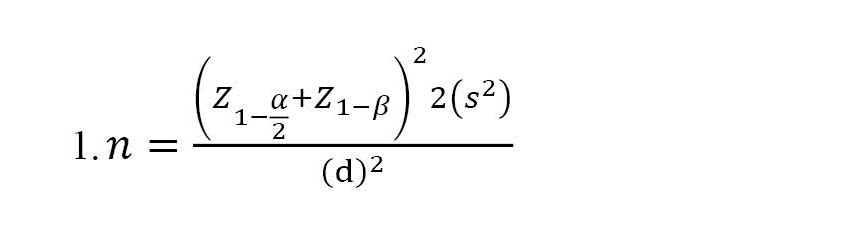
The present study was a controlled randomized clinical trial with three groups (intervention, sham, and control). The subjects were selected from the patients referred to the Ahvaz Imam Khomeini Hospital, as well as the patients who had been referred to the orthopedic private clinics in Khuzestan Province, Iran. According to the purpose of the research and a previous study (Li et al., 2016), considering β=0.2, α=0.05, s=3.3, and d=2.1, as well as a potential 20% sample attrition, the sample size was estimated at 26 subjects for each group (78 subjects in total) using the Equation 1:
The inclusion criteria included patients with a confirmed diagnosis of osteoarthritis by an orthopedist, 50 to 70 years old, with severe knee pain (a score above 3 on the VAS), not under other complementary medicine treatments or meditation techniques such as yoga and relaxation, without knee injuries preventing acupressure in that point, no rheumatoid arthritis or lupus, and the ability to learn and perform the intervention. The exclusion criteria were as follows: Not applying continuous acupressure according to the program, requiring surgery during the intervention, doing the intervention less than 5 days a week, and unwillingness to continue the program.
The subjects were randomly assigned to three groups through permutated block randomization with a block size of 4, using a table of random permutations. A statistician prepared the randomization list. According to the randomization list, the intervention instructions were placed in a sealed envelope by someone outside the study, unaware of the research objectives. He offered the envelopes to the patients according to the corresponding codes. The subjects were randomly allocated into three groups: Self-acupressure (n=26), sham (n=26), and control (n=26) (Figure 1).

Instruments
Demographic information questionnaire
This questionnaire gathers information about gender, age, height and weight, marital status, level of education, body mass index (BMI), duration of the osteoarthritis, and other underlying diseases of the patient. The questionnaire was assessed by 10 faculty members of the School of Nursing and Midwifery, Ahvaz University of Medical Sciences, and their comments were applied.
The Western Ontario and McMaster Universities osteoarthritis index (WOMAC)
This index was developed for patients with knee pain and includes 24 questions and 3 sections: The presence of pain, joint stiffness, and daily functioning. The first part contains 5 questions about the presence of pain while doing some tasks. The second part deals with the symptoms and joint stiffness with 2 questions about knee swelling, a feeling of rubbing or extra noise in the knee, the ability to flex and extend the knee, and the degree of joint dryness at the beginning of the morning and the end of the day after activity. The third part examines the difficulty in daily tasks and functional activities. It includes 17 questions relating to activities like going down and up the stairs, changing the position from sitting to standing, picking up an object from the ground, walking, getting in and out of the car, going shopping, putting on and taking off socks, getting up and lying down in bed, getting in and out of the bathroom, going in and out of the toilet, carrying heavy objects and doing light household chores like dusting. The questions of this index are scored on a scale of 0 to 4: None (0), mild (1), moderate (2), severe (3) and extreme (4). The subscale scores range from 0-20 for pain, 0-8 for stiffness, and 0-68 for physical function. The sum of all three subscale scores gives a total WOMAC score, and higher scores indicate greater severity of the patient’s symptoms. Different studies have used the WOMAC index (Li et al., 2018). The reliability of this index has been confirmed in the Netherlands with a Cronbach α coefficient of 0.88 (Bilbao et al., 2011). The reliability of the Persian version of this index has been confirmed in a pilot study on 10 elderly subjects with a Cronbach α coefficient of 0.963 (Bastani et al., 2015). The patients in all three groups completed the WOMAC index before the intervention and at the end of the fourth and eighth weeks of the study period.
Visual analog scale (VAS)
This scale is widely known and frequently used in various studies to assess pain intensity, in which samples choose a number between 0 and 10 for pain intensity based on their personal feelings (Yu et al., 2019). All three groups completed the VAS before the intervention and every week during the study period for 8 consecutive weeks via telephone interviews.
The analgesics checklist
This checklist was employed to determine the patient’s use of analgesics, including the type of medicine and the prescribed dose. After being prepared by the researcher, this checklist was approved by the faculty members of the Nursing and Midwifery School of Ahvas Jundishapur University of Medical Sciences. All three groups completed the analgesics checklist every day during the study period for 8 consecutive weeks via telephone interviews.
Study procedure
To teach the intervention to the patients, first, the researcher learned the necessary skills to perform the acupressure method under the supervision of a physical medicine and rehabilitation specialist. The procedure’s method is that patients first sit on a chair or the edge of the bed and determine the 5 desired points around their knee (Figure 2). The patients must hold the injured knee with their hand for 3 minutes and massage the area without gloves and without using oil or ointment so that they feel that the desired area is heated. Then, they should apply pressure to each specified point with their thumb for one minute. The method of applying pressure is 5 seconds and 5 seconds of rest in each of the 5 points. This action continues for 1 minute and then is repeated at the next point for one minute. This procedure should be done once a day for 8 consecutive weeks. The training of patients in the sham group was the same as the intervention group, with the difference that the points related to acupressure were taught to this group with a difference of 1 cm higher than the patients in the intervention group. Feedback was received from them to check the accuracy of learning. The control group received no intervention.

Data analysis
The obtained data were analyzed using the chi-square test, one-way analysis of variance (ANOVA), nonparametric ANOVA (Kruskal-Wallis), and repeated measures ANOVA in SPSS software, version 20. A generalized linear model (GLM) test was performed to eliminate the effect of confounding factors of gender. The significance level of the tests was considered at P<0.05.
3. Results
A total of 78 people participated in the study. Three subjects were excluded during the study (one due to joint replacement surgery and the other two due to not consistently performing acupressure as scheduled). Finally, the data of 75 subjects were analyzed. Twenty-seven subjects were in the intervention group, 23 in the sham group, and 25 in the control group (Figure 1). The demographic characteristics of the groups are presented and compared in Table 1. Except for the significant gender difference (P=0.012) between the three groups, their personal and disease characteristics were comparable.
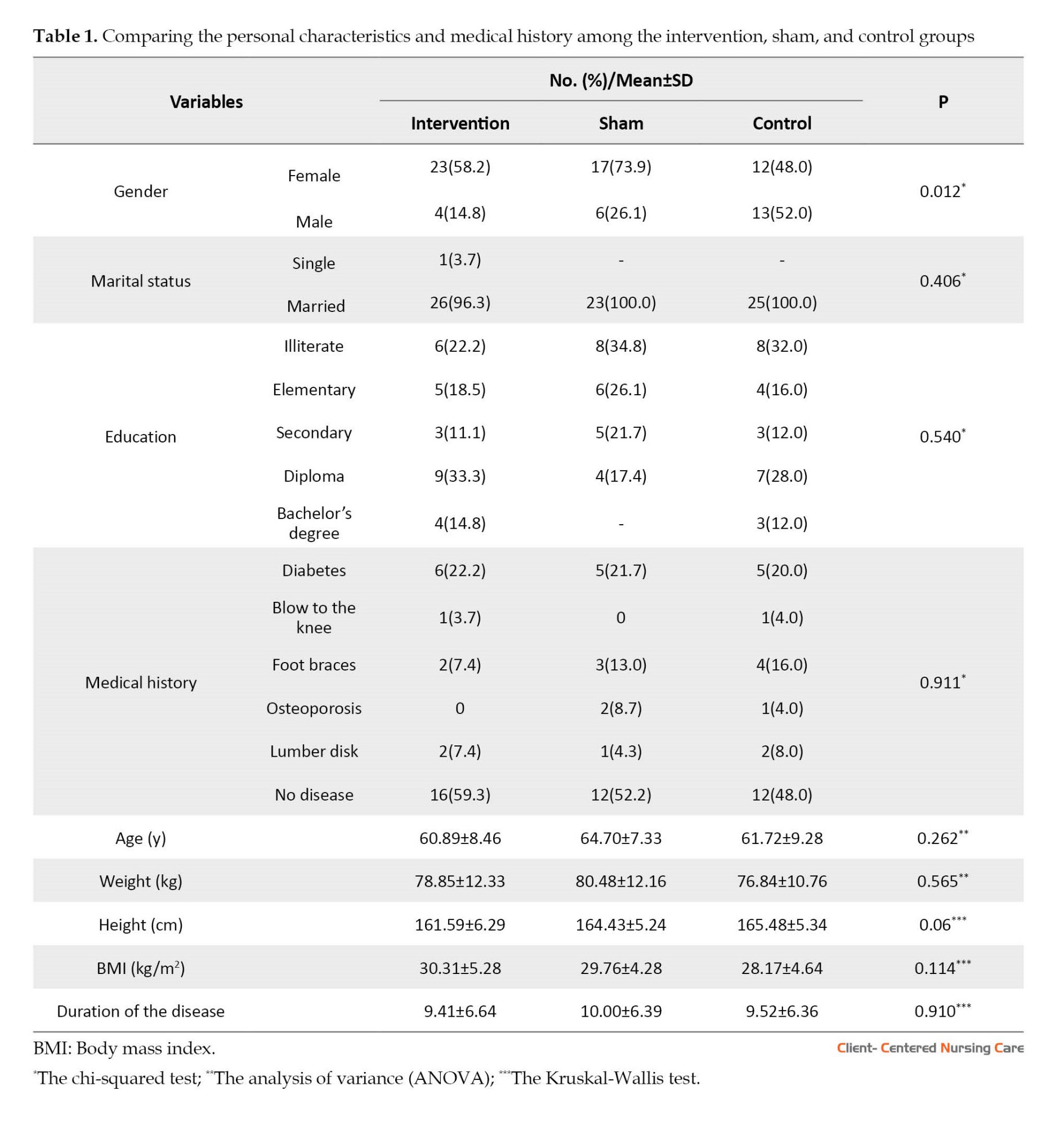
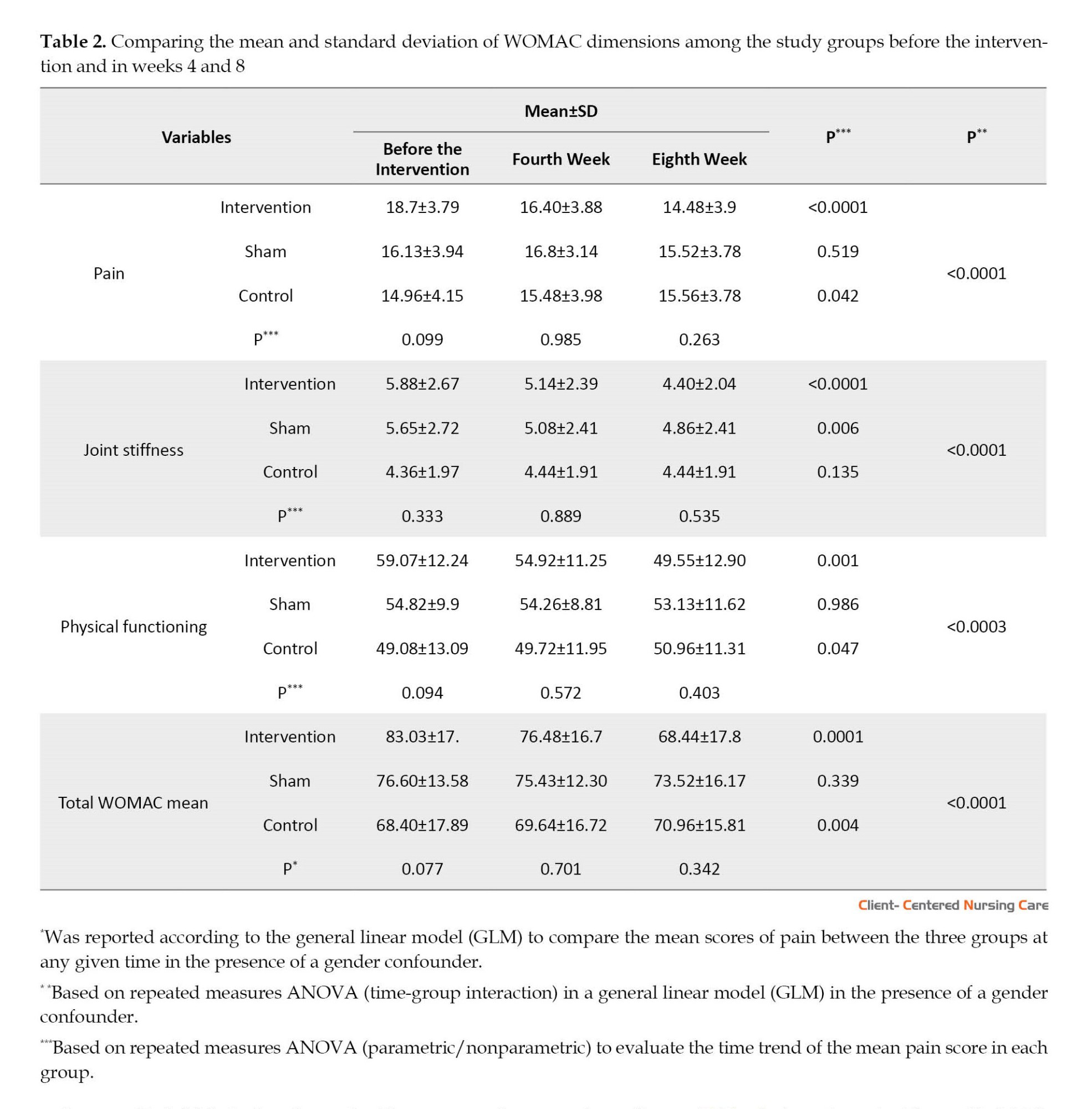
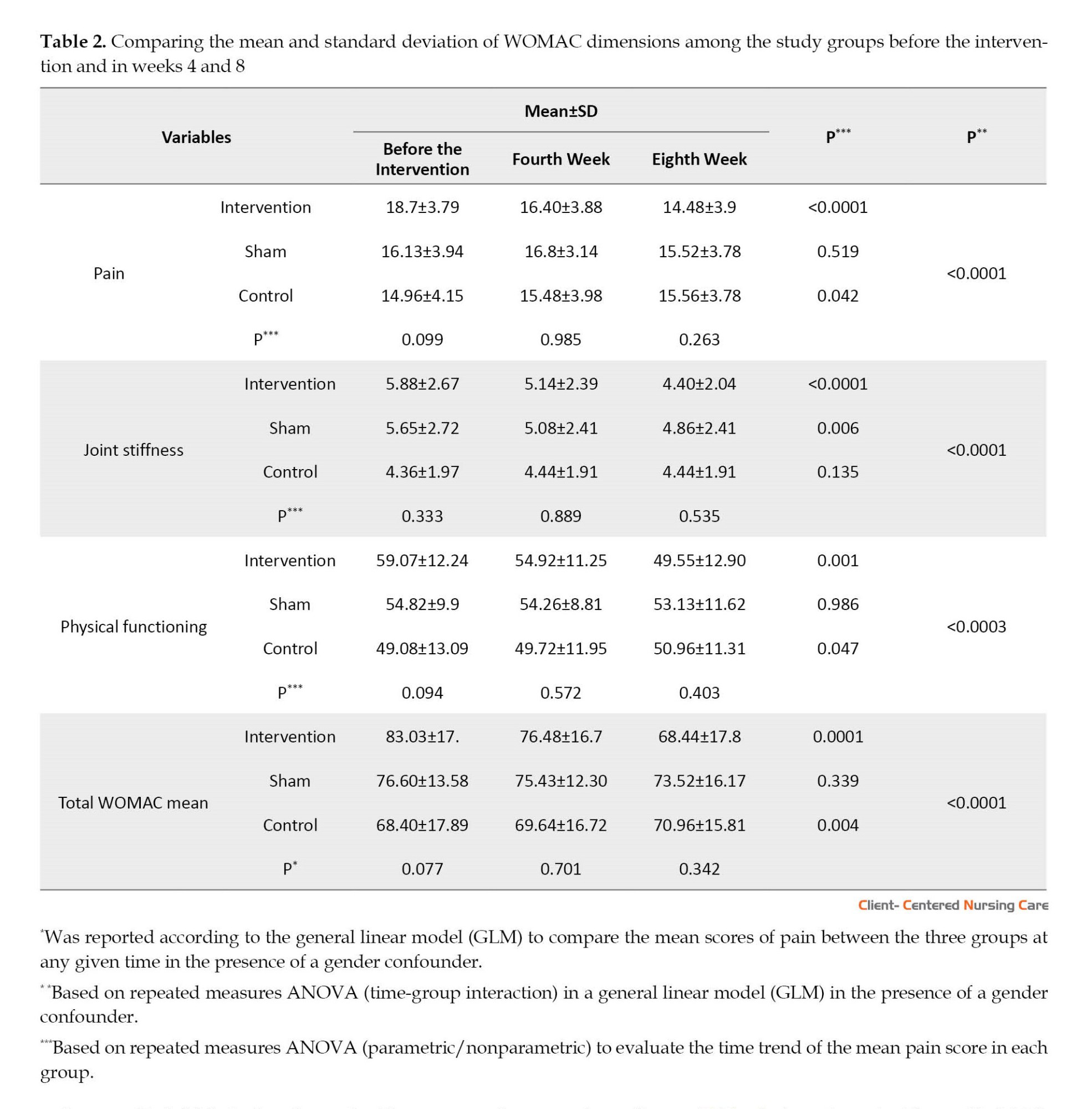
Table 2 presents a statistically significant difference between the three groups regarding the mean scores of pain, joint stiffness, and physical functioning at all three time points. The mean score of pain had a significantly decreasing trend in the intervention group over time (P<0.0001) but a significantly increasing trend in the control group (P<0.042). According to the results of repeated measures ANOVA, the mean pain score was significantly different between the three groups during the study period (P<0.0001). The mean score of joint stiffness had a significant decreasing trend in the intervention group (P<0.0001) and a significant decrease at different time points in the sham group (P=0.006). However, an increasing trend was seen in the control group, which was not significant (P=0.135). There was also a significant difference between groups at different time points (P<0.0001). The mean physical functioning score was significantly different between the three groups at different time points (P=0.0003). It had a significantly decreasing trend in the intervention group (P=0.0001) and a significantly increasing trend in the control group (P=0.047). The total WOMAC score was significantly different between the three groups during the study period (P<0.0001). The mean score of total WOMAC had a significant decreasing trend in the intervention group (P<0.0001) but a significant increasing trend in the control group (P=0.004) during the study. There was a significant difference between the total WOMAC scores between the three groups (P<0.0001).
According to Table 3, the mean pain intensity score significantly decreases in both intervention and sham groups (P<0.0001). An increasing trend in the control group is not significant (P=0.875). From the fifth week onwards, a statistically significant difference in pain intensity is observed between the three groups. According to Table 3, the lowest mean scores in week 5 (P=0.011), week 6 (P=0.004), week 7 (P=0.002), and week 8 (P<0.0001) belonged to the intervention group. Pain intensity was significantly different among the groups during the study period (P<0.0001).

According to Table 4, there is a significant (P=0.026) decreasing trend in the mean frequency of analgesic use in the intervention group and an insignificant (P=0.205) decreasing trend in the sham group. There is also an increasing trend in the mean frequency of analgesic use in the control group, which is not significant (P=0.247). The highest pre-intervention mean scores were associated with the intervention group (P=0.021). The lowest mean scores in week 1 (P=0.022), week 2 (P=0.027), week 5 (P=0.005), and weeks 6, 7, and 8 (P<0.001) belonged to the intervention group. There was a significant difference between the three groups regarding the mean frequency of analgesic use (P=0.026)

4. Discussion
This study investigated the effect of self-acupressure on pain, joint stiffness, and physical functioning of patients with knee osteoarthritis referred to Imam Khomeini Hospital and the orthopedic clinics in Ahvaz City. According to the data related to demographic characteristics, apart from the age variable, there was no significant difference between the three study groups. Knee osteoarthritis was more common in women than men, and the similarity of this finding with the results of other studies was expected (Abdian et al., 2015; Hasan Dokht et al., 2019). The findings regarding pain, joint stiffness, daily functioning, and the total WOMAC indicated statistically significant differences between the three groups. A study by Li. et al. (2018), which examined the effect of self-acupressure on adult patients with knee osteoarthritis, reported similar results. The results of another study which compared the effect of acupressure and self-care training on the severity of dysmenorrhea were in line with the present study (Ansaripour et al., 2015). In a study that evaluated the impact of acupressure on fatigue in female nurses with chronic back pain, reduced pain was reported during the second and fourth weeks of the intervention (Movahedi et al., 2017). In another study on the impact of self-administered acupressure on knee pain among postmenopausal women with knee osteoarthritis, no statistically significant results were observed (Zhang et al., 2012). Moreover, no significant decrease in pain was observed in a study evaluating the effectiveness of acupressure as an adjuvant therapy for sodium valproate in patients with migraine (Xu & Mi, 2017).
According to the results of our study, the mean score of pain had a significant decreasing trend in the intervention group and an increasing significant trend in the control group. Additionally, the results of repeated measures ANOVA showed that the mean pain score was significantly different between the three groups during the study. In a study that investigated the effectiveness of acupressure versus isometric exercise on pain, stiffness, and physical performance of female patients with knee osteoarthritis, the pain score in the acupressure group was significantly reduced. Like the current study, this study used the WOMAC scale to collect data (Sorour et al., 2014). In addition, the results of a study conducted in Germany that compared the effect of acupressure with usual care on menstrual pain showed that the pain in the acupressure group was significantly reduced (Blödt et al., 2018). The results of the research by Li et al. (2016) on the impact of self-administered acupressure on symptom management in older people with knee osteoarthritis also showed reduced pain. The study by Najafi et al. (2019) also reported decreased pain caused by intramuscular magnesium sulfate injection using manual acupressure. Also, Lee and Park, (2019) reported pain reduction in a study on the effect of auricular acupressure on pain, pain threshold, disability, and cervical spine’s range of motion in adults with chronic neck pain. The outcomes were assessed by VAS, neck-disability index, and cervical spine’s range of motion. Measurements were taken 3 times: Before, during the 2 weeks of intervention, and after the intervention. Another study was conducted among students to compare the effect of acupressure and self-care behaviors education on the severity of primary dysmenorrhea based on VAS. The results showed significant differences in pain severity within the groups before and after the intervention (P<0.05) but no significant differences between the three groups (Ansaripour et al., 2015). However, the study on migraine pain reported different results. In this study, the efficacy of sodium valproate combined with acupressure was not more significant than that of sodium valproate alone regarding pain relief (Xu & Mi, 2017). Another study on the effect of acupressure on postoperative pain among adolescents showed reduced pain (Pouy et al., 2022). The impact of acupressure on neck pain syndrome was reported to be moderate, according to the results of a Chinese study (Kwon & Lee, 2018).
There was a significant decreasing trend in joint stiffness in the intervention and sham groups. There was also a significant difference between the groups over time in our study. The results of a study by Sorour et al. (2014) also showed the positive effect of acupressure on reducing joint stiffness. However, in the study by Zhan et al. (2012) on the impact of self-acupressure on joint stiffness among postmenopausal women with knee osteoarthritis, the results were not significant. The difference between Zhan’s study and the present study can be explained by the differences in the inclusion criteria, randomization method (simple randomization method was used in Zhan’s study, and permutation block method was used in the present study), and telephone follow-up (lack of follow-up program in Zhan’s study).
The present study’s findings indicate that the mean score of physical functioning limitation followed a significantly decreasing trend in the intervention group and a significantly increasing trend in the control group. There was also a significant difference between the groups during the study regarding physical functioning. The study by Sorour et al. (2014) also reported positive outcomes; however, the scores of stiffness and impaired physical functioning were significantly lower in the isometric group (P<0.001) compared to the acupressure and control groups. A study on the impact of self-acupressure on symptom management in older adults with knee osteoarthritis also indicated a significant improvement in physical functioning (Li et al., 2016). Another study by Li et al. (2018) among adult patients with knee arthritis also showed an improvement in physical functioning after performing acupressure. Nevertheless, the study’s results by Zhang et al., 2012 did not report any positive impacts on physical functioning after self-acupressure.
There was a significant decreasing trend in the total WOMAC score in the intervention group and an increasing trend in the control group in our study; also, the total WOMAC score was significantly different between the three groups during the study period. In a study that assessed the effectiveness of acupressure versus isometric exercise on pain, stiffness, and physical function in knee osteoarthritis female patients, the total WOMAC score decreased in all three groups, with the two intervention groups showing greater reduction compared with the control group (Sorour et al., 2014). In the study by Zhang et al., 2012 on the impact of self-administered acupressure on osteoarthritis symptoms among postmenopausal women with knee osteoarthritis, unlike the present study, no statistical difference was observed between the acupressure compared with usual care.
The findings regarding the mean pain intensity score before the intervention and during the first to eighth weeks showed a significant decrease in both intervention and sham groups. From the fifth week onwards, the intensity of pain was significantly different between the three groups, and the lowest mean scores were obtained in weeks 5, 6, 7, and 8 in the intervention group. As positive results are gained over time, the intervention should be done for some time to achieve positive results. In a study that examined the feasibility of training self-administered acupressure exercises among postmenopausal women with osteoarthritic knee, pain significantly decreased from the first to the twelfth week. In this study, the data were collected by the WOMAC scale (Zhang et al., 2012). Ansaripour et al., 2015 also reported that performing acupressure reduces dysmenorrhea pain among female students. Movahedi et al., 2017 reported similar results in a study that evaluated the effect of acupressure on fatigue in female nurses with chronic low back pain. However, the results of a Chinese migraine study differed from those of the current research (Xu & Mi, 2017). The difference in the research population can explain the reason for the difference in the results.
According to the present study’s findings, analgesic use had a significant decreasing trend in the intervention group, while no significant reduction was observed in the sham group. The results of a German study on the impact of self-administered acupressure on menstrual pain showed a reduced use of analgesics in the intervention group (Blödt et al., 2018).
5. Conclusion
The findings of this study showed that self-acupressure could reduce the intensity of pain and joint stiffness and improve the physical performance of patients with knee osteoarthritis. It is recommended that nurses and nursing students learn acupressure techniques and teach them to patients with knee osteoarthritis. Conducting this study with a larger sample size regarding knee osteoarthritis and other involved joints is also recommended. This study was conducted for a short time. More appropriate and reliable results will be obtained by conducting similar studies over an extended time.
One of the limitations of this study was related to patients’ fatigue and mental state when reporting symptoms, especially pain intensity. This issue could affect their answers, which was beyond the researcher’s control.
Ethical Considerations
Compliance with ethical guidelines
This study was registered by the Iran Registry of Clinical Trials (Code: IRCT20181217042032N1). It was also approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Code: IR.AJUMS.REC.1397.539). All study subjects completed the informed consent form. The subjects were assured of anonymity and confidentiality of their information. They were informed that they could withdraw from the study without any consequences if they did not wish to continue the research process.
Funding
This study was financially supported by Ahvaz Jundishapur University of Medical Sciences.
Authors' contributions
Conceptualization: Laleh Raygan; Study design: Laleh Raygan, Simin Jahani and Nasrin Elahi; Supervision, reporting the results: Elham Maraghi, Simin Jahani and Nasrin Elahi; Data collection: Laleh Raygan, Safa Najafi and Mohammad Fakoor; Data analysi and data interception: Elham Maraghi; Writing the paper and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to the patients who participated in this project and tolerated us in all stages of this research.
References
Abedian, Z., et al., 2015. The effect of acupressure on sleep quality in menopausal women: A randomized control trial. Iranian Journal of Medical Sciences, 40(4), pp. 328–34. [PMID]
Ansaripour, L., et al., 2018. Comparison of the influence of acupressure and self-care behavior education on the severity of primary dysmenorrhea based on visual analogue scale among students. International Journal of Medical Research & Health Sciences, 5(10), pp.200-7. [Link]
Bastani, F., Sobhani, M. & Emamzadeh Ghasemi, H. S., 2015. Effect of acupressure on fatigue in women with multiple sclerosis. Global Journal of Health Science, 7(4), pp. 375–81. [DOI:10.5539/gjhs.v7n4p375] [PMID] [PMCID]
Bilbao, A., et al., 2011. Validation of a proposed WOMAC short form for patients with hip osteoarthritis. Health and Quality of Life Outcomes, 9, pp. 75. [DOI:10.1186/1477-7525-9-75] [PMID] [PMCID]
BBlödt, S., et al., 2018. Effectiveness of app-based self-acupressure for women with menstrual pain compared to usual care: A randomized pragmatic trial. American Journal of Obstetrics and Gynecology, 218(2), pp. 227.e1–9. [DOI:10.1016/j.ajog.2017.11.570] [PMID]
Covey C. J. & Shmerling, R. H. 2021. Approach to the adult with unspecified knee pain [Intenet]. Viewed 11 November 2023. [Link]
Gupta, P., Jindal, P. & Kumar, N., 2019. Role of pre-emptive Huff’s manoeuvre and acupressure in reducing the incidence of fentanyl induced cough; a risk factor for postoperative nausea vomiting in female patients: A prospective randomised controlled study. Indian Journal of Anaesthesia, 63(10), pp. 834–40.[DOI:10.4103/ija.IJA_549_19] [PMID] [PMCID]
Hasandokht, T., et al., 2019. [Evaluation of relation between cardiovascular risk factors and osteoarthritis: Results of a cross-sectional Study (Persian)]. Feyz, 23(2), pp.209-15. [Link]
Kwon, C. Y. & Lee, B., 2018. Clinical effects of acupressure on neck pain syndrome (nakchim): A systematic review. Integrative Medicine Research, 7(3), pp. 219–30. [DOI:10.1016/j.imr.2018.01.002] [PMID] [PMCID]
Levinger, P., et al., 2017. The effect of vitamin D status on pain, lower limb strength and knee function during balance recovery in people with knee osteoarthritis: An exploratory study. Archives of Osteoporosis,12(1), pp. 83. [DOI:10.1007/s11657-017-0378-4] [PMID]
Lee, S. & Park, H., 2019. Effects of auricular acupressure on pain and disability in adults with chronic neck pain. Applied Nursing Research, 45, pp. 12-16. [DOI:10.1016/j.apnr.2018.11.005] [PMID]
LI, L. W., et al., 2016. Feasibility of a randomized controlled trial of self-administered acupressure for symptom management in older adults with knee osteoarthritis. Journal of Alternative and Complementary Medicine (New York, N.Y.), 22(5), pp. 396–403. [DOI:10.1089/acm.2015.0231] [PMID]
Li, L. W., et al., 2018. Self-acupressure for older adults with symptomatic knee osteoarthritis: A randomized controlled trial. Arthritis Care & Research, 70(2), pp. 221–9. [DOI:10.1002/acr.23262] [PMID]
Mehta, P., et al., 2016. Contemporary acupressure therapy: Adroit cure for painless recovery of therapeutic ailments. Journal of Traditional and Complementary Medicine, 7(2), pp. 251–63. [DOI:10.1016/j.jtcme.2016.06.004] [PMID] [PMCID]
Movahedi, M., 2017. The effect of acupressure on fatigue among female nurses with chronic back pain. Applied Nursing Research, 36, pp. 111-4. [DOI:10.1016/j.apnr.2017.06.006] [PMID]
Najafi, S. S., et al., 2019. The effect of manual acupressure (Point BL32) on pain associated with intramuscular injections of magnesium sulfate. Journal of Acupuncture and Meridian Studies, 12(2), pp. 67–72. [DOI:10.1016/j.jams.2018.07.002] [PMID]
Pouy, S., et al., 2019. Effect of acupressure on post tonsillectomy pain in adolescents: A randomized, single-blind, placebo-controlled trial study. International Journal of Adolescent Medicine and Health, 34(1). [DOI:10.1515/ijamh-2019-0065] [PMID]
Ruiz Iban, M. A., et al., 2018. Use of strong opioids for chronic pain in osteoarthritis: An insight into the Latin American reality. Expert Review of Clinical Pharmacology, 11(1), pp. 47–59. [DOI:10.1080/17512433.2018.1381556] [PMID]
Safiri, S., et al., 2020. Global, regional and national burden of osteoarthritis 1990-2017: A systematic analysis of the Global Burden of Disease Study 2017. Annals of The Rheumatic Diseases, 79(6), pp. 819–28. [DOI:10.1136/annrheumdis-2019-216515] [PMID]
Shafiee-Darabi, S., et al., 2015. [Effect of acupressure on pain and fatigue in people with chronic heart failure (Persian)]. Iranian Journal of Cardiovascular Nursing, 3(4), pp. 14-22. [Link]
Shariati, A., et al., 2012. The effect of acupressure on sleep quality in hemodialysis patients. Complementary Therapies in Medicine, 20(6), pp. 417–23. [DOI:10.1016/j.ctim.2012.08.001] [PMID]
Sharif Nia, H., et al., 2017. Effect of acupressure on pain in Iranian leukemia patients: A randomized controlled trial study. International Journal of Nursing Practice, 23(2), pp. 10.1111/ijn.12513.[DOI:10.1111/ijn.12513] [PMID]
Sorour, A. S., Ayoub, A. S. & Abd El Aziz, E. M., 2014. Effectiveness of acupressure versus isometric exercise on pain, stiffness, and physical function in knee osteoarthritis female patients. Journal of Advanced Research, 5(2), pp. 193–200. [DOI:10.1016/j.jare.2013.02.003] [PMID] [PMCID]
Tiwari, A., et al., 2016. Self-administered acupressure for symptom management among Chinese family caregivers with caregiver stress: A randomized, wait-list controlled trial. BMC Complementary and Alternative Medicine, 16(1), PP. 424.[DOI:10.1186/s12906-016-1409-1] [PMID] [PMCID]
Weber, A., et al., 2019. Association between osteoarthritis and increased risk of dementia: A systemic review and meta-analysis. Medicine, 98(10), pp. e14355. [DOI:10.1097/MD.0000000000014355] [PMID] [PMCID]
Xu, J. H. & Mi, H. Y., 2017. A randomized controlled trial of acupressure as an adjunctive therapy to sodium valproate on the prevention of chronic migraine with aura. Medicine, 96(27), pp. e7477. [DOI:10.1097/MD.0000000000007477] [PMID] [PMCID]
Yang, L. H., et al., 2017. Efficacy of auricular acupressure for chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. Evidence-Based Complementary and Alternative Medicine: eCAM, 2017, pp. 6383649.[DOI:10.1155/2017/6383649] [PMID] [PMCID]
YU, S., Hunter, D. & Curtis, M. 2019. Investigational approaches to the management of osteoarthritis [Internet]. Viewed 11 November 2023. [Link]
Zeddou, M., 2019. Osteoarthritis is a low-grade inflammatory disease: Obesity’s involvement and herbal treatment.Evidence-Based Complementary and Alternative Medicine: eCAM, 2019, pp. 2037484. [DOI:10.1155/2019/2037484] [PMID] [PMCID]
Zhang, Y., et al., 2012. Training self-administered acupressure exercise among postmenopausal women with osteoarthritic knee pain: A feasibility study and lessons learned. Evidence-Based Complementary and Alternative Medicine, 2012. pp. 570431. [DOI:10.1155/2012/570431] [PMID] [PMCID]
Osteoarthritis or rheumatoid arthritis is a painful condition caused by the gradual loss of joint cartilage associated with inflammation. Osteoarthritis often affects the hands, knees, and spine. The patients experience general symptoms, such as pain, stiffness, and movement difficulties (Zeddou, 2019). Approximately 1 in 4 people in the UK complain of knee pain, most often due to osteoarthritis (Weber et al., 2019). In Iran, the incidence rates of knee arthritis in the age group of 15-85 years are 15.3% in urban population and 19.3% in rural population (Abedian et al., 2015). As the aging population increases, the prevalence of osteoarthritis increases, resulting in a growing concern regarding its indirect costs (Safiri et al., 2020; Ruiz Iban et al., 2018). Chronic knee pain adversely affects daily routine and quality of life in 25% of adults (Levinger et al., 2017). The resulting pain is one of the causes of disability among people over 50 years old (Weber et al., 2019). Needless to say that pain represents one of the priorities to be addressed (Covey & Shmerling, 2021). The patients constantly complain of pain originating from multiple regions (Weber et al., 2019). This chronic pain leads to inadequate activity, limited participation in activities of daily living (ADL), and reduced physical functioning. It also damages the quality of life, mood, and sleep, leading to fatigue. People with chronic pain have the lowest quality of life compared with other patients. This condition usually accompanies the feeling of hopelessness and doubles the risk of suicide compared to people without chronic pain. In the United States alone, approximately 15 million people complain of their poor quality of life due to pain (Safiri et al., 2020).
Acupressure is an alternative therapy usually employed in conjunction with acupuncture or reflexology. Acupressure is an ancient Chinese method based on the belief in the human body’s flow of vital energy called QI (or Chi, life energy). The energy flows in body channels, regulated by the individual’s body system. The unbalanced flow of QI results in the disease. Stimulation and pressure on specific body points open the channels, regulate energy flow, and balance the QI energy in the body, thus restoring health (Li et al., 2016).
Furthermore, applying acupressure in specific trigger points is believed to transmit pleasant beats to the brain 4 times faster than painful stimulants, blocking neural impulses’ path and preventing slower pain messages from reaching the brain. This technique helps improve or strengthen the threshold of pain perception in the body. In addition, mechanical pressure such as massaging and acupressure reduces tissue adhesion, stimulates relaxation, increases local blood circulation, increases parasympathetic nerve activity, increases muscle temperature, and reduces neuromuscular irritability (Sharif Nia et al., 2017). Acupressure can be performed by nurses, midwives, and even patients themselves if they are appropriately trained (Yu et al., 2019; Shariati et al., 2012).
Positive effects of acupressure have already been reported for various conditions, such as pain in primary dysmenorrhea (Mehta et al., 2017; Tiwari et al., 2016), severe back pain in patients with ankylosing spondylitis (Yang et al., 2017), extreme fatigue in women with multiple sclerosis (Bastani et al., 2015), the pain and fatigue in patients with chronic heart failure (Shafiee-Darabi et al., 2015), and the sleep quality of hemodialysis patients (Shariati et al., 2012). Some advantages of self-acupressure are flexibility in time and place, low intervention cost, empowering the patient, and increasing self-care. This therapy is also safe and acceptable from the patient’s perspective, as it can be implemented at home and reduces health care costs (Sharif Nia et al., 2017). Even studies that reported no positive outcome have suggested repeating the research with larger populations (Zhang et al., 2012; Li et al, 2018; Gupta et al., 2019).
Therefore, this study was performed to determine the impact of self-acupressure on pain, joint stiffness, and physical performance of patients with knee osteoarthritis.
2. Materials and Methods
Study design, setting, and sample
The present study was a controlled randomized clinical trial with three groups (intervention, sham, and control). The subjects were selected from the patients referred to the Ahvaz Imam Khomeini Hospital, as well as the patients who had been referred to the orthopedic private clinics in Khuzestan Province, Iran. According to the purpose of the research and a previous study (Li et al., 2016), considering β=0.2, α=0.05, s=3.3, and d=2.1, as well as a potential 20% sample attrition, the sample size was estimated at 26 subjects for each group (78 subjects in total) using the Equation 1:
The inclusion criteria included patients with a confirmed diagnosis of osteoarthritis by an orthopedist, 50 to 70 years old, with severe knee pain (a score above 3 on the VAS), not under other complementary medicine treatments or meditation techniques such as yoga and relaxation, without knee injuries preventing acupressure in that point, no rheumatoid arthritis or lupus, and the ability to learn and perform the intervention. The exclusion criteria were as follows: Not applying continuous acupressure according to the program, requiring surgery during the intervention, doing the intervention less than 5 days a week, and unwillingness to continue the program.
The subjects were randomly assigned to three groups through permutated block randomization with a block size of 4, using a table of random permutations. A statistician prepared the randomization list. According to the randomization list, the intervention instructions were placed in a sealed envelope by someone outside the study, unaware of the research objectives. He offered the envelopes to the patients according to the corresponding codes. The subjects were randomly allocated into three groups: Self-acupressure (n=26), sham (n=26), and control (n=26) (Figure 1).

Instruments
Demographic information questionnaire
This questionnaire gathers information about gender, age, height and weight, marital status, level of education, body mass index (BMI), duration of the osteoarthritis, and other underlying diseases of the patient. The questionnaire was assessed by 10 faculty members of the School of Nursing and Midwifery, Ahvaz University of Medical Sciences, and their comments were applied.
The Western Ontario and McMaster Universities osteoarthritis index (WOMAC)
This index was developed for patients with knee pain and includes 24 questions and 3 sections: The presence of pain, joint stiffness, and daily functioning. The first part contains 5 questions about the presence of pain while doing some tasks. The second part deals with the symptoms and joint stiffness with 2 questions about knee swelling, a feeling of rubbing or extra noise in the knee, the ability to flex and extend the knee, and the degree of joint dryness at the beginning of the morning and the end of the day after activity. The third part examines the difficulty in daily tasks and functional activities. It includes 17 questions relating to activities like going down and up the stairs, changing the position from sitting to standing, picking up an object from the ground, walking, getting in and out of the car, going shopping, putting on and taking off socks, getting up and lying down in bed, getting in and out of the bathroom, going in and out of the toilet, carrying heavy objects and doing light household chores like dusting. The questions of this index are scored on a scale of 0 to 4: None (0), mild (1), moderate (2), severe (3) and extreme (4). The subscale scores range from 0-20 for pain, 0-8 for stiffness, and 0-68 for physical function. The sum of all three subscale scores gives a total WOMAC score, and higher scores indicate greater severity of the patient’s symptoms. Different studies have used the WOMAC index (Li et al., 2018). The reliability of this index has been confirmed in the Netherlands with a Cronbach α coefficient of 0.88 (Bilbao et al., 2011). The reliability of the Persian version of this index has been confirmed in a pilot study on 10 elderly subjects with a Cronbach α coefficient of 0.963 (Bastani et al., 2015). The patients in all three groups completed the WOMAC index before the intervention and at the end of the fourth and eighth weeks of the study period.
Visual analog scale (VAS)
This scale is widely known and frequently used in various studies to assess pain intensity, in which samples choose a number between 0 and 10 for pain intensity based on their personal feelings (Yu et al., 2019). All three groups completed the VAS before the intervention and every week during the study period for 8 consecutive weeks via telephone interviews.
The analgesics checklist
This checklist was employed to determine the patient’s use of analgesics, including the type of medicine and the prescribed dose. After being prepared by the researcher, this checklist was approved by the faculty members of the Nursing and Midwifery School of Ahvas Jundishapur University of Medical Sciences. All three groups completed the analgesics checklist every day during the study period for 8 consecutive weeks via telephone interviews.
Study procedure
To teach the intervention to the patients, first, the researcher learned the necessary skills to perform the acupressure method under the supervision of a physical medicine and rehabilitation specialist. The procedure’s method is that patients first sit on a chair or the edge of the bed and determine the 5 desired points around their knee (Figure 2). The patients must hold the injured knee with their hand for 3 minutes and massage the area without gloves and without using oil or ointment so that they feel that the desired area is heated. Then, they should apply pressure to each specified point with their thumb for one minute. The method of applying pressure is 5 seconds and 5 seconds of rest in each of the 5 points. This action continues for 1 minute and then is repeated at the next point for one minute. This procedure should be done once a day for 8 consecutive weeks. The training of patients in the sham group was the same as the intervention group, with the difference that the points related to acupressure were taught to this group with a difference of 1 cm higher than the patients in the intervention group. Feedback was received from them to check the accuracy of learning. The control group received no intervention.

Data analysis
The obtained data were analyzed using the chi-square test, one-way analysis of variance (ANOVA), nonparametric ANOVA (Kruskal-Wallis), and repeated measures ANOVA in SPSS software, version 20. A generalized linear model (GLM) test was performed to eliminate the effect of confounding factors of gender. The significance level of the tests was considered at P<0.05.
3. Results
A total of 78 people participated in the study. Three subjects were excluded during the study (one due to joint replacement surgery and the other two due to not consistently performing acupressure as scheduled). Finally, the data of 75 subjects were analyzed. Twenty-seven subjects were in the intervention group, 23 in the sham group, and 25 in the control group (Figure 1). The demographic characteristics of the groups are presented and compared in Table 1. Except for the significant gender difference (P=0.012) between the three groups, their personal and disease characteristics were comparable.
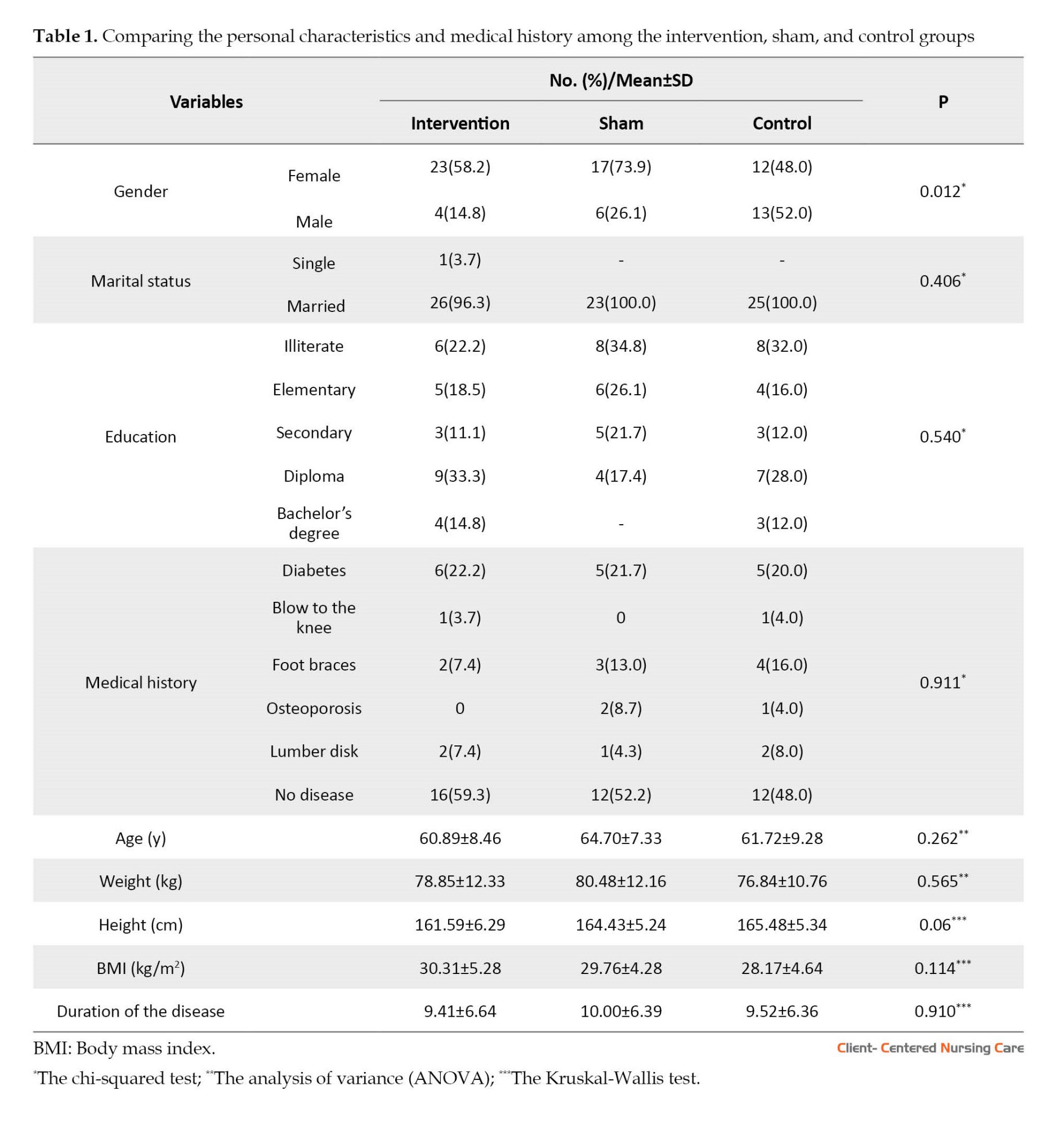
Table 2 presents a statistically significant difference between the three groups regarding the mean scores of pain, joint stiffness, and physical functioning at all three time points. The mean score of pain had a significantly decreasing trend in the intervention group over time (P<0.0001) but a significantly increasing trend in the control group (P<0.042). According to the results of repeated measures ANOVA, the mean pain score was significantly different between the three groups during the study period (P<0.0001). The mean score of joint stiffness had a significant decreasing trend in the intervention group (P<0.0001) and a significant decrease at different time points in the sham group (P=0.006). However, an increasing trend was seen in the control group, which was not significant (P=0.135). There was also a significant difference between groups at different time points (P<0.0001). The mean physical functioning score was significantly different between the three groups at different time points (P=0.0003). It had a significantly decreasing trend in the intervention group (P=0.0001) and a significantly increasing trend in the control group (P=0.047). The total WOMAC score was significantly different between the three groups during the study period (P<0.0001). The mean score of total WOMAC had a significant decreasing trend in the intervention group (P<0.0001) but a significant increasing trend in the control group (P=0.004) during the study. There was a significant difference between the total WOMAC scores between the three groups (P<0.0001).
According to Table 3, the mean pain intensity score significantly decreases in both intervention and sham groups (P<0.0001). An increasing trend in the control group is not significant (P=0.875). From the fifth week onwards, a statistically significant difference in pain intensity is observed between the three groups. According to Table 3, the lowest mean scores in week 5 (P=0.011), week 6 (P=0.004), week 7 (P=0.002), and week 8 (P<0.0001) belonged to the intervention group. Pain intensity was significantly different among the groups during the study period (P<0.0001).

According to Table 4, there is a significant (P=0.026) decreasing trend in the mean frequency of analgesic use in the intervention group and an insignificant (P=0.205) decreasing trend in the sham group. There is also an increasing trend in the mean frequency of analgesic use in the control group, which is not significant (P=0.247). The highest pre-intervention mean scores were associated with the intervention group (P=0.021). The lowest mean scores in week 1 (P=0.022), week 2 (P=0.027), week 5 (P=0.005), and weeks 6, 7, and 8 (P<0.001) belonged to the intervention group. There was a significant difference between the three groups regarding the mean frequency of analgesic use (P=0.026)

4. Discussion
This study investigated the effect of self-acupressure on pain, joint stiffness, and physical functioning of patients with knee osteoarthritis referred to Imam Khomeini Hospital and the orthopedic clinics in Ahvaz City. According to the data related to demographic characteristics, apart from the age variable, there was no significant difference between the three study groups. Knee osteoarthritis was more common in women than men, and the similarity of this finding with the results of other studies was expected (Abdian et al., 2015; Hasan Dokht et al., 2019). The findings regarding pain, joint stiffness, daily functioning, and the total WOMAC indicated statistically significant differences between the three groups. A study by Li. et al. (2018), which examined the effect of self-acupressure on adult patients with knee osteoarthritis, reported similar results. The results of another study which compared the effect of acupressure and self-care training on the severity of dysmenorrhea were in line with the present study (Ansaripour et al., 2015). In a study that evaluated the impact of acupressure on fatigue in female nurses with chronic back pain, reduced pain was reported during the second and fourth weeks of the intervention (Movahedi et al., 2017). In another study on the impact of self-administered acupressure on knee pain among postmenopausal women with knee osteoarthritis, no statistically significant results were observed (Zhang et al., 2012). Moreover, no significant decrease in pain was observed in a study evaluating the effectiveness of acupressure as an adjuvant therapy for sodium valproate in patients with migraine (Xu & Mi, 2017).
According to the results of our study, the mean score of pain had a significant decreasing trend in the intervention group and an increasing significant trend in the control group. Additionally, the results of repeated measures ANOVA showed that the mean pain score was significantly different between the three groups during the study. In a study that investigated the effectiveness of acupressure versus isometric exercise on pain, stiffness, and physical performance of female patients with knee osteoarthritis, the pain score in the acupressure group was significantly reduced. Like the current study, this study used the WOMAC scale to collect data (Sorour et al., 2014). In addition, the results of a study conducted in Germany that compared the effect of acupressure with usual care on menstrual pain showed that the pain in the acupressure group was significantly reduced (Blödt et al., 2018). The results of the research by Li et al. (2016) on the impact of self-administered acupressure on symptom management in older people with knee osteoarthritis also showed reduced pain. The study by Najafi et al. (2019) also reported decreased pain caused by intramuscular magnesium sulfate injection using manual acupressure. Also, Lee and Park, (2019) reported pain reduction in a study on the effect of auricular acupressure on pain, pain threshold, disability, and cervical spine’s range of motion in adults with chronic neck pain. The outcomes were assessed by VAS, neck-disability index, and cervical spine’s range of motion. Measurements were taken 3 times: Before, during the 2 weeks of intervention, and after the intervention. Another study was conducted among students to compare the effect of acupressure and self-care behaviors education on the severity of primary dysmenorrhea based on VAS. The results showed significant differences in pain severity within the groups before and after the intervention (P<0.05) but no significant differences between the three groups (Ansaripour et al., 2015). However, the study on migraine pain reported different results. In this study, the efficacy of sodium valproate combined with acupressure was not more significant than that of sodium valproate alone regarding pain relief (Xu & Mi, 2017). Another study on the effect of acupressure on postoperative pain among adolescents showed reduced pain (Pouy et al., 2022). The impact of acupressure on neck pain syndrome was reported to be moderate, according to the results of a Chinese study (Kwon & Lee, 2018).
There was a significant decreasing trend in joint stiffness in the intervention and sham groups. There was also a significant difference between the groups over time in our study. The results of a study by Sorour et al. (2014) also showed the positive effect of acupressure on reducing joint stiffness. However, in the study by Zhan et al. (2012) on the impact of self-acupressure on joint stiffness among postmenopausal women with knee osteoarthritis, the results were not significant. The difference between Zhan’s study and the present study can be explained by the differences in the inclusion criteria, randomization method (simple randomization method was used in Zhan’s study, and permutation block method was used in the present study), and telephone follow-up (lack of follow-up program in Zhan’s study).
The present study’s findings indicate that the mean score of physical functioning limitation followed a significantly decreasing trend in the intervention group and a significantly increasing trend in the control group. There was also a significant difference between the groups during the study regarding physical functioning. The study by Sorour et al. (2014) also reported positive outcomes; however, the scores of stiffness and impaired physical functioning were significantly lower in the isometric group (P<0.001) compared to the acupressure and control groups. A study on the impact of self-acupressure on symptom management in older adults with knee osteoarthritis also indicated a significant improvement in physical functioning (Li et al., 2016). Another study by Li et al. (2018) among adult patients with knee arthritis also showed an improvement in physical functioning after performing acupressure. Nevertheless, the study’s results by Zhang et al., 2012 did not report any positive impacts on physical functioning after self-acupressure.
There was a significant decreasing trend in the total WOMAC score in the intervention group and an increasing trend in the control group in our study; also, the total WOMAC score was significantly different between the three groups during the study period. In a study that assessed the effectiveness of acupressure versus isometric exercise on pain, stiffness, and physical function in knee osteoarthritis female patients, the total WOMAC score decreased in all three groups, with the two intervention groups showing greater reduction compared with the control group (Sorour et al., 2014). In the study by Zhang et al., 2012 on the impact of self-administered acupressure on osteoarthritis symptoms among postmenopausal women with knee osteoarthritis, unlike the present study, no statistical difference was observed between the acupressure compared with usual care.
The findings regarding the mean pain intensity score before the intervention and during the first to eighth weeks showed a significant decrease in both intervention and sham groups. From the fifth week onwards, the intensity of pain was significantly different between the three groups, and the lowest mean scores were obtained in weeks 5, 6, 7, and 8 in the intervention group. As positive results are gained over time, the intervention should be done for some time to achieve positive results. In a study that examined the feasibility of training self-administered acupressure exercises among postmenopausal women with osteoarthritic knee, pain significantly decreased from the first to the twelfth week. In this study, the data were collected by the WOMAC scale (Zhang et al., 2012). Ansaripour et al., 2015 also reported that performing acupressure reduces dysmenorrhea pain among female students. Movahedi et al., 2017 reported similar results in a study that evaluated the effect of acupressure on fatigue in female nurses with chronic low back pain. However, the results of a Chinese migraine study differed from those of the current research (Xu & Mi, 2017). The difference in the research population can explain the reason for the difference in the results.
According to the present study’s findings, analgesic use had a significant decreasing trend in the intervention group, while no significant reduction was observed in the sham group. The results of a German study on the impact of self-administered acupressure on menstrual pain showed a reduced use of analgesics in the intervention group (Blödt et al., 2018).
5. Conclusion
The findings of this study showed that self-acupressure could reduce the intensity of pain and joint stiffness and improve the physical performance of patients with knee osteoarthritis. It is recommended that nurses and nursing students learn acupressure techniques and teach them to patients with knee osteoarthritis. Conducting this study with a larger sample size regarding knee osteoarthritis and other involved joints is also recommended. This study was conducted for a short time. More appropriate and reliable results will be obtained by conducting similar studies over an extended time.
One of the limitations of this study was related to patients’ fatigue and mental state when reporting symptoms, especially pain intensity. This issue could affect their answers, which was beyond the researcher’s control.
Ethical Considerations
Compliance with ethical guidelines
This study was registered by the Iran Registry of Clinical Trials (Code: IRCT20181217042032N1). It was also approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Code: IR.AJUMS.REC.1397.539). All study subjects completed the informed consent form. The subjects were assured of anonymity and confidentiality of their information. They were informed that they could withdraw from the study without any consequences if they did not wish to continue the research process.
Funding
This study was financially supported by Ahvaz Jundishapur University of Medical Sciences.
Authors' contributions
Conceptualization: Laleh Raygan; Study design: Laleh Raygan, Simin Jahani and Nasrin Elahi; Supervision, reporting the results: Elham Maraghi, Simin Jahani and Nasrin Elahi; Data collection: Laleh Raygan, Safa Najafi and Mohammad Fakoor; Data analysi and data interception: Elham Maraghi; Writing the paper and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to the patients who participated in this project and tolerated us in all stages of this research.
References
Abedian, Z., et al., 2015. The effect of acupressure on sleep quality in menopausal women: A randomized control trial. Iranian Journal of Medical Sciences, 40(4), pp. 328–34. [PMID]
Ansaripour, L., et al., 2018. Comparison of the influence of acupressure and self-care behavior education on the severity of primary dysmenorrhea based on visual analogue scale among students. International Journal of Medical Research & Health Sciences, 5(10), pp.200-7. [Link]
Bastani, F., Sobhani, M. & Emamzadeh Ghasemi, H. S., 2015. Effect of acupressure on fatigue in women with multiple sclerosis. Global Journal of Health Science, 7(4), pp. 375–81. [DOI:10.5539/gjhs.v7n4p375] [PMID] [PMCID]
Bilbao, A., et al., 2011. Validation of a proposed WOMAC short form for patients with hip osteoarthritis. Health and Quality of Life Outcomes, 9, pp. 75. [DOI:10.1186/1477-7525-9-75] [PMID] [PMCID]
BBlödt, S., et al., 2018. Effectiveness of app-based self-acupressure for women with menstrual pain compared to usual care: A randomized pragmatic trial. American Journal of Obstetrics and Gynecology, 218(2), pp. 227.e1–9. [DOI:10.1016/j.ajog.2017.11.570] [PMID]
Covey C. J. & Shmerling, R. H. 2021. Approach to the adult with unspecified knee pain [Intenet]. Viewed 11 November 2023. [Link]
Gupta, P., Jindal, P. & Kumar, N., 2019. Role of pre-emptive Huff’s manoeuvre and acupressure in reducing the incidence of fentanyl induced cough; a risk factor for postoperative nausea vomiting in female patients: A prospective randomised controlled study. Indian Journal of Anaesthesia, 63(10), pp. 834–40.[DOI:10.4103/ija.IJA_549_19] [PMID] [PMCID]
Hasandokht, T., et al., 2019. [Evaluation of relation between cardiovascular risk factors and osteoarthritis: Results of a cross-sectional Study (Persian)]. Feyz, 23(2), pp.209-15. [Link]
Kwon, C. Y. & Lee, B., 2018. Clinical effects of acupressure on neck pain syndrome (nakchim): A systematic review. Integrative Medicine Research, 7(3), pp. 219–30. [DOI:10.1016/j.imr.2018.01.002] [PMID] [PMCID]
Levinger, P., et al., 2017. The effect of vitamin D status on pain, lower limb strength and knee function during balance recovery in people with knee osteoarthritis: An exploratory study. Archives of Osteoporosis,12(1), pp. 83. [DOI:10.1007/s11657-017-0378-4] [PMID]
Lee, S. & Park, H., 2019. Effects of auricular acupressure on pain and disability in adults with chronic neck pain. Applied Nursing Research, 45, pp. 12-16. [DOI:10.1016/j.apnr.2018.11.005] [PMID]
LI, L. W., et al., 2016. Feasibility of a randomized controlled trial of self-administered acupressure for symptom management in older adults with knee osteoarthritis. Journal of Alternative and Complementary Medicine (New York, N.Y.), 22(5), pp. 396–403. [DOI:10.1089/acm.2015.0231] [PMID]
Li, L. W., et al., 2018. Self-acupressure for older adults with symptomatic knee osteoarthritis: A randomized controlled trial. Arthritis Care & Research, 70(2), pp. 221–9. [DOI:10.1002/acr.23262] [PMID]
Mehta, P., et al., 2016. Contemporary acupressure therapy: Adroit cure for painless recovery of therapeutic ailments. Journal of Traditional and Complementary Medicine, 7(2), pp. 251–63. [DOI:10.1016/j.jtcme.2016.06.004] [PMID] [PMCID]
Movahedi, M., 2017. The effect of acupressure on fatigue among female nurses with chronic back pain. Applied Nursing Research, 36, pp. 111-4. [DOI:10.1016/j.apnr.2017.06.006] [PMID]
Najafi, S. S., et al., 2019. The effect of manual acupressure (Point BL32) on pain associated with intramuscular injections of magnesium sulfate. Journal of Acupuncture and Meridian Studies, 12(2), pp. 67–72. [DOI:10.1016/j.jams.2018.07.002] [PMID]
Pouy, S., et al., 2019. Effect of acupressure on post tonsillectomy pain in adolescents: A randomized, single-blind, placebo-controlled trial study. International Journal of Adolescent Medicine and Health, 34(1). [DOI:10.1515/ijamh-2019-0065] [PMID]
Ruiz Iban, M. A., et al., 2018. Use of strong opioids for chronic pain in osteoarthritis: An insight into the Latin American reality. Expert Review of Clinical Pharmacology, 11(1), pp. 47–59. [DOI:10.1080/17512433.2018.1381556] [PMID]
Safiri, S., et al., 2020. Global, regional and national burden of osteoarthritis 1990-2017: A systematic analysis of the Global Burden of Disease Study 2017. Annals of The Rheumatic Diseases, 79(6), pp. 819–28. [DOI:10.1136/annrheumdis-2019-216515] [PMID]
Shafiee-Darabi, S., et al., 2015. [Effect of acupressure on pain and fatigue in people with chronic heart failure (Persian)]. Iranian Journal of Cardiovascular Nursing, 3(4), pp. 14-22. [Link]
Shariati, A., et al., 2012. The effect of acupressure on sleep quality in hemodialysis patients. Complementary Therapies in Medicine, 20(6), pp. 417–23. [DOI:10.1016/j.ctim.2012.08.001] [PMID]
Sharif Nia, H., et al., 2017. Effect of acupressure on pain in Iranian leukemia patients: A randomized controlled trial study. International Journal of Nursing Practice, 23(2), pp. 10.1111/ijn.12513.[DOI:10.1111/ijn.12513] [PMID]
Sorour, A. S., Ayoub, A. S. & Abd El Aziz, E. M., 2014. Effectiveness of acupressure versus isometric exercise on pain, stiffness, and physical function in knee osteoarthritis female patients. Journal of Advanced Research, 5(2), pp. 193–200. [DOI:10.1016/j.jare.2013.02.003] [PMID] [PMCID]
Tiwari, A., et al., 2016. Self-administered acupressure for symptom management among Chinese family caregivers with caregiver stress: A randomized, wait-list controlled trial. BMC Complementary and Alternative Medicine, 16(1), PP. 424.[DOI:10.1186/s12906-016-1409-1] [PMID] [PMCID]
Weber, A., et al., 2019. Association between osteoarthritis and increased risk of dementia: A systemic review and meta-analysis. Medicine, 98(10), pp. e14355. [DOI:10.1097/MD.0000000000014355] [PMID] [PMCID]
Xu, J. H. & Mi, H. Y., 2017. A randomized controlled trial of acupressure as an adjunctive therapy to sodium valproate on the prevention of chronic migraine with aura. Medicine, 96(27), pp. e7477. [DOI:10.1097/MD.0000000000007477] [PMID] [PMCID]
Yang, L. H., et al., 2017. Efficacy of auricular acupressure for chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. Evidence-Based Complementary and Alternative Medicine: eCAM, 2017, pp. 6383649.[DOI:10.1155/2017/6383649] [PMID] [PMCID]
YU, S., Hunter, D. & Curtis, M. 2019. Investigational approaches to the management of osteoarthritis [Internet]. Viewed 11 November 2023. [Link]
Zeddou, M., 2019. Osteoarthritis is a low-grade inflammatory disease: Obesity’s involvement and herbal treatment.Evidence-Based Complementary and Alternative Medicine: eCAM, 2019, pp. 2037484. [DOI:10.1155/2019/2037484] [PMID] [PMCID]
Zhang, Y., et al., 2012. Training self-administered acupressure exercise among postmenopausal women with osteoarthritic knee pain: A feasibility study and lessons learned. Evidence-Based Complementary and Alternative Medicine, 2012. pp. 570431. [DOI:10.1155/2012/570431] [PMID] [PMCID]
Type of Study: Research |
Subject:
General
Received: 2023/02/26 | Accepted: 2023/07/15 | Published: 2023/11/1
Received: 2023/02/26 | Accepted: 2023/07/15 | Published: 2023/11/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |