Sat, Jan 31, 2026
[Archive]
Volume 10, Issue 3 (Summer 2024)
JCCNC 2024, 10(3): 223-230 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Carvello M, Lupo R, Rum G, Vitale E, Conte L, Cremonini V et al . Mind the Gap Between Theory and Practice: Nursing Students and Tutors in Comparison. JCCNC 2024; 10 (3) :223-230
URL: http://jccnc.iums.ac.ir/article-1-566-en.html
URL: http://jccnc.iums.ac.ir/article-1-566-en.html
Maicol Carvello1 

 , Roberto Lupo2
, Roberto Lupo2 
 , Giulia Rum3
, Giulia Rum3 
 , Elsa Vitale4
, Elsa Vitale4 
 , Luana Conte *5
, Luana Conte *5 

 , Valeria Cremonini6
, Valeria Cremonini6 

 , Ivan Rubbi6
, Ivan Rubbi6 



 , Roberto Lupo2
, Roberto Lupo2 
 , Giulia Rum3
, Giulia Rum3 
 , Elsa Vitale4
, Elsa Vitale4 
 , Luana Conte *5
, Luana Conte *5 

 , Valeria Cremonini6
, Valeria Cremonini6 

 , Ivan Rubbi6
, Ivan Rubbi6 

1- Community Hospital, Local Health Authority (ASL) of Romagna, Ravenna, Italy.
2- San Giuseppe da Copertino Hospital, Local Health Authority (ASL) of Lecce, Copertino, Italy.
3- Villa Adalgisa Hospice, Ravenna, Italy.
4- Local Health Authority (ASL) of Bari, Bari, Italy.
5- Laboratory of Biomedical Physics and Environment, Department of Mathematics and Physics ,luana.conte@unisalento.it
6- Department of Medical and Surgical Sciences, School of Nursing, University of Bologna, Bologna, Italy.
2- San Giuseppe da Copertino Hospital, Local Health Authority (ASL) of Lecce, Copertino, Italy.
3- Villa Adalgisa Hospice, Ravenna, Italy.
4- Local Health Authority (ASL) of Bari, Bari, Italy.
5- Laboratory of Biomedical Physics and Environment, Department of Mathematics and Physics ,
6- Department of Medical and Surgical Sciences, School of Nursing, University of Bologna, Bologna, Italy.
Full-Text [PDF 529 kb]
(1898 Downloads)
| Abstract (HTML) (4046 Views)
Full-Text: (692 Views)
Introduction
An internship provides a privileged context for nursing students to obtain professional competencies and an opportunity to translate knowledge into practice that contributes to transforming theoretical understanding into intellectual, psychomotor and social skills (Ahmari Tehran et al., 2021). The concept of mentoring has existed for many years. Still, in recent decades, it has gained significance in healthcare education and professional training, increasingly understood as a bilateral relationship between the intern and the educator, where both parties have the opportunity to grow and develop (Burgess et al., 2018; La Sala et al., 2021).
Integrating theoretical content with practical application through internships often presents significant challenges, primarily from behavioral, attitudinal, environmental and organizational factors (Ngozika Ugwu et al., 2023). This issue underscores the importance of mentorship, which should be seen as a competent process of transmitting procedural, experiential and social know-how (La Sala et al., 2021).
The gap between education and clinical practice understood as the disparity between idealized practice and common practice or the difference between general principles taught and their application in specific situations, has always been a challenge for education experts (Shoghi et al., 2019). Several international studies conducted in the United States, the United Kingdom, Australia and Canada suggest that one possible reason behind this phenomenon is the lack of a structured and defined connection between clinical contexts and nursing education, as well as between instructors and nurses (Vosoughi et al., 2022).
This gap can negatively impact patient safety, influencing the quality of care, care outcomes and students’ educational experiences, leading to dissatisfaction (Saifan et al., 2021). Newly graduated nurses are at risk of experiencing the so-called “transition shock,” which leads them to conclude that a portion of their education has been futile and that following traditional routines is the best choice (Safazadeh et al., 2018).
The relationship between knowledge and practice is vital to support clinical decision-making and the development of the nursing profession. One key aspect of nursing education is how to motivate students to learn effectively and desirably apply their knowledge in clinical practice (Shoghi et al., 2019).
Some student experiences indicate that using valid and updated knowledge acquired by learners from their peers in educational settings is sometimes met with resistance from clinical hospital staff. This condition seems to be due to various reasons, such as lack of time (Hashemiparast et al., 2019), heavy workloads, a routine and monotonous approach to care and a stressful clinical learning environment (Salifu et al., 2019).
The process of constructing professional identity occurs in relation to a reference group of other professionals, and this process takes place throughout one’s personal experience, starting from education and internships (Arreciado Marañón & Isla Pera, 2015). So, nursing mentors must create a knowledge channel that facilitates the sharing, transfer, and implementation of evidence-based guidelines.
To date, no study in the Italian context has compared the perceptions of nursing students and clinical mentors regarding the theory-practice gap phenomenon. Through an observational investigation, this study examines whether and how nursing students attending the bachelor of science (BS) in Nursing program and clinical internship tutors perceive a gap between the theory taught during lectures and the practical care provided during internships. The study also evaluates any factors that are opposing knowledge translation.
Materials and Methods
Study design, setting and sample
This research is an observational, cross-sectional study. The investigation includes the nursing BS programs at two Italian Universities (the University of Bari and the Polytechnic University of the Marche located in Ancona, Italy). Requests for participation in the study were sent to the responsible for didactic activities of the nursing BS degree programs. A questionnaire was prepared using Google Forms and distributed to participants through the program secretariats in a digital format. Responses were collected between June 1 and July 31, 2022. Participation in the study was voluntary, and the eligible samples were recruited using convenience sampling. They included all students enrolled in the third year of the nursing BS degree program or those who had completed it (n=107) and nurses currently serving as internship mentors (n=48).
Measurement and data collection
The research instrument is a customized questionnaire. The questions were designed to explore conceptual areas (pedagogical deficits, relational deficits) previously investigated in other semi-structured interviews from existing literature and adapted to the Italian context (Factor et al., 2017; Hashemiparast et al., 2019). The questionnaire consisted of two sections, one for students and one for internship tutors, each containing 7 items customized differently for the two participant groups. Participants are asked to respond by selecting the option that best reflects their perception and expressing their degree of agreement on a 4-point Likert scale, ranging from totally disagree=1 to totally agree=4.
For students, the questions were supposed to assess the perceived theory-practice gap, whether the student can identify the observed discrepancy, how they feel about it, whether they need to adapt to the context despite being aware of acting differently from theory and whether there has been interest and willingness to engage in discussions with the tutor. Complementary questions were posed to tutors, examining whether students were free in their perception to report the theory-practice gap and whether they provided satisfactory explanations in the presence of a discrepancy. The questionnaire also investigates the potential initiation of communication problems and the perceived necessity for students to adapt their behaviors to their context.
The questionnaire is further integrated with sociodemographic questions, including gender and age for students and tutors. Additionally, tutors were asked about their educational qualifications, years of work experience, and current working environment. The questionnaire demonstrated good internal consistency (α=0.752). The tool was evaluated by experts from the faculty and educational tutors of the Nursing degree course. After suggesting some modifications, the experts approved the tool.
Data analysis
The analysis was carried out using Jamovi software, version 2.3.18 and Microsoft Office Excel software. Descriptive statistics calculations were performed with a 95% confidence interval (CI). P were determined using the chi-square test for nominal and the t-test for ordinal variables. Correlations were calculated using the Spearman coefficient, and internal consistency was determined with the Cronbach α.
Results
The overall sample consisted of 107 students (69.0%) (group 1), including 83 women (77.5%) and 24 men (22.5%), with an mean age of 24.4±4.60 years, 48 (31.0%) clinical tutors (Group 2), including 34 women (77.0%) and 11 men (23.0%) with an mean age of 48.4±7.14 years. Regarding clinical tutors’ qualifications, 33.3% (n=16) held a regional diploma, 14,6% (n=7) had a BS, 22.9% (n=11) held a BS with post-basic training, 10.4% (n=5) held a master of science (MS), and 18.8% (n=9) had a MS with post-basic training. The working areas of clinical tutors were as follows: 20.8% (n=10) in surgical wards, 24.9% (n=12) in medical-specialized wards, 14.6% (n=7) in community hospitals, 12.5% (n=6) in critical care, 10.4% (n=5) in operating rooms, 8.3% (n=4) in medical wards, 6.3% (n=3) in outpatient clinics and 2.1% (n=1) in radiology and intensive care unit. Years of experience were classified, with 43.8% (n=21) having 16 to 25 years of experience and the same percentage having over 25 years of experience. Additionally, 12.5% (n=6) had work experience ranging from 1 to 15 years.
Significant differences were observed between the two groups for all items in the instrument (P<0.0001) (Table 1).
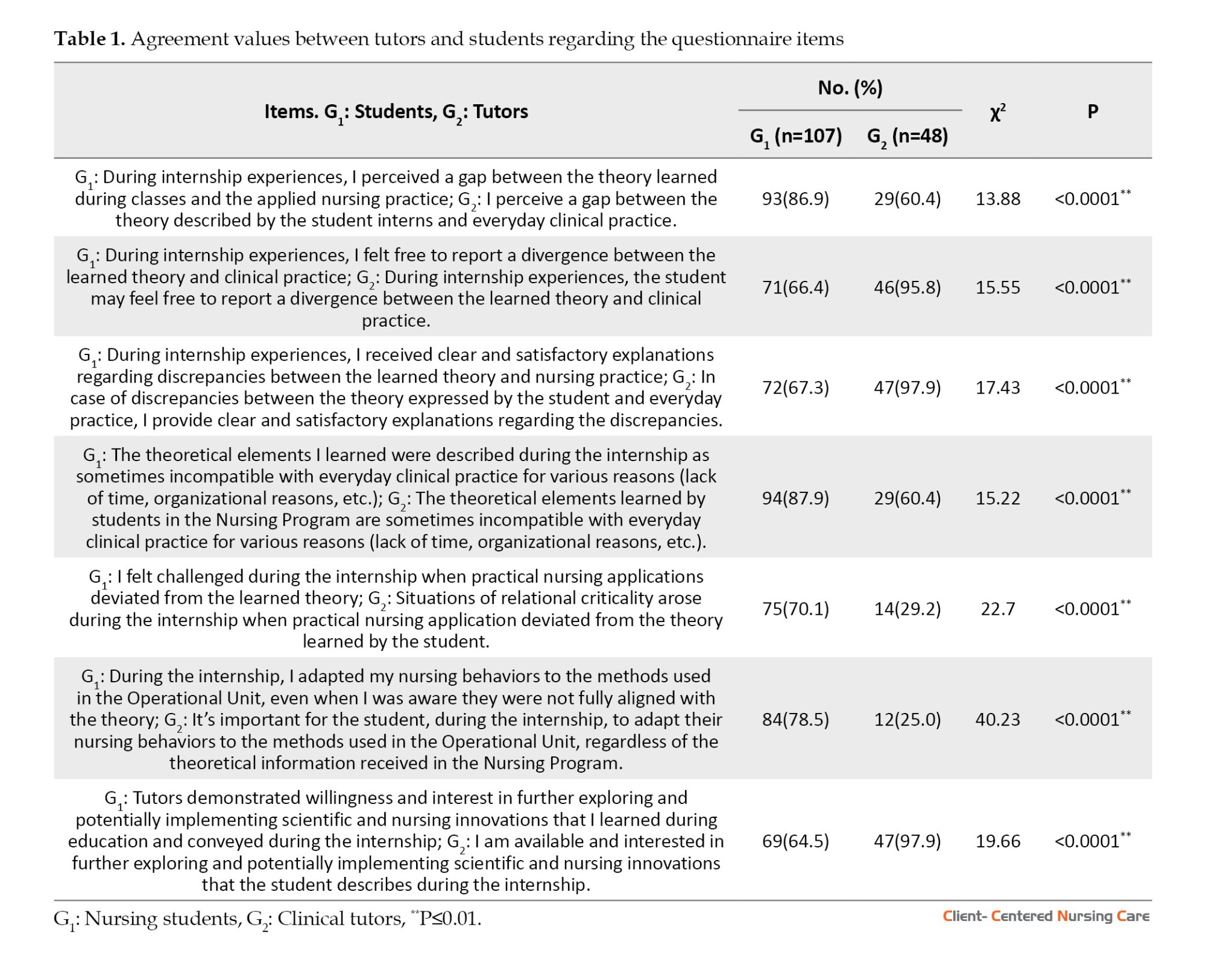
Parametric calculation using the t-test with the summation of Likert scores from all items in both groups confirmed a substantial difference between group 1 (Mean±SD=16.3±2.90; median=16.0) and group 2 (Mean±SD=20.7±2.37; median=20.5) (P<0.001).
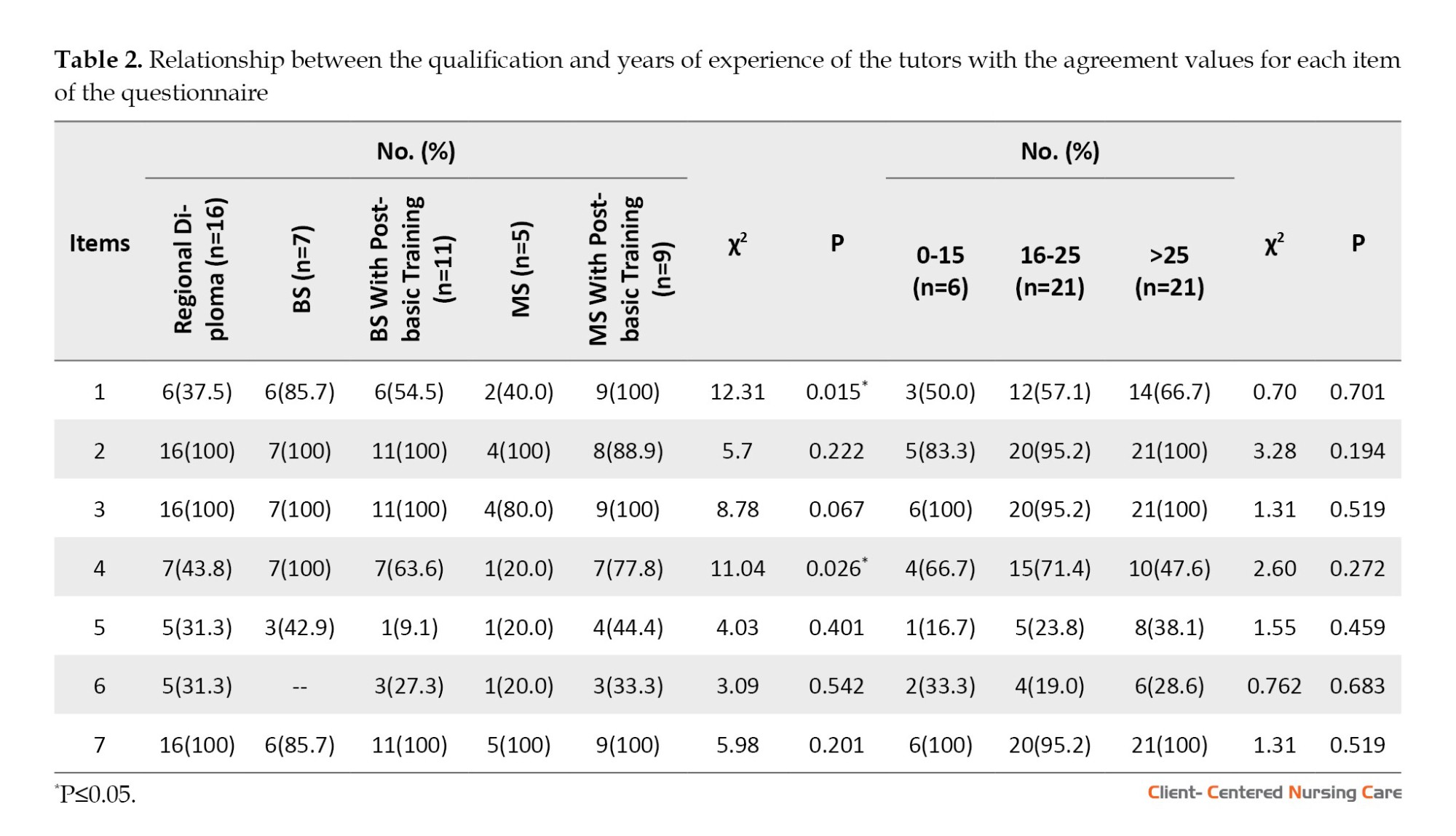
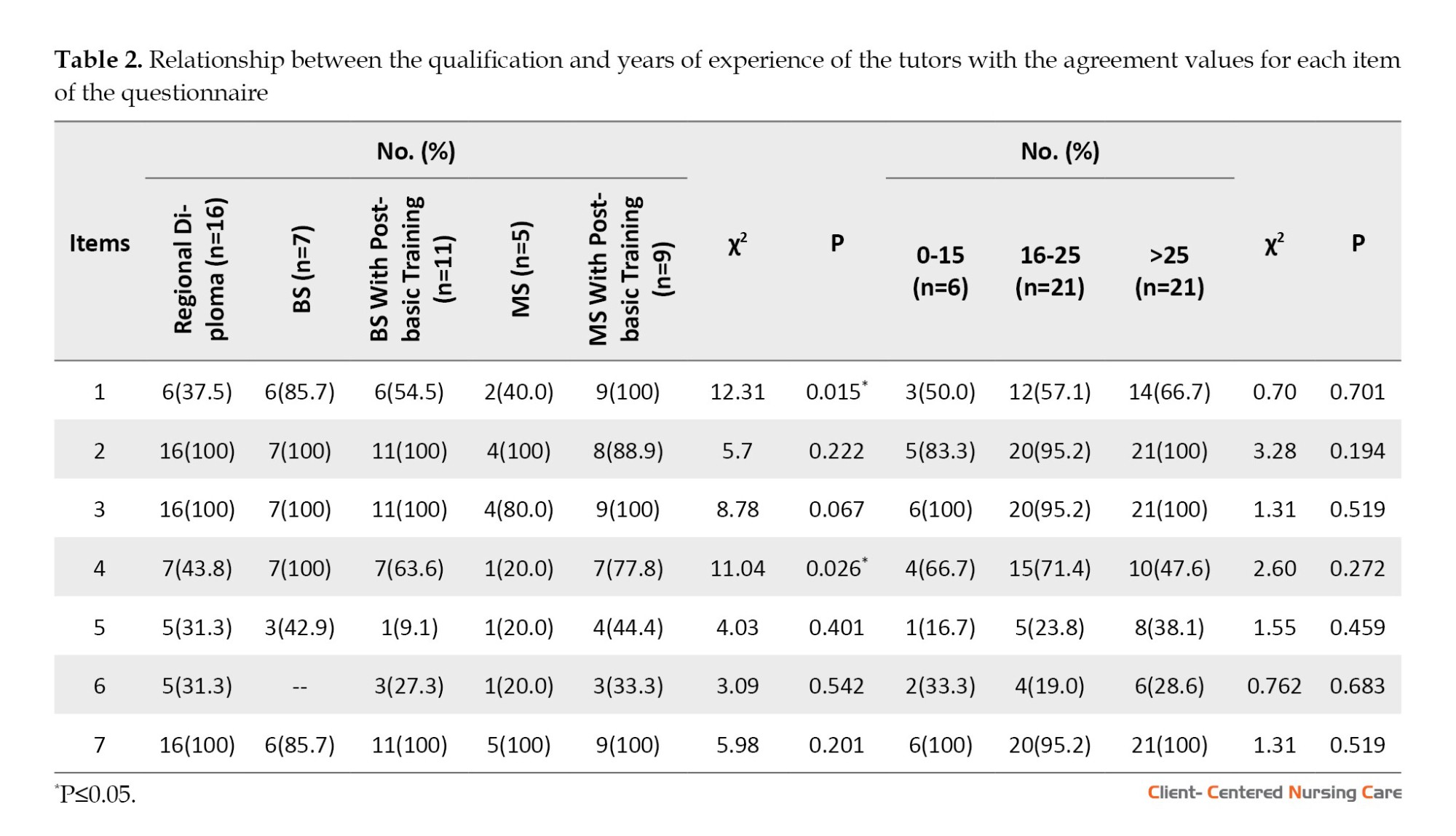
In the group of tutors, when relating the independent variables (graduation, years of experience) to the dependent variables, it is evident that questions 1 and 4 appear to be significantly influenced by the professionals’ training and their experience with nursing students placed in their organizations (P=0.015 and P=0.026, respectively). The years of service did not significantly affect the answer to question number 7 in the group of tutors (Table 2). No relationship was found between the tutors’ agreement with the theory-practice gap and their experience in clinical training.
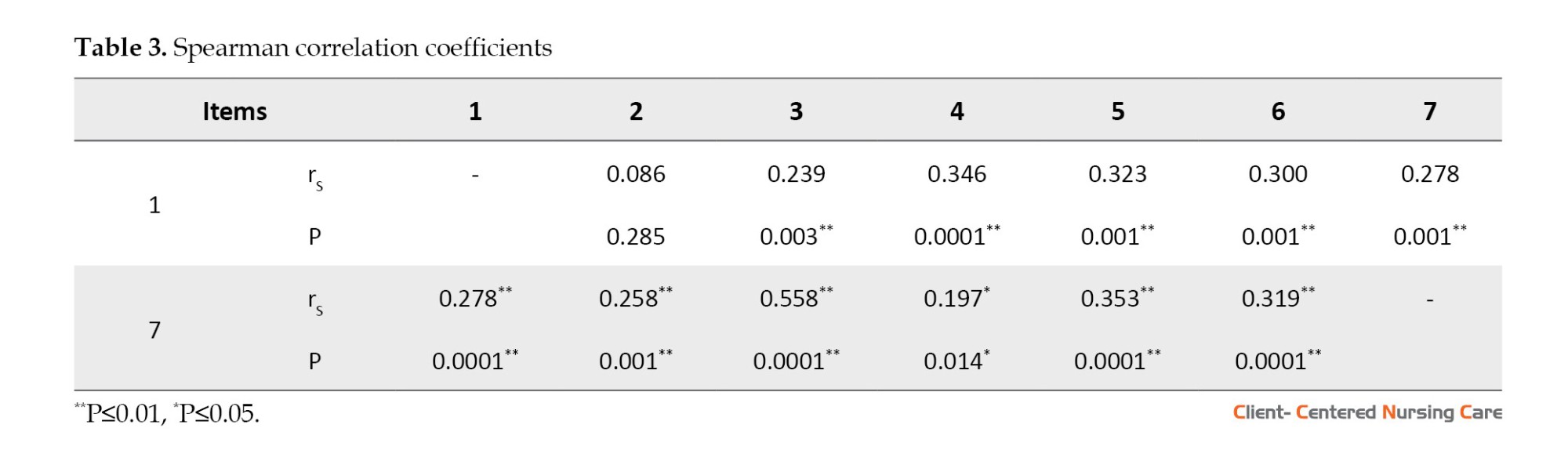
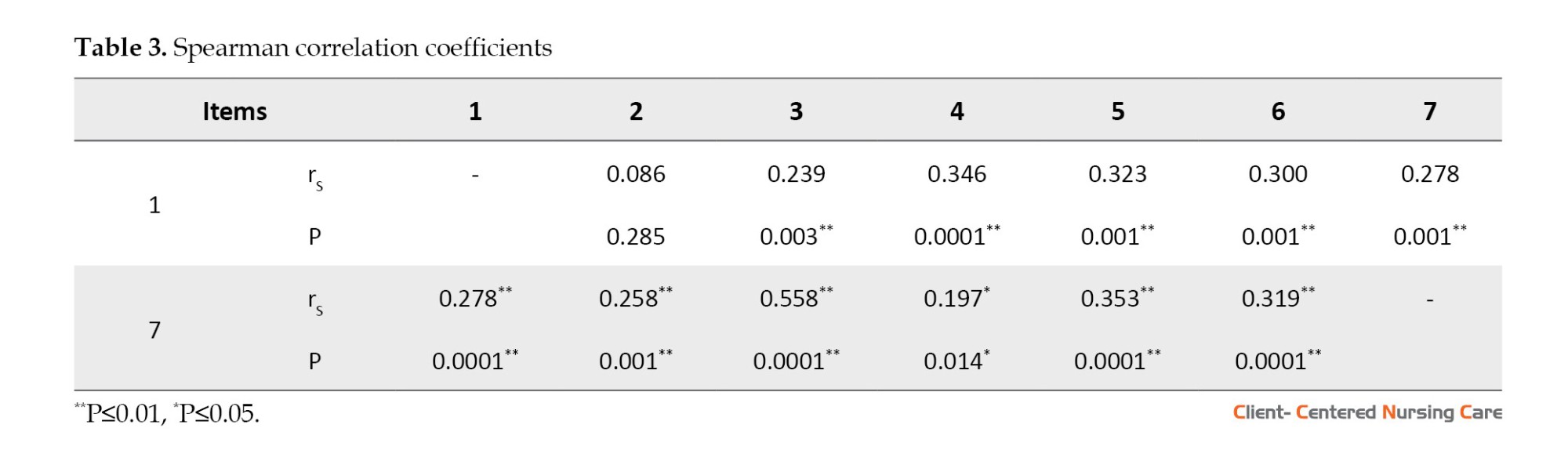
In the Spearman correlation matrix (Table 3), item 1 positively correlates with questions 3, 4, 5, 6 and 7. Item 7, which pertains to the tutor’s willingness to explore and implement new scientific and clinical developments in internship practice, correlates with all the questions in the questionnaire.
Discussion
Evidence suggests that students in clinical learning settings often struggle to match the theoretical content learned in the classroom with what they perform in practice (Hashemiparast et al., 2019). Meanwhile, the study by Factor et al., (2017) indicates that when students encounter clinical situations, they find it challenging to generalize and apply the nursing knowledge and theories they have learned. This condition arises because they discover discrepancies between what was learned in the classroom and how skills are carried out in the real-world context. We found that most third-year nursing students perceive a substantial gap between the theoretical education received and the clinical practice observed during internship periods. This perception was consistently confirmed irrespective of the age and gender of the participants. Even more cautiously, the same perception is significantly observed in the responses of internship tutors, regardless of their working experience. Evidence-based practice is crucial for university-level nursing education and graduates, serving as a way for the nursing discipline to minimize the gap between theory and practice (Mackey & Bassendowski, 2017).
This result is confirmed when over 70% of students express difficulty, perhaps also operational, aligning the concepts learned during theoretical education or laboratory practice with their experiences during clinical internships. This outcome is likely attributable to a generational gap concerning the innovative aspects brought by students. As years of experience increase, there tends to be a propensity for a more conservative approach rather than questioning what has already been learned. This tendency might also relate to the introduction of new scientific innovations. Another factor reinforcing the gap between theory and practice is apparent when analyzing the responses to item 4, which investigated potential incompatibilities between theory and everyday clinical practice. This issue may relate to the organizational situation of each operational unit. Factors such as staffing levels, work organization, time constraints, resource shortages, and the nurse-patient ratio appear to impact the ability to teach students. This finding is in line with the study by Hashemiparast et al. (2019), which discusses the system’s resistance to applying theoretical knowledge. The data suggest that clinical staff, due to various reasons like lack of time or resources, prevent students from applying theoretical knowledge taught in class.
The gap, clearly acknowledged by both parties, would still be bridged for two-thirds of the students through clear and satisfactory explanations provided by tutors upon students’ requests. Nonetheless, around 33% of students disagreed with this statement (item 3), suggesting an unresolved discomfort. This negative sentiment is more pronounced among male students, possibly stemming from inherent difficulties in interacting with tutors, who are predominantly female nursing professionals. Notably, 98% of tutors fully agree with the statement, hinting at a potentially defensive response. A similar pattern is observed in item 2, where over 90% of tutors express agreement, while only one in three students disagrees with the ability to freely express discordance between theory and practice. This partial but noteworthy communication challenge with tutors seems to manifest in students’ adaptive behavior to the practices of the clinical unit during their internships. Despite being aware of deviating from learned protocols, procedures, and guidelines, students adapt to the unit’s methods. This finding aligns with the study by Factor et al., (2017), which attributes this behavior to a structural deficit stemming from resource shortages and a lack of procedures and protocols, forcing students into improvisation and practice modification. However, this attitude is not shared by tutors, who believe in the importance of aligning theory and practice. Yet, in daily activities, as demonstrated by item 4, they struggle to integrate theory into everyday clinical practice. This partial but noteworthy communication challenge with tutors seems to manifest in students’ adaptive behavior to the practices of the clinical unit during their internships. Despite being aware of deviating from learned protocols, procedures and guidelines, students adapt to the unit’s methods. This sentiment is shared by nearly all tutors and 64.5% of students. The results of a study by Kaphagawani and Useh (2018) also confirmed this tendency, stating that tutors are not only eager to teach but are always available for students despite their growing workload.
The conducted study presents some limitations. Firstly, the number of participants in the survey, mainly clinical tutors, is limited. The second limitation is the lack of psychometrics of the instrument used. However, the instrument’s internal consistency has been confirmed and validated by experienced individuals. The cross-sectional nature of the study does not allow for causal conclusions. Despite these limitations, the study provides valuable insight into the current relevance of this topic within the clinical university environment, highlighting the need for active efforts from both sides to address the issue.
Conclusion
This study explored some possible motivations underlying the dichotomy between theory and practice in the clinical university context from the perspective of students and internship tutors. Addressing the issue of the theory-practice gap, particularly during the tutoring period, could represent one of the possible solutions to bridge the gap. The structured discussion moments during the mentoring period might prove beneficial. For instance, scheduling meetings among tutors, students, and course coordinators, especially in the early stages of the internship, could facilitate students’ inclination to express themselves. In any case, these critical moments could serve as a helpful tool for students to reflect on their knowledge and develop critical thinking. This investigation has provided further insights into the subject’s literature while raising additional questions. It would be advisable to maintain a high level of attention to the topic by conducting further studies that explore, through different inquiries, additional variables underlying the phenomenon.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of University of Bologna (Code: 0121436/2022). Participation was anonymous and obtained through informed consent by completing the questionnaire.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to this manuscript.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Participants in the study and the collaborating universities are appreciated for contributing to the research.
References
An internship provides a privileged context for nursing students to obtain professional competencies and an opportunity to translate knowledge into practice that contributes to transforming theoretical understanding into intellectual, psychomotor and social skills (Ahmari Tehran et al., 2021). The concept of mentoring has existed for many years. Still, in recent decades, it has gained significance in healthcare education and professional training, increasingly understood as a bilateral relationship between the intern and the educator, where both parties have the opportunity to grow and develop (Burgess et al., 2018; La Sala et al., 2021).
Integrating theoretical content with practical application through internships often presents significant challenges, primarily from behavioral, attitudinal, environmental and organizational factors (Ngozika Ugwu et al., 2023). This issue underscores the importance of mentorship, which should be seen as a competent process of transmitting procedural, experiential and social know-how (La Sala et al., 2021).
The gap between education and clinical practice understood as the disparity between idealized practice and common practice or the difference between general principles taught and their application in specific situations, has always been a challenge for education experts (Shoghi et al., 2019). Several international studies conducted in the United States, the United Kingdom, Australia and Canada suggest that one possible reason behind this phenomenon is the lack of a structured and defined connection between clinical contexts and nursing education, as well as between instructors and nurses (Vosoughi et al., 2022).
This gap can negatively impact patient safety, influencing the quality of care, care outcomes and students’ educational experiences, leading to dissatisfaction (Saifan et al., 2021). Newly graduated nurses are at risk of experiencing the so-called “transition shock,” which leads them to conclude that a portion of their education has been futile and that following traditional routines is the best choice (Safazadeh et al., 2018).
The relationship between knowledge and practice is vital to support clinical decision-making and the development of the nursing profession. One key aspect of nursing education is how to motivate students to learn effectively and desirably apply their knowledge in clinical practice (Shoghi et al., 2019).
Some student experiences indicate that using valid and updated knowledge acquired by learners from their peers in educational settings is sometimes met with resistance from clinical hospital staff. This condition seems to be due to various reasons, such as lack of time (Hashemiparast et al., 2019), heavy workloads, a routine and monotonous approach to care and a stressful clinical learning environment (Salifu et al., 2019).
The process of constructing professional identity occurs in relation to a reference group of other professionals, and this process takes place throughout one’s personal experience, starting from education and internships (Arreciado Marañón & Isla Pera, 2015). So, nursing mentors must create a knowledge channel that facilitates the sharing, transfer, and implementation of evidence-based guidelines.
To date, no study in the Italian context has compared the perceptions of nursing students and clinical mentors regarding the theory-practice gap phenomenon. Through an observational investigation, this study examines whether and how nursing students attending the bachelor of science (BS) in Nursing program and clinical internship tutors perceive a gap between the theory taught during lectures and the practical care provided during internships. The study also evaluates any factors that are opposing knowledge translation.
Materials and Methods
Study design, setting and sample
This research is an observational, cross-sectional study. The investigation includes the nursing BS programs at two Italian Universities (the University of Bari and the Polytechnic University of the Marche located in Ancona, Italy). Requests for participation in the study were sent to the responsible for didactic activities of the nursing BS degree programs. A questionnaire was prepared using Google Forms and distributed to participants through the program secretariats in a digital format. Responses were collected between June 1 and July 31, 2022. Participation in the study was voluntary, and the eligible samples were recruited using convenience sampling. They included all students enrolled in the third year of the nursing BS degree program or those who had completed it (n=107) and nurses currently serving as internship mentors (n=48).
Measurement and data collection
The research instrument is a customized questionnaire. The questions were designed to explore conceptual areas (pedagogical deficits, relational deficits) previously investigated in other semi-structured interviews from existing literature and adapted to the Italian context (Factor et al., 2017; Hashemiparast et al., 2019). The questionnaire consisted of two sections, one for students and one for internship tutors, each containing 7 items customized differently for the two participant groups. Participants are asked to respond by selecting the option that best reflects their perception and expressing their degree of agreement on a 4-point Likert scale, ranging from totally disagree=1 to totally agree=4.
For students, the questions were supposed to assess the perceived theory-practice gap, whether the student can identify the observed discrepancy, how they feel about it, whether they need to adapt to the context despite being aware of acting differently from theory and whether there has been interest and willingness to engage in discussions with the tutor. Complementary questions were posed to tutors, examining whether students were free in their perception to report the theory-practice gap and whether they provided satisfactory explanations in the presence of a discrepancy. The questionnaire also investigates the potential initiation of communication problems and the perceived necessity for students to adapt their behaviors to their context.
The questionnaire is further integrated with sociodemographic questions, including gender and age for students and tutors. Additionally, tutors were asked about their educational qualifications, years of work experience, and current working environment. The questionnaire demonstrated good internal consistency (α=0.752). The tool was evaluated by experts from the faculty and educational tutors of the Nursing degree course. After suggesting some modifications, the experts approved the tool.
Data analysis
The analysis was carried out using Jamovi software, version 2.3.18 and Microsoft Office Excel software. Descriptive statistics calculations were performed with a 95% confidence interval (CI). P were determined using the chi-square test for nominal and the t-test for ordinal variables. Correlations were calculated using the Spearman coefficient, and internal consistency was determined with the Cronbach α.
Results
The overall sample consisted of 107 students (69.0%) (group 1), including 83 women (77.5%) and 24 men (22.5%), with an mean age of 24.4±4.60 years, 48 (31.0%) clinical tutors (Group 2), including 34 women (77.0%) and 11 men (23.0%) with an mean age of 48.4±7.14 years. Regarding clinical tutors’ qualifications, 33.3% (n=16) held a regional diploma, 14,6% (n=7) had a BS, 22.9% (n=11) held a BS with post-basic training, 10.4% (n=5) held a master of science (MS), and 18.8% (n=9) had a MS with post-basic training. The working areas of clinical tutors were as follows: 20.8% (n=10) in surgical wards, 24.9% (n=12) in medical-specialized wards, 14.6% (n=7) in community hospitals, 12.5% (n=6) in critical care, 10.4% (n=5) in operating rooms, 8.3% (n=4) in medical wards, 6.3% (n=3) in outpatient clinics and 2.1% (n=1) in radiology and intensive care unit. Years of experience were classified, with 43.8% (n=21) having 16 to 25 years of experience and the same percentage having over 25 years of experience. Additionally, 12.5% (n=6) had work experience ranging from 1 to 15 years.
Significant differences were observed between the two groups for all items in the instrument (P<0.0001) (Table 1).
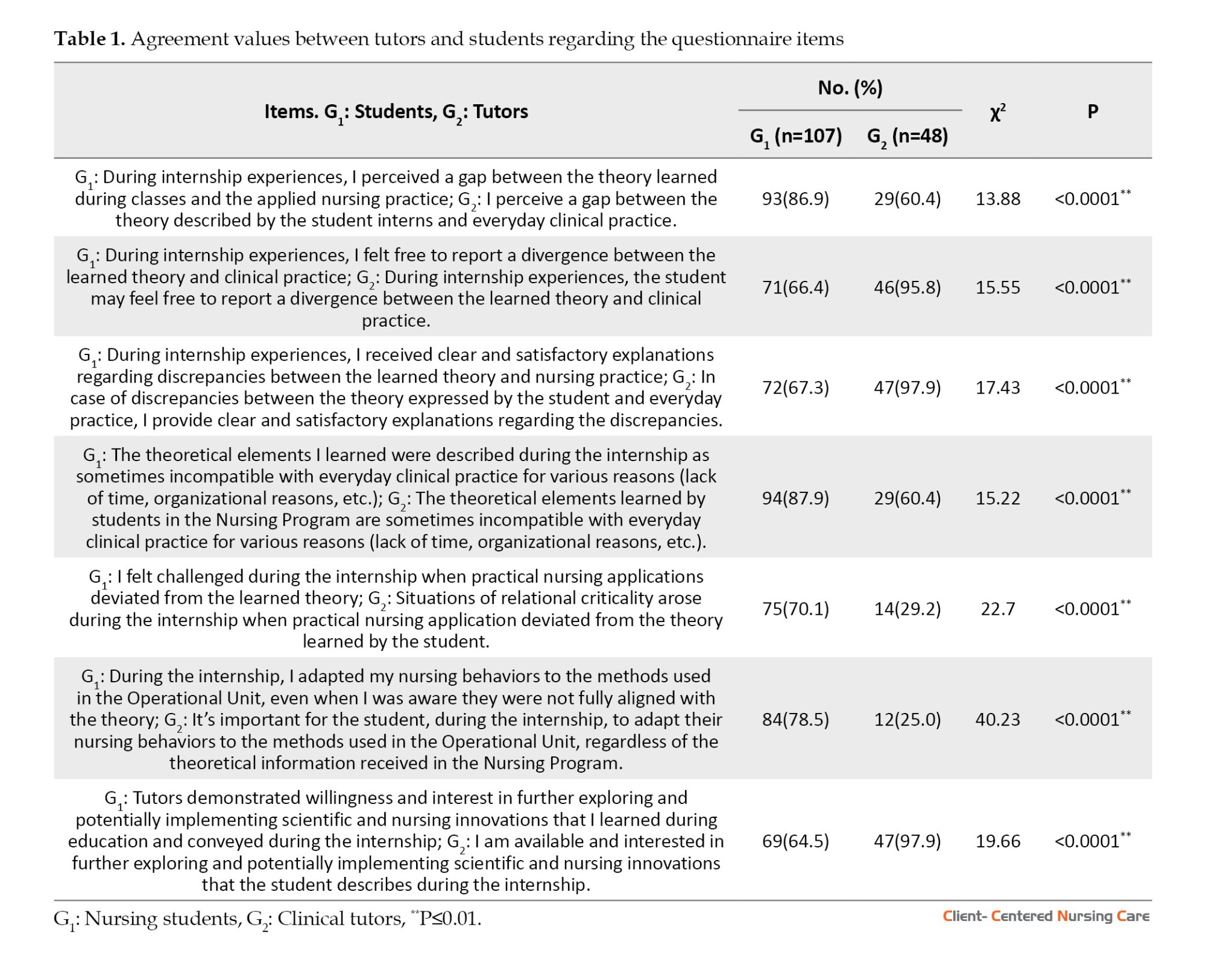
Parametric calculation using the t-test with the summation of Likert scores from all items in both groups confirmed a substantial difference between group 1 (Mean±SD=16.3±2.90; median=16.0) and group 2 (Mean±SD=20.7±2.37; median=20.5) (P<0.001).
In the group of tutors, when relating the independent variables (graduation, years of experience) to the dependent variables, it is evident that questions 1 and 4 appear to be significantly influenced by the professionals’ training and their experience with nursing students placed in their organizations (P=0.015 and P=0.026, respectively). The years of service did not significantly affect the answer to question number 7 in the group of tutors (Table 2). No relationship was found between the tutors’ agreement with the theory-practice gap and their experience in clinical training.
In the Spearman correlation matrix (Table 3), item 1 positively correlates with questions 3, 4, 5, 6 and 7. Item 7, which pertains to the tutor’s willingness to explore and implement new scientific and clinical developments in internship practice, correlates with all the questions in the questionnaire.
Discussion
Evidence suggests that students in clinical learning settings often struggle to match the theoretical content learned in the classroom with what they perform in practice (Hashemiparast et al., 2019). Meanwhile, the study by Factor et al., (2017) indicates that when students encounter clinical situations, they find it challenging to generalize and apply the nursing knowledge and theories they have learned. This condition arises because they discover discrepancies between what was learned in the classroom and how skills are carried out in the real-world context. We found that most third-year nursing students perceive a substantial gap between the theoretical education received and the clinical practice observed during internship periods. This perception was consistently confirmed irrespective of the age and gender of the participants. Even more cautiously, the same perception is significantly observed in the responses of internship tutors, regardless of their working experience. Evidence-based practice is crucial for university-level nursing education and graduates, serving as a way for the nursing discipline to minimize the gap between theory and practice (Mackey & Bassendowski, 2017).
This result is confirmed when over 70% of students express difficulty, perhaps also operational, aligning the concepts learned during theoretical education or laboratory practice with their experiences during clinical internships. This outcome is likely attributable to a generational gap concerning the innovative aspects brought by students. As years of experience increase, there tends to be a propensity for a more conservative approach rather than questioning what has already been learned. This tendency might also relate to the introduction of new scientific innovations. Another factor reinforcing the gap between theory and practice is apparent when analyzing the responses to item 4, which investigated potential incompatibilities between theory and everyday clinical practice. This issue may relate to the organizational situation of each operational unit. Factors such as staffing levels, work organization, time constraints, resource shortages, and the nurse-patient ratio appear to impact the ability to teach students. This finding is in line with the study by Hashemiparast et al. (2019), which discusses the system’s resistance to applying theoretical knowledge. The data suggest that clinical staff, due to various reasons like lack of time or resources, prevent students from applying theoretical knowledge taught in class.
The gap, clearly acknowledged by both parties, would still be bridged for two-thirds of the students through clear and satisfactory explanations provided by tutors upon students’ requests. Nonetheless, around 33% of students disagreed with this statement (item 3), suggesting an unresolved discomfort. This negative sentiment is more pronounced among male students, possibly stemming from inherent difficulties in interacting with tutors, who are predominantly female nursing professionals. Notably, 98% of tutors fully agree with the statement, hinting at a potentially defensive response. A similar pattern is observed in item 2, where over 90% of tutors express agreement, while only one in three students disagrees with the ability to freely express discordance between theory and practice. This partial but noteworthy communication challenge with tutors seems to manifest in students’ adaptive behavior to the practices of the clinical unit during their internships. Despite being aware of deviating from learned protocols, procedures, and guidelines, students adapt to the unit’s methods. This finding aligns with the study by Factor et al., (2017), which attributes this behavior to a structural deficit stemming from resource shortages and a lack of procedures and protocols, forcing students into improvisation and practice modification. However, this attitude is not shared by tutors, who believe in the importance of aligning theory and practice. Yet, in daily activities, as demonstrated by item 4, they struggle to integrate theory into everyday clinical practice. This partial but noteworthy communication challenge with tutors seems to manifest in students’ adaptive behavior to the practices of the clinical unit during their internships. Despite being aware of deviating from learned protocols, procedures and guidelines, students adapt to the unit’s methods. This sentiment is shared by nearly all tutors and 64.5% of students. The results of a study by Kaphagawani and Useh (2018) also confirmed this tendency, stating that tutors are not only eager to teach but are always available for students despite their growing workload.
The conducted study presents some limitations. Firstly, the number of participants in the survey, mainly clinical tutors, is limited. The second limitation is the lack of psychometrics of the instrument used. However, the instrument’s internal consistency has been confirmed and validated by experienced individuals. The cross-sectional nature of the study does not allow for causal conclusions. Despite these limitations, the study provides valuable insight into the current relevance of this topic within the clinical university environment, highlighting the need for active efforts from both sides to address the issue.
Conclusion
This study explored some possible motivations underlying the dichotomy between theory and practice in the clinical university context from the perspective of students and internship tutors. Addressing the issue of the theory-practice gap, particularly during the tutoring period, could represent one of the possible solutions to bridge the gap. The structured discussion moments during the mentoring period might prove beneficial. For instance, scheduling meetings among tutors, students, and course coordinators, especially in the early stages of the internship, could facilitate students’ inclination to express themselves. In any case, these critical moments could serve as a helpful tool for students to reflect on their knowledge and develop critical thinking. This investigation has provided further insights into the subject’s literature while raising additional questions. It would be advisable to maintain a high level of attention to the topic by conducting further studies that explore, through different inquiries, additional variables underlying the phenomenon.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of University of Bologna (Code: 0121436/2022). Participation was anonymous and obtained through informed consent by completing the questionnaire.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to this manuscript.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Participants in the study and the collaborating universities are appreciated for contributing to the research.
References
Arreciado Marañón, A. & Isla Pera, M. P., 2015. Theory and practice in the construction of professional identity in nursing students: A qualitative study. Nurse Education Today, 3(7), pp. 859-63. [DOI:10.1016/j.nedt.2015.03.014] [PMID]
Burgess, A., van Diggele, C. & Mellis, C., 2018. Mentorship in the health professions: A review. The Clinical Teacher, 15(3), pp. 197-202. [DOI:10.1111/tct.12756] [PMID]
Factor, E. M. R. Matienzo, E.T. & de Guzman, A. B., 2017. A square peg in a round hole: Theory-practice gap from the lens of Filipino student nurses. Nurse Education Today, 57, pp. 82-7. [DOI:10.1016/j.nedt.2017.07.004] [PMID]
Ahmari Tehran, H., et al., 2021. ‘The challenges of clinical education in nursing: A qualitative analysis of nursing students and clinical instructors’ perspectives. Journal of Nursing and Midwifery Sciences, 8(4), pp. 260-7. [Link]
Hashemiparast, M., Negarandeh, R. & Theofanidis, D., 2019. ‘Exploring the barriers of utilizing theoretical knowledge in clinical settings: A qualitative study. International Journal of Nursing Sciences, 6(4), pp. 399–405. [DOI:10.1016/j.ijnss.2019.09.008] [PMID] [PMCID]
Kaphagawani, N. C. & Useh, U., 2018. Clinical Supervision and Support: Exploring pre-registration nursing students’ clinical practice in Malawi.’ Annals of Global Health, 84(1), pp. 100-9. [DOI:10.29024/aogh.16] [PMID] [PMCID]
Mackey, A. & Bassendowski, S., 2017. The history of evidence-based practice in nursing education and practice. Journal of Professional Nursing, 33(1), pp. 51-5. [DOI:10.1016/j.profnurs.2016.05.009] [PMID]
NgozikaUgwu, S., et al., 2023. Causes and effects of theory-practice gap during clinical practice: The lived experiences of baccalaureate nursing students. International Journal of Qualitative Studies on Health and Well-Being, 18(1), pp. 2164949. [DOI:10.1080/17482631.2023.2164949] [PMID] [PMCID]
Safazadeh, S., et al., 2018. Exploring the reasons for theory-practice gap in emergency nursing education: A qualitative research. Journal of Education and Health Promotion, 7, pp. 132. [DOI:10.4103/jehp.jehp_25_18] [PMID] [PMCID]
Saifan, A., et al., 2021. Solutions to bridge the theory-practice gap in nursing education in the UAE: A qualitative study. BMC Medical Education, 21(1) pp. 490. [DOI:10.1186/s12909-021-02919-x] [PMID] [PMCID]
La Sala, R., et al., 2021.Competence assessment of the clinical tutor: A multicentric observational study. Acta Bio-Medica : Atenei Parmensis, 92(Suppl 2), pp. e2021016. [PMCID]
Salifu, D. A., et al., 2019. Experiences and perceptions of the theory-practice gap in nursing in a resource-constrained setting: A qualitative description study.’ Nursing Open, 6(1), pp. 72–83. [DOI:10.1002/nop2.188] [PMID] [PMCID]
Type of Study: Research |
Subject:
General
Received: 2023/12/16 | Accepted: 2024/02/7 | Published: 2024/08/1
Received: 2023/12/16 | Accepted: 2024/02/7 | Published: 2024/08/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |