Thu, Aug 14, 2025
[Archive]
Volume 10, Issue 2 (Spring 2024)
JCCNC 2024, 10(2): 135-146 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Masharipova A, Nurgaliyeva N, Derbissalina G. Nurses’ Level of Preparedness to Provide Palliative Care and Its Relationship With Their Evidence-based Practice. JCCNC 2024; 10 (2) :135-146
URL: http://jccnc.iums.ac.ir/article-1-519-en.html
URL: http://jccnc.iums.ac.ir/article-1-519-en.html
1- Department of General Practice With the Course of Evidence–based Medicine, NJSC Astana Medical University, Astana, Kazakhstan. , alexa_0706@mail.ru
2- Department of General Practice With the Course of Evidence–based Medicine, NJSC Astana Medical University, Astana, Kazakhstan.
2- Department of General Practice With the Course of Evidence–based Medicine, NJSC Astana Medical University, Astana, Kazakhstan.
Full-Text [PDF 689 kb]
(575 Downloads)
| Abstract (HTML) (1938 Views)
● Palliative care is an integral component of the primary health care system.
● Nurses in this study had a low or inadequate knowledge about palliative care and a negative or neutral attitude toward it.
● The nurses’ lack of knowledge and skills in evidence-based practice may contribute to their lack of preparedness to provide palliative care.
Demographic and occupational factors, such as age, work experience, level of education, and attendance at palliative care training, can affect the nurses’ knowledge of palliative care and attitude to the care of dying patients.
● Nurses in this study had a low or inadequate knowledge about palliative care and a negative or neutral attitude toward it.
● The nurses’ lack of knowledge and skills in evidence-based practice may contribute to their lack of preparedness to provide palliative care.
Demographic and occupational factors, such as age, work experience, level of education, and attendance at palliative care training, can affect the nurses’ knowledge of palliative care and attitude to the care of dying patients.
Plain Language Summary
Through palliative care, nurses improve the quality of life of seriously-ill patients and their families. They can use special measures to predict, prevent, and reduce their suffering. This type of care is essential for end-of-life patients. Evidence-Based nursing practice is high-quality nursing care considering up-to-date scientific research rather than relying on traditional methods, peer recommendations, or personal beliefs. This study showed that knowledge of palliative care among primary health care nurses in Astana City, Kazakhstan, was low or inadequate, and the attitude toward dying patients in most cases was neutral. Nurses mostly scored low on the professional competencies in evidence-based nursing practice, mainly in the practice aspect. Moreover, there was a strong direct relationship between knowledge and attitude to palliative care and the level of evidence-based practice proficiency.
Full-Text: (363 Views)
Introduction
The World Health Organization (WHO) defines palliative care (PC) as improving the quality of life of seriously-ill patients and their families facing a life-threatening illness. PC includes physical, psychological, social, and spiritual aspects (WHO, 2020). PC should not be provided only at the end of the patient’s life; it should begin from the moment of diagnosis and continue throughout the entire period of the disease (Mills et al., 2018).
Nurses spend more time with patients and their families than other healthcare professionals. Qualified care reduces the suffering and burden of seriously-ill patients (Schroeder & Lorenz, 2018). Palliative nursing is a holistic approach to managing the symptoms of incurable diseases while simultaneously eliminating pain and other symptoms, psychosocial problems, maintaining spirituality, and the quality of life of a seriously-ill patient (Cross, 2019).
PC is successfully implemented due to the combined influence of good knowledge, attitudes, beliefs, and extensive experience of medical professionals. The negative attitude of nurses towards death and the care of dying people can significantly affect the quality of PC (Wang et al., 2016).
It is necessary to note the important role of nurses in ensuring universal access to PC, especially at the primary health care (PHC) stage, because the vast majority of people in need of PC prefer to die at home. Therefore, from a medical and ethical point of view, PC must be provided at home as part of PHC (WHO, 2018; Lakasing, 2023).
Nurses often have to master several functions on their right at home at the patient’s bedside because PC is a complex integrated approach that requires a specialist’s developed practical skills and personal qualities. Evidence-based practice (EBP) plays an essential role in navigating situations better at the bedside of patients (Sekse et al., 2018; Rosa, 2018). It is proven that nurses who actively combine patient preferences with EBP can improve the quality of life of patients and individual care (Achora & Labrague, 2019). However, at the moment, there are no studies devoted to the problem of the introduction of evidence-based medicine in nursing care at the PHC stage. Most scientific research on introducing evidence-based nursing was conducted in inpatient hospitals (Mathieson et al., 2019). Many countries already have mobile PC teams consisting of doctors, nurses, physiotherapists, and social workers who provide PC at home. In Kazakhstan, such mobile brigades are just beginning to form, but they still do not function properly. The new state program of Healthcare Development for 2020-2025 in Kazakhstan provides for the creation of mobile teams in all PHC organizations throughout the country by 2025 to increase the availability of PC services, regardless of the geographical and financial situation of citizens (Ministry of Justice of the Republic of Kazakhstan, 2019).
Although the palliative care system in Kazakhstan has been reformed several times, according to statistics, more than 80% of doctors and nurses lack basic knowledge of palliative care (Masharipova et al., 2022). The problem of training PC specialists should be recognized at the state level. It is necessary to improve the system for training medical specialists in PC (Kunirova & Shakenova, 2017). Thus, this study aimed to assess nurses’ knowledge of PC and attitudes towards caring for dying patients and its relationship with their EBP (knowledge/skills, attitude, and practice) in PHC organizations of Astana City, Kazakhstan.
Materials and Methods
Study design and participants
This descriptive, cross-sectional study was conducted from 2022 to 2023. Ten PHC organizations in the city of Astana were randomly selected. The sample size was computed considering that approximately 3000 nurses are officially employed in Astana City organizations. A convenience sampling method was used to choose the subjects, and a total of 565 nurses working in PHC organizations in Astana and providing PC for seriously-ill patients at home as part of PHC were recruited. The inclusion criteria were nurses who worked in PHC in Astana, and their duties included providing PC to patients at home.
Measurements
At first, the nurses’ demographic and professional characteristics, such as age, gender, work experience, level of education, and participation in training courses about PC, were collected.
A translated version (Russian and Kazakh) of the palliative care quiz for nursing (PCQN), Frommelt attitudes towards care of the dying (FATCOD), and the evidence-based practice questionnaire (EBPQ) were utilized to collect the remaining data. These are specialized questionnaires that are widely used by researchers all over the world.
PCQN was developed by Ross and colleagues in 1996 (Ross et al., 1996). This quiz contains 20 questions, which are grouped into three subscales: Philosophy and principles of PC (items 1, 9, 12, 17), management and control of pain and other symptoms (items 2, 3, 4, 6, 7, 8, 10, 13, 14, 15, 16, 18, 20), and psychosocial aspects of care (items 5, 11, 19). These categories can be summarized to get a total knowledge score for each participant. Total scores range from 0 to 20, with higher scores indicating higher knowledge. The choices of answers are “true”, “false”, and “I do not know”. The final answers are coded as follows: 1 for correct answer and 0 for incorrect answer or “I do not know”. This instrument measures nurses’ basic PC knowledge. According to the data obtained by the authors, the scale demonstrated high content validity and reasonable reliability (test re-test=0.57 and Kuder-Richardson 20=0.78). The internal consistency of the translated version of this questionnaire was high (Cronbach α values for the whole scale were 0.82, as well as 0.86, 0.78, and 0.82 for the subscales).
FATCOD questionnaire (Frommelt, 1991) was used to measure the respondent’s attitude towards a dying patient and his or her family. This questionnaire consists of 30 items. Each question is rated on a 5-point Likert scale ranging from “strongly disagree=1” to “strongly agree=5”. The scale contains an equal number of positively and negatively formulated statements (15 each), with reversed scores assigned to negative statements (1=strongly agree, 2=agree, 3=not sure, 4=disagree, and 5=strongly disagree). The resulting total scores ranged from 30 to 150, with higher scores reflecting a more positive attitude and a low score indicating a negative attitude of respondents towards caring for dying patients. Twenty statements of the FATCOD scale reflect the attitude of nurses directly to the patient (a possible range of 20-100), and the remaining ten statements indicate the attitude of nurses to the patient’s family (a possible range of 10-50). The overall score is transposed to a percentage scale of 0 to 100. Scores more than 65% of the total possible score (>108) were considered positive attitudes; between 50% and 65% (91-108) neutral; and less than 50% (<91) negative attitudes (Ali & Ayoub, 2010). The validity and reliability of the FATCOD has been tested extensively. The reliability coefficient of the FATCOD scale ranges from 0.85 to 0.94. The content validity is 1.00 (Grubb & Arthur, 2015). The Cronbach α of the translated version was 0.85.
EBPQ was developed by Upton and Upton (2006). It was used to assess the nurses’ knowledge, skills, attitudes, and practice of EBP. EBPQ is a self-assessment by medical professionals of their own EBP, which describes nurses’ day-to-day use of EBP. This questionnaire contains 3 subscales that represent knowledge or skills (14 statements), attitudes (4 pairs of statements), and practice of EBP (6 statements). These 24 items are rated on a Likert-type scale from 1 to 7. The total score ranges from 24 to 168 points, with greater scores indicating higher knowledge regarding EBP, more positive attitudes, and more frequent use of EBP. Responses to each EBPQ item are considered negative if scores are between one and four (Al-Busaidi et al., 2019). Initially, 20 nurses were selected to conduct a pilot study, as a result of which we determined the Cronbach α value (total=0.88) and its values for the subscales, from 0.80 to 0.91.
All three questionnaires were used after translation, back-translation, and preliminary testing. Two independent translators, whose native languages were Russian and Kazakh, participated in the translation stage. The back-translation stage involved two independent translators whose native language was English. To check the understanding of the questionnaire, 20 PHC nurses took part in the preliminary testing stage. The Cronbach α was calculated and found acceptable in all three questionnaires.
Using Google Forms, we collected data from January 2022 to March 2023, including demographic and occupational characteristics and questions on three questionnaires: PCQN, FATCOD, and EBPQ.
Data analysis
Demographic and occupational variables were analyzed using descriptive statistics (percentage, frequency, Mean±SD). The independent t-test was used to examine the correlation between PCQN, FATCOD, EBPQ mean scores, and some characteristics: Gender and attending training regarding PC. To check the association between PCQN, FATCOD, EBPQ mean scores and age, work experience, and level of education, we used one-way analysis of variance (ANOVA). The Scheffe test was used to compare group means in ANOVA. The correlation of PCQN, FATCOD mean scores, and EBPQ scale mean scores were evaluated using the Kendall tau rank correlation coefficient. The significance level was considered at 0.05. Hierarchical multiple regression was performed to determine the factors affecting nurses’ competence level in the PC field. SPSS software, version 24, was used to analyze the data.
Results
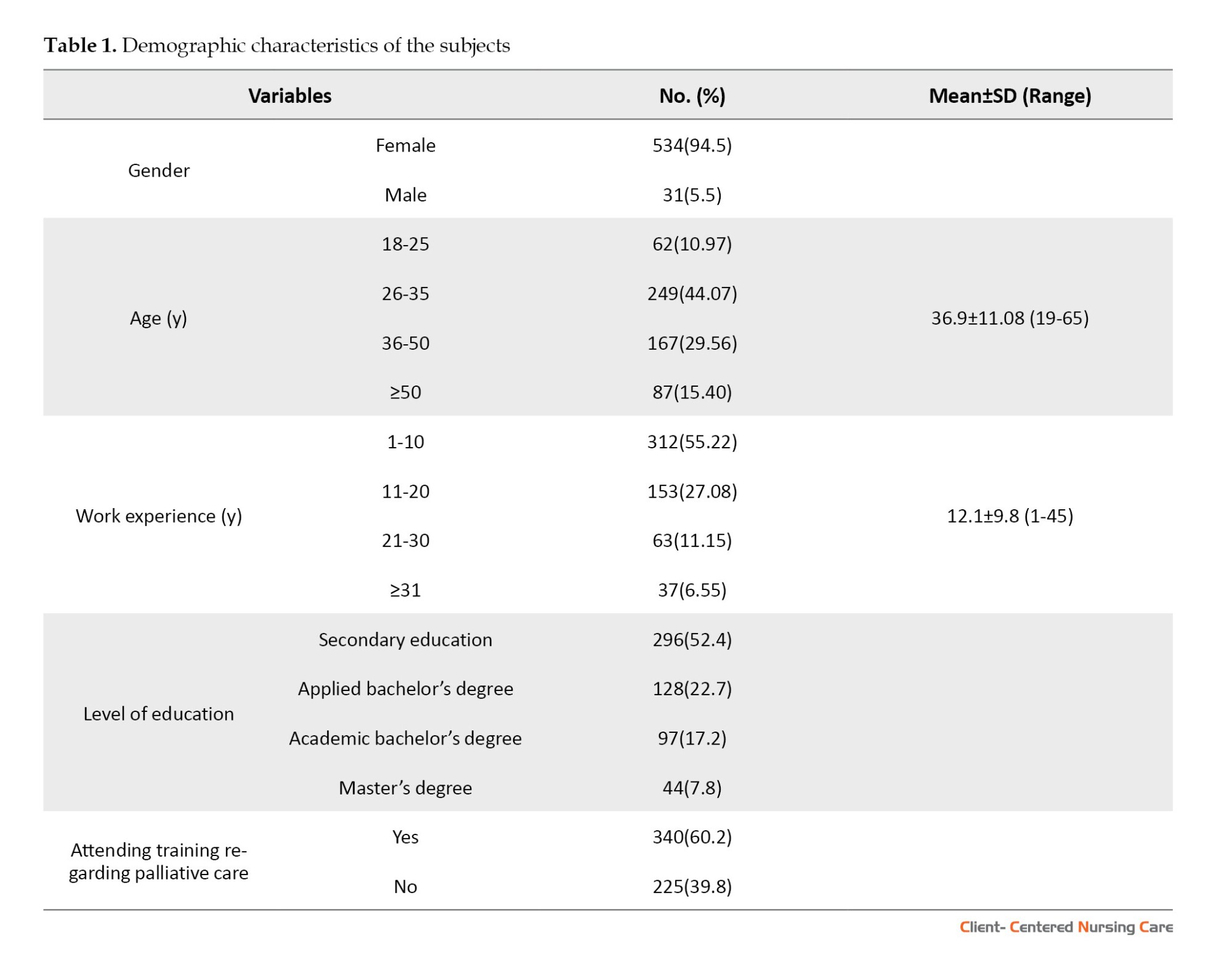
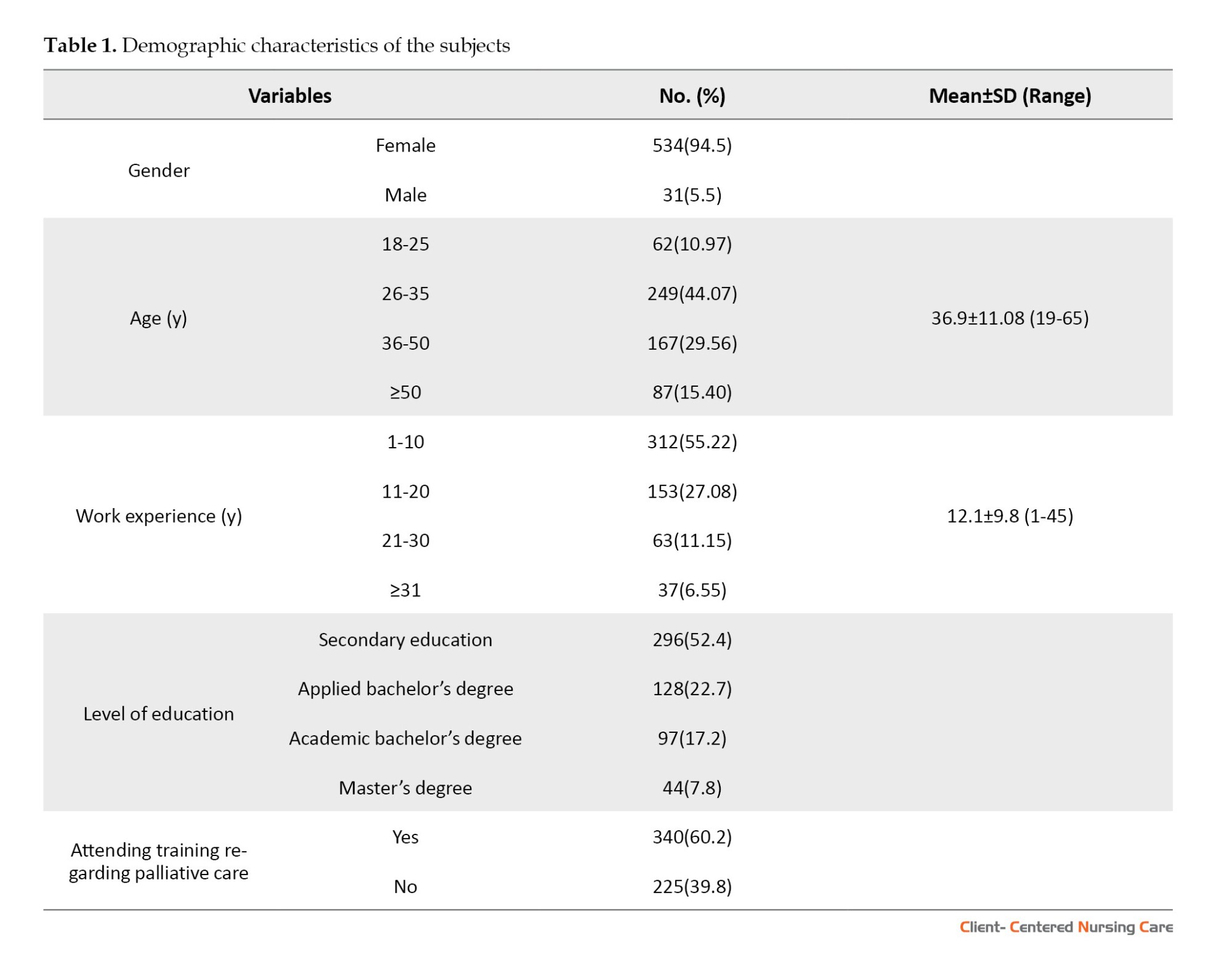
Most of the subjects were female (94.5%). The respondents’ ages ranged from 19 to 65 years, with a mean age of 36.90±11.08 years. The mean duration of their clinical experience was 12.11±9.83 years. More than half (52.4%) of the subjects held a diploma of secondary vocational education in nursing. Most nurses (60.2%) had participated in basic or advanced palliative nursing care courses at least once. Table 1 presents the respondents’ demographic characteristics.
The level of knowledge of nurses in palliative care
The total mean score of the nurses’ level of knowledge in PC at home was 9.06±2.93 out of 20. The minimum and maximum scores were 0 and 19. None of the subjects scored the highest possible score.
The results indicated that almost two-thirds of the respondents (63%) scored between 6 and 10 points, which can be interpreted as their limited knowledge. Furthermore, only 9 nurses (1.59%) scored above 15, representing adequate knowledge about PC.
Most of the correct answers to the questions were in the category of “management and control of pain and other symptoms” (49.95%). The smallest number of correct answers belonged to the “philosophy and principles of PC” (35.18%).
Nurses’ attitude towards caring for dying patients
The mean total score on FATCOD was 94.50±12.41 (approximately two-thirds of the possible score), with a range of 38-142.
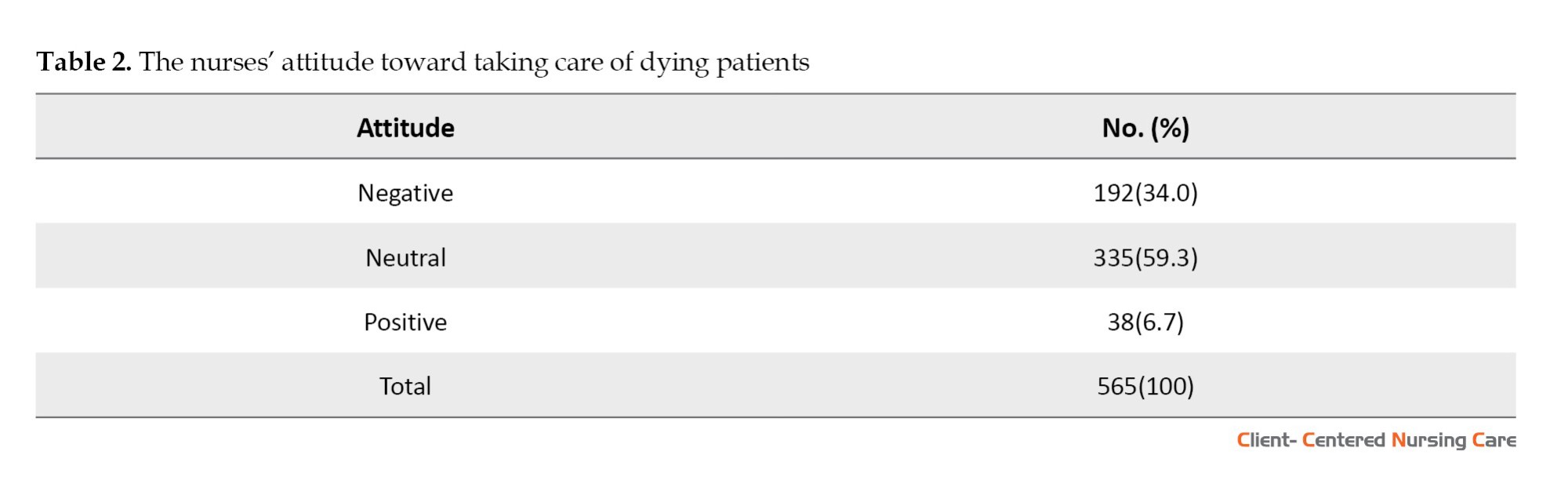
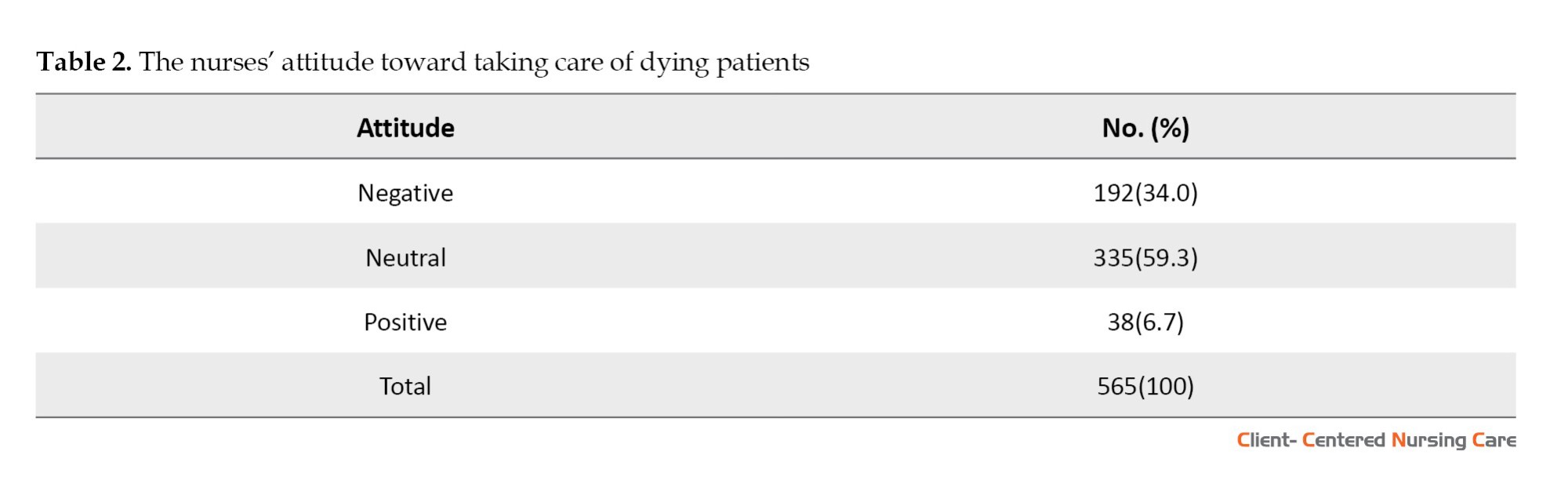
Table 2 shows that one-third of nurses (34%) had a negative attitude toward PC, and only 6.7% of respondents had a positive attitude. Most nurses (59.3%) had a neutral attitude towards caring for dying patients.
As the analysis of the nurses’ attitude towards caring for the dying showed, almost all the respondents (90%) scored 81-110 (possible score 30-150), indicating that nurses possess neutral or negative attitudes towards caring for dying patients. The mean score for attitude towards caring for the dying was 60.37±8.59, with a range of 23-88. Most nurses’ (85%) score ranged from 51 to 70 (expected range of scores 20-100). The mean score on the attitude towards patients’ families subscale was 32.92±5.48, varying from 12 to 49 (possible score 10-50), where 68% of nurses scored 31-40.
EBP knowledge, attitude, and application
The mean total score was 109.7±25.4 points out of 168 (4.39 out of 7 points (95% CI, 4.31%, 4.48%). The attitude subscale obtained the highest mean score (4.55±1.41), followed by knowledge/skills (4.45±1.28) and practice (3.90±1.31) subscales. Responses were considered negative if scores were between one and four. So, 32.6% of nurses scored below 4 points, which indicates a low level of professional competence in the field of EBP. Only 1 respondent scored the highest possible score.
Associations between demographic/professional characteristics and research variables
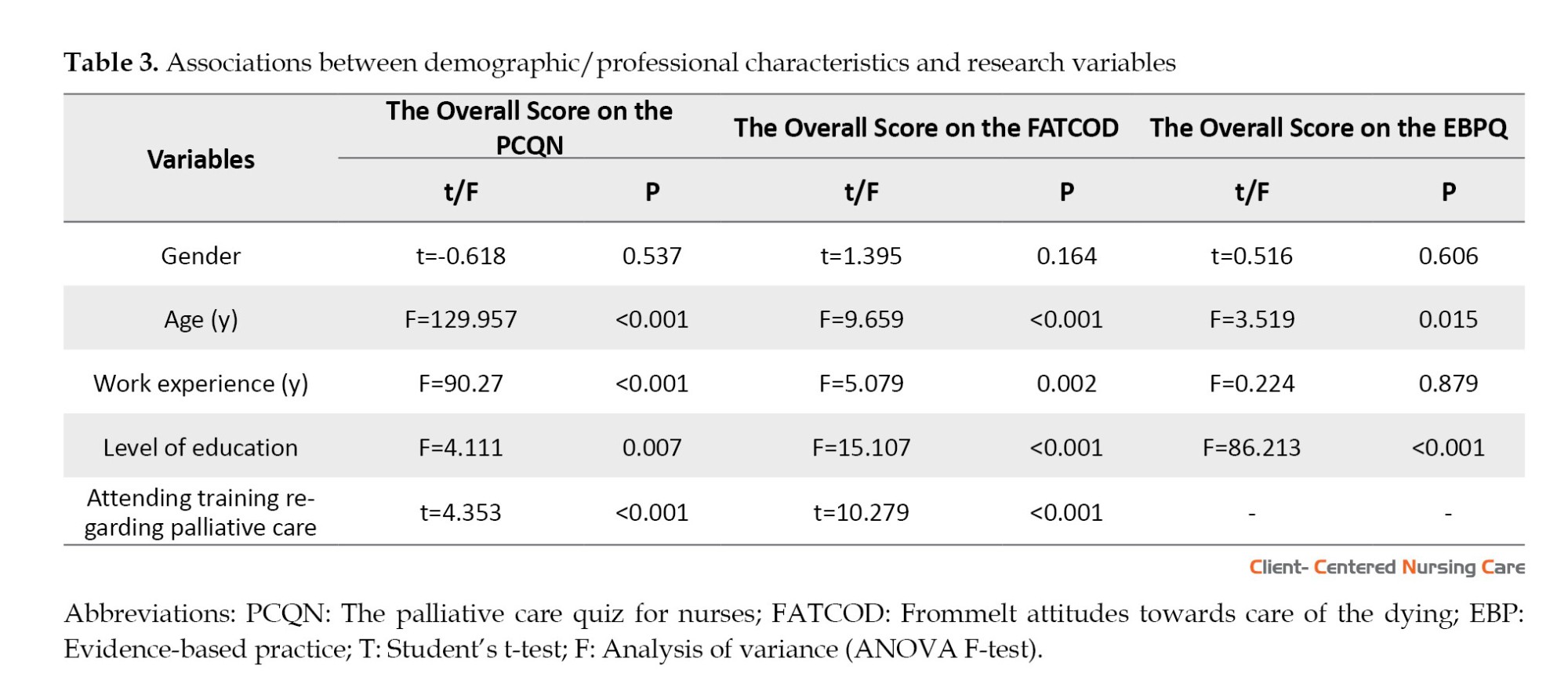
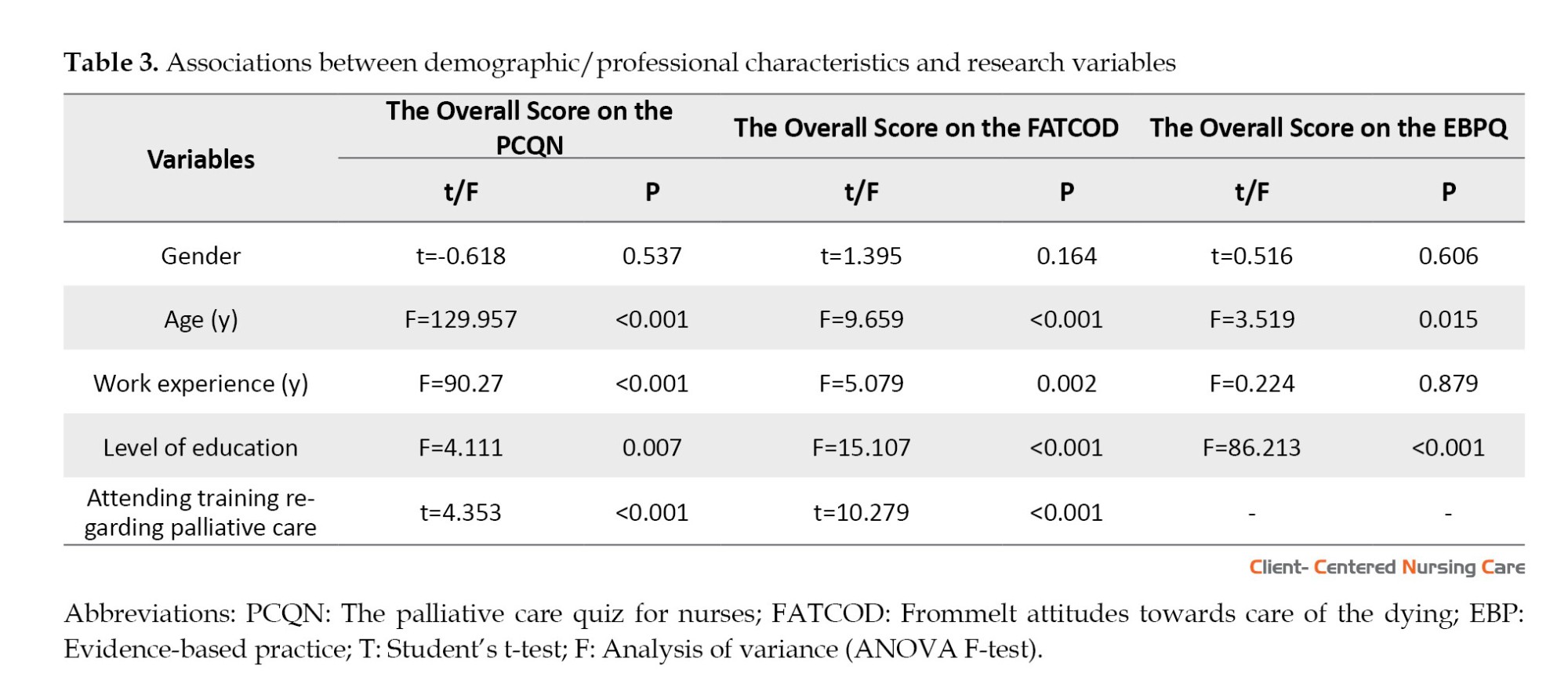
The results revealed that only older nurses (P<0.001) and those who had more work experience (P<0.001) significantly differed in their mean total score on the PCQN scale. Factors such as level of education (P=0.007) and attending training regarding PC (P=0.000) were positively associated with the total score of PCQN.
There was a significant relationship between the overall score on the FATCOD scale and almost all characteristics except for gender.
Nurses with a higher level of education obtained significantly higher total scores on the EBPQ scale (P<0.001). Significant differences were also found regarding the nurses’ age (P=0.015) (Table 3).
The relationship between the level of nurses’ preparedness to provide PC and EBP
The total score of EBPQ was significantly correlated with the total score of the PCQN scale (P=0.013) and its subscale “management and control of pain and symptoms” (P=0.032), as well as to the total score of FATCOD scale (P<0.001) and its subscales: Attitude to patient (P<0.001), attitude to family (P<0.001). The “practice” subscale of the EBPQ questionnaire was significantly correlated only with the total FATCOD scale (P<0.001) and the subscale “attitude to the patient” (P=0.003). The “knowledge/skills” subscale of the EBPQ showed a significant correlation with all variables, specifically with the PCQN scale (P=0.001), its subscales (philosophy and principles (P=0.000), psychosocial aspects (P=0.036), management and control of pain and symptoms (P=0.005), and FATCOD scale (P<0.001) and subscales (attitude to patient [P<0.001], attitude to family [P<0.001]). However, there was no significant association between the “attitude” subscale of EBPQ and other variables (Table 4).

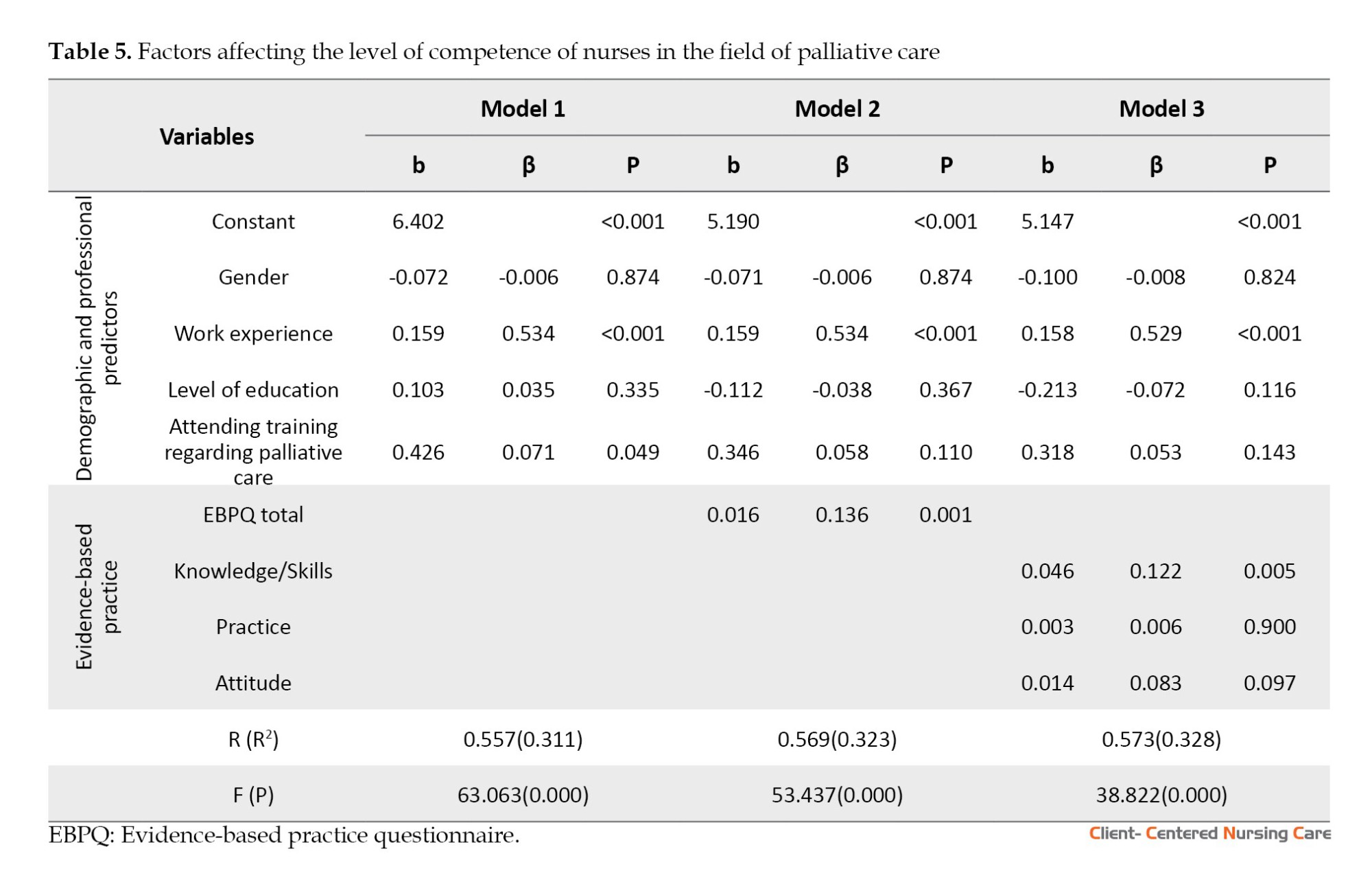
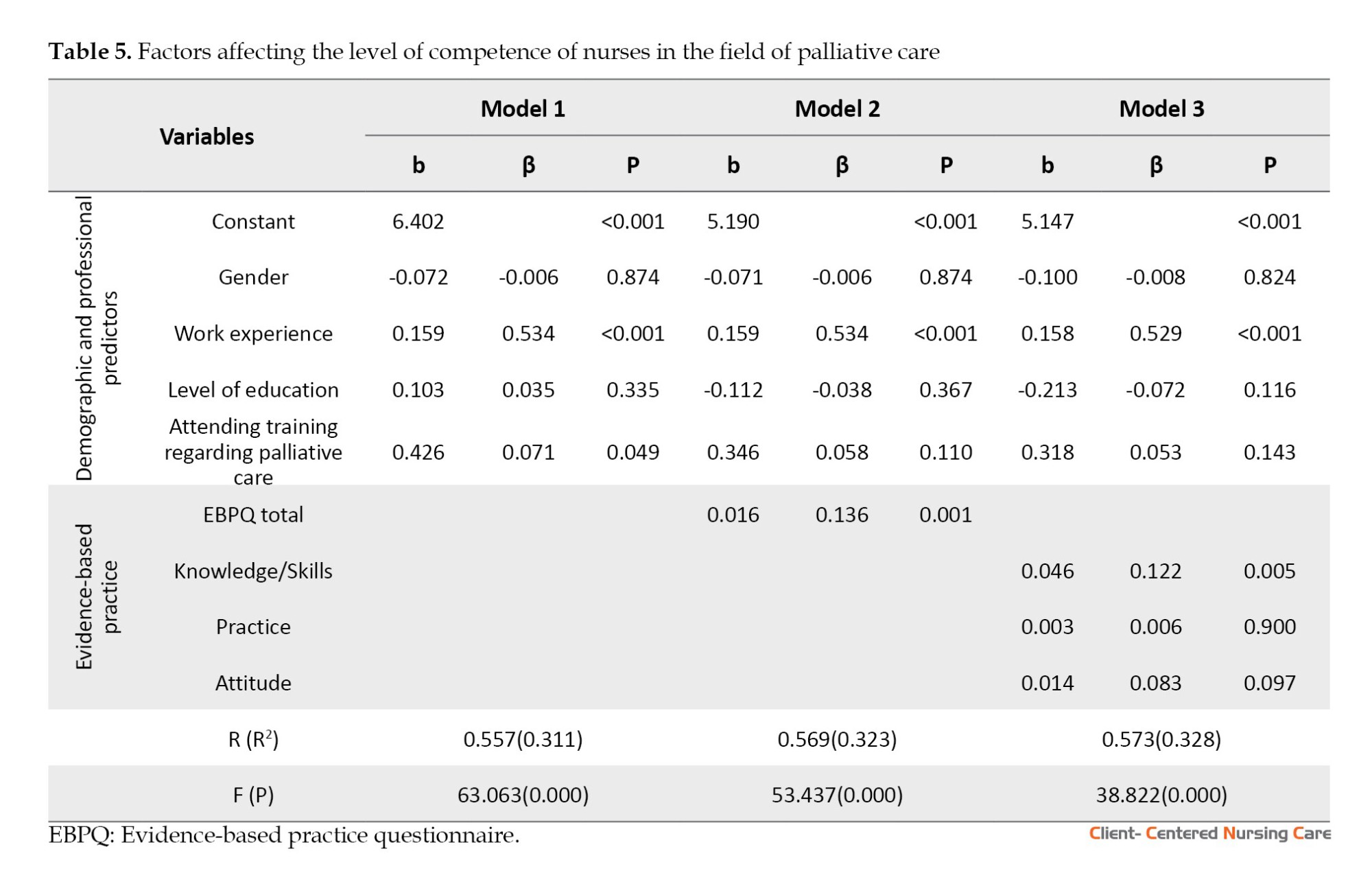
The impact of several parameters (gender, work experience, level of education, attending training regarding PC, EBPQ score, and its three subscales) on nurses’ competence level in PC was examined through a three-stage hierarchical multiple regression. Work experience was excluded from independent variables as age was highly correlated. Before regression analysis, the data were checked for multicollinearity and autocorrelation. Variance inflation factor (0.009-2.051) indicates the absence of multicollinearity. The Durbin-Watson value was 1.953, which suggests no autocorrelation.
Model 1 includes only demographic and professional factors (gender, work experience, level of education, attending training regarding PC) as predictors. The multiple correlation coefficient R-value is 0.557 (moderate correlation on the Chaddock scale). Thus, there was a positive correlation between the predictor variables and nurses’ competence level in PC. In model 1, only work experience (β=0.534; P<0.001) and attending training regarding PC (β=0.049; P<0.001) were statistically significant, although the effect of the latter was not very high. Given that R2 is 0.311, work experience and attending training regarding PC explain 31.1% of the variance of nurses’ competence level in the PC field.
Model 2 added the overall EBPQ score to demographic and professional predictors. This predictor has a statistically significant direct relationship with the level of knowledge about PC (β=0.136; P=0.001). The work experience remained statistically significant (β=0.534; P<0.001). The remaining predictors remained statistically insignificant. The R-value for model 2 is 0.569 (R2=0.323); therefore, the model explains 32.3% of the variance.
In model 3, the overall EBPQ score was replaced by its three subscales (knowledge/skills, practice, attitude). The values of R and R2 slightly increased to 0.573 and 0.328, respectively. Therefore, the model explains 32.8% of the variance. Among the three subscales, only the knowledge/skills scale demonstrated a statistically significant impact on nurses’ competence level in PC (β=0.122; P=0.005). The subscales of practice and attitude were not statistically significant (β=0.006 [P=0.900] and β=0.083 [P=0.097], respectively). As in the previous model, work experience is still statistically significant (β=0.529; P<0.001).
It could be seen that all three models were significant (P<0.001). It was noted that the F value was largest for the model 1 (63.063) (Table 5).
Discussion
The present study assessed the level of nurses’ knowledge about PC and attitude towards caring for dying patients and its relationship with EBP (knowledge/skills, attitude, and practice) among nurses of PHC organizations. To the best of our knowledge, this is the first study that examines these relationships among nurses of PHC organizations.
Our findings indicated that the nurses’ knowledge about PC was low or inadequate (total means score 9.06 out of 20). Similar findings have been reported by previous studies conducted in Ethiopia (Etafa et al., 2020), Iran (Dehghannezhad et al., 2021), and India (Gupta et al., 2023). However, compared with other published literature in which the PCQN was also used, the total PCQN score in our study was higher than that of Southeastern Iranian nurses (Iranmanesh et al., 2014), Indonesian (Hertanti et al., 2021), Palestinian (Toqan et al., 2023), and Mongolian (Gelegjamts et al., 2020) nurses, where the mean scores were 7.59±2.28, 7.78±3.56, 7.75±2.96, and 7.15±2.31, respectively. However, studies conducted in countries where PC is well developed have shown better results than in our study (12.89 and 12.3 points) (Mitchell et al., 2016; Raudonis et al., 2002). Similar to the results of this study, in many previous studies, the highest number of correct answers was related to the pain and symptom management subscale (Abuhammad et al., 2021; Dimoula et al., 2019). The reason for the higher level of knowledge about pain relief and other related symptoms may be that nurses, especially those working in PHC organizations, often care for patients with chronic diseases who require daily pain relief and symptom control.
Disciplines on PC have been introduced in Kazakhstan medical universities and colleges, and advanced training courses have been designed. Despite this, our study showed that 40% of nurses have never been trained in PC. This result is consistent with previous studies conducted in Palestine (Abu-Odah et al., 2022), Jordan (Abuhammad et al., 2021), and Egypt (Mohamed & Ibrahim, 2021).
The mean score of the FATCOD was 94.50 (i.e. neutral attitude), and the majority of nurses (59.3%) had a neutral attitude toward caring for dying patients. It is higher than the results found among nurses in Ethiopian public hospitals (Etafa et al., 2020) and Nigerian teaching hospitals (Faronbi et al., 2021) but lower than that of nurses in Australia (Tait et al., 2015), Vietnam (Nguyen & Nguyen, 2015), Japan (Matsui, 2022), and the USA (Clemens et al., 2021). Differences in the attitude of nurses may indicate differences in beliefs and cultural characteristics of the above regions that need to be investigated.
In our study, work experience and attending PC training were significantly associated with the nurses’ attitude toward caring for dying patients. Similar results have been obtained by a study in Sweden among registered nurses and undergraduate nursing students, which revealed the positive impact of long work experience and attendance at PC courses on the overall FATCODE mean score (Fristedt et al., 2021).
Furthermore, our study established that nurses’ age and level of education influenced their attitudes toward caring for dying patients. Thus, older nurses and those with a higher level of education showed a more positive attitude. These factors are strongly supported by similar studies in Jordan (Abu Hasheesh et al., 2013; Zahran et al., 2022) and Iran (Jafari et al., 2015).
The correlation between knowledge and attitude toward dying patients that we found in this study is confirmed by previous studies (Etafa et al., 2020; Dimoula et al., 2019; Kim et al., 2020). Although, some studies have not found such a relationship (Iranmanesh et al., 2014; Zhou et al., 2020). The mean score on EBPQ was 4.39 out of 7 points in the present study. This score is slightly higher than the result obtained from registered nurses in traditional Chinese medicine hospitals (Zhou et al., 2016) but lower than that of surveys conducted in Spain and Latin America, Oman, Egypt, and Jordan, where the mean scores ranged between 4.96 and 5.5 (Al-Busaidi et al., 2019; Pеrez-Campos et al., 2014; Youssef et al., 2018).
In our study, as in most other similar studies, EBPQ subscale scores were highest for “attitude” followed by “knowledge/skills” and “practice” (Maydick-Youngberg et al., 2021). According to the results of our research, most nurses scored low on the “practice subscale”. This finding is consistent with another study conducted among nurses in Nepal, where nurses’ scores on the three subscales were arranged in the same sequence (Karki et al., 2015). Also, in their study, Karki and colleagues mentioned a lack of time and resources, difficulty understanding research articles and translating the findings to practice, and limited autonomy to modify their practice according to EBP as the greatest barriers (Karki et al., 2015).
The results regarding the factors affecting EBP were contradictory. We have found a statistically significant influence of age and level of education, but some studies refute this (Al-Busaidi et al., 2019; Zhou et al., 2016).
Conclusion
Our findings were indicative of insufficient knowledge about PC and a neutral or negative attitude towards caring for dying patients among nurses working in PHC organizations in Astana. Demographic and professional factors such as age, work experience, level of education, and attending PC training affected the nurses’ knowledge about PC and attitude towards caring for dying patients.
The lack of knowledge and skills of nurses in the field of EBP may contribute to insufficient knowledge about PC, possibly due to the lack of knowledge necessary to formulate a clinical question, search, and selection of scientific publications. It may be necessary to strengthen the theoretical part of the nursing curriculum in the “evidence-based practice” section and to add continuing PC education to the nursing curriculum to improve the quality of end-of-life care. Implementing initiatives and strategies to promote EBP among nurses in various medical institutions could use the results of this study as a foundation. Future studies may be required to investigate this issue because this study did not specifically address barriers to EBP in PC.
There were some limitations in our study. Two of the three questionnaires used in our research are self-report questionnaires (PCQN was a true-false scale, but FATCOD and EBPQ were self-reported questionnaires), which can lead to potential bias and overestimation of some results. This study was conducted only in the city of Astana, which reduces the generalization of the results obtained. Finally, cross-sectional research allows us to determine associations, but not causal relationships, when analyzing potential predictors of nurses’ knowledge and attitude and their relationship with their EBP.
Ethical Considerations
Compliance with ethical guidelines
Before starting the study, we received formal permission from the Local Bioethical Committee of NpJSC Astana Medical University (Protocol No.: 15 of October 21, 2021). This study was conducted in accordance with ethical principles (Helsinki Declaration, developed in 1964). The survey was anonymous, and its purpose and implications for the research results were explained before it began. Each participant was asked to sign an informed consent form.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Investigation, data gathering, and data analysis: Masharipova Alexandra and Nurgaliyeva Nassikhat; Supervision: Derbissalina Gulmira; Conceptualization, study design, writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to the heads of Primary Health Care Organizations in Astana for their support and access to nurses. The authors are also grateful to all the nurses who participated in the study.
References
Hasheesh, M. O. A., et al., 2013. Nurses’ characteristics and their attitudes toward death and caring for dying patients in a public hospital in Jordan. Health Science Journal, 7(4), pp. 384-94. [Link]
Abuhammad, S., et al., 2021. Knowledge of pediatric palliative care among medical students in Jordan: A cross-sectional study. Annals of Medicine and Surgery (2012), 64, pp. 102246. [DOI:10.1016/j.amsu.2021.102246] [PMID]
Abu-Odah, H., Molassiotis, A. & Liu, J. Y. W., 2022. Assessment of the educational and health care system-related issues from physicians’ and nurses’ perspectives before developing a palliative care program within the palestinian health care system: A cross-sectional study. Journal of Hospice and Palliative Nursing, 24(3), pp. E59–75. [DOI:10.1097/NJH.0000000000000840] [PMID]
Achora, S. & Labrague, L. J., 2019. An integrative review on knowledge and attitudes of nurses toward palliative care: Implications for practice. Journal of Hospice and Palliative Nursing, 21(1), pp. 29-37. [DOI:10.1097/NJH.0000000000000481] [PMID]
Ali, W. G. M. & Ayoub, N. S., 2010. Nurses’ attitudes towards caring for dying patient in Mansoura University hospitals. Journal of Medicine and Biomedical Sciences, 1(1), pp. 16-23. [Link]
Al-Busaidi, I. S., et al., 2019. Nurses’ knowledge, attitudes, and implementation of evidence-based practice in Oman: A multi-institutional, cross-sectional study. Oman Medical Journal, 34(6), pp. 521–7. [DOI:10.5001/omj.2019.95] [PMID]
Clemens, E. J., et al., 2021. Effect of death and dying elective on student empathy and attitudes toward mortality. Currents in Pharmacy Teaching & Learning, 13(12), pp. 1627–33. [DOI:10.1016/j.cptl.2021.09.029] [PMID]
Cross L. A., 2019. Compassion fatigue in palliative care nursing: A concept analysis. Journal of Hospice and Palliative Nursing, 21(1), pp. 21-8. [DOI:10.1097/NJH.0000000000000477] [PMID]
Dehghannezhad, J., et al., 2021. Home care nurses’ attitude towards and knowledge of home palliative care in Iran: A cross-sectional study. Iranian Journal of Nursing and Midwifery Research, 26(3), pp. 272–8. [DOI:10.4103/ijnmr.IJNMR_249_19] [PMID]
Dimoula, M., et al., 2019. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurse Education Today, 74, pp. 7–14. [DOI:10.1016/j.nedt.2018.11.025] [PMID]
Etafa, W., et al., 2020. Nurses’ knowledge about palliative care and attitude towards end- of-life care in public hospitals in Wollega zones: A multicenter cross-sectional study. Plos One, 15(10), pp. e0238357. [DOI:10.1371/journal.pone.0238357] [PMID]
Faronbi, J. O., et al., 2021. Nurses’ attitude toward caring for dying patients in a Nigerian Teaching Hospital. SAGE Open Nursing, 7, pp. 23779608211005213. [DOI:10.1177/23779608211005213] [PMID]
Fristedt, S., et al., 2021. Registered nurses and undergraduate nursing students’ attitudes to performing end-of-life care. Nurse Education Today, 98, pp. 104772. [DOI:10.1016/j.nedt.2021.104772] [PMID]
Frommelt, K. H., 1991. The effects of death education on nurses’ attitudes toward caring for terminally ill persons and their families. The American Journal of Hospice & Palliative Care, 8(5), pp. 37–43. [DOI:10.1177/104990919100800509] [PMID]
Gelegjamts, D., et al., 2020. Undergraduate nursing students’ palliative care knowledge and attitudes towards end-of-life care: A cross-sectional descriptive study. Contemporary Nurse, 56(5-6), pp. 477–90. [DOI:10.1080/10376178.2021.1890165] [PMID]
Grubb, C. & Arthur, A., 2016. Student nurses’ experience of and attitudes towards care of the dying: A cross-sectional study. Palliative Medicine, 30(1), pp. 83–8. [DOI:10.1177/0269216315616762] [PMID]
Gupta, M., et al., 2023. Impact of end-of-life nursing education consortium on palliative care knowledge and attitudes towards care of dying of nurses in India: A Quasi-Experimental Pre-Post Study. The American Journal of Hospice & Palliative Care, 40(5), pp. 529–38. [DOI:10.1177/10499091221108342] [PMID]
Hertanti, N. S., et al., 2021. Palliative Care Quiz for Nurses-Indonesian Version (PCQN-I): A cross-cultural adaptation, validity, and reliability study. Indian Journal of Palliative Care, 27(1), pp. 35–42. [DOI:10.4103/IJPC.IJPC_76_20] [PMID]
Iranmanesh, S., et al., 2014. Nurses’ knowledge about palliative care in Southeast Iran. Palliative & Supportive Care, 12(3), pp. 203–10. [DOI:10.1017/S1478951512001058] [PMID]
Jafari, M., et al., 2015. Caring for dying patients: attitude of nursing students and effects of education. Indian Journal of Palliative Care, 21(2), pp. 192–7. [DOI:10.4103/0973-1075.156497] [PMID]
Karki, S., et al., 2015. Perceptions and attitudes towards evidence based practice among nurses and nursing students in Nepal. Kathmandu University Medical Journal (KUMJ), 13(52), pp. 308–15. [DOI:10.3126/kumj.v13i4.16829] [PMID]
Kim, S., Lee, K. & Kim, S., 2020. Knowledge, attitude, confidence, and educational needs of palliative care in nurses caring for non-cancer patients: A cross-sectional, descriptive study. BMC Palliative Care, 19(1), pp. 105. [DOI:10.1186/s12904-020-00581-6] [PMID]
Kunirova, G. & Shakenova, A., 2018. Palliative care in Kazakhstan. Journal of Pain and Symptom Management, 55(2S), pp. S36–40. [DOI:10.1016/j.jpainsymman.2017.03.028] [PMID]
Masharipova, A., Nurgaliyeva, N. & Derbissalina, G., 2022. The problem of preparedness of nursing staff to provide palliative nursing care (a literature review). Georgian Medical News, (325), pp. 27–32. [PMID]
Mathieson, A., Grande, G. & Luker, K., 2019. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: A systematic mixed-studies review and qualitative synthesis. Primary Health Care Research & Development, 20, pp. e6. [DOI:10.1017/S1463423618000488] [PMID]
Matsui, M., 2022. Nurses’ symptom management and views on death and caring for heart failure and chronic obstructive pulmonary disease. International Journal of Palliative Nursing, 28(5), pp. 214–21.[DOI:10.12968/ijpn.2022.28.5.214] [PMID]
Maydick-Youngberg D, Gabbe L, Simmons G, et al. (2021). Assessing evidence-based practice knowledge: An innovative approach by a nursing research council. Journal of Nursing Administration, 51(5):279-286. [DOI:10.1097/NNA.0000000000001013] [PMID]
Mills, J., Wand, T. & Fraser, J. A., 2018. Exploring the meaning and practice of self-care among palliative care nurses and doctors: A qualitative study. BMC Palliative Care, 17(1), pp. 63. [DOI:10.1186/s12904-018-0318-0] [PMID]
Mitchell, G., et al., 2016. Care home managers’ knowledge of palliative care: A Northern Irish study. International Journal of Palliative Nursing, 22(5), pp. 230–5. [DOI:10.12968/ijpn.2016.22.5.230] [PMID]
Mohamed R. F. & Ibrahim, R. A., 2021. Effect of palliative care guideline on nurses’ knowledge, attitude, and practice at intensive care unit. Egyptian Journal of Nursing and Health Sciences, 2(2), pp. 81-109. [DOI:10.21608/ejnhs.2021.196022]
Nguyen, L.T. & Nguyen, H. T., 2015. Attitudes towards caring for terminally-ill patients among in-serviced nursing students at Hanoi Medical University, Vietnam. Vietnam Journal of Medicine and Pharmacy, 7(1), pp. 55-63. [Link]
Ministry of Justice of the Republic of Kazakhstan. State program for the development of healthcare of the Republic of Kazakhstan for 2020 – 2025 [Internet]. Viewed 13 March 2023, [Link]
Lakasing, E., 2013. Palliative care in primary care [Inretnet]. Viewed 23 Apr 2023, [Link]
Pérez-Campos, M. A., et al., 2014. Knowledge, attitude and use of evidence-based practice among nurses active on the internet. Investigacion Y Educacion en Enfermeria, 32(3), pp. 451–60. [DOI:10.17533/udea.iee.v32n3a10] [PMID]
Raudonis, B. M., Kyba, F. C. & Kinsey, T. A., 2002. Long-term care nurses’ knowledge of end-of-life care. Geriatric Nursing (New York, N.Y.), 23(6), pp. 296–301. [DOI:10.1067/mgn.2002.130270] [PMID]
Ross MM, McDonald B, McGuinness J. (1996). The palliative care quiz for nursing (PCQN): the development of an instrument to measure nurses’ knowledge of palliative care. J Adv Nurs. 23(1):126-137. [DOI:10.1111/j.1365-2648.1996.tb03106.x] [PMID]
Rosa, W. E., 2018. Integrating palliative care into global health initiatives: opportunities and challenges. Journal of Hospice and Palliative Nursing, 20(2), pp. 195–200. [DOI:10.1097/NJH.0000000000000415] [PMID]
Schroeder, K. & Lorenz, K., 2018. Nursing and the future of palliative care. Asia-Pacific Journal of Oncology Nursing, 5(1), pp. 4–8. [DOI:10.4103/apjon.apjon_43_17] [PMID]
Sekse, R. J. T., Hunskår, I. & Ellingsen, S., 2018. The nurse’s role in palliative care: A qualitative meta-synthesis. Journal of Clinical Nursing, 27(1-2), pp. e21–e38. [DOI:10.1111/jocn.13912] [PMID]
Tait, V., et al., 2015. Attitudes of nonpalliative care nurses towards palliative care. International Journal of Palliative Care, 2015, pp. 1-6. [DOI:10.1155/2015/469174]
Toqan, D., et al., 2023. Perception of nurses’ knowledge about palliative care in West Bank/ Palestine: Levels and influencing factors. Journal of Palliative Care, 38(3), pp. 336–44.[DOI:10.1177/08258597221133958] [PMID]
Upton D, Upton P., (2006). Development of an evidence-based practice questionnaire for nurses. Journal of Advanced Nursing., 53(4):454-8. [DOI: 10.1111/j.1365-2648.2006.03739.x] [PMID]
Wang, L. P., et al., 2016. Development and Psychometric Testing Chinese Version of the Frommelt Attitude Toward Care of the Dying Scale, Form B in nurses and nursing students. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education, 31(1), pp. 123–30. [DOI:10.1007/s13187-015-0810-7] [PMID]
World Health Organization (WHO), 2020. Palliative care. Geneva: WHO. [Link]
World Health Organization. Integrating palliative care and sumptom relief into primary health care. Geneva: World Health Organization; 2018. [Link]
Youssef, N. F. A., et al., 2018. Egyptian and Jordanian nurse educators’ perception of barriers preventing the implementation of evidence-based practice: A cross-sectional study. Nurse Education Today, 64, pp. 33–41. [DOI:10.1016/j.nedt.2018.01.035] [PMID]
Zhou, F., et al., 2016. Attitude, knowledge, and practice on evidence-based nursing among registered nurses in traditional Chinese medicine hospitals: A multiple center cross-sectional survey in China. Evidence-Based Complementary and Alternative Medicine: eCAM, 2016, pp. 5478086. [DOI:10.1155/2016/5478086] [PMID]
Zahran, Z., et al., 2022. Nursing students’ attitudes towards death and caring for dying patients. Nursing Open, 9(1), pp. 614–23. [DOI:10.1002/nop2.1107] [PMID]
Zhou, Y., Li, Q. & Zhang, W., 2020. Undergraduate nursing students’ knowledge, attitudes and self-efficacy regarding palliative care in China: A descriptive correlational study. Nursing Open, 8(1), pp. 343–53. [DOI:10.1002/nop2.635] [PMID]
The World Health Organization (WHO) defines palliative care (PC) as improving the quality of life of seriously-ill patients and their families facing a life-threatening illness. PC includes physical, psychological, social, and spiritual aspects (WHO, 2020). PC should not be provided only at the end of the patient’s life; it should begin from the moment of diagnosis and continue throughout the entire period of the disease (Mills et al., 2018).
Nurses spend more time with patients and their families than other healthcare professionals. Qualified care reduces the suffering and burden of seriously-ill patients (Schroeder & Lorenz, 2018). Palliative nursing is a holistic approach to managing the symptoms of incurable diseases while simultaneously eliminating pain and other symptoms, psychosocial problems, maintaining spirituality, and the quality of life of a seriously-ill patient (Cross, 2019).
PC is successfully implemented due to the combined influence of good knowledge, attitudes, beliefs, and extensive experience of medical professionals. The negative attitude of nurses towards death and the care of dying people can significantly affect the quality of PC (Wang et al., 2016).
It is necessary to note the important role of nurses in ensuring universal access to PC, especially at the primary health care (PHC) stage, because the vast majority of people in need of PC prefer to die at home. Therefore, from a medical and ethical point of view, PC must be provided at home as part of PHC (WHO, 2018; Lakasing, 2023).
Nurses often have to master several functions on their right at home at the patient’s bedside because PC is a complex integrated approach that requires a specialist’s developed practical skills and personal qualities. Evidence-based practice (EBP) plays an essential role in navigating situations better at the bedside of patients (Sekse et al., 2018; Rosa, 2018). It is proven that nurses who actively combine patient preferences with EBP can improve the quality of life of patients and individual care (Achora & Labrague, 2019). However, at the moment, there are no studies devoted to the problem of the introduction of evidence-based medicine in nursing care at the PHC stage. Most scientific research on introducing evidence-based nursing was conducted in inpatient hospitals (Mathieson et al., 2019). Many countries already have mobile PC teams consisting of doctors, nurses, physiotherapists, and social workers who provide PC at home. In Kazakhstan, such mobile brigades are just beginning to form, but they still do not function properly. The new state program of Healthcare Development for 2020-2025 in Kazakhstan provides for the creation of mobile teams in all PHC organizations throughout the country by 2025 to increase the availability of PC services, regardless of the geographical and financial situation of citizens (Ministry of Justice of the Republic of Kazakhstan, 2019).
Although the palliative care system in Kazakhstan has been reformed several times, according to statistics, more than 80% of doctors and nurses lack basic knowledge of palliative care (Masharipova et al., 2022). The problem of training PC specialists should be recognized at the state level. It is necessary to improve the system for training medical specialists in PC (Kunirova & Shakenova, 2017). Thus, this study aimed to assess nurses’ knowledge of PC and attitudes towards caring for dying patients and its relationship with their EBP (knowledge/skills, attitude, and practice) in PHC organizations of Astana City, Kazakhstan.
Materials and Methods
Study design and participants
This descriptive, cross-sectional study was conducted from 2022 to 2023. Ten PHC organizations in the city of Astana were randomly selected. The sample size was computed considering that approximately 3000 nurses are officially employed in Astana City organizations. A convenience sampling method was used to choose the subjects, and a total of 565 nurses working in PHC organizations in Astana and providing PC for seriously-ill patients at home as part of PHC were recruited. The inclusion criteria were nurses who worked in PHC in Astana, and their duties included providing PC to patients at home.
Measurements
At first, the nurses’ demographic and professional characteristics, such as age, gender, work experience, level of education, and participation in training courses about PC, were collected.
A translated version (Russian and Kazakh) of the palliative care quiz for nursing (PCQN), Frommelt attitudes towards care of the dying (FATCOD), and the evidence-based practice questionnaire (EBPQ) were utilized to collect the remaining data. These are specialized questionnaires that are widely used by researchers all over the world.
PCQN was developed by Ross and colleagues in 1996 (Ross et al., 1996). This quiz contains 20 questions, which are grouped into three subscales: Philosophy and principles of PC (items 1, 9, 12, 17), management and control of pain and other symptoms (items 2, 3, 4, 6, 7, 8, 10, 13, 14, 15, 16, 18, 20), and psychosocial aspects of care (items 5, 11, 19). These categories can be summarized to get a total knowledge score for each participant. Total scores range from 0 to 20, with higher scores indicating higher knowledge. The choices of answers are “true”, “false”, and “I do not know”. The final answers are coded as follows: 1 for correct answer and 0 for incorrect answer or “I do not know”. This instrument measures nurses’ basic PC knowledge. According to the data obtained by the authors, the scale demonstrated high content validity and reasonable reliability (test re-test=0.57 and Kuder-Richardson 20=0.78). The internal consistency of the translated version of this questionnaire was high (Cronbach α values for the whole scale were 0.82, as well as 0.86, 0.78, and 0.82 for the subscales).
FATCOD questionnaire (Frommelt, 1991) was used to measure the respondent’s attitude towards a dying patient and his or her family. This questionnaire consists of 30 items. Each question is rated on a 5-point Likert scale ranging from “strongly disagree=1” to “strongly agree=5”. The scale contains an equal number of positively and negatively formulated statements (15 each), with reversed scores assigned to negative statements (1=strongly agree, 2=agree, 3=not sure, 4=disagree, and 5=strongly disagree). The resulting total scores ranged from 30 to 150, with higher scores reflecting a more positive attitude and a low score indicating a negative attitude of respondents towards caring for dying patients. Twenty statements of the FATCOD scale reflect the attitude of nurses directly to the patient (a possible range of 20-100), and the remaining ten statements indicate the attitude of nurses to the patient’s family (a possible range of 10-50). The overall score is transposed to a percentage scale of 0 to 100. Scores more than 65% of the total possible score (>108) were considered positive attitudes; between 50% and 65% (91-108) neutral; and less than 50% (<91) negative attitudes (Ali & Ayoub, 2010). The validity and reliability of the FATCOD has been tested extensively. The reliability coefficient of the FATCOD scale ranges from 0.85 to 0.94. The content validity is 1.00 (Grubb & Arthur, 2015). The Cronbach α of the translated version was 0.85.
EBPQ was developed by Upton and Upton (2006). It was used to assess the nurses’ knowledge, skills, attitudes, and practice of EBP. EBPQ is a self-assessment by medical professionals of their own EBP, which describes nurses’ day-to-day use of EBP. This questionnaire contains 3 subscales that represent knowledge or skills (14 statements), attitudes (4 pairs of statements), and practice of EBP (6 statements). These 24 items are rated on a Likert-type scale from 1 to 7. The total score ranges from 24 to 168 points, with greater scores indicating higher knowledge regarding EBP, more positive attitudes, and more frequent use of EBP. Responses to each EBPQ item are considered negative if scores are between one and four (Al-Busaidi et al., 2019). Initially, 20 nurses were selected to conduct a pilot study, as a result of which we determined the Cronbach α value (total=0.88) and its values for the subscales, from 0.80 to 0.91.
All three questionnaires were used after translation, back-translation, and preliminary testing. Two independent translators, whose native languages were Russian and Kazakh, participated in the translation stage. The back-translation stage involved two independent translators whose native language was English. To check the understanding of the questionnaire, 20 PHC nurses took part in the preliminary testing stage. The Cronbach α was calculated and found acceptable in all three questionnaires.
Using Google Forms, we collected data from January 2022 to March 2023, including demographic and occupational characteristics and questions on three questionnaires: PCQN, FATCOD, and EBPQ.
Data analysis
Demographic and occupational variables were analyzed using descriptive statistics (percentage, frequency, Mean±SD). The independent t-test was used to examine the correlation between PCQN, FATCOD, EBPQ mean scores, and some characteristics: Gender and attending training regarding PC. To check the association between PCQN, FATCOD, EBPQ mean scores and age, work experience, and level of education, we used one-way analysis of variance (ANOVA). The Scheffe test was used to compare group means in ANOVA. The correlation of PCQN, FATCOD mean scores, and EBPQ scale mean scores were evaluated using the Kendall tau rank correlation coefficient. The significance level was considered at 0.05. Hierarchical multiple regression was performed to determine the factors affecting nurses’ competence level in the PC field. SPSS software, version 24, was used to analyze the data.
Results
Most of the subjects were female (94.5%). The respondents’ ages ranged from 19 to 65 years, with a mean age of 36.90±11.08 years. The mean duration of their clinical experience was 12.11±9.83 years. More than half (52.4%) of the subjects held a diploma of secondary vocational education in nursing. Most nurses (60.2%) had participated in basic or advanced palliative nursing care courses at least once. Table 1 presents the respondents’ demographic characteristics.
The level of knowledge of nurses in palliative care
The total mean score of the nurses’ level of knowledge in PC at home was 9.06±2.93 out of 20. The minimum and maximum scores were 0 and 19. None of the subjects scored the highest possible score.
The results indicated that almost two-thirds of the respondents (63%) scored between 6 and 10 points, which can be interpreted as their limited knowledge. Furthermore, only 9 nurses (1.59%) scored above 15, representing adequate knowledge about PC.
Most of the correct answers to the questions were in the category of “management and control of pain and other symptoms” (49.95%). The smallest number of correct answers belonged to the “philosophy and principles of PC” (35.18%).
Nurses’ attitude towards caring for dying patients
The mean total score on FATCOD was 94.50±12.41 (approximately two-thirds of the possible score), with a range of 38-142.
Table 2 shows that one-third of nurses (34%) had a negative attitude toward PC, and only 6.7% of respondents had a positive attitude. Most nurses (59.3%) had a neutral attitude towards caring for dying patients.
As the analysis of the nurses’ attitude towards caring for the dying showed, almost all the respondents (90%) scored 81-110 (possible score 30-150), indicating that nurses possess neutral or negative attitudes towards caring for dying patients. The mean score for attitude towards caring for the dying was 60.37±8.59, with a range of 23-88. Most nurses’ (85%) score ranged from 51 to 70 (expected range of scores 20-100). The mean score on the attitude towards patients’ families subscale was 32.92±5.48, varying from 12 to 49 (possible score 10-50), where 68% of nurses scored 31-40.
EBP knowledge, attitude, and application
The mean total score was 109.7±25.4 points out of 168 (4.39 out of 7 points (95% CI, 4.31%, 4.48%). The attitude subscale obtained the highest mean score (4.55±1.41), followed by knowledge/skills (4.45±1.28) and practice (3.90±1.31) subscales. Responses were considered negative if scores were between one and four. So, 32.6% of nurses scored below 4 points, which indicates a low level of professional competence in the field of EBP. Only 1 respondent scored the highest possible score.
Associations between demographic/professional characteristics and research variables
The results revealed that only older nurses (P<0.001) and those who had more work experience (P<0.001) significantly differed in their mean total score on the PCQN scale. Factors such as level of education (P=0.007) and attending training regarding PC (P=0.000) were positively associated with the total score of PCQN.
There was a significant relationship between the overall score on the FATCOD scale and almost all characteristics except for gender.
Nurses with a higher level of education obtained significantly higher total scores on the EBPQ scale (P<0.001). Significant differences were also found regarding the nurses’ age (P=0.015) (Table 3).
The relationship between the level of nurses’ preparedness to provide PC and EBP
The total score of EBPQ was significantly correlated with the total score of the PCQN scale (P=0.013) and its subscale “management and control of pain and symptoms” (P=0.032), as well as to the total score of FATCOD scale (P<0.001) and its subscales: Attitude to patient (P<0.001), attitude to family (P<0.001). The “practice” subscale of the EBPQ questionnaire was significantly correlated only with the total FATCOD scale (P<0.001) and the subscale “attitude to the patient” (P=0.003). The “knowledge/skills” subscale of the EBPQ showed a significant correlation with all variables, specifically with the PCQN scale (P=0.001), its subscales (philosophy and principles (P=0.000), psychosocial aspects (P=0.036), management and control of pain and symptoms (P=0.005), and FATCOD scale (P<0.001) and subscales (attitude to patient [P<0.001], attitude to family [P<0.001]). However, there was no significant association between the “attitude” subscale of EBPQ and other variables (Table 4).

The impact of several parameters (gender, work experience, level of education, attending training regarding PC, EBPQ score, and its three subscales) on nurses’ competence level in PC was examined through a three-stage hierarchical multiple regression. Work experience was excluded from independent variables as age was highly correlated. Before regression analysis, the data were checked for multicollinearity and autocorrelation. Variance inflation factor (0.009-2.051) indicates the absence of multicollinearity. The Durbin-Watson value was 1.953, which suggests no autocorrelation.
Model 1 includes only demographic and professional factors (gender, work experience, level of education, attending training regarding PC) as predictors. The multiple correlation coefficient R-value is 0.557 (moderate correlation on the Chaddock scale). Thus, there was a positive correlation between the predictor variables and nurses’ competence level in PC. In model 1, only work experience (β=0.534; P<0.001) and attending training regarding PC (β=0.049; P<0.001) were statistically significant, although the effect of the latter was not very high. Given that R2 is 0.311, work experience and attending training regarding PC explain 31.1% of the variance of nurses’ competence level in the PC field.
Model 2 added the overall EBPQ score to demographic and professional predictors. This predictor has a statistically significant direct relationship with the level of knowledge about PC (β=0.136; P=0.001). The work experience remained statistically significant (β=0.534; P<0.001). The remaining predictors remained statistically insignificant. The R-value for model 2 is 0.569 (R2=0.323); therefore, the model explains 32.3% of the variance.
In model 3, the overall EBPQ score was replaced by its three subscales (knowledge/skills, practice, attitude). The values of R and R2 slightly increased to 0.573 and 0.328, respectively. Therefore, the model explains 32.8% of the variance. Among the three subscales, only the knowledge/skills scale demonstrated a statistically significant impact on nurses’ competence level in PC (β=0.122; P=0.005). The subscales of practice and attitude were not statistically significant (β=0.006 [P=0.900] and β=0.083 [P=0.097], respectively). As in the previous model, work experience is still statistically significant (β=0.529; P<0.001).
It could be seen that all three models were significant (P<0.001). It was noted that the F value was largest for the model 1 (63.063) (Table 5).
Discussion
The present study assessed the level of nurses’ knowledge about PC and attitude towards caring for dying patients and its relationship with EBP (knowledge/skills, attitude, and practice) among nurses of PHC organizations. To the best of our knowledge, this is the first study that examines these relationships among nurses of PHC organizations.
Our findings indicated that the nurses’ knowledge about PC was low or inadequate (total means score 9.06 out of 20). Similar findings have been reported by previous studies conducted in Ethiopia (Etafa et al., 2020), Iran (Dehghannezhad et al., 2021), and India (Gupta et al., 2023). However, compared with other published literature in which the PCQN was also used, the total PCQN score in our study was higher than that of Southeastern Iranian nurses (Iranmanesh et al., 2014), Indonesian (Hertanti et al., 2021), Palestinian (Toqan et al., 2023), and Mongolian (Gelegjamts et al., 2020) nurses, where the mean scores were 7.59±2.28, 7.78±3.56, 7.75±2.96, and 7.15±2.31, respectively. However, studies conducted in countries where PC is well developed have shown better results than in our study (12.89 and 12.3 points) (Mitchell et al., 2016; Raudonis et al., 2002). Similar to the results of this study, in many previous studies, the highest number of correct answers was related to the pain and symptom management subscale (Abuhammad et al., 2021; Dimoula et al., 2019). The reason for the higher level of knowledge about pain relief and other related symptoms may be that nurses, especially those working in PHC organizations, often care for patients with chronic diseases who require daily pain relief and symptom control.
Disciplines on PC have been introduced in Kazakhstan medical universities and colleges, and advanced training courses have been designed. Despite this, our study showed that 40% of nurses have never been trained in PC. This result is consistent with previous studies conducted in Palestine (Abu-Odah et al., 2022), Jordan (Abuhammad et al., 2021), and Egypt (Mohamed & Ibrahim, 2021).
The mean score of the FATCOD was 94.50 (i.e. neutral attitude), and the majority of nurses (59.3%) had a neutral attitude toward caring for dying patients. It is higher than the results found among nurses in Ethiopian public hospitals (Etafa et al., 2020) and Nigerian teaching hospitals (Faronbi et al., 2021) but lower than that of nurses in Australia (Tait et al., 2015), Vietnam (Nguyen & Nguyen, 2015), Japan (Matsui, 2022), and the USA (Clemens et al., 2021). Differences in the attitude of nurses may indicate differences in beliefs and cultural characteristics of the above regions that need to be investigated.
In our study, work experience and attending PC training were significantly associated with the nurses’ attitude toward caring for dying patients. Similar results have been obtained by a study in Sweden among registered nurses and undergraduate nursing students, which revealed the positive impact of long work experience and attendance at PC courses on the overall FATCODE mean score (Fristedt et al., 2021).
Furthermore, our study established that nurses’ age and level of education influenced their attitudes toward caring for dying patients. Thus, older nurses and those with a higher level of education showed a more positive attitude. These factors are strongly supported by similar studies in Jordan (Abu Hasheesh et al., 2013; Zahran et al., 2022) and Iran (Jafari et al., 2015).
The correlation between knowledge and attitude toward dying patients that we found in this study is confirmed by previous studies (Etafa et al., 2020; Dimoula et al., 2019; Kim et al., 2020). Although, some studies have not found such a relationship (Iranmanesh et al., 2014; Zhou et al., 2020). The mean score on EBPQ was 4.39 out of 7 points in the present study. This score is slightly higher than the result obtained from registered nurses in traditional Chinese medicine hospitals (Zhou et al., 2016) but lower than that of surveys conducted in Spain and Latin America, Oman, Egypt, and Jordan, where the mean scores ranged between 4.96 and 5.5 (Al-Busaidi et al., 2019; Pеrez-Campos et al., 2014; Youssef et al., 2018).
In our study, as in most other similar studies, EBPQ subscale scores were highest for “attitude” followed by “knowledge/skills” and “practice” (Maydick-Youngberg et al., 2021). According to the results of our research, most nurses scored low on the “practice subscale”. This finding is consistent with another study conducted among nurses in Nepal, where nurses’ scores on the three subscales were arranged in the same sequence (Karki et al., 2015). Also, in their study, Karki and colleagues mentioned a lack of time and resources, difficulty understanding research articles and translating the findings to practice, and limited autonomy to modify their practice according to EBP as the greatest barriers (Karki et al., 2015).
The results regarding the factors affecting EBP were contradictory. We have found a statistically significant influence of age and level of education, but some studies refute this (Al-Busaidi et al., 2019; Zhou et al., 2016).
Conclusion
Our findings were indicative of insufficient knowledge about PC and a neutral or negative attitude towards caring for dying patients among nurses working in PHC organizations in Astana. Demographic and professional factors such as age, work experience, level of education, and attending PC training affected the nurses’ knowledge about PC and attitude towards caring for dying patients.
The lack of knowledge and skills of nurses in the field of EBP may contribute to insufficient knowledge about PC, possibly due to the lack of knowledge necessary to formulate a clinical question, search, and selection of scientific publications. It may be necessary to strengthen the theoretical part of the nursing curriculum in the “evidence-based practice” section and to add continuing PC education to the nursing curriculum to improve the quality of end-of-life care. Implementing initiatives and strategies to promote EBP among nurses in various medical institutions could use the results of this study as a foundation. Future studies may be required to investigate this issue because this study did not specifically address barriers to EBP in PC.
There were some limitations in our study. Two of the three questionnaires used in our research are self-report questionnaires (PCQN was a true-false scale, but FATCOD and EBPQ were self-reported questionnaires), which can lead to potential bias and overestimation of some results. This study was conducted only in the city of Astana, which reduces the generalization of the results obtained. Finally, cross-sectional research allows us to determine associations, but not causal relationships, when analyzing potential predictors of nurses’ knowledge and attitude and their relationship with their EBP.
Ethical Considerations
Compliance with ethical guidelines
Before starting the study, we received formal permission from the Local Bioethical Committee of NpJSC Astana Medical University (Protocol No.: 15 of October 21, 2021). This study was conducted in accordance with ethical principles (Helsinki Declaration, developed in 1964). The survey was anonymous, and its purpose and implications for the research results were explained before it began. Each participant was asked to sign an informed consent form.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Investigation, data gathering, and data analysis: Masharipova Alexandra and Nurgaliyeva Nassikhat; Supervision: Derbissalina Gulmira; Conceptualization, study design, writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to the heads of Primary Health Care Organizations in Astana for their support and access to nurses. The authors are also grateful to all the nurses who participated in the study.
References
Hasheesh, M. O. A., et al., 2013. Nurses’ characteristics and their attitudes toward death and caring for dying patients in a public hospital in Jordan. Health Science Journal, 7(4), pp. 384-94. [Link]
Abuhammad, S., et al., 2021. Knowledge of pediatric palliative care among medical students in Jordan: A cross-sectional study. Annals of Medicine and Surgery (2012), 64, pp. 102246. [DOI:10.1016/j.amsu.2021.102246] [PMID]
Abu-Odah, H., Molassiotis, A. & Liu, J. Y. W., 2022. Assessment of the educational and health care system-related issues from physicians’ and nurses’ perspectives before developing a palliative care program within the palestinian health care system: A cross-sectional study. Journal of Hospice and Palliative Nursing, 24(3), pp. E59–75. [DOI:10.1097/NJH.0000000000000840] [PMID]
Achora, S. & Labrague, L. J., 2019. An integrative review on knowledge and attitudes of nurses toward palliative care: Implications for practice. Journal of Hospice and Palliative Nursing, 21(1), pp. 29-37. [DOI:10.1097/NJH.0000000000000481] [PMID]
Ali, W. G. M. & Ayoub, N. S., 2010. Nurses’ attitudes towards caring for dying patient in Mansoura University hospitals. Journal of Medicine and Biomedical Sciences, 1(1), pp. 16-23. [Link]
Al-Busaidi, I. S., et al., 2019. Nurses’ knowledge, attitudes, and implementation of evidence-based practice in Oman: A multi-institutional, cross-sectional study. Oman Medical Journal, 34(6), pp. 521–7. [DOI:10.5001/omj.2019.95] [PMID]
Clemens, E. J., et al., 2021. Effect of death and dying elective on student empathy and attitudes toward mortality. Currents in Pharmacy Teaching & Learning, 13(12), pp. 1627–33. [DOI:10.1016/j.cptl.2021.09.029] [PMID]
Cross L. A., 2019. Compassion fatigue in palliative care nursing: A concept analysis. Journal of Hospice and Palliative Nursing, 21(1), pp. 21-8. [DOI:10.1097/NJH.0000000000000477] [PMID]
Dehghannezhad, J., et al., 2021. Home care nurses’ attitude towards and knowledge of home palliative care in Iran: A cross-sectional study. Iranian Journal of Nursing and Midwifery Research, 26(3), pp. 272–8. [DOI:10.4103/ijnmr.IJNMR_249_19] [PMID]
Dimoula, M., et al., 2019. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurse Education Today, 74, pp. 7–14. [DOI:10.1016/j.nedt.2018.11.025] [PMID]
Etafa, W., et al., 2020. Nurses’ knowledge about palliative care and attitude towards end- of-life care in public hospitals in Wollega zones: A multicenter cross-sectional study. Plos One, 15(10), pp. e0238357. [DOI:10.1371/journal.pone.0238357] [PMID]
Faronbi, J. O., et al., 2021. Nurses’ attitude toward caring for dying patients in a Nigerian Teaching Hospital. SAGE Open Nursing, 7, pp. 23779608211005213. [DOI:10.1177/23779608211005213] [PMID]
Fristedt, S., et al., 2021. Registered nurses and undergraduate nursing students’ attitudes to performing end-of-life care. Nurse Education Today, 98, pp. 104772. [DOI:10.1016/j.nedt.2021.104772] [PMID]
Frommelt, K. H., 1991. The effects of death education on nurses’ attitudes toward caring for terminally ill persons and their families. The American Journal of Hospice & Palliative Care, 8(5), pp. 37–43. [DOI:10.1177/104990919100800509] [PMID]
Gelegjamts, D., et al., 2020. Undergraduate nursing students’ palliative care knowledge and attitudes towards end-of-life care: A cross-sectional descriptive study. Contemporary Nurse, 56(5-6), pp. 477–90. [DOI:10.1080/10376178.2021.1890165] [PMID]
Grubb, C. & Arthur, A., 2016. Student nurses’ experience of and attitudes towards care of the dying: A cross-sectional study. Palliative Medicine, 30(1), pp. 83–8. [DOI:10.1177/0269216315616762] [PMID]
Gupta, M., et al., 2023. Impact of end-of-life nursing education consortium on palliative care knowledge and attitudes towards care of dying of nurses in India: A Quasi-Experimental Pre-Post Study. The American Journal of Hospice & Palliative Care, 40(5), pp. 529–38. [DOI:10.1177/10499091221108342] [PMID]
Hertanti, N. S., et al., 2021. Palliative Care Quiz for Nurses-Indonesian Version (PCQN-I): A cross-cultural adaptation, validity, and reliability study. Indian Journal of Palliative Care, 27(1), pp. 35–42. [DOI:10.4103/IJPC.IJPC_76_20] [PMID]
Iranmanesh, S., et al., 2014. Nurses’ knowledge about palliative care in Southeast Iran. Palliative & Supportive Care, 12(3), pp. 203–10. [DOI:10.1017/S1478951512001058] [PMID]
Jafari, M., et al., 2015. Caring for dying patients: attitude of nursing students and effects of education. Indian Journal of Palliative Care, 21(2), pp. 192–7. [DOI:10.4103/0973-1075.156497] [PMID]
Karki, S., et al., 2015. Perceptions and attitudes towards evidence based practice among nurses and nursing students in Nepal. Kathmandu University Medical Journal (KUMJ), 13(52), pp. 308–15. [DOI:10.3126/kumj.v13i4.16829] [PMID]
Kim, S., Lee, K. & Kim, S., 2020. Knowledge, attitude, confidence, and educational needs of palliative care in nurses caring for non-cancer patients: A cross-sectional, descriptive study. BMC Palliative Care, 19(1), pp. 105. [DOI:10.1186/s12904-020-00581-6] [PMID]
Kunirova, G. & Shakenova, A., 2018. Palliative care in Kazakhstan. Journal of Pain and Symptom Management, 55(2S), pp. S36–40. [DOI:10.1016/j.jpainsymman.2017.03.028] [PMID]
Masharipova, A., Nurgaliyeva, N. & Derbissalina, G., 2022. The problem of preparedness of nursing staff to provide palliative nursing care (a literature review). Georgian Medical News, (325), pp. 27–32. [PMID]
Mathieson, A., Grande, G. & Luker, K., 2019. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: A systematic mixed-studies review and qualitative synthesis. Primary Health Care Research & Development, 20, pp. e6. [DOI:10.1017/S1463423618000488] [PMID]
Matsui, M., 2022. Nurses’ symptom management and views on death and caring for heart failure and chronic obstructive pulmonary disease. International Journal of Palliative Nursing, 28(5), pp. 214–21.[DOI:10.12968/ijpn.2022.28.5.214] [PMID]
Maydick-Youngberg D, Gabbe L, Simmons G, et al. (2021). Assessing evidence-based practice knowledge: An innovative approach by a nursing research council. Journal of Nursing Administration, 51(5):279-286. [DOI:10.1097/NNA.0000000000001013] [PMID]
Mills, J., Wand, T. & Fraser, J. A., 2018. Exploring the meaning and practice of self-care among palliative care nurses and doctors: A qualitative study. BMC Palliative Care, 17(1), pp. 63. [DOI:10.1186/s12904-018-0318-0] [PMID]
Mitchell, G., et al., 2016. Care home managers’ knowledge of palliative care: A Northern Irish study. International Journal of Palliative Nursing, 22(5), pp. 230–5. [DOI:10.12968/ijpn.2016.22.5.230] [PMID]
Mohamed R. F. & Ibrahim, R. A., 2021. Effect of palliative care guideline on nurses’ knowledge, attitude, and practice at intensive care unit. Egyptian Journal of Nursing and Health Sciences, 2(2), pp. 81-109. [DOI:10.21608/ejnhs.2021.196022]
Nguyen, L.T. & Nguyen, H. T., 2015. Attitudes towards caring for terminally-ill patients among in-serviced nursing students at Hanoi Medical University, Vietnam. Vietnam Journal of Medicine and Pharmacy, 7(1), pp. 55-63. [Link]
Ministry of Justice of the Republic of Kazakhstan. State program for the development of healthcare of the Republic of Kazakhstan for 2020 – 2025 [Internet]. Viewed 13 March 2023, [Link]
Lakasing, E., 2013. Palliative care in primary care [Inretnet]. Viewed 23 Apr 2023, [Link]
Pérez-Campos, M. A., et al., 2014. Knowledge, attitude and use of evidence-based practice among nurses active on the internet. Investigacion Y Educacion en Enfermeria, 32(3), pp. 451–60. [DOI:10.17533/udea.iee.v32n3a10] [PMID]
Raudonis, B. M., Kyba, F. C. & Kinsey, T. A., 2002. Long-term care nurses’ knowledge of end-of-life care. Geriatric Nursing (New York, N.Y.), 23(6), pp. 296–301. [DOI:10.1067/mgn.2002.130270] [PMID]
Ross MM, McDonald B, McGuinness J. (1996). The palliative care quiz for nursing (PCQN): the development of an instrument to measure nurses’ knowledge of palliative care. J Adv Nurs. 23(1):126-137. [DOI:10.1111/j.1365-2648.1996.tb03106.x] [PMID]
Rosa, W. E., 2018. Integrating palliative care into global health initiatives: opportunities and challenges. Journal of Hospice and Palliative Nursing, 20(2), pp. 195–200. [DOI:10.1097/NJH.0000000000000415] [PMID]
Schroeder, K. & Lorenz, K., 2018. Nursing and the future of palliative care. Asia-Pacific Journal of Oncology Nursing, 5(1), pp. 4–8. [DOI:10.4103/apjon.apjon_43_17] [PMID]
Sekse, R. J. T., Hunskår, I. & Ellingsen, S., 2018. The nurse’s role in palliative care: A qualitative meta-synthesis. Journal of Clinical Nursing, 27(1-2), pp. e21–e38. [DOI:10.1111/jocn.13912] [PMID]
Tait, V., et al., 2015. Attitudes of nonpalliative care nurses towards palliative care. International Journal of Palliative Care, 2015, pp. 1-6. [DOI:10.1155/2015/469174]
Toqan, D., et al., 2023. Perception of nurses’ knowledge about palliative care in West Bank/ Palestine: Levels and influencing factors. Journal of Palliative Care, 38(3), pp. 336–44.[DOI:10.1177/08258597221133958] [PMID]
Upton D, Upton P., (2006). Development of an evidence-based practice questionnaire for nurses. Journal of Advanced Nursing., 53(4):454-8. [DOI: 10.1111/j.1365-2648.2006.03739.x] [PMID]
Wang, L. P., et al., 2016. Development and Psychometric Testing Chinese Version of the Frommelt Attitude Toward Care of the Dying Scale, Form B in nurses and nursing students. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education, 31(1), pp. 123–30. [DOI:10.1007/s13187-015-0810-7] [PMID]
World Health Organization (WHO), 2020. Palliative care. Geneva: WHO. [Link]
World Health Organization. Integrating palliative care and sumptom relief into primary health care. Geneva: World Health Organization; 2018. [Link]
Youssef, N. F. A., et al., 2018. Egyptian and Jordanian nurse educators’ perception of barriers preventing the implementation of evidence-based practice: A cross-sectional study. Nurse Education Today, 64, pp. 33–41. [DOI:10.1016/j.nedt.2018.01.035] [PMID]
Zhou, F., et al., 2016. Attitude, knowledge, and practice on evidence-based nursing among registered nurses in traditional Chinese medicine hospitals: A multiple center cross-sectional survey in China. Evidence-Based Complementary and Alternative Medicine: eCAM, 2016, pp. 5478086. [DOI:10.1155/2016/5478086] [PMID]
Zahran, Z., et al., 2022. Nursing students’ attitudes towards death and caring for dying patients. Nursing Open, 9(1), pp. 614–23. [DOI:10.1002/nop2.1107] [PMID]
Zhou, Y., Li, Q. & Zhang, W., 2020. Undergraduate nursing students’ knowledge, attitudes and self-efficacy regarding palliative care in China: A descriptive correlational study. Nursing Open, 8(1), pp. 343–53. [DOI:10.1002/nop2.635] [PMID]
Type of Study: Research |
Subject:
General
Received: 2023/08/17 | Accepted: 2023/12/13 | Published: 2024/05/1
Received: 2023/08/17 | Accepted: 2023/12/13 | Published: 2024/05/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






